Abstract
The transmission of coronaviruses can be affected by several factors, including the climate. Due to the rapid spread of COVID-19 and the urgent need for rapid responses to contain the pandemic, it is essential to understand the role that weather conditions on the transmission of SARS-CoV-2. We evaluate the influence of meteorological factors on the incidence of COVID-19 during the first wave of the epidemic in Catalonia. We conducted a geographical analysis at the county level to evaluate the association between mean temperature, absolute humidity, solar radiation, and the cumulative incidence of COVID-19. Next, we used a time-series design to assess the short-term effects of meteorological factors on the daily incidence of COVID-19. We found a geographical association between meteorological factors and the cumulative incidence of COVID-19, from the end of March to June 2020, and a lesser extent in the short-term on the daily incidence during the first wave of the epidemic in Spain. Our findings suggest that warm and wet climates may reduce the incidence of COVID-19 in Catalonia. However, policy makers must interpret with caution any COVID-19 risk predictions based on climate information alone.
Keywords: SARS-CoV-2, COVID-19, Incidence, Temperature, Absolute humidity, Solar radiation
Graphical abstract
1. Introduction
The first confirmed case of SARS-CoV-2 in the region of Catalonia, Spain, was identified on February 25th, 2020. Since then, the epidemic spread countrywide, and Catalonia became the second most affected region in Spain. On June 30th, when the post-lockdown period ended and allegedly Spain returned to normality, more than 60,000 cases had been diagnosed and 5000 deaths had been reported during the first wave of the epidemic in Catalonia.
The transmission of coronaviruses can be affected by several factors, including the climate. From the knowledge of other viral respiratory diseases (e.g., influenza) suggests that the transmission of SARS-CoV-2 can be affected by outdoor seasonal climate factors, like ambient temperature and humidity [1,2]. Therefore, it is essential to understand the role that weather conditions could have on the transmission of SARS-CoV-2. Many studies have been conducted since the beginning of the pandemic on the effects of environmental conditions and potential seasonality of COVID-19 [3]. Most are based on geographical correlations comparing the incidence of COVID-19 between countries in different regions. These studies are prone to confounding because did not account for North-to-South different socio-economic conditions [4] nor the delay in spread to warmer regions due to travel patterns [5], and might have some measurement error due to high spatial variability when estimating a fixed temperature exposure for large geographic areas [6]. At the temporal scale, few studies have been conducted locally. Also, COVID-19 disease has been prevalent for only half a year and environmental time-series data for a full seasonal cycle are not yet available [4]. Thus, reported associations could be spurious due to the short study period [7]. A systematic review concluded that the evidence far suggests a weak modulation effect, currently overwhelmed by the scale and rate of the spread of COVID-19 [4].
In our local setting, preliminary results in the city of Barcelona suggested a possible association between maximum temperature and the daily incidence of COVID-19 [7]. However, the evidence is still inconclusive. We aim to evaluate the influence of meteorological factors on the incidence of COVID-19 at the geographic and temporal aggregation levels to understand their possible role in the transmission of SARS-CoV-2 appropriately.
2. Materials and methods
2.1. Setting and data collection
Catalonia is the second largest region in Spain, with a population of more than 7.6 million inhabitants, including the city of Barcelona, the second-largest nationwide (1.7 million). It is located in the northeast corner of Spain, and and organized in 42 counties administratively grouped into four provinces, with a respective capital city (Appendix Fig. A.1).
For each county, we collected daily counts of incident cases diagnosed from a positive PCR test between March 2nd and June 30th, 2020. Data was provided by the Health Evaluation and Quality Agency of Catalonia (AQuAS, https://aquas.gencat.cat/ca/actualitat/ultimes-dades-coronavirus/). Daily average (24 h), minimum and maximum ambient temperatures, absolute humidity and solar radiation levels from weather stations at each county capital city were provided by the Meteorological Service of Catalonia (MeteoCat, https://www.meteo.cat/). Conversely, solar radiation was not available for eight counties.
We also collected socioeconomic and demographic variables for each county in the last year, such as gross domestic product (GDP) per capita, population density, and proportion of population older than 65 years. Data was collected from the Statistical Institute of Catalonia (IDESCAT, https://www.idescat.cat/).
