Abstract
Introduction
The gut microbiota may be relevant in the development of type 1 diabetes (T1D). We examined the effects of Lactobacillus rhamnosus GG and Bifidobacterium lactis Bb12 on beta-cell function in children with newly diagnosed T1D.
Research design and methods
Children aged 8–17 years with newly (within 60 days) diagnosed T1D were enrolled in a double-blind, randomised controlled trial in which they received L. rhamnosus GG and B. lactis Bb12 at a dose of 109 colony-forming units or placebo, orally, once daily, for 6 months. The follow-up was for 12 months. The primary outcome measure was the area under the curve (AUC) of the C-peptide level during 2-hour responses to a mixed meal.
Results
Ninety-six children were randomised (probiotics, n=48; placebo n=48; median age 12.3 years). Eighty-eight (92%) completed the 6-month intervention, and 87 (91%) completed the follow-up at 12 months. There was no significant difference between the study groups for the AUC of the C-peptide level. For the secondary outcomes at 6 months, there were no differences between the study groups. At 12 months, with one exception, there also were no significant differences between the groups. Compared with the placebo group, there was a significantly increased number of subjects with thyroid autoimmunity in the probiotic group. However, at baseline, there was also a higher frequency of thyroid autoimmunity in the probiotic group. There were no cases of severe hypoglycemia or ketoacidosis in any of the groups. No adverse events related to the study products were reported.
Conclusions
L. rhamnosus GG and B. lactis Bb12, as administered in this study, had no significant effect in maintaining the residual pancreatic beta-cell function in children with newly diagnosed T1D. It remains unclear which probiotics, if any, alone or in combination, are potentially the most useful for management of T1D.
Trial registration number
Keywords: diabetes mellitus, type 1, inflammation, cytokines
Significance of this study.
What is already known about this subject?
Current studies suggest that the interaction between the gut microbiota and the immune system may be a major factor influencing type 1 diabetes (T1D) development.
A prospective cohort study showed a decreased risk of islet autoimmunity in children, with the HLA-DR3/4 genotype, supplemented with probiotics within 0–27 days after birth.
However, there are no data on the effects of probiotics in subjects with newly recognised T1D.
What are the new findings?
This double-blind randomised controlled trial indicates that administration of Lactobacillus rhamnosus GG and Bifidobacterium lactis Bb12 at a dose of 109 colony-forming units has no significant effect on preserving the residual pancreatic beta-cell function in children with newly diagnosed T1D.
The administration of L. rhamnosus GG and B. lactis Bb12 as dosed in this study was well tolerated with no adverse effects in children with T1D.
How might these results change the focus of research or clinical practice?
Unless the role of the gut microbiota would be questioned, it may be considered as a target for improving outcomes in subjects with T1D.
Further studies are needed to explore the effects of various gut microbiota modifications on islet cell autoimmunity.
This includes other probiotics, as their effects are largely strain specific.
Introduction
Type 1 diabetes (T1D) is an autoimmune disease that causes beta-cell destruction and insulin deficiency. The incidence of T1D is rising in many countries, including Poland.1 Both genetic predisposition and environmental factors influence the development of T1D. In children, the highest seroconversion to autoantibody positivity occurs during the first 3 years of life.2 However, individual differences in the duration of the prediabetes period are observed, ranging from a few months to >20 years, with the average duration of the prediabetic period between 2.5 and 3 years.3 Environmental factors, including disturbances in the gut microbiota, might play an important role as potential cause or contributing factor in the development of T1D.4
The gut microbiota in children stabilizes and reaches greater diversity and its adult-like composition at approximately 3 years of age. Commensal microbiota interact with the immune system during both eubiosis and dysbiosis. During dysbiosis (imbalances in the composition and function of the gut microbiota), some bacteria induce regulatory T (T-reg) cell differentiation and the secretion of anti-inflammatory cytokines, whereas other bacteria influence T helper type 17 (Th17) cell differentiation and the secretion of pro-inflammatory cytokines, contributing to some autoimmune diseases.5 In patients with T1D, an increased ratio of Bacteroidetes/Firmicutes has been found. Bacteroides species increase mucin degradation and lead to increased permeability of intestinal mucosa that increases antigen penetration and stimulation of the immune system. Additionally, a deficiency of short-chain fatty acid-producing bacteria affects modulation of T-reg cell differentiation and stimulates autoimmunization in islet autoantibody-positive cases6 and subjects with T1D.7 In subjects with T1D, a reduction in Lactobacillus and Bifidobacterium species was noted in fecal samples.8 Lactobacillus and Bifidobacterium species are the most common probiotics used to constitute intestinal microbial homeostasis, inhibit growth of pathogens and modulate local and systemic immune responses. Bifidobacterium species, due to promotion of carbohydrate fermentation and generation of acetate and lactate, enhance gut-barrier function and induce T-reg cell differentiation.9
Targeting the gut microbiome with probiotics, prebiotics or synbiotics could potentially reduce the risk of T1D or modulate its course.10 However, data remain limited. In animals, as reviewed in detail elsewhere,11 probiotics showed effects on a number of T1D-associated outcomes. However, the effects are likely to be strain specific. For example, oral transfer of Lactobacillus johnsonii N6.2 (LjN6.2) from Bio-Breeding diabetes-resistant rats to Bio-Breeding diabetes-prone rodents mediated resistance to the onset of T1D. In contrast, the administration of Lactobacillus reuteri, under the same conditions, failed to cause resistance to T1D.12 The inhibition of T1D in rats fed LjN6.2 correlated to a LjN6.2-mediated Th17 bias, represented by higher levels of IL-17A and IL-23R,13 indicating different effects of various probiotic bacteria on the immune system.
