Abstract
Background and Objectives
Much of the research surrounding firefighter health has concerned the hazards intuitively associated with the occupation, such as physical, thermal, and chemical risks. However, an additional aspect of their work environment, psychosocial stressors, has begun to attract a growing level of attention. Work‐related psychosocial stress may best be described as mental and emotional strain caused by a combination of workplace events and characteristics, and the objective of our review was to identify the health outcomes associated with these stressors in firefighters.
Methods
A systematic review was performed of studies reporting on the psychosocial stressors and the associated health outcomes experienced by firefighters. Data sources included the MEDLINE, PsychInfo, and CINAHL databases.
Results
Twenty‐nine studies met the inclusion criteria. Upon analysis, we found that firefighters experienced a range of psychosocial stressors (including interpersonal conflict and concerns over organizational fairness) and observed that these stressors were associated with a number of health‐related outcomes that could be arranged into six areas: depression‐suicidality, non‐depressive mental health problems, burnout, alcohol use disorders, sleep quality, and physiological parameters and somatic disorders.
Conclusion
Our findings strongly suggest that work‐related psychosocial stressors can affect the health and well‐being of those in the fire service, and highlight that interventions meant to address these psychosocial risk factors should focus upon promoting self‐esteem, enhancing self‐efficacy, and strengthening social support.
Keywords: firefighter, first responder, health and well‐being, mental health, psychosocial stress
1. INTRODUCTION
Although certain factors are common across nearly all occupations, there can be little doubt that some occupational groups are comparatively unique. One of the best examples of such a group is public safety personnel, whose members undertake work that may routinely present significant emotional, psychological, and physical challenges. Indeed, one of these groups, the fire service, engages in a wide range of tasks that serve to clearly set them apart. For example, in many jurisdictions, firefighting has progressed from the already significant responsibilities related to fire prevention and suppression to also include rescue operations, hazardous material response, and the provision of emergency medical services. 1 , 2 As well, changes in a variety of contextual factors, such as residential fire dynamics, the growth of wildland–urban interfaces, and demographic shifts, have further complicated work within the fire service. 3 , 4 , 5
As might be expected, given their essential role in emergency preparedness, the occupational environment of firefighters has been the focus of much research, and this effort has helped to establish that their working conditions are linked to a variety of health concerns. 6 , 7 , 8 Over the past few decades, much of the research investigating firefighter health has concerned the sort of hazards that would intuitively be associated with the occupation, such as physical, thermal, ergonomic, and chemical risks. In addition, attention has been directed at the effects of traumatic/critical incidents. 9 , 10 However, an additional aspect of their environment—psychosocial workplace stressors—has begun to attract a growing level of attention.
Job‐related psychosocial stress may best be described as a combination of work events and characteristics that affect individuals by applying mental and emotional strain, and has become the subject of heightened interest given evidence that these factors can negatively affect the health of an individual, regardless of company size, area of expertise, or their position within the company. 11 For example, a meta‐analytical review investigating psychosocial stress in the work environment and mental health outcomes supported the notion that exposure to such stressors prospectively increased the risk of common mental health disorders. 12 As well, a subsequent systematic review also found strong evidence for an association of work‐related, psychosocial stressors with the incidence of various stress‐related disorders. 13 In addition, ongoing exposure to psychosocial stressors can lead to fatigue, burnout, and a variety of chronic diseases within a workforce. 11 , 14 Similarly, a number of health‐related behaviors associated with chronic disease development (eg, smoking, alcohol abuse, and physical inactivity) have been linked with exposure to psychosocial stressors. 15 , 16 , 17
As research into the influence of psychosocial stressors experienced by firefighters has steadily grown, there is a need to identify and synthesize the evidence highlighting the effect of these stressors on the general health of this occupational group. Therefore, the objective of our review was to investigate the academic literature to answer the following key research question: what health outcomes are associated with the work‐related psychosocial stressors typically experienced by those within the fire service?
2. METHODS
2.1. Search strategy and selection criteria
A review of the literature was carried out by two of the researchers (SI and JM) employing a strategy developed by all of the authors. Those databases thought to possess the most relevant journals were searched (Medline, CINAHL, and PsychINFO) using MeSH terms and author keywords, such as stress, psychosocial stress, firefighters, burnout, emotional disorders, and chronic disorders/illness (a detailed description of the search strategies can be found in the appendix). Prior to beginning the search, a protocol outlining both the eligibility criteria and extraction procedure was developed. For inclusion, articles were required to have (1) been published in the English language, (2) involved a general sampling of firefighters (as opposed to including only participants with a particular experience, such as traumatic exposure) (3) measured psychosocial stress, (4) assessed at least one health‐related outcome, and (5) applied an analytical method to directly examine the nature of the association between psychosocial stress and a health‐related outcome.
Although many studies investigated different stressors pertaining to firefighters (such as toxicant exposure), we focused on those that specifically investigated some element of psychosocial stress. As effects upon firefighter health and well‐being were the outcome of interest for our review, any article measuring physiological, pathological, psychological, or behavioral changes was captured for further assessment. Notably, previous systematic reviews, conference proceedings, and editorials were excluded. Duplicates were identified and removed using a RefWorks database. Articles meeting eligibility criteria underwent full‐text review, and their accompanying reference lists were perused for additional articles not identified in the original search.
2.2. Data extraction and analysis
The Cochrane Consumers and Communication Review Group data extraction template guided the development of our data extraction procedure; 18 information was collected on study location and design, sample characteristics, tools used for psychosocial stress measurement, health outcomes examined, and the primary findings (which were summarized in both a qualitative and quantitative manner). To assist in the evaluation of the assembled reports, we assigned a design and reporting score (DRS) to each one based upon whether the study included eight items that we felt were important elements: a statement that the study had undergone review by an ethics committee, a statement that informed consent had been sought, a description of participant characteristics (at a minimum, age and gender), a description of the psychometric properties of the stress measurement tool (that is, Cronbach's alpha), an informative description of the health outcome measurement tool (typically, a meaningful summary of the tool together with at least one relevant citation), the provision of descriptive statistics for the measurement tools (minimally, the mean and standard deviation of scores, or values for at least one of the instruments used), a comment regarding whether the assumptions underlying the analytical tools were considered (eg, normality, or collinearity), and consideration regarding potential study limitations. Notably, the 29 reports tended to display most of the items on our checklist (average DRS = 5.8, standard deviation = 1.4). Two reviewers (SI and JM) independently examined each study and settled any disagreements related to data extraction through discussion leading to consensus.
3. RESULTS
3.1. Study and sample characteristics
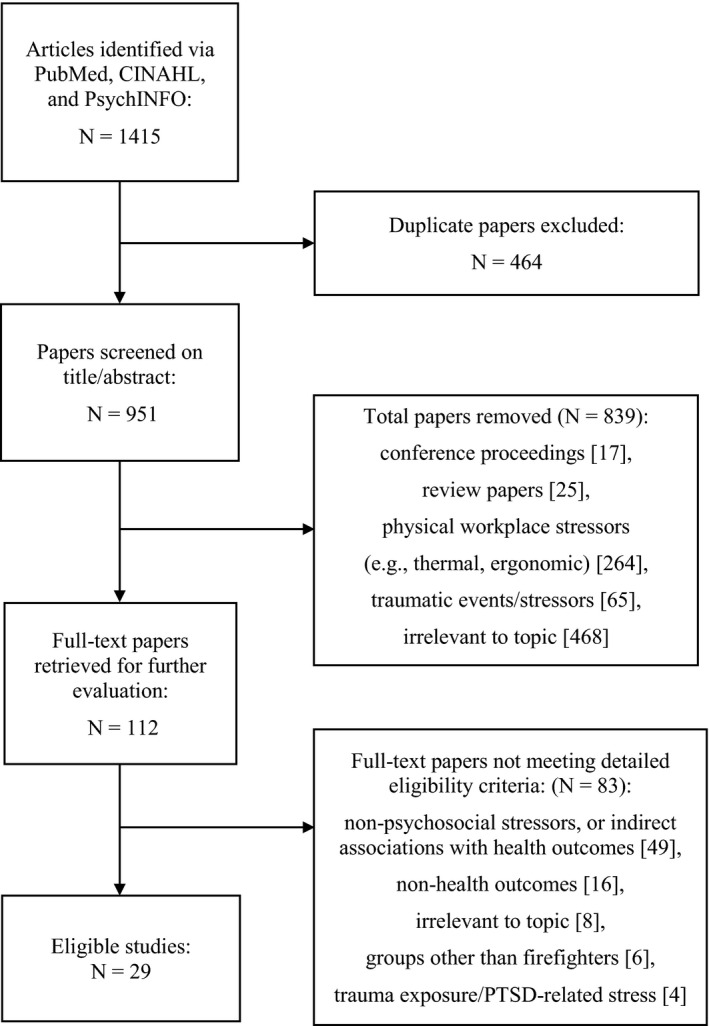
Our initial literature search returned 1415 articles, which were then screened for eligibility (a description of the identification and screening process may be found in the appendix). After removing duplicates, we reviewed titles and abstracts and eliminated those reports not fitting our inclusion criteria, which left 112 studies. After a full‐text review and evaluation of associated reference lists (to identify relevant articles that may not have been captured in our database search), we settled on 29 studies investigating psychosocial stress and its association with some aspect of firefighter health.
During the analysis, a noticeable degree of methodological heterogeneity was observed across the eligible articles. For example, significant variation was found in the measurement tools used for the evaluation of psychosocial stress; in particular, 15 different scales were used, with the most common one (the Korean Occupational Stress Scale) appearing in 6 studies, and most appearing in only a single report. In addition, 18 separate health‐related signs, symptoms, or disorders were assessed, with similar ones often examined using more than one tool; for instance, the four studies focused on excessive alcohol use employed three different scales. As a result, the extracted data were not considered appropriate for a meta‐analysis; instead, we chose to arrange the reports according to six themes (each of which were discussed in at least three reports): depression‐suicidality, non‐depressive mental health problems, burnout, alcohol use disorders, sleep quality, and physiological parameters and somatic disorders (Tables 1, 2, 3, 4, 5, 6). Notably, some reports assessed more than a single health outcome, and were therefore placed under more than one theme.
TABLE 1.
