Abstract
The radiology department was categorized as a “high risk area” during the severe acute respiratory syndrome (SARS) outbreak in 2003 and is similarly considered a “high risk area” during the current coronavirus (COVID-19) pandemic. The purpose of infection control is to isolate patients with suspected or confirmed COVID-19 from uninfected people by utilizing separate equipment, spaces, and healthcare workers. Infection control measures should be prioritized to prevent the nosocomial spread of infection. We established a COVID-19 infection control team in our radiology department. The team's responsibilities include triaging patients with confirmed or suspected COVID-19, performing imaging and reporting, using dedicated equipment, disinfecting the equipment and the immediate environment, and staff scheduling.
Keywords: COVID-19, Coronavirus, Guidelines, Infection control, Radiology
Introduction
The COVID-19 pandemic has proven to be a challenging time for hospitals around the world. A large influx of patients in many countries has overwhelmed staff and resources. Administrators have had to rapidly devise strategies to handle the surge in patient volume. While these strategies were initially aimed at maintaining organization and conserving resources, it quickly became apparent that infection control measures also had to be implemented. Otherwise, spread of the virus to uninfected patients and hospital staff would occur unabated.
One location within the hospital that is of particular risk for COVID-19 spread to occur is the radiology department. Because hospital staff, infected patients, and non-infected patients all traverse the radiology department, the risk of nosocomial infection is high. Indeed, infection of hospital staff and initially non-infected patients by infected patients has been documented to have occurred in the radiology department.1 , 2 To combat this risk, certain measures can and should be taken. Some radiology departments around the world have described in the literatures the specific practices that have led to their success. These practices include defining safe and unsafe zones within the department, designating certain equipment for use on infected patients only, predetermining safe transfer routes between a patient's room and the radiology department, and imaging infected patients within a set time window only.3, 4, 5 In some regions, lack of understanding amongst hospital staff about how COVID-19 is transmitted may increase the risk of nosocomial infection, and therefore education is also an important part of any successful infection control strategy.1 , 3
Taiwan's experience with SARS allowed us to seamlessly implement management and infection control strategies during the COVID-19 outbreak. Based on the SARS infection control guidelines issued by the Taiwan Centers for Disease Control, radiology departments and all imaging rooms are classified as high-risk areas of the hospital. Top-down management and infection control strategies focus exclusively on the isolation of patients with suspected or confirmed COVID-19 from non-infected patients by utilizing separate paths, spaces, equipment, and staff. To prevent cross-infection within a hospital, infection control measures between staff in the department should be carried out daily. Staff who are in direct contact with patients who are suspected or confirmed to be infected must work as a group but apart from other staff.
Successful management and infection control with regards to SARS or COVID-19 relies on adherence to procedures by all departmental staff. More importantly, frontline healthcare workers should be provided with sufficient personal protective equipment (PPE) and administrative support.6, 7, 8, 9 The dedication and commitment of every staff member is also important to ensure that high-quality care is provided to all patients.10, 11, 12, 13, 14
Our hospital regularly maintains 15 functional negative pressure isolation rooms as well as 730 general inpatient beds, with a bed turnover rate averaging 7 days. On a daily basis, the hospital sees approximately 4500 outpatients and 150 emergency patients. During the initial wave of COVID-19 pandemic, we performed 100–450 chest X-rays monthly on patients at fever stations or in isolation rooms.
In this article, we share the COVID-19 management and infection control practices utilized by our radiology department, emphasizing the ‘double zero’ infection control goal and step-by-step practices to achieve it.
Establishment of a COVID-19 response team
The COVID-19 response team in the radiology department should be led by the department head and be composed of a chief technologist, a lead nurse, an administrative staff leader, and a frontline worker representative.
Goal
Our objective is the ‘double zero’ goal during the COVID-19 outbreak: zero cross-infections between patients and zero nosocomial infections among the departmental staff.
Staff responsibilities
-
1.Department Chair/Vice-Chair:
-
(a)Follow the hospital infection control policy and coordinate with other departments in implementing infection control concepts and procedures in the radiology department.
-
(b)Establish and implement radiology infection control practices that are consistent with the hospital infection control policy.
-
(c)Chair weekly meetings to coordinate various professional leaders for management and infection control in the radiology department.
