Abstract
Background
Since consistent evidence on the effectiveness of acupuncture in the treatment of chronic obstructive pulmonary disease (COPD) is not available, this overview aims to summarize and critically evaluate the methodological and evidence quality of systematic reviews (SRs) on this topic.
Methods
Eight electronic databases were searched to identify relevant SRs of the use of acupuncture in the treatment of COPD from inception to January 2021. Two researchers independently screened the literature, extracted the data, and cross-checked the data. The Assessing the Methodological Quality of Systematic Reviews 2 (AMSTAR 2) list was used to assess the methodological quality of SRs. The Grades of Recommendations, Assessment, Development and Evaluation (GRADE) system was used to assess the quality of evidence for the outcomes of interest.
Results
Nine SRs that conducted quantitative syntheses were included in this overview. The methodological quality of the SRs and the quality of evidence for the main outcome measures were generally unsatisfactory. Only 2 SRs were rated as low methodological quality by AMSTAR 2, and the remaining SRs were rated as critically low quality. The key limitations of the SRs were lack of a protocol and registration or a list of excluded studies. We did not find high-quality evidence to confirm the effectiveness of acupuncture for COPD, and the main reason was that the qualitative data synthesis relied on trials with small sample sizes and critically low quality.
Conclusion
Acupuncture appears to be an effective therapeutic method for COPD, but the credibility of the results is limited owing to the generally low methodological quality and evidence quality of the included SRs. Further rigorous and comprehensive studies are required to provide robust evidence and draw definitive conclusions.
Keywords: acupuncture, chronic obstructive pulmonary disease, overview, AMSTAR 2, GRADE, systematic review
Introduction
Chronic obstructive pulmonary disease (COPD), which is characterized by persistent airway inflammation and gradual progression of irreversible airway obstruction, is one of the top three causes of death worldwide.1 According to estimates, more than 5 million 400 thousand people will die of COPD or related diseases in the next 40 years, which carries heavy economic and social burdens.1–3 Drug therapy for COPD is long, costly and often associated with drug-related toxicity, therefore, Global Initiative for Chronic Obstructive Lung Disease (GOLD) guideline states that nonpharmacological treatment is complementary to pharmacological treatment and should form part of the comprehensive management of COPD.1,4 Pulmonary rehabilitation (PR) has been recommended as a beneficial nonpharmacological intervention for patients with COPD, but poor referral and uptake rates by suitable patients with COPD are global issues.5–7 Therefore, new nonpharmacological therapies are urgently needed to slow or even stop the progression of COPD.
Acupuncture is an important component of traditional Chinese medical (TCM) and an effective alternative therapy that is used to prevent and treat many diseases, including respiratory diseases.8–10 Proponents argue that acupuncture is effective at relieving symptoms and improving quality of life and activity endurance, and it is associated with fewer adverse effects than conventional approaches used to treat COPD.11 In recent years, with the increasing number of clinical studies12–14 on acupuncture treatment of COPD, a certain number of systematic reviews (SRs)15–23 have been published to provide corresponding evidence supporting clinical decision-making. However, based on preliminary studies, the results of different systematic evaluations are not completely consistent, which are unable to effectively guide clinical practice.
Meta-analysis is considered the highest scientific level for summarizing the results from different analyses. However, considering heterogeneity often exists in published SRs and the evidence from different SRs on the same topic was often conflicting, it has risks accepting the results of a single SR uncritically.24–26 An overview of SRs is required to overcome the limitations of individual SRs and provide comprehensive evidence. In this study, Assessing the Methodological Quality of Systematic Reviews 2 (AMSTAR 2) and the Grades of Recommendations, Assessment, Development and Evaluation (GRADE) system were applied to comprehensively evaluate the quality of the methodology and evidence of existing SRs, thus evaluating the applicability and safety of acupuncture and providing a basis for future high-quality research on acupuncture treatment of COPD.
Materials and Methods
Search Strategy
Electronic literature searches were conducted in PubMed, Embase, Cochrane Library, Web of Science, China National Knowledge Infrastructure Database (CNKI), WANFANG DATA, Chinese Biomedical Literature Database (CBM) and Chongqing VIP (CQVIP), all from inception to January 20, 2021. No restrictions were imposed on the source, publication date, or language of the SRs. The search terms and basic search strategy were as follows: (“COPD” OR “chronic obstructive pulmonary disease” OR “COAD” OR “chronic obstructive lung disease” OR “pulmonary disease, chronic obstructive”) AND (“acupuncture” OR “acupuncture therapy” OR “manual acupuncture” OR “electroacupuncture” OR “auricular acupuncture” OR “warm acupuncture” OR “acupoints”) AND (“systematic review” OR “meta-analysis” OR “systematic assessment”). Detailed search strategies are shown in Table S1. In addition, the references of relevant reviews were searched manually to ensure comprehensive data collection.
Inclusion and Exclusion Criteria
We included studies that met the following criteria:
Study Design and Population: SRs were based on RCTs of acupuncture for COPD. The participants were diagnosed with COPD according to any internationally recognized clinical guidelines, and no restriction was placed on gender or the stage of COPD (stable or acute exacerbation).
Interventions: Treatment measures in the intervention group included various invasive acupuncture therapies (needle acupuncture, electroacupuncture, auricular acupuncture, and body acupuncture, et al) or acupuncture combined with medication therapy, pulmonary rehabilitation, but studies using non-invasive techniques such as single moxibustion, acupressure, and point application were excluded. Treatments applied to the control group included comfort therapy (sham acupuncture or blank control) or other therapies (medication therapy or other nondrug therapies).
Outcomes: At least one of the prespecified outcomes was reported: 1) exercise capacity: 6-minute walking distance (6MWD); 2) health-related quality of life: St. George’s Respiratory Questionnaire (SGRQ); 3) lung function: FEV1%pre, FEV1/FVC.
We excluded studies that met the following criteria:
Studies that were published in abstract form with no full text.
Non-RCT SRs, commentaries, guidelines, protocols, editorials and narrative reviews;
Duplicated publications of the same SRs.