Human data on the effects of probiotics in subjects with T1D are also limited. However, early probiotic supplementation within 0–27 days after birth in children positive for the HLA-DR3/4 genotype was associated with a decreased risk of islet autoimmunity when compared with probiotic supplementation after 27 days or no probiotic supplementation (HR 0.66; 95% CI 0.46 to 0.94 for the group as a whole, and 0.40; 95% CI 0.21 to 0.74 for those who had the HLA-DR3/4 genotype).14
The aim of our study was to examine the effects of Lactobacillus rhamnosus GG and Bifidobacterium lactis Bb12 on beta-cell function in children with newly diagnosed T1D. In April 2020, L. rhamnosus was renamed to Lacticaseibacillus rhamnosus; however, the abbreviated form remained unchanged.15 Thus, hereafter, the term L. rhamnosus GG will be used throughout the manuscript. We hypothesised that gut microbiota modulation with the combination of these two probiotics may be used as a tool to modulate the immune system for preventing islet cell destruction. We also speculated that children who receive L. rhamnosus GG and B. lactis Bb12 at the recognition of T1D will have more preserved beta-cell function than children who receive placebo. Previously, it has been documented that both strains have potential properties that potentially counteract the development of immune diseases.16
Methods
The full protocol of this trial was published before the start of the study in BMJ Open.17 The guidelines from the Consolidated Standards of Reporting Trials statement were followed for reporting this study.18 The trial was registered prior to the inclusion of the first patient.
Study design and participants
This was a double-blind, randomised, placebo-controlled trial with allocation of 1:1. Children aged 8–17 years with newly (within 60 days) diagnosed T1D (as defined by the International Society for Paediatric and Adolescent Diabetes criteria), the presence of at least one positive autoantibody (autoantibodies to glutamic acid decarboxylase (anti-GAD), the tyrosine phosphatase-related insulinoma-associated 2 molecule (anti-IA-2) or islet cell cytoplasmic autoantibodies (ICA)), and a fasting C-peptide level ≥0.4 ng/mL were eligible for inclusion. Exclusion criteria included antibiotic treatment, use of probiotics or gastrointestinal infection (all within 2 weeks prior to enrolment) as well as chronic gastrointestinal diseases (eg, inflammatory bowel disease, celiac disease, food allergy) or immunodeficiency.
Intervention
If a diagnosis of T1D was made, the child was assessed for eligibility and written informed consent was obtained. All patients started functional insulin therapy (FIT) with continuous subcutaneous insulin infusion (CSII) or multiple daily injections.
Eligible children received a combination of two probiotics: L. rhamnosus GG (strain deposit number ATCC 53103) and B. lactis Bb12 (DSM 15954) at a dose of 109 colony-forming units (CFU) or placebo (maltodextrin). Both study products were administered orally, in capsules, once daily, for 6 months. All study participants were followed up every 3 months for up to 12 months after the start of the intervention.
In all children, at T1D diagnosis, a blood sample was obtained for the measurement of fasting C-peptide, anti-GAD, anti-IA-2 and ICA (analyzed by radiobinding assays). At the T1D recognition and at month 12, antithyroid peroxidase (anti-TPO), antithyroglobulin (anti-Tg), serum thyroid-stimulating hormone, free thyroxine and antitissue transglutaminase type 2 (anti-TG2) antibodies (analyzed by ELISA test) were assessed. Glycated hemoglobin (HbA1c) levels were measured by high-performance liquid chromatography at the T1D onset and at months 6 and 12. Serum concentrations of zonulin were measured by ELISA test (IDK Zonulin ELISA, REF K5601, Immunodiagnostik, Benheim, Germany) at months 6 and 12. The cytokines were analyzed using flow cytometry BD Cytometric Bead Array (CBA) Human Enhanced Sensitivity Kit (catalog no. 561523) and CBA Human Enhanced Sensitivity Flex Set for interleukin (IL)-2, IL-10, IL-1β, interferon-gamma (IFN-γ) and tumor necrosis factor-α (TNF-α) (Becton Dickinson, Heidelberg, Germany).
At study entry and at all study visits, all eligible children underwent a physical examination, including evaluation of anthropometric measurements (weight, height and body mass index (BMI)), and were stratified accordingly to Tanner developmental stage ≤3 or >3. All information regarding treatment modality (eg, pump, infusion) and antibiotic use were collected at these visits. The total daily insulin dose and basal insulin were downloaded from insulin pumps or were collected from patients’ diaries.
In our study, we used the mixed-meal tolerance test (MMTT) for measuring endogenous insulin production in blood samples.19 The MMTT was performed every 30 min for 2 hours after a mixed meal consumption at allocation and at months 6 and 12. For the MMTT, all eligible participants consumed (before 10:00 hours in the fasting state) a standard, mixed meal (liquid-meal BOOST test (6 mL/kg max 360 mL, Nestle, Vevey, Switzerland; 237 mL contains 41 g carbohydrates, 10 g protein, 4 g fat, energy value 240 kcal)).
Compliance was assessed by collecting empty packages. Participants receiving >75% of the recommended doses were considered as compliant.
Outcomes
The primary outcome measure was area under the curve (AUC) of the C-peptide level during 2-hour responses to a mixed meal.
The secondary outcome measures included fasting C-peptide concentration, insulin requirement (U/kg body mass), HbA1c, cytokines (IL-1β, IL-2, IL-10, TNF-α and IFN-γ), gut permeability (zonulin levels), anthropometric parameters (weight, height, BMI z-score), occurrence of other autoimmune diseases (eg, autoimmune thyroid disease, celiac disease), acute complications of T1D such as severe hypoglycemia or ketoacidosis and side effects.
Sample size
The study planned to detect a 50% increase in the (untransformed) 2-hour AUC of C-peptide values in MMTT at month 12 in the treated group relative to the placebo group.20 A normalizing transformation ln(x+1) for C-peptide AUC was used. To provide 85% power using a one-sided test at the confidence level of 0.05, with 1:1 randomization and assuming a drop-out rate of 10%, a sample size of 96 subjects was needed.
Randomization and blinding
Block randomisation, with a block size of 4, was done with a computer-generated random number list prepared by an investigator with no clinical involvement in the trial. The list was concealed from the clinicians enrolling patients and assessing outcomes, as well as from the parents and the person responsible for the statistical analysis until completion of the study. The study products were prepared in identical packages by the Chr. Hansen Holding, Denmark, an independent company not involved in the conduct of the trial. The study products were packaged and assigned consecutive numbers according to the randomisation list by independent personnel.
Data collection and management
All study participants were assigned a study identification number. Case report forms (CRFs) were completed on paper forms. Data were entered and stored in a password-protected electronic database. The original paper copies of CRFs and all study data were stored in a locker within the study site, accessible to the involved researchers only.
