Abstract
The tracheal cartilaginous sleeve (TCS) is a rare, difficult to diagnose airway malformation in which segmented tracheal rings are replaced by a solid sheath of cartilage. TCS is a significant cause of morbidity and mortality in patients with syndromic craniosynostosis, and early diagnosis is essential. We report a case in which ultrasound (US) was used to diagnose TCS in a patient with Pfeiffer syndrome. This is the first case demonstrating the use of US as the initial tool to diagnose TCS. The case supports ongoing research investigating the use of US as a screening and diagnostic imaging modality for TCS.
Keywords: Craniosynostosis, Pfeiffer syndrome, Trachea, Tracheal cartilaginous sleeve, Ultrasound
1. Introduction
The tracheal cartilaginous sleeve (TCS) is a rare, life threatening and difficult to diagnose airway malformation which results from vertical fusion of the tracheal cartilaginous rings, with an intact membranous tracheal wall posteriorly. This results in a ‘C’ shaped sheath of solid cartilage anteriorly and laterally along the trachea. The anomaly results in altered airway protective mechanisms and increases the risk for pulmonary complications. Most children with TCS have syndromic craniosynostosis, such as Pfeiffer, Crouzon, Apert and Beare-Stevenson syndromes [1]. TCS is traditionally diagnosed via rigid bronchoscopy or at the time of tracheostomy. The diagnosis can be difficult to make on bronchoscopy and requires a very high index of suspicion. TCS cannot be diagnosed using computed tomography (CT) or magnetic resonance imaging (MRI) as neither of these modalities enable accurate visualization of tracheal cartilage. Ultrasound (US) is non-invasive and eliminates the risks of ionizing radiation and anesthesia associated with other imaging modalities and endoscopic airway evaluation. The use of ultrasound to diagnose TCS was described in one recent case report; in which US was performed in a 2-month-old after suspicion for TCS had been raised on bronchoscopy [2]. In this report, we describe the use of US as the initial tool to diagnose TCS in a newborn with Pfeiffer syndrome.
2. Case presentation
A newborn female with Pfeiffer syndrome (FGFR2 variant NM_000141.4:p.Tryp290Cys (W290C)), was intubated immediately after birth due to acute hypoxic and hypercarbic respiratory failure and admitted to the neonatal intensive care unit. CT of the head revealed syndromic multi-sutural synostosis, skull base hypoplasia, midface hypoplasia, nasal and choanal stenosis, and external auditory canal stenosis. There was concern for TCS given the patient’s high-risk genotype, so US of the neck was performed by the Pediatric Radiology team on hospital day 6. A small-footprint linear 15 mHz transducer (“hockey stick”) was employed. The patient had been placed on spinal precautions due to congenital segmentation anomalies. The precautions limited cervical mobility and access and lead to the choice of the small-footprint linear transducer. US demonstrated diffusely thickened anterior tracheal cartilage without identifiable normal cartilaginous rings, suggesting a complete TCS (Fig. 1). On hospital day 26, the patient was taken to the operating room for endoscopic airway evaluation to aid in determining an airway management plan. Micro direct laryngoscopy and bronchoscopy were notable for a narrow hypopharynx, enlarged arytenoid cartilages and vocal fold granulation tissue. Significant redundancy of posterior tracheal wall mucosa was noted, and no clear cartilaginous rings were appreciated from subglottis to carina (Fig. 2). Given the diagnosis of TCS, the patient’s severe multi-level airway obstruction associated with midface hypoplasia and the endoscopic findings described above, as well as institutional experience with the W290C genotype, the decision was made to not extubate and to proceed with definitive airway intervention via tracheostomy. The patient underwent tracheostomy on hospital day 35 with the Pediatric Otolaryngology service, and the TCS diagnosis was confirmed during the procedure (Fig. 3).
Fig. 1. Tracheal cartilaginous sleeve on ultrasound.
