Abstract
Objectives:
This cross-sectional study examines the association between perceived sidewalk conditions and neighborhood participation among older adults in the REasons for Geographic and Racial Differences in Stroke (REGARDS) Study.
Methods:
Between 2013–2016 14,233 REGARDS participants completed a second in-home visit. Using logistic regression, we cross-sectionally examined if perceived severity of sidewalk problems was associated with going into the neighborhood less than once compared to 1–7 times per week.
Results:
The analytic sample included participants (N=9,863) with non-missing data. The likelihood of going into the neighborhood less than 1 time per week was greater among participants who reported minor (OR=1.15; 95% CI: 1.00, 1.33), somewhat serious (OR=1.41; 95% CI: 1.17, 1.70) and very serious (OR=1.65; 95% CI: 1.38, 1.98) sidewalk problems in their neighborhood compared to those reporting no sidewalk problems, independent of demographic, socioeconomic, and impairment characteristics.
Discussion:
Perceived sidewalk problems appear to deter neighborhood participation among older adults.
Keywords: Aging in place, Neighborhood sidewalks, Built environment, Participation
Introduction
It is well established through framework, theory, and empirical investigation that context is critical for the course and direction of aging (Brenner & Clarke, 2018; Carp, 1967; Kim & Clarke, 2015; Lawton & Nahemow, 1973; Ng et al., 2018; Spring, 2018). These investigations have developed into an entire field of environmental gerontology dedicated to understanding how to optimize relationships between aging adults and their physical and social environments. This expanding field is not surprising given the majority of older adults’ daily activities take place in the home and neighborhood environment, constituting these as major living spaces for adults as they age (Baltes, Maas, Wilms, Borchelt, & Little, 1999). Studies in this area have found that aging is influenced by multidimensional (e.g. environmental demands, individual capacity) and dynamic factors (Nahemow & Lawton, 1973). To encourage healthy aging, it is essential to quantify effects of surrounding neighborhood environments on neighborhood participation (World Health Organization, 2002).
Accessible and safe neighborhood environments, including built environment characteristics, are critical components for older adults to remain active and independent within their communities (Kerr, Rosenberg, & Frank, 2012). Older adults may be more vulnerable to increased demands of the built environment due to changes in physiologic and neuromuscular function associated with aging (Nahemow & Lawton, 1973). Empirical investigation has found that the built environment plays an important role for continued neighborhood participation and engagement among older adults. For example, heavy traffic volume and minimal residential security signs have been shown to be negatively associated with social interaction, obtaining preventive health care, and voting in the most recent government elections among older adults (P. J. Clarke, Ailshire, Nieuwenhuijsen, & de Kleijn-de Vrankrijker, 2011). In addition, built environment attributes (e.g. residential density, street connectivity, land use mix, walkability, public transport, aesthetics, and safety) have been shown to be an important driver of physical activity behavior among older adults (Barnett, Barnett, Nathan, Van Cauwenberg, & Cerin, 2017; Cerin, Nathan, van Cauwenberg, Barnett, & Barnett, 2017; Van Cauwenberg, Nathan, Barnett, Barnett, & Cerin, 2018). In a recent systematic review, Barnett et al. (2017) found that walkability (i.e. access to destinations and services) and personal safety from crime were all positively associated with physical activity behavior among older adults. However, the built environment encompasses many different facets of the outdoor streetscape (e.g. connectivity, access to destinations, accessibility, social disorder). This can make it difficult to provide pointed recommendations for improvements of the urban landscape to promote neighborhood participation and active aging within the population.
One feature of the built environment that older adults have identified as important, but has received limited attention in the literature, is access to safe and high-quality neighborhood sidewalks. As people grow older, the neighborhood sidewalk may provide a critical connection to the outside world. In a poll conducted by the American Association of Retired Persons (AARP), 40% of adults indicated that the sidewalks within their neighborhood were inadequate, and 50% did not have a safe route to cross main roads near their home (Lynott et al., 2009). Of those reporting problems within their community, half said they would walk, bike, or take the bus more often if the problems were resolved (Lynott et al., 2009). Within a survey conducted in Belo Horizonte, Brazil, nearly half (48.2%) of participants were concerned about walking around in their neighborhood because they were fearful of falling due to sidewalk defects (Ferreira, Cesar, Camargos, Lima-Costa, & Proietti, 2010). This fear is justified given the fact that each year more than 9,000 older pedestrian fall-related injuries in the United States involve a curb (Naumann, Dellinger, Haileyesus, & Ryan, 2011). Furthermore, using the National Health Interview Survey sample adult core, Theis and Furner (2011) found that sidewalks and curbs were one of the most frequently reported environmental barriers leading to a participation restriction in neighborhood life, especially among those with chronic health conditions.
Even though survey-based research suggests participation in the community is affected by the ability of older adults to safely use their built environment, there is limited evidence that explores the explicit relationship between sidewalk problems and neighborhood participation among older adults. The Chicago Community Adult Health Study found that sidewalk quality is associated with mobility difficulty, but only among adults with severe physical impairment (P. Clarke, Ailshire, Bader, Morenoff, & House, 2008). Furthermore, sidewalks and streets in poor conditions were associated with a decreased likelihood of voting among those with mobility difficulty (P. J. Clarke et al., 2011). A recent study of older adults living in Finland found the relationship between quality of sidewalks and physical activity was dependent on neighborhood type (Keskinen, Rantakokko, Suomi, Rantanen, & Portegijs, 2019). Evenness of sidewalks was associated with the likelihood of physical activity, but only among those living in areas outside of city centers and not within more densely populated environments (Keskinen et al., 2019). Conversely, a longitudinal study within the South Holland city of Spijkenisse in the Netherlands, found that sidewalk features were not associated with self-reported difficulty in activities of daily living (ADL) or outdoor active transport (i.e. walking or cycling for transport) among older adults 65 years and older, after controlling for age and sex (Etman, Kamphuis, Pierik, Burdorf, & Van Lenthe, 2016). There is a need to better understand the relationship between sidewalks and neighborhood participation given the disagreement in the literature. Furthermore, all of the above-mentioned projects had limited geographic variability, limiting their generalizability to the population at large.
To better understand the role of sidewalks for neighborhood participation in older adults, we expand on previous literature and investigate the association between sidewalk conditions and neighborhood participation in a large, geographically diverse cohort of older Americans. Specifically, we answer the question: is severity of sidewalk problems associated with lower levels of neighborhood participation (frequency of going into the neighborhood) among older adults? We hypothesize that living in an area where no sidewalks or poorly maintained sidewalks were considered a very serious problem would restrict the frequency of neighborhood participation among older people. We also hypothesized that the relationship between sidewalk problems and frequency of participation would interact with self-reported limitations in ADL and mobility aid use to restrict the frequency of neighborhood participation.
Methods
Study Population
This study includes cross-sectional analyses from data of the REasons for Geographic and Racial Differences in Stroke (REGARDS) cohort study. REGARDS is a longitudinal closed cohort study within the United States examining risk factors associated with incident stroke (V. J. Howard et al., 2005). REGARDS randomly selected potential participants from a commercially available national list purchased through Genesys Incorporated, the same source utilized for recruitment in other large-scale surveillance studies (G. Howard et al., 2017; Schneider, Clark, Rakowski, & Lapane, 2012). Due to the project goals, participants who self-identified as non-Hispanic Black or those living within the stroke belt were oversampled. The stroke belt is a region in the southeastern United States with high incidence of stroke and cardiovascular disease, and includes the following states: Alabama, Arkansas, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, and Tennessee. A total of 30,239 participants were enrolled in REGARDS, and participant recruitment took place between January 2003 and October 2007. Inclusion criteria for enrollment into REGARDS consists of individuals: over the age of 45 years, self-identified as Black or White, no prior history of stroke, no recent history of a cancer diagnosis that required chemotherapy, English speaker, and not on a waiting list to enter a nursing home (V. J. Howard et al., 2005).