Statistical analysis
C-peptide AUC was calculated with the use of trapezoidal rule over the 120 min period based on the time points of 0, 30, 60, 90 and 120 min. Nominal variables are presented as n (% of total group) and continuous variables are presented as mean±SD or median (Q1; Q3, ie, 25th; 75th percentile), depending on data normality. Normality of distribution was verified with the Shapiro-Wilk test as well based on visual assessment of histograms. Non-normally distributed C-peptide AUC data were log-transformed with ln(x+1) formula and retested. Non-parametric analyses were then applied to C-peptide AUC, since data did not conform to a normal distribution after transformation. Continuous variables were compared with the use of independent samples t-test or Mann-Whitney U test, as appropriate. Dichotomous (nominal) variables were compared between the groups with χ2 test or Fisher’s exact test. Mean difference or median difference (MD) (for continuous variables) and relative risk (RR) (for nominal variables) between groups were calculated with 95% CI. Spearman’s correlation coefficient was used to assess correlations between C-peptide AUC and other parameters. All tests were two-tailed, and differences were considered significant at the level of p<0.05. Analyses were conducted in statistical software R, V.3.5.1 (http://cran.r-project.org). Additionally, for the primary outcome, we created a linear mixed model including all repeated measures (baseline, 6 months, 12 months) and patient as a random effect to assess the impact of probiotic administration on AUC.
Results
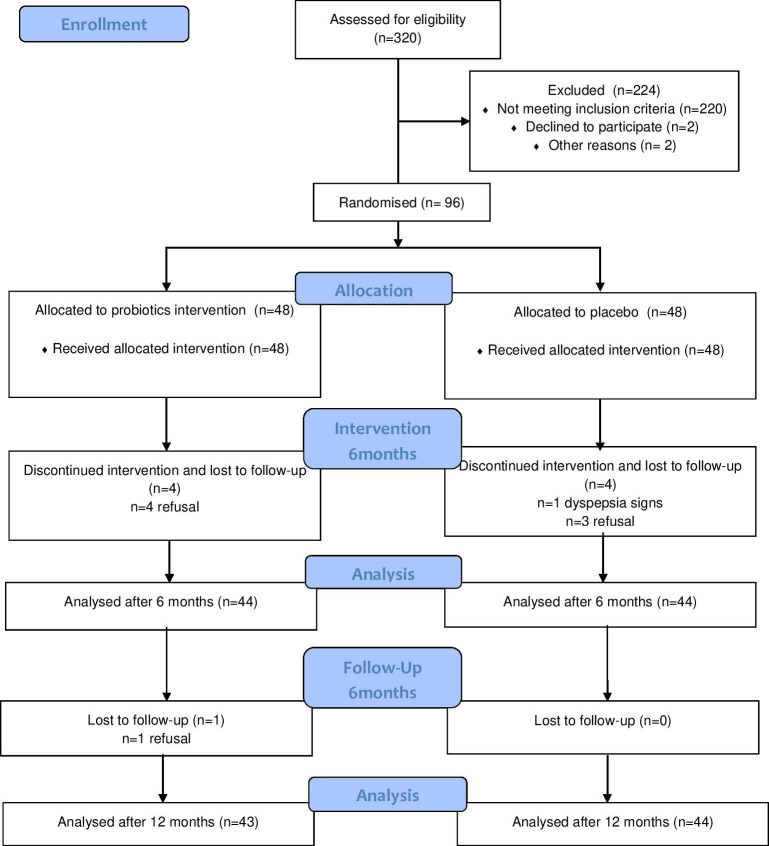
Participants were recruited among children with newly diagnosed T1D from the paediatric diabetes outpatient clinics at two participating centres in Warsaw, Poland (Department of Paediatrics, the Medical University of Warsaw and Department of Endocrinology and Diabetology, Children’s Memorial Health Institute) between July 2017 and January 2019. Of the 96 children who underwent randomisation, 48 were assigned to the probiotic group (L. rhamnosus GG and B. lactis Bb12) and 48 were assigned to the placebo group. A total of 88 (92%) completed the 6-month intervention, and 87 (91%) remained for analysis at 12 months. The flow diagram of the trial shows the subjects’ progression through the study (figure 1). Overall, eight children (four in each group) were lost to follow-up. There was no significant difference in the drop-out rates between the groups.
Figure 1.
Flow chart of subject participating in the study.
The characteristics of the children were similar between the groups at baseline, except for a higher number of children with thyroid autoimmunity determined by the presence of one of the thyroid antibodies (anti-Tg or anti-TPO) in the probiotic group (table 1).
Table 1.
Baseline characteristics
| Variable | Probiotics | Placebo |
| n | 48 | 48 |
| Female, n (%) | 23 (47.9) | 18 (37.5) |
| Age (years) | 12.31±2.13 | 13.17±2.59 |
| Height (SDS) | 0.62±1.01 | 0.64±1.02 |
| Height (cm) | 156.64±11.91 | 160.66±14.79 |
| Weight, SDS | 0.42±0.80 | 0.50±0.88 |
| Weight (kg) | 47.50±10.22 | 53.01±15.54 |
| BMI (SDS) | 0.20±0.84 | 0.24±1.02 |
| Time from diagnosis to recruitment, days (SD) | 40.4±16.2 | 29.65±19.6 |
| Tanner scale (4–5), n (%) | 12 (25.0) | 16 (33.3) |
| AUCCpep | 4.68 (3.55; 6.98) | 3.90 (2.93; 6.89) |
| C-peptide (ng/mL), median (Q1; Q3) | 1.03 (0.75; 1.37) | 0.97 (0.60; 1.54) |
| Insulin requirement (U/kg body mass) | 0.29±0.17 | 0.36±0.2 |
| Basal insulin (% of TDD), median (Q1; Q3) | 29.31 (17.80; 44.77) | 25 (16.44; 42.81) |
| HbA1c (%) | 7.8 (7.08; 8.30) | 8.10 (7.30; 9.70) |
| HbA1c (mmol/mol), median (Q1; Q3) | 65 (56; 83) | 62 (54; 67) |
| IL-1β (fg/mL), median (Q1; Q3) | 0.00 (0.00; 79.39) | 0.00 (0.00; 39.17) |
| IL-2 (fg/mL), median (Q1; Q3) | 0.00 (0.00; 0.88) | 0.00 (0.00; 0.00) |
| IL-10 (fg/mL), median (Q1; Q3) | 281.69 (99.04; 465.96) | 151.09 (73.27; 370.84) |
| IFN-γ (fg/mL), median (Q1; Q3) | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) |
| TNF-α (fg/mL), median (Q1; Q3) | 0.00 (0.00; 18.22) | 0.00 (0.00; 14.71) |
| GADA (IU/mL), median (Q1; Q3) | 7.16 (0.78; 48.05) | 5.81 (1.7; 24.03) |
| GADA positive, n (%) | 35 (72.9) | 38 (79.2) |
| IA2A (IU/mL), median (Q1; Q3) | 12.3 (1.11; 21.13) | 3.99 (0.8; 21.8) |
| IA2A positive, n (%) | 33 (68.8) | 30 (62.5) |
| ICA positive, n (%) | 45 (93.8) | 48 (100.0) |
| TSH | 2.08±0.95 | 2.22±1.22 |
| fT4 | 1.02±0.11 | 1.03±0.13 |
| Thyroid antibodies, n (%) | 20 (41.7) | 10 (20.8) |
| Celiac autoimmunity, n (%) | 0 (0.0) | 0 (0.0) |
AUC, area under the curve of the C-peptide during 2-hour responses to a mixed meal; BMI, body mass index; GADA, glutamic acid decarboxylase antibodies; HbA1c, glycated hemoglobin; IA2A, antityrosine phosphatase antibodies; ICA, islet cell antibodies; IFN-γ, interferon-gamma; IL, interleukin; SDS, SD scores; TDD, total daily insulin; TNF-α, tumor necrosis factor-α; TSH, thyroid-stimulating hormone.