Literature Screening and Data Extraction
We searched the databases according to the predeveloped standardized search strategy. All retrieved literatures were imported into Endnote X8 software (Tomson Research Soft, Stanford, CT, USA). Two reviewers (LC and ZZF) independently screened for candidates according to the inclusion and exclusion criteria by reading the title and abstract. Then, the full texts were downloaded for further screening. At the same time, bibliographic references were also reviewed to identify possible SRs. The disagreements were resolved by discussion. If necessary, the discrepancies were resolved by consulting the third reviewer (YX).
The characteristics of SRs were extracted, including author, title, publication year, sample size, intervention, outcomes, quality assessment tool, and conclusions. Data were independently extracted by two reviewers (LC and ZZF) using Microsoft Excel, and two reviewers cross checked to eliminate mis-entry. Discrepancies were resolved by a discussion among the team members or arbitrated by the third reviewer (YX).
Quality Assessment
Two reviewers (LC and XLL) independently evaluated the quality of the included reviews by AMSTAR 2,24 an updated and improved version of the AMSTAR,27,28 which is available at https://amstar.ca/index.php. It contains 16 items, and seven items (items 2, 4, 7, 9, 11, 13, and 15) are critical domains. Moreover, AMSTAR 2 proposes a four-level scheme (high, moderate, low, and critically low) to rate the overall confidence of the included SRs, and each item was evaluated as “yes”, “partial yes” and “no”.
Strategy for Data Synthesis
We reported the results narratively in text and tables, together with comments on the quality of the evidence. We organized the data by intervention target and types of reported outcomes.
Grading of the Quality of Evidence
Two reviewers (LC and XLL) independently used the GRADE29 system to assess the quality of primary evidence. The following criteria were considered: risk of bias, inconsistencies, indirectness, inaccuracy, and publication bias. The quality of evidence for the outcomes was downgraded from four points initially to one point for each “not reported” or “serious” rating and to two points for each “very serious” rating. Then, meta-analyses were rated as “high” (4 points), “moderate” (3 points), “low” (2 points) or “very low” (≤ 1 point) quality of evidence. Any disagreements were resolved by consensus or discussion with the third reviewer (JSL). A descriptive analysis was used for the efficacy evaluation.
Results
Literature Search and Selection
A total of 151 potentially related literature were retrieved from 8 databases. After 78 duplicated literatures were omitted, the titles and abstracts of 73 literatures were screened, and 52 literatures were excluded because they failed to meet the inclusion criteria. After downloading and reading the other 21 literatures, 12 literatures were excluded (The list of excluded studies with reasons for exclusion are presented in Table S2). Finally, we included 9 SRs.15–23 The process of the literature search and screen is shown in Figure 1.
Figure 1.
Flowchart of literature selection.
Characteristics of the SRs
The characteristics of the 9 SRs included in our final analysis are summarized in Table 1. Five SRs16,17,21–23 were published in Chinese, and the other 415,18–20 were published in English. The number of RCTs included in these SRs varied widely, ranging from 7 to 27, and the total number of participants ranged from 326 to 1298. The interventions administered to the therapy groups are mainly acupuncture, acupuncture plus medication or acupuncture plus pulmonary rehabilitation; the interventions administered to the control groups were mainly medication, sham acupuncture, or pulmonary rehabilitation. The treatment duration ranged from one week to one year. All SRs evaluated the methodological quality of the original research; 8 SRs15–22 applied the Cochrane Handbook for Systematic Reviews of Interventions, and the other23 applied the Jadad scale.
Table 1.
Characteristics of the Included Systematic Reviews
| First Author, Year | Country | Trials (Sample Size) | Intervention | Treatment Duration | Outcomes | Quality Assessment Tool | Overall Conclusion | |
|---|---|---|---|---|---|---|---|---|
| Treatment Group | Control Group | |||||||
| Coyle, 201415 | Australia | 12 (841) | AT | MT | 7 d-1 y | Effective rate; lung function (FEV1 and FVC); arterial blood gases (PaO2 and PaCO2); 6MWD; CAT; acute exacerbation | Cochrane risk of bias tool | AT might improve lung function and the effective rate in people with COPD; however, the evidence is not convincing. |
| Cao, 201716 | China | 9 (326) | AT+PR; AT+MT; AT | SAT+PR; SAT+MT; SAT | 10 d-12 w | 6MWD; SGRQ; lung function (FEV1 and FVC) | Cochrane risk of bias tool | AT is a safe and effective treatment for COPD. |
| Li, 201717 | China | 7 (398) | AT+MT; AT+PR | MT; SAT+PR | 27 d-6 m | Effective rate; lung function (FEV1%pre and FEV1/FVC); 6MWD |
Cochrane risk of bias tool | AT may increase the clinical efficiency, improve the lung function and the quality of life, but there was no significant difference in the 6MWD. |
| Wang, 201818 | China | 19 (1298) | AT+PR; AT+MT; AT+PR+MT | MT; PR; SAT+MT; PR+MT; SAT+PR | 3 w-6 m | Effective rate; dyspnoea (Borg, mMRC); QoL (SGRQ, CAT, and EQ-5D); 6MWD; arterial blood gas; lung function (FEV1, FVC, PEF, FEV1%pre, FEV1/FVC); acute exacerbation | Cochrane risk of bias tool | AT may be effective in improving functional effects, quality of life and pulmonary function in COPD patients. |
| Carles, 201919 | Spain | 27 (-) | AT+PR; AT+MT; AT+PR+MT | PR; MT; PR+MT; SAT+MT; SAT+PR+MT | 10 d-100 d | Dyspnoea (Borg, mMRC, and DVAS); QoL (SGRQ and CAT); lung function (FEV1%pre, FVC, FEV1/FVC, PEF, and TLC); 6MWD | Cochrane risk of bias tool | AT may improve QoL and exercise capacity in patients with stable COPD. Mixed results were obtained for lung function, but those statistically significant differences were not clinically relevant. |
| Hsieh, 201920 | China | 12 (798) | AT+MT; AT+PR+MT; AT+PR | MT; PR+MT; PR | 4 w-14 w | Effective rate; lung function (FEV1, FEV1/FVC, MVV, TLC, RV, and RV/TLC); ISWT; dyspnoea (Borg and mMRC); QoL (SGRQ, EQ-5D, and CAT); arterial blood gases (PaO2 and PaCO2) | Cochrane risk of bias tool | AT is an effective adjunct non-pharmacological treatment to improve HRQL in patients receiving medical treatment for COPD. |
| Xie, 201921 | China | 8 (498) | AT+ MT | MT | 14 d-20 d | Lung function (FEV1 and FEV1/FVC); CAT; mMRC | Cochrane risk of bias tool | AT may improve FEV1% and FEV1/FVC, and reduce the CAT scores and mMRC scores of patients with AECOPD. |
| Zheng, 201922 | China | 10 (902) | AT + MT | MT | 1 w-6 m | Effective rate; lung function (FEV1, FVC, FEV1%pre, and FEV1/FVC); CD4+/CD8+ | Cochrane risk of bias tool | AT may improve the efficiency and the immune function of patients of COPD, but does not improve lung function. |
| Wang, 202023 | China | 9 (682) | AT+PR; AT+MT; AT + MT | PR; MT; SAT+MT | 1 w-6 m | 6MWD; SGRQ; lung function (FEV1, FEV1%pre, FVC%, FEV1/FVC, PEF, TLC, and MVV); arterial blood gases (PaO2 and PaCO2); | Jadad scale | AT is a safe and effective treatment for COPD. |
Note: Acupuncture therapy included needle acupuncture, acupuncture point injection therapy.