After verbal consent via telephone, participants completed a baseline computer-assisted telephone interview to obtain demographic and medical information. The telephone interview was followed by an in-home physical examination approximately three to four weeks later. A total of 30,239 participants completed the initial interview. The final sample comprised 56% from stroke belt, 42% Black, and 55% women (V. J. Howard et al., 2005). Approximately ten years after the baseline interview, participants were contacted with an invitation to participate in a follow-up assessment. The follow-up assessment included a computer-assisted telephone interview, in-home interview, and self-administered questions contained in a leave behind survey (Long et al., 2019; Mefford et al., 2018). The follow-up assessments took place between May 2013 and November 2016, with approximately half (N=14,233; 47%) of participants from the full cohort completing the second in-home examination and telephone interview (Long et al., 2019; Mefford et al., 2018). The current project included all participants who had complete data on the main exposure, main outcome, and all covariates of interest. Written informed consent was obtained at the in-home visit and the study was approved by all participating Institutional Review Boards.
Sidewalk Problems
Sidewalk problems were assessed at the second in-home interview via self-report. Participants were asked: “Think about your neighborhood as a whole, then please choose the best option for each of the following (items) to show how much of a problem each one is in your neighborhood.” Participants responded to how much of a problem “No sidewalks or poorly maintained sidewalks” were within their neighborhood. Participants could respond by indicating that no sidewalks or poorly maintained sidewalks were a very serious problem, somewhat serious problem, minor problem, or not really a problem.
Neighborhood Participation
As a measure of neighborhood participation, frequency of going into the neighborhood was assessed at the second in-home interview using the University of Alabama at Birmingham Life-Space Assessment. The Life-Space Assessment is a tool that captures community mobility based on the distance through which a person reports moving during the 4 weeks that precede the assessment (Baker, Bodner, & Allman, 2003; Peel et al., 2005). Life-space was assessed using various spatial scales, ranging from within the participant’s bedroom to beyond their neighborhood. The Life-Space Assessment has been validated as an important clinical measure of community mobility, mortality, nursing home admissions, and hospitalization (Baker et al., 2003; C. J. Brown et al., 2009; Gottlieb, Smith, Wolfenden, Allman, & Tangpricha, 2011; Mackey et al., 2014; Peel et al., 2005; Sheppard, Sawyer, Ritchie, Allman, & Brown, 2013). Within this questionnaire, participants were asked the frequency of getting to places within the neighborhood. Participants responded to the question: “During the past four weeks, how often did you get to places in your neighborhood, other than your own yard or apartment building?” Options for response included: not at all, less than 1 time per week, 1–2 times per week, 4–6 times per week, or daily. Frequent walking episodes within the neighborhood are associated with social participation among older adults (Richard, Gauvin, Gosselin, & Laforest, 2008). Therefore, getting into the neighborhood environment is a necessary component of neighborhood participation.
Covariates
Age was reported as a continuous variable from the follow-up (second) computer assisted telephone interview. Race was captured by participants self-identifying as non-Hispanic White or non-Hispanic Black at baseline interview. Gender, defined as either Male or Female, was measured at baseline through self-report. Individual level socioeconomic status was assessed by asking about individual level income (less than $20,000, $20,000-$34,999, $35,000-$74,999, $75,000 or more) and education (less than high school, high school graduate, some college, college graduate or more) at the baseline interview. Activity limitations were captured using five items representing ADL during the follow-up (second) interview (Katz, Downs, Cash, & Grotz, 1970; Katz, Ford, Moskowitz, Jackson, & Jaffe, 1963). The questions ask participants about difficulty getting out of bed or chair, eating, dressing, bathing, and using the toilet. For each question, participants indicated one of three options: “I could do it by myself with no difficulty”, “I could do it by myself with some difficulty”, or “I would need someone to help me do it”. If a participant reported “I could do it by myself with some difficulty”, “I would need someone to help me do it”, or “Don’t Know/Not Sure” for one of the five ADL questions they were categorized as having an activity limitation. The use of mobility aids was captured during the follow-up (second) interview through the Life-Space Assessment. Within this assessment participants are asked “During the past four weeks, did you use aids or equipment, such as a cane, walker, wheelchair, or something like that” within the neighborhood. The participants responded yes or no to indicate their use of a mobility aid within their neighborhood, resulting in a binary variable where 1 represents participants use a mobility aid within their neighborhood and 0 represents participants who do not use a mobility aid within their neighborhood.
Statistical Analysis
Descriptive statistics of individual characteristics were examined by frequency of going into the neighborhood. To examine the association between sidewalk problems and frequency of going into the neighborhood, we recoded frequency of going into the neighborhood into a binary variable (1 = participants who self-report ‘not at all’ or ‘less than 1 time per week’; 0 = participants who self-report moving throughout the neighborhood 1 or more times per week). Leaving the house less than once per week is often used as criteria for house bound status, and has been associated with morbidity and disability among older adults (Ganguli, Fox, Gilby, & Belle, 1996; Kono & Kanagawa, 2001). Sidewalk problems were treated as a categorical variable with “No sidewalks or poorly maintained sidewalks” being self-reported as “Not really a problem” as the reference group. Using logistic regression, we cross-sectionally examined if sidewalk problems were associated with odds of going into the neighborhood less than 1 time per week compared to 1–7 times per week.
In the first model (Model 1), we assessed the unadjusted effect of sidewalk problems on frequency of going into the neighborhood. Sidewalk problems were treated as a categorical variable with 4 values, using ‘not really a problem’ as the reference group. In Model 2, we adjusted for demographic characteristics including age, race, and gender. Model 3, further adjusted for the socioeconomic status of the participants, captured using two variables: individual level income and education level. Model 4 adjusted for participants self-reported activity limitations. Model 5 adjusted for self-reported mobility aid use within the neighborhood. Within Model 5 a global trend test was performed to assess the shape of relationship between severity of sidewalk problems and frequency of going into the neighborhood.
Lastly, we empirically evaluated the ecological model of aging, which states that the impact of environmental barriers and facilitators varies by personal and functional capacities (Nahemow & Lawton, 1973). Using the previously developed models, we evaluated interaction effects within this logistic model on both additive and multiplicative scales (Knol, van der Tweel, Grobbee, Numans, & Geerlings, 2007; Knol & VanderWeele, 2012; Knol et al., 2011). Measure of interaction on the additive scale was evaluated using the relative excess risk due to interaction (RERI) measure, and interaction on the multiplicative scale was evaluated using the ratio of odds ratios (Knol & VanderWeele, 2012). RERI represents the differences in differences in odds ratios. Model 6 tested interaction on the additive and multiplicative scale between sidewalk problems and self-reported activity limitations, and Model 7 tested the interaction on the additive and multiplicative scale between sidewalk problems and self-reported mobility aid use. Analyses were conducted using STATA 15.0 (College Station, Texas), and an additive interaction tool developed by Knol was used to calculate RERI and corresponding confidence intervals using the delta method (Hosmer & Lemeshow, 1992; Knol & VanderWeele, 2012).
Results
In this cross-sectional study, a total of 9,863 participants from the REGARDS had non-missing data from the follow-up survey and were included in this analysis (Figure 1). As shown in Table 1, the average age of participants did not vary across the severity of sidewalk problems. The proportion of White participants and Male participants decreased with increased severity of sidewalk problems. The proportion of mobility aid users, participants reporting activity limitations, and participants going out less than one time per week increased with increased severity of sidewalk problems. In this population, the proportion of people with higher education or income tended to report less severe sidewalk problems.