The primary and secondary outcomes at month 6 (end of the intervention) and month 12 (end of a follow-up period) are presented in tables 2 and 3, respectively.
Table 2.
Primary and secondary outcomes at 6 months (end of intervention)
| N | Probiotics | N | Placebo | MD/RR (95% CI) | P value | |
| Primary outcome | ||||||
| AUCCpep | 44 | 3.38 (2.24; 4.52) | 44 | 3.30 (2.14; 4.56) | 0.08 (−0.80 to 0.78) | 0.993 |
| Secondary outcomes | ||||||
| C-peptide (ng/mL) | 44 | 0.89 (0.61; 1.15) | 44 | 0.94 (0.57; 1.17) | −0.05 (−0.18 to 0.20) | 0.832 |
| Insulin requirement (U/kg/day) | 44 | 0.36±0.23 | 44 | 0.39±0.25 | −0.03 (−0.13 to 0.08)* | 0.626† |
| HbA1c (%) | 45 | 6.20 (5.60; 6.60) | 45 | 6.50 (5.90; 7.05) | −0.30 (−0.60 to 0.00006) | 0.058 |
| HbA1c (mmol/mmol) | 44 (38; 49) | 49 (41; 54) | ||||
| IL-1β (fg/mL) | 44 | 0.00 (0.00; 8.02) | 43 | 0.00 (0.00; 26.45) | 0.00 (−0.00004 to 0.00004) | 0.241 |
| IL-2 (fg/mL) | 44 | 0.00 (0.00; 1.02) | 44 | 0.00 (0.00; 0.00) | 0.00 (−0.00007 to 0.00004) | 0.472 |
| IL-10 (fg/mL) | 45 | 222.86 (42.78; 323.11) | 45 | 159.06 (33.64; 295.69) | 63.80 (−41.38 to 87.44) | 0.470 |
| IFN-γ (fg/mL) | 45 | 0.00 (0.00; 0.00) | 45 | 0.00 (0.00; 0.00) | 0.00 (0.00 to 0.00) | n/a |
| TNF-α (fg/mL) | 44 | 0.00 (0.00; 5.66) | 42 | 0.00 (0.00; 18.79) | 0.00 (−0.00001 to 0.0001) | 0.594 |
| Zonulin (ng/mL) | 44 | 673.72 (537.71; 827.21) | 46 | 761.80 (634.79; 838.74) | −88.08 (−138.42 to 39.46) | 0.294 |
| BMI-SDS | 45 | 0.06±0.92 | 45 | 0.32±0.91 | −0.26 (−0.65 to 0.12)* | 0.178† |
| GADA (IU/mL) | 45 | 7.43 (0.94; 38.90) | 44 | 5.97 (1.16; 32.98) | 1.46 (−2.87 to 5.33) | 0.924 |
| GADA positive, n (%) | 45 | 33 (73.3) | 44 | 33 (75.0) | 0.98 (0.77 to 1.25)‡ | >0.999§ |
| IA2A (IU/mL) | 45 | 8.20 (1.92; 15.20) | 44 | 4.75 (0.80; 14.75) | 3.45 (−1.53 to 4.74) | 0.509 |
| IA2A positive, n (%) | 45 | 33 (75.0) | 44 | 27 (61.4) | 1.96 (0,89 to 1.60)‡ | 0.328§ |
| ICA positive, n (%) | 45 | 45 (100.0) | 44 | 44 (100.0) | n/a‡ | >0.999¶ |
Values are expressed as means±SD or median with lower and upper quartile (Q1; Q3), unless otherwise indicated.
P<0.05 was considered as significant.
*Mean between groups for continuous variables (depending on normality of data) calculated as probiotic group minus placebo group with 95% CI.
†Groups compared with t-test or with Mann-Whitney U test (remaining variables).
‡RR with 95% CI for nominal variables.
§Groups compared with χ2 test.
¶Groups compared with Fisher’s exact test (nominal variables).
AUCCpep, area under the curve of the C-peptide level during 2-hour responses to a mixed meal; BMI, body mass index; GADA, glutamic acid decarboxylase antibodies; HbA1c, glycated hemoglobin; IA2A, antityrosine phosphatase antibodies; ICA, islet cell antibodies; IFN-γ, interferon-gamma; IL, interleukin; MD, mean difference or median difference; n/a, not available; RR, relative risk; SDS, SD scores; TDD, total daily insulin dose; TNF-α, tumour necrosis factor-α.
Table 3.