Characteristics and key findings from studies examining the relationship between psychosocial stressors and depression‐suicidality in firefighters
| Author, year of publication (DRS) | Study location | Study design | Sample size | Psychosocial stress measurement tool | Health outcome; measurement tool | Core results: narrative | Core results: quantitative |
|---|---|---|---|---|---|---|---|
|
An et al, 2015 (4/8) |
Seoul, South Korea |
longitudinal (panel design with two waves of data collection) |
186 men |
Korean Occupational Stress Scale, short form |
depression; Korean version of the Beck Depression Inventory |
Risk of depression was inversely related to how positively a firefighter viewed their organizational system. | OR (adjusted for age, job class, and shift work) for depression with high organizational system stress (including 95% CIs): 8.03; 1.73, 37.22 |
|
Carpenter et al, 2015 (7/8) |
USA (various urban settings) |
cross‐sectional |
299 men 35 women |
Sources of Occupational Stress scale, short form |
suicidal ideation; ideation item from either the Beck Depression Inventory – II, or from the Beck Depression Inventory for Primary Care |
Suicidal ideation was more prevalent amongst those reporting higher levels of occupational stress. | individuals with above median levels of occupational stress reported having at least 1 episode of suicidal ideation [χ2(1) = 5.10, Fisher's exact P =.035] |
|
Jahnke et al, 2019 (8/8) |
USA and Canada | cross‐sectional |
1773 women (~98% from USA) |
Chronic Work Discrimination and Harassment, abbreviated scale |
depression; Center for Epidemiologic Studies – short depression scale |
The risk of depression increased with the level of perceived discrimination and harassment. | those with the highest level of perceived discrimination and harassment had an elevated risk of depressive symptoms (OR = 4.20; 95% CI = 3.25, 5.67) |
|
Park et al, 2019 (5/8) |
South Korea | cross‐sectional |
42 326 men 3372 women |
Korean Occupational Stress Scale, difficult physical environment sub‐scale |
suicidal ideation; Suicidal Behaviors Questionnaire, revised |
Occupational stress from the physical work environment influenced an increase in suicidal ideation. | high occupational stress increased risk for suicidal ideation in the past year (OR = 1.19; 95% CI = 1.16, 1.22) |
|
Payne & Kinman, 2019 (7/8) |
United Kingdom | cross‐sectional |
773 men 136 women |
Health and Safety Executive Management Standards Tool |
work‐related anxiety and depression; Warr's scale of job‐related affective well‐being, modified version |
Job demands and job resources significantly contributed to work‐related depression. | relationship conflicts (β = 0.17, P <.001) and a sense of control (β = 0.09, P <.01) were significantly associated with work‐related depression |
|
Saijo et al, 2007 (5/8) |
Hokkaido, Japan | cross‐sectional |
1626 men 46 women (same data set used in Saijo et al, 2008) |
National Institute for Occupational Safety and Health generic job stress questionnaire, Japanese version |
depression; Center for Epidemiologic Studies – depression scale |
High variance in workload, high intergroup conflict, high role conflict, and low self‐esteem significantly increased risk for depressive symptoms. |
high variance in workload (OR; 95% CIs): 2.05; 1.29, 3.25 high intergroup conflict: 1.91; 1.26, 2.88 high role conflict: 1.87; 1.24, 2.80 low self‐esteem: 5.78; 3.93, 8.50 |
|
Saijo et al, 2008 (6/8) |
Hokkaido, Japan | cross‐sectional |
1209 men 92 women (same data set used in Saijo et al, 2007, with a focus on those working 24 h shifts) |
National Institute for Occupational Safety and Health generic job stress questionnaire, Japanese version |
depression; Center for Epidemiologic Studies – depression scale |
High variance in workload, high intergroup conflict, high role ambiguity, and low self‐esteem significantly increased risk for depressive symptoms. |
high variance in workload (OR; 95% CIs): 2.08; 1.22, 3.56 high intergroup conflict: 1.70; 1.02, 2.85 high role ambiguity: 1.63; 1.04, 2.56 low self‐esteem: 5.16; 3.32, 8.01 |
|
Stanley et al, 2018 (8/8) |
southern USA (urban setting) |
cross‐sectional |
785 men 40 women 6 transgender |
Sources of Occupational Stress scale, short form |
depression; Center for Epidemiologic Study – depression scale |
Occupational stress and depressive symptoms showed a linear relationship. | occupational stress was significantly correlated with depressive symptoms (r = 0.48, P <.01) |
|
Stanley et al, 2018 (8/8) |
southern USA (urban setting) |
cross‐sectional |
785 men 40 women 6 transgender |
Sources of Occupational Stress scale, short form |
suicidal ideation; Suicidal Behaviors Questionnaire, revised |
Increasing occupational stress predicted greater levels of suicidal ideation and behavior. | lifetime suicidal ideation (β = 0.013, P <.001), past year suicidal ideation (β = 0.006, P <.005), lifetime suicide threats (β = 0.003, P <.003), and current suicidal intent (β = 0.008, P <.003) were significantly associated with work‐related stress |
BDI, Beck Depression Inventory; CI, confidence interval; DRS, design and reporting score; OR, odds ratio; SOOS, sources of occupational stress.
TABLE 2.
Characteristics and key findings from studies examining the relationship between psychosocial stressors and non‐depressive mental health problems in firefighters
|
Author, year of publication (DRS) |
Study location | Study design | Sample size | Psychosocial stress measurement tool | Health outcome; measurement tool | Core results: narrative | Core results: quantitative |
|---|---|---|---|---|---|---|---|
|
Jahnke et al, 2019 (8/8) |
USA and Canada | cross‐sectional |
1773 women (~98% from USA) |
Chronic Work Discrimination and Harassment, abbreviated scale |
anxiety; Mental Health Inventory, anxiety sub‐scale |
More symptoms of anxiety over the past month were observed in firefighters with the highest level of perceived discrimination and harassment. | Those in the highest tertile of perceived discrimination and harassment reported approximately 30% more symptoms of anxiety than those in the lowest tertile (P <.001) |
|
Jahnke et al, 2019 (8/8) |
USA and Canada | cross‐sectional |
1773 women (~98% from USA) |
Chronic Work Discrimination and Harassment, abbreviated scale |
PTSD; Trauma Screening Questionnaire |
The risk of PTSD‐related symptoms increased with the level of perceived discrimination and harassment. | those with the highest level of perceived discrimination and harassment had an elevated risk of PTSD symptoms (OR = 2.67; 95% CI = 1.82, 3.93) |
|
Mitani et al, 2006 (4/8) |
Japan (1 rural fire service, 1 urban fire service) |
cross‐sectional |
237 men 4 women |
Japan Brief Job Stress Questionnaire |
PTSD; revised Impact Event Scale, Japanese version |
A greater amount of perceived job stress was associated with a greater frequency of self‐reported post‐traumatic symptoms. | job stress was significantly correlated with PTSD symptoms (r = 0.37, P <.01) |
|
Payne & Kinman, 2019 (7/8) |
United Kingdom | cross‐sectional |
773 men 136 women |
Health and Safety Executive Management Standards Tool |
work‐related anxiety and depression; Warr's scale of job‐related affective well‐being, modified version |
Job demands and job resources significantly contributed to work‐related anxiety. | relationship conflicts (β = 0.12, P <.01) and role clarity (β = 0.08, P <.05) were significantly related to work anxiety |
|
Saijo et al, 2012 (6/12) |
Hokkaido, Japan | cross‐sectional |
1621 men 46 women |
National Institute for Occupational Safety and Health generic job stress questionnaire, Japanese version |
PTSD; Impact of Event scale – revised, Japanese version |
After adjustment for age and gender, the PTSD‐positive group endorsed significantly higher inter‐group conflict and role ambiguity, and lower social support from supervisors. |
When comparing high vs low PTSD groups: high role ambiguity: Cohen's d = 0.27, P =.002 low social support from supervisor: Cohen's d = 0.22, P =.19 |
|
Teoh et al, 2019 (7/8) |
Minas Gerais, Brazil | cross‐sectional |
276 men 36 women |
Job Stress Scale, Portuguese version |
psychiatric morbidity; self‐report questionnaire |
Increased job demands lead to greater psychiatric morbidity, whereas improved job control had a beneficial effect. | job demands (β = 0.12, P <.05) and job control (β = −0.30, P <.001) were significant predictors of psychiatric morbidity |
CI, confidence interval; DRS, design and reporting score; OR, odds ratio; PTSD, post‐traumatic stress disorder.
TABLE 3.
Characteristics and key findings from studies examining the relationship between psychosocial stressors and burnout in firefighters
| Author, year of publication (DRS) | Study location | Study design | Sample size | Psychosocial stress measurement tool | Health outcome; measurement tool | Core results: narrative | Core results: quantitative |
|---|---|---|---|---|---|---|---|
|
Angelo & Chambel, 2015 (6/8) |
Portugal (sampling from all 18 districts) |
longitudinal (panel design with two waves of data collection) |
586 men 65 women |
Organizational Demand Scale |
burnout; emotional exhaustion and cynicism sub‐scales of the Maslach burnout inventory, general version |
Increased perception of organizational demands predicted likelihood of burnout, which, in turn, was associated with an altered perception of job demands. |
organizational demands had a positive, cross‐lagged effect on burnout (β = 0.10, P <.05) |
|
Makara‐Studzinska et al, 2019 (8/8) |
Poland (sampling from 12 different provinces) |
cross‐sectional |
580 men |
Perceived Stress Scale |
burnout; Link Burnout Questionnaire (LBQ) |
Perceived stress was associated with most domains measured by the LBQ (psychophysical exhaustion, sense of professional inefficacy, disillusion), but not all (relationship deterioration). | perceived stress significantly influenced psychophysical exhaustion (β = 0.92, P <.001), sense of professional inefficacy (β = 0.61, P =.005), and disillusion (β = 1.64, P =.004) |
|
Makara‐Studzinska et al, 2020 (5/8) |
Poland (sampling from 12 different provinces) |
cross‐sectional |
576 men |
Perceived Stress Scale |
burnout; Link Burnout Questionnaire (LBQ) |
Perceived stress was correlated with all four domains captured by the LBQ. | perceived stress was significantly correlated with psychophysical exhaustion (r = 0.49, P <.001), relationship deterioration (r = 0.30, P <.001), sense of professional inefficacy (r = 0.36, P <.001), and disillusion (r = 0.46, P <.001) |
|
Mitani et al, 2006 (4/8) |
Japan (1 rural fire service, 1 urban fire service) |
cross‐sectional |
237 men 4 women |
Japan Brief Job Stress Questionnaire |
burnout; Maslach burnout inventory |
Social support was negatively correlated with, and job stress was positively correlated with, certain burnout sub‐scales (emotional exhaustion and de‐personalization). |
social support (r = ‐0.32, P <.01) and job stress (r = 0.60, P <.01) were correlated with emotional exhaustion social support (r = ‐0.36, P <.01) and job stress (r = 0.51, P <.01) were correlated with depersonalization |
|
Smith et al, 2019 (8/8) |
southeastern USA (urban setting) |
cross‐sectional |
198 men 10 women |
Perceived Work Stress Scale (derived from Cohen's Perceived Stress Scale) |
burnout; Malach‐Pines burnout scale |
Work stress showed a strong, positive association with burnout. |
work stress significantly predicted burnout (β = 0.50, P <.01) |
CI, confidence interval; DRS, design and reporting score; LBQ, Link burnout questionnaire; OR, odds ratio.