-
(d)Provide information regarding infection control and updated polices to all staff members.
-
(e)Ensure that workplaces are clean and hygienic in the radiology department.
-
(a)
-
2.Staff radiologists/residents:
-
(a)Staff radiologists communicate with clinicians who order imaging examinations and provide image interpretation, perform interventional procedures, and supervise radiology residents with regards to infection control.
-
(b)Radiology residents perform examinations and provide initial interpretations, reporting under the supervision of staff radiologists.
-
(a)
-
3.Radiological technologists:
-
(a)The chief technologist coordinates and monitors infection control procedures performed by all radiological technologists. It is important that technologists are appropriately grouped during scheduling of staff who will be performing portable X-rays on patients with suspected or confirmed COVID-19. The chief technologist will also attend daily institutional COVID-19 meetings and inform the response team of updated messages or policies.
-
(b)Other radiological technologists should follow operating procedures during all examinations. Senior technologists are responsible for training junior technologists in the use of portable X-ray devices.
-
(a)
-
4.Nurses:
-
(a)The lead nurse coordinates and monitors infection control maneuvers performed by the nursing staff and should work with the hospital infection control team to set up management and infection control procedures for the radiology department. The lead nurse should assign a team member to monitor, record, and report on stored PPE in the radiology department.
-
(b)Nursing staff in the radiology department is fixed. All nurses triage patients and practice environmental infection control in the radiology department. They should strictly follow infection control guidelines when performing disinfection procedures before, during, and after examinations of patients with suspected or confirmed COVID-19.
-
(a)
-
5.Administrative staff:
-
(a)The administrative leader coordinates and monitors administrative support for all frontline workers.
-
(b)The front desk reception staff double checks the screening procedures for patients who have differing imaging needs. An on-duty nurse will back up the front-desk staff when they require professional help.
-
(a)
-
6.
Cleaning staff:
A non-rotating cleaning staff member will disinfect the spaces dedicated to suspected or confirmed COVID-19 patients in the department. A senior nurse will train the staff member and ensure compliance with infection prevention practices.
Duty shift
-
1.
Radiological technologists responsible for COVID-19 examinations are divided into 2 groups of 2 staff members who work 8 h per shift. The COVID-19 group manages patients under investigation (PUIs) at the fever station and takes those who are confirmed positive to a negative pressure room. After imaging confirms that a patient is positive, the technologist should shower before returning to the department.
-
2.
Pregnant technologists will not be scheduled to perform portable examinations.
-
3.
Radiology residents rotate along with the technologists managing suspected or confirmed COVID-19 patients and are supervised by a senior staff member.
Building team accountability
The department head and team leaders meet weekly to ensure that effective reporting, communication, and feedback systems are in alignment with the ‘double zero’ goal and that quality of patient care is maintained.
-
1.
The radiology residents review and present X-rays or CT images (if any) of patients with suspected or confirmed COVID-19 to the attending radiologists. The chest radiologist (a rotating position) and a resident present COVID-19 updates to the response team.
-
2.
The lead nurse reports on the use and remaining stock of PPE (the safety stock for the department is 20 days), the physical status of departmental staff, and reflections from the frontline staff or patients (if any).
-
3.
The chief technologist reports on the number of portable X-rays or CT scans performed on patients with suspected or confirmed COVID-19, the emotional health status of staff members, and any updates regarding workflow from the daily institutional briefing.
-
4.
The administrative leader reports on departmental costs and revenues as well as individual rewards for frontline healthcare workers who perform mobile X-rays in negative pressure rooms or at a fever stations or who perform procedures on patients.
-
5.
The department head should ensure that efforts are performed from the bottom up and provide support as needed. Important information should be immediately posted to the departmental bulletin board.
Patient triage
The purpose of patient triage is to recognize patients with suspected COVID-19 as early as possible. Risk assessment begins at the hospital entrance, where well-trained staff first encounter patients. Every person entering the hospital should wear a face mask. Upon arrival, each patient receives a case identification through their national health insurance card, which also links to that patient's immigration and travel data. Patients are subsequently screened for a history of close contact with others who have had suspected or confirmed COVID-19 or respiratory symptoms, a loss of taste and/or smell, or diarrhea (after April 5). To avoid touching, checklists were completed by hospital staff using a computer system to help visitors.