Primary and secondary outcomes at 12 months (end of follow-up)
| N | Probiotics | N | Placebo | MD/RR (95% CI) | P value | |
| Primary outcome | ||||||
| AUCCpep | 43 | 1.87 (1.09; 2.64) | 44 | 2.56 (1.24; 4.17) | −0.69 (−1.30 to 0.22) | 0.205 |
| Secondary outcome | ||||||
| C-peptide (ng/mL) | 43 | 0.59 (0.34; 0.84) | 45 | 0.66 (0.30; 1.02) | −0.07 (−0.23 to 0.12) | 0.640 |
| Insulin requirement (U/kg/day) | 45 | 0.54±0.25 | 44 | 0.51±0.27 | 0.03 (−0.08 to 0.14)* | 0.619† |
| HbA1c (%) | 44 | 6.70 (6.20; 7.13) | 45 | 6.70 (6.10; 7.40) | 0.00 (−0.40 to 0.40) | 0.928 |
| HbA1c (mmol/mmol) | 50 (44; 54) | 50 (43; 57) | ||||
| IL-1β (fg/mL) | 45 | 0.00 (0.00; 34.57) | 44 | 0.00 (0.00; 53.92) | 0.00 (−0.00008 to 0.00002) | 0.693 |
| IL-2 (fg/mL) | 43 | 0.00 (0.00; 0.00) | 45 | 0.00 (0.00; 0.00) | 0.00 (−0.00002 to 0.00003) | 0.403 |
| IL-10 (fg/mL) | 44 | 203.60 (92.80; 407.62) | 46 | 196.11 (82.32; 339.98) | −7.49 (−52.69 to 104.22) | 0.521 |
| IFN-γ (fg/mL) | 44 | 0.00 (0.00; 0.00) | 46 | 0.00 (0.00; 0.00) | 0.00 (0.00 to 0.00) | 0.339 |
| TNF-α (fg/mL) | 43 | 0.00 (0.00; 8.81) | 43 | 0.00 (0.00; 4.75) | 0.00 (−0.00005 to 0.00001) | 0.774 |
| Zonulin (ng/mL) | 45 | 698.48 (638.90; 900.44) | 44 | 711.92 (612.65; 829.75) | −13.44 (−83.50 to 62.52) | 0.724 |
| BMI-SDS | 44 | 0.03±0.39 | 45 | 0.04±0.27 | −0.01 (−0.15 to 0.13)* | 0.869† |
| GADA (IU/mL) | 44 | 3.48 (0.75; 42.93) | 46 | 3.81 (0.90; 24.70) | −0.33 (−2.72 to 1.45) | 0.971 |
| GADA positive, n (%) | 44 | 30 (68.2) | 46 | 31 (67.4) | 1.01 (0.76 to 1.35)‡ | >0.999§ |
| IA2A (IU/mL) | 44 | 9.30 (1.10; 18.35) | 46 | 3.24 (0.80; 10.23) | 6.06 (−0.00003 to 7.11) | 0.079 |
| IA2A positive, n (%) | 44 | 31 (70.5) | 46 | 27 (58.7) | 1.20 (0.88 to 1.63)‡ | 0.345§ |
| ICA positive, n (%) | 44 | 44 (100.0) | 46 | 46 (100.0) | n/a‡ | >0.999¶ |
| TSH | 46 | 1.92±0.96 | 46 | 2.12±1.06 | −0.20 (−0.61 to 0.22)* | 0.352† |
| fT4 | 46 | 0.97±0.12 | 46 | 0.94±0.10 | 0.03 (−0.01 to 0.08)* | 0.150† |
| Thyroid Ab, n (%) | 46 | 15 (32.6) | 46 | 6 (13.0) | 2.50 (1.06 to 5.87)‡ | 0.047§ |
| Celiac disease autoimmunity, n (%) | 44 | 1 (2.3) | 46 | 0 (0.0) | n/a‡ | 0.489¶ |
Values are expressed as means±SD or median with lower and upper quartile (Q1; Q3), unless otherwise indicated.
P<0.05 was considered as significant.
*MD between groups for continuous variables (depending on normality of data) calculated as probiotic group minus placebo group with 95% CI.
†Groups compared with t-test or with Mann-Whitney U test (remaining variables).
‡RR with 95% CI for nominal variables.
§Groups compared with χ2 test.
¶Groups compared with Fisher’s exact test (nominal variables).
Ab, antibody; AUCCpep, area under the curve of the C-peptide level during 2-hour responses to a mixed meal; BMI, body mass index; GADA, glutamic acid decarboxylase antibodies; HbA1c, glycated hemoglobin; IA2A, antityrosine phosphatase antibodies; ICA, islet cell antibodies; IFN-γ, interferon-gamma; IL, interleukin; MD, mean difference or median difference; n/a, not available; RR, relative risk; SDS, SD scores; TNF-α, tumor necrosis factor-α; TSH, thyroid-stimulating hormone.
For the primary outcome, there was no significant difference between the study groups in the AUC of the C-peptide level (AUCCpep) during 2-hour responses to a mixed meal at any time point. As these data for the primary outcome (AUC) contained repeated measures, we also ran an analysis combining all measures together (a linear mixed model was used). The results of this analysis did not change the conclusions from the previous analysis: fixed effect for group variable (probiotic/control) had t=−0.761, p=0.448. Therefore, we cannot conclude that the probiotic effect on AUC was significant.
For the secondary outcomes at 3 and 6 months, there were no differences between the study groups. At 12 months, with one exception, there also were no significant differences between the groups. Compared with the placebo group, there was a significantly increased number of subjects with thyroid autoimmunity in the probiotic group (15/46 vs 6/46, respectively, RR 2.5, 95% CI 1.06 to 5.87; p=0.047).
Throughout the study period, there were no acute complications of T1D such as severe hypoglycemia or ketoacidosis in any of the groups. No adverse events were reported by the participants. Throughout the study, there were no significant differences between the study groups in cytokine or zonulin levels.
Post hoc, we additionally assessed changes (baseline vs 6 and 12 months, and 6 vs 12 months) for the following parameters: AUCCpep, insulin requirement, HbA1c, levels of cytokines and zonulin (only 6 vs 12 months change), BMI-SDS and antibodies such as GADA, IA2A and ICA (table 4). With few exceptions, there were no significant differences between the study groups. First, during the follow-up period (6 vs 12 months after the intervention), there was a significantly higher increase in the mean change in total insulin daily dose in the probiotic group compared with the placebo group (MD −0.11 U/kg/day, 95% CI −0.22 to −0.004, p=0.042). Second, the increase in mean change in HbA1c from 6 to 12 months was higher in the probiotic group compared with the placebo group (MD −0.50%, 95% CI −0.70 to −0.10, p=0.009). Third, during the intervention period (months 0–6), there was significantly higher reduction in the mean change in IL-1β in the probiotic group compared with the placebo group (MD 0.00 fg/mL, 95% CI 0.00001 to 3.23, p=0.032). Finally, there was significantly lower reduction in the mean change in IA2A from 6 to 12 months in the probiotic group compared with the placebo group (p=0.004), and lower decline in GADA in the probiotic groups at 6–12 months, although of borderline significance (p=0.051).