2.2. Design and statistical analysis
In a first stage, we conducted a geographical analysis at the county level. We evaluated the association between the meteorological variables and the cumulative incidence of COVID-19 using a Poisson regression model with robust sandwich standard errors to account for clustering within provinces [8]. All the regression models were adjusted for county-specific GDP, population density, and population older than 65 years. We evaluated the time-varying effects before (March 2nd to March 15th), during (March 16th to May 24th), and after (May 25th to June 15th) the lockdown periods fitting interaction terms with the meteorological variables.
In a second stage, we pooled the county data using a time-series design [9] to evaluate the short-term effects of meteorological variables on the daily incidence of COVID-19. Data was analyzed using a Poisson regression model allowing for features specific to the infectious disease context [10], such as residual autocorrelation, lagged effects and overdispersion. We used a random slope model adjusting for trend, weekdays, lockdown periods, and residual autocorrelation by fitting the logarithm of the lagged outcome [11]. Since the median incubation period for COVID-19 is over 5–6 days [12], we used a one week distributed lag model [13].
Estimated effects are reported as Relative Risk (RR), with 95% confidence interval (95% CI), for a unit increase in the meteorological variables. All the analyses were conducted using Stata Statistical Software, release 16 (StataCorp, TX, 2019).
3. Results
3.1. Geographical analysis
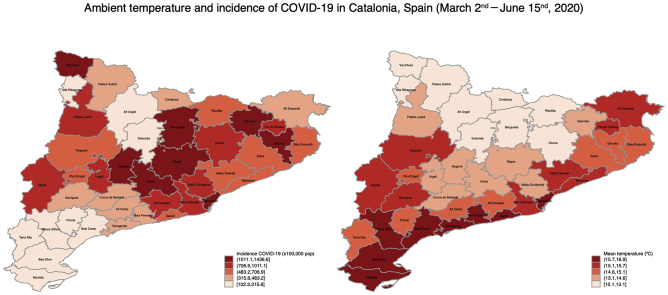
Fig. 1 shows the geographical distribution of the cumulative incidence of COVID-19 and the mean temperature before, during and after the lockdown periods. Before the lockdown, the average cumulative incidence was of 11.9 cases/100,000 (range from 0 to 96.9), and the mean temperature was of 10.9 °C (5.5 to 14.9). During the lockdown, the incidence raised to 602.5 (94.5 to 1290.2) decreasing afterwards during the post-lockdown period to 62.5 (0 to 446.8). While the mean temperature kept increasing during and after the lockdown periods; 13.9 °C (9.8 to 16.3) and 18.2 °C (13.2 to 20.8), respectively. Absolute humidity and solar radiation showed a pattern of increase during the periods before, during and after the lockdown similar to mean temperature (Appendix Fig. A.2) with average values for absolute humidity of 6.8 g/m3 (4.6 to 8.1), 9.1 g/m3 (6.3 to 10.9) and 11.4 g/m3 (8.0 to 13.5), and solar radiation of 14.8 MJ/m2 (12.3 to 16.1), 18.0 MJ/m2 (16.2 to 19.3) and 23.9 MJ/m2 (18.2 to 27.2), respectively.
Fig. 1.
Geographical distribution of the cumulative incidence of COVID-19 (per 100,000 pop.) and mean temperature (°C) for the 42 counties in Catalonia, before, during, and after the lockdown periods.
