Abstract
Purpose
This study evaluated the influence of a metal artifact reduction (MAR) tool in a cone-beam computed tomography (CBCT) device on the diagnosis of vertical root fractures (VRFs) in teeth with different root filling materials.
Materials and Methods
Forty-five extracted human premolars were classified into three subgroups; 1) no filling; 2) gutta-percha; and 3) metallic post. CBCT images were acquired using an Orthopantomograph 300 unit with and without a MAR tool. Subsequently, the same teeth were fractured, and new CBCT scans were obtained with and without MAR. Two oral radiologists evaluated the images regarding the presence or absence of VRF. Receiver operating characteristic (ROC) curves and diagnostic tests were performed.
Results
The overall area under the curve values were 0.695 for CBCT with MAR and 0.789 for CBCT without MAR. The MAR tool negatively influenced the overall diagnosis of VRFs in all tested subgroups, with lower accuracy (0.45–0.72), sensitivity (0.6–0.67), and specificity (0.23–0.8) than were found for the images without MAR. In the latter group, the accuracy, sensitivity, and specificity values were 0.68–0.77, 0.67–083, and 0.53–087, respectively. However, no significant difference was found between images with and without MAR for the no filling and gutta-percha subgroups (P>0.05). In the metallic post subgroup, CBCT showed a significant difference according to MAR use (P<0.05).
Conclusion
The OP 300 MAR tool negatively influenced the detection of VRFs in teeth with no root canal filling, gutta-percha, or metallic posts. Teeth with metallic posts suffered the most from the negative impact of MAR.
Keywords: Cone-Beam Computed Tomography, Tooth Fractures, Artifacts
Introduction
The diagnosis and treatment of vertical root fractures (VRFs) are often challenging. Their diagnosis is often imprecise, since classic radiographic signs, such as bone loss in the adjacent periodontal region or periodontal ligament thickening, are not always present. Furthermore, the accuracy of 2-dimensional radiographs for the diagnosis of VRFs depends on a specific radiographic angulation, which is not always possible.1
To overcome the major limitations of 2-dimensional radiographs, cone-beam computed tomography (CBCT) has been widely used in several clinical situations. In endodontics, CBCT has been applied for the assessment of apical periodontitis, complex surgical cases, root canal anatomy, dental trauma, tooth resorption, and root fractures.2,3,4,5 Some studies have reported that CBCT showed higher values of accuracy and sensitivity in the diagnosis of VRFs than periapical radiography.6,7 However, CBCT presented lower accuracy for root-filled teeth.8,9,10,11,12
The presence of high-density materials, mainly gutta-percha and metallic posts, in the region of interest during image acquisition produces significant beam hardening and streak artifacts that compromise image quality,13,14 particularly for VRF diagnosis.15 As a result, metallic objects (posts and restorations), and even gutta-percha, create hypodense lines in the final CBCT images, which can often be misdiagnosed as VRFs, leading to incorrect treatment.16,17,18 These artifacts contribute to a uniquely unfavorable diagnostic scenario since VRFs are disproportionately prevalent in endodontically treated teeth.19
Artifact reduction tools are designed to improve CBCT images' quality when high-density artifact-generating materials are present in the region of interest. Metal artifact reduction (MAR) tools apply algorithms during the image reconstruction process to reduce or eliminate artifact effects in CBCT.20,21 However, some studies have suggested that MAR might not always improve image quality, especially in the diagnosis of root fractures.22,23,24 New diagnostic tools need to be tested to demonstrate their real effectiveness in improving VRF detection. Therefore, the main purpose of this study was to evaluate the influence of an artifact reduction tool on the detection of vertical root fractures in teeth with different types of intracanal materials.
Materials and Methods
This observational ex vivo study was approved by the institutional review board of Anápolis University Center, Brazil (# 3.008.747) and complied with the Helsinki Declaration.
Forty-five single-rooted healthy premolars, extracted for orthodontic or periodontal reasons between 2017 and 2018, were included in this study. The teeth were stored in a 0.2% thymol solution and periodontal scaling was performed to remove soft tissues attached to the root. Periapical radiographs of all teeth were acquired using a Focus™ (Instrumentarium Dental, Kavo, Biberach, Germany) device with the following technical parameters: 60 kVp, 7 mA, and 0.2 s. The images were taken using a digital photostimulable phosphor system (KaVo Scan eXam, Kavo/Gendex, Des Plaines, IL, USA) and analyzed using the Cliniview® (Instrumentarium Dental™, Kavo, Biberach, Germany) software. These radiographs were taken to select teeth without pulp stones, external or internal resorption, incomplete root formation, or fractures. The selected teeth were randomly divided into 3 subgroups consisting of 15 teeth each: 1) no filling, 2) gutta-percha, and 3) metallic post.
