Abstract
Properly performing minimally invasive colorectal procedures requires specific skills. With a focus on patient safety, the training of surgeons on patients is only accepted under exceptionally controlled, expensive, and challenging conditions. Moreover, many new techniques in colorectal surgery have been developed. Therefore, undertaking minimally invasive colorectal surgery in modern times requires specific psychomotor skills that trainee surgeons must gather in less time. In addition, there are not enough proctors with sufficient expertise for such an expressive number of new different techniques likes transanal and robotic procedures.
Studies that have demonstrated an improvement in minimally invasive surgery skills to the actual operating room in general surgery and a stepwise approach to surgical simulation with a combination of various training methods appears to be useful in colorectal surgery training programs. However, the scientific evidence on the transfer of skills specifically for colorectal surgery is extremely scarce and very variable. Thus, the evaluation of the results remains quite difficult. In this review, we present the best available evidence on the types of training based on simulation, their characteristics, advantages and disadvantages, and finally the results available on their adoption. Nevertheless, scientific evidence about the benefit of simulation training in minimally invasive colorectal surgery is limited and there is a need to build more robust evidence.
Keywords: surgical simulation, colorectal surgery, minimally invasive colorectal surgery, robotic colorectal surgery
Advances in science and technology have led to changes in established procedures and the introduction of entirely new and less invasive operations or access routes in colorectal surgery. However, at the beginning of their training, surgeons inexperienced in techniques of recent introduction, even when adequately supervised, can make mistakes. As a result, if concrete steps to ensure patient safety have not been undertaken, the entire process of introducing new technologies can be put at risk. In this sense, the role of simulation-based training is very attractive and increasingly important. 1
Traditionally, in surgery and other medical specialties, the transfer of skills used to be done through a model where the surgeon in training played the role of an apprentice. This model, known in the United States and Europe as the William Halsted model (“see one, do one, teach one” method) introduced at Johns Hopkins University in 1889, served conventional surgery well for more than a century. 2 In that role, the apprentice surgeon observed the performance of the senior surgeon first and then performed the operation under supervision. However, this model depended entirely on outpatient and inpatient flows and on the senior surgeon surgical agenda. In addition, different procedures have different learning curves. Competent surgeons performing one procedure may not be as competent performing another one. So, how could senior surgeons possibly teach all?
Laparoscopic cholecystectomy resulted in a rupture with this traditional teaching model. A new condition was imposed: the need to acquire specific skills and in nothing similar to those practiced in conventional surgery. Moreover, surgeons who had already completed their training cycle and were in a teaching position also needed skills training. More than 20 years have passed since the introduction of laparoscopic cholecystectomy in the early 1990s when Eric Mühe and Philippe Mouret changed the face of surgery forever. Since then, randomized trials and meta-analyses have demonstrated superior immediate results of laparoscopic colectomy when compared with conventional surgery regarding immediate surgical outcomes. 3 Ultimately, results of noninferiority of laparoscopic colectomy in relation to the conventional approach regarding to oncological outcomes could also be demonstrated for the radical surgical treatment of colon 4 5 and rectal cancer. 6 7
Minimally invasive colectomy is a technically challenging procedure. The technical complexity is probably associated with the still relatively low adoption rate of minimally invasive (laparoscopic or robotic) colectomy when compared with other minimally invasive operations like cholecystectomy or fundoplication. 8 In addition, trainee surgeons need to acquire more sophisticated technical skills in less time and often supervised by senior surgeons eventually unfamiliar with too many new minimally invasive procedures in colorectal surgery—single-port laparoscopy colectomy, natural orifice transluminal endoscopic surgery, natural orifice specimen extraction, transanal endoscopic microsurgery, transanal minimally invasive surgery, transanal total mesorectal excision (TaTME), minimally invasive complete mesocolic excision, and multiport or single-site robotic colectomy.
Special surgical competencies are necessary to overcome technical difficulties associated to minimally invasive colorectal surgery. The challenges associated with undertaking a complete minimally invasive colectomy comes from the need for mobilizing a long bowel segment, dissecting and dividing large vessels, constructing a well-irrigated and tension-free intestinal anastomosis, and removing a large specimen through the smallest possible incision or through a natural orifice. As if it was not enough, these extremely complex steps shall be successfully executed in the case of conventional laparoscopy by using a technology attached to two-dimensional and unstable view, long nonarticulated instruments limited by a fixed entry point and limited (although not absent) tactile feedback. Furthermore, an elevated rate of adverse clinical outcomes at the beginning of the learning curve remains a concerning issue mainly because it is no longer accepted that surgeons acquire personal experience at the expense of patient safety. Ultimately, there is a significant financial cost associated with surgical training in the operating room. 9 Based on the considerations above, the minimally invasive surgical community decided to reshape training strategy to facilitate acquisition of the minimum skills set necessary for performing minimally invasive surgery mainly due to the fact that during a laparoscopic colectomy, the senior surgeons cannot directly guide the trainee's hands during the procedure. Therefore, it was of central importance to allow surgeons to acquire important skills outside of the operating room, aiming to a safe introduction of new techniques into surgical practice. Medical societies and international medical organizations, like the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) and the European Association of Endoscopic Surgeons, defined minimum requirements for surgical training before clinically performing minimally invasive surgery.
