Abstract
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes coronavirus disease 2019 (Covid-19), has been a serious threat to global health. Previous work has focused primarily on hospitalized patients or on identifying risk factors for disease severity and mortality once the infection has taken place. We sought to leverage the ubiquity of smartphones and mobile applications to study risk factors for Covid-19 infection in a large, geographically heterogenous cohort.
Methods
We analyzed data obtained from the Covid-19 Citizen Science (CCS) Study, a worldwide, mobile application-based cohort. After employing forward selection to identify variables with p values < 0.1, multivariable logistic regression models were utilized to identify independent risk factors associated with prevalent SARS-CoV-2 infection.
Results
Among 36,041 participants in 113 countries and all 50 states in the US, 484 participants had prevalent SARS-CoV-2 infection. After multivariable adjustment, being a healthcare worker, living with at least one school-aged child, having pets at home, and having immunodeficiency were each associated with an increased odds of SARS-CoV-2. The association between pets and prevalent SARS-CoV-2 was driven by dog ownership. After adjustment for the same covariates, Asian or Pacific Islander race, receiving a flu shot within the past year, increased level of education, and smoking or vaping marijuana within the last 30 days were each associated with a lower odds of SARS-CoV-2.
Conclusion
We identified various characteristics and behaviors, many of which are potentially modifiable, associated with prevalent SARS-CoV-2 infection in a world-wide mobile application-based cohort.
Keywords: COVID-19, epidemiology, cohort study, digital health, mobile applications
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes coronavirus disease 2019 (Covid-19), has had a significant impact on communities across the globe. Identifying risk factors associated with Covid-19 may prove valuable to the delivery of targeted public health interventions, providing more personalized advice to high-risk patient populations, and better informing the global response to the pandemic. Participation among community members and organizations has played a key role during the Covid-19 pandemic,1 and identifying potentially modifiable risk factors that can support community-based interventions is vital for containment of the pandemic. Previous work has focused on hospitalized patients2 or on disease severity and mortality once infection has taken place.3 Furthermore, smartphone technology on its own, and as an extension of telemedicine, has had various applications during the Covid-19 pandemic.4 We therefore sought to leverage the ubiquity of smartphones and mobile applications to study risk factors for Covid-19 infection in a large, geographically heterogenous cohort.
Methods
We conducted a cross-sectional study using data obtained from the Covid-19 Citizen Science (CCS) Study, a worldwide, mobile application-based cohort (https://covid19.eurekaplatform.org). Surveys pertinent to the current analyses are included in the Supplemental Materials. Questions where “effect-cause” relationships could obscure inferred causal relationships with prevalent disease were excluded.
Prevalent SARS-CoV-2 infection was defined as a history of a positive polymerase chain reaction (PCR) test for active infection. Participants were initially screened in the baseline survey for a history of any positive test for infection. Given an affirmative response to that initial question, participants were asked to distinguish between a PCR test for active infection versus an antibody test for prior infection. Self-report was verified by documentation of test results (Supplemental Materials). We identified variables exhibiting p values < 0.1 for associations with prevalent disease after adjusting for age, sex, race/ethnicity and then employed forward selection in a multivariable logistic regression model, retaining variables with p values < 0.1. Statistical analyses were performed using Stata, version 16 (College Station, TX). Two-tailed p-values < 0.05 were considered statistically significant. The study was approved by the University of California, San Francisco Institutional Review Board. All participants provided informed electronic consent.
Results
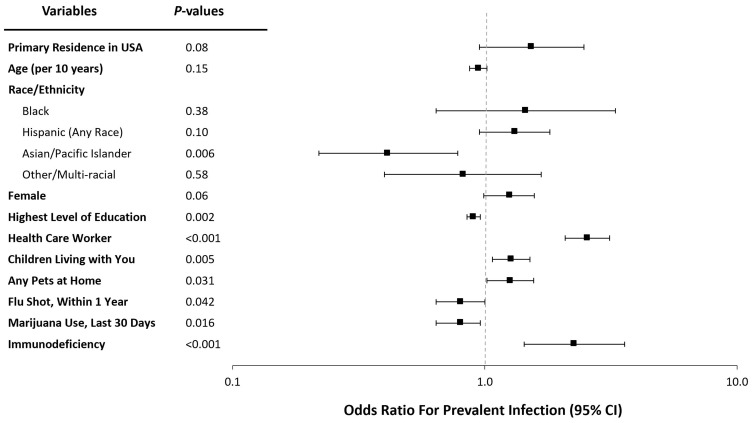
Among 36,041 participants in 113 countries and all 50 states in the US, 484 participants had prevalent SARS-CoV-2 infection (Supplemental Figure 1) (4297 participants had a negative test, and 31,260 participants were not tested). Baseline participant characteristics are shown in Table 1. After multivariable adjustment, being a healthcare worker, living with at least one school-aged child, having pets at home, and having immunodeficiency were each associated with an increased odds of SARS-CoV-2 (Figure 1). The association between pets and prevalent SARS-CoV-2 was driven by dog ownership (Supplemental Tables 1 and 2). After multivariable adjustment for the same covariates, Asian or Pacific Islander race, receiving a flu shot within the past year, increased level of education, and smoking or vaping marijuana within the last 30 days were each associated with a lower odds of SARS-CoV-2 (Figure 1).