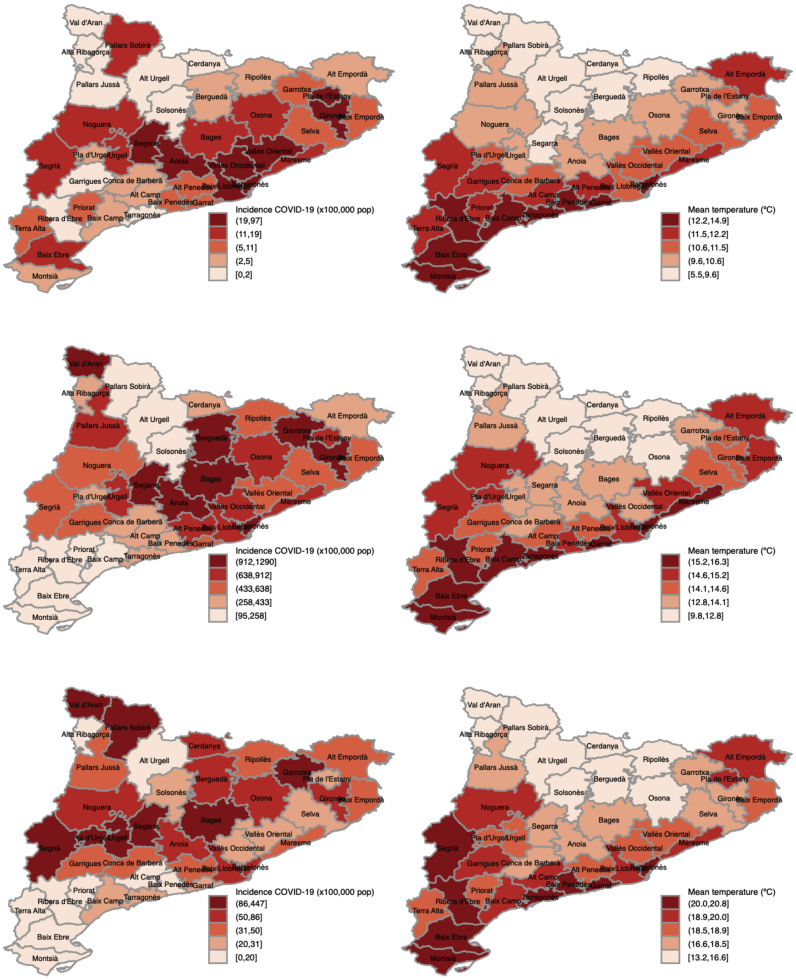
Mean temperature and absolute humidity are associate with the reduction of the cumulative incidence of COVID19. An average increase of 1 °C in mean temperature shows an significant reduction of 20% (RR = 0.79, 95% CI = [0.73, 0.85]) in the incidence, while an increase of 1 g/m3 in absolute humidity shows a reduction in the incidence of nearly 35% (RR = 0.62, 95% CI = [0.54, 0.71]). Solar radiation is also associated with a reduction of 10% (RR = 0.90, 95% CI = [0.73, 1.11]) in the incidence of COVID-19, although it was not statistically significant; however, we should acknowledge that data on solar radiation was not available for nine counties. The pattern of these associations did not change substantially before, during and after the lockdown periods (Fig. 2).
Fig. 2.
Geographical association between meteorological factors and the cumulative incidence of COVID-19 in Catalonia, before, during, and after the lockdown periods.
3.2. Time-series analysis
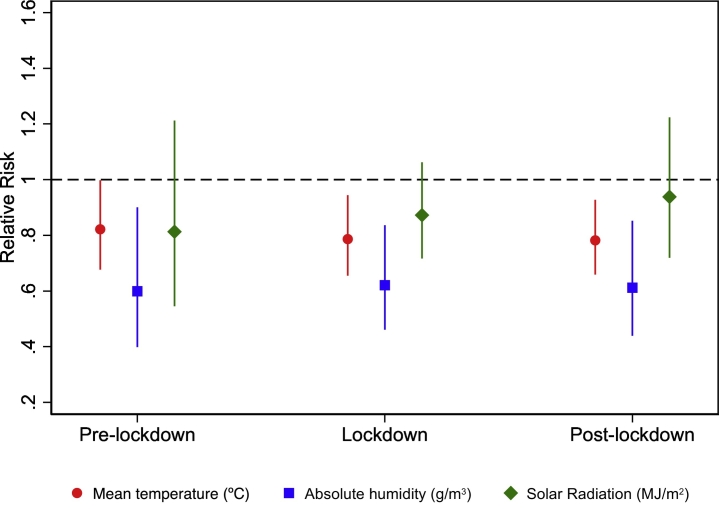
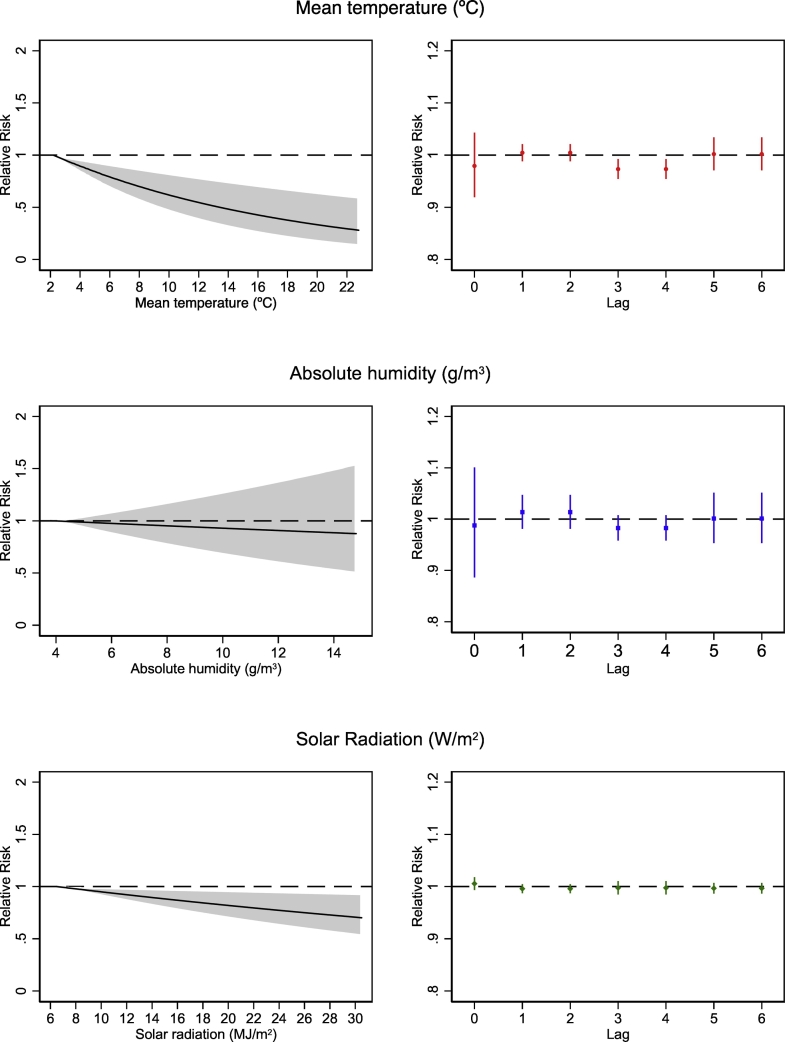
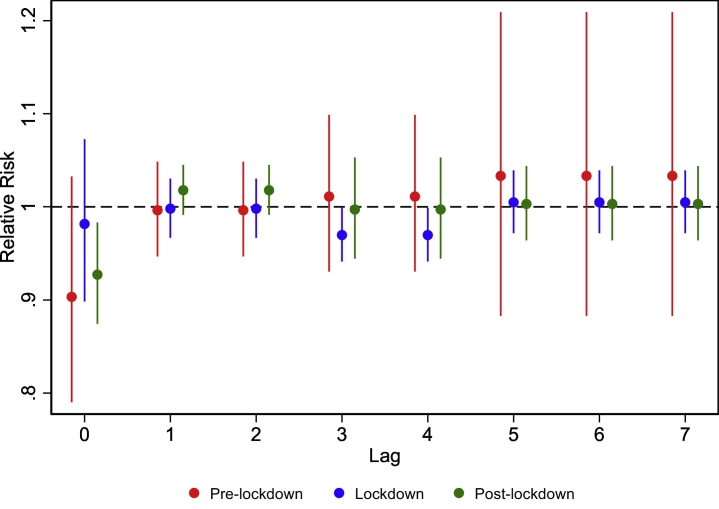