The strategies commonly used for transferring skills in minimally invasive surgery generally are divided into two phases: preclinical and clinical training. No matter what program the surgical trainee is enrolled (if residency or fellowship), the two phases can often be noticed. The preclinical phase includes the acquisition of theoretical knowledge, training in the dry laboratory (physical [box simulators] reality and virtual reality [VR] simulators) and in the wet laboratory (animal and human tissue). The clinical phase includes proctoring and mentoring.
Types of Simulation-Based Training
Box and Physical Reality Simulators
Box simulators represent the first gateway of simulation-based training. Very simply designed, they are a platform that includes a box with holes where there are inserted trocars, simulating an insufflated peritoneal cavity. Real laparoscopic instruments are used by the trainees and there is a camera that simulates the endoscope. In these simulators, training sessions can take place with the use of inanimate models of human organs like foam models (dry laboratory) or with surgical pieces of animals (wet laboratory). There are several basic tasks frequently conducted in the boxes 10 like transfer (plastic rings or small spheres can be transferred from one hand to another of the surgeon, or within one side of the operating field), cut (performing of a predetermined cut on a gauze pad to improve sense of depth and adequate use of traction and countertraction), endo-suture, and knotting. Box simulators provide tactile feedback and they are portable, relatively inexpensive, do not demand significant human resources, only the time of the trainee and the trainer. Practicing in a box simulator, though, lacks a clinical context and interactivity as in the operating room. The little association with the real world can lead to demotivation and less effort in the execution of the task or in its repetition, which ends up introducing a bias in the evaluation. Another disadvantage is that it enables the assessment of a limited skills set. Moreover, physical reality trainers require replacement of parts or models, hence leading to increasing costs. Ultimately, box trainers lack automated performance assessment, since the entire training supervising process demands a significant amount of time of senior surgeons.
One of the first results about skills transfer of skills to the operating room using a box trainer was published by Scott et al. 11 In this study, the hypothesis of training in a predetermined sequence of tasks would affect performance of surgical residents in laparoscopic operations. Twenty-two surgery residents were randomized to undergo skill training (30 minutes a day for 10 days) or not (control group). The study group practiced the tasks on the simulator an average of 138 times (94–171) while the control group did not practice any tasks. All research subjects underwent structured assessment using Objective Structured Assessment of Technical Skills 12 before and after training. Residents undergoing skills training improved in 4 of 8 criteria assessed by the tool (tissue handling, instrument handling, use of assistants, and overall performance). As expected, the only criterion that did not improve after training was knowledge about the surgery, as there was no theoretical content available in the study. The authors concluded by the significant improvement that can be expected from skills training on hand-eye coordination of junior residents and that such a training program should be included in residency program. Another important landmark work was conducted by Fried et al. 10 They have published the results of using a box simulator, the McGill Inanimate System for Training and Evaluation of Laparoscopic Skills (MISTELS) which was adopted by SAGES in its well-known Fundamentals of Laparoscopic Surgery program. In this study, 20 medical students from McGill University (Montreal, Canada) performed the intracorporeal and extracorporeal knots in the box. Then the students were randomized for training or not in the MISTELS of the transfer exercise. After four weekly sessions, the two groups of students were asked to repeat the intra- and extracorporeal knot tasks. There was a significant improvement in endo-suture ability for the group that was selected for training.
Over the years, the simple task repetition environment of the box simulators was replaced by the simulation of a specific anatomy such as the female pelvis or the thoracic cavity. This modification marks the appearance of the so-called physical reality simulators. In them, in addition to testing basic surgical skills, it was possible to simulate more structured operative times such as intestinal suture, anastomosis construction, and endo-stapling.
Virtual Reality Simulators
Until recently, VR simulators have been pointed out to have as a main disadvantage focusing on basic technical skills instead of full surgical procedures. This statement was true, but not anymore due to the development of new equipment.
VR simulators have undergone profound changes in the last years and are now able to provide a significant advantage over physical reality and animal/cadaver models. Computer-generated simulations are traditionally used by airline pilots and flight crews. 13 The term VR refers to a “computer-generated representation of an environment that allows sensory interaction, resulting in the impression of being really present.” 14 Despite its high initial cost, the advantages of the VR simulator are evident and include high fidelity, usability, and reproducibility for routine and risky technical maneuvers, maneuvers repetition without the need of additional preparation, low costs of maintenance and upgrades, complexity degree may be determined by trainee or senior, and availability of a built-in automated performance score and record.
In 1993, Richard Satava 15 first proposed the use of VR simulators in training in surgery and defined the five basic prerequisites of realistic simulation: fidelity (image must have sufficient resolution to appear real), object properties (organs and tissue must be deformed when touched and must fall by gravity), interactivity (surgeon's hand and the instrumental must have a realistic interaction with the organs), sensory input—return of touch, pressure must be felt by the user, and reactivity (organs must react properly to manipulation or cutting like bleeding or leaking fluids).