Finally, every person entering through the main hospital entrance or through the emergency department is scanned with an infrared thermal camera. Body temperatures at or above 37.50 °C are confirmed using a tympanic thermometer.
All patients are classified into one of three groups based on risk level, and each is guided through a separate pathway for imaging (Table 1, Table 2 ).
-
1.
Patients with laboratory-confirmed COVID-19 are taken to an isolation room by well-trained hospital staff dressed in PPE. Once the patient is in the isolation room, a radiological technologist performs imaging as necessary using a portable X-ray device. The on-duty technologist in the COVID-19 group follows tertiary protection procedures during imaging when imaging is absolutely necessary.
-
2.
Patients with suspected COVID-19 and PUIs are taken to the fever station by well-trained hospital staff dressed in PPE. The fever station is located outside the emergency room. Patients are not permitted to enter the hospital at this point and are instead guided to the fever station via a route that is entirely exterior to the hospital. Patients are then imaged using a portable X-ray device (if needed) at the fever station. Imaging staff adopt secondary protection.
-
3.
Uninfected patients are imaged according to routine procedures. The frontline healthcare worker employs primary protection.
Table 1.
The use of personal protective equipment (PPE) in performing examinations in a radiology department.
| Protection grade | PPE level | Applicable staff |
|---|---|---|
| Primary protection | Surgical mask or N95 mask |
|
| Secondary protection | Surgical mask or N95 mask + goggles +1 layer of long-sleeved gown +1 layer of gloves (must cover sleeves) | Those who perform exams using a ‘physical touch’ with non-suspect patients |
| Tertiary protection | Head cover (fluid-repellent cap) + N95 mask + goggles & face shield + 2 layers of protective gown (inner long-sleeved + outer waterproof) + 2 layers of gloves (powder free, must cover sleeves) + shoe covers | Those who perform exams of suspect/confirmed patients in a negative pressure room, fever screening station, or any exam room |
Table 2.
Coronavirus disease 2019 (COVID-19) case as defined by the World Health Organization.
| Suspect case |
|
|
|
| Probable case |
|
|
| Confirmed case |
| A person with laboratory-confirmed COVID-19 infection irrespective of clinical signs and symptoms. |
| Person Under Investigation (PUI)a |
| Any person who is currently under investigation for having COVID-19 (a suspect case) or who was under investigation but whose test results are negative or inconclusive (a probable case). |
PUI is a category specified by the Centers for Disease Control.
Imaging studies and workflow
Imaging indications
All imaging examinations must be used only for clinical problem-solving. Any procedures likely to induce coughing should be avoided if possible, and if not, should be performed cautiously. People arriving for health screening exams (e.g., mammograms) are scheduled in separate time slots and with different equipment.
-
1.
X-rays
-
(a)
Current evidence does not indicate that findings on chest X-ray appear before fever or positive RT-PCR tests in people with COVID-19.10 Chest X-ray lacks sensitivity for the detection of the subtle ground glass appearance of early pulmonary COVID-19 and is therefore not useful for the screening of asymptomatic PUIs.
-
(b)
X-rays are required for PUIs without apparent fever (<380C) but who have been bedridden long term, are elderly, or have kidney disease, cancer, diabetes, or have undergone steroid treatment.
-
2.
CT scans
-
(a)
A CT scan is not used to screen for or as a first-line test to diagnose COVID-1910 because the CT room requires deep cleaning before subsequent examinations can be performed and because the images lack specificity for COVID-19.
-
(b)
When a CT scan is absolutely necessary for an infected person with COVID-19, appropriate infection control should be vigorously followed before, during, and after the procedure. Use of a contrast agent is discouraged.
-
3.
Interventional procedures
-
(a)
Elective interventional procedures are postponed unless the procedure is absolutely urgent and necessary.
-
(b)
When not urgent, procedures are discouraged because they consume PPE and other resources and cause delays in procedures on other patients that are absolutely urgent and necessary. Our interventional radiologists must fully discuss the necessity of the procedure with the ordering physician and, on a case-by-case basis, judge the risks and benefits to postponing the procedure.
-
4.
