Abstract
Objective:
This study aimed to provide further evidence on the accuracy of tumor size estimates and influencing factors.
Materials and Methods:
In this cross-sectional study, patients with a biopsy-proven diagnosis of breast cancer referred to our hospital to obtain a preoperative magnetic resonance imaging (MRI) between 2015 and 2016 were included. Data from 76 breast cancer patients with 84 lesions were collected. All participants underwent ultrasonography and MRI, and their mammograms (MGMs) were reevaluated for tumor size estimation. Measurements by the three imaging modalities were compared with the pathologically determined tumor size to assess their accuracy. Influencing factors such as surgical management, molecular and histopathological subtypes, and Breast Imaging Reporting and Data System enhancement types in MRI were also assessed.
Results:
The rates of concordance with the gold standard were 64.3%, 76.2%, and 82.1% for MGM, ultrasound (US), and MRI measurements, respectively. Therefore, the highest concordance rate was observed in MRI-based estimates. Among the discordant cases, US and MGM underestimation were more prevalent (70%); nevertheless, MRI showed significant overestimation (80%). Tumor size estimates in patients whose MRIs presented with either non-mass enhancement [p=0.030; odds ratio (OR)=17.2; 95% confidence interval (CI): 1.3–225.9] or mass lesion with non-mass enhancement (p=0.001; OR=51.0; 95% CI: 5.0–518.4) were more likely to be discordant with pathological measurements compared with those in cases with only mass lesion on their MRIs.
Conclusion:
MRI was more accurate than either US or MGM in estimating breast tumor size but had the highest overestimation rate. Therefore, caution should be practiced in interpreting data obtained from subjects whose MRIs present with non-mass enhancement or mass lesion with non-mass enhancement.
Keywords: Breast neoplasms, mammography, ultrasonography, magnetic resonance imaging, tumor size, molecular subtypes
Introduction
Breast cancer is the second most common cause of cancer-related mortality in women worldwide, with a lifetime risk of approximately 12% (1). Tumor size is one of the main prognostic factors in breast cancer and is reported to correlate with lymph node involvement, tumor grade, and overall survival rate (2). Tumor size is also a factor assessed to determine treatment plans: breast conservation, mastectomy, or neoadjuvant chemotherapy (3).
Accordingly, precise estimation of tumor size is of utmost importance for planning a therapeutic strategy, and the main imaging modalities are mammogram (MGM), ultrasound (US), and magnetic resonance imaging (MRI). Each of these modalities has certain strengths and weaknesses in breast tumor evaluation. For instance, MGM is superior in identifying malignant calcifications; however, the obscurity of the margins and magnification variability limits the accuracy of measurements by this method (4). The sensitivity of MGM to detect malignant lesions in younger patients with dense breast tissue is also reported to be poor (5, 6). As for US, its ability to measure tumors in multiple planes is a great strength that enables a skilled operator to make measurements of its largest dimension (7). However, one main limitation of US is that it is highly operator dependent (8). MRI also offers the merit of multiplanar imaging along with a higher accuracy in assessing multicentric and multifocal lesions (9, 10); however, MRI has been reported to overestimate tumor size (9, 11), and the extent of background parenchymal enhancement (BPE) affects its accuracy (12).
In this regard, studies have assessed the accuracy of tumor size estimation by MGM and US (11, 13, 14, 15), and compared their measurements with those by MRI (10, 16, 17). In comparing US and MGM, some studies have reported that US has a higher accuracy than MGM (7, 11, 15, 18), whereas others found the opposite (13, 14, 19). Among the studies that compared all three modalities, some reported MRI to have a higher accuracy (16, 20), whereas others found that MGM was more accurate (21, 22).
Considering the variability of the findings of the current literature on this subject, this study was designed to provide further evidence regarding the accuracy of MGM, US, and MRI in estimating breast tumor size by evaluating their concordance with the pathologically determined size of the surgical specimen and the effects of various factors on the accuracy of their measurements.
Study design
In this cross-sectional study, the target population included patients with a biopsy-proven diagnosis of breast cancer [Breast Imaging Reporting and Data System (BI-RADS) VI] (23), who were referred to Laleh Hospital in Tehran to obtain a preoperative MRI between 2015 and 2016. Indications for preoperative MRI in these patients included the following:
• Screening for presence of multifocal or multicentric lesions within the ipsilateral breast, for instance, in patients with invasive lobular carcinoma (ILC)
• Screening for involvement of the contralateral breast, for example, in patients with ductal carcinoma in situ (DCIS)
• Providing a more accurate evaluation of patients with dense breast composition, for example, candidates for breast-conserving surgery (BCS).
Patients who received neoadjuvant chemotherapy and subjects with gaps of longer than 1 month between their breast biopsy and MRI were excluded.