Abbreviations: AT, acupuncture therapy; SAT, sham acupuncture therapy; MT, medication therapy; PR, pulmonary rehabilitation; d, day; w, week; m, month; y, year; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; FEV1%pre, forced expiration volume in 1 s/prediction; FEV1/FVC, percentage of forced expiratory volume and forced vital capacity in 1 s; PEF, peak expiratory flow; MVV, maximal voluntary ventilation; TLC, total lung capacity; RV, residual volume; IVC, inspiratory vital capacity; 6MWD, six-minute walk distance; ISWT, incremental shuttle walk test; QoL, quality of life; SGRQ, St. George’s respiratory questionnaire; CAT, COPD assessment test; EQ-5D, EuroQol five dimensions questionnaire; mMRC, Modified Medical Research Council; DVAS, dyspnoea visual analogue scale; SSAI, Spielberger’s state anxiety inventory; GDS, geriatric depression scale; HAM-A, Hamilton anxiety rating scale; HAM-D, Hamilton depression rating scale.
Methodological Quality
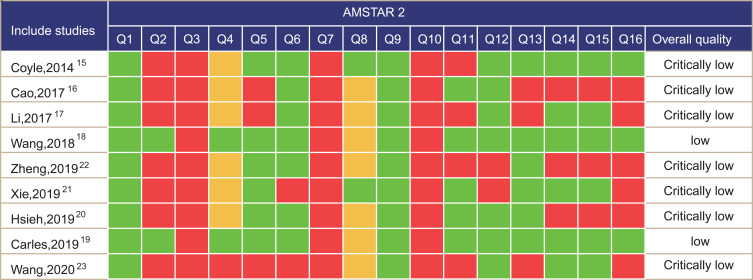
No SRs presented high and moderate levels of methodological quality based on the AMSTAR 2 scores; only 2 SRs18,19 scored at low overall levels, while the other 7 SRs15–17,20–23 scored at critically low levels (see Figure 2). The key factors affecting the methodological quality of the SRs were item 2 (only 2 SRs18,19 established a prior study protocol) and item 7 (none of the SRs explained the reasons for selecting the study type or provided a complete list of excluded studies with reasons). Seven SRs15–17,20–23 reported incomplete elements of the literature search strategy and did not describe the use of a specific search strategy. Four SRs15,17,22,23 used appropriate statistical methods to synthesize the results, but the sources of heterogeneity were not analysed. Three SRs16,17,23 did not consider the risk of bias of individual studies when interpreting and discussing the results. Three SRs16,20,22 did not investigate the possibility of publication bias or discuss the effect of publication bias on outcomes when quantitatively merging the results.
Figure 2.
Quality assessment according to the AMSTAR-2 items for included systematic reviews. Q1: Did the research questions and inclusion criteria for the review include the components of population, intervention, comparison, outcome (PICO)? Q2: Did the report of the review contain an explicit statement that the review methods were established prior to the conduct of the review and did the report justify any significant deviations from the protocol? Q3: Did the review authors explain their selection of the study designs for inclusion in the review? Q4: Did the review authors use a comprehensive literature search strategy? Q5: Did the review authors perform study selection in duplicate? Q6: Did the review authors perform data extraction in duplicate? Q7: Did the review authors provide a list of excluded studies and justify the exclusions? Q8: Did the review authors describe the included studies in adequate detail? Q9: Did the review authors use a satisfactory technique for assessing the risk of bias (RoB) in individual studies that were included in the review? Q10: Did the review authors report on the sources of funding for the studies included in the review? Q11: If meta-analysis was performed did the review authors use appropriate methods for statistical combination of results? Q12: If meta-analysis was performed, did the review authors assess the potential impact of RoB in individual studies on the results of the meta-analysis or other evidence synthesis? Q13: Did the review authors account for RoB in individual studies when interpreting/discussing the results of the review? Q14: Did the review authors provide a satisfactory explanation for, and discussion of, any heterogeneity observed in the results of the review? Q15: If they performed quantitative synthesis did the review authors carry out an adequate investigation of publication bias (small study bias) and discuss its likely impact on the results of the review? Q16: Did the review authors report any potential sources of conflict of interest, including any funding they received for conducting the review?.