In the no filling group, no treatment was done. The root canals in the gutta-percha group were instrumented using an Mtwo NiTi® rotary system (VDW, Munich, Germany) up to file size #40. Subsequently, the roots were filled using a single-cone technique with Mtwo gutta-percha (VDW GmbH, Munich, Germany) and AH 26 cement (Dentsply DeTrey GmbH, Konstanz, Germany) according to the manufacturer's instructions. The 15 teeth from the metallic post group received the same root treatment as those in the gutta-percha group, and were subsequently decoronated, leaving a standardized root length of 16 mm, guided by the use of a digital caliper. After decoronation, two-thirds of the root canal of each tooth was prepared to receive a metallic post. The remaining gutta-percha had an approximate length of 3 mm. Digital periapical radiographs were taken to assist in the preparation. Impressions of the root canals were made using acrylic resin (Duralay®, Reliance Dental Manufacturing LLC, Alsip, IL, USA). Metallic posts (nickel-chromium alloy) were then prepared and inserted in each root canal.
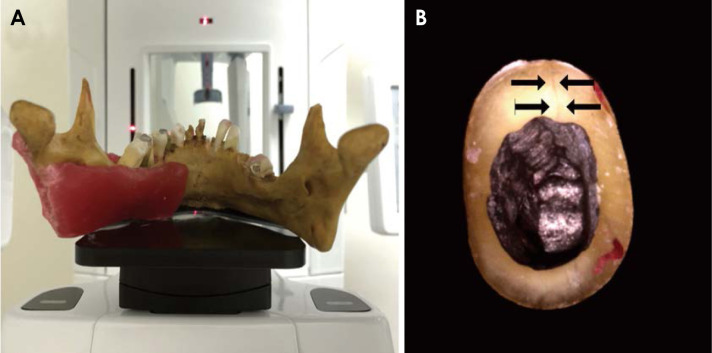
To simulate clinical conditions, the periodontal ligament space was artificially reproduced with the addition of silicone fluid, and the roots25 were placed randomly into dry mandibular sockets. The human mandible was covered with a 5.3-mm-thick layer of wax on the lingual and buccal sides to simulate soft tissue attenuation. Subsequently, CBCT images were acquired using an Orthopantomograph® OP300 (Instrumentarium Kavo Kerr Corp, Tuusula, Finland) device (Fig. 1A), with the following technical parameters: a field of view (FOV) of 6 cm×4 cm; a voxel size of 0.085 mm; 90 kVp; 10 mA; and 6.1 s. CBCT scans were obtained from the 45 teeth before they were fractured, first without selecting the MAR tool, and then with MAR tool selection.
Fig. 1. A. The phantom is positioned in the Orthopantomograph® OP 300. B. Premolar bonded after fracture.
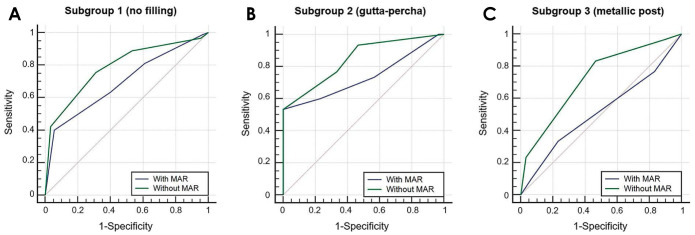
Fractures were induced on a Universal Instron (Instron, Canton, MA, USA) testing machine using a 500 N load cell with a cross-speed of 1 mm/min. A tapered metal tip was inserted into the canal's coronal opening, and as soon as the fracture occurred, the machine stopped automatically. Fractures were confirmed by direct visual inspection of each tooth. In cases with fragment separation, the teeth were bonded with cyanoacrylate (Fig. 1B). After being fractured, all the samples underwent new CBCT acquisitions, following the same technical parameters, with and without MAR, resulting in a total of 180 CBCT volumes (Fig. 2).