Table 4.
Post hoc analyses
| Variables | Probiotics | Placebo | MD (95% CI) | P value |
| AUCCpep | ||||
| AUCCpep (0–6 months change) | −1.46 (−2.91; 0.17) | −0.38 (−1.86; 0.41) | −1.08 (−1.74 to 0.43) | 0.174 |
| AUCCpep (6–12 months change) | 0.20 (−0.73; 1.06) | 0.35 (−0.19; 1.36) | −0.15 (−0.93 to 0.34) | 0.330 |
| AUCCpep (0–12 months change) | −3.10 (−3.74; 1.08) | −1.60 (−3.58; −0.53) | −1.50 (−1.77 to 0.45) | 0.254 |
| Insulin (U/kg/day) | ||||
| Insulin0–6 months change | 0.08±0.17 | 0.01±0.21 | 0.07 (−0.01 to 0.15)* | 0.091† |
| Insulin0–12 months change | 0.16±0.17 | 0.12±0.21 | 0.04 (−0.04 to 0.13)* | 0.291† |
| Insulin6–12 months change | 0.24±0.21 | 0.13±0.29 | 0.11 (0.004 to 0.22)* | 0.042† |
| HbA1c (%) | ||||
| HbA1c0–6 months change | −1.65 (−2.13; 0.68) | −1.40 (−2.60; −0.50) | −0.25 (−0.60 to 0.70) | 0.956 |
| HbA1c6–12 months change | 0.50 (0.10; 0.95) | 0.00 (0.35; 0.60) | 0.50 (0.10 to 0.70) | 0.009 |
| HbA1c0–12 months change | −1.05 (−1.88; 0.30) | −1.10 (−2.90; −0.20) | −0.05 (−0.40 to 1.00) | 0.396 |
| IL-1β (fg/mL) | ||||
| IL-1β0–6 months change | 0.00 (−15.67; 0.00) | 0.00 (0.00; 6.40) | 0.00 (−3.23 to −0.00001) | 0.032 |
| IL-1β6–12 months change | 0.00 (0.00; 0.00) | 0.00 (−6.40; 0.00) | 0.00 (−0.00001 to 3.01) | 0.355 |
| IL-1β0–12 months change | 0.00 (−34.86; 0.00) | 0.0 (−4.88; 0.00) | 0.00 (−2.68 to 0.00001) | 0.256 |
| IL-2 (fg/mL) | ||||
| IL-20–6 months change | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) | 0.00 (−0.00006 to 0.00004) | 0.302 |
| IL-26–12 months change | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) | 0.00 (−0.00005 to 0.00002) | 0.702 |
| IL-20–12 months change | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) | 0.00 (−0.00005 to 0.00004) | 0.951 |
| IL-10 (fg/mL) | ||||
| IL-100–6 months change | −51.82 (164.13; 26.37) | −26.87 (−126.09; 30.20) | −24.95 (−96.69 to 44.38) | 0.445 |
| IL-106–12 months change | 1.37 (−72.90; 129.76) | 7.01 (−40.51; 122.01) | −5.64 (−63.95 to 71.38) | 0.974 |
| IL-100–12 months change | −22.94 (−127.67; 62.53) | −20.15 (−164.32; 99.09) | −2.79 (−90.37 to 81.52) | 0.933 |
| IFN-γ (fg/mL) | ||||
| IFN-γ0–6 months change | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) | 0.00 (0.00 to 0.00) | 0.323 |
| IFN-γ6–12 months change | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) | 0.00 (0.00 to 0.00) | 0.339 |
| IFN-γ0–12 months change | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) | 0.00 (−0.0001 to 0.0001) | >0.999 |
| TNF-α (fg/mL) | ||||
| TNF-α0–6 months change | 0.00 (0.00; 0.15) | 0.00 (0.00; 3.26) | 0.00 (−0.00001 to 0.000001) | 0.845 |
| TNF-α6–12 months change | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) | 0.00 (−0.0001 to 0.00002) | 0.932 |
| TNF-α0–12 months change | 0.00 (0.00; 1.29) | 0.00 (0.00; 0.00) | 0.00 (−0.0001 to 2.57) | 0.383 |
| Zonulin (ng/mL) | ||||
| Zonulin6–12 months change | 59.72 (−23.12; 145.15) | 7.71 (−93.22; 71.59) | 52.01 (−7.00 to 128.62) | 0.079 |
| BMI-SDS | ||||
| BMI-SDS0–6 months change | −0.10±0.49 | 0.06±0.46 | −0.16 (−0.36 to 0.04)* | 0.119† |
| BMI-SDS6–12 months change | 0.09±0.89 | 0.33±0.97 | −0.24 (−0.63 to 0.15)* | 0.216† |
| BMI-SDS0–12 months change | −0.07±0.62 | 0.10±0.50 | −0.17 (−0.41 to 0.07)* | 0.153† |
| GADA (IU/mL) | ||||
| GADA0–6 months change | 0.00 (−2.88; 1.20) | 0.00 (−1.21; 1.56) | 0.00 (−2.24 to 0.85) | 0.591 |
| GADA6–12 months change | 0.00 (−1.50; 0.40) | −1.11 (−4.63; 0.00) | 1.11 (−0.0001 to 2.64) | 0.051 |
| GADA0–12 months change | −0.03 (−6.20; 0.24) | −0.31 (−2.65; 0.17) | 0.28 (−1.16 to 3.70) | 0.622 |
| IA2A (IU/mL) | ||||
| IA2A0–6 months change | 0.00 (−7.30; 1.60) | 0.00 (−5.15; 0.68) | 0.00 (−2.69 to 1.60) | 0.977 |
| IA2A 6–12 months change | 0.00 (−0.98; 1.35) | −0.50 (−3.40; 0.00) | 0.50 (0.15 to 3.20) | 0.004 |
| IA2A0–12 months change | −0.20 (−9.38; 1.67) | −0.23 (−6.83; 0.00) | 0.03 (−1.48 to 3.36) | 0.448 |
Values are expressed as means±SD or median with lower and upper quartile (Q1; Q3).