Based on these inclusion and exclusion criteria, eligible subjects were recruited through a convenience sampling method. All participants underwent ultrasonography and MRI, and their MGMs were also reevaluated. A breast specialist radiologist with more than 10 years of experience in the field performed the US assessment and evaluated the MGMs and MRIs of all patients.
Magnetic resonance imaging
Breast MRI was conducted using a dedicated surface breast coil of a Siemens Avanto 1.5 Tesla MRI scanner (Siemens Healthcare, Erlangen, Germany) with the patient lying in a prone position. Standard sequences were obtained, including an axial turbo inversion recovery magnitude (TR/TE 5600/59 ms; a flip angle of 142°; viewfield of 340 mm; matrix size of 314×320; slice thickness of 4 mm; acquisition time of 2 min and 55 s), an axial nonfat suppressed T1-weighted flash 3D (TR/TE 8.6/4.7; a flip angle of 20°; viewfield of 340 mm; matrix size of 323×448; slice thickness of 1 mm; acquisition time of 1 min and 45 s), and axial T1-weighted flash 3D pre-contrast and post-contrast sequences (TR/TE 6/1.69 ms; a flip angle of 10°; viewfield of 340 mm; matrix size of 342×384; slice thickness of 1.6 mm; acquisition time of 7 min and 36 s). Six post-contrast dynamic sequences with 55-s intervals starting at 20 s were obtained. Intravenous administration of 0.1 mmol/L gadopentetate dimeglumine (Magnevist, Bayer, Germany) was used as the contrast in this protocol. T1 contrast-enhanced subtraction images were used for visual evaluation and categorization of BPE into four levels, namely, minimal, mild, moderate, and marked, based on the fifth edition of BI-RADS criteria (24). Lesions were classified into three groups according to their MRI image appearance including mass lesions, non-mass enhancements, and mass lesions with non-mass components. The maximum diameter of the tumor was measured on the second subtraction post-contrast sequences and recorded in millimeters.
Ultrasonography
The same radiologist, who was blinded to the MRI results, performed US assessment using a digital ultrasound scanner (Phillips iU22 Manufactured by Philips Ultrasound Bothell-Everett Highway Bothell, WA 98021-8431 USA) equipped with a 6–14 Megahertz linear probe. The size of the tumor was determined at its greatest dimension and recorded for statistical analyses.
Mammography
Patients’ MGMs obtained using full-field digital mammography unit were reevaluated in both the craniocaudal and mediolateral-oblique views. Patients were categorized into three groups, namely, mass, microcalcification, and distortion, based on the main characteristic of their lesions on MGMs. The maximum size of the lesion was also measured on the images and recorded in millimeters.
Histopathological assessments
The final pathology of the tumor and its grade were recorded on the basis of post-surgical evaluations. Standard immunohistochemical methods were used to determine the positivity of the tumor for estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2), and Ki-67 protein level. Based on the results of these assessments, ER-positive, PR-positive, and HER2-negative tumors were classified as luminal A molecular subtype, whereas ER-positive, PR-positive, and either HER2-positive or high Ki-67 level lesions were categorized as luminal B (25). HER2 overexpression was also defined as the specimen positive for HER2 >30% of invasive tumor cells (3+) but negative for both ER and PR. Finally, the pathologic tumor size was also measured by a breast pathologist, and the greatest lesion diameter was recorded in millimeters for analyses.
Statistical analysis
All analyses were conducted using SPSS software for Windows, version 22 (IBM Corp, Armonk, NY, USA) (26). Primary descriptive statistics of the study were reported as frequency distribution, mean, and standard deviation. Concordance between the measurements made by each of the three imaging modalities with the pathologically determined tumor size was evaluated using a cut-off point of 5 mm according to previous studies (27, 28, 29, 30).
The effects of various factors were evaluated on the accuracy of tumor size measurement using the three imaging techniques. To evaluate the correlation between qualitative variables, chi-squared and Fisher’s Exact tests were used as needed. To determine the independent risk factors for discordance between measurements, multivariate logistic regression analysis was performed. The variables found to be significantly correlated with the discordance of the measurements in univariate analysis were included in the regression models. A p-value of less than 0.05 was considered statistically significant in all analyses.
Ethical considerations
The objectives and methods of the study were thoroughly explained to the patients, and informed written consent was obtained from all subjects willing to participate in the study. They were reassured that their inclusion in the survey would not affect their treatment in any way and that they could withdraw from the study at any time. Data gathered from patients were considered confidential and used anonymously, and only the main researchers had access to the information. The study protocol was evaluated and approved by the Institutional Review Board of the Tehran University of Medical Sciences.
Results
Descriptive statistics
A total of 86 breast cancer patients were recruited to participate in the study, of which 10 received neoadjuvant chemotherapy before surgical resection of the tumor and were subsequently excluded. Data from 76 patients with 84 lesions in their breasts were analyzed in the study. Descriptive statistics for variables of interest are presented in Table 1.