Fig. 2. Coronal slices show root fracture (arrows) in cone-beam computed tomography acquisitions with and without MAR. A. No filling. B. Gutta-percha. C. Metallic post.
All CBCT evaluations were conducted in a blinded manner by 2 trained oral and maxillofacial radiologists, with 10 and 8 years of experience, respectively, who had previously been calibrated. The images used for calibration were not included in the analysis. The radiologists assessed the presence or absence of VRFs through a dynamic evaluation of the CBCT volume in all anatomical planes, using InVivo Dental software (ver. 5.4, Anatomage, San Jose, CA, USA). The observers could navigate in all multiplanar reconstructions (including axial, sagittal and coronal), and were free to tilt the CBCT volume in any direction.
All images, including both the fractured and non-fractured teeth, were scrambled by the main researcher and assessed by the examiners in random order on the same computer with a 29-inch monitor (Ultra HD LED, 3840×2160 pixels, 28″, DELL, Round Rock, TX, USA) in a dimmed room. Although the teeth were scanned in groups of 6 to simulate clinical conditions, each tooth was analyzed individually to avoid bias. The examiners were allowed to adjust brightness and contrast, and to use the zoom and enhancement filter tools. A 5-point scale was adopted to register VRF detection as follows; 1: definitely absent, 2: probably absent, 3: uncertainty, 4: probably present, and 5: definitely present. Reproducibility was assessed by a second evaluation of 30% of the sample by the same examiners after at least 15 days.
Statistical analyses were performed using MedCalc® 19.0.3 for Windows (MedCalc Software, Mariakerke, Belgium). Receiver operating characteristic (ROC) curve analysis was conducted to evaluate the diagnostic accuracy of CBCT according to the use of the MAR tool for the diagnosis of VRFs. The areas under the ROC curves for both groups with and without MAR were compared using the DeLong test,26 and the level of significance was set at 5% (P<0.05). ROC curves were also created and compared for the 3 subgroups (no filling, gutta-percha, and metallic post). Diagnostic tests such as accuracy, sensitivity, specificity, positive predictive value, and negative predictive value were calculated for both groups and all 3 subgroups. For this analysis, the answers given by the examiners were dichotomized. Scores of 1, 2, and 3 were considered as indicating the absence of VRF, and scores of 4 and 5 as indicating the presence of VRF.24 The Kendall coefficient of concordance was used to establish inter-examiner agreement, and the kappa coefficient was used to determine intraexaminer agreement.
Results
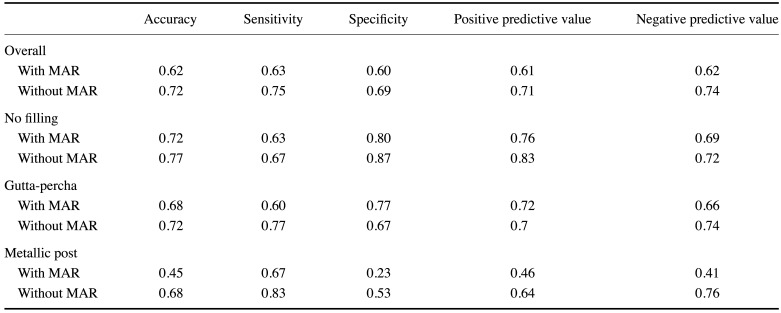
The ROC curves of the images with and without MAR are shown in Figure 3. The areas under the curve were 0.695 and 0.789 for CBCT with and without MAR, respectively. The DeLong test revealed a significant difference between the two groups (P<0.05) with better performance found when MAR was not used group. The inter-examiner kappa value showed substantial agreement for images with (0.737) and without (0.786) MAR. Intra-examiner reproducibility indicated moderate agreement for images with MAR and without MAR (0.533 and 0.433, respectively). Figure 4 shows the ROC curves in the 3 different subgroups. No significant difference was found between images with and without MAR for either the no filling or gutta-percha subgroup (P>0.05). In contrast, in the metallic post subgroup, images with MAR showed a significant difference compared to those without MAR (P<0.05).
Fig. 3. Receiver operating characteristic curves for all observers based on cone-beam computed tomographic image with and without metal artifact reduction (MAR).