Figure 1.
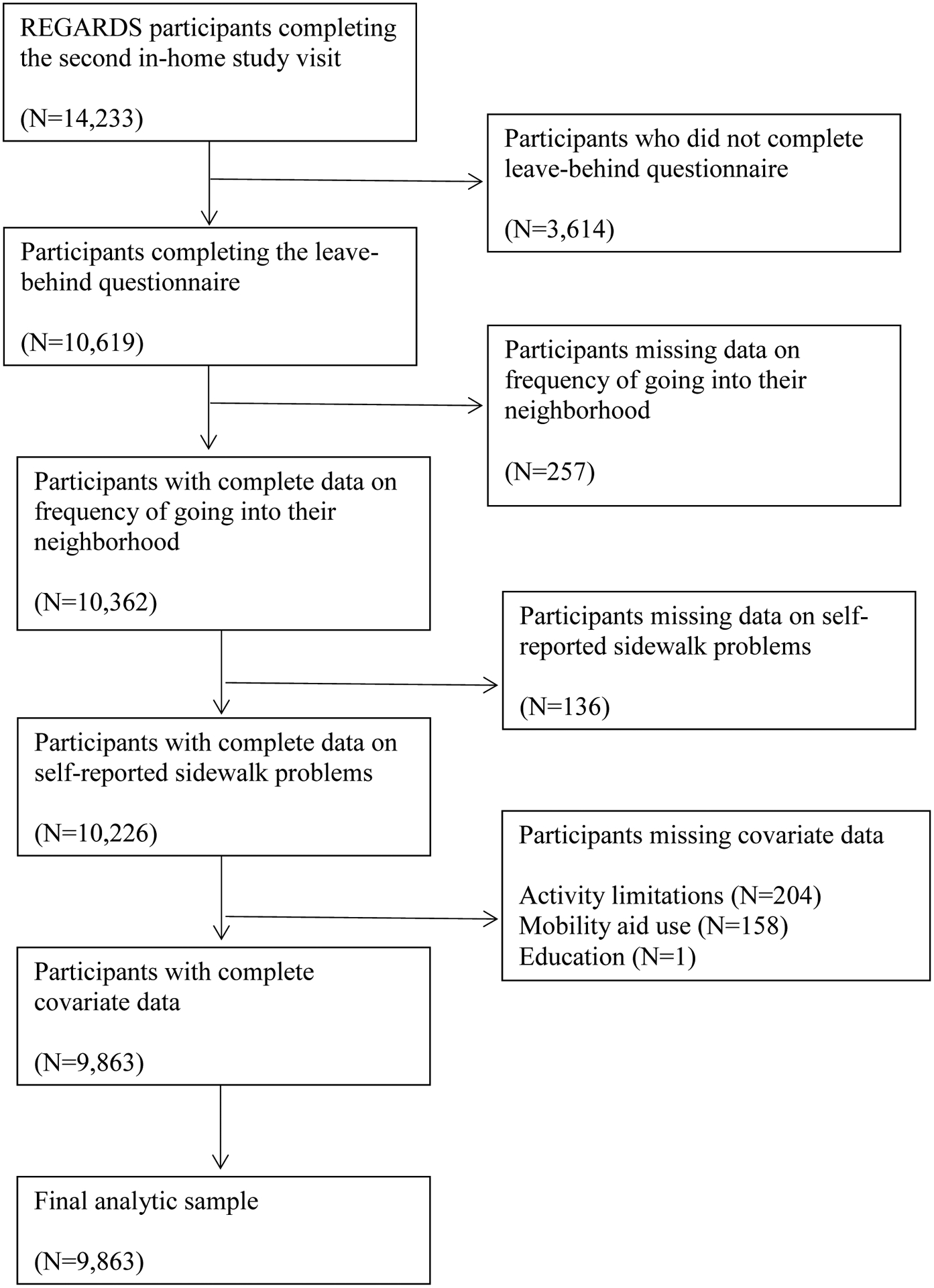
Flow chart of number of participants included and excluded from the analytic sample, and detailed reason for exclusion of participants.
Note: REGARDS = REasons for Geographic and Racial Differences in Stroke
Table 1.
Descriptive statistics for participants within the current study (N=9,863) stratified by self-reported sidewalk problems within the neighborhood
| “No sidewalks or poorly maintained sidewalks” within the neighborhood are… | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total Sample | Not really a problem | Minor problem | Somewhat serious problem | Very serious problem | ||||||||||
| Sample characteristic1 | N = 9,863 | N = 5,653 | N = 2,363 | N = 959 | N =888 | |||||||||
| Age, years (mean [SD]) | 72.3 | (8.3) | 72.7 | (8.3) | 72.2 | (8.4) | 71.5 | (8.2) | 71.2 | (8.0) | ||||
| Race | ||||||||||||||
| White | 6820 | (69%) | 3997 | (71%) | 1664 | (70%) | 638 | (67%) | 521 | (59%) | ||||
| Black | 3043 | (31%) | 1656 | (29%) | 699 | (30%) | 321 | (33%) | 367 | (41%) | ||||
| Gender | ||||||||||||||
| Female | 5545 | (56%) | 3108 | (55%) | 1312 | (56%) | 543 | (57%) | 582 | (66%) | ||||
| Male | 4318 | (44%) | 2545 | (45%) | 1051 | (44%) | 416 | (43%) | 306 | (34%) | ||||
| Income | ||||||||||||||
| $75,000 + | 2155 | (22%) | 1363 | (24%) | 525 | (22%) | 158 | (16%) | 109 | (12%) | ||||
| $35,000–$74,000 | 3368 | (34%) | 1922 | (34%) | 828 | (35%) | 324 | (34%) | 294 | (33%) | ||||
| $20,000–$34,000 | 2140 | (22%) | 1183 | (21%) | 484 | (20%) | 241 | (25%) | 232 | (26%) | ||||
| less than $20,000 | 1136 | (12%) | 567 | (10%) | 261 | (11%) | 136 | (14%) | 172 | (19%) | ||||
| Refused | 1064 | (11%) | 618 | (11%) | 265 | (11%) | 100 | (10%) | 81 | (9%) | ||||
| Education | ||||||||||||||
| College Graduate | 4346 | (44%) | 2532 | (45%) | 1155 | (49%) | 385 | (40%) | 274 | (31%) | ||||
| Some college | 2598 | (26%) | 1454 | (26%) | 611 | (26%) | 276 | (29%) | 257 | (29%) | ||||
| High school/GED | 2280 | (23%) | 1307 | (23%) | 481 | (20%) | 227 | (24%) | 265 | (30%) | ||||
| Less than High School | 639 | (6%) | 360 | (6%) | 116 | (5%) | 71 | (7%) | 92 | (10%) | ||||
| ADL Limitations | ||||||||||||||
| No | 8727 | (88%) | 5087 | (90%) | 2073 | (88%) | 806 | (84%) | 761 | (86%) | ||||
| Yes | 1136 | (12%) | 566 | (10%) | 290 | (12%) | 153 | (16%) | 127 | (14%) | ||||
| Mobility Aid Use | ||||||||||||||
| No | 8567 | (87%) | 4950 | (88%) | 2055 | (87%) | 816 | (85%) | 746 | (84%) | ||||
| Yes | 1296 | (13%) | 703 | (12%) | 308 | (13%) | 143 | (15%) | 142 | (16%) | ||||
| Going into neighborhood | ||||||||||||||
| < 1 time per week | 1543 | (16%) | 777 | (14%) | 363 | (15%) | 190 | (20%) | 213 | (24%) | ||||
| 1–7 times per week | 8320 | (84%) | 4876 | (86%) | 2000 | (85%) | 769 | (80%) | 675 | (76 %) | ||||
Note: SD = Standard Deviation; GED = General Educational Development; ADL = Activities of Daily Living
Variable distributions are reported as n (%) unless otherwise specified.