*MD between groups for continuous variables (depending on normality of data) calculated as probiotic group minus placebo group with 95% CI.
†Groups compared with t-test or with Mann-Whitney U test (remaining variables).
AUCCpep, area under the curve of the C-peptide level during 2-hour responses to a mixed meal; BMI, body mass index; GADA, glutamic acid decarboxylase antibodies; HbA1c, glycated hemoglobin; IA2A, antityrosine phosphatase antibodies; IFN-γ, interferon-gamma; IL, interleukin; MD, mean difference or median difference; SDS, SD scores; TDD, total daily insulin dose; TNF-α, tumor necrosis factor-α.
Discussion
Principal findings
The results of this double-blind, placebo-controlled, randomised trial indicate that L. rhamnosus GG and B. lactis Bb12, as administered in this study, have no significant effect in maintaining the residual pancreatic beta-cell function in children with newly diagnosed T1D. Throughout the study period, there was no significant difference between the study groups for the AUC of the C-peptide level during 2-hour responses to a mixed meal test. For the secondary outcomes at 6 months, there were no differences between the study groups. At 12 months, with one exception, there also were no significant differences between the groups. Compared with the placebo group, there was a significantly increased number of subjects with thyroid autoimmunity in the probiotic group. However, at baseline, there was also a higher frequency of thyroid autoimmunity in the probiotic group than the placebo group (20/48 vs 10/48, respectively). Throughout the study period, there were no acute complications of T1D such as severe hypoglycemia or ketoacidosis in any of the groups. There were also no significant differences between the study groups for cytokine or zonulin levels. No adverse events related to use of the study products were reported.
Of note are the HbA1c values. During the study period, in both groups, HbA1c values were in line with current Polish recommendations (HbA1c ≤6.5%),21 suggesting that glycemic control was comparable and appropriate. However, compared with the placebo group, HbA1c was lower in the probiotic group. Although the difference was of borderline statistical significance (p=0.058), our findings may suggest the potential of the studied probiotics for the management of T1D. However, the study was not powered for this outcome.
Further studies are warranted to explore the effects of probiotics on islet cell autoimmunity. Our post hoc analyses showed a significantly lower decline of IA2A and a borderline lower decline of GADA in the probiotic group compared with the placebo group between 6 and 12 months. Earlier studies indicate that antibody titers for GAD-65 are positively associated with the capacity of insulin secretion and that rapid increases in autoantibody titers strongly predict progression to overt diabetes.22 Post hoc analyses also showed that after the cessation of the intervention, in the probiotic group compared with the placebo group, the change in the insulin requirement was higher and the HbA1c change from 6 to 12 months was also higher. Overall, these findings may suggest that either probiotics should not be given or, if given, the administration should not be stopped.
Comparison with previous findings
To the best of our knowledge, this is the first randomised trial to assess the effects of any of the probiotics on beta-cell function in children with newly diagnosed T1D. However, the Environmental Determinants of Diabetes in the Young prospective, cohort study examined the association between early probiotic exposure and islet autoimmunity in children genetically at increased risk for T1D. This study found that early (ie, during the first 27 days of life) administration of probiotics (mainly Lactobacillus and Bifidobacterium, given either as a supplement or in infant formula supplemented with probiotics) may be associated with a reduced risk of islet autoimmunity, especially in children with the highest-risk human leukocyte antigen (HLA) genotype of DR3/4 (HR 0.4, 95% CI 0.21 to 0.74), but no reduction was seen in children with moderately higher-risk genotypes.14 We did not perform genetic tests; thus, the effects of genotypes in our study population remain unclear.
In addition to probiotics, synbiotics (which refers to a substance that combines both a probiotic and prebiotic) are used to modulate the gut microbiota. One recent randomized controlled trial in 44 Iranian children with T1D found that the supplementation with a synbiotic (Lactobacillus sporogenesis GBI-30 and fructooligosaccharides) for 8 weeks resulted in a significant decrease in the HbA1c and marginally significant decrease in fasting blood glucose.23
Strengths and limitations
The strengths of this study include adequate randomisation, allocation concealment and intention-to-treat analysis. Follow-up was adequate. Data were obtained from 92% of the enrolled participants. All of these features minimise the risk of biases. The potential limitations of the trial are the lack of microbiota testing and lack of genetic testing for predisposition to T1D.
The lack of an effect may be explained by several factors. First, factors related to the probiotics themselves, that is, the wrong selection of the probiotic strains. In our trial, we chose L. rhamnosus GG and B. lactis Bb12, two probiotics with documented clinical efficacy in other indications.24 However, documented efficacy in one condition does not guarantee efficacy in another condition. Second, the dose of the probiotics. We chose a daily dose of 109 CFU for 6 months. However, there were no clinical data to support this dosage, and our decision was based on the probiotic doses typically used and recommended by the manufacturer. Similarly, the duration of the intervention was chosen arbitrarily. A higher dose and/or longer administration may be needed to observe an effect. Third, the lack of an effect may be due to the insufficient colonization rate of L. rhamnosus GG and B. lactis Bb12, thus, an inability to exert their probiotic effects. However, colonization is not needed for probiotics to exert beneficial effects, as other mechanisms may be involved. Fourth, considering that probiotics are widely used in our setting, the lack of an effect also may be due to the unreported use of probiotics, particularly considering the long intervention period. Lastly, probiotics may not have a clinically significant effect on the course of T1D once it has already developed.
Conclusion and implications for practice
The results of this double-blind, placebo-controlled, randomised trial indicate that L. rhamnosus GG and B. lactis Bb12, as administered in this study, have no significant effect in maintaining the residual pancreatic beta-cell function in children with newly diagnosed T1D.
It remains to be established which probiotics, if any, alone or in combination, and at which doses, are potentially the most useful for management of T1D.
Acknowledgments
The authors would like to thank Chr. Hansen Holding, Denmark that provided probiotic and placebo product for the present study. The authors would also like to thank all the subjects who participated in this study.
Footnotes
Contributors: AS conceptualized the study. LG, AS and HS contributed to the initial protocol of the study. LG, MS, JŚ, MW-M, AO, AS-E, UD and AS were mainly responsible for data collection. LG and AS were mainly responsible for data analysis and data interpretation. LG assumed the main responsibility for writing the first draft of this manuscript. All authors contributed to (and agreed on) the final version. LG is a guarantor.