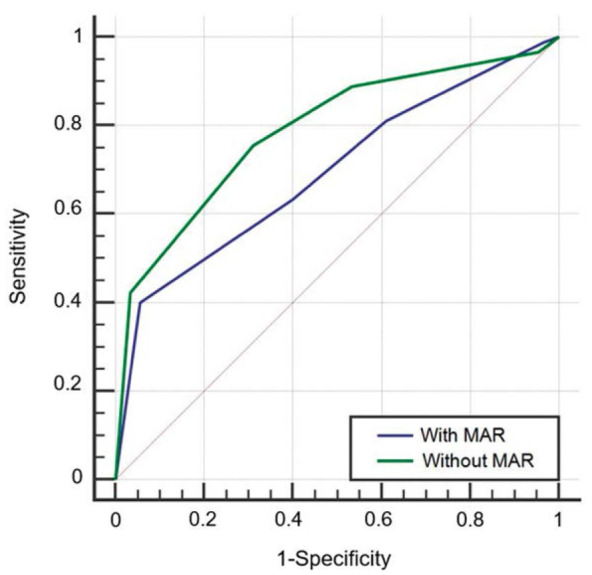
Fig. 4. Receiver operating characteristic curves for groups with and without MAR, showing detailed performance for each of the 3 subgroups. A. No filling. B. Gutta-percha. C. Metallic post.
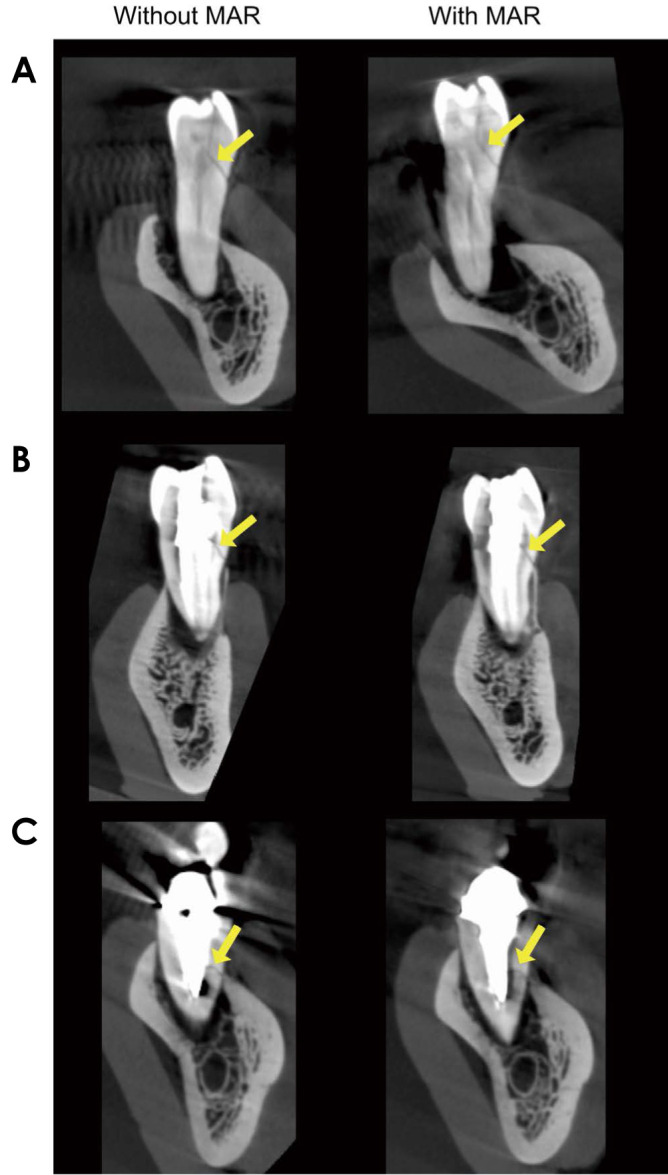
Table 1 summarizes the overall accuracy, sensitivity, spe-cificity, positive predictive value (PPV), and negative predictive value (NPV), with and without the use of MAR. Higher values were obtained for the images without MAR. The results of the same tests for each subgroup (no filling, guttapercha, and metallic post) with and without MAR can also be observed in Table 1. The lowest accuracy values (0.45 and 0.68 for images with MAR and without MAR, respectively) were found for the metallic post subgroup and the gutta-percha subgroup with MAR. The highest accuracy value was found in the subgroup with no root canal filling in the absence of MAR.