Ultrasound
-
(a)
Ultrasound is not used as a first-line test to solve clinical problems related to suspected or confirmed COVID-19.
-
(b)
Healthcare workers or sonographers must wear secondary PPE when performing examinations on patients without COVID-19.
Prioritization of exams
-
1.
Patients with confirmed COVID-19 are imaged in a negative pressure room and are scheduled for the morning after the order is submitted, if it is received by 9:30 pm the day prior. Portable exam equipment will be used. Stat orders are reserved exclusively for emergencies.
-
2.
The PUIs at the fever screening station are imaged in order of suspicion from low to high. Portable X-ray equipment is used to perform the imaging during a specific time slot every 1–2 h.
-
3.
Uninfected people are scheduled for imaging exams or interventional procedures as usual.
Exam workflow
-
1.
X-rays
X-rays are not used to triage patients or screen PUIs. Additionally, they are not used for daily follow-up of patients with mild COVID-19. X-ray exams are performed approximately every 2–3 days during the hospitalization.
-
(a)
Three portable X-ray devices are used. One in the negative pressure room, one at the outdoor fever screening station, and one in other wards for uninfected patients.
-
(b)
A chest PA projection and a lateral view are obtained unless a different view is absolutely necessary. Digital wireless systems are used for all imaging.
-
(c)
Patients with mild cases should be examined before those with severe cases.
-
(d)
Healthcare workers must wear tertiary PPE when imaging a person with COVID-19 in an isolation room.
-
2.
CT exams
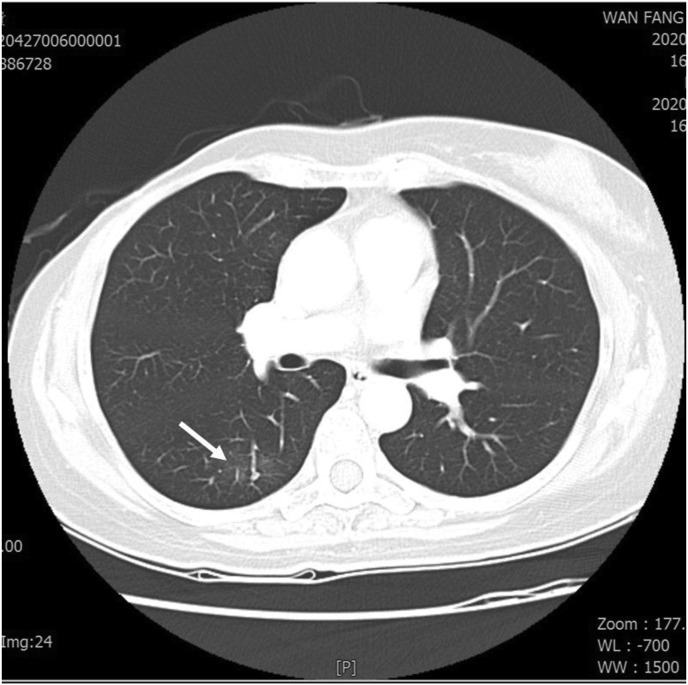
Chest CT is not used to triage patients, screen PUIs, or diagnose patients with confirmed COVID-19 unless they are at risk for disease progression or display persistent RT-PCR (polymerase chain reaction) positivity during hospitalization. Pulmonary COVID-19 usually manifests on chest CT as scattered areas of peripherally predominant ground glass. Typical findings are shown in Fig. 1 .
-
(a)
In principle, transferring a patient with COVID-19 from the negative pressure room should be avoided.
-
(b)
If a CT examination can solve a clinical problem or if the imaging results can change the treatment, patients may leave the negative pressure room for the CT examination.
-
(c)
If a patient must be transferred, an N95 mask should be donned, and the patient should cooperate with infection control procedures, following the transport route as determined by the hospital's infection control office.
-
(d)
Independent ventilation supplies the CT room. Healthcare workers must wear tertiary PPE when performing the CT scan.
-
3.
Interventional imaging
-
(a)
Patients with confirmed COVID-19 should don N95 masks and cooperate with infection control procedures, following the transport route as determined by the hospital's infection control office.
-
(b)
All interventional radiologists and healthcare workers must wear tertiary PPE when performing aerosol-generating procedures, caring for patients who are at risk for the mechanical dispersal of aerosols in the IR room, and during cardiopulmonary resuscitation.