Construction validity is a fundamental feature of any type of simulator. Demonstrating the validity of constructing a model means verifying its ability to differentiate between novice and expert surgeons. 16 Some authors have demonstrated the construction validity of VR simulators. In 2001, Gallagher et al 17 tested this characteristic of one of the first available VR simulators, the Swedish MIST-VR. The performance evaluation in the simulator of the surgeons participating in the study allowed them to be properly differentiated so that the performance in the VR simulator proved to be a useful and objective tool in the assessment of psychomotor skills normally used in minimally invasive surgery.
In VR simulators, trainee surgeons can be guided through a series of training scenarios of progressive difficulty complexity. These scenarios include either a simulation of a box trainer where the basic skills can be trained or the more advanced theater of a full laparoscopic case like a sigmoid left colectomy. Therefore, trainee surgeons are allowed a step-by-step skill development as well as transition of competencies from training to clinical practice. In VR simulators, a comprehensive set of different basic procedures can be trained, including navigation, cutting, suturing, needle driving, energy (diathermy and ultrasonic), and stapler use. 3 In addition, VR simulators also provide automated performance assessment. This assessment derives from specific metrics recorded during the training. Examples of such metrics are task completion time, number of errors, and the virtual instruments' path length. Therefore, by utilizing validated metrics, VR simulators provide important feedback for their individual psychomotor and cognitive skills required for performing a real laparoscopic surgery.
Regarding laparoscopic surgery, it was already demonstrated that training in a VR simulator leads to improvement of performance during the execution of the considered simulator task. 18 19 Other authors have demonstrated that the achieved improved performance may be observed during a real laparoscopic task. 20 Ultimately, it has already been demonstrated that VR simulation-based practice leads to improvement of performance in the operating theater, which remains the sole and most important goal of a surgical simulation-based program. 21 It is a specific feature of VR simulators, the output of performance in technical skills according to built-in automated metrics. One important feature of VR simulation-based training in laparoscopic colorectal surgery, would be to know upfront, which simulator metrics are associated to a better performance for a specific procedure, such as a laparoscopic colectomy. With this purpose, surgeons novice to a laparoscopic colectomy underwent a single-session VR simulation training. 22 Next, they all performed a laparoscopic left colectomy in the swine. Operations were recorded and reviewed by two expert surgeons using a performance evaluation score specific to laparoscopic colectomy. Linear regression analysis was used to identify simulator metrics related to better score performance. It was observed that the VR simulator parameters strongly correlated with specific skills during laparoscopic colectomy in the swine model—the safe use of electrosurgery or energy device and the quality of the medial-to-lateral dissection. The good news is that not only a single VR simulation session in a specific clinical module is useful for novice surgeons to address their baseline skills, but this information may be useful in an attempt to tailor simulation-based practice according to a trainee surgeon needs.
Augmented Reality Simulators
Augmented (AR) or mixed reality refers to supplementing the real-world imaging provided to the surgeon by introducing virtual objects (holograms) which appear in coexistence with the ones from the real world. For an application to be characterized as AR, it must fulfill the following requirements: real and virtual objects must be combined in a common environment, the system must run interactively and in real time, and real and virtual objects must be spatially registered.
This occurs in real-time via a dedicated hardware and software. A basic AR method is to superimpose a hologram on a real-world image captured by a camera and displaying the combination of these on a computer/tablet/head-mounted (smart glasses) display. One of the key aspects of AR is that the surgeon does not have to look away from the surgical site. Furthermore, using AR enables visualizing structures such as major vessels and nerves or other vital tissues. Another important functionality is the ability to control the opacity of displayed objects. Ultimately, it is possible to utilize voice or gesture recognition to create enabling hands-free control of the used device. This is highly desirable in surgery as it allows surgeons to control the device without need of breaking aseptic protocols. On the other hand, a still important limitation of AR simulation in surgery derives form the need of targeting deformable structures which present with significant changes during the procedure. Although it is feasible to monitor the operative field by using real-time ultrasound, computed tomography, or magnetic resonance imaging and correct the displayed three-dimensional (3D) model, there is a significant clinical delay on image interposition due to the still significant amount of time required to capture and reconstruct medical images. Of special importance to the readers of this chapter, it is more difficult to use AR in abdominal surgery because during laparoscopy, the amount of organ movement is significant. Therefore, although extremely promising, AR in abdominal surgery has been used more frequently for navigation during liver and pancreatic surgery as it allows better projection of large vessels and more precise tumor location.