Table 1. Diagnostic tests for vertical root fracture detection with and without metal artifact reduction (MAR) overall and in different subgroups.
Discussion
This study analyzed the influence of the MAR function of OP300 on the diagnosis of vertical root fractures. The use of MAR tools should reduce the artifacts in the final image and, consequently, increase the values of accuracy and other diagnostic tests. However, the overall results showed that the use of MAR decreased the accuracy of VRF detection. Likewise, sensitivity, specificity, and both positive and negative predictive values were also lower when the MAR tool was used.
The diagnostic test values showed slight differences according to whether MAR was used in each of the 3 subgroups evaluated individually, except in the metallic post subgroup, which showed a considerable difference for all tests. This result was also noticed in the ROC curve comparison, since the metallic post subgroup was the only subgroup that showed a statistically significant difference according to MAR use. These findings indicate that, paradoxically, the MAR tool had the greatest negative impact in the subgroup with higher artifact production. These results impacted the overall results for VRF detection when using the MAR tool. Since the other 2 subgroups (no filling and gutta-percha) showed no significant difference according to MAR use, the metallic post subgroup was primarily responsible for the poor overall accuracy.
It is essential to emphasize that although MAR may enhance image quality,20,27,28 it does not necessarily positively influence the diagnosis. Previous studies have not yet concluded whether MAR enhances root fracture detection.
Our results align with those of a study by Bechara et al.,22 who evaluated the performance of 2 artifact reduction tools (ProMax® and Master 3D®) in the diagnosis of VRFs in endodontically treated teeth, and concluded that both MAR tools performed poorly in the diagnosis of VRFs using 2 different devices. Rezende et al.29 observed similar results in their analysis of the influence of MAR on the diagnosis of VRFs in different groups of teeth. They concluded that the application of MAR did not improve the diagnosis of VRFs. Diagnostic accuracy was lower for teeth with a cast gold pin, regardless of whether the tool was used. In this case, the diagnosis was hindered in the group in which artifacts were most pronounced. These results agree with the present study, in which the teeth with metallic posts showed the lowest accuracy.
According to the present study and previous studies,23,29 MAR application did not improve the detection of VRFs in endodontically treated teeth (gutta-percha) or teeth with the presence of metallic posts. It is known that CBCT devices utilize specific reconstruction algorithms that influence image quality and diagnostic feasibility; nevertheless, acquisition parameters such as FOV, voxel size, peak kilovoltage, and tube current undoubtedly also have a significant impact on the final image. Post-processing software systems are now available to assist in complex endodontic cases, but they have not yet been tested for the diagnosis of VRFs.30 These findings suggest that manufacturers should focus on improving MAR tools to contribute to a more accurate diagnosis of VRFs. Although limited information is available from CBCT manufacturers concerning the operation of MAR algorithms, it is believed that they are activated based on a threshold. Any structure different from the gray values threshold will be corrected, changing the values corresponding to very hypodense bands or very hyperdense streaks of hyperdense materials, such as gutta-percha and metallic posts.31 However, this reduction of gray values, apparently, does not lead to a more accurate diagnosis. In this study, when MAR was used, the fracture line and dentin density became similar, which is the most probable explanation for the decreased accuracy.
For VRF diagnosis, the image quality should be capable of reproducing the hypodense fracture line in contrast with the adjacent structures. The image quality in CBCT is influenced by different factors: FOV, voxel size, signal-to-noise ratio, contrast, spatial resolution, scatter, artifacts, detector quality, and reconstruction algorithms.32,33 In this study, a 6 cm×4 cm FOV, a voxel size of 0.085 mm, and settings of 90 kVp and 10 mA were used. This protocol is recommended for diagnosing and managing endodontic problems when a high level of detail is required. The small FOV promotes a high detail and resolution because it reduces scattering, thereby improving image quality.2 A larger FOV and, consequently, larger voxel size produces images with lower spatial resolution. However, detecting a greater number of X-ray photons in larger voxels (in the X-ray detector), results in a higher signal and less image noise.34 In contrast, Yamamoto-Silva et al.31 concluded that a small voxel size increased the accuracy of CBCT for VRF diagnosis, despite its association with higher noise. A compensatory method was performed in our study by increasing the mA setting (10 mA) to improve the signal-to-noise ratio. Knowing that small voxels, like those used in the present study (0.085 mm), can produce more artifacts in the final image, further studies are necessary to test the balance between a high spatial resolution and image noise.