Table 1. Descriptive statistics of evaluated variables in the study.
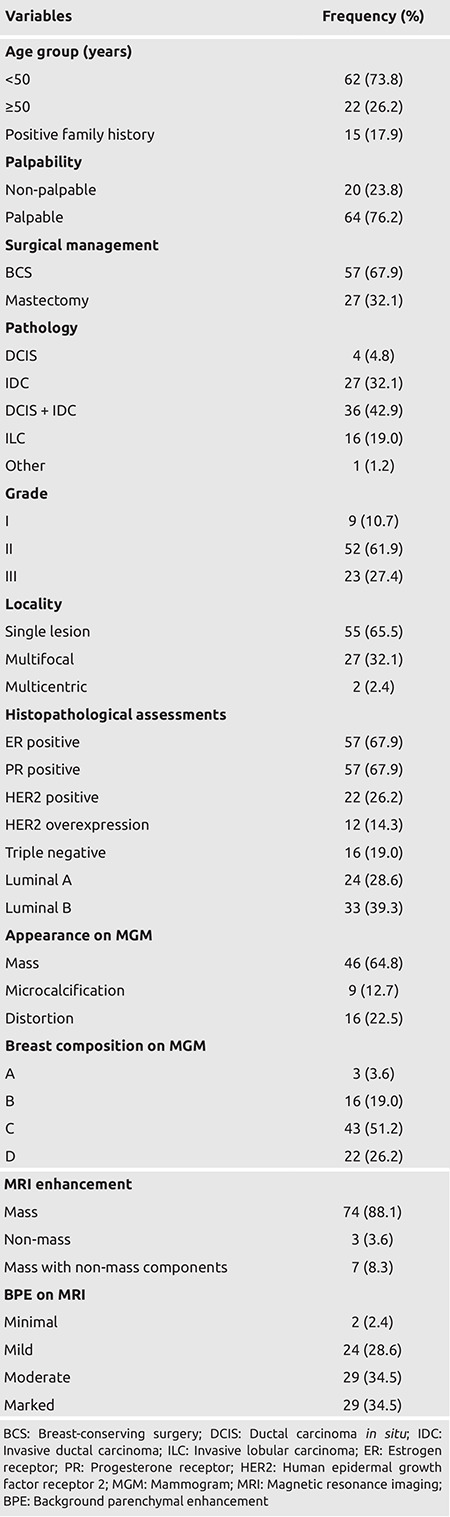
Most participants (67.9%) underwent BCS and 27 (32.1%) mastectomy. The most common pathology type in these patients was a combination of DCIS and invasive ductal carcinoma (IDC) (42.9%); 27 (32.1%) lesions were reported to be IDC, 16 (19.0%) ILC, and 4 (4.8%) DCIS alone.
Based on the results of immunohistochemical assessments, HER2 overexpression was reported in 12 cases (14.3%), and 16 (19.0%) were found to be triple negative, and the molecular subtype was luminal A in 24 lesions (28.6%) and luminal B in 33 (39.3%).
As for the findings of imaging modalities, no particular lesions were observed in 13 MGMs (15.5%). The lesion was visualized as a mass in 46 MGMs (54.8%) and as distortion in 16 (19.0%), whereas microcalcifications were observed in nine MGMs (10.7%). Breast composition in most cases (51.2%) was reported as C, whereas in 22 (26.2%), 16 (19.0%), and 3 (3.6%) cases were D, B, and A, respectively. However, the lesion was visualized as a mass in 74 (88.1%) of the evaluated MRIs, non-mass enhancement in 3 (3.6%), and both mass lesions and non-mass components in 7 (8.3%). Based on the MRIs of these cases, BPE was also reported to be minimal in 2 (2.4%), mild in 24 (28.6%), moderate in 29 (34.5%), and marked in 29 (34.5%).
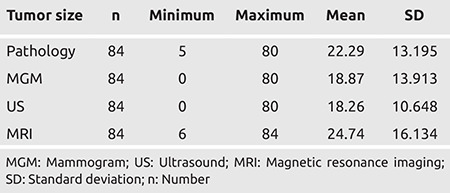
Table 2 presents the overall statistics of the measurements of the three imaging modalities and pathological assessments. According to these findings, MGM measurements were concordant with pathologically determined tumor sizes in 54 lesions (64.3%). Among the 30 (35.7%) discordant cases, underestimation (70.0%) was more prevalent than overestimation (30.0%). As for the US, the estimates were concordant with the gold standard in 64 cases (76.2%), with 80% of the discordant measurements being underestimates and 20% overestimates. The highest concordance rate was observed in MRI-based estimates (82.1%) with only 15 cases showing discordance, which is composed of underestimates in three cases (20%) and overestimates in 12 (80.0%).