Fig. 3 (left panel) shows the cumulative effects, up to one week, of meteorological variables on the daily incidence of COVID-19. We evaluated the linearity of the associations without observing evidence of departure from linearity (Appendix Fig. A.4). The incidence decreased significantly by −6% (RR = 0.94, 95% CI = [0.85, 1.04]) for a rise of 1 °C of daily mean temperature, −1.2% (RR = 0.99, 95% CI = [0.85, 1.04]) for a rise of 1 g/m3 of absolute humidity, and − 1.5% (RR = 0.98, 95% CI = [0.97, 1.02]) for a rise of 1 MJ/m2 of solar radiation. Looking at the specific lagged effects (Fig. 3, right panel) the incidence decreased significantly by −2.7% (RR = 0.97, 95% CI = [0.95, 0.99]) for a rise of 1 °C of daily mean temperature at lags 3 to 4, and by −1.7% (RR = 0.98, 95% CI = [0.96, 1.01]) for a rise of 1 g/m3 of absolute humidity also at lags 3 to 4. Solar radiation shows a consistent negative association from lags 1 to 6, although it was not significant. Mean temperature show a similar pattern before and after the lockdown periods, with immediate effects observed at lag 0 (Fig. 4). While during the lockdown the largest effects are observed at lags 3 and 4. The pattern for absolute humidity and solar radiation did not change substantially before, during and after the lockdown periods.