As an ex vivo experiment, this study may not accurately reproduce clinical conditions. A previous in vivo study5 showed a sensitivity of 88% and a specificity of 75% when using CBCT to detect VRFs, but MAR was not tested. It is not ethically permissible to perform tests with ionizing radiation in patients for experimental purposes. Furthermore, a reliable gold-standard method would require tooth extraction, which is not a reasonable treatment for many clinical cases. Therefore, due to these clinical limitations of root fracture studies, in vitro and ex vivo studies are essential for orienting clinical approaches and supporting the decisionmaking process. Another limitation is related to the moderate level of intra-examiner agreement, despite the calibration and long experience of the observers. Other studies have also found moderate and poor agreement,14,17,35 suggesting that CBCT is still an unreliable method for detecting VRFs, especially in the presence of a metallic post. This can be explained by the partial volume averaging effect, which takes place when a voxel lies on the limits of 2 objects of different densities and impairs the detection of delicate structures, such as VRFs.36
Our findings align with most previous studies in the literature, showing that VRF diagnosis remains a clinical challenge and MAR still has limited use. Therefore, the aim should be to develop better software, focusing on the improvement of these tools and their application in images from different CBCT devices. Periapical radiography should be encouraged as the first complementary approach to assess the presence of VRFs, particularly for teeth with a metallic post.17,24,37
In conclusion, the OP 300 MAR tool negatively influenced the diagnosis of VRFs. The worst performance was obtained for the metallic post group. Our results align with most previous studies, showing that MAR still has limited utility for this purpose. These findings suggest that manufacturers should focus on the improvement of MAR tools to improve the accuracy of VRF diagnosis.
Acknowledgements
We would like to thank the Biomechanics Laboratory of the Federal University of Goiás and Anápolis University Center for technical support.
Footnotes
Conflicts of Interest: None
References
- 1.Khasnis SA, Kidiyoor KH, Patil AB, Kenganal SB. Vertical root fractures and their management. J Conserv Dent. 2014;17:103–110. doi: 10.4103/0972-0707.128034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel S, Brown J, Pimentel T, Kelly RD, Abella F, Durack C. Cone beam computed tomography in endodontics- a review of the literature. Int Endod J. 2019;52:1138–1152. doi: 10.1111/iej.13115. [DOI] [PubMed] [Google Scholar]
- 3.Patel S, Dawood A, Ford TP, Whaites E. The potential applications of cone beam computed tomography in the management of endodontic problems. Int Endod J. 2007;40:818–830. doi: 10.1111/j.1365-2591.2007.01299.x. [DOI] [PubMed] [Google Scholar]
- 4.Scarfe WC, Levin MD, Gane D, Farma AG. Use of cone beam computed tomography in endodontics. Int J Dent. 2009;2009:634567. doi: 10.1155/2009/634567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edlund M, Nair MK, Nair UP. Detection of vertical root fractures by using cone-beam computed tomography: a clinical study. J Endod. 2011;37:768–772. doi: 10.1016/j.joen.2011.02.034. [DOI] [PubMed] [Google Scholar]
- 6.Salineiro FC, Kobayashi-Velasco S, Braga MM, Cavalcanti MG. Radiographic diagnosis of root fractures: a systematic review, meta-analyses and sources of heterogeneity. Dentomaxillofac Radiol. 2017;46:20170400. doi: 10.1259/dmfr.20170400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ma RH, Ge ZP, Li G. Detection accuracy of root fractures in cone-beam computed tomography images: a systematic review and meta-analysis. Int Endod J. 2016;49:646–654. doi: 10.1111/iej.12490. [DOI] [PubMed] [Google Scholar]