Table 2. Overall statistics of the measurements by the three imaging modalities and pathological assessments.
Analytical statistics
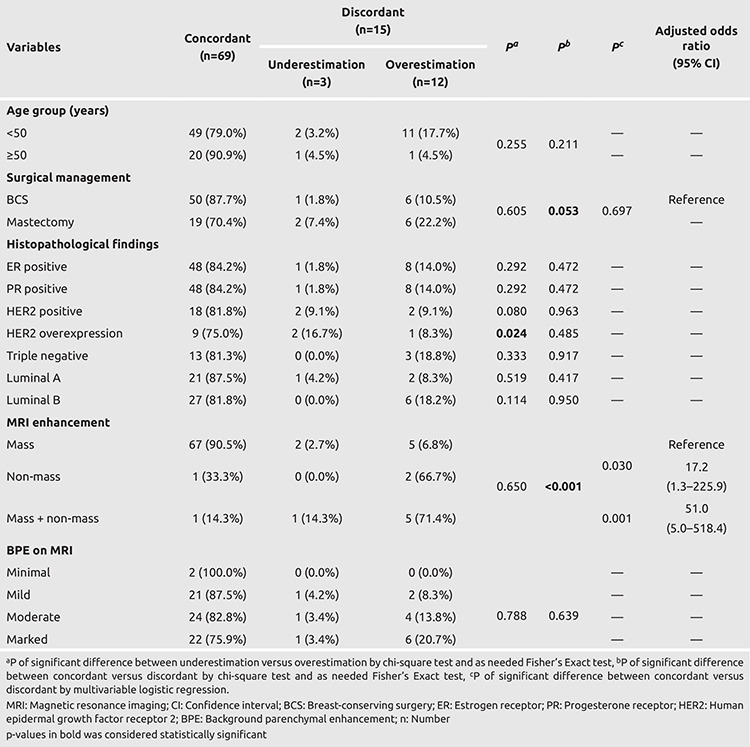
The correlation between the accuracy of tumor size measurements by each of the three imaging modalities was evaluated for all variables included in the study. Accordingly, Tables 3, 4, and 5 present the results of these analyses for MGM, US, and MRI, respectively.
Table 3. Correlation between the evaluated factors in the study with accuracy of tumor size estimation via MGM.
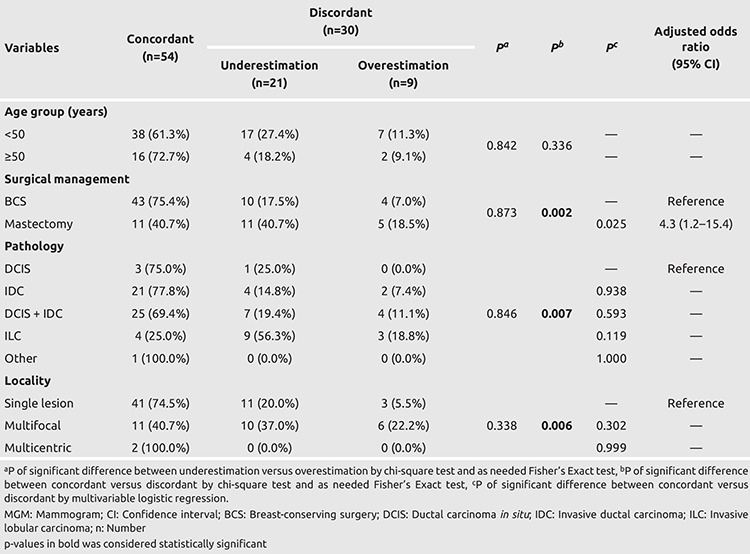
Table 4. Correlation between the evaluated factors in the study with accuracy of tumor size estimation via US.

Table 5. Correlation between the evaluated factors in the study with accuracy of tumor size estimation via MRI.
As can be seen, none of the included variables were significantly correlated with the type of discordance between MGM and pathological measurements. Univariate analyses showed that the surgical management type (p=0.002), tumor pathology (p=0.007), and lesion locality (p=0.006) were significantly correlated with the accuracy of MGM measurements. Subsequently, these variables were included in a regression model, and the results of which showed that tumor size estimates via MGM in patients that underwent mastectomy were more likely to be discordant with the pathological measurements compared with that in subjects who underwent BCS [p=0.025; odds ratio (OR): 4.3; 95% confidence interval (CI): 1.2–15.4].
As presented in Table 4, univariate analysis found that surgical management type (p<0.001) and lesion pathology (p=0.039) were significantly correlated with the accuracy of US. A regression model including these two variables showed that tumor size estimation via US in cases that underwent mastectomy was more likely to be discordant with the pathological measurements compared with that in patients who underwent BCS (p=0.006; OR: 5.7; 95% CI: 1.7–19.3).