Animal and Human Cadaveric Models
It seems reasonable to assume that animal models offer a degree of fidelity that cannot be superseded by any other simulation model. 23 Live and anesthetized animals favor the development of some skills necessary for performance in the operating room, including going through the preparation of the room, instrumental, and equipment readiness. Another advantage of an animal model is that they favor the user to work in a team as well as to experience the authority gradient in the operating room. There is no doubt that operative steps like vascular division and dissection in anatomical planes are very reliable in swines. 24 As a matter of fact, colectomy in the swine model is a very standardized procedure. It is possible to simulate colon dissection, vascular ligation, endoscopic rectal transection, proceeding to the auxiliary incision with resection of the specimen, and fashioning the anastomosis. On the other hand, human anatomy cannot be properly reproduced in the animal model and the observation that the animal model is not reliable is quite common among surgeons in training. 25 For example, the swine model represents an excellent option for left colectomy training. It enables dissection, vascular control, rectal transection, and full double-stapled anastomosis. On the other hand, training laparoscopic colectomy in the pig model lacks the right colectomy training. Moreover, laboratory animals are generally expensive to dispose of since specialized personnel and the need for anesthesia are indispensable in addition to the need to look for the supplier and the place where the animals are dispensed. Some countries such as the United Kingdom also prohibit the use of animals as a result of the ethical controversy surrounding the issue, 26 but allow the use of tissues from dead animals such as sheep and pigs.
Human cadaveric surgical simulation in several specialties and not only in colorectal surgery are generally used to provide an immersive and high-fidelity experience to trainers. Moreover, the surgical training model on a human cadaver seems to be the best from an anatomical point of view. 27 28 However, the availability of human cadavers for the training of minimally invasive surgeons is limited. Therefore, they are used less frequently due to the difficulty in turning the model available and also due to high cost. In addition, despite correct anatomy, the lack of bleeding, pulse, and breathing movements compromise the accuracy of the model.
In 2003, the American Society of Colon and Rectal Surgeons started organizing an annual colorectal laparoscopic surgery course with the use of a practical part on cadavers. 27 Course participants from 2003 to 2005 were asked to answer a questionnaire. One week after the course, a laparoscopic colectomy was performed by 53% of the participants and by 90% of them after 1 month. The questionnaire also revealed that at that time the main factor driving students to enroll in the course was the cadaver training model. Despite the limitations associated with this type of study with questionnaires and without a comparative group, the authors concluded that the completion of a practical course with a cadaver model allowed for the rapid adoption of laparoscopic colectomy.
Perhaps an area of prominence where cadaver simulation represents an outstanding tool for skills transfer in minimally invasive colorectal surgery has been teaching TaTME. TaTME represents an extremely valuable approach to initiate and complete TME using a minimally invasive approach in complex situations such as in obese male patients harboring more distal rectal cancers. In TaTME, dissection, to become technically competent, new didactic resources such as online presentations and videos of live surgeries may have partly addressed learning needs. However, more structured theoretical and practical insights are central. To successfully undertake TaTME, full purse-string insertion in the distal rectum above the tumor represents a key initial requirement and also a challenging one. Next, bottom-up dissection of the TME plane also provides important challenges. The anatomy of the pelvic fascial seen from below using an endoscopic platform may lead the surgeon away from the mesorectum and toward the pelvic sidewall. If this happens, damage to nerve plexuses and even inadvertent dissection of the prostate leading to urethral injury was described. 29
The outcomes of 65 delegates attending one of the first TaTME cadaveric simulation courses in U.K. were addressed by Wynn et al. 30 Trainees reported high levels of satisfaction and have achieved good quality mesorectal specimens under supervision. In the report, nearly 50% of the respondents had performed TaTME surgery after 6 months and 95% of all delegates stated an intention to use TaTME as an approach to rectal cancer in future.
There is no doubt that human cadaver simulation represents a special tool in some subareas of minimally invasive colorectal surgery such as in TaTME. The simulation of this procedure in swine lacks fidelity and it is not yet available in VR simulators. However, it turns out that the realism of preclinical simulation in cadavers is not enough to guarantee the so needed effectiveness and safety regarding patients of surgeons undergoing training in TaTME as recently reproduced by Atallah et al. 31 In this report, human cadaveric hands-on courses on TaTME were conducted in the United States for 1 year. In this series, 81 attending colorectal surgery trainees completed the course. During the training, 71% achieved an adequate TME specimen. The authors conducted then an online survey to assess postcourse experience with the TaTME approach. Thirty-eight (46.9%) of 81 attendee surgeons responded to the survey. Among these surgeons, there were 5 reported cases of urethral injury leading to a high incidence (20%) of this severe complication detected on the survey. This finding represents an important concern with the uptake of TaTME. Based mainly on this finding, the authors concluded that although cadaveric courses represent an important resource to skills acquisition, they are probably insufficient to empower surgeons with the skill set necessary to safely perform TaTME.
Effectiveness of Technology-Enhanced Simulation for Training and Adoption in Minimally Invasive Colorectal Surgery
There is currently no reported direct evidence of skills transfer specific to minimally invasive colorectal surgery derived from simulation-based training. However, regarding laparoscopic surgery overall, regardless of outcome, level of the trainee surgeon, study design, or a specific laparoscopic task considered, simulation-based training when compared with no training is largely more effective according to a systematic review. 32 For the comparison of simulation-based training versus no intervention in this study, 151 studies were included. Another curious finding of this very large systematic review was that box simulators were associated with slightly greater outcomes than VR simulators, regarding to the learner's satisfaction with the training. However, VR simulators are an expensive resource. The lack of a clear advantage of VR over box simulators leads to questioning the value of the first ones in the surgical training curricula.