- 8.Chang E, Lam E, Shah P, Azarpazhooh A. Cone-beam computed tomography for detecting vertical root fractures in endodontically treated teeth: a systematic review. J Endod. 2016;4:177–185. doi: 10.1016/j.joen.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Corbella S, Del Fabbro M, Tamse A, Rosen E, Tsesis I, Taschieri S. Cone beam computed tomography for the diagnosis of vertical root fractures: a systematic review of the literature and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118:593–602. doi: 10.1016/j.oooo.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 10.Hassan B, Metska ME, Ozok AR, van der Stelt P, Wesselink PR. Comparison of five cone beam computed tomography systems for the detection of vertical root fractures. J Endod. 2010;36:126–129. doi: 10.1016/j.joen.2009.09.013. [DOI] [PubMed] [Google Scholar]
- 11.Rosen E, Taschieri S, Del Fabbro M, Beitlitum I, Tsesis I. The diagnostic efficacy of cone-beam computed tomography in endodontics: a systematic review and analysis by a hierarchical model of efficacy. J Endod. 2015;41:1008–1014. doi: 10.1016/j.joen.2015.02.021. [DOI] [PubMed] [Google Scholar]
- 12.Talwar S, Utneja S, Nawal RR, Kaushik A, Srivastava D, Oberoy SS. Role of cone-beam computed tomography in diagnosis of vertical root fractures: a systematic review and meta-analysis. J Endod. 2016;42:12–24. doi: 10.1016/j.joen.2015.09.012. [DOI] [PubMed] [Google Scholar]
- 13.Draenert FG, Coppenrath E, Herzog P, Müller S, Mueller-Lisse UG. Beam hardening artefacts occur in dental implant scans with the NewTom cone beam CT but not with the dental 4-row multidetector CT. Dentomaxillofac Radiol. 2007;36:198–203. doi: 10.1259/dmfr/32579161. [DOI] [PubMed] [Google Scholar]
- 14.Vasconcelos KF, Nicolielo LF, Nascimento MC, Haiter-Neto F, Bóscolo FN, Van Dessel J, et al. Artefact expression associated with several cone-beam computed tomographic machines when imaging root filled teeth. Int Endod J. 2015;48:994–1000. doi: 10.1111/iej.12395. [DOI] [PubMed] [Google Scholar]
- 15.Queiroz PM, Santaella GM, da Paz TD, Freitas DQ. Evaluation of a metal artefact reduction tool on different positions of a metal object in the FOV. Dentomaxillofac Radiol. 2017;46:20160366. doi: 10.1259/dmfr.20160366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schulze R, Heil U, Gross D, Bruellmann DD, Dranischnikow E, Schwanecke U, et al. Artefacts in CBCT: a review. Dentomaxillofac Radiol. 2011;40:265–273. doi: 10.1259/dmfr/30642039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neves FS, Freitas DQ, Campos PS, Ekestubbe A, Lofthang-Hansen S. Evaluation of cone-beam computed tomography in the diagnosis of vertical root fractures: the influence of imaging modes and root canal materials. J Endod. 2014;40:1530–1536. doi: 10.1016/j.joen.2014.06.012. [DOI] [PubMed] [Google Scholar]
- 18.Wanderley VA, Neves FS, Nascimento MC, Monteiro GQ, Lobo NS, Oliveira ML, et al. Detection of incomplete root fractures in endodontically treated teeth using different high-resolution cone-beam computed tomographic imaging protocols. J Endod. 2017;43:1720–1724. doi: 10.1016/j.joen.2017.05.017. [DOI] [PubMed] [Google Scholar]
- 19.Fuss Z, Lustig J, Tamse A. Prevalence of vertical root fractures in extracted endodontically treated teeth. Int Endod J. 1999;32:283–286. doi: 10.1046/j.1365-2591.1999.00208.x. [DOI] [PubMed] [Google Scholar]
- 20.Queiroz PM, Groppo FC, Oliveira ML, Haiter-Neto F, Freitas DQ. Evaluation of the efficacy of a metal artifact reduction algorithm in different cone beam computed tomography scanning parameters. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;123:729–734. doi: 10.1016/j.oooo.2017.02.015. [DOI] [PubMed] [Google Scholar]