Table 2 displays the results of the logistic regression, estimating the odds for going into the neighborhood less than one time per week. Within the unadjusted model (Model 1), we observed a dose-response relationship between our exposure and outcome. Increased severity of sidewalk problems is associated with an increased likelihood of going into the neighborhood less than one time per week. The likelihood of going into the neighborhood less than one time per week was higher among those with minor (OR: 1.14; 95% CI: 1.00, 1.30), somewhat serious (OR: 1.55; 95% CI: 1.30, 1.85), and very serious sidewalk problems (OR: 1.98; 1.67, 2.35). This relationship was maintained throughout the model building process, after accounting for age, race, gender, income, and education. Activity limitations significantly increased the likelihood of going into the neighborhood less than one time per week (Model 4; OR = 2.56; 95% CI: 2.21, 2.95). After accounting for self-reported activity limitations, our observed dose response relationship between the severity of sidewalk problems and frequency of going into the neighborhood was maintained. Minor (OR=1.15; 95% CI: 1.00, 1.33), somewhat serious (OR = 1.41; 95% CI: 1.17, 1.70) and very serious (OR = 1.65; 95% CI: 1.37, 1.97) sidewalk problems were significantly associated with the frequency of going into the neighborhood within Model 4. There was no change in the effect estimates for the relationship between the severity of sidewalk problems and frequency of going into the neighborhood after accounting for mobility aid use (Model 5). The global trend test within Model 5 indicated a significant linear trend (χ2=32.9; p<0.001) between severity of sidewalk problems and likelihood of going into the neighborhood less than one time per week. Mobility aid use also increased the likelihood of going into the neighborhood less than one time per week (Model 5; OR=1.19; 95% CI:1.02, 1.40). Within our fully adjusted model, Model 5, the likelihood of going into the neighborhood less than one time per week was greater with increasing age (OR = 1.02; 95% CI: 1.02, 1.03), among those self-identifying as Black (OR = 1.81, 95% CI: 1.61, 2.05), and among those with lower socioeconomic status. The likelihood of going into the neighborhood less than one time per week among men was 0.87 (95% CI: 0.77, 0.99) times the likelihood among women. Participants reporting at least one activity limitation (OR = 2.42; 95% CI: 2.08, 2.82) and using a mobility aid (OR = 1.19; 95% CI: 1.02, 1.40) were more likely to go into the neighborhood less than one time per week compared to those with no activity limitations and no mobility aid use, respectively.
Table 2.
Results from the logistic regression analysis examining the association between self-reported sidewalk problems and going into the neighborhood environment less than one time per weeka
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| 0.16 | (0.15, 0.17) | 0.01 | (0.01, 0.02) | 0.01 | (0.01, 0.02) | 0.01 | (0.01, 0.02) | 0.01 | (0.01, 0.02) | |
| Sidewalk problemsb | ||||||||||
| Minor | 1.14 | (1.00, 1.30) | 1.16 | (1.01, 1.33) | 1.18 | (1.02, 1.36) | 1.15 | (1.00, 1.33) | 1.15 | (1.00, 1.33) |
| Somewhat serious | 1.55 | (1.30, 1.85) | 1.58 | (1.32, 1.89) | 1.49 | (1.24, 1.79) | 1.41 | (1.17, 1.70) | 1.41 | (1.17, 1.70) |
| Very serious | 1.98 | (1.67, 2.35) | 1.88 | (1.57, 2.25) | 1.69 | (1.41, 2.02) | 1.65 | (1.37, 1.97) | 1.65 | (1.38, 1.98) |
| Age | 1.04 | (1.03, 1.04) | 1.03 | (1.02, 1.03) | 1.02 | (1.02, 1.03) | 1.02 | (1.02, 1.03) | ||
| Black race | 2.20 | (1.96, 2.47) | 1.85 | (1.64, 2.08) | 1.83 | (1.62, 2.06) | 1.81 | (1.61, 2.05) | ||
| Male | 0.75 | (0.66, 0.84) | 0.86 | (0.76, 0.97) | 0.87 | (0.77, 0.98) | 0.87 | (0.77, 0.99) | ||
| Incomec | ||||||||||
| $35,000–$74,000 | 1.27 | (1.05, 1.54) | 1.24 | (1.02, 1.50) | 1.23 | (1.02, 1.50) | ||||
| $20,000–$34,000 | 1.66 | (1.35, 2.04) | 1.55 | (1.26, 1.91) | 1.53 | (1.25, 1.89) | ||||
| < $20,000 | 2.13 | (1.69, 2.69) | 1.89 | (1.50, 2.39) | 1.86 | (1.47, 2.35) | ||||
| Refused | 1.67 | (1.32, 2.11) | 1.56 | (1.23, 1.98) | 1.55 | (1.22, 1.97) | ||||
| Educationd | ||||||||||
| Some college | 1.36 | (1.17, 1.58) | 1.36 | (1.17, 1.58) | 1.35 | (1.16, 1.58) | ||||
| High school/GED | 1.61 | (1.38, 1.87) | 1.63 | (1.40, 1.91) | 1.63 | (1.40, 1.90) | ||||
| Less than high school | 2.16 | (1.74, 2.67) | 2.14 | (1.72, 2.66) | 2.14 | (1.72, 2.66) | ||||
| Activity limitation | 2.56 | (2.21, 2.95) | 2.42 | (2.08, 2.82) | ||||||
| Mobility aid use | 1.19 | (1.02, 1.40) | ||||||||
Note: CI = confidence interval; GED = General Educational Development
Relative to going into the neighborhood one to seven times per week
Reference group is sidewalks are “Not really a problem”
Reference group is income $75,000 or greater
Reference group is a college graduate education and above
The results of Model 6 and stratified models are presented within Table 3. Odds ratios and 95% confidence intervals for going into the neighborhood less than one time per week are presented for any activity limitations with no sidewalk problems (OR=2.63; 95% CI: 2.13, 3.24), minor sidewalk problems (OR=2.82; 95% CI: 2.14, 3.72), somewhat serious sidewalk problems (OR=3.07; 95% CI: 2.14, 4.40), and very serious problems (OR=3.67; 95% CI: 2.51, 5.36), where those with no activity limitations and no sidewalk problems is the reference category. Estimates were smaller in magnitude among for no activity limitations with minor sidewalk problems (OR=1.17; 95% CI: 1.00, 1.37), somewhat serious sidewalk problems (OR=1.49; 95% CI: 1.21, 1.83), and very serious sidewalk problems (1.71; 95% CI: 1.40, 2.09), where those with no activity limitations and no sidewalk problems treated as the reference category. The RERI for minor sidewalk problems, somewhat serious sidewalk problems, and very serious sidewalk problems were 0.02 (95% CI: −0.87, 0.91), −0.04 (95% CI: −1.41, 1.32), and 0.33 (95% CI: −1.13, 1.79), respectively. All measures of RERI were near 0, indicating that the estimated joint effect on the additive scale of severity of sidewalk problems and activity limitations was similar to the sum of the estimated associations, meaning there is little evidence of interaction on the additive scale. The measure of interaction on the multiplicative scale, the ratio of odds ratios, for minor sidewalk problems (Ratio ORs: 0.91; 95% CI: 0.64, 1.30), somewhat serious sidewalk problems (Ratio ORs: 0.79; 95% CI: 0.51, 1.22), and very serious sidewalk problems (Ratio ORs: 0.81; 95% CI: 0.52, 1.28) were near a value of 1. This indicates that the joint effect on the odds ratio scale was similar to the product of the estimated effects of activity limitations and severity of sidewalk problems alone. Thus, our results show little evidence of interaction on the multiplicative scale.