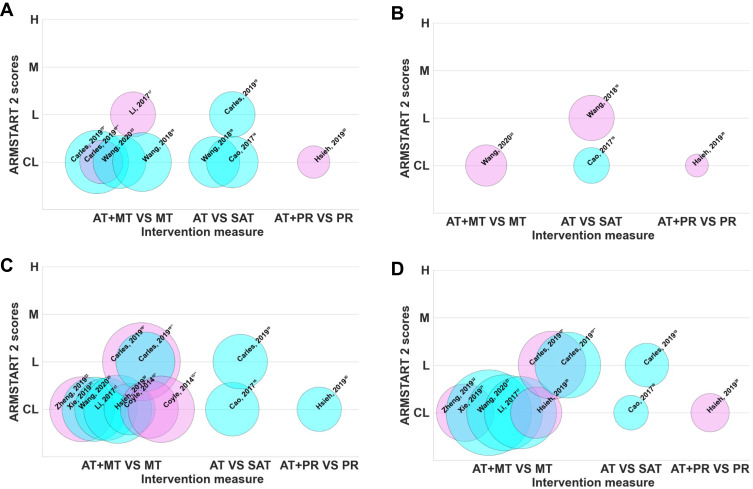
Effectiveness of Acupuncture and Evidence Quality
Since the obtained data were unable to be quantitatively analysed, a descriptive analysis method was adopted to evaluate the outcomes of interest in the SRs included in this study, and the GRADE system were assessed for each single outcome. Specific research results are presented in Table 2 and Figure 3.
Table 2.
Quality of Evidence in Included Systematic Reviews with GRADE
| Outcome Measures | Systematic Reviews | N/n | Effect Estimate (95% CI) | Quality Assessment | Quality of Evidence | ||||
|---|---|---|---|---|---|---|---|---|---|
| Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | |||||
| 6 MWD | AT+MT vs MT | ||||||||
| Carles et al 201919 | 4(306)* | MD 33.05(19.11, 46.99) | 0 | −1b | 0 | −1c | 0 | Low | |
| 2(142)** | MD 0.65(−20.74, 22.04) | −1a | 0 | 0 | −1c | 0 | Low | ||
| Wang et al 202023 | 4(212) | MD 10.16(4.34, 15.99) | −1a | 0 | 0 | −1c | 0 | Low | |
| Li et al 201717 | 3(155) | MD 14.71(−17.09, 6.50) | 0 | 0 | 0 | −1c | 0 | Moderate | |
| Wang et al 201818 | 4(263) | MD 35.15(2.37, 67.92) | 0 | −1b | 0 | −1c | 0 | Low | |
| AT vs SAT | |||||||||
| Wang et al 201818 | 4(198) | MD 63.05(39.27, 86.83) | 0 | −1b | 0 | −1c | 0 | Low | |
| Cao et al 201716 | 5(203) | MD 33.69(5.85, 61.52) | −1a | 0 | 0 | −1c | 0 | Low | |
| Carles et al 201919 | 4(158) | MD 76.68(39.93, 113.43) | 0 | 0 | 0 | −1c | 0 | Moderate | |
| AT+PR vs PR | |||||||||
| Hsieh et al 201920 | 1(80) | MD 8.40(−5.88, 22.68) | 0 | −1b | 0 | −1c | 0 | Low | |
| SGRQ | AT+MT vs MT | ||||||||
| Wang et al 202023 | 2(130) | MD −2.76(−5.65, 0.14) | −1a | 0 | 0 | −1c | 0 | Low | |
| AT vs SAT | |||||||||
| Cao et al 201716 | 2(98) | MD - 9.00(−14.44, −3.56) | 0 | 0 | 0 | −1c | 0 | Moderate | |
| Wang et al 201818 | 3(157) | MD −10.66(−22.24, 0.92) | 0 | 0 | 0 | −1c | 0 | Moderate | |
| AT + PR vs PR | |||||||||
| Hsieh et al 201920 | 1(40) | MD 0.3(−6.83, 7.43) | −1a | −1b | 0 | −1c | −1e | Very Low | |
| FEV1% | AT +MT vs MT | ||||||||
| Zheng et al 201922 | 4(321) | SMD 0.10(−0.62, 0.82) | 0 | −1b | 0 | −1c | 0 | Low | |
| Xie et al 201921 | 6(313) | MD 4.94(1.75, 8.11) | −1a | −1b | 0 | −1c | 0 | Very Low | |
| Wang et al 202023 | 6(296) | MD 5.93(5.73, 6.14) | −1a | 0 | 0 | −1c | −1d | Very Low | |
| Li et al 201717 | 6 (354) | MD 1.98(0.14, 3.82) | 0 | 0 | 0 | −1c | 0 | Moderate | |
| Hsieh et al 201920 | 3(200) | MD 1.98(0.26, 3.70) | −1a | 0 | 0 | −1c | −1e | Very Low | |
| Carles et al 201919 | 9(462)* | MD 1.04(−0.21, 2.29) | −1a | 0 | 0 | 0 | 0 | Moderate | |
| 4(267)** | MD 3.09(1.00, 5.18) | −1a | 0 | 0 | −1c | 0 | Low | ||
| Coyle et al 201415 | 2(256) * | MD −5.06(−25.38, 15.26) | −1a | 0 | 0 | −1c | 0 | Low | |
| 3(336) ** | MD 1.46(−1.20, 4.11) | −1a | 0 | 0 | −1c | 0 | Low | ||
| AT vs SAT | |||||||||
| Cao et al 201716 | 5(219) | MD 4.93(1.87, 7.99) | 0 | 0 | 0 | −1c | 0 | Moderate | |
| Carles et al 201919 | 6(227) | MD 5.40(2.90, 7.91) | 0 | 0 | 0 | −1c | 0 | Moderate | |
| AT + PR vs PR | |||||||||
| Hsieh et al 201920 | 2(150) | MD 7.80(6.91, 8.68) | −1a | 0 | 0 | −1c | −1e | Very Low | |
| FEV1/FVC | AT +MT vs MT | ||||||||
| Zheng et al 201922 | 3(251) | SMD −0.13(−0.37,0.12) | −1a | 0 | 0 | −1c | 0 | Low | |
| Xie et al 201921 | 10(558) | MD 4.40(0.72, 8.08) | −1a | 0 | 0 | 0 | 0 | Moderate | |
| Wang et al 202023 | 6(438) | MD 10.16(4.34, 15.99) | −1a | 0 | 0 | 0 | 0 | Moderate | |
| Li et al 201717 | 7(398) | MD 0.47(0.27, 0.67) | −1a | 0 | 0 | −1c | −1d | Very Low | |
| Hsieh et al 201920 | 3(200) | MD 1.56(−0.18, 3.29) | −1a | 0 | 0 | −1c | −1e | Very Low | |
| Carles et al 201919 | 7(349) * | MD 1.33(−1.19, 3.85) | −1a | −1b | 0 | −1c | 0 | Very Low | |
| 4(330) ** | MD 3.42(1.55, 5.29) | −1a | −1b | 0 | −1c | 0 | Very Low | ||
| AT vs SAT | |||||||||
| Cao et al 201716 | 3(91) | MD 7.57(0.34, 14.80) | −1a | 0 | 0 | −1c | −1d | Very Low | |
| Carles et al 201919 | 4(145) | MD 6.64(3.44, 9.83) | 0 | 0 | 0 | −1c | 0 | Moderate | |
| AT+PR vs PR+MT | |||||||||
| Hsieh et al 201920 | 2(112) | MD −3.50(−10.11, 3.12) | −1a | −1b | 0 | −1c | −1e | Very Low | |
Notes: N: number of studies; n: number of participants; *stable COPD; **acute exacerbation of COPD; athe design of the experiment with a large bias in random, distributive hiding, or blind; bthe confidence interval overlaps less, the heterogeneity test P is very small, and I2 is larger; cthe sample size is small, and the confidence interval is wide; dfunnel graph asymmetry; efewer studies are included, and there may be greater publication bias.