Fig. 3.
Association between meteorological factors and daily incidence of COVID-19 (left panel), and their lagged effects on daily incidence of COVID-19 in Catalonia (right panel).
Fig. 4.
Lagged effects of mean temperature (°C) on daily incidence of COVID-19 in Catalonia before, during, and after the lockdown periods.
4. Discussion
We found a geographical association between meteorological factors and the cumulative incidence of COVID-19 in Catalonia, from early March to the end of June 2020, and a lesser extent in the short-term on the daily incidence during the first wave of the epidemic in Spain.
The cumulative incidence during the study period in Catalonia (822 cases per 100.000 people) was larger than in the neighborhood regions of Aragon (492), at the west, and Valencia (244), at the south [14]. To our knowledge, no other studies have yet been carried out on the impact of meteorological factors on the incidence of COVID-19 in the regions bordering Catalonia or nationwide in Spain.
At the geographical level, we observed that the cumulative incidence was lower in those counties with higher temperature and absolute humidity, and remained constant before, during and after the lockdown periods. These findings are in agreement with the evidence recently summarized in two systematic reviews [4,15]. The spread of COVID-19 may be influenced by temperature and humidity. Warmer and humid climates may show less transmission of the SARS-CoV-2 virus. Although most of the studies used daily mean temperature, there is a discordance on the use of humidity [4,14]. Relative humidity depends strongly on temperature and atmospheric pressure. An invariable amount of water vapour in the air will give very different relative humidity values during the daytime. In springtime, most of the study period, the thermic amplitude is higher than 20 °C. We estimated that relative humidity would be less representative than absolute humidity related to the amount of water per volume unit under these conditions. However, the quality of the evidence was low due to the observational design of the studies and the inherent risk of bias [15]. Moreover, meteorological variables alone could not explain most of the variability in disease transmission [5], but in many of the reviewed studies, non-meteorological factors have not been taken into account properly. In our study, temperature and absolute humidity have been associated with the incidence of COVID-19 independently from demographic and socioeconomic factors after adjusting for county-specific GDP, population density and population older than 65 years. Likewise, counties with lower income were associated with higher incidence of COVID-19, which is in agreement with previous published studies in Catalonia [16,17].
At the temporal level, we observed lagged effects of 3–4 days on the daily incidence COVID-19, mainly for temperature. The results observed before and after the lockdown periods suggest a larger immediate effect, at lag 0, similar to that reported in our previous study in the city of Barcelona [7]. Hence, temperature could play a specific role in reducing the daily incidence of COVID-19 at the short-term. However, during the lockdown period, the effect is delayed to 3–4 days, and being substantially small. This could suggest that the effect of temperature was modulated by the restrictive measures implemented by the Spanish Government to reduce the incidence of COVID-19 during the lockdown period. However, these results should be interpreted with caution due to the small number of days in each period. Only a small part of the reviewed studies have evaluated the short-term effects of meteorological factors on the daily incidence of COVID-19 [4,15], and none has accounted for features specific to the infectious disease context [10,18]. In our analysis we have carefully considered the autocorrelation by disease transmission fitting the logarithm of the lagged outcome [11]; a plausible lag structure using a one week distributed lag model since the median incubation period for COVID-19 is over 5–6 days [12]; association patterns evaluating departure from linearity, and; accounted for over dispersion.