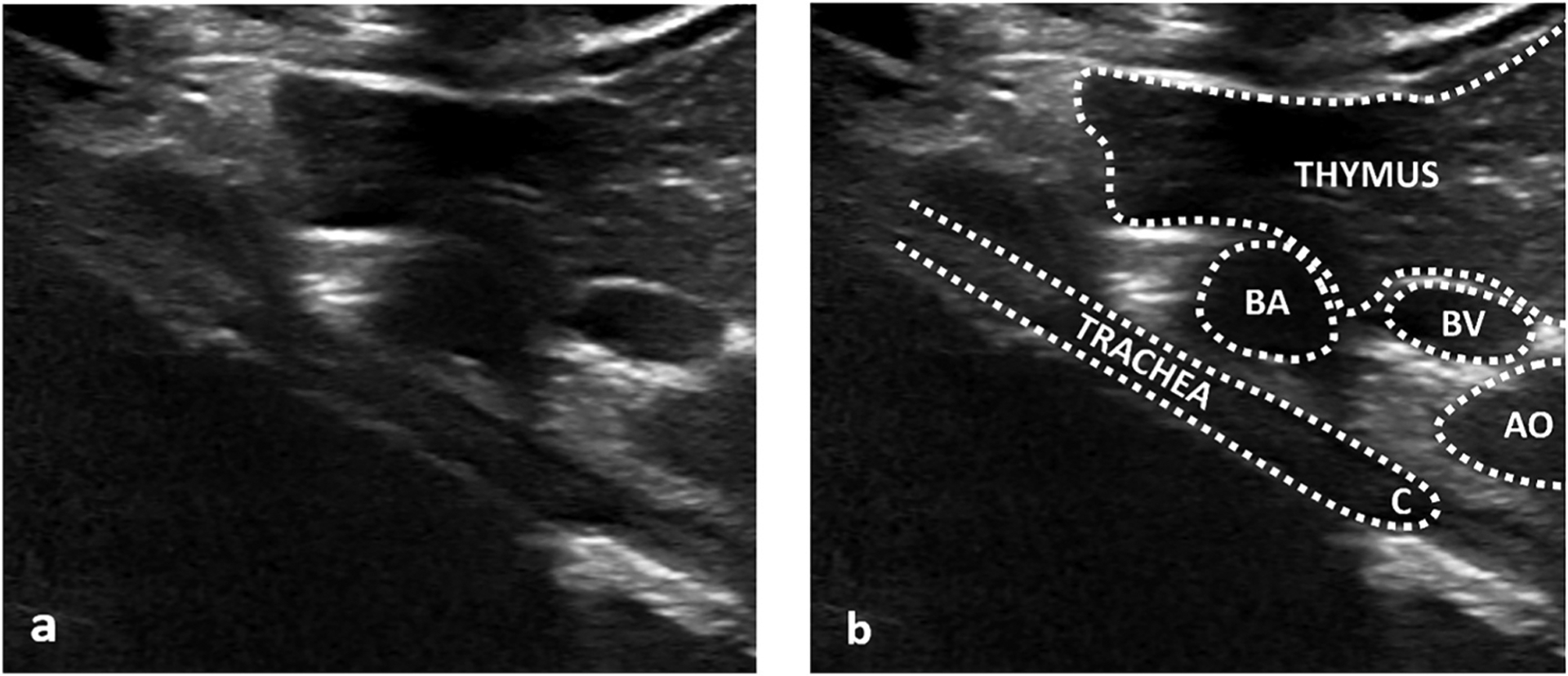
Unlabeled (a) and labeled (b) longitudinal ultrasound images from a right parasternal approach and thymic window showing the abnormal trachea (TRACHEA) as a thick, unsegmented structure in the central mediastinum, ending at the carina (C). Nearby thymus (THYMUS) and vascular structures (BA – brachiocephalic artery, BV – left brachiocephalic vein, AO – aortic arch) are labeled for anatomic orientation. Shadowing deep to the trachea is expected due to the air column. A right parasternal approach is recommended to avoid confusing a gas filled esophagus (not shown) with an unsegmented trachea as their appearance can be similar.
Fig. 2. Tracheal cartilaginous sleeve on endoscopy.