TABLE 4.
Characteristics and key findings from studies examining the relationship between psychosocial stressors and alcohol abuse in firefighters
| Author, year of publication (DRS) | Study location | Study design | Sample size | Psychosocial stress measurement tool | Alcohol abuse measurement tool | Core results: narrative | Core results: quantitative |
|---|---|---|---|---|---|---|---|
|
Arbona et al, 2017 (6/8) |
southwestern USA (urban setting) |
cross‐sectional |
1036 men |
Perceived Stress Scale (PSS‐10) | Rapid Alcohol Problems Screen (RAPS‐4) | Higher levels of perceived stress were observed among those with higher levels of alcohol abuse. |
greater RAPS‐4 scores significantly predicted greater PSS‐10 scores [β(black) = 0.13; β(Latino) = 0.22; P <.001] |
|
Hosoda et al, 2012 (4/8) |
Tottori prefecture, Japan | cross‐sectional |
246 men |
Brief Job Stress Questionnaire | alcohol use disorders identification test (AUDIT) | A poor perception of one's workplace environment showed a positive relationship with alcohol dependence. | perceptions of workplace environment and AUDIT scores were significantly correlated (r = 0.13, P =.047) |
|
Jahnke et al, 2019 (8/8) |
USA and Canada | cross‐sectional |
1773 women (~98% from USA) |
Chronic Work Discrimination and Harassment, abbreviated scale | CAGE questionnaire | The risk of alcohol abuse increased with the level of perceived discrimination and harassment. | those with the highest level of perceived discrimination and harassment had an elevated risk of alcohol abuse (OR = 1.54; 95% CI = 1.09, 2.17) |
|
Kim et al, 2018 (8/8) |
Gyeonggi province, South Korea | cross‐sectional |
6484 men 667 women |
Korean Occupational Stress Scale, short form |
Alcohol Use Disorders Identification Test (AUDIT) |
Perceived job stress was associated with an increased likelihood of alcohol abuse. |
AUDIT scores significantly predicted greater perceived stress (β = 0.007, P <.001) |
AUDIT, alcohol use disorders identification test; CAGE, “cut‐annoyed‐guilty‐eye”; CI, confidence interval; DRS, design and reporting score; OR, odds ratio; PSS, perceived stress scale; RAPS, rapid alcohol problems screen.
TABLE 5.
Characteristics and findings from studies measuring psychosocial stressors and their relationship with sleep disorders in firefighters
|
Author, Year of Publication (DRS) |
Study Location |
Study Design | Sample Size | Psychosocial Stress Measurement Tool | Health Outcome; Measurement Tool |
Core Results: narrative |
Core Results: quantitative |
|---|---|---|---|---|---|---|---|
|
Haddock et al, 2013 (6/8) |
midwestern USA (11 sites in 8 states) |
cross‐sectional |
458 men |
Perceived Stress Scale |
excessive daytime sleepiness (EDS); Epworth sleepiness scale |
Perceived stress was not associated with excessive daytime sleepiness. | the effect size (Cohen's d) of the difference in perceived stress between those with and without off‐duty EDS was 0.16 |
|
Lim et al, 2014 (5/8) |
South Korea (metropolitan region) | cross‐sectional |
657 men |
Korean Occupational Stress Scale (KOSS), short form |
sleep quality; Pittsburgh Sleep Quality Index, Korean version |
Although occupational stress was correlated with most KOSS sub‐scales, total stress was not able to predict poor sleep quality. | occupational stress did not increase risk for poor sleep quality (OR = 0.93; 95% CI = 0.93, 2.72) |
|
Yook, 2019 (7/8) |
Seoul, South Korea | cross‐sectional |
705 men |
Korean Occupational Stress Scale |
sleep quality; Pittsburgh Sleep Quality Index (PSQI), Korean version |
Occupational stress impaired each of the seven sub‐factors measured by the PSQI. | occupational stress was significantly correlated with a reduced PSQI score (r = 0.276, P =.001) |
Abbreviations CI, confidence intervals; DRS, design and reporting score; EDS, excessive daytime sleepiness; KOSS, Korean Occupational Stress Scale; OR, odds ratio; PSQI, Pittsburgh Sleep Quality Index.
TABLE 6.
Characteristics and key findings from studies examining the relationship between psychosocial stressors and physiological parameters and somatic disorders in firefighters
| Author, year of publication (DRS) | Study location | Study design | Sample size | Psychosocial stress measurement tool(s) | Health outcome; measurement tool |
Core results: narrative |
Core results: quantitative |
|---|---|---|---|---|---|---|---|
|
Choi et al, 2016 (6/8) |
USA (southern California) |
cross‐ sectional |
321 men 9 women |
Job Content Questionnaire Effort‐Reward Imbalance Questionnaire |
hypertension; systolic BP ≥ 140 mmHg, diastolic BP ≥ 90 mmHg, or anti‐hypertensive medication use |
Systolic BP was slightly higher among male firefighters who felt their job had grown more demanding over the past few years. | those who perceived an increase in work demand displayed a slight increase in BP (2.7 mmHg; P =.058) |
|
Damrongsak et al, 2017 (6/8) |
USA (southeastern urban centre) |
cross‐ sectional |
298 men |
Job Stress Survey |
back pain; health risk appraisal questionnaire |
Occupational stress was not observed to increase risk for current back pain. | occupational stress (particularly, job pressure and lack of organizational support) did not increase risk for current back pain (OR = 1.02; P =.17) |
|
Jang et al, 2016 (6/8) |
South Korea |
cross‐sectional |
1140 men 77 women (same data set used in Jang et al, 2017) |
Korean Occupational Stress Scale |
gastro–oesophageal reflux disease (GERD); Montreal criteria |
Job demands, interpersonal conflict, lack of reward, and occupational climate increased risk for GERD. |
(OR; 95% CIs) job demands (1.83; 1.34, 2.52) interpersonal conflict (2.07; 1.06, 3.51) lack of reward (2.17; 1.21, 3.88) occupational climate (1.49; 1.09, 2.02) |
|
Jang et al, 2017 (6/8) |
South Korea |
cross‐ sectional |
1140 men 77 women (same data set used in Jang et al, 2016) |
Korean Occupational Stress Scale |
functional gastrointestinal disorders of the digestive system (FGIDS); Rome III criteria |
Job demands, interpersonal conflict, and lack of reward increased risk for FGIDS. |
(OR; 95% CIs) job demands (1.79; 1.11, 2.89) interpersonal conflict (2.21; 1.25, 4.33) lack of reward (2.39; 1.08, 5.26) |
|
Kim et al, 2013 (4/8) |
South Korea |
cross‐ sectional |
21,466 men (same data set used in Kim et al, 2017) |
Korean Occupational Stress Scale, short form |
work‐related musculoskeletal disorders; Korean National Institute of Occupational Safety and Health Symptom survey |
Job demands, job insecurity, organizational system, lack of reward, and occupational climate increased risk for musculoskeletal disorders. |
(adjusted OR; 95% CIs) job demands (1.52; 1.35, 1.70) job insecurity (1.14; 1.01, 1.28) organizational system (1.37; 1.21, 1.58) lack of reward (2.39; 1.08, 5.26) occupational climate (1.24; 1.11, 1.40) |
|
Kim et al, 2017 (4/8) |
South Korea | cross‐ sectional |
24,209 Men (same data set used in Kim et al, 2013) |
Korean Occupational Stress Scale, short form |
lower back pain; Korean Occupational Safety and Health Agency screening criteria | Job demands, and organizational injustice increased risk for lower back pain in a graded manner. |
(adjusted OR; 95% CIs) job demands (1.55; 1.35, 1.77) organizational injustice (1.53; 1.04, 2.24) |
|
Shin et al, 2016 (3/8) |
South Korea |
cross‐ sectional |
645 men |
Korean Occupational Stress Scale |
heart rate variability (HRV); measured in time and frequency domains |
After adjustment, occupational climate and organizational system reduced certain HRV parameters. | low assessment of occupational climate reduced HRV parameters in both time and frequency domains (P <.05); low view of organizational system reduced HRV in a frequency domain parameter (P <.05) |
|
Soteriades et al, 2019 (5/8) |
Cyprus | cross‐sectional |
380 men 50 women |
Copenhagen Psychosocial Questionnaire, stress sub‐scale |
musculoskeletal (MSK) problems; Nordic Musculoskeletal Questionnaire |
Increased work‐related stress was associated with more MSK problems. | those scoring above the mean level on the stress sub‐scale had an increased risk of MSK problems (OR = 1.52; 95% CI = 1.02, 2.25) |
|
Yook, 2019 (7/8) |
Seoul, South Korea | cross‐sectional |
705 men |
Korean Occupational Stress Scale |
heart rate variability; measured in time and frequency domains |
Occupational stress was not able to predict HRV in either the time, or frequency domain. |
occupational stress was not correlated with HRV domains: SDNN (r = 0.027, P =.47), RMSSD (r = 0.036, P =.34), logLF (r = 0.011, P =.77), logHF (r = 0.008, P =.84) |
BP, blood pressure; CI, confidence interval; DRS, design and reporting score; FGIDS, functional gastrointestinal disorders of the digestive system; GERD, gastro‐oesophageal reflux disease; HF, high‐frequency band; HRV, heart rate variability; LF, low‐frequency band; MSK, musculoskeletal; OR, odds ratio; RMSSD, root mean square of successive differences between heartbeats; SDNN, standard deviation of the normal‐to‐normal sinus‐initiated inter‐beat interval.