-
(c)
Independent ventilation supplies the angiography room.
Figure 1.
High resolution CT scan of chest shows a focal ground glass opacity (arrow) at lower lobe of right lung in a COVID-19 patient with underlying disease of right-side breast cancer, status post operation and chemotherapy.
Spatial and personnel control
-
1.
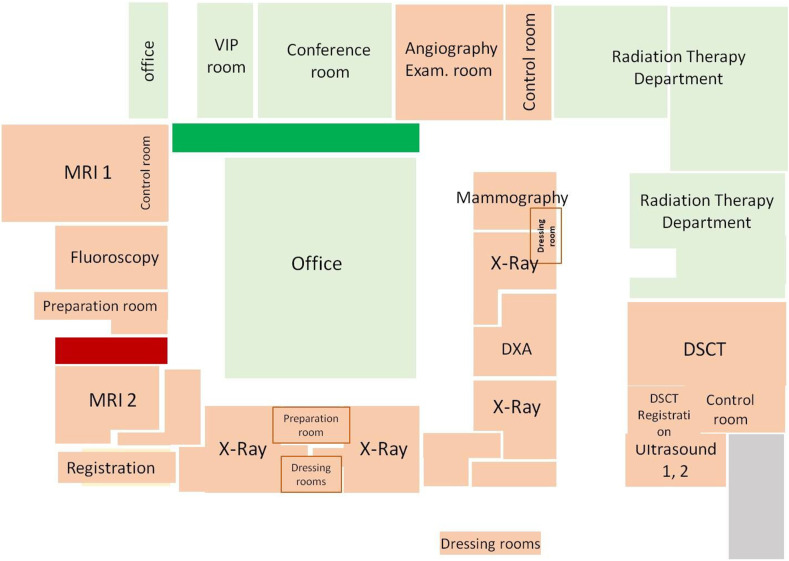
The departmental space is divided into two zones (Fig. 2). The ‘risk’ zone comprises the imaging rooms, corridors, and counter; all staff should don secondary protection, and eating and drinking are prohibited. The ‘clean’ zone comprises the film reading room, meeting room, pantry, and offices; all staff members should don primary protection.
-
2.
All uninfected patients should undergo their examinations at noon (12:00 pm−2:00 pm) to prevent cross-contamination with outpatients and to therefore reduce the risk of nosocomial infection.
-
3.
Patients with confirmed COVID-19 will be examined last in the daily schedule.
-
4.
Conversation during meals is avoided, and staff members are seated with their backs toward one another. Eating and drinking are not allowed during daily conferences and educational meetings.
-
5.
Inter-departmental meetings are suspended, and video conferencing is used for real-time discussions.
-
6.
Visitors, including food delivery workers and family, are not allowed in the department; they can be met in the waiting area.
-
7.
All meetings or events are to be scaled down in terms of attendance. Alternatively, the online platform Zoom is used to conduct live meetings.
Figure 2.
Illustration of the two zones in our department space. Within the ‘risk’ zone (coral), all staff should don secondary protection, eating and drinking are prohibited. In the ‘clean’ zone (lime), all staff should don primary protection. Exit routes (green, clean zone; apple, risk zone).
Disinfection of the environment and equipment
-
1.
Seats will be arranged so that participants are at least 1 m apart in the waiting area.
-
2.
The on-duty radiological technologist for each imaging room will spray and wipe the exam table and imaging plate holder immediately after each exam is completed. The same disinfectant (75% alcohol) is regularly (3 times daily) used on equipment, room doors, and waiting room seats.
-
3.
At each workspace, all healthcare staff regularly (3 times daily) take turns using 75% ethyl alcohol to spray and wipe the surfaces of desks and tables, door handles, telephone keypads, handsets, and computer keyboards.
-
4.
All reception desks, imaging rooms, offices, counters, store rooms, and film reading rooms will have dispensers containing sanitizing hand disinfectant that are regularly refilled.
-
5.
The doors of every room (except the imaging rooms) are kept open to reduce the chance that door handles become contaminated.
-
6.
Hospital cleaning staff will use bleach prepared by the hospital infection control team to disinfect the floor daily.