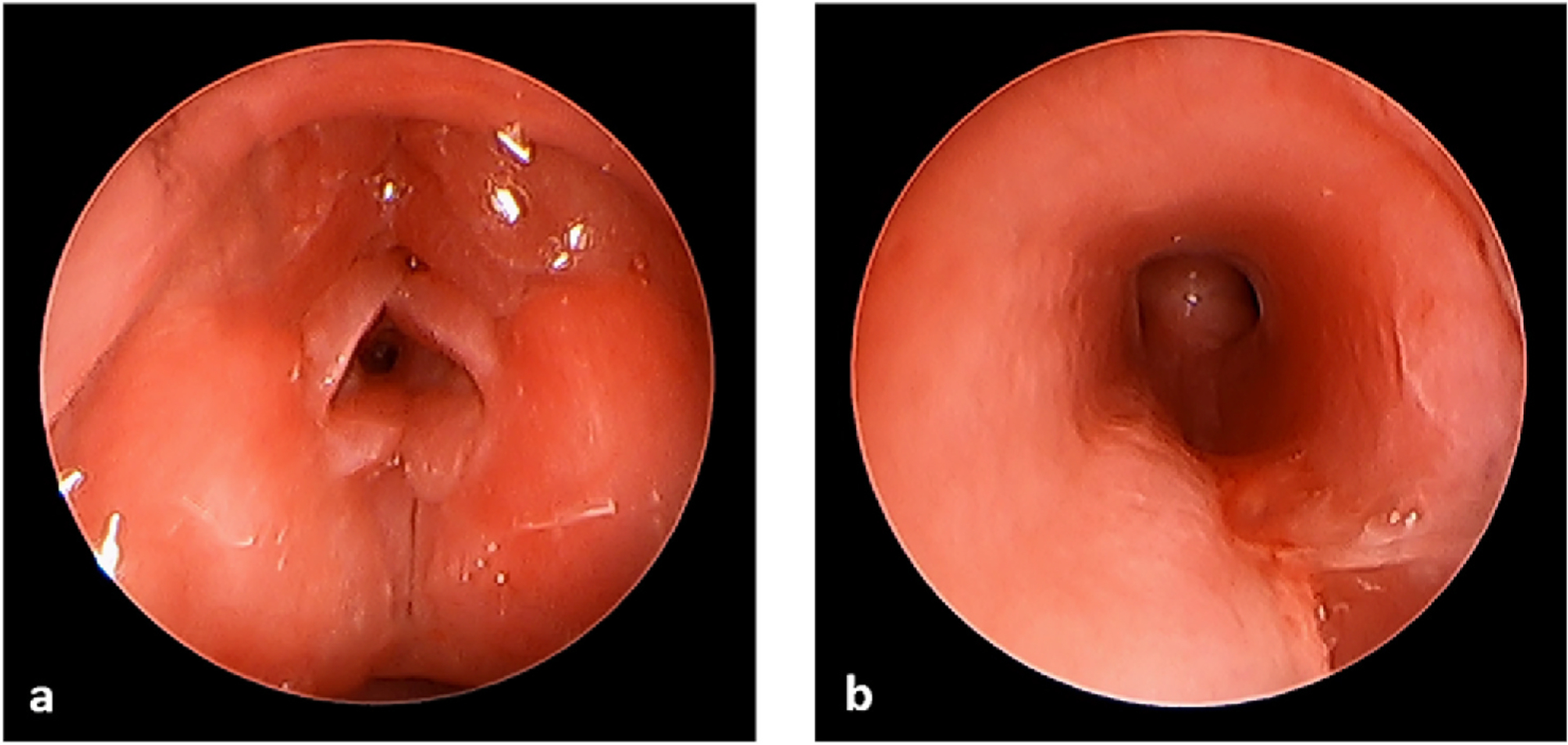
Images obtained during endoscopy showing enlarged arytenoid cartilages and vocal fold granulation tissue (a) and redundancy of posterior tracheal wall mucosa without clear cartilaginous rings throughout the trachea (b).
Fig. 3. Tracheal cartilaginous sleeve on tracheostomy.