The transmission mechanisms of viral infections, such as influenza [1,2], and other coronaviruses, such as SARS-CoV-1 [19,20] and MERS-CoV [21], have already shown that hot and humid climates decrease the viability of these viruses. Low temperature and humidity have a high viral stability, and respiratory droplets and aerosols, as containers of viruses, remain in suspension longer in dry air [22], and can also demote the hosts immunity and make them more susceptible to the virus [23]. In our study, we showed it is difficult to characterize at the temporal level the local temperatures and humidity conditions associated with the virus spread. However, it seems more affordable to determine at the geographical level the type of climate conditions in the counties where transmission is occurring. The spread of the epidemic is too complex to be explained solely about climatic conditions. Demographic and socioeconomic factors, and public health interventions including social distancing, use of mask, and personal hygiene conditions can modify the spread of COVID-19 and modulate the effect of meteorological factors. For this reason, we cannot assure that the effects we found in this study are direct or indirect or, more likely, a combination of both. In this sense, it is possible that in periods of non-confinement (before and after the lockdown), the higher the temperature, the greater the probability that people will leave their homes, and the lower the probability they will become infected when being outdoors. However, we should also consider the limitation of using a single weather station as a proxy for a whole county and the data accuracy, the timing of, or delay in, reporting COVID-19 cases during the evolutionary phases of the pandemic between counties [24,25].
Therefore, scientific evidence about the contribution of environmental factors in the spread of COVID-19 is needed, in combination with an understanding of the role demographic and socioeconomic factors and public health interventions [25]. It is necessary to contextualize these findings considering the spread of COVID-19. Seasonal effects of meteorological variables will be more evident in subsequent years. Ecological studies based on geographical and temporal aggregations are relatively simple to carry out because of global data availability on COVID19 [26,27]. However, since they are prone to confounding with a high risk of bias, and due to the urgent need to search for immediate answers to contain the pandemic, some of the earlier published studies contributed more to noise than to epidemiological evidence [4,15]. Epidemiological studies for research on COVID-19 should rely on multi-level investigations with appropriate study designs to provide robust scientific evidence [28]. Multiple environmental factors and appropriate spatial and temporal resolution need to be carefully investigated, jointly with demographic and socioeconomic factors, and public health interventions during the evolutionary phases of the COVID-19 pandemic. They should also account the differences and accuracy in the COVID-19 case definitions [24], and data availability between and within geographical settings, and with time [25].
5. Conclusion
Our findings suggest that warm and wet climates may reduce the incidence of COVID-19 in Catalonia during the first wave of the epidemic in Spain. However, further studies will need to consider population movement from locations with a high incidence, population susceptibility, and surveillance for respiratory infections. Meanwhile, health authorities must interpret with caution any COVID-19 risk predictions based on climate information alone.
Authors' contributions
All authors contributed to the conception and design of the research. TM and MR collected the data. AT conducted the statistical analysis and drafted the manuscript. TM, MR and MS reviewed the manuscript critically. All authors read and approved the final version of the manuscript and agreed to be accountable for all aspects of the work.
Funding
MS appreciates the funding from SUPERA COVID19 Fund, from SAUN (Santander Universidades), CRUE and CSIC; as well as from Pfizer Global Medical Grants. The funding sources did not participate in the design or conduct of the study, the collection, management, analysis, or interpretation of the data, or the preparation, review, or approval of the manuscript.
Declaration of Competing Interest
The authors declare is no conflict of interest.
Acknowledgements
AT and MS developed this study within the Observatory Big Data for the Prevention of Epidemics in Catalonia. It was presented at the international virtual symposium on Climatological, Meteorological and Environmental factors in the COVID-19 Pandemic (World Meteorological Organisation, 4-6 August 2020). We acknowledge the anonymous reviewers for their detailed comments to help us reach a broader audience.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.onehlt.2021.100239.