Table 3.
Evaluation of additive and multiplicative interaction between severity of sidewalk problems and activity limitations on the likelihood of going into the neighborhood less than one time per week compared to the likelihood of going into the neighborhood one to seven times per week.
| Activity Limitations | ORs (95% CI) for activity limitations within strata of sidewalk problemsb | Measure of interaction on additive scale: RERI (95% CI)c | Measure of interaction on multiplicative scale: Ratio of ORs (95% CI)d | |||||
|---|---|---|---|---|---|---|---|---|
| None | Any | |||||||
| N Y=1/Y=0a |
OR (95% CI) | N Y=1/Y=0a |
OR (95% CI) | |||||
| Severity of Sidewalk Problems | Not really a problem | 597/4490 | 1.00 | 180/386 | 2.63 (2.13, 3.24); P<0.01 | 2.52 (2.03, 3.13); P<0.01 | ||
| Minor problem | 272/1801 | 1.17 (1.00, 1.37); P=0.05 | 91/199 | 2.82 (2.14, 3.72); P<0.01 | 2.40 (1.77, 3.27); P<0.01 | 0.02 (-0.87, 0.91); P=0.48 | 0.91 (0.64, 1.30); P=0.62 | |
| Somewhat serious problem | 138/668 | 1.49 (1.21, 1.83); P<0.01 | 52/101 | 3.07 (2.14, 4.40); P<0.01 | 2.12 (1.39, 3.23); P<0.01 | −0.04 (−1.41, 1.32); P=0.53 | 0.79 (0.51, 1.22); P=0.29 | |
| Very serious problem | 161/600 | 1.71 (1.40, 2.09); P<0.01 | 52/75 | 3.67 (2.51, 5.36); P<0.01 | 2.32 (1.51, 3.55); P<0.01 | 0.33 (−1.13, 1.79); P=0.33 | 0.81 (0.52, 1.28); P=0.38 | |
| ORs (95% CI) for minor sidewalk problems within strata of activity limitationse | 1.18 (1.01, 1.38); P=0.04 | 1.05 (0.77, 1.43); P=0.78 | ||||||
| ORs (95% CI) for somewhat serious sidewalk problems within strata of activity limitationse | 1.49 (1.21, 1.84); P<0.01 | 1.11 (0.75, 1.64); P=0.61 | ||||||
| ORs (95% CI) for very serious sidewalk problems within strata of activity limitationse | 1.72 (1.41, 2.10); P<0.01 | 1.36 (0.91, 2.04); P=0.14 | ||||||
Note: OR = Odds Ratio; CI = Confidence Interval; RERI = Relative Excess Risk due to Interaction; All odds ratios presented in this table are adjusted for age, race, gender, individual income, individual education, mobility aid use (Model 6); Table presentation is following the recommendations from Knol and VanderWeele (2012).
Y=1 represents the number of participants reporting going into the neighborhood less than one time per week, Y=0 represents the number of participants reporting going into the neighborhood one to seven times per week
Odds ratios obtained from separate, stratified models among participants reporting severity of sidewalk problems as: not really a problem (N= 5,653), minor problem (N=2,363), somewhat serious problem (N=959), very serious problem (N=888). Adjusted odds ratios of the relationship between activity limitations and going into the neighborhood less than one time per week compared to one to seven times per week reported above.
Relative Excess Risk due to Interaction (RERI) represents the differences in differences in odds ratios. RERI can be more precisely written as: OR11- (OR10+OR01-1), OR12- (OR10+OR02-1), OR13- (OR10+OR03-1) for minor, somewhat serious, and very serious sidewalk problems, respectively. Where activity limitations = i (0 = no activity limitations, 1 = any activity limitations) and sidewalk problems = j (0 = Not really a problem, 1 = Minor problem, 2 = Somewhat serious problem, 3 = Very serious problem) for all ORij.
Ratio of Odds Ratios can be written as: OR11/(OR10×OR01), OR12/(OR10×OR02), OR13/(OR10×OR03) for minor, somewhat serious, and very serious sidewalk problems, respectively. Where activity limitations = i (0 = no activity limitations, 1 = any activity limitations) and sidewalk problems = j (0 = Not really a problem, 1 = Minor problem, 2 = Somewhat serious problem, 3 = Very serious problem) for all ORij.
Odds ratio obtained from separate, stratified models among participants reporting the number of activity limitations: none (N= 8,727), any (N= 1,136). Adjusted odds ratios of the relationship between severity of sidewalk problems and going into the neighborhood less than one time per week compared to one to seven times per week reported above.
The results of Model 7 and stratified models are presented within Table 4. Odds ratios and 95% confidence intervals for going into the neighborhood less than one time per week are presented for ever using a mobility aid in the neighborhood with no sidewalk problems (OR: 1.34; 95% CI: 1.09, 1.65), minor sidewalk problems (OR: 1.45; 95% CI: 1.09, 1.94), somewhat serious sidewalk problems (OR: 1.47; 95% CI: 0.99, 2.19), and very serious problems (OR: 1.50; 1.01, 2.23), where those who never use a mobility aid and no sidewalk problems is the reference category. Odds ratios and 95% confidence intervals for going into the neighborhood less than one time per week when never using a mobility aid in the neighborhood with minor sidewalk problems (OR: 1.17; 95% CI: 1.00, 1.37), somewhat serious sidewalk problems (OR: 1.50; 95% CI: 1.22, 1.84), and very serious sidewalk problems (OR: 1.80; 95% CI: 1.48, 2.20), where those with no activity limitations and no sidewalk problems treated as the reference category. Similar to results displayed in Table 3, the RERI and ratio of odds ratios provide little evidence of interaction between mobility aid use and severity of sidewalk problems on the additive scale. The ratio of odds ratios for very serious sidewalk problems (Ratio ORs: 0.62; 95% CI: 0.39, 0.99) was less than 0, meaning that there is some indication that the joint relationship between mobility aid use and very serious sidewalk problems is less than the product of the individual relationships alone.
Table 4.
Evaluation of additive and multiplicative interaction between severity of sidewalk problems and mobility aid use on the likelihood of going into the neighborhood less than one time per week compared to the likelihood of going into the neighborhood one to seven times per week.