Figure 3.
Evidence mapping of the interest outcomes. Bubbles: the studies included in this article (first author, publication year); Bubble size: sample size; X-axis: different intervention measures included; Y-axis: AMSTAR score; color: light blue represents the P-value<0.05, light purple represents the P-value>0.05; (A) evidence mapping of 6MWD; (B) evidence mapping of SGRQ; (C) evidence mapping of FEV1%pre; (D) evidence mapping of FEV1/FEV.
Notes: *Stable COPD, **acute exacerbation of COPD.
Abbreviations: CL, critically low; L, low; M, moderate; H, high; AT, acupuncture therapy; SAT, sham acupuncture therapy; MT, medication therapy; PR, pulmonary rehabilitation.
6MWD
A total of 5 SRs16–19,23 analysed the outcome of the 6MWD test: 1) Four SRs17–19,23 compared acupuncture plus medical treatment with medicine treatment. Among these articles, one SR19 conducted a subgroup analysis of patients with different clinical stages of COPD, showing a significant improvement only in patients with stable COPD (MD 33.05, 95% CI 19.11 to 46.99, low quality). Two SRs18,23 reported obvious improvements in the acupuncture group (MD 10.16, 95% CI 4.34 to 15.99, low quality; MD 35.15, 95% CI 2.73 to 67.92, low quality); one SR17 showed a nonsignificant improvement (MD 14.71, 95% CI −17.09 to 6.50, moderate quality). 2) Three SRs16,18,19 compared acupuncture with sham acupuncture and showed a significant improvement in the 6MWD of in the acupuncture group (MD 63.05, 95% CI 39.27 to 86.83, low quality; MD 33.69, 95% CI 5.58 to 61.52, low quality; MD 76.68, 95% CI 39.93 to 113.43, moderate quality). 3) When comparing acupuncture plus pulmonary rehabilitation with pulmonary rehabilitation,20 statistically significant differences were not observed between the groups (MD 8.40, 95% CI −5.88 to 22.68, low quality). The evidence mapping of 6MWD is shown in Figure 3A.
SGRQ
A total of 4 SRs16,18,20,23 analysed SGRQ (Figure 3B): 1) One SR23 compared acupuncture plus medicine treatment with medicine treatment, and no significant difference was detected between the two groups (MD −2.76, 95% CI −5.65 to 0.14, low quality). 2) Two SRs16,18 compared acupuncture with sham acupuncture: 1 SR16 indicated a statistically significant difference between the two groups (MD −9.00, 95% CI −14.44 to −3.56, moderate quality); the other18 showed an improvement that was not statistically significant in the two groups (MD −10.66, 95% CI −22.24 to 0.92, moderate quality). 3) A significant difference in SGRQ was not observed between acupuncture and pulmonary rehabilitation group and the pulmonary rehabilitation group (MD 0.3, 95% CI −6.83 to 7.43, very low quality).
FEV1%pre
Eight SRs15–17,19–23 were conducted to systematically analyse the outcome of FEV1%pre (Figure 3C): 1) Seven SRs15,17,19–23 compared acupuncture plus medicine treatment with medicine treatment. Two SRs15,19 conducted a subgroup analysis of patients with different clinical stages of COPD; one review15 reported that acupuncture significantly improved FEV1%pre only in patients with acute exacerbations of COPD (MD 3.09, 95% CI 1.00 to 5.18, low quality); another review19 reported no significant difference in either patients with stable or acute exacerbations of COPD between the two groups. Four17,20,21,23 of the 5 SRs without a staging analysis showed that the change in FEV1%pre between interventions was statistically significant (MD 4.94, 95% CI 1.75 to 8.11, very low quality; MD 5.93, 95% CI 5.73 to 6.14, very low quality; MD 1.98, 95% CI 0.14 to 3.82, moderate quality; MD 1.98, 95% CI 0.26 to 3.70, very low quality); one SR22 showed no significant difference in FEV1%pre between the two groups (MD 0.10, 95% CI −0.62 to 0.82, low quality). 2) Two SRs16,19 compared acupuncture with sham acupuncture. The improvement in FEV1%pre in the acupuncture group was more significant than in the control group (MD 4.93, 95% CI 1.87 to 7.99, moderate quality; MD 5.40, 95% CI 2.90 to 7.91, moderate quality). 3) One SR20 compared acupuncture plus pulmonary rehabilitation with pulmonary rehabilitation, and more obvious improvements were noted in the acupuncture group than in the control group (MD 7.80, 95% CI 6.91 to 8.68, very low quality).