Table 1.
Baseline Characteristics of Participants with and without a Positive SARS-CoV-2 Test for Active Infection
| Tested Positive N=484 |
Everyone Else (Tested Negative, Not Tested) N=35,557 |
p-value | |
|---|---|---|---|
| Primary Residence in USA | 461 (95.2%) | 32,989 (92.8%) | 0.033 |
| Median Age (IQR) | 42.0 (36.0–51.0)a | 43.0 (35.0–54.0)b | 0.17 |
| Female Biological Sex | 361 (75.8%) | 23,163 (65.1%) | <0.001 |
| Race/Ethnicity | <0.001 | ||
| White | 403 (84.7%) | 28,902 (81.3%) | |
| Black | 7 (1.5%) | 336 (0.9%) | |
| Hispanic (any race) | 47 (9.9%) | 2581 (7.3%) | |
| Asian or Pacific Islander | 10 (2.1%) | 1919 (5.4%) | |
| Other (including multiracial) | 9 (1.9%) | 813 (2.3%) | |
| Highest Level of Education | <0.001 | ||
| Less than high school | 3 (0.6%) | 164 (0.5%) | |
| High school graduate | 27 (5.7%) | 1356 (3.8%) | |
| College Graduate (including associate degree) | 268 (55.4%) | 17,552 (49.4%) | |
| Graduate school | 171 (35.3%) | 15,035 (42.3%) | |
| Other | 7 (1.4%) | 427 (1.2%) | |
| Healthcare worker | 181 (37.4%) | 7299 (20.5%) | <0.001 |
| Children living with you | 205 (42.4%) | 11,529 (32.4%) | <0.001 |
| Children home from college living with you | 40 (8.3%) | 2778 (7.8%) | 0.67 |
| Any pets at home | 357 (73.8%) | 22, 882 (64.4%) | <0.001 |
| Cigarettes: any use in last 30 days | 25 (5.4%) | 1906 (5.4%) | 0.92 |
| E-cigarettes: any use in last 30 days | 13 (2.8%) | 1041 (2.9%) | 0.89 |
| Marijuana: any use in last 30 days | 31 (6.8%) | 3300 (9.3%) | 0.027 |
| Atrial fibrillation | 7 (1.5%) | 952 (2.7%) | 0.09 |
| Anemia | 54 (11.4%) | 3512 (9.9%) | 0.36 |
| Asthma | 52 (11.0%) | 3482 (9.8%) | 0.49 |
| Cancer | 14 (3.0%) | 1023 (2.9%) | 1.00 |
| Coronary artery disease | 8 (1.7%) | 825 (2.2%) | 0.45 |
| Congestive heart failure | 3 (0.6%) | 220 (0.6%) | 1.00 |
| Chronic obstructive pulmonary disease | 10 (2.1%) | 569 (1.6%) | 0.46 |
| Diabetes | 18 (3.8%) | 1400 (3.9%) | 0.91 |
| High blood pressure | 86 (18.1%) | 6777 (19.1%) | 0.48 |
| Human immunodeficiency virus | 4 (0.8%) | 139 (0.4%) | 0.13 |
| Immunodeficiency | 20 (4.2%) | 701 (2.0.%) | 0.003 |
| Myocardial infarct | 3 (0.6%) | 340 (1.0%) | 0.64 |
| Pregnant | 10 (2.1%) | 306 (0.9%) | 0.011 |
| Sleep apnea | 45 (9.5%) | 3578 (10.1%) | 0.60 |
| Stroke | 5 (1.1%) | 433 (1.2%) | 1.00 |
| Received flu shot within the year | 352 (72.9%) | 26,258 (73.8%) | 0.64 |
Notes: aThe youngest and oldest ages of participants within the “Tested Positive” group was 18 years and 78 years, respectively. bThe youngest and oldest ages of participants within the “Everyone Else” group was 18 years and 91 years, respectively.