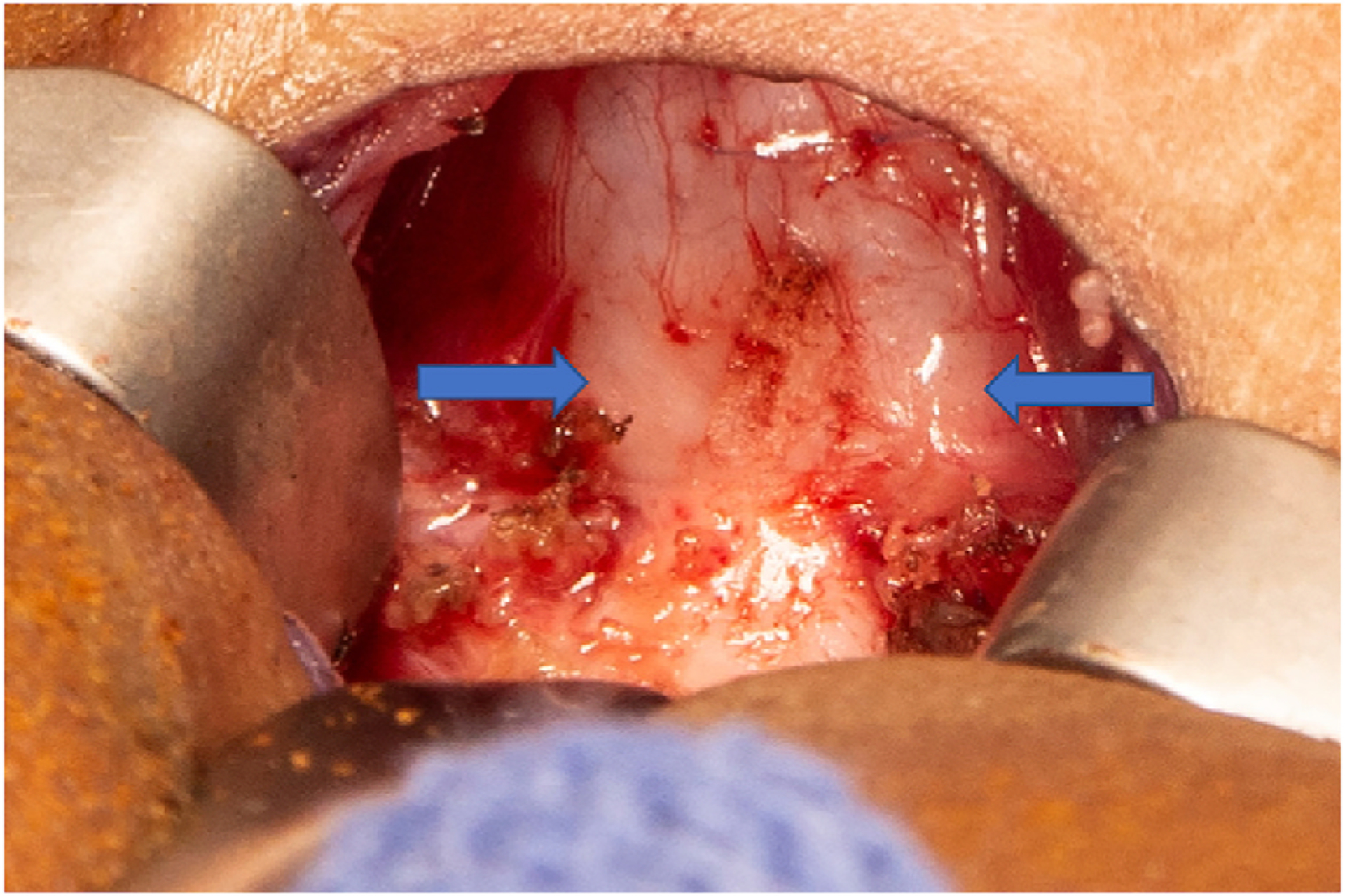
Intraoperative image obtained during tracheostomy placement. Arrows outline the trachea. A continuous tracheal cartilaginous sleeve is present without individual tracheal rings. The strap muscles are retracted laterally.
Written permission to publish this case report was obtained from the patient’s parent per institutional guidelines.
3. Discussion
TCS is an uncommon airway anomaly in which there is absence of normal tracheal ring segmentation. Vertical fusion of the tracheal rings results in a solid sheath of cartilage along the anterior and lateral trachea, restricting the ability of the trachea to increase in size with normal growth. This limitation on tracheal development may cause airway stenosis, which increases the risk of sudden death in the event of tracheal occlusion. Increased tracheal rigidity and narrowing are also believed to alter airflow dynamics and impair normal airway protective mechanisms.
Almost all patients with TCS have a craniosynostosis syndrome and TCS is a significant source of morbidity and mortality in these children. A recent study by Wenger et al. reported a prevalence of 22% in children with syndromic craniosynostosis and a study by Pickrell et al. found an 80% incidence of at least partial tracheal ring fusion [1,3]. The condition is life-threatening with a high mortality rate if not treated with tracheostomy. A meta-analysis by Lertsburapa et al. included all published cases of TCS and found a 90% risk of death by the age of 2 years without tracheostomy [4]. These studies highlight the critical importance of screening for and diagnosing TCS early so that definitive airway management via tracheostomy may be performed in a timely manner.