Appendix A. Supplementary data
Supplementary material 1
References
- 1.Moriyama M., Hugentobler W.J., Iwasaki A. Seasonality of respiratory viral infections. Annu Rev Virol. 2020 Sep 29;7(1):83–101. doi: 10.1146/annurev-virology-012420-022445. 32196426 (Epub 2020/03/21) [DOI] [PubMed] [Google Scholar]
- 2.Hemmes J.H., Winkler K.C., Kool S.M. Virus survival as a seasonal factor in influenza and poliomylitis. Antonie Van Leeuwenhoek. 1962;28:221–233. doi: 10.1007/BF02538737. 13953681 (Epub 1962/01/01) [DOI] [PubMed] [Google Scholar]
- 3.Virtual Symposium on Climatological, Meteorological and Environmental (CME) Factors in the COVID-19 Pandemic. 4–6 August 2020. [Google Scholar]
- 4.Smit A.J., Fitchett J.M., Engelbrecht F.A., Scholes R.J., Dzhivhuho G., Sweijd N.A. Winter is coming: a southern hemisphere perspective of the environmental drivers of SARS-CoV-2 and the potential seasonality of COVID-19. Int. J. Environ. Res. Public Health. 2020 Aug 5;17(16) doi: 10.3390/ijerph17165634. (PubMed PMID: 32764257. PMCID: PMC7459895. Epub 2020/08/09) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Reilly K.M., Auzenbergs M., Jafari Y., Liu Y., Flasche S., Lowe R. Effective transmission across the globe: the role of climate in COVID-19 mitigation strategies. Lancet Planetary Health. 2020;4(5) doi: 10.1016/S2542-5196(20)30106-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soares P.M.M., Cardoso R.M., Miranda P.M.A., de Medeiros J., Belo-Pereira M., Espirito-Santo F. WRF high resolution dynamical downscaling of ERA-Interim for Portugal. Clim. Dyn. 2012;39(9–10):2497–2522. [Google Scholar]
- 7.Tobías A., Molina T. Is temperature reducing the transmission of COVID-19? Environ. Res. 2020 doi: 10.1016/j.envres.2020.109553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bertanha M., Moser P. Spatial errors in count data regressions. J. Econometric Methods. 2016;5(1) [Google Scholar]
- 9.Bhaskaran K., Gasparrini A., Hajat S., Smeeth L., Armstrong B. Time series regression studies in environmental epidemiology. Int. J. Epidemiol. 2013 Aug;42(4):1187–1195. doi: 10.1093/ije/dyt092. (PubMed PMID: 23760528. PMCID: PMC3780998. Epub 2013/06/14) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Imai C., Armstrong B., Chalabi Z., Mangtani P., Hashizume M. Time series regression model for infectious disease and weather. Environ. Res. 2015 Oct;142:319–327. doi: 10.1016/j.envres.2015.06.040. (PubMed PMID: 26188633. Epub 2015/07/21) [DOI] [PubMed] [Google Scholar]
- 11.Brumback B.A., Ryan L.M., Schwartz J.D., Neas L.M., Stark P.C., Burge H.A. Transitional regression models, with application to environmental time series. J. Am. Stat. Assoc. 2000;95(449) [Google Scholar]
- 12.Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported Confirmed Cases: Estimation and Application. Ann. Intern. Med. 2020 May 5;172(9):577–582. doi: 10.7326/M20-0504. (PubMed PMID: 32150748. PMCID: PMC7081172. Epub 2020/03/10) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gasparrini A., Armstrong B., Kenward M.G. Distributed lag non-linear models. Stat. Med. 2010 Sep 20;29(21):2224–2234. doi: 10.1002/sim.3940. (PubMed PMID: 20812303. PMCID: PMC2998707. Epub 2010/09/03) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Valls J., Tobias A., Satorra P., Tebe C. COVID19-Tracker: a shiny app to analise data on SARS-CoV-2 epidemic in Spain. Gac. Sanit. 2021 Jan-Feb;35(1):99–101. doi: 10.1016/j.gaceta.2020.04.002. PubMed PMID: 32417117. PMCID: PMC7184003. Epub 2020/05/18. COVID19-Tracker: una aplicacion Shiny para analizar datos de la epidemia de SARS-CoV-2 en Espana. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mecenas P., Bastos R., Vallinoto A.C.R., Normando D. Effects of temperature and humidity on the spread of COVID-19: A systematic review. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0238339. (e0238339. PubMed PMID: 32946453. PMCID: PMC7500589. Epub 2020/09/19) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mari-Dell’Olmo M., Gotsens M., Pasarin M.I., Rodriguez-Sanz M., Artazcoz L., Garcia de Olalla P. Socioeconomic inequalities in COVID-19 in a european urban area: two waves, two patterns. Int. J. Environ. Res. Public Health. 2021 Jan 30;18(3) doi: 10.3390/ijerph18031256. (PubMed PMID: 33573323. PMCID: PMC7908269. Epub 2021/02/13) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saez M., Tobias A., Barcelo M.A. Effects of long-term exposure to air pollutants on the spatial spread of COVID-19 in Catalonia, Spain. Environ. Res. 2020 Dec;191:110177. doi: 10.1016/j.envres.2020.110177. (PubMed PMID: 32931792. PMCID: PMC7486876. Epub 2020/09/16) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Imai C., Hashizume M. A systematic review of methodology: time series regression analysis for environmental factors and infectious diseases. Trop Med Health. 2015 Mar;43(1):1–9. doi: 10.2149/tmh.2014-21. (PubMed PMID: 25859149. PMCID: PMC4361341. Epub 2015/04/11) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chan K.H., Peiris J.S., Lam S.Y., Poon L.L., Yuen K.Y., Seto W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv Virol. 2011:734690. doi: 10.1155/2011/734690. (PubMed PMID: 22312351. PMCID: PMC3265313. Epub 2012/02/09) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yuan J., Yun H., Lan W., Wang W., Sullivan S.G., Jia S. A climatologic investigation of the SARS-CoV outbreak in Beijing, China. Am. J. Infect. Control. 2006 May;34(4):234–236. doi: 10.1016/j.ajic.2005.12.006. (PubMed PMID: 16679182. PMCID: PMC7115332. Epub 2006/05/09) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Altamimi A., Ahmed A.E. Climate factors and incidence of Middle East respiratory syndrome coronavirus. J Infect Public Health. 2020 May;13(5):704–708. doi: 10.1016/j.jiph.2019.11.011. (PubMed PMID: 31813836. PMCID: PMC7102558. Epub 2019/12/10) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lowen A.C., Steel J. Roles of humidity and temperature in shaping influenza seasonality. J. Virol. 2014 Jul;88(14):7692–7695. doi: 10.1128/JVI.03544-13. (PubMed PMID: 24789791. PMCID: PMC4097773. Epub 2014/05/03) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kudo E., Song E., Yockey L.J., Rakib T., Wong P.W., Homer R.J. Low ambient humidity impairs barrier function and innate resistance against influenza infection. Proc. Natl. Acad. Sci. U. S. A. 2019 May 28;116(22):10905–10910. doi: 10.1073/pnas.1902840116. (PubMed PMID: 31085641. PMCID: PMC6561219. Epub 2019/05/16) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pearce N., Vandenbroucke J.P., VanderWeele T.J., Greenland S. Accurate statistics on COVID-19 are essential for policy guidance and decisions. Am. J. Public Health. 2020 Apr;23:e1–e3. doi: 10.2105/AJPH.2020.305708. 32324422 (Epub 2020/04/24) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zeka A., Tobias A., Leonardi G., Bianchi F., Lauriola P., Crabbe H. Responding to COVID-19 requires strong epidemiological evidence of environmental and societal determining factors. Lancet Planetary Health. 2020;4(9) doi: 10.1016/S2542-5196(20)30169-8. e375-e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xu B., Gutierrez B., Mekaru S., Sewalk K., Goodwin L., Loskill A. Epidemiological data from the COVID-19 outbreak, real-time case information. Sci Data. 2020 Mar 24;7(1):106. doi: 10.1038/s41597-020-0448-0. (PubMed PMID: 32210236. PMCID: PMC7093412. Epub 2020/03/27) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pekkanen J., Pearce N. Environmental epidemiology: challenges and opportunities. Environ. Health Perspect. 2001 Jan;109(1):1–5. doi: 10.1289/ehp.011091. (PubMed PMID: 11171517. PMCID: PMC1242043. Epub 2001/02/15) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 1