| Mobility aid use | ORs (95% CI) for mobility aid use within strata of sidewalk problemsb | Measure of interaction on additive scale: RERI (95% CI)c | Measure of interaction on multiplicative scale: Ratio of ORs (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|
| Never | Ever | |||||||
| N Y=1/Y=0a |
OR (95% CI) | N Y=1/Y=0a |
OR (95% CI) | |||||
| Severity of Sidewalk Problems | Not really a problem | 595/4355 | 1.00 | 182/521 | 1.34 (1.09, 1.65); P<0.01 | 1.29 (1.04, 1.61); P=0.02 | ||
| Minor problem | 285/1770 | 1.17 (1.00, 1.37); P=0.05 | 78/230 | 1.45 (1.09, 1.94); P=0.01 | 1.25 (0.91, 1.73); P=0.17 | −0.06 (−0.55, 0.43); P=0.59 | 0.93 (0.65, 1.32); P=0.67 | |
| Somewhat serious problem | 150/666 | 1.50 (1.22, 1.84); P<0.01 | 40/103 | 1.47 (0.99, 2.19); P=0.06 | 0.95 (0.60, 1.52); P=0.84 | −0.36 (−1.04, 0.31); P=0.85 | 0.73 (0.46, 1.17); P=0.19 | |
| Very serious problem | 173/573 | 1.80 (1.48, 2.20); P<0.01 | 40/102 | 1.50 (1.01, 2.23); P=0.05 | 0.94 (0.60, 1.48); P=0.79 | −0.65 (−1.36, 0.07); P=0.96 | 0.62 (0.39, 0.99); P=0.04 | |
| ORs (95% CI) for minor sidewalk problems within strata of mobility aid usee | 1.17 (1.00, 1.37); P=0.05 | 1.03 (0.75, 1.42); P=0.84 | ||||||
| ORs (95% CI) for somewhat serious sidewalk problems within strata of mobility aid usee | 1.48 (1.21, 1.82); P<0.01 | 1.10 (0.73, 1.66); P=0.66 | ||||||
| ORs (95% CI) for very serious sidewalk problems within strata of mobility aid usee | 1.77 (1.45, 2.16); P<0.01 | 1.15 (0.76, 1.74); P=0.52 | ||||||
Note: OR = Odds Ratio; CI = Confidence Interval; RERI = Relative Excess Risk due to Interaction; All odds ratios presented in this table are adjusted for age, race, gender, individual income, individual education, mobility aid use (Model 7); Table presentation is following the recommendations from Knol and VanderWeele (2012).
Y=1 represents the number of participants reporting going into the neighborhood less than one time per week, Y=0 represents the number of participants reporting going into the neighborhood one to seven times per week
Odds ratios obtained from separate, stratified models among participants reporting severity of sidewalk problems as: not really a problem (N= 5,653), minor problem (N=2,363), somewhat serious problem (N=959), very serious problem (N=888). Adjusted odds ratios of the relationship between mobility aid use and going into the neighborhood less than one time per week compared to one to seven times per week reported above.
Relative Excess Risk due to Interaction (RERI) represents the differences in differences in odds ratios. RERI can be more precisely written as: OR11-(OR10+OR01-1), OR12-(OR10+OR02-1), OR13-(OR10+OR03-1) for minor, somewhat serious, and very serious sidewalk problems, respectively. Where mobility aid use = i (0 = never using mobility aid, 1 = ever using mobility aid) and sidewalk problems = j (0 = Not really a problem, 1 = Minor problem, 2 = Somewhat serious problem, 3 = Very serious problem) for all ORij.
Ratio of Odds Ratios can be written as: OR11/(OR10×OR01), OR12/(OR10×OR02), OR13/(OR10×OR03) for minor, somewhat serious, and very serious sidewalk problems, respectively. Where mobility aid use = i (0 = never using mobility aid, 1 = ever using mobility aid) and sidewalk problems = j (0 = Not really a problem, 1 = Minor problem, 2 = Somewhat serious problem, 3 = Very serious problem) for all ORij.
Odds ratio obtained from separate, stratified models among participants reporting mobility aid use: never (N= 8,567), ever (N= 1,296). Adjusted odds ratios of the relationship between severity of sidewalk problems and going into the neighborhood less than one time per week compared to one to seven times per week reported above.
Discussion
Our study found a significant association between perceived severity of sidewalk problems and outdoor neighborhood participation, independent of individual demographic, socioeconomic, and impairment characteristics. We also observed that increased age, self-identifying as Black, self-identifying as female, lower education, and lower income were associated with decreased neighborhood participation. In addition, activity limitations and the use of mobility aids were associated with decreased neighborhood participation. We did not observe significant interactions between perceived sidewalk problems and activity limitations on the additive or multiplicative scales. However, there was evidence to suggest an interaction between sidewalk problems and mobility aid use on the multiplicative scale. We found that mobility aid use in neighborhood environments with very serious sidewalk problems was associated with lower likelihood of going into the neighborhood less than one time per week. Mobility aid use appeared to be a protective factor of low levels of neighborhood participation when there were problems with neighborhood sidewalks.
We had hypothesized that participants who self-reported activity limitations and those using mobility aids would be more vulnerable to barriers in the outdoor built environment. Given findings of previous research we expected perceived sidewalk problems to be associated with less frequent neighborhood participation, particularly in those with underlying limitations in mobility function (P. J. Clarke et al., 2019).We did not observe interactions between severity of sidewalk problems and activity limitations. This might be because other environmental barriers preclude participants from ever encountering their neighborhood sidewalks. For example, if a wheelchair user has a step entrance into their home they may not be able to accurately rate the condition of their neighborhood sidewalks because the barrier of steps into their home are so restrictive that they do not encounter the outdoor space and subsequent sidewalk problems (S. C. Brown et al., 2008). Thus, sidewalk problems appear to be detrimental to neighborhood participation regardless of one’s underlying functional capacity While we did observe differences in the significance of relationships between severity of sidewalk problems and going into the neighborhood environment between strata of activity limitations, the direction and dose-response relationship was similar. Among those reporting no activity limitations we see a dose-response relationship, where increasing severity of sidewalk problems is associated with significantly higher odds of going into the neighborhood environment less than one time per week. We observe a similar dose-response relationship among participants reporting any activity limitations, however these relationships were non-significant. Our observed difference in significance between strata is likely driven by large differences in sample size between the two groups.
We did observe a negative interaction between very serious sidewalk problems and mobility aid use. It is possible that participants going into the neighborhood using a mobility aid are more aware of poor sidewalk conditions within their neighborhood and use the severity of sidewalk problems scale differently than those who do not use a mobility aid (Skantz et al., 2020). Furthermore, mobility aid users may have already adopted modifications to successfully overcome obstacles within their outdoor environment and rate challenges differently. In a recent study, authors found that when older adults engaged in adaptive walking modifications, such as using a mobility device, age related declines in autonomy and life-space were delayed (Skantz et al., 2020). Therefore, participants using mobility aids may have knowledge, skills, and expertise to successfully overcome environmental obstacles in their neighborhood.
This study adds to the current literature by examining the association between severity of sidewalk problems and neighborhood participation in a national United States sample of older adults. The findings of the current project agree with previous research conducted in the Chicago Community Adult Health Study, concluding that sidewalk quality is associated with neighborhood participation. Despite the fact that the current study utilized self-perceived sidewalk problems and the Chicago Community Adult Health Study used objective audit measures, both projects came to the same conclusion. Given both of these samples were taken from a United States population this may explain why we observe similar results. These findings are in conflict with findings from Etman et al. (2016), where researchers found that functional features were not associated with self-reported difficulty in activities of daily living or outdoor active transport (i.e. walking or cycling for transport) among older adults 65 years and older, after controlling for age and sex (Etman et al., 2016). Cultural differences between the Netherlands and the United States may in part explain the differences observed between these two projects. In addition, Etman et al. (2016) used a composite measure of neighborhood functional features (e.g. benches, waste bins), which may have diluted the true association between sidewalk characteristics and neighborhood participation. Future research is needed to fully understand the role of sidewalks on neighborhood participation. There is a need to validate these findings in other populations and examine the association between objectively measured built environment features with neighborhood participation among older adults.