When diagnosed prior to tracheostomy, TCS is usually diagnosed on bronchoscopy. Bronchoscopic airway evaluation in these cases is often limited by inflammation or abnormalities in the overlying mucosa which alter the ability to visualize tracheal ring topography; thus requiring a high level of clinical suspicion to make the TCS diagnosis. Bronchoscopy also involves significant risks associated with general anesthesia, particularly in this patient population. Radiologic imaging could provide a non-invasive, safe way to screen for TCS. CT and MRI have previously been utilized for airway architecture evaluation, however these modalities do not allow for adequate visualization of tracheal cartilage. Other considerable drawbacks include high cost, prolonged image acquisition time (MRI), need for sedation, and ionizing radiation exposure (CT) [5]. Ultrasound has significant advantages including lower cost, greater portability, and elimination of the risks of ionizing radiation and general anesthesia. US has higher spatial resolution when evaluating small, superficial structures and has previously been successfully utilized to evaluate tracheal ring topography in cystic fibrosis [5]. Prior to the present report, ultrasonographic diagnosis of TCS had been described only once, and was performed in a 2-month-old after suspicious findings for TCS were noted on bronchoscopy [2]. While the prior case established that US could be used to diagnose TCS, the present report demonstrates the use of US for early screening and initial diagnosis of TCS in a high-risk infant on day 6 of life. The diagnosis was then confirmed on endoscopic airway evaluation and on tracheostomy.
In this case, a small-footprint linear 15 mHz transducer was utilized, though probe selection should be at the discretion of the imager based on image quality and anatomic requirements. Ideally, both cervical tracheal images and mediastinal tracheal images in longitudinal and transverse axes should be acquired. Images from a parasternal approach with a thymic window allow for deeper mediastinal evaluation and right parasternal images avoid confusion with the esophagus, assuming normal esophageal situs. Transverse cine image sweep can be helpful to assess for rings in both cervical and mediastinal images.
We propose US as a non-invasive, safe and effective method for the initial diagnosis of TCS and suggest that US may be used to screen patients at high risk for the condition. Further research to investigate US as a tool for screening and diagnosis of TCS is warranted.
4. Conclusion
TCS is a life threatening, under recognized, and difficult to diagnose airway anomaly associated with craniosynostosis syndromes. Early diagnosis and management of this condition are essential. US evaluation of the airway may provide an effective and noninvasive way to screen for and diagnose TCS.
Funding
Dr. Lam is supported by National Institute on Deafness and Other Communication Disorders, USA, T-32 DC000018, Research Training in Otolaryngology..
Footnotes
Declaration of competing interest
The authors have no financial relationships, or conflicts of interest to disclose.
References
- [1].Wenger TL, Dahl J, Bhoj EJ, Rosen A, Mcdonald-Mcginn D, Zackai E, Jacobs I, Heike CL, Hing A, Santani A, Inglis AF, Sie KCY, Cunningham M, Perkins J, Tracheal cartilaginous sleeves in children with syndromic craniosynostosis, Genet. Med 19 (2017) 62–68, 10.1038/gim.2016.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Wanner MR, Marine MB, Dahl JP, Ultrasound diagnosis of tracheal cartilaginous sleeve in a patient with Pfeiffer syndrome, Pediatr. Radiol 48 (2018) 1814–1816, 10.1007/s00247-018-4207-8. [DOI] [PubMed] [Google Scholar]
- [3].Pickrell BB, Meaike JD, Canãdas KT, Chandy BM, Buchanan EP, Tracheal cartilaginous sleeve in syndromic craniosynostosis: an underrecognized source of significant morbidity and mortality, J. Craniofac. Surg 28 (2017) 696–699, 10.1097/SCS.0000000000003489. [DOI] [PubMed] [Google Scholar]
- [4].Lertsburapa K, Schroeder JW, Sullivan C, Tracheal cartilaginous sleeve in patients with craniosynostosis syndromes: a meta-analysis, J. Pediatr. Surg 45 (2010) 1438–1444, 10.1016/j.jpedsurg.2009.09.005. [DOI] [PubMed] [Google Scholar]
- [5].Diwakar A, Adam RJ, Michalski AS, Tamegnon MM, Fischer AJ, Launspach JL, Horan RA, Kao SC, Chaloner K, Meyerholz DK, Stoltz DA, Sonographic evidence of abnormal tracheal cartilage ring structure in cystic fibrosis, in: Laryngoscope, John Wiley and Sons Inc., 2015, pp. 2398–2404, 10.1002/lary.25255. [DOI] [PMC free article] [PubMed] [Google Scholar]