Most of the studies used a cross‐sectional design (27/29), with only two using a longitudinal design. 19 , 20 A clear majority of the reports focused upon firefighters within either Asia (15/29; particularly, South Korea), or the United States (8/29), with the remaining studies drawn from South American (1/29) and European (5/29) populations. The total number of participants investigated across the studies was 89,262 with sample sizes ranging from 186 to 45,698 (median = 651). Overall, 15 studies examined both male and female firefighters, 12 reports focused solely on male firefighters, 1 study involved just female firefighters, 21 and 1 report considered male, female and transgender firefighters. 22
3.2. Psychosocial stressors and depression‐suicidality
We identified eight studies that examined whether an association was present between psychosocial stressors and depression‐suicidality in firefighters (Table 1). Most of the selected reports focused upon depression, and they consistently observed that work‐related psychosocial stress could influence the likelihood that a firefighter would experience depressive symptoms. For example, An et al, 19 one of the two longitudinal studies that we encountered, observed that a high‐level of stress rooted in a firefighter's organizational system caused a marked increase in their risk for depression (OR 8.03; 95% CI: 1.73, 37.22); within the study, organizational system stress was largely related to how employees viewed their organization's fairness, the level of organizational support they received, and whether they believed their position and progress were appropriate relative to their abilities. In addition, we found three cross‐sectional reports 22 , 23 , 24 that made use of the Center for Epidemiologic Study Depression Scale, and each one observed a positive relationship between occupational stress and depressive symptoms; notably, the two reports from Saijo et al 23 , 24 found a high variance in workload and high intergroup conflict were among the most important factors influencing the association between occupational stress and depressed mood. Similarly, another report that used a different measure of work‐related well‐being found that relationship conflicts were a significant variable underlying depressed mood. 25 The final depression‐related study that we located was unique among all of the work that we reviewed, in that the investigators focused just on female firefighters. 21 The authors noted that the risk of depressive symptoms increased with the level of perceived work‐related discrimination, and the risk profile was clearest among those experiencing the greatest levels of harassment (OR 4.20; 95% CI: 3.25, 5.67).
Two of the reports that addressed the relationship between occupational stress and suicidality in firefighters used the revised Suicide Behaviors Questionnaire (SBQ‐R), 26 whereas the remaining study used the suicidal ideation item from the Beck Depression Inventory. With a sample of nearly a thousand participants, the first report 22 found that scores on the Sources of Occupational Stress Scale (which captures many of the psychological stressors inherent in firefighting) 27 were able to significantly predict each of the four items assessed by the SBQ‐R (indicating a relationship with not only the lifetime prevalence and frequency of suicidal ideation, but also the relative likelihood of suicidal behavior). The second report employed a large nationwide survey of Korean firefighters to determine that occupational stress caused by difficulties in the physical work environment increased the risk for suicidal ideation over the past year (OR 1.19; 95% CI: 1.16, 1.22); notably, the authors chose to measure only this element of the SBQ‐R. 28 The final study also found a clear association between occupational stressors and suicidal ideation, but observed that this relationship was only apparent amongst those firefighters who reported having a low level of social support. 29
3.3. Psychosocial stressors and non‐depressive mental health problems
We located five studies that considered whether non‐depressive mental health problems (primarily, those related to anxiety) in firefighters might be associated with work‐related stress (Table 2). The largest study we captured, which focused exclusively upon female participants, observed that workplace discrimination and harassment clearly increased the frequency and severity of current anxiety symptoms. 21 In a similar fashion, relationship conflicts were also found to increase the likelihood of work‐related anxiety amongst a mixed sample of male and female firefighters. 25 In taking a comparatively broader view of psychosocial stressors in the work environment, Teoh et al 30 found that a firefighters’ perceptions of their workplace demand and their perceived level of influence significantly predicted psychiatric morbidity (a measure encompassing symptoms of common mental health disorders, including anxiety).
Post‐traumatic stress disorder (PTSD) has gained increasing attention as a problem facing public safety personnel. 10 , 31 Of the three PTSD‐related reports that we found, two were focused upon male and female Japanese firefighters, and observed that greater levels of perceived job stress were associated with a greater probability of self‐reported post‐traumatic symptoms 32 , 33 ; as well, among those experiencing symptoms, inter‐group conflict and low levels of supervisor support were found to be important moderating variables. The third report concerned American female firefighters, and found that those experiencing the highest level of discrimination were more than twice as likely to report symptoms reflective of PTSD. 21
3.4. Psychosocial stressors and burnout
Burnout is typically regarded as a psychological response to chronic occupational stress, and tends to be characterized by emotional exhaustion, disengagement, and a reduced feeling of job‐related efficacy. 34 We captured five reports that focused upon determining whether work‐related stressors might be antecedents to burnout among firefighters (Table 3). The first of these reports used a cross‐lagged panel analysis to measure reciprocal relationships between organizational demands and burnout in a large sample of Portuguese firefighters. 20 Interestingly, the authors observed that the perception of increased organizational demands by their participants predicted the likelihood of burnout, which, in turn, was associated with an altered perception of job demands. With a focus on several hundred male and female firefighters, two cross‐sectional studies also found that job stressors and strains were positively associated with burnout. 32 , 35 The final two reports we were able to locate centred on male firefighters in Poland, and found that their perceptions of life stress were consistently correlated with most of the domains normally associated with burnout (notably, these reports used an instrument that assessed general life stress, not just stress originating from work). 36 , 37
3.5. Psychosocial stressors and alcohol use disorders
Alcohol use disorders encompass a variety of health risk behaviors, including excessive drinking and driving while impaired, which may have profound effects upon both the individual and those around them. 38 In our scan of the literature, we found four reports that examined the interaction between psychosocial stress and patterns of alcohol use within firefighters (Table 4). The largest study that we encountered involved 6484 male and 667 female firefighters from South Korea, and found that perceived job stress significantly predicted an increased likelihood of alcohol abuse. 39 Using the same tool to assess problems with alcohol use, Hosoda et al 40 found that having a poor perception of their workplace environment was a key factor influencing alcohol dependence among male Japanese firefighters. With a focus on a large group of North American female firefighters, Jahnke et al 21 observed that those with the highest level of perceived discrimination and harassment had a clearly elevated risk of alcohol abuse (OR 1.54; 95% CI: 1.09, 2.17). Unlike the other reports on this topic, the final one that we discovered used a general measure of psychosocial stress (as opposed to an instrument concentrated upon work‐related stressors), but still observed that levels of alcohol abuse rose with levels of perceived stress. 41
3.6. Psychosocial stressors and sleep quality
An adequate amount of restful sleep is not only essential for proper cognitive function, but its absence is also a notable risk factor for a variety of health problems ranging from impaired mood to workplace injury. 42 , 43 We found three studies that investigated the association between various psychosocial stressors and the quality of sleep among firefighters (Table 5). Although, Haddock et al 44 observed that American firefighters who worked longer shifts (48‐hour shifts) were significantly more likely to experience excessive daytime sleepiness (EDS) compared with their counterparts who worked 24‐hour shifts, the level of EDS was not influenced by the degree of perceived general life stress. In a similar fashion, work‐related psychosocial stress was not able to predict poor sleep quality amongst a large sample of Korean firefighters (although, many occupational stress factors were correlated with sleep quality). 45 By contrast, Yook, 46 using very similar tools to measure both work stressors and sleep quality within Korean firefighters, noted a graded relationship wherein increasing occupational stress was linked with declining sleep quality.
3.7. Psychosocial stressors, altered physiological parameters, and somatic disorders
3.7.1. Cardiovascular function
We found a single report 47 investigating the association between work‐related stress (particularly, concern raised by increasing job demands) and elevated blood pressure in a cohort of firefighters (Table 6). Using an amalgamated scale to assess work‐related stress, the study revealed a clear (albeit modest) increase in systolic blood pressure amongst those who felt that their work had grown more demanding.
Heart rate variability (HRV) is a measure of periodic variation in heart rate over time that reflects autonomic nervous system function; 48 although HRV is not a health outcome per se, given that work stress can affect HRV 49 and that autonomic imbalance may be regarded as an important antecedent to heart disease, 50 we decided to include studies using the measure. We captured two studies that investigated whether job‐related stressors could alter HRV in Korean firefighters. Interestingly, although each study used the same occupational stress scale, their observations were quite different. After adjusting for job characteristics, the first report found that concerns about both the occupational climate and organizational system were associated with undesirable changes in certain HRV parameters. 51 By contrast, the second report observed that scores for none of the eight factors composing the Korean Occupational Stress Scale influenced any of the standard HRV parameters. 46
3.7.2. Musculoskeletal disorders
Work‐related musculoskeletal disorders (WMSD) encompass a range of conditions that may interfere with employee health and job performance, including lower back pain, muscle sprains, and ligament damage. 52 Of the WMSDs typically experienced by firefighters, back pain appears to be the most common complaint, and we located two reports that examined its relationship with occupational stress. Using a very large sample of male Korean firefighters, Kim et al 53 observed that the risk of back pain was clearly affected by two key occupational factors, organizational injustice (OR 1.53; 95% CI: 1.04, 2.24) and high job demands (OR 1.55; 95% CI: 1.35, 1.77). However, in a comparatively smaller sample of male American firefighters Damrongsak et al 54 did not find that back pain could be predicted with job‐related stress (although a participant's age and history of back pain were highly predictive).
In the same large sample of Korean firefighters noted earlier, Kim et al 55 found that the risk of WMSDs was affected by several occupational factors, although lack of reward (OR 2.39; 95% CI: 1.08, 5.26) and high job demands (OR 1.52; 95% CI: 1.35, 1.70) were the most influential. Similarly, in a smaller, albeit mixed gender, sample of European firefighters, those with the greatest level of work‐related stress, had an increased risk of musculoskeletal problems (OR 1.52; 95% CI: 1.02, 2.25). 56
3.7.3. Gastrointestinal disorders
Functional gastrointestinal disorders may affect multiple sites along the length of the digestive tract, and we captured two studies that investigated whether risk for these illnesses may be affected by psychosocial work‐place stressors using the same large, mixed gender cohort of Korean firefighters. The first study, Jang et al 57 revealed that several occupational factors increased risk for gastro–oesophageal reflux disease, with lack of reward (OR 2.17; 95% CI: 1.21, 3.88) and interpersonal conflict (OR 2.07; 95% CI: 1.06, 3.51) exerting the most influence. The other report focused upon irritable bowel syndrome, but also observed that lack of reward (OR 2.39; 95% CI: 1.08, 5.26) and interpersonal conflict (OR 2.21; 95% CI: 1.25, 4.33) were the most impactful of the occupational characteristics that showed a relationship. 58
4. DISCUSSION
4.1. Main findings of the study
The aim of our review was to survey the research landscape to provide evidence about whether the work‐related psychosocial stressors experienced by firefighters could alter the likelihood that they would experience undesirable health‐related changes. As was expected, we found that job‐related stress could influence firefighter health; however, we were surprised by the breadth of areas affected, which included depression, anxiety, burnout, alcohol use, sleep quality, cardiovascular activity, musculoskeletal problems, and gastrointestinal function. In addition, we observed that the health‐related resilience of firefighters in the face of occupational stressors could be moderated by a small collection of factors: some of these variables seemed to promote resilience (self‐esteem, social support, and distress tolerance), whereas others seemed to discourage resilience (interpersonal conflict, discrimination‐harassment, and perceptions of workplace fairness).