Aging in place represents people maintaining residence in their home and community irrespective of age, income, or disability (Center for Disease Control and Prevention, 2009). Aging in place benefits both society and individuals. Maintaining home residence reduces individual cost, preserves social connections, increases personal independence, and people benefit from the familiarity with surroundings. For these and other reasons, it is not surprising that 90% of people aged 65 years and older wish to reside in their own homes for as long as possible (Burton, Mitchell, & Stride, 2011). One factor that may impact the quality of aging in place are the sidewalks directly outside of a person’s home. As people grow older, the neighborhood sidewalk may provide a critical connection to the outside world. Sidewalks may serve as the artery that allows for engagement in the community, and when sidewalks are absent, inhospitable, or uninviting this could cut off a main conduit between the individual and society. This study found that sidewalk problems were associated with older adult’s neighborhood participation, and sidewalk problems may serve as a physical barrier that restricts continued neighborhood participation. Sidewalks may not only restrict the individual themselves, but also restrict opportunities for society to benefit from older adults’ knowledge, experience, and insight. Safe, accessible sidewalks are needed to create inclusive environments for our aging population. The development of community infrastructure requires involvement from a diverse set of actors, including older adults and people with disabilities. Leveraging insights and opinions from community members will lead to sustainable neighborhood development that meets the needs of the population (Buffel, Phillipson, & Scharf, 2012).
Strengths and Limitations
There are several strengths and limitations that should be considered when interpreting the findings of this empirical study. Strengths to this investigation is the use of a large dataset of older adults throughout the United States. This sample was diverse in demographic, socioeconomic, and geographic characteristics allowing for greater external validity and generalizability to Black and White older adults within the United States. However, this project had notable limitations. This study was cross sectional in nature, therefore we cannot determine temporality of the exposure or outcome variables. However, this project contributes to our current understanding of the person-environment interactions among older adults in the United States, and highlights the critical role of sidewalk problems for neighborhood participation. Participants self-reported both exposure and outcome variables, therefore our measurement of these variables is subject to same source bias where those with lowest participation in the neighborhood may not be able to accurately identify the severity of problems with their neighborhood sidewalks because they encounter them more infrequently. It is possible that participants using mobility aids are more aware of poor sidewalk conditions within their neighborhood and use the severity of sidewalk problems scale differently than participants who do not use a mobility aids, which would lead to bias in the measurement of our main exposure. There is the possibility that we were unable to take into consideration unmeasured confounders that obscure the true relationship between individual and environmental characteristics and neighborhood participation that were not included in our analysis. Lastly, activity limitations and mobility aid use were used as proxy indicators of underlying function due to lack of information on participants’ lower extremity function or capacity within the project.
Conclusions
These study findings support previous research concluding that sidewalks are an important built environment feature relevant for participation among older adults. It is critical for communities to ensure that there is equitable access to services, goods, and social events happening within the neighborhood environment. Not only do sidewalks provide a medium through which community members can traverse from one place to another, but they also provide opportunity for social interaction among citizens. These interactions can cultivate a more cohesive environment where members of the community know and watch out for one another to keep their community safe. This project found that adverse consequences of sidewalk problems did not interact with activity limitations to restrict neighborhood participation. Therefore, sidewalk problems seemed to be detrimental to older adults neighborhood participation, regardless of underlying activity limitations. The presence of, and quality of neighborhood sidewalks are an essential component to foster healthy aging in cities and communities for our aging population. Future research should investigate the association between sidewalks and participation utilizing longitudinal data sources.
Acknowledgments
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NINDS or the NIA. Representatives of the NINDS were involved in the review of the manuscript but were not directly involved in the collection, management, analysis, or interpretation of the data. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org. Representatives from NINDS did not have any role in the design and conduct of the study, the collection, management, analysis, and interpretation of the data, or the preparation or approval of the manuscript.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research project was supported by cooperative agreement U01 NS041588 co-funded by the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institute on Aging (NIA), National Institutes of Health, and Department of Health and Human Service. Additional funding was provided by investigator initiated grant (R01 NS092706, Natalie Colabianchi and Suzanne Judd, MPIs). Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (F31 HD098870, Twardzik, PI).
Footnotes
Declaration of Conflicting Interests
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article
REFERENCES
- Baker PS, Bodner EV, & Allman RM (2003). Measuring life-space mobility in community-dwelling older adults. J Am Geriatr Soc, 51(11), 1610–1614. [DOI] [PubMed] [Google Scholar]
- Baltes MM, Maas I, Wilms H-U, Borchelt M, & Little TD (1999). Everyday competence in old and very old age: Theoretical considerations and empirical findings. The Berlin aging study: Aging from, 70, 384–402. [Google Scholar]
- Barnett DW, Barnett A, Nathan A, Van Cauwenberg J, & Cerin E (2017). Built environmental correlates of older adults’ total physical activity and walking: a systematic review and meta-analysis. Int J Behav Nutr Phys Act, 14(1), 103. doi: 10.1186/s12966-017-0558-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner AB, & Clarke PJ (2018). Understanding Socioenvironmental Contributors to Racial and Ethnic Disparities in Disability Among Older Americans. Res Aging, 40(2), 103–130. doi: 10.1177/0164027516681165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CJ, Roth DL, Allman RM, Sawyer P, Ritchie CS, & Roseman JM (2009). Trajectories of life-space mobility after hospitalization. Ann Intern Med, 150(6), 372–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SC, Mason CA, Perrino T, Lombard JL, Martinez F, Plater-Zyberk E, … Szapocznik J. (2008). Built environment and physical functioning in Hispanic elders: the role of “eyes on the street”. Environ Health Perspect, 116(10), 1300–1307. doi: 10.1289/ehp.11160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buffel T, Phillipson C, & Scharf T (2012). Ageing in urban environments: Developing ‘age-friendly’cities. Critical Social Policy, 32(4), 597–617. [Google Scholar]
- Carp FM (1967). The impact of environment on old people. The Gerontologist, 7(2_Part_1), 106–108. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention. (2009). Healthy Places Terminology. Healthy Places. Retrieved from https://www.cdc.gov/healthyplaces/terminology.htm [Google Scholar]
- Cerin E, Nathan A, van Cauwenberg J, Barnett DW, & Barnett A (2017). The neighbourhood physical environment and active travel in older adults: a systematic review and meta-analysis. Int J Behav Nutr Phys Act, 14(1), 15. doi: 10.1186/s12966-017-0471-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P, Ailshire JA, Bader M, Morenoff JD, & House JS (2008). Mobility disability and the urban built environment. Am J Epidemiol, 168(5), 506–513. doi: 10.1093/aje/kwn185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke PJ, Ailshire JA, Nieuwenhuijsen ER, & de Kleijn-de Vrankrijker MW (2011). Participation among adults with disability: the role of the urban environment. Soc Sci Med, 72(10), 1674–1684. doi: 10.1016/j.socscimed.2011.03.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke PJ, Twardzik E, Meade MA, Peterson MD, & Tate D (2019). Social Participation Among Adults Aging With Long-Term Physical Disability: The Role of Socioenvironmental Factors. J Aging Health, 31(10_suppl), 145S–168S. doi: 10.1177/0898264318822238 [DOI] [PubMed] [Google Scholar]