Figure 1.
Forest plot of adjusted odds ratios for participants with prevalent positive SARS-CoV-2 test results. Race/ethnicity categories were compared against non-Hispanic white participants. Y error bars indicate 95% confidence intervals.
Discussion
We identified characteristics associated with prevalent SARS-CoV-2 infection in a world-wide mobile application-based cohort. Our observation that healthcare workers experience a higher likelihood of infection has biological plausibility and fits with previous evidence.5 Although disease transmission has been described from children6 and may theoretically occur from pets,7 these data suggest that each may be an independent risk factor for infection. A higher risk among dog owners may arise from environmental exposures during dog-walking or fomite-based exposure from dog petting.
Although previous evidence demonstrates a higher risk of infection among black and LatinX individuals,8 here we found that Asians experience the lowest risk. A higher degree of education is commonly a protective factor against disease. The observation that recent marijuana smoking or vaping was associated with a lower risk was surprising—while it is possible this reflected “effect-cause” (for example, those feeling ill were less likely to use the drug), we did not find a similar association with e-cigarettes or smoking tobacco. While the flu vaccine would not be considered to confer cross-immunity with coronaviruses, the lower risk among those who received the flu shot could reflect more overall healthy behaviors or perhaps reflects a general immune system boost that renders individuals less prone to viral infection.
While a strength of the current study is that it was not constrained to individuals seeking medical care, we acknowledge that we cannot exclude residual or unmeasured confounding in this observational study and that our study population, all with smartphones, does not necessarily reflect the general population. We also relied on interpretation from participants regarding what constituted a personal history of immunodeficiency, where immunodeficiency represents a broad phenomenon, though we included separate survey questions assessing a history of more specific immunosuppressive conditions such as for diabetes and human immunodeficiency virus (HIV). There is also the possibility that those who smoke or vape marijuana may have been less likely to receive SARS-CoV-2 testing, which could have ultimately contributed to the observed inverse relationship between smoking or vaping marijuana and prevalent SARS-CoV-2 infections. Furthermore, the analyses treated participants who were not tested for SARS-CoV-2 infection as if they had not been infected and we acknowledge that there may have been participants in this group with prevalent infections that were therefore under-ascertained. We do not believe this would have led to spurious false-positive results, but on the contrary, this may have led to underestimating the strengths of our observed relationships.
Conclusion
In conclusion, we identified various characteristics and behaviors, many of which are potentially modifiable, that are associated with prevalent SARS-CoV-2 infection in a world-wide mobile application-based cohort. We believe that these findings will be broadly useful for targeted public health interventions in efforts to further contain the pandemic.
Funding Statement
This study was funded by grants IU2CEB021881-01 and 3U2CEB021881-05S1 from the National Institute of Biomedical Imaging and Bioengineering at the National Institutes of Health to Drs. Marcus, Olgin, and Pletcher. The sponsors had no role in study design, data collection, analysis, interpretation of the data, writing of the paper, or the decision to publish the paper.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Disclosure
Dr Mark J Pletcher reports grants from PCORI, NIH, and Bill and Melinda Gates Foundation, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
- 1.Sahu KK, Kumar R. Preventive and treatment strategies of COVID-19: from community to clinical trials. J Family Med Prim Care. 2020;9(5):2149–2157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cummings MJ, Baldwin MR, Abrams D, et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. 2020;395(10239):1763–1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Iyengar K, Upadhyaya GK, Vaishya R, Jain V. COVID-19 and applications of smartphone technology in the current pandemic. Diabetes Metab Syndr. 2020;14(5):733–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475–e483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park YJ, Choe YJ, Park O, et al. Contact tracing during coronavirus disease outbreak, South Korea, 2020. Emerg Infect Dis. 2020;26(10):2465–2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kiros M, Andualem H, Kiros T, et al. COVID-19 pandemic: current knowledge about the role of pets and other animals in disease transmission. Virol J. 2020;17(1):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vahidy FS, Nicolas JC, Meeks JR, et al. Racial and ethnic disparities in SARS-CoV-2 pandemic: analysis of a COVID-19 observational registry for a diverse US metropolitan population. BMJ Open. 2020;10(8):e039849. [DOI] [PMC free article] [PubMed] [Google Scholar]