According to the results presented in Table 5, underestimation of tumor size by MRI was more prevalent in patients with HER2 overexpression (p=0.024). Univariate analysis found that MRI enhancement type (p<0.001) was significantly correlated with MRI accuracy. The surgical management type also had a borderline p-value of 0.053, and both of these variables were included in the regression model. This analysis showed that tumor size estimates in patients whose MRIs showed either non-mass enhancement (p=0.030; OR: 17.2; 95% CI: 1.3–225.9) or mass lesion with non-mass enhancement (p=0.001; OR: 51.0; 95% CI: 5.0–518.4) were more likely to be discordant with pathological measurements compared with that in cases with only mass lesions on their MRIs (Figures 1 and 2).
Figure 1.
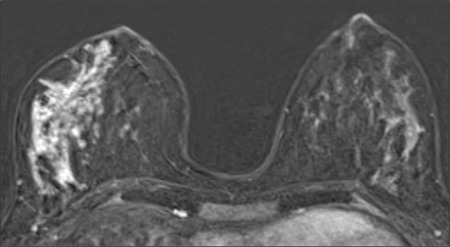
Non-mass enhancement. Magnetic resonance imaging of non-mass enhancement in a 30-year-old patient with invasive ductal carcinoma and extensive ductal carcinoma in situ component. The non-mass enhancement measured 76 mm along the maximum diameter, whereas the pathology reported 11 mm invasive component along with 55 mm in situ component. MRI inaccurately measured the tumor size in this non-mass enhancement
MRI: Magnetic resonance imaging
Figure 2.
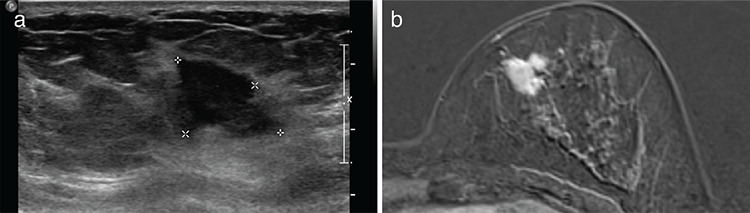
Concordant mass in magnetic resonance imaging (MRI) and ultrasound (US). A 32-year-old patient with invasive ductal carcinoma measuring 22 mm in the pathology (a). US shows an irregular mass measuring 19 mm in the upper inner quadrant of the left breast (b). MRI shows lobulated- enhancing mass with 22 mm in the longest dimension. In this patient, MRI and US are in concordance with the pathology
Discussion and Conclusion
This study provided further evidence on the accuracy of MGM, US, and MRI in estimating breast tumor size by evaluating their concordance with the gold standard of pathological measurements of the surgical specimen. We also investigated the effects of various factors on the accuracy of their measurements, including histology type, molecular subtypes, breast density, BI-RADS type of enhancement, and BPE.
Statistical analysis of data gathered from 84 lesions in 76 breast cancer patients found that the rates of concordance with the gold standard were 64.3%, 76.2%, and 82.1% for MGM, US, and MRI measurements, respectively. The proportion of discordant cases that were reported to be an overestimation of the actual tumor size was 30% for MGM, 20% for US, and 80.0% for MRI.
As mentioned, many studies have evaluated the accuracy of tumor size estimates from these three imaging modalities with contradictory results. For instance, some studies have reported US to be more accurate than MGM (7, 11, 15, 18), whereas others have reported the opposite (13, 14, 21, 31). Boetes et al. (20) analyzed histologic results and imaging findings of 61 tumors in 60 women who had mastectomies and reported MRI to have the highest accuracy among the three imaging modalities, with MGM and US underestimating tumor sizes by 14% and 18%, respectively. Meanwhile, Gruber et al. (21) analyzed data from 121 patients with primary breast cancer and reported that US significantly underestimated tumor size. The study further revealed that MRI overestimated lesion dimensions, but the differences were not significant, whereas MGM showed the most accurate measurements with no significant difference with histological sizing (21). In a more extensive survey conducted on 6,543 patients with unifocal, unilateral primary breast cancer, Stein et al. (32) reported a slightly higher correlation between MGM and pathological examination than US (r=0.61 vs 0.60, respectively).
Further analyses showed that tumor size estimation with either of the two imaging modalities of MGM and US in patients who underwent mastectomy was more likely to be discordant with pathological measurements compared with that in subjects who underwent BCS. These findings could be attributed to underestimate tumor size in mastectomy specimens by pathology. Just as Rominger et al. (33) explained, mastectomy specimens are sliced and evaluated along the anatomical axis, not the tumor axis. Accordingly, they suggested taking advantage of preoperative MRI for determining the axis, along which the tumor should be sliced for pathological evaluations. For MRI, owing to its overall higher accuracy for all lesions, the correlation between the type of surgical intervention and concordance with the gold standard loses its significance, and the pattern of enhancement becomes more prominent. In this regard, the analyses showed that tumor size estimation in patients whose MRIs presented with either non-mass enhancement or mass lesion with non-mass enhancement was more likely to be discordant with the pathological measurements compared with that in cases with only mass lesion on their MRIs.