-
7.
After all imaging is complete, 75% alcohol will be used to thoroughly wipe the imaging equipment and any other paraphernalia (chairs, electrical wires, plugs, etc.) Bleach can cause rust, so alcohol is preferred.
Audit
In addition to complying with infection control and protection rules in the hospital and the department, staff can strengthen safety protocols through audit.
-
1.
When radiological technologists perform portable imaging in a negative pressure room, two people must be present. One is responsible for imaging, and the other will supervise and assist.
-
2.
Two people should not simultaneously put on PPE. One person should gown up while the other supervises that process. It is best if one person at a time dresses according to protocol (Table 3 ), and head gowning (donning masks, head covers, and face shields) should take place in front of a mirror. A healthcare worker that has finished gowning up can then supervise others while they gown up. Similar procedures are to be followed for degowning.
-
3.
In addition to emphasizing supervision during gowning, senior staff should begin leading less experienced staff in gowning drills. Every staff member should practice gowning at least five times, and staff should confirm that they are familiar with the gowning procedure before they can work in a negative pressure room.
-
4.
All departmental staff should measure and record their oral temperatures daily at 10 am. Each staff member should have a personal oral thermometer, and after each use, it will be disinfected using a swab with 75% alcohol. The COVID-19 team must report to the Department Head and Infection Control Office when an oral temperature reading from a staff member exceeds 38 °C. The febrile staff member should then be sent to the fever station for further management. The same applies if a staff member develops respiratory symptoms of unknown cause.
Table 3.
Proper don, use, and doff procedures for personal protective equipment (PPE) by radiology professionals when performing examinations in areas with COVID-19.
| Procedure | Actions |
|---|---|
Allocate portable X-ray equipment for a nursing station
|
Sign in at Control Point Step 1 – Wash hands Step 2 – Ensure all PPE items are available in your size |
Inner protective layer
|
Step 1 – Put on properly fitted lead apron Step 2 – Put on long sleeved, fluid-repellent, disposable inner protective gown Step 3 – Put on inner surgical latex gloves (covering the sleeves of the protective gown) |
Outer protective layer |
Step 1 – Put on coverall back fastening, fluid-resistant outer protective gown (e.g., Tyvek suit) Step 2 – Put on and secure fluid-repellent cap Step 3 – Wash hands Step 4 – Put on N95 mask and check fit Step 5 – Put on goggles Step 6 – Put on full-face shield Step 7 – Put on outer gloves with long tight-fitting cuffs (must completely cover the sleeves of the protective gown) |
| Buddy–buddy check Protective cover for X-ray equipment 
|
Step 1 – Check each other's PPE Step 2 – Buddy writes your name on your outer gown and vice versa |
| Open door, enter, and keep door of the isolation room closed | Perform exam |
Before leaving the isolation room
|
Step 1 – Remove first plastic layer from the cassette and discard in the infectious waste bin in the isolation room (do not discard in the anteroom) Step 2 – Move the portable device to the ante room and close the door Step 3 – Remove the outer layer of gloves and discard in the infectious waste bin in the isolation room (do not discard in the anteroom) |
| Step 1 – Remove goggles, put in 75% alcohol for soaking Step 2 – Remove protective gown (from the clean side) Step 3 – Remove surgical mask Step 4 – Remove head cover, shoe cover, and hood Step 5 – Remove second layer of gloves Step 6 – Remove last layer of gloves, and use 75% alcohol to wipe the X-ray machine (Spray alcohol on a cloth and use it to wipe the machine, taking care not to spray alcohol directly onto the machine) Step 7 – Push the X-ray machine to the fixed position |
|
Before nursing station
|
Step 1- Remove inner isolation gown and last pair of gloves Step 2- Wash hands Step 3- Step on disinfection mat |
| Open the door and enter the nursing station | Step 1 – Using a hand towel to hold the door handle, push the door open and enter the nursing station Step 2 – Remove N95 mask Step 3 – Wash hands Step 4 – Put on new N95 mask |
Self-care
-
1.
Each staff member should maintain sufficient sleep, a balanced diet, and a positive mood. Any physical or psychological discomfort should be reported to the chief technician who should subsequently adjust that person's work schedule with the portable examination equipment. Staff should immediately reveal to the chief technician any lapses in focus so that suitable manpower adjustments can be made.