Of the health problems we found that were associated with occupational stressors, a few were particularly notable; first among these were depressive symptoms, which seemed to accompany higher levels of work‐related psychosocial stressors amongst firefighters from several international jurisdictions. In each of these studies, the demands placed upon participants (in the form of factors such as intergroup conflict and perceived discrimination) were able to (presumably) exceed the available countervailing resources, and the imbalance may help to explain why the prevalence of depression in the fire service tends to exceed that observed in the general population. 19 , 59 As well, given that depression is an established risk factor for suicidal ideation, the inability to counterbalance job‐related psychosocial demands may be one of the upstream reasons underlying why firefighters are at increased risk for suicide. 60 , 61 Interestingly, the clear link observed between perceived discrimination‐harassment and depressive symptoms in female firefighters 21 may help to explain why Park et al 28 found that female gender was a risk factor for suicidal ideation within Korean firefighters.
Along with depression, burnout consistently appeared as a serious psychological effect of long‐term exposure to a difficult and demanding work environment. Although burnout is a multi‐faceted psychological syndrome, 34 emotional exhaustion (a decrease in the energy, or desire to perform work) and emotional withdrawal (a disengagement from work) are two of its characteristic features; importantly, both of these elements tended to be seen in firefighters with high levels of perceived stress. In an attempt to alleviate the changing perceptions of work and diminished job satisfaction that arise with burnout, firefighters may engage in short‐term displacement behaviors, like alcohol use. 62 Indeed, we observed that a high level of perceived stress (caused by factors such as a poor perception of one's work environment, discrimination‐harassment, or an inability to cope) significantly predicted a higher level of alcohol abuse among firefighters. As a result, although the excessive alcohol use that has been observed within the fire service is likely attributable to the effects of traumatic exposure, work‐related psychosocial stressors (either directly, or upstream of burnout) may also play a role in the development of this behavior. 39 , 40 , 63 , 64
Although increased risk for depressive symptoms, burnout, and alcohol use disorders were among the clearest outcomes of job‐related psychosocial stressors that we found, we also observed that cardiovascular, musculoskeletal, and gastrointestinal disorders were often associated with undesirable levels of stress. A number of earlier reports have shown that firefighters do experience a level of cardiovascular disease greater than the general population, 65 , 66 and suggest that this increased prevalence is likely attributable to variables such as shift work and irregular physical exertion; however, we found studies showing that a poor “organizational system” (characterized by features such as unfair organizational policies, organisztional injustice, and unsatisfactory organizational support) was associated with both increased pulse wave velocity (a measure of arterial stiffness) 46 and decreased HRV (periodic variation in heart rate), 51 both of which have been shown to increase risk for mortality related to cardiovascular disease. 67
Work‐related psychological burden may also activate a cascade of events, including increased muscle tone/activity (leading to fatigue), slower recovery, intensification of pain perception, weakened pain coping mechanisms, increased inflammation, and diminished circulation and supply of oxygen to tissues, that influence the development of musculoskeletal problems. 55 , 68 As well, psychosocial factors may exert a substantial effect on gastrointestinal disorders in firefighters; however, interestingly, a poor organizational system was more closely related to irritable bowel syndrome, whereas an unfavorable occupational climate seemed more likely to affect gastro–oesophageal reflux disease risk. Although the mechanisms that may underlie the connection between psychosocial stress and gastrointestinal function remains unclear, a dysregulated gut–brain axis, alterations to the gut microbiome, and a reduction in gut motility are all factors proposed as playing a role in the onset and exacerbation of symptoms. 57 , 58
4.1.1. Factors moderating work‐related psychosocial stress in firefighters
A job demands–resources framework suggests that each job makes varied demands on an employee, and that the efforts needed to respond to these demands can deplete a person's energy and impair their health and well‐being; in addition, the model suggests that there are resources available to employees that may help them to address work‐related stressors. 69 One of the most important resources that workers may use to counterbalance demands is resilience, which is often described as a cognitive factor that assists adaptation to difficult circumstances despite previous adverse experience. 70 Resilience has been found to reduce the probability that a stressor leads to psychiatric problems, 71 , 72 and has been observed to buffer the impact of traumatic events on the development of PTSD symptoms in firefighters. 73 During the review of those studies that formed our data set, we began to see a pattern emerge with regards to resilience among firefighters: certain variables seemed likely to enhance resilience (self‐esteem, distress tolerance, and social support), whereas several others seemed likely to diminish resilience (interpersonal conflict, discrimination‐harassment, and a poor perception of workplace fairness).
The first factor that seemed able to promote resilience was self‐esteem. In particular, a pair of reports from Japan showed that low self‐esteem was the variable displaying the strongest association with increased risk for depressive symptoms. 23 , 24 A subsequent report by the same group also connected low levels of self‐esteem with an increased likelihood to experience PTSD symptoms. 33 Indeed, the apparent ability of self‐esteem to buffer the effects of job‐related stress agrees with an earlier report that examined American firefighters, 74 and resonates with other work showing that self‐esteem is both related to depression and critical to mental and physical health. 75 , 76
The second resilience‐promoting resource that emerged was the perceived, or actual ability to endure negative emotional, or physical states, which may be captured by a pair of conceptually similar constructs: distress tolerance and self‐efficacy. In a large sample of American firefighters, Stanley et al 22 showed that distress tolerance was able to buffer the effects of occupational stress upon suicidality among firefighters. As well, in a similarly large group of Polish firefighters, Makara‐Studzinska et al 36 , 37 observed that self‐efficacy clearly moderated the effect of perceived stress upon burnout; indeed, the studies found that regardless of the level of perceived stress, lower levels of self‐efficacy evoked stronger feelings of psychophysical exhaustion. Interestingly, the studies that we examined agreed with earlier work by Regehr et al, 77 which discussed the importance of self‐efficacy as a moderator of the effect that trauma can have upon new firefighter recruits. Given that firefighters may experience the awareness of imminent dangers that could challenge them to the limit of their abilities, their level of distress tolerance (or self‐efficacy) is a particularly valuable cognitive resource.
The final element that seemed to boost resilience was social support, which agrees with earlier work showing that camaraderie may be a more important predictor of mental health in firefighters than general global resources. 78 For example, as levels of perceived support decreased, regardless of whether the source was from managers, family, or friends, the manifestation of symptoms linked to depression increased; 23 , 24 as well, a relationship between psychosocial stress and suicidal ideation was observed only amongst firefighters who reported feeling an inadequate level of social support. 29 Importantly, these findings are consistent with previous studies that explored the effect of social support on depression in both first responders and the general population. 79 , 80 As well, firefighters who lacked social support (from co‐workers and family) experienced more negative symptoms of burnout (ie, emotional exhaustion and depersonalization), which suggests that perceived social support provides a feeling of belonging and enhances the capacity to manage stress. 32 Lastly, findings that show a positive association of PTSD with low social support suggest that an inadequate degree of perceived social support might amplify the risk for this psychopathology by impacting the interpretation of potentially traumatic events. 9 , 33
Of the variables that seemed likely to reduce resilience, the first that we consistently observed was interpersonal conflict. For instance, relationship conflicts within a large sample of British firefighters emerged as a key determinant of work‐related anxiety and depression. 25 In a similar manner, work with Japanese firefighters also found that inter‐group conflict threatened mental well‐being among firefighters by elevating risk for depressive symptoms. 23 , 24 Notably, friction amongst those in the fire service may have effects that extend beyond mental health; for example, Jang et al 57 , 58 observed that high levels of inter‐personal conflict increased the probability of gastrointestinal disorders. Conflicts within an organization likely impair health not just by acting as an undesirable job demand, but also by reducing the likelihood that an individual may seek support for problems; that is, conflict may prevent a person from receiving the social support known to promote resilience.
The second factor that we found had the potential to drain away resilience was discrimination‐harassment; although this variable may be regarded as a sub‐type of inter‐personal conflict, given its unique character and established effect upon occupational health disparities, 81 , 82 we decided to note it separately. Although we found only a single report that directly measured perceived discrimination‐harassment, 21 both the sample size of the report and (more notably) the clear associations that it presented warranted close attention. In particular, the authors found that risk for anxiety, depression, and alcohol use disorders all clearly rose with the level of perceived discrimination‐harassment. The observations are especially important given previous work showing that female firefighters do experience greater levels of discrimination‐harassment relative to their male counterparts. 83 In addition, although they did not focus upon workplace discrimination‐harassment, the report by Arbona et al, 41 which involved Black and Latino firefighters in the United States, also revealed that risk for alcohol use disorders rose with the degree of perceived stress (at least some of which may be attributable to the experience of discrimination‐harassment). 84 , 85
The remaining variable that seemed able to interfere with resilience was whether a firefighter viewed their work environment in a poor light. For example, An et al 19 found that the risk of depression rose as firefighters viewed their workplace less favorably, whereas Hosoda et al 40 observed that a poor view of one's work environment was significantly correlated with alcohol dependence. Interestingly, a negative view of one's working climate was also shown to increase risk for gastrointestinal problems, musculoskeletal disorders, and lower back pain. 53 , 55 , 57 As the transactional model of stress advances the view that stress results from a person's interactions with their environment and how they perceive and appraise these interactions, 35 the widespread health effects of negatively viewing a workplace are not surprising. Of course, one of the reasons that addressing a negative view of the workplace may be particularly challenging is that, although subjectively clear and meaningful, the problem can be difficult to objectively identify.