Rominger et al. (33) also found that the only factor that significantly predicts discordance between MRI and histological measurements is non-mass enhancement of the lesion. Their findings were congruent with the results of this study; however, in our study, the number of non-mass enhancement and mass lesions with non-mass enhancement was limited.
In another study, Baek et al. (34) showed that HER2 overexpression along with BPE could affect the accuracy of measurements using MRI; however, the most important factor that contributed to the discordance of MRI measurements with that of the pathological evaluations is the BI-RADS enhancement type. Our study also showed that HER2 overexpression is related to the underestimation of tumor size in MRI (p=0.024), but the most significant attributing factor was the lesion enhancement type (mass vs non-mass).
Previous studies have reported that MGM and US tend to underestimate the size of ILCs. In our series, 19% of the lesions were diagnosed as ILC, and the rates of concordance for US and MGM were 50% and 25%, respectively, whereas MRI provided a concordance rate of 68%. Therefore, congruent with previous studies, our results showed that MRI is more accurate for tumor size measurement in ILC subtype lesions, and the accuracy of this modality is less affected by the histopathological subtype (21, 35).
Overall, despite the higher accuracy of MRI compared with that of US and MGM in estimating breast tumor sizes, the high cost, higher overestimation rate, and limited availability have prevented widespread application of this imaging modality in standard practice. In this regard, it seems that MRI should be reserved for specific subject groups categorized as high risk by the American Cancer Society. Caution should be practiced in interpreting data obtained from subjects whose MRIs present with non-mass enhancement, since tumor size could be overestimated by MRI in these subgroups.
Although the limited sample population included in this survey could have affected the results of our analyses, the specific setting of this study enabled us to gather information from the three imaging modalities in all our subjects, which minimized missing data in the analyses. Reevaluation of the patients’ MGMs along with their USs and MRIs by a single breast specialist radiologist with extensive experience in the field decreased interobserver variability to its minimum; however, this is noted as a limitation because of the possibility of intraobserver error. Further investigations are required to determine the factors associated with tumor size estimation discordance via imaging modalities with pathological measurements.
In conclusion, MRI was more accurate than US and MGM in estimating breast tumor size with concordance rates of 82.1%, 76.2%, and 64.3% respectively, but it had the highest overestimation rate (80%) among the three modalities. Thus, caution should be practiced in interpreting data obtained from subjects whose MRIs present with non-mass enhancement or mass lesion with non-mass.
Key Points
• MRI is the most accurate imaging technique in estimating breast tumor size.
• MRI is more accurate for tumor size measurement in ILC subtype lesions.
• HER2 overexpression is related to underestimation of tumor size in MRI.
Footnotes
Ethics Committee Approval: The study protocol was evaluated and approved by the Institutional Review Board of the Tehran University of Medical Sciences (no: IR.TUMS.VCR.REC.1395.604, date: 2016/9/13).
Informed Consent: The objectives and methods of the study were thoroughly explained to the patients, and informed written consent was obtained from all subjects willing to participate in the study.
Peer-review: Externally-peer reviewed.
Authorship Contributions
Concept: S.A., M.R.; Design: S.A., M.R., A.K.; Supervision: M.R., N.S., A.K.; Funding: M.R.; Materials: S.A., M.R., A.K.; Data Collection and/or Processing: S.A., M.R., N.S., A.K.; Analysis and/or Interpretation: S.A., M.R., N.S., A.K.; Literature Review: S.A.; Writing: S.A., N.S.; Critical Review: M.R., A.K.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors did not receive any financial support or grant.
References
- 1.U.N.I.o. Health, National Cancer Institute. Surveillance, Epidemiology, and End Results Program. National Cancer Institute. 2011; Available at: [Internet] https://seer.cancer.gov/statfacts/html/breast.html .