-
2.
Work attire is not to be worn home.
Conclusion
The establishment of management and infection control practices in a radiology department is only the first step. Continuous on-the-job education and training, supervision and audit mechanisms, and increasing awareness are key factors to ensure achievement of the ‘double zero’ goal.
Advances in knowledge
Patients with suspected or confirmed COVID-19 should be isolated from non-infected patients by utilizing separate paths, spaces, equipment, and staff. Frontline healthcare workers should be provided with sufficient personal protective equipment.
Author contributions
W.P.C. made substantial contributions to conception and study design; M-S.Y., M-F.L., H-C.C., R.O.K., W-S.L. contributed to data acquisition, analysis, or interpretation; W.P.C. composed the first draft. All authors made critical revisions related to important intellectual content, and all approved the final version for publication and agreed to be accountable for all aspects of the work and so appropriately investigate and resolve questions related to the accuracy and integrity of any part of the work.
Funding
The authors state that this work has not received any funding.
Declaration of competing interest
None declared.
Acknowledgments
The authors thank the Infection Control Office of Wan Fang Hospital for guidance.
References
- 1.Sheng W.H., Ko W.C., Huang Y.C., Hsueh P.R. SARS-CoV-2 and COVID-19. J Microbiol Immunol Infect. 2020;53:363–364. doi: 10.1016/j.jmii.2020.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee P.I., Hsueh P.R. Emerging threats from zoonotic coronaviruses-from SARS and MERS to 2019-nCoV. J Microbiol Immunol Infect. 2020 Feb 4;S1684–1182(20):30011–30016. doi: 10.1016/j.jmii.2020.02.001. [Epub ahead of print].PMID: 32035811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chou C.C., Shen C.F., Chen S.J., Chen H.M., Wang Y.C., Chang W.S., et al. Recommendations and guidelines for the treatment of pneumonia in Taiwan. J Microbiol Immunol Infect. 2019;52:172–199. doi: 10.1016/j.jmii.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 4.Yen M.Y., Schwartz J., Chen S.Y., King C.C., Yang G.Y., Po-Ren Hsueh. Interrupting COVID-19 transmission by implementing enhanced traffic control bundling: implications for global prevention and control efforts. J Microbiol Immunol Infect. 2020;53:377–380. doi: 10.1016/j.jmii.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang C.J., Chen T.C., Chen Y.H. The preventive strategies of community hospital in the battle of fighting pandemic COVID-19 in Taiwan. J Microbiol Immunol Infect. 2020;53:381–383. doi: 10.1016/j.jmii.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taiwan Centers for Disease Control The facts regarding Taiwan's email to alert WHO to possible danger of COVID-19. 2020. https://www.cdc.gov.tw/En/Bulletin/Detail/PAD-lbwDHeN_bLa-viBOuw?typeid=158 Available via.
- 7.Gorbalenya A.E., Baker S.C., Baric R.S. bioRxiv (preprint); 2020. Severe acute respiratory syndrome-related coronavirus: the species and its viruses—a statement of the Coronavirus Study Group. [DOI] [Google Scholar]
- 8.World Health Organization . 2020. WHO timeline - COVID-19.https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19 Available via. [Google Scholar]
- 9.World Health Organization Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. Scientific Brief. 2020 https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations 29 March 2020. Available via. [Google Scholar]
- 10.World Health Organization Coronavirus disease (COVID-19) outbreak situation, as of 5 June 2020. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019?gclid=EAIaIQobChMIkfb_ja3s6QIVFXZgCh3VzAs0EAAYASAAEgKaQvD_BwE Available via.
- 11.Cheng S.C., Chang Y.C., Fan Chiang Y.L. First case of coronavirus disease 2019 (COVID-19) pneumonia in Taiwan. J Formos Med Assoc. 2020;119:747–751. doi: 10.1016/j.jfma.2020.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive eesting. J Am Med Assoc. 2020 doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 13.Taiwan Centers for Disease Control 2020. https://www.cdc.gov.tw/En/Bulletin/Detail/cbvWKr36Rrs0v1DAjc0dCg?typeid=158 Available via.
- 14.ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection Available via.