To help answer the question on the role of VR simulations for skills transfer in laparoscopic surgery, Alaker et al 33 have recently published a dedicated systematic review and meta-analysis on the comparison of VR simulation training with no training and with other simulation techniques. When VR simulation-based training was compared with no training, it was possible to assemble data from 579 participants enrolled in 24 randomized controlled trials (RCTs). The primary outcome measures of change in time and scores associated with the training tasks were reported in most studies. According to the majority of these reports, VR simulation-based training was superior to no training. Things get a little more complicated when skills transfer to the trainee surgeon after training in a VR simulator are compared with after training in a box simulator. In the meta-analysis, 9 studies with 557 participants provided this information. The primary outcome measures of time and score were assessed in all the studies. The meta-analysis of comparing VR to box trainers fell in slight favor of the VR training. It is our impression that training in the box simulator leads to enhanced skills transfer due to the fact that it is more difficult for subjects to get used to the VR simulator than the box trainer. Furthermore, different tasks require different skills set. According to Chmarra et al, 34 for training tasks requiring force application, simulators with haptic feedback (the box simulators) are needed. For tasks requiring hand-eye coordination such as peg transfer, simulators with no such haptics, like the VR ones may suffice. Those might be part of the explanation of why comparing the results of skills transfer from different simulation techniques may be challenging.
A potential application of simulation-based training into surgical practice may include a form of warm-up. A VR simulation warm-up module is performed just before undertaking the real procedure. For laparoscopic cholecystectomy, the positive effect for experienced surgeons on specific psychomotor skills performing cholecystectomies after a warm-up were already demonstrated in two randomized trial. 35 36 In colorectal surgery, evidence for a routine warm-up is still lacking. However, the hypothesis that a short-duration (warm-up) skills training in a VR simulator could positively impact the performance of surgical residents was tested positive in a single-blinded randomized trial using technical performance during a colectomy in the swine model as the main outcome. In a small study, 37 it was demonstrated that a single short-duration VR simulator practice positively impacted novice surgeons' generic and specific skills performance required to accomplish laparoscopic colectomy in a swine model. In our opinion, these data should be interpreted with caution, especially regarding the potential benefits of warming-up for more-experienced surgeon.
Robotic Surgery
As with colorectal laparoscopic surgery, there are no studies dedicated specifically to the role of simulation-based training in the transfer of specific skills for performing robotic colorectal surgery. Moreover, to the best of our knowledge, it remains unclear which tasks and metrics are the most effective in distinguishing different levels of experience on the da Vinci surgical system.
Regarding VR robotic surgery simulation platforms, robotics-based task modules provide the learning environment for surgeons to develop basic robotic skills and clinical simulation modules (like hysterectomy, prostatectomy, thoracoscopic lobectomy, inguinal hernia, and right colectomy). Two standalone platforms for VR simulation in robotic surgery with the da Vinci robotic system (Intuitive, Inc., Sunnyvale, CA) remains the most popular worldwide, the pioneer dV Trainer, manufactured by Mimic Technologies (Seattle, WA) and the latest RobotiX Mentor manufactured by 3D Systems (formerly Simbionix, Cleveland, OH) ( Fig. 1 ). Likewise, VR simulators are already available on the surgeon's console of the da Vinci robotic system. According to the system, they might be the pioneer da Vinci Skills Simulator or dVSS (Mimic Technologies) and the latest SimNow (3D Systems). The aforementioned platforms remain the widely investigated systems. However, there are two additional VR-based simulation platforms for robotic surgery: the Surgical Education Platform (SEP; SimSurgery, Oslo, Norway) and the Robotic Surgical System (RoSS; Simulated Surgical Systems, San Jose, CA).
Fig. 1.
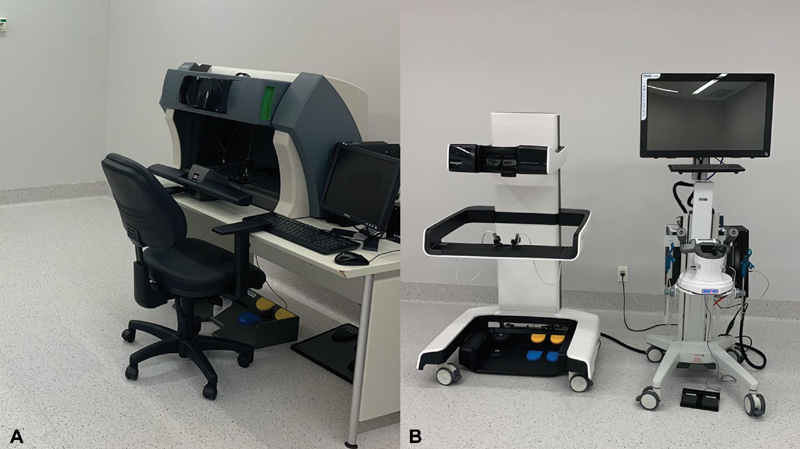
The two most popular platforms for virtual reality (VR) standalone simulation in robotic surgery: ( A ) dV Trainer (Mimic Technologies, Seattle, WA), and ( B ) RobotiX Mentor (3D Systems, Cleveland, OH).