- 2.Szabó BK, Aspelin P, Wiberg MK, Tot T, Boné B. Invasive breast cancer: correlation of dynamic MR features with prognostic factors. Eur Radiol. 2003;13:2425–2435. doi: 10.1007/s00330-003-2000-y. [DOI] [PubMed] [Google Scholar]
- 3.Houssami N, Ciatto S, Macaskill P, Lord SJ, Warren RW, Dixon JM. Accuracy and surgical impact of magnetic resonance imaging in breast cancer staging: systematic review and meta-analysis in detection of multifocal and multicentric cancer. J Clin Oncol. 2008;26:3248–3258. doi: 10.1200/JCO.2007.15.2108. [DOI] [PubMed] [Google Scholar]
- 4.Feig S. Breast masses, Mammographic and sonographic evaluation. Radiol Clin North Am. 1992;30:67–92. [PubMed] [Google Scholar]
- 5.Yang WT, Lam W, Cheung H, Suen M, King W, Metreweli C. Sonographic, magnetic resonance imaging, and mammographic assessments of preoperative size of breast cancer. J Ultrasound Med. 1997;16:791–797. doi: 10.7863/jum.1997.16.12.791. [DOI] [PubMed] [Google Scholar]
- 6.Fornage BD, Toubas O, Morel M. Clinical, mammographic, and sonographic determination of preoperative breast cancer size. Cancer. 1987;60:765–771. doi: 10.1002/1097-0142(19870815)60:4<765::aid-cncr2820600410>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 7.Madjar H, Ladner H, Sauerbrei W, Oberstein A, Prömpeler H, Pfleiderer A. Preoperative staging of breast cancer by palpation, mammography and high‐resolution ultrasound. Ultrasound Obstet Gynecol. 1993;3:185–190. doi: 10.1046/j.1469-0705.1993.03030185.x. [DOI] [PubMed] [Google Scholar]
- 8.Farina R, Sparano A. Errors in sonography. In: Errors in Radiology. Milano:Springer. 2012;. p.:79–85. [Google Scholar]
- 9.Lehman CD, Gatsonis C, Kuhl CK, Hendrick RE, Pisano ED, Hanna L. MRI evaluation of the contralateral breast in women with recently diagnosed breast cancer. N Engl J Med. 2007;356:1295–1303. doi: 10.1056/NEJMoa065447. [DOI] [PubMed] [Google Scholar]
- 10.Berg WA, Gutierrez L, NessAiver MS, Carter WB, Bhargavan M, Lewis RS, et al. Diagnostic accuracy of mammography, clinical examination, US, and MR imaging in preoperative assessment of breast cancer. Radiology. 2004;233:830–849. doi: 10.1148/radiol.2333031484. [DOI] [PubMed] [Google Scholar]
- 11.Hieken TJ, Harrison J, Herreros J, Velasco JM. Correlating sonography, mammography, and pathology in the assessment of breast cancer size. Am J Surg. 2001;182:351–354. doi: 10.1016/s0002-9610(01)00726-7. [DOI] [PubMed] [Google Scholar]
- 12.Iacconi C, Thakur SB, Dershaw DD, Brooks J, Fry CW, Morris EA. Impact of fibroglandular tissue and background parenchymal enhancement on diffusion weighted imaging of breast lesions. Eur J Radiol. 2014;83:2137–2143. doi: 10.1016/j.ejrad.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 13.Golshan M, Fung B, Wiley E, Wolfman J, Rademaker A, Morrow M. Prediction of breast cancer size by ultrasound, mammography and core biopsy. Breast. 2004;13:265–271. doi: 10.1016/j.breast.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 14.Heusinger K, Löhberg C, Lux M, Papadopoulos T, Imhoff K, Schulz-Wendtland R. Assessment of breast cancer tumor size depends on method, histopathology and tumor size itself. Breast Cancer Res Treat. 2005;94:17–23. doi: 10.1007/s10549-005-6653-x. [DOI] [PubMed] [Google Scholar]
- 15.Shoma A, Moutamed A, Ameen M, Abdelwahab A. Ultrasound for accurate measurement of invasive breast cancer tumor size. Breast J. 2006;12:252–256. doi: 10.1111/j.1075-122X.2006.00249.x. [DOI] [PubMed] [Google Scholar]
- 16.Wasif N, Garreau J, Terando A, Kirsch D, Mund DF, Giuliano AE. MRI versus ultrasonography and mammography for preoperative assessment of breast cancer. Am Surg. 2009;75:970–975. [PubMed] [Google Scholar]
- 17.Lim HI, Choi JH, Yang JH, Han BK, Lee JE, Lee SK. Does pre-operative breast magnetic resonance imaging in addition to mammography and breast ultrasonography change the operative management of breast carcinoma? Breast Cancer Res Treat. 2010;119:163. doi: 10.1007/s10549-009-0525-8. [DOI] [PubMed] [Google Scholar]
- 18.Fasching PA, Heusinger K, Loehberg CR, Wenkel E, Lux MP, Schrauder M. Influence of mammographic density on the diagnostic accuracy of tumor size assessment and association with breast cancer tumor characteristics. Eur J Radiol. 2006;60:398–404. doi: 10.1016/j.ejrad.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Verma R, Mathur R, Raikwar R, Kaushal M, Miishra H, Shukla R, et al. Comparison of clinical assessment, mammography, and ultrasound in pre-operative estimation of primary breast-cancer size: a practical approach. Internet J Surg. 2008;16:12. [Google Scholar]