FEV1/FVC
A total of 7 SRs16,17,19–23 analysed the outcome of FEV1/FVC (Figure 3D): 1) Six SRs17,19–23 compared acupuncture plus medicine treatment with medicine treatment. One SR19 reported that acupuncture significantly improved FEV1/FVC only in patients with acute exacerbations of COPD (MD 3.42, 95% CI 1.55 to 5.29, very low quality); Three17,21,23 of the 5 SRs without a staging analysis showed greater improvements in FEV1/FVC in the acupuncture group than in the control group (MD 4.40, 95% CI 0.72 to 8.08, moderate quality; MD 10.16, 95% CI 4.34 to 15.99, moderate quality; MD 0.47, 95% CI 0.27 to 0.67, very low quality), two SRs20,22 showed no significant difference between the two groups (SMD −0.13, 95% CI −0.37 to 0.12, low quality; MD 1.56, 95% CI −0.18 to 3.29, very low quality). 2) Two SRs16,19 compared acupuncture with sham acupuncture and revealed a significant difference between the two groups (MD 7.57, 95% CI 0.34 to 14.80, very low quality; MD 6.64, 95% CI 3.44 to 9.83, moderate quality). 3) One SR20 compared acupuncture plus pulmonary rehabilitation with pulmonary rehabilitation, but did not observe a significant difference between the two groups (MD −3.50, 95% CI −10.11 to 3.12, very low quality).
Safety and Adverse Events
Of all 9 SRs, adverse effects were mentioned in 8 SRs.15,16,18–23 Of these 8 SRs, 5 SRs15,16,19,20,22 stated that no adverse events were reported in the studies they included; 2 SRs18,23 reported mild adverse reactions but did not describe them in detail; and the remaining SR21 reported that the adverse events caused by acupuncture included subcutaneous haemorrhage, pinprick pain sensations, and an inability to tolerate stimulation. However, a meta-analysis was unable to be conducted due to insufficient data.
Discussion
Main Findings
Overview of SRs is an increasingly popular form of evidence synthesis, and that provides more authentic and reliable evidence for clinical decision-making.30 Previous researches have shown that acupuncture is an effective in the treatment of for COPD.8,13,14 This overview provided a comprehensive mapping of the evidence on the effectiveness of acupuncture for COPD. A total of 9 SRs were included in this overview, the evaluation with AMSTAR 2 showed that the quality of included SRs was low or critically low and the results of the GRADE system evaluation showed that the strength of evidence was very low to low for most outcomes.
Assessment of the Quality of the Included SRs
AMSTAR 2 was used to evaluate the methodological quality of the included SRs. The overall methodological quality of the 9 SRs included in this study was “low” and “critically low”. Specifically, in our study, SRs frequently lacked details on the prior registration and/or publication of protocol, failed to provide of list of excluded studies at full-text level or did not assess the potential effect of the risk of bias on the results. The proportion of reviews with protocol registration in our study was 22%. The Preferred Reporting Items for SRs and Meta-analyses (PRISMA) statement first proposed registry for the protocol of SRs, and it notes that prospective registrations of SRs might reduce the probability of bias in the review and improve the transparency of the research since the authors report their methods and statistical analysis a priori.31 According to the assessment performed in this study, none of the 9 SRs met item 7. The list of excluded studies and the reason for the exclusion must be explained since the effect of the excluded studies on a systematic literature review cannot be determined if the list of excluded studies and reasons for exclusion are not provided at the same time.24 Although all SRs used appropriate methods for the risk of bias assessment, only some SRs considered the effect of the quality of included trials on their results. SR researchers should be aware that simply assessing the risk of bias is not sufficient, and its effect on the results of the review should be assessed. Considering the critically low quality of all the included SRs, the results should be interpreted with caution.
Overall Completeness and Applicability of the Evidence
The 6MWD and SGRQ were used as indexes to evaluate the exercise capacity and quality of life of patients with COPD.32,33 FEV1%pre and FEV1/FVC were recommended to determine the diagnosis and prognosis of COPD.34,35 In the present study, we analysed these four outcomes of interest in 3 subgroups divided according to different intervention measures. The results revealed inconsistent results from diverse subgroups. In the subgroup of acupuncture compared with sham acupuncture, all correlation studies showed that intervention groups presented a significantly improved in 6MWD, FEV1%pre and FEV1/FVC, half of studies exhibited statistically significant improvement in SGRQ. Notably, the majority of these results also have clinical implications, although the minimal clinically important difference (MCID) was also considered.36,37 However, unifying conclusions cannot be drawn from the equivocal results of the remaining 2 subgroups (acupuncture plus medicine treatment compared with medicine treatment, and acupuncture plus pulmonary rehabilitation compared with pulmonary rehabilitation). We speculated that the reason for this phenomenon is the differences in the acupoints, acupuncture occasion, acupuncture manipulation, and stimulation volume.
In our study, the overall quality of the evidence supporting the outcome indicators was mainly “low” and “very low”, and no evidence was considered “high”. Based on our study, we identified possible reasons for the inconsistency of research results and the reduction in the evidence level, as described below. 1) Poor methodological quality of the included RCTs. Most of the trials mentioned grouping using randomization methods but did not describe specific methods. Additionally, considering the operando visualization of acupuncture, it is very difficult to conduct blinded methods. 2) High heterogeneity existed among some studies. The sources of heterogeneity were derived from differences in acupuncture types and the frequency and duration of treatment. 3) The quality of the evidence was downgraded due to the wide confidence interval or the sample size that did not meet the optimal information size.