- 21.Helvacioglu-Yigit D, Demirturk Kocasarac H, Bechara B, Noujeim M. Evaluation and reduction of artifacts generated by 4 different root-end filling materials by using multiple cone-beam computed tomography imaging settings. J Endod. 2016;42:307–314. doi: 10.1016/j.joen.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 22.Bechara B, Alex McMahan C, Moore WS, Noujeim M, Teixeira FB, Geha H. Cone beam CT scans with and without artefact reduction in root fracture detection of endodontically treated teeth. Dentomaxillofac Radiol. 2013;42:20120245. doi: 10.1259/dmfr.20120245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bezerra IS, Neves FS, Vasconcelos TV, Ambrosano GM, Freitas DQ. Influence of the artefact reduction algorithm of Picasso Trio CBCT system on the diagnosis of vertical root fractures in teeth with metal posts. Dentomaxillofac Radiol. 2015;44:20140428. doi: 10.1259/dmfr.20140428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Junqueira RB, Verner FS, Campos CN, Devito KL, do Carmo AM. Detection of vertical root fractures in the presence of intracanal metallic post: a comparison between periapical radiography and cone-beam computed tomography. J Endod. 2013;39:1620–1624. doi: 10.1016/j.joen.2013.08.031. [DOI] [PubMed] [Google Scholar]
- 25.Soares CJ, Pizi EC, Fonseca RB, Martins LR. Influence of root embedment material and periodontal ligament simulation on fracture resistance tests. Braz Oral Res. 2005;19:11–16. doi: 10.1590/s1806-83242005000100003. [DOI] [PubMed] [Google Scholar]
- 26.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845. [PubMed] [Google Scholar]
- 27.Bechara B, McMahan CA, Geha H, Noujeim M. Evaluation of a cone beam CT artefact reduction algorithm. Dentomaxillofac Radiol. 2012;41:422–428. doi: 10.1259/dmfr/43691321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bechara BB, Moore WS, MacMahan CA, Noujeim M. Metal artefact reduction with cone beam CT: an in vitro study. Dentomaxillofac Radiol. 2012;41:248–253. doi: 10.1259/dmfr/80899839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Rezende Barbosa GL, Sousa Melo SL, Alencar PN, Nascimento MC, Almeida SM. Performance of an artefact reduction algorithm in the diagnosis of in vitro vertical root fracture in four different root filling conditions on CBCT images. Int Endod J. 2016;49:500–508. doi: 10.1111/iej.12477. [DOI] [PubMed] [Google Scholar]
- 30.Bueno MR, Estrela C, Azevedo BC, Diogenes A. Development of a new cone-beam computed tomography software for endodontic diagnosis. Braz Dent J. 2018;29:517–529. doi: 10.1590/0103-6440201802455. [DOI] [PubMed] [Google Scholar]
- 31.Fontenele RC, Nascimento EH, Santaella GM, Freitas DQ. Does the metal artifact reduction algorithm activation mode influence the magnitude of artifacts in CBCT images? Imaging Sci Dent. 2020;50:23–30. doi: 10.5624/isd.2020.50.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yamamoto-Silva FP, de Oliveira Siqueira CF, Silva MA, Fonseca RB, Santos AA, Estrela C, et al. Influence of voxel size on cone-beam computed tomography-based detection of vertical root fractures in the presence of intracanal metallic posts. Imaging Sci Dent. 2018;48:177–184. doi: 10.5624/isd.2018.48.3.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Özer SY. Detection of vertical root fractures by using cone beam computed tomography with variable voxel sizes in an in vitro model. J Endod. 2011;37:75–79. doi: 10.1016/j.joen.2010.04.021. [DOI] [PubMed] [Google Scholar]
- 34.Bechara B, McMahan CA, Moore WS, Noujeim M, Geha H, Teixeira FB. Contrast-to-noise ratio difference in small field of view cone beam computed tomography machines. J Oral Sci. 2012;54:227–232. doi: 10.2334/josnusd.54.227. [DOI] [PubMed] [Google Scholar]
- 35.Patel S, Brady E, Wilson R, Brown J, Mannocci F. The detection of vertical root fractures in root filled teeth with periapical radiographs and CBCT scans. Int Endod J. 2013;46:1140–1152. doi: 10.1111/iej.12109. [DOI] [PubMed] [Google Scholar]
- 36.Brady E, Mannocci F, Brown J, Wilson R, Patel S. A comparison of cone beam computed tomography and periapical radiography for the detection of vertical root fractures in nonendodontically treated teeth. Int Endod J. 2014;47:735–746. doi: 10.1111/iej.12209. [DOI] [PubMed] [Google Scholar]
- 37.da Silveira PF, Vizzotto MB, Liedke GS, da Silveira HL, Montagner F, da Silveira HE. Detection of vertical root fractures by conventional radiographic examination and cone beam computed tomography - an in vitro analysis. Dent Traumatol. 2013;29:41–46. doi: 10.1111/j.1600-9657.2012.01126.x. [DOI] [PubMed] [Google Scholar]