4.2. Limitations of the current review
When viewing the outcomes of our review, a few methodological considerations should be noted. First, due to our review of only articles published in the English language, the possibility exists that we failed to include relevant research. As well, as we only assessed published studies, a source selection (ie, publication bias) may have affected our study. Furthermore, most of the included studies were based on a cross‐sectional design, which limits the ability to draw definitive causal connections. Finally, any interpretation of our results should also carefully consider the substantial variability we observed in how work‐related psychosocial stress among firefighters was measured. The questionnaires used across the reviewed studies varied according to geographical settings and needs, length, and the particular features of stress being appraised, which (understandably) leads to variability in the characteristics and magnitude of psychosocial stress being measured. Considering the mentioned limitations, our findings should be considered cautiously.
4.3. Conclusions and implications for research and public health
To the best of our knowledge, our systematic review represents the first attempt to broadly identify health outcomes related to the psychosocial stressors encountered by those within the fire service. Our work identified both the variety of psychosocial stressors experienced by firefighters and that these factors had considerable reach, given evidence for their effect upon depression‐suicidality, non‐depressive mental health problems, burnout, alcohol use disorders, sleep quality, and physiological parameters and somatic disorders. In an attempt to further understand the nature of the relationships at play, future research should include either efforts to build consensus around a pre‐existing tool that may be used to assess psychosocial stress within firefighters (a move that seems to have already occurred within the Korean research community), and/or to craft an instrument that would have the degree of broad appeal needed to be adopted as the standard measurement tool. In addition, given the apparent lack of prospective studies, future work should strive to include longitudinal designs aimed at securing evidence of causal relationships. As well, our hope is that some of the work to be done in the area will examine how the experience of stress becomes biologically embedded in a manner that leads to the health and behavior‐related changes observed; in particular, we would be keen to see measurements of the physiological imprint that can be left by stress (ie, allostatic load). 86
With regards to occupational health and well‐being, the results from our review will add to the growing body of evidence suggesting that work‐related psychosocial stressors play an important role in the development of risk for a wide variety of undesirable health outcomes and behaviors. Although we certainly need to improve our understanding of how psychosocial stress becomes biologically embedded in such a way as to affect disease risk, the available evidence points to reasonably straightforward interventions that could both help mitigate unfavorable health outcomes and yield broader benefits. In particular, stakeholders should consider how policies within their institutions may be developed with the goal of promoting and preserving resilience within firefighters by encouraging self‐esteem, social support, distress tolerance, and a positive view of their workplace, while discouraging interpersonal conflict and discrimination‐harassment.
DISCLOSURE
Approval of the research protocol: N/A. Informed consent: N/A. Registry and the registration no. of the study/trial: N/A. Animal studies: N/A. Conflict of interest: The authors declare that they have no conflict of interest.
Supporting information
Supplementary Material
ACKNOWLEDGMENTS
Our work was generously supported by an Occupational Health and Safety (OHS) Futures Grant provided to JGM by the Government of Alberta, Canada [grant number 095 244 771].
APPENDIX A. Database search strategies developed for the systematic review.
|
Database: PUBMED (firefighter OR firefighters OR firefighting OR fire‐fighter OR "fire fighter" OR fireman OR "fire service") AND ("psychosocial stress" OR "psychosocial stressors" OR stress OR stressors) Filters: Humans, English Filters: Human, English |
|---|
| Search results: 553 |
|
Database: CINAHL (Firefighter* OR firefighting OR fire‐fighter OR "fire fighter" OR fireman OR "fire service" ) AND ( "psychosocial stress" OR "psychosocial stress" OR stress OR stressors ) Filters: English, Academic articles |
|---|
| Search result: 367 |
|
Database: PsycInfo Firefighter* OR firefighting OR fire‐fighter OR "fire fighter" OR fireman OR "fire service" ) AND ( "psychosocial stress" OR "psychosocial stress" OR stress OR stressors Filters: Journal |
|---|
| Search result: 495 |
APPENDIX B. The process used to identify the studies that formed the basis for our systematic review.
APPENDIX C. The noted reports are review articles concerning firefighter health that were removed from consideration during our review of the titles and abstracts captured in our database search.
Berger, W., Coutinho, E. S. F., Figueira, I., Marques‐Portella, C., Luz, M. P., Neylan, T. C., Marmar C., & Mendlowicz, M. V. (2012). Rescuers at risk: a systematic review and meta‐regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Social Psychiatry and Psychiatric Epidemiology, 47(6), 1001‐1011.
Bolm‐Audorff, U., Petereit‐Haack, G., & Seidler, A. (2019). Relationship between occupational trauma, posttraumatic stress disorder and depression‐an assessment of systematic reviews. Psychiatrische Praxis, 46(4), 184‐190.
Crawford, J. O., & Graveling, R. A. (2012). Non‐cancer occupational health risks in firefighters. Occupational Medicine, 62(7), 485‐495.
Fisher, P., & Etches, B. (2003). A comprehensive approach to workplace stress & trauma in fire‐fighting: A review document prepared for the International Association of Firefighters 17th Redmond Symposium. In 17th Redmond Symposium, San Francisco, CA.
Fowler, C. T. (2003). Human health impacts of forest fires in the southern United States: a literature review. Journal of Ecological Anthropology, 7(1), 39‐63.
Fraess‐Phillips, A., Wagner, S., & Harris, R. L. (2017). Firefighters and traumatic stress: A review. International Journal of Emergency Services.
Greinacher, A., Derezza‐Greeven, C., Herzog, W., & Nikendei, C. (2019). Secondary traumatization in first responders: a systematic review. European Journal of Psychotraumatology, 10(1), 1 562 840.
Groot, E., Caturay, A., Khan, Y., & Copes, R. (2019). A systematic review of the health impacts of occupational exposure to wildland fires. International Journal of Occupational Medicine and Environmental Health, 32(2), 121‐140.
Haugen, P. T., Evces, M., & Weiss, D. S. (2012). Treating posttraumatic stress disorder in first responders: A systematic review. Clinical Psychology Review, 32(5), 370‐380.
Jones, S. (2017). Describing the mental health profile of first responders: A systematic review. Journal of the American Psychiatric Nurses Association, 23(3), 200‐214.
Kales, S. N., Tsismenakis, A. J., Zhang, C., & Soteriades, E. S. (2009). Blood pressure in firefighters, police officers, and other emergency responders. American Journal of Hypertension, 22(1), 11‐20.
Kang, M. J., Kim, Y. H., & Han, S. W. (2019). A systematic review of the variables related to post‐traumatic stress disorder in firefighters. Fire Science and Engineering, 33(2), 164‐172.
Larsson, G., Berglund, A. K., & Ohlsson, A. (2016). Daily hassles, their antecedents and outcomes among professional first responders: A systematic literature review. Scandinavian Journal of Psychology, 57(4), 359‐367.
de Paula Lima, E., & Assunção, A. Á. (2011). Prevalence and factors associated with Posttraumatic Stress Disorder (PTSD) in emergency workers: a systematic literature review. Revista Brasileira de Epidemiologia, 14(2), 217‐30.
Lowell, A., Suarez‐Jimenez, B., Helpman, L., Zhu, X., Durosky, A., Hilburn, A., Schneier, F., Gross, R., & Neria, Y. (2018). 9/11‐related PTSD among highly exposed populations: a systematic review 15 years after the attack. Psychological Medicine, 48(4), 537.
Mao, X., Fung, O. W. M., Hu, X., & Loke, A. Y. (2018). Psychological impacts of disaster on rescue workers: A review of the literature. International Journal of Disaster Risk Reduction, 27, 602‐617.
McEntire, S. J., Suyama, J., & Hostler, D. (2013). Mitigation and prevention of exertional heat stress in firefighters: a review of cooling strategies for structural firefighting and hazardous materials responders. Prehospital Emergency Care, 17(2), 241‐260.
McFarlane, A. C. (1998). Epidemiological evidence about the relationship between PTSD and alcohol abuse: the nature of the association. Addictive Behaviors, 23(6), 813‐825.
Neria, Y., Nandi, A., & Galea, S. (2008). Post‐traumatic stress disorder following disasters: a systematic review. Psychological Medicine, 38(4), 467.
Orr, R., Simas, V., Canetti, E., & Schram, B. (2019). A profile of injuries sustained by firefighters: A critical review. International Journal of Environmental Research and Public Health, 16(20), 3931.
Perroni, F., Guidetti, L., Cignitti, L., & Baldari, C. (2014). Psychophysiological responses of firefighters to emergencies: A review. The Open Sports Sciences Journal, 7(1).
Plat, M. J., Frings‐Dresen, M. H. W., & Sluiter, J. K. (2011). A systematic review of job‐specific workers’ health surveillance activities for fire‐fighting, ambulance, police and military personnel. International Archives of Occupational and Environmental Health, 84(8), 839‐857.
Soteriades, E. S., Smith, D. L., Tsismenakis, A. J., Baur, D. M., & Kales, S. N. (2011). Cardiovascular disease in US firefighters: a systematic review. Cardiology in Review, 19(4), 202‐215.
Sritharan, J., Pahwa, M., Demers, P. A., Harris, S. A., Cole, D. C., & Parent, M. E. (2017). Prostate cancer in firefighting and police work: a systematic review and meta‐analysis of epidemiologic studies. Environmental Health, 16(1), 1‐12.
Stanley, I. H., Hom, M. A., & Joiner, T. E. (2016). A systematic review of suicidal thoughts and behaviors among police officers, firefighters, EMTs, and paramedics. Clinical Psychology Review, 44, 25‐44.
Igboanugo S, Bigelow PL, Mielke JG. Health outcomes of psychosocial stress within firefighters: A systematic review of the research landscape. J Occup Health. 2021;63:e12219. 10.1002/1348-9585.12219
SI and JGM conceived of the idea for the project, completed the data collection and analysis, and prepared the manuscript; PLB provided constructive feedback on the study design and helped to edit the manuscript.
REFERENCES
- 1. DeJoy DM, Smith TD, Dyal MA. Safety climate and firefighting: Focus group results. J Safety Res. 2017;62:107‐116. 10.1016/j.jsr.2017.06.011 [DOI] [PubMed] [Google Scholar]
- 2. Vock D. Fire departments struggle to meet new demands. Governing: The future of States and Localities. https://www.governing.com/topics/public‐justice‐safety/gov‐firefighters‐firehouse. Published 2018.
- 3. Comeau E. The role of demographics in fire safety. Firehouse. https://www.firehouse.com/prevention‐investigation/article/10493436/the‐role‐of‐demographics‐in‐fire‐safety. Published 2009.
