We read with great interest the excellent article titled “Unilateral axillary Adenopathy in the setting of COVID-19 vaccine” by Mehta et al. in the January 2021 issue of Clinical Imaging.1 The authors describe the phenomenon of unilateral axillary lymphadenopathy related to Covid-19 vaccine injection in the ipsilateral arm, having encountered four cases on sonography during routine breast imaging since the initiation of Covid-19 vaccination programmes. Lack of knowledge of this phenomenon can lead to erroneous diagnosis of metastatic nodal disease.
We recently encountered the same issue in our practice, in a fifty-year-old male patient who underwent PET/CT to investigate for metastatic disease. Several unilateral FDG avid axillary lymph nodes were identified (Fig. 1 ), which was incongruent with the site of the primary malignancy and the otherwise normal study. This posed a diagnostic dilemma, before further inquiry revealed the patient had been inoculated with a second dose of the Pfizer mRNA Covid-19 vaccine in the ipsilateral arm 10 days prior.
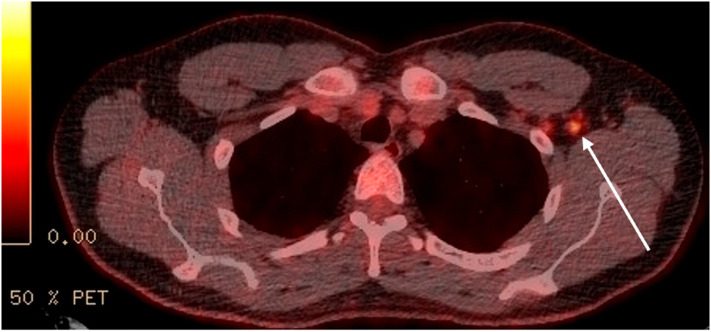
Fig. 1.
PET/CT demonstrating FDG avid left axillary lymphadenopathy in a fifty year old man, 10 days after inoculation with Pfizer mRNA Covid-19 vaccine in the ipsilateral arm.
The incidence of axillary lymphadenopathy following vaccination was as high as 16% in clinical trials.2 As mass vaccination programmes become established it is likely that we will see the prevalence of reactive unilateral axillary lymphadenopathy rise over the coming months, which will be apparent across a spectrum of modalities including CT, MRI, ultrasound and PET/CT. It is important that radiologists are aware of this finding to avoid over staging patients.
We commend the authors for raising awareness of this phenomenon, which will help reduce unnecessary invasive investigations and patient anxiety.
Funding sources
None.
Declaration of competing interest
No disclosures.
References
- 1.Mehta N., Sales R., Babagbemi K., et al. Unilateral axillary adenopathy in the setting of COVID-19 vaccine. Clin Imaging. 2021;75:12–15. doi: 10.1016/j.clinimag.2021.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Local Reactions, Systemic Reactions, Adverse Events, and Serious Adverse Events . Cdc.gov; 2021. Moderna COVID-19 Vaccine|CDC [Internet]https://www.cdc.gov/vaccines/covid-19/info-by-product/moderna/reactogenicity.html [cited 14 February 2021]. Available from: [Google Scholar]