Implications for Future Practice and Research
Because of its superior availability and relatively low clinical side effects, acupuncture has become an important complementary and alternative therapy for numerous diseases.38,39 We found some positive evidence supporting the use of acupuncture in the treatment of COPD, although the GRADE quality of evidence was assessed as low. Due to these concerns, more rigorous larger-scale and well-designed RCTs are needed to provide higher quality evidence and evaluate the efficacy of acupuncture for COPD. First, RCTs should follow the corresponding guidelines such as CONSORT40 (Consolidated Standards of Reporting Trials) which applied to all kinds of RCTs or the characteristic guidelines such as STRICTA41 (Standards for Reporting Interventions in Controlled Trials of Acupuncture) for acupuncture. Second, many different types of acupuncture are used to treat COPD in clinical practice. Therefore, future studies comparing different acupuncture interventions are needed to identify the most effective acupuncture method. Furthermore, the optimal duration and frequency of treatment are also important for patients with COPD. Third, all SRs must be registered in advance to facilitate processing transparency and to avoid the risk of bias in methodology. Additionally, crucial safety evaluations of acupuncture in the treatment of COPD are needed in clinical trials, and cost-effectiveness studies should be performed to evaluate acupuncture as a treatment for COPD. This approach will provide a comprehensive assessment of the effectiveness and safety of acupuncture for COPD.
Study Limitations
Several limitations need to be taken into account when interpreting our results. First, we only searched Chinese and English databases, and thus SRs published in other languages that met the inclusion criteria may have been missed. Second, the evaluation process of AMSTAR 2 and GRADE is inevitably subjective and may lead to bias, though this study had been independently evaluated and checked by two researchers. Third, we only narrative summarized rather than quantitatively analysed the effectiveness of interventions because of obvious clinical and statistical heterogeneity between the included systematic reviews, as well as complex categories of interventions. Lastly, since the number of analysed articles was limited, we were unable to include factors such as the different types of acupuncture and stages of COPD in subgroup analyses.
Conclusion
What is the precise role of acupuncture in the treatment of COPD? In our study, the methodological quality of the included SRs varied, the quality of evidence underlying these outcomes was mixed (very low to moderate), and the firm conclusions on this question are difficult to draw. Therefore, while constantly improving the experimental design, researchers should combine the characteristics of acupuncture diagnosis and treatment with modern clinical RCTs to produce more high-quality, scientific and accurate clinical evidence.
Funding Statement
This research was supported by grants from the Program of National Natural Science Foundation of China (No. 81830116); the Qihuang Scholars Award of the State TCM Academic Leader Program (No.(2018)284); National Key Research & Development Program of China (No. 2018YFC1704800, 2018YFC1704802); Program for Science & Technology Innovation Talents in Universities of Henan Province (No. 19HASTIT008).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (updated 2020). Available from: http://www.goldcopd.org. Accessed November. 22, 2020. [Google Scholar]
- 2.Xia Y, Wu Q, Wang H, et al. Global, regional and national burden of gout, 1990–2017: a systematic analysis of the global burden of disease study. Rheumatology. 2020;59(7):1529–1538. doi: 10.1093/rheumatology/kez476 [DOI] [PubMed] [Google Scholar]
- 3.Steel N, Ford JA, Newton JN, et al. Changes in health in the countries of the UK and 150 English Local Authority areas 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2018;392(10158):1647–1661. doi: 10.1016/s0140-6736(18)32207-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. doi: 10.1164/rccm.201204-0596PP [DOI] [PubMed] [Google Scholar]
- 5.Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–e64. doi: 10.1164/rccm.201309-1634ST [DOI] [PubMed] [Google Scholar]
- 6.Johnston K, Young M, Grimmer K, Antic R, Frith P. Frequency of referral to and attendance at a pulmonary rehabilitation programme amongst patients admitted to a tertiary hospital with chronic obstructive pulmonary disease. Respirology. 2013;18(7):1089–1094. doi: 10.1111/resp.12128 [DOI] [PubMed] [Google Scholar]
- 7.O’Connor C, Lawson R, Waterhouse J, Mills GH. Is inspiratory muscle training (IMT) an acceptable treatment option for people with chronic obstructive pulmonary disease (COPD) who have declined pulmonary rehabilitation (PR) and can IMT enhance PR uptake? A single-group prepost feasibility study in a home-based setting. BMJ Open. 2019;9(8):e028507. doi: 10.1136/bmjopen-2018-028507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.von Trott P, Oei SL, Ramsenthaler C. Acupuncture for breathlessness in advanced diseases: a systematic review and meta-analysis. J Pain Symptom Manage. 2020;59(2):327–338.e323. doi: 10.1016/j.jpainsymman.2019.09.007 [DOI] [PubMed] [Google Scholar]
- 9.Shen X, Xia J, Adams C. Acupuncture for schizophrenia. Schizophr Bull. 2014;40(6):1198–1199. doi: 10.1093/schbul/sbu135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tu J-F, Yang J-W, Shi G-X, et al. Efficacy of intensive acupuncture versus sham acupuncture in knee osteoarthritis: a randomized controlled trial. Arthritis Rheumatol. 2020. doi: 10.1002/art.41584 [DOI] [PubMed] [Google Scholar]
- 11.Suzuki M, Namura K, Ohno Y, et al. Combined standard medication and acupuncture for COPD: a case series. Acupunct Med. 2012;30(2):96–102. doi: 10.1136/acupmed-2011-010112 [DOI] [PubMed] [Google Scholar]