Moglia et al 38 have recently conducted a comprehensive systematic review on the use of VR simulators for robotic surgery. Although colorectal surgery was not a surgical specialty included in the review, reports on robotic general surgery were included. VR simulators were rated “good” for realism (face validity) and for usefulness as a training tool (content validity). However, regarding the aspect of construct validity (capability of discerning between novice and expert surgeons), due to the numerous training methodologies across the studies, there was clear limitation.
As for laparoscopic surgery, one important question regarding VR simulation in robotic surgery is regarding which of the many provided metrics inside the simulator modules are useful for evaluation of a determined surgical trainee. Lyons et al 39 have evaluated the content of the 33 modules provided by the da Vinci Skills Simulator (Intuitive Surgical, Sunnyvale, CA) according to a board of experts, they have come to a conclusion that 8 of the 33 modules have proven to be essential. These 8 tasks were used for evaluating the performance of 46 surgeons and trainees on the simulator (25 novices, 8 intermediates, and 13 experts). According to the authors, metrics that performed particularly well were overall score, time, and economy of motion. These metrics have differentiated novices from experts across all tasks. Moreover, instrument collision, master workspace, and critical errors were also useful metrics.
The current evidence on skills transfer from VR simulation in robotic surgery is difficult to analyze. Moglia et al 38 have included 9 studies in a systematic review. In these studies, the number of included patients is relatively small (range 12–53). Although 7 studies are RCTs 40 41 42 43 44 45 46 (generating level 2 evidence according to the Oxford Centre for Evidence-based Medicine), the intervention effect (VR simulation-based training) was measured by task performance on an inanimate model in all, except for one study on hysterectomies on humans 47 and one study where the test task was undertaken on a pig model. 42 Only one study 41 included general surgery residents. All the remaining evidence refers to urology or gynecologic surgery trainees. The only possible conclusion at this moment is that there is still no evidence of skills transfer to real patients in the operating room undergoing robotic surgery derived from VR training, although there is evidence regarding skills acquisition after training in a robotic simulator.
Acknowledgments
None.
Footnotes
Conflict of Interest None declared.
References
- 1.Sachdeva A K, Russell T R.Safe introduction of new procedures and emerging technologies in surgery: education, credentialing, and privileging Surg Clin North Am 20078704853–866., vi–vii [DOI] [PubMed] [Google Scholar]
- 2.Scott D J, Cendan J C, Pugh C M, Minter R M, Dunnington G L, Kozar R A. The changing face of surgical education: simulation as the new paradigm. J Surg Res. 2008;147(02):189–193. doi: 10.1016/j.jss.2008.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tjandra J J, Chan M KY. Systematic review on the short-term outcome of laparoscopic resection for colon and rectosigmoid cancer. Colorectal Dis. 2006;8(05):375–388. doi: 10.1111/j.1463-1318.2006.00974.x. [DOI] [PubMed] [Google Scholar]
- 4.Lacy A M, García-Valdecasas J C, Delgado S.Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial Lancet 2002359(9325):2224–2229. [DOI] [PubMed] [Google Scholar]
- 5.Fleshman J, Branda M, Sargent D J. Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA. 2015;314(13):1346–1355. doi: 10.1001/jama.2015.10529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.COLOR II Study Group . Bonjer H J, Deijen C L, Abis G A. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med. 2015;372(14):1324–1332. doi: 10.1056/NEJMoa1414882. [DOI] [PubMed] [Google Scholar]
- 7.MRC CLASICC trial group Guillou P J, Quirke P, Thorpe H.Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial Lancet 2005365(9472):1718–1726. [DOI] [PubMed] [Google Scholar]
- 8.Kemp J A, Finlayson S RG. Nationwide trends in laparoscopic colectomy from 2000 to 2004. Surg Endosc. 2008;22(05):1181–1187. doi: 10.1007/s00464-007-9732-8. [DOI] [PubMed] [Google Scholar]
- 9.Bridges M, Diamond D L. The financial impact of teaching surgical residents in the operating room. Am J Surg. 1999;177(01):28–32. doi: 10.1016/s0002-9610(98)00289-x. [DOI] [PubMed] [Google Scholar]