Funding: Nutricia Foundation (grant RG 5/2016) and the Polish Diabetes Association.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The study was approved by the Ethics Committee of the Medical University of Warsaw, KB/77/2014.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on reasonable request. All data relevant to the study are included in the article. All data pertaining to this work are stored in the Pediatric Hospital of Medical University of Warsaw.
References
- 1.Szalecki M, Wysocka-Mincewicz M, Ramotowska A, et al. Epidemiology of type 1 diabetes in Polish children: a multicentre cohort study. Diabetes Metab Res Rev 2018;34:dmrr.2962. 10.1002/dmrr.2962 [DOI] [PubMed] [Google Scholar]
- 2.Krischer JP, Lynch KF, Schatz DA, et al. The 6 year incidence of diabetes-associated autoantibodies in genetically at-risk children: the TEDDY study. Diabetologia 2015;58:980–7. 10.1007/s00125-015-3514-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knip M, Honkanen J. Modulation of type 1 diabetes risk by the intestinal microbiome. Curr Diab Rep 2017;17:105. 10.1007/s11892-017-0933-9 [DOI] [PubMed] [Google Scholar]
- 4.Siljander H, Honkanen J, Knip M. Microbiome and type 1 diabetes. EBioMedicine 2019;46:512–21. 10.1016/j.ebiom.2019.06.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Oliveira GLV, Leite AZ, Higuchi BS, et al. Intestinal dysbiosis and probiotic applications in autoimmune diseases. Immunology 2017;152:1–12. 10.1111/imm.12765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Goffau MC, Luopajärvi K, Knip M, et al. Fecal microbiota composition differs between children with β-cell autoimmunity and those without. Diabetes 2013;62:1238–44. 10.2337/db12-0526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Goffau MC, Fuentes S, van den Bogert B, et al. Aberrant gut microbiota composition at the onset of type 1 diabetes in young children. Diabetologia 2014;57:1569–77. 10.1007/s00125-014-3274-0 [DOI] [PubMed] [Google Scholar]
- 8.Murri M, Leiva I, Gomez-Zumaquero JM, et al. Gut microbiota in children with type 1 diabetes differs from that in healthy children: a case-control study. BMC Med 2013;11:46. 10.1186/1741-7015-11-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sales-Campos H, Soares SC, Oliveira CJF. An introduction of the role of probiotics in human infections and autoimmune diseases. Crit Rev Microbiol 2019;45:413–32. 10.1080/1040841X.2019.1621261 [DOI] [PubMed] [Google Scholar]
- 10.Jamshidi P, Hasanzadeh S, Tahvildari A, et al. Is there any association between gut microbiota and type 1 diabetes? A systematic review. Gut Pathog 2019;11:49. 10.1186/s13099-019-0332-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mishra SP, Wang S, Nagpal R, et al. Probiotics and prebiotics for the amelioration of type 1 diabetes: present and future perspectives. Microorganisms 2019;7:67. 10.3390/microorganisms7030067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Valladares R, Sankar D, Li N, et al. Lactobacillus johnsonii N6.2 mitigates the development of type 1 diabetes in BB-DP rats. PLoS One 2010;5:e10507. 10.1371/journal.pone.0010507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lau K, Benitez P, Ardissone A, et al. Inhibition of type 1 diabetes correlated to a Lactobacillus johnsonii N6.2-mediated Th17 bias. J Immunol 2011;186:3538–46. 10.4049/jimmunol.1001864 [DOI] [PubMed] [Google Scholar]
- 14.Uusitalo U, Liu X, Yang J, et al. Association of early exposure of probiotics and islet autoimmunity in the TEDDY study. JAMA Pediatr 2016;170:20–8. 10.1001/jamapediatrics.2015.2757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zheng J, Wittouck S, Salvetti E, et al. A taxonomic note on the genus Lactobacillus: Description of 23 novel genera, emended description of the genus Lactobacillus Beijerinck 1901, and union of Lactobacillaceae and Leuconostocaceae. Int J Syst Evol Microbiol 2020;70:2782–858. 10.1099/ijsem.0.004107 [DOI] [PubMed] [Google Scholar]
- 16.Liu Y, Alookaran JJ, Rhoads JM. Probiotics in Autoimmune and Inflammatory Disorders. Nutrients. 2018 Oct 18;10:1537. [DOI] [PMC free article] [PubMed]
- 17.Groele L, Szajewska H, Szypowska A. Effects of Lactobacillus rhamnosus GG and Bifidobacterium lactis Bb12 on beta-cell function in children with newly diagnosed type 1 diabetes: protocol of a randomised controlled trial. BMJ Open 2017;7:e017178. 10.1136/bmjopen-2017-017178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet 2001;357:1191–4. 10.1016/S0140-6736(00)04337-3 [DOI] [PubMed] [Google Scholar]
- 19.Greenbaum CJ, Mandrup-Poulsen T, McGee PF, et al. Mixed-meal tolerance test versus glucagon stimulation test for the assessment of beta-cell function in therapeutic trials in type 1 diabetes. Diabetes Care 2008;31:1966–71. 10.2337/dc07-2451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lachin JM, McGee PL, Greenbaum CJ, et al. Sample size requirements for studies of treatment effects on beta-cell function in newly diagnosed type 1 diabetes. PLoS One 2011;6:e26471. 10.1371/journal.pone.0026471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guidelines on the management of diabetic patients. A position of diabetes Poland. Clinical Diabetology 2019. [Google Scholar]
- 22.Yamamura S, Fukui T, Mori Y, et al. Circulating anti-glutamic acid decarboxylase-65 antibody titers are positively associated with the capacity of insulin secretion in acute-onset type 1 diabetes with short duration in a Japanese population. J Diabetes Investig 2019;10:1480–9. 10.1111/jdi.13052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zare Javid A, Aminzadeh M, Haghighi-Zadeh MH, et al. The effects of synbiotic supplementation on glycemic status, lipid profile, and biomarkers of oxidative stress in type 1 diabetic patients. A placebo-controlled, double-blind, randomized clinical trial. Diabetes Metab Syndr Obes 2020;13:607–17. 10.2147/DMSO.S238867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Szajewska H, Hojsak I. Health benefits of Lactobacillus rhamnosus GG and Bifidobacterium animalis subspecies lactis BB-12 in children. Postgrad Med 2020;132:441–51. 10.1080/00325481.2020.1731214 [DOI] [PubMed] [Google Scholar]