- 12.Feng J, Wang X, Li X, Zhao D, Xu J. Acupuncture for chronic obstructive pulmonary disease (COPD): a multicenter, randomized, sham-controlled trial. Medicine. 2016;95(40):e4879. doi: 10.1097/md.0000000000004879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Suzuki M, Muro S, Fukui M, et al. Effects of acupuncture on nutritional state of patients with stable chronic obstructive pulmonary disease (COPD): re-analysis of COPD acupuncture trial, a randomized controlled trial. BMC Complement Altern Med. 2018;18(1):287. doi: 10.1186/s12906-018-2341-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maekura T, Miki K, Miki M, Kitada S, Maekura R. Clinical effects of acupuncture on the pathophysiological mechanism of chronic obstructive pulmonary disease during exercise. Int J Chron Obstruct Pulmon Dis. 2019;14:2787–2798. doi: 10.2147/copd.s225694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coyle ME, Shergis JL, Huang ET-Y, et al. Acupuncture therapies for chronic obstructive pulmonary disease: a systematic review of randomized, controlled trials. Altern Ther Health Med. 2014;20(6):10–23. [PubMed] [Google Scholar]
- 16.Cao IL, He HL, Zhou XM. Meta analysis of the therapeutic effect of acupuncture on chronic obstructive pulmonary disease. Global Tradit Chin Med. 2017;10(07):899–904. doi: 10.3969/j.issn.1674-1749.2017.07.038 [DOI] [Google Scholar]
- 17.Tang J-F, Li,W-X, Zhang F. Discrimination of Radix Polygoni Multiflori from different geographical areas by UPLC-QTOF/MS combined with chemometrics. Henan Univ Chin Med. 2017;12. doi: 10.1186/s13020-017-0155-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang JJ, Li JS, Yu XQ, Xie Y. Acupuncture therapy for functional effects and quality of life in COPD patients: a systematic review and meta-analysis. Biomed Res Int. 2018;2018:3026726. doi: 10.1155/2018/3026726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fernández-Jané C, Vilaró J, Fei Y, et al. Filiform needle acupuncture for copd: a systematic review and meta-analysis. Complement Ther Med. 2019;47:102182. doi: 10.1016/j.ctim.2019.08.016 [DOI] [PubMed] [Google Scholar]
- 20.Hsieh P-C, Yang M-C, Wu Y-K, et al. Acupuncture therapy improves health-related quality of life in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Complement Ther Clin Pract. 2019;35:208–218. doi: 10.1016/j.ctcp.2019.02.016 [DOI] [PubMed] [Google Scholar]
- 21.Xie HF. Effect of acupuncture therapy for acute exacerbation of chronic obstructive pulmonary disease, A systematic review and meta-analysis [Thesis of master’s degree]. Beijing Univ Chin Med. 2019. [Google Scholar]
- 22.Zheng WJ, Peng ZJ, Zhang TG, et al. A meta- analysis and trial sequential analysis of acupoint injection with chuankezhi injection for treating stable-stage patients with chronic obstructive lung disease. Traditl Chin Drug Res Clin Pharmacol. 2019;30(6):725–732. doi: 10.19378/j.issn.1003-9783.2019.06.015 [DOI] [Google Scholar]
- 23.Wang YD, Li FS, Li Z, Yue JN, Ma CL. Systematic evaluation of acupuncture on pulmonary rehabilitation in patients with stable chronic obstructive pulmonary disease. Mod Tradit Chin Med Mater Medica World Sci Technol. 2020;22(01):196–204. doi: 10.11842/wst.20190222003 [DOI] [Google Scholar]
- 24.Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(oct18 2):d5928. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murad MH, Montori VM, Ioannidis JPA, et al. How to read a systematic review and meta-analysis and apply the results to patient care: users’ guides to the medical literature. JAMA. 2014;312(2):171–179. doi: 10.1001/jama.2014.5559 [DOI] [PubMed] [Google Scholar]
- 27.Shea BJ, Hamel C, Wells GA, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol. 2009;62(10):1013–1020. doi: 10.1016/j.jclinepi.2008.10.009 [DOI] [PubMed] [Google Scholar]
- 28.Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7(1):10. doi: 10.1186/1471-2288-7-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490. doi: 10.1136/bmj.328.7454.1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hartling L, Chisholm A, Thomson D, Dryden DM, Smalheiser NR. A descriptive analysis of overviews of reviews published between 2000 and 2011. PLoS One. 2012;7(11):e49667. doi: 10.1371/journal.pone.0049667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339(jul21 1):b2700. doi: 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chandra D, Wise RA, Kulkarni HS, et al. Optimizing the 6-min walk test as a measure of exercise capacity in COPD. Chest. 2012;142(6):1545–1552. doi: 10.1378/chest.11-2702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen HY, Ma CH, Cao KJ, et al. A systematic review and meta-analysis of herbal medicine on chronic obstructive pulmonary diseases. Evid Based Complement Alternat Med. 2014;2014:925069. doi: 10.1155/2014/925069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhou Y, Zhong N-S, Li X, et al. Tiotropium in early-stage chronic obstructive pulmonary disease. N Engl J Med. 2017;377(10):923–935. doi: 10.1056/NEJMoa1700228 [DOI] [PubMed] [Google Scholar]
- 35.Cruickshank-Quinn CI, Jacobson S, Hughes G, et al. Metabolomics and transcriptomics pathway approach reveals outcome-specific perturbations in COPD. Sci Rep. 2018;8(1):17132. doi: 10.1038/s41598-018-35372-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Holland AE, Hill CJ, Rasekaba T, Lee A, Naughton MT, McDonald CF. Updating the minimal important difference for six-minute walk distance in patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2010;91(2):221–225. doi: 10.1016/j.apmr.2009.10.017 [DOI] [PubMed] [Google Scholar]
- 37.Jones PW. St. George’s Respiratory Questionnaire: MCID. COPD. 2005;2(1):75–79. doi: 10.1081/copd-200050513 [DOI] [PubMed] [Google Scholar]
- 38.He Y, Guo X, May BH, et al. Clinical evidence for association of acupuncture and acupressure with improved cancer pain: a systematic review and meta-analysis. JAMA Oncol. 2020;6(2):271–278. doi: 10.1001/jamaoncol.2019.5233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Armour M, Smith CA, Wang L-Q, et al. Acupuncture for depression: a systematic review and meta-analysis. J Clin Med. 2019;8(8):8. doi: 10.3390/jcm8081140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. 2010;63(8):834–840. doi: 10.1016/j.jclinepi.2010.02.005 [DOI] [PubMed] [Google Scholar]
- 41.MacPherson H, Altman DG, Hammerschlag R, et al. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. PLoS Med. 2010;7(6):e1000261. doi: 10.1371/journal.pmed.1000261 [DOI] [PMC free article] [PubMed] [Google Scholar]