- 10.Fried G M, Feldman L S, Vassiliou M C.Proving the value of simulation in laparoscopic surgery Ann Surg 200424003518–525., discussion 525–528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scott D J, Bergen P C, Rege R V. Laparoscopic training on bench models: better and more cost effective than operating room experience? J Am Coll Surg. 2000;191(03):272–283. doi: 10.1016/s1072-7515(00)00339-2. [DOI] [PubMed] [Google Scholar]
- 12.Martin J A, Regehr G, Reznick R. Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg. 1997;84(02):273–278. doi: 10.1046/j.1365-2168.1997.02502.x. [DOI] [PubMed] [Google Scholar]
- 13.Neary P C, Boyle E, Delaney C P, Senagore A J, Keane F BV, Gallagher A G. Construct validation of a novel hybrid virtual-reality simulator for training and assessing laparoscopic colectomy; results from the first course for experienced senior laparoscopic surgeons. Surg Endosc. 2008;22(10):2301–2309. doi: 10.1007/s00464-008-9900-5. [DOI] [PubMed] [Google Scholar]
- 14.Coleman J, Nduka C C, Darzi A. Virtual reality and laparoscopic surgery. Br J Surg. 1994;81(12):1709–1711. doi: 10.1002/bjs.1800811204. [DOI] [PubMed] [Google Scholar]
- 15.Satava R M. Virtual reality surgical simulator. The first steps. Surg Endosc. 1993;7(03):203–205. doi: 10.1007/BF00594110. [DOI] [PubMed] [Google Scholar]
- 16.Woodrum D T, Andreatta P B, Yellamanchilli R K, Feryus L, Gauger P G, Minter R M. Construct validity of the LapSim laparoscopic surgical simulator. Am J Surg. 2006;191(01):28–32. doi: 10.1016/j.amjsurg.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 17.Gallagher A G, Richie K, McClure N, McGuigan J. Objective psychomotor skills assessment of experienced, junior, and novice laparoscopists with virtual reality. World J Surg. 2001;25(11):1478–1483. doi: 10.1007/s00268-001-0133-1. [DOI] [PubMed] [Google Scholar]
- 18.Grantcharov T P, Kristiansen V B, Bendix J, Bardram L, Rosenberg J, Funch-Jensen P. Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg. 2004;91(02):146–150. doi: 10.1002/bjs.4407. [DOI] [PubMed] [Google Scholar]
- 19.Gallagher A G, Seymour N E, Jordan-Black J-A, Bunting B P, McGlade K, Satava R M. Prospective, randomized assessment of transfer of training (ToT) and transfer effectiveness ratio (TER) of virtual reality simulation training for laparoscopic skill acquisition. Ann Surg. 2013;257(06):1025–1031. doi: 10.1097/SLA.0b013e318284f658. [DOI] [PubMed] [Google Scholar]
- 20.Torkington J, Smith S G, Rees B I, Darzi A. Skill transfer from virtual reality to a real laparoscopic task. Surg Endosc. 2001;15(10):1076–1079. doi: 10.1007/s004640000233. [DOI] [PubMed] [Google Scholar]
- 21.Seymour N E, Gallagher A G, Roman S A.Virtual reality training improves operating room performance: results of a randomized, double-blinded study Ann Surg 200223604458–463., discussion 463–464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Araujo S EA, Seid V E, Bertoncini A B, Horcel L A, Nahas S C, Cecconello I. Single-session baseline virtual reality simulator scores predict technical performance for laparoscopic colectomy: a study in the swine model. J Surg Educ. 2014;71(06):883–891. doi: 10.1016/j.jsurg.2014.05.017. [DOI] [PubMed] [Google Scholar]
- 23.Sugden C, Aggarwal R. Assessment and feedback in the skills laboratory and operating room. Surg Clin North Am. 2010;90(03):519–533. doi: 10.1016/j.suc.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 24.Choy I, Okrainec A. Simulation in surgery: perfecting the practice. Surg Clin North Am. 2010;90(03):457–473. doi: 10.1016/j.suc.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 25.Lin E, Szomstein S, Addasi T, Galati-Burke L, Turner J W, Tiszenkel H I. Model for teaching laparoscopic colectomy to surgical residents. Am J Surg. 2003;186(01):45–48. doi: 10.1016/s0002-9610(03)00107-7. [DOI] [PubMed] [Google Scholar]
- 26.Tan S SY, Sarker S K. Simulation in surgery: a review. Scott Med J. 2011;56(02):104–109. doi: 10.1258/smj.2011.011098. [DOI] [PubMed] [Google Scholar]
- 27.Ross H M, Simmang C L, Fleshman J W, Marcello P W. Adoption of laparoscopic colectomy: results and implications of ASCRS hands-on course participation. Surg Innov. 2008;15(03):179–183. doi: 10.1177/1553350608322100. [DOI] [PubMed] [Google Scholar]
- 28.Udomsawaengsup S, Pattana-arun J, Tansatit T. Minimally invasive surgery training in soft cadaver (MIST-SC) J Med Assoc Thai. 2005;88 04:S189–S194. [PubMed] [Google Scholar]
- 29.Rouanet P, Mourregot A, Azar C C. Transanal endoscopic proctectomy: an innovative procedure for difficult resection of rectal tumors in men with narrow pelvis. Dis Colon Rectum. 2013;56(04):408–415. doi: 10.1097/DCR.0b013e3182756fa0. [DOI] [PubMed] [Google Scholar]