- 4. Kerber S. Analysis of changing residential fire dynamics and its implications on firefighter operational timeframes. Fire Technol. 2012;48(4):865‐891. 10.1007/s10694-011-0249-2 [DOI] [Google Scholar]
- 5. Radeloff VC, Helmers DP, Kramer HA, et al. Rapid growth of the US wildland‐urban interface raises wildfire risk. Proc Natl Acad Sci U S A. 2018;115(13):3314‐3319. 10.1073/pnas.1718850115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Guidotti TL, Clough VM. Occupational Health concerns of firefighting. Annu Rev Public Health. 1992;13:151‐171. [DOI] [PubMed] [Google Scholar]
- 7. Melius J. Occupational health for firefighters. Occup Med (Chic Ill). 2001;16(1):101‐108. [PubMed] [Google Scholar]
- 8. Jahnke SA, Poston WSC, Jitnarin N, Keith Haddock C. Health concerns of the U.S. fire service: Perspectives from the firehouse. Am J Heal Promot. 2012;27(2):111‐118. 10.4278/ajhp.110311-QUAL-109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Meyer EC, Zimering R, Daly E, Knight J, Kamholz BW, Gulliver SB. Predictors of posttraumatic stress disorder and other psychological symptoms in trauma‐exposed firefighters. Psychol Serv. 2012;9(1):1‐15. 10.1037/a0026414 [DOI] [PubMed] [Google Scholar]
- 10. Berger W, Figueira I, De SS, et al. Rescuers at risk: a systematic review and meta‐regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Soc Psychiatry Psychiatr Epidemiol. 2012;47(6):1001‐1011. 10.1007/s00127-011-0408-2.Rescuers [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ganster DC, Rosen CC. Work stress and employee health: A multidisciplinary review. J Manage. 2013;39(5):1085‐1122. 10.1177/0149206313475815 [DOI] [Google Scholar]
- 12. Stanfeld S, Candy B. Psychosocial work environment and mental health ‐ a meta‐analytic review. Scand J Work Environ Health. 2006;32(6):443‐462. [DOI] [PubMed] [Google Scholar]
- 13. Nieuwenhuijsen K, Bruinvels D, Frings‐Dresen M. Psychosocial work environment and stress‐related disorders, a systematic review. Occup Med (Lond). 2010;60(4):277‐286. 10.1093/occmed/kqq081 [DOI] [PubMed] [Google Scholar]
- 14. Quick JC, Henderson DF. Occupational stress: Preventing suffering, enhancing wellbeing. Int J Environ Res Public Health. 2016;13:1‐11. 10.3390/ijerph13050459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Griep RH, Nobre AA, Guimarães M, et al. Job strain and unhealthy lifestyle: Results from the baseline cohort study, Brazilian Longitudinal Study of Adult Health (ELSA‐Brasil). BMC Public Health. 2015;15:1‐10. 10.1186/s12889-015-1626-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rutters F, Pilz S, Koopman AD, et al. Social Science & Medicine The association between psychosocial stress and mortality is mediated by lifestyle and chronic diseases: The Hoorn Study. Soc Sci Med. 2014;118:166‐172. 10.1016/j.socscimed.2014.08.009 [DOI] [PubMed] [Google Scholar]
- 17. Siegrist J, Rödel A. Work stress and health risk behavior. Scand J Work Environ Health. 2006;32(6):473‐481. 10.5271/sjweh.1052 [DOI] [PubMed] [Google Scholar]
- 18. Ryan R. Cochrane Consumers and Communication Review Group: data synthesis and analysis. 2013;1‐5.http://cccrg.cochrane.org/author‐resources.
- 19. An S‐J, Chung YK, Kim BH, et al. The effect of organisational system on self‐rated depression in a panel of male municipal firefighters. Ann Occup Environ Med. 2015;27:1‐7. 10.1186/s40557-014-0044-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ângelo RP, Chambel MJ. The reciprocal relationship between work characteristics and employee burnout and engagement: A longitudinal study of firefighters. Stress Health. 2015;31(2):106‐114. 10.1002/smi.2532 [DOI] [PubMed] [Google Scholar]
- 21. Jahnke SA, Haddock CK, Jitnarin N, et al. The prevalence and health impacts of frequent work discrimination and harassment among women firefighters in the US fire service. Biomed Res Int. 2019;2019:5‐9. 10.1155/2019/6740207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Stanley IH, Boffa JW, Smith LJ, et al. Occupational stress and suicidality among firefighters: Examining the buffering role of distress tolerance. Psychiatry Res. 2017;2018(266):90‐96. 10.1016/j.psychres.2018.05.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Saijo Y, Ueno T, Hashimoto Y. Job stress and depressive symptoms among Japanese fire fighters. Am J Ind Med. 2007;50:470‐480. 10.1002/ajim.20460 [DOI] [PubMed] [Google Scholar]
- 24. Saijo Y, Ueno T, Hashimoto Y. Twenty‐four‐hour shift work, depressive symptoms, and job dissatisfaction among Japanese firefighters. Am J Ind Med. 2008;51:380‐391. 10.1002/ajim.20571 [DOI] [PubMed] [Google Scholar]
- 25. Payne N, Kinman G. Job demands, resources and work‐related well‐being in UK firefighters. Occup Med (Chic Ill). 2019;69(8–9):604‐609. 10.1093/occmed/kqz167 [DOI] [PubMed] [Google Scholar]
- 26. Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The suicidal behaviors questionnaire‐revised (SBQ‐R): validation with clinical and non‐clinical samples. Assessment. 2001;8(4):443‐454. [DOI] [PubMed] [Google Scholar]
- 27. Kimbrel NA, Steffen LE, Meyer EC, et al. A revised measure of occupational stress for firefighters: Psychometric properties and relationship to posttraumatic stress disorder, depression, and substance abuse. Psychol Serv. 2011;8(4):294‐306. 10.1037/a0025845 [DOI] [Google Scholar]
- 28. Park H, Kim JI, Min B, Oh S, Kim JH. Prevalence and correlates of suicidal ideation in Korean firefighters: A nationwide study. BMC Psychiatry. 2019;19(1):1‐9. 10.1186/s12888-019-2388-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Carpenter GSJ, Carpenter TP, Kimbrel NA, et al. social support, stress, and suicidal Ideation in Professional Firefighters. Am J Heal Behav. 2015;39(2):191‐196. [DOI] [PubMed] [Google Scholar]
- 30. Teoh KRH, Lima E, Vasconcelos A, Nascimento E, Cox T. Trauma and work factors as predictors of firefighters’ psychiatric distress. Occup Med (Chic Ill). 2019;69(8–9):598‐603. 10.1093/occmed/kqz168 [DOI] [PubMed] [Google Scholar]
- 31. Haugen PT, Evces M, Weiss DS. Treating posttraumatic stress disorder in first responders: A systematic review. Clin Psychol Rev. 2012;32(5):370‐380. 10.1016/j.cpr.2012.04.001 [DOI] [PubMed] [Google Scholar]
- 32. Mitani S, Fujita M, Nakata K, Shirakawa T. Impact of post‐traumatic stress disorder and job‐related stress on burnout: A study of fire service workers. J Emerg Med. 2006;31(1):7‐11. 10.1016/j.jemermed.2005.08.008 [DOI] [PubMed] [Google Scholar]
- 33. Saijo Y, Ueno T, Hashimoto Y. Post‐traumatic stress disorder and job stress among firefighters of urban Japan. Prehosp Disaster Med. 2012;27(1):59‐63. 10.1017/S1049023X12000222 [DOI] [PubMed] [Google Scholar]
- 34. Maslach C, Schaufeli W, Leiter M. Job burnout. Annu Rev Psychol. 2001;52:397‐422. [DOI] [PubMed] [Google Scholar]
- 35. Smith TD, DeJoy DM, Dyal MA(, Huang G. Impact of work pressure, work stress and work–family conflict on firefighter burnout. Arch Environ Occup Heal. 2019;74(4):215‐222. 10.1080/19338244.2017.1395789 [DOI] [PubMed] [Google Scholar]
- 36. Makara‐Studzińska M, Golonka K, Izydorczyk B. Self‐efficacy as a moderator between stress and professional burnout in firefighters. Int J Environ Res Public Health. 2019;16(2): 10.3390/ijerph16020183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Makara‐Studzińska M, Wajda Z, Lizińczyk S. Years of service, self‐efficacy, stress and burnout among Polish firefighters. Int J Occup Med Environ Health. 2020;33(3):283‐297. 10.13075/IJOMEH.1896.01483 [DOI] [PubMed] [Google Scholar]
- 38. Schuckit MA. Alcohol‐use disorders. Lancet. 2009;373(9662):492‐501. 10.1016/S0140-6736(09)60009-X [DOI] [PubMed] [Google Scholar]
- 39. Kim JI, Park H, Kim JH. The mediation effect of PTSD, perceived job stress and resilience on the relationship between trauma exposure and the development of depression and alcohol use problems in Korean firefighters: A cross‐sectional study. J Affect Disord. 2017;2018(229):450‐455. 10.1016/j.jad.2017.12.055 [DOI] [PubMed] [Google Scholar]
- 40. Hosoda T, Osaki Y, Okamoto H, Wada T, Otani S. Evaluation of relationships among occupational stress, alcohol dependence and other factors in male personnel in a Japanese local fire fighting organization. Yonago Acta Med. 2012;55:63‐68. [PMC free article] [PubMed] [Google Scholar]
- 41. Arbona C, Pao C, Long A, Olvera N. Perceived stress in Black and Latino Male firefighters: Associations with Risk and protective factors. Ethn Dis. 2017;27(4):421‐428. 10.18865/ed.27.4.421.Keywords [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lee EK, Douglass AB. Sleep in psychiatric disorders: Where are we now? Can J Psychiatry. 2010;55(7):403‐412. 10.1177/070674371005500703 [DOI] [PubMed] [Google Scholar]
- 43. Uehli K, Mehta AJ, Miedinger D, et al. Sleep problems and work injuries: A systematic review and meta‐analysis. Sleep Med Rev. 2014;18(1):61‐73. 10.1016/j.smrv.2013.01.004 [DOI] [PubMed] [Google Scholar]
- 44. Haddock CK, Poston WSC, Jitnarin N, Jahnke SA. Excessive daytime sleepiness in firefighters in the central United States. J Occup Env Med. 2013;55(4):416‐423. 10.1097/JOM.0b013e31827cbb0b [DOI] [PubMed] [Google Scholar]