- 20.Boetes C, Mus R, Holland R, Barentsz JO, Strijk SP, Wobbes T. Breast tumors: comparative accuracy of MR imaging relative to mammography and US for demonstrating extent. Radiology. 1995;197:743–747. doi: 10.1148/radiology.197.3.7480749. [DOI] [PubMed] [Google Scholar]
- 21.Gruber IV, Rueckert M, Kagan KO, Staebler A, Siegmann KC, Hartkopf A. Measurement of tumour size with mammography, sonography and magnetic resonance imaging as compared to histological tumour size in primary breast cancer. BMC Cancer. 2013;13:328. doi: 10.1186/1471-2407-13-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ramirez SI, Scholle M, Buckmaster J, Paley RH, Kowdley GC. Breast cancer tumor size assessment with mammography, ultrasonography, and magnetic resonance imaging at a community based multidisciplinary breast center. Am Surg. 2012;78:440–446. [PubMed] [Google Scholar]
- 23.D’Orsi CJ, Sickles EA, Mendelson EB, Morris EA. ACR BI-RADS Atlas, Breast Imaging Reporting and Data System. 5th ed. Reston, VA; American College of Radiology. 2013. [Google Scholar]
- 24.Morris EA. Diagnostic breast MR imaging: current status and future directions. Radiol Clin North Am. 2007;45:863–880. doi: 10.1016/j.rcl.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 25.Ebili HO, Oluwasola AO, Olopade OI. Molecular subtypes of breast cancer, Personalized Management of Breast Cancer, Holloway, T.L., Jatoi, I., Eds. Future Medicine Ltd.: London, UK. 2014;pp.:20–33. [Google Scholar]
- 26.Corp I. IBM SPSS statistics for windows, version 22.0, IBM Corp Armonk, NY. 2014. Available from: [Internet] https://www.ibm.com/support/pages/how-cite-ibm-spss-statistics-or-earlier-versions-spss .
- 27.Grimsby GM, Gray R, Dueck A, Carpenter S, Stucky CC, Aspey H. Is there concordance of invasive breast cancer pathologic tumor size with magnetic resonance imaging? Am J Surg. 2009;198:500–504. doi: 10.1016/j.amjsurg.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 28.Onesti JK, Mangus BE, Helmer SD, Osland JS. Breast cancer tumor size: correlation between magnetic resonance imaging and pathology measurements. Am J Surg. 2008;196:844–850. doi: 10.1016/j.amjsurg.2008.07.028. [DOI] [PubMed] [Google Scholar]
- 29.Luparia A, Mariscotti G, Durando M, Ciatto S, Bosco D, Campanino PP. Accuracy of tumour size assessment in the preoperative staging of breast cancer: comparison of digital mammography, tomosynthesis, ultrasound and MRI. Radiol Med. 2013;118:1119–1136. doi: 10.1007/s11547-013-0941-z. [DOI] [PubMed] [Google Scholar]
- 30.Lai HW, Chen DR, Wu YC, Chen CJ, Lee CW, Kuo SJ. Comparison of the diagnostic accuracy of magnetic resonance imaging with sonography in the prediction of breast cancer tumor size: a concordance analysis with histopathologically determined tumor size. Ann Surg Oncol. 2015;22:3816–3823. doi: 10.1245/s10434-015-4424-4. [DOI] [PubMed] [Google Scholar]
- 31.Alikhassi A, Omranipour R, Shahriyaran S, Hadji M, Abdi A, Alikhassy Z. Correlation between imaging and pathologic measurement of breast cancer tumor size. Arch Breast Cancer. 2015;2:64–68. [Google Scholar]
- 32.Stein RG, Wollschläger D, Kreienberg R, Janni W, Wischnewsky M, Diessner J. The impact of breast cancer biological subtyping on tumor size assessment by ultrasound and mammography-a retrospective multicenter cohort study of 6543 primary breast cancer patients. BMC Cancer. 2016;16:459. doi: 10.1186/s12885-016-2426-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rominger M, Berg D, Frauenfelder T, Ramaswamy A, Timmesfeld N. Which factors influence MRI-pathology concordance of tumour size measurements in breast cancer? Eur Radiol. 2016;26:1457–1465. doi: 10.1007/s00330-015-3935-5. [DOI] [PubMed] [Google Scholar]
- 34.Baek JE, Kim SH, Lee AW. Background parenchymal enhancement in breast MRIs of breast cancer patients: Impact on tumor size estimation. Eur J Radiol. 2014;83:1356–1362. doi: 10.1016/j.ejrad.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 35.França LKL, Bitencourt AGV, Paiva HLS, Silva CB, Pereira NP, Paludo J. Role of magnetic resonance imaging in the planning of breast cancer treatment strategies: comparison with conventional imaging techniques. Radiol Bras. 2017;50:76–81. doi: 10.1590/0100-3984.2015.0124. [DOI] [PMC free article] [PubMed] [Google Scholar]