- Etman A, Kamphuis CB, Pierik FH, Burdorf A, & Van Lenthe FJ (2016). Residential area characteristics and disabilities among Dutch community-dwelling older adults. Int J Health Geogr, 15(1), 42. doi: 10.1186/s12942-016-0070-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira FR, Cesar CC, Camargos VP, Lima-Costa MF, & Proietti FA (2010). Aging and Urbanization: The Neighborhood Perception and Functional Performance of Elderly Persons in Belo Horizonte Metropolitan Area-Brazil. J Urban Health, 87(1), 54–66. doi: 10.1007/s11524-009-9406-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay J, Franke T, McKay H, & Sims-Gould J (2015). Therapeutic landscapes and wellbeing in later life: Impacts of blue and green spaces for older adults. Health & place, 34, 97–106. [DOI] [PubMed] [Google Scholar]
- Ganguli M, Fox A, Gilby J, & Belle S (1996). Characteristics of rural homebound older adults: a community‐based study. J Am Geriatr Soc, 44(4), 363–370. [DOI] [PubMed] [Google Scholar]
- Gottlieb ER, Smith EC, Wolfenden LL, Allman RM, & Tangpricha V (2011). Life-space mobility is associated with frequency of hospitalization in adults with cystic fibrosis. Clin Respir J, 5(4), 245–251. doi: 10.1111/j.1752-699X.2010.00225.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosmer DW, & Lemeshow S (1992). Confidence interval estimation of interaction. Epidemiology, 452–456. [DOI] [PubMed] [Google Scholar]
- Howard G, McClure LA, Moy CS, Howard VJ, Judd SE, Yuan Y, … Kleindorfer DO. (2017). Self-reported stroke risk stratification: reasons for geographic and racial differences in stroke study. Stroke, 48(7), 1737–1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, … Howard G. (2005). The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology, 25(3), 135–143. doi: 10.1159/000086678 [DOI] [PubMed] [Google Scholar]
- Katz S, Downs TD, Cash HR, & Grotz RC (1970). Progress in development of the index of ADL. The Gerontologist, 10(1_Part_1), 20–30. [DOI] [PubMed] [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, & Jaffe MW (1963). Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. Jama, 185(12), 914–919. [DOI] [PubMed] [Google Scholar]
- Kerr J, Rosenberg D, & Frank L (2012). The role of the built environment in healthy aging: community design, physical activity, and health among older adults. Journal of Planning Literature, 27(1), 43–60. [Google Scholar]
- Keskinen KE, Rantakokko M, Suomi K, Rantanen T, & Portegijs E (2019). Environmental Features Associated With Older Adults’ Physical Activity in Different Types of Urban Neighborhoods. Journal of Aging and Physical Activity, 1(aop), 1–9. [DOI] [PubMed] [Google Scholar]
- Kim M, & Clarke P (2015). Urban social and built environments and trajectories of decline in social engagement in vulnerable elders: findings from Detroit’s Medicaid home and community-based waiver population. Res Aging, 37(4), 413–435. doi: 10.1177/0164027514540687 [DOI] [PubMed] [Google Scholar]
- Knol MJ, van der Tweel I, Grobbee DE, Numans ME, & Geerlings MI (2007). Estimating interaction on an additive scale between continuous determinants in a logistic regression model. International journal of epidemiology, 36(5), 1111–1118. [DOI] [PubMed] [Google Scholar]
- Knol MJ, & VanderWeele TJ (2012). Recommendations for presenting analyses of effect modification and interaction. International journal of epidemiology, 41(2), 514–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knol MJ, VanderWeele TJ, Groenwold RH, Klungel OH, Rovers MM, & Grobbee DE (2011). Estimating measures of interaction on an additive scale for preventive exposures. European journal of epidemiology, 26(6), 433–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kono A, & Kanagawa K (2001). Characteristics of housebound elderly by mobility level in Japan. Nursing & health sciences, 3(3), 105–111. [DOI] [PubMed] [Google Scholar]
- Lawton MP, & Nahemow L (1973). Ecology and the aging process.
- Long DL, Howard G, Long DM, Judd S, Manly JJ, McClure LA, … Glymour MM. (2019). An Investigation of Selection Bias in Estimating Racial Disparity in Stroke Risk Factors: The REGARDS Study. American journal of epidemiology, 188(3), 587–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynott J, Haase J, Nelson K, Taylor A, Twaddell H, Ulmer J, … Stollof ER. (2009). Planning complete streets for an aging America. Retrieved from
- Mackey DC, Cauley JA, Barrett-Connor E, Schousboe JT, Cawthon PM, & Cummings SR (2014). Life-space mobility and mortality in older men: a prospective cohort study. J Am Geriatr Soc, 62(7), 1288–1296. doi: 10.1111/jgs.12892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mefford MT, Tajeu GS, Tanner RM, Colantonio LD, Monda KL, Dent R, … Muntner P. (2018). Willingness to be Reinitiated on a Statin (from the REasons for Geographic and Racial Differences in Stroke Study). Am J Cardiol, 122(5), 768–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mowen A, Orsega-Smith E, Payne L, Ainsworth B, & Godbey G (2007). The role of park proximity and social support in shaping park visitation, physical activity, and perceived health among older adults. Journal of Physical Activity and Health, 4(2), 167–179. [DOI] [PubMed] [Google Scholar]
- Nahemow L, & Lawton MP (1973). Toward an ecological theory of adaptation and aging. Environmental design research, 1, 24–32. [Google Scholar]
- Naumann RB, Dellinger AM, Haileyesus T, & Ryan GW (2011). Older adult pedestrian injuries in the United States: causes and contributing circumstances. International journal of injury control and safety promotion, 18(1), 65–73. [DOI] [PubMed] [Google Scholar]
- Ng TP, Nyunt MSZ, Shuvo FK, Eng JY, Yap KB, Hee LM, … Scherer S. (2018). The Neighborhood Built Environment and Cognitive Function of Older Persons: Results from the Singapore Longitudinal Ageing Study. Gerontology, 64(2), 149–156. doi: 10.1159/000480080 [DOI] [PubMed] [Google Scholar]
- Peel C, Sawyer Baker P, Roth DL, Brown CJ, Brodner EV, & Allman RM (2005). Assessing mobility in older adults: the UAB Study of Aging Life-Space Assessment. Phys Ther, 85(10), 1008–1119. [PubMed] [Google Scholar]
- Richard L, Gauvin L, Gosselin C, & Laforest S (2008). Staying connected: neighbourhood correlates of social participation among older adults living in an urban environment in Montreal, Quebec. Health promotion international, 24(1), 46–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider KL, Clark MA, Rakowski W, & Lapane KL (2012). Evaluating the impact of non-response bias in the Behavioral Risk Factor Surveillance System (BRFSS). J Epidemiol Community Health, 66(4), 290–295. [DOI] [PubMed] [Google Scholar]
- Sheppard KD, Sawyer P, Ritchie CS, Allman RM, & Brown CJ (2013). Life-space mobility predicts nursing home admission over 6 years. J Aging Health, 25(6), 907–920. doi: 10.1177/0898264313497507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skantz H, Rantanen T, Palmberg L, Rantalainen T, Aartolahti E, Portegijs E, … Rantakokko M. (2020). Outdoor mobility and use of adaptive or maladaptive walking modifications among older people. The Journals of Gerontology: Series A, 75(4), 806–812. [DOI] [PubMed] [Google Scholar]
- Spring A (2018). Short- and Long-Term Impacts of Neighborhood Built Environment on Self-Rated Health of Older Adults. Gerontologist, 58(1), 36–46. doi: 10.1093/geront/gnx119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theis KA, & Furner SE (2011). Shut-In? Impact of Chronic Conditions on Community Participation Restriction among Older Adults. J Aging Res, 2011, 759158. doi: 10.4061/2011/759158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Cauwenberg J, Nathan A, Barnett A, Barnett DW, & Cerin E (2018). Relationships Between Neighbourhood Physical Environmental Attributes and Older Adults’ Leisure-Time Physical Activity: A Systematic Review and Meta-Analysis. Sports Med, 48(7), 1635–1660. doi: 10.1007/s40279-018-0917-1 [DOI] [PubMed] [Google Scholar]
- Vaughan M, LaValley MP, AlHeresh R, & Keysor JJ (2016). Which features of the environment impact community participation of older adults? A systematic review and meta-analysis. J Aging Health, 28(6), 957–978. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2002). Active ageing: A policy framework. Retrieved from