- 45. Lim D, Baek K, Chung I, Lee M. Factors related to sleep disorders among male firefighters. Ann Occup Environ Med. 2014;26(1):1‐8. 10.1186/2052-4374-26-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Yook YS. Firefighters’ occupational stress and its correlations with cardiorespiratory fitness, arterial stiffness, heart rate variability, and sleep quality. PLoS One. 2019;14(12):1‐9. 10.1371/journal.pone.0226739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Choi B, Schnall P, Dobson M. Twenty‐four‐hour work shifts, increased job demands, and elevated blood pressure in professional firefighters. Int Arch Occup Environ Health. 2016;89(7):1111‐1125. 10.1007/s00420-016-1151-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Togo F, Takahashi M. Heart rate variability in occupational health ‐ a systematic review. Ind Health. 2009;47:589‐602. [DOI] [PubMed] [Google Scholar]
- 49. Chandola T, Britton A, Brunner E, et al. Work stress and coronary heart disease: what are the mechanisms. Eur Heart J. 2008;29(5):640‐648. [DOI] [PubMed] [Google Scholar]
- 50. Thayer J, Yamamoto S, Brosschot J. The relationship of autonomic imbalance, heart rate variability and cardiovascular risk factors. Int J Cardiol. 2010;141(2):122‐131. [DOI] [PubMed] [Google Scholar]
- 51. Shin J, Lee J, Yang S, Lee M, Chung I. Factors related to heart rate variability among firefighters. Ann. Occup Environ Med. 2016;28(1):1‐9. 10.1186/s40557-016-0111-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Punnett L, Wegman DH. Work‐related musculoskeletal disorders: The epidemiologic evidence and the debate. J Electromyogr Kinesiol. 2004;14(1):13‐23. 10.1016/j.jelekin.2003.09.015 [DOI] [PubMed] [Google Scholar]
- 53. Kim MG, Seo J, Kim K, Ahn Y. Nationwide firefighter survey: the prevalence of lower back pain and its related psychological factors among Korean firefighters. Int J Occup Saf Ergon. 2016;1‐10. 10.1080/10803548.2016.1219149 [DOI] [PubMed] [Google Scholar]
- 54. Damrongsak M, Prapanjaroensin A, Brown KC. Predictors of back pain in firefighters. Work Heal Saf. 2017;20(10):1‐9. 10.1177/2165079917709020 [DOI] [PubMed] [Google Scholar]
- 55. Kim MG, Kim K, Ryoo J, Yoo S. Relationship between occupational stress and work‐related musculoskeletal disorders in Korean male firefighters. Ann Occup Environ Med. 2013;25(9):1‐7. 10.1186/2052-4374-25-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Soteriades ES, Psalta L, Leka S, Spanoudis G. Occupational stress and musculoskeletal symptoms in firefighters. Int J Occup Med Environ Health. 2019;32(3):341‐352. 10.13075/ijomeh.1896.01268 [DOI] [PubMed] [Google Scholar]
- 57. Jang S, Ryu H, Choi S, Lee S. Psychological factors influence the gastroesophageal reflux disease (GERD) and their effect on quality of life among firefighters in South Korea. Int J Occup Environ Health. 2016;22(4):315‐320. 10.1080/10773525.2016.1235675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Jang S, Ryu H, Choi S, Lee S. Psychological factors influence the irritable bowel syndrome and their effect on quality of life among firefighters in South Korea. pschiatary investig. 2017;14(4):434‐440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Fullerton CS, Ursano RJ, Wang L. Acute stress disorder, posttraumatic stress disorder, and depression in disaster of rescue workers. Am J Psychiatry. 2004;161(8):1370‐1376. 10.1176/appi.ajp.161.8.1370 [DOI] [PubMed] [Google Scholar]
- 60. Stanley IH, Hom MA, Hagan CR, Joiner TE. Career prevalence and correlates of suicidal thoughts and behaviors among firefighters. J Affect Disord. 2015;187:163‐171. 10.1016/j.jad.2015.08.007 [DOI] [PubMed] [Google Scholar]
- 61. Stanley IH, Hom MA, Joiner TE. A systematic review of suicidal thoughts and behaviors among police officers, firefighters, EMTs, and paramedics. Clin Psychol Rev. 2016;44:25‐44. 10.1016/j.cpr.2015.12.002 [DOI] [PubMed] [Google Scholar]
- 62. Bacharach SB, Bamberger PA, Doveh E. Firefighters, critical incidents, and drinking to cope: The adequacy of unit‐level performance resources as a source of vulnerability and protection. J Appl Psychol. 2008;93(1):155‐169. 10.1037/0021-9010.93.1.155 [DOI] [PubMed] [Google Scholar]
- 63. Piazza‐Gardner AK, Barry AE, Chaney E, Dodd V, Weiler R, Delisle A. Covariates of alcohol consumption among career firefighters. Occup Med (Lond). 2014;64(8):580‐582. 10.1093/occmed/kqu124 [DOI] [PubMed] [Google Scholar]
- 64. Zegel M, Tran JK, Vujanovic AA. Posttraumatic stress, alcohol use, and alcohol use motives among firefighters: The role of distress tolerance. Psychiatry Res. 2019;282:112633. 10.1016/j.psychres.2019.112633 [DOI] [PubMed] [Google Scholar]
- 65. Kales SN, Soteriades ES, Christophi CA, Christiani DC. Emergency duties and deaths from heart disease among firefighters in the United States. N Engl J Med. 2007;356(12):1207‐1215. 10.1136/bmj.318.7197.1565a [DOI] [PubMed] [Google Scholar]
- 66. Soteriades ES, Smith DL, Tsismenakis AJ, Baur DM, Kales SN. Cardiovascular disease in US firefighters: A systematic review. Cardiol Rev. 2011;19(4):202‐215. [DOI] [PubMed] [Google Scholar]
- 67. Hamer M, Molloy GJ, Stamatakis E. Psychological distress as a risk factor for cardiovascular events. Pathophysiological and behavioral mechanisms. J Am Coll Cardiol. 2008;52(25):2156‐2162. 10.1016/j.jacc.2008.08.057 [DOI] [PubMed] [Google Scholar]
- 68. Visser B, Van DJH. Pathophysiology of upper extremity muscle disorders. J Electromyogr Kinesiol. 2006;16:1‐16. 10.1016/j.jelekin.2005.06.005 [DOI] [PubMed] [Google Scholar]
- 69. Demerouti E, Nachreiner F, Bakker A, Schaufeli WB. The job demands‐resources model of burnout. J Appl Psychol. 2001;86(3):499‐512. [PubMed] [Google Scholar]
- 70. Luthar SS, Cicchetti D. The construct of resilience: Implications for interventions and social policies. Dev Psychopathol. 2000;12(4):857‐885. 10.1017/S0954579400004156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Edwards KM, Probst DR, Rodenhizer‐Stämpfli KA, Gidycz CA, Tansill EC. Multiplicity of child maltreatment and biopsychosocial outcomes in young adulthood: The moderating role of resiliency characteristics among female survivors. Child Maltreat. 2014;19:188‐198. 10.1177/1077559514543354 [DOI] [PubMed] [Google Scholar]
- 72. Green KT, Calhoun PS, Dennis MF, et al. Exploration of the resilience construct in posttraumatic stress disorder severity and functional correlates in military combat veterans who have served since September 11, 2001. J Clin Psychiatry. 2010;71(7):823‐830. 10.4088/JCP.09m05780blu [DOI] [PubMed] [Google Scholar]
- 73. Lee JS, Ahn YS, Jeong KS, Chae JH, Choi KS. Resilience buffers the impact of traumatic events on the development of PTSD symptoms in firefighters. J Affect Disord. 2014;162:128‐133. 10.1016/j.jad.2014.02.031 [DOI] [PubMed] [Google Scholar]
- 74. Petrie K, Rotheram MJ. Insulators against stress: Self‐esteem and assertiveness. Psychol Rep. 1982;50:963‐966. [DOI] [PubMed] [Google Scholar]
- 75. Whisman MA, Kwon P. Life stress and dysphoria: The role of self‐esteem and hopelessness. J Pers Soc Psychol. 1993;65(5):1054‐1060. 10.1037/0022-3514.65.5.1054 [DOI] [PubMed] [Google Scholar]
- 76. Mann M, Hosman CMH, Schaalma HP, De Vries NK. Self‐esteem in a broad‐spectrum approach for mental health promotion. Health Educ Res. 2004;19(4):357‐372. 10.1093/her/cyg041 [DOI] [PubMed] [Google Scholar]
- 77. Regehr C, Hill J, Knott T, Sault B. Social support, self‐efficacy and trauma in new recruits and experienced firefighters. Stress Heal. 2003;19:189‐193. 10.1002/smi.974 [DOI] [Google Scholar]
- 78. Tuckey MR, Hayward R. Global and occupation‐specific emotional resources as buffers against the emotional demands of fire‐fighting. Appl Psychol. 2011;60(1):1‐23. 10.1111/j.1464-0597.2010.00424.x [DOI] [Google Scholar]
- 79. Park K, Wilson M, Lee M. Effects of social support at work on depression and organizational productivitty. Am J Heal Behav. 2004;28(5):444‐455. 10.5993/AJHB.28.5.7 [DOI] [PubMed] [Google Scholar]
- 80. Prati G, Pietrantoni L. The relation of perceived and received social support to mental health among first responders: a meta‐analytic review. J Community Psychol. 2010;38(3):403‐417. 10.1002/jcop [DOI] [Google Scholar]
- 81. Okechukwu CA, Souza K, Davis KD, de Castro AB. Discrimination, harassment, abuse, and bullying in the workplace: Contribution of workplace injustice to occupational health disparities. Am J Ind Med. 2014;57(5):573‐586. 10.1002/ajim.22221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Xu YE, Chopik WJ. Identifying moderators in the link between workplace discrimination and health/well‐being. Front Psychol. 2020;11:1‐14. 10.3389/fpsyg.2020.00458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Griffith J, Schultz J, Wakeham R, Schultz M. A replication of the 2008 U.S. national report card study on women in firefighting. Bus Rev Cambridge. 2016;24(1):13‐18. [Google Scholar]
- 84. Williams DR. The health of men: Structured inequalities and opportunities. Am J Public Health. 2003;93(5):724‐731. 10.2105/AJPH.93.5.724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Perez S, Gavin J, Diaz V. Stressors and coping mechanism associated with perceived stress in Latinos. Ethn Dis. 2015;25:78‐82. [PubMed] [Google Scholar]
- 86. Mauss D, Li J, Schmidt B, Angerer P, Jarczok M. Measuring allostatic load in the workforce: A systematic review. Ind Health. 2015;53(1):5‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