- 30.Wynn G R, Austin R CT, Motson R W. Using cadaveric simulation to introduce the concept and skills required to start performing transanal total mesorectal excision. Colorectal Dis. 2018;20(06):496–501. doi: 10.1111/codi.14034. [DOI] [PubMed] [Google Scholar]
- 31.Atallah S B, DuBose A C, Burke J P. Uptake of transanal total mesorectal excision in North America: initial assessment of a structured training program and the experience of delegate surgeons. Dis Colon Rectum. 2017;60(10):1023–1031. doi: 10.1097/DCR.0000000000000823. [DOI] [PubMed] [Google Scholar]
- 32.Zendejas B, Brydges R, Hamstra S J, Cook D A. State of the evidence on simulation-based training for laparoscopic surgery: a systematic review. Ann Surg. 2013;257(04):586–593. doi: 10.1097/SLA.0b013e318288c40b. [DOI] [PubMed] [Google Scholar]
- 33.Alaker M, Wynn G R, Arulampalam T. Virtual reality training in laparoscopic surgery: a systematic review & meta-analysis. Int J Surg. 2016;29:85–94. doi: 10.1016/j.ijsu.2016.03.034. [DOI] [PubMed] [Google Scholar]
- 34.Chmarra M K, Dankelman J, van den Dobbelsteen J J, Jansen F-W. Force feedback and basic laparoscopic skills. Surg Endosc. 2008;22(10):2140–2148. doi: 10.1007/s00464-008-9937-5. [DOI] [PubMed] [Google Scholar]
- 35.Calatayud D, Arora S, Aggarwal R. Warm-up in a virtual reality environment improves performance in the operating room. Ann Surg. 2010;251(06):1181–1185. doi: 10.1097/SLA.0b013e3181deb630. [DOI] [PubMed] [Google Scholar]
- 36.Moldovanu R, Târcoveanu E, Dimofte G, Lupaşcu C, Bradea C. Preoperative warm-up using a virtual reality simulator. JSLS. 2011;15(04):533–538. doi: 10.4293/108680811X13176785204409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Araujo S EA, Delaney C P, Seid V E. Short-duration virtual reality simulation training positively impacts performance during laparoscopic colectomy in animal model: results of a single-blinded randomized trial: VR warm-up for laparoscopic colectomy. Surg Endosc. 2014;28(09):2547–2554. doi: 10.1007/s00464-014-3500-3. [DOI] [PubMed] [Google Scholar]
- 38.Moglia A, Ferrari V, Morelli L, Ferrari M, Mosca F, Cuschieri A. A systematic review of virtual reality simulators for robot-assisted surgery. Eur Urol. 2016;69(06):1065–1080. doi: 10.1016/j.eururo.2015.09.021. [DOI] [PubMed] [Google Scholar]
- 39.Lyons C, Goldfarb D, Jones S L. Which skills really matter? Proving face, content, and construct validity for a commercial robotic simulator. Surg Endosc. 2013;27(06):2020–2030. doi: 10.1007/s00464-012-2704-7. [DOI] [PubMed] [Google Scholar]
- 40.Korets R, Mues A C, Graversen J A. Validating the use of the Mimic dV-trainer for robotic surgery skill acquisition among urology residents. Urology. 2011;78(06):1326–1330. doi: 10.1016/j.urology.2011.07.1426. [DOI] [PubMed] [Google Scholar]
- 41.Cho J S, Hahn K Y, Kwak J M. Virtual reality training improves da Vinci performance: a prospective trial. J Laparoendosc Adv Surg Tech A. 2013;23(12):992–998. doi: 10.1089/lap.2012.0396. [DOI] [PubMed] [Google Scholar]
- 42.Whitehurst S V, Lockrow E G, Lendvay T S. Comparison of two simulation systems to support robotic-assisted surgical training: a pilot study (Swine model) J Minim Invasive Gynecol. 2015;22(03):483–488. doi: 10.1016/j.jmig.2014.12.160. [DOI] [PubMed] [Google Scholar]
- 43.Vaccaro C M, Crisp C C, Fellner A N, Jackson C, Kleeman S D, Pavelka J. Robotic virtual reality simulation plus standard robotic orientation versus standard robotic orientation alone: a randomized controlled trial. Female Pelvic Med Reconstr Surg. 2013;19(05):266–270. doi: 10.1097/SPV.0b013e3182a09101. [DOI] [PubMed] [Google Scholar]
- 44.Kiely D J, Gotlieb W H, Lau S. Virtual reality robotic surgery simulation curriculum to teach robotic suturing: a randomized controlled trial. J Robot Surg. 2015;9(03):179–186. doi: 10.1007/s11701-015-0513-4. [DOI] [PubMed] [Google Scholar]
- 45.Stegemann A P, Ahmed K, Syed J R. Fundamental skills of robotic surgery: a multi-institutional randomized controlled trial for validation of a simulation-based curriculum. Urology. 2013;81(04):767–774. doi: 10.1016/j.urology.2012.12.033. [DOI] [PubMed] [Google Scholar]
- 46.Chowriappa A, Raza S J, Fazili A. Augmented-reality-based skills training for robot-assisted urethrovesical anastomosis: a multi-institutional randomised controlled trial. BJU Int. 2015;115(02):336–345. doi: 10.1111/bju.12704. [DOI] [PubMed] [Google Scholar]
- 47.Culligan P, Gurshumov E, Lewis C, Priestley J, Komar J, Salamon C. Predictive validity of a training protocol using a robotic surgery simulator. Female Pelvic Med Reconstr Surg. 2014;20(01):48–51. doi: 10.1097/SPV.0000000000000045. [DOI] [PubMed] [Google Scholar]


