Abstract
This study investigated the effects of weather conditions, air pollutants, and the air quality index (AQI) on daily cases of COVID-19 in the Bangkok Metropolitan Region (BMR). In this research, we collected data from January 1 to March 30, 2020 (90 days). This study used secondary data of meteorological and air pollutant parameters obtained from the Pollution Control Department of the Ministry of Natural Resources and Environment as well as daily confirmed COVID-19 case data in the BMR obtained from the official webpage of the Department of Disease Control, Ministry of Public Health, Thailand. We employed descriptive statistics, and Spearman and Kendall rank correlation tests were used to investigate the associations of weather variables, air pollutants, AQI with daily confirmed COVID-19 cases. Our findings indicate that CO, NO2, SO2, O3 PM10, PM2.5, AQI have a significantly negative association with daily confirmed COVID-19 cases in the BMR, whereas meteorological parameters such as temperature, relative humidity (RH), absolute humidity (AH) and wind speed (WS) showed significant positive associations with daily confirmed COVID-19 cases in the BMR. Our study is a useful supplement to encourage regulatory bodies to promote environmental strategies, as air pollution regulation could be a sustainable policy for mitigating the harmful effects of air pollutants. Furthermore, this study provides new insights into the relationship between daily meteorological factors, AQI, and air pollutants and daily confirmed COVID-19 cases in the BMR. These data may provide useful information to the public health authorities and decision makers in Thailand, as well as to the World Health Organization (WHO), in order to set proper strategic aimed at reducing the impact of the COVID-19. Future studies concerning SARS-CoV-2 and other viruses should investigate the possibility of infectious droplet dispersion in indoor and outdoor air during and after the epidemic outbreak.
Keywords: SARS-CoV-2, Wind speed, Absolute humidity, Transmission, Air pollution, COVID-19
1. Introduction
The 2019 novel coronavirus disease is called SARS-CoV-2 (COVID-19) and has become a deadly pandemic. The nature and transmission of COVID-19 are not explicit. The COVID-19 outbreak started in December 2019 in Wuhan city, Hubei Province, China (Chauhan and Singh, 2020). SARS-CoV-2 rapidly spread throughout China and to many countries (Ju et al., 2021) and has become a global public health problem (Zhu et al., 2020). In Thailand, the first official announcement of confirmed COVID-19 cases was reported on 12 January 2020 (DDC, 2020). In 2000, a positive relationship between air pollution and the case fatality rate of SARS-CoV-1 was reported in the People's Republic of China during the coronavirus epidemic (Cui et al., 2003), and it has been reported that the optimum temperature range associated with SARS cases was between 16 °C and 28 °C; temperatures within this range may enhance virus growth (Tan et al., 2005). In 2020, a study by Setti et al. (2020) carried out in Italy determined the geographical distribution of daily PM10 exceedance and the initial spreading of COVID-19 in 110 Italian provinces.
Several current studies state that chronic exposure to certain air pollutants leads to more severe COVID-19 and complicates the recovery of persons infected with this disease (Domingo et al., 2020). Recently, studies on the effects of meteorological factors showed that average temperature, relative humidity (RH), wind speed (WS), and absolute humidity (AH) have significant positive associations with the number of confirmed COVID-19 cases in Bangladesh (Islam et al., 2020a). Studies on ambient temperature and COVID-19 infection found that, at temperatures below 3 °C, each 1 °C rise was associated with a 4.86% increase in COVID-19 cases in China (Xie and Zhu, 2020). Recently, Wu et al. (2020a) reported that an increase of only 1 μg/m3 in PM2.5 was associated with an 11% increase in COVID-19 death (95% CI, 6%–17%). An increase in the long-term-averaged PM2.5 of 1 m3 was associated with a 12% increase in COVID-19 cases in England (Travaglio et al., 2021), and long-term exposure to outdoor air pollutants is known to cause chronic lung inflammation, which may influence the increased severity of COVID-19 disease due to SARS-CoV-2 (Coker et al., 2020). When the combustion of carbonaceous fuels is incomplete, air pollutants are released, and the AQI and meteorological conditions increase (Fazlzadeh et al., 2015). CO measurements could provide potentially useful information on different anthropogenic activities (Hanaoka and Masui, 2020). Furthermore, a rise in CO concentrations could be associated with much lower rainfall amounts observed during the study period in a given region (Bedi et al., 2020); increased CO concentrations have been reported to affect the respiratory system, lungs, and blood and central nervous systems, and exposure to CO leads to several health consequences based on the health and physiological conditions of the exposed person, the pollutant concentration, and the time of exposure (Reboul et al., 2012; WHO, 2010). In addition, prolonged exposure to air pollution, even in young and healthy subjects, results in the stimulation of chronic inflammation (Conticini et al., 2020). In particular, particulate contamination impacts the human airway, possibly promoting viral infections and increasing vulnerability to infections (Chen et al., 2020; Mehmood et al., 2020). Thus, populations exposed to high concentrations of PM2.5 particles are more prone to developing chronic respiratory conditions that are favourable to infective agents (Mehmood et al., 2020). Moreover, it has been found that long-term exposure to ambient air pollution might increase COVID-19 mortality (Hoang and Tran, 2020, Wu et al., 2020a). Air pollution concerning meteorological conditions may affect the trends of severe acute respiratory syndrome viral outbreaks by altering host immunity and the survival of viruses (Cai et al., 2007). Scholars have recently been examining a potential correlation between air pollution and the COVID-19 outbreak. This literature evaluates various studies on this particular topic (Dutheil et al., 2020; Frontera et al., 2020a, 2020b; Martelletti and Martelletti, 2020; Zhu et al., 2020; Zoran et al., 2020), as well as studies on COVID-19, air pollution and meteorology—an intricate relation (Srivastava, 2021). Several studies worldwide have shown that humidity plays a crucial role in morbidity and mortality due to COVID-19 (Srivastava, 2021). Moreover, the AQI, PM2.5, NO2, and temperature are variables that could promote the sustained transmission of COVID-19 (Li et al., 2020). However, it has not yet been confirmed whether the virus remains viable and virulent on particulate matter surfaces (Srivastava, 2021), and the influences of weather and air pollutant factors are unclear, especially on SARS-CoV-2. To date, the roles of air pollution and meteorological factors on virus transmission are not clear (Lolli et al., 2020). The primary source of air pollution in Bangkok and its vicinity is traffic, followed by industry. Moreover, burning in the open and temperature inversion, coupled with a calm wind, causes air pollution to accumulate in large quantities. This phenomenon was observed on certain days from winter to early summer and is a significant cause of abnormal PM2.5 levels during this period. This pollution, together with the current case rates showing the BMR as the region with the highest number of confirmed COVID-19 cases, therefore highlights Bangkok as a choice study area for this research.
The present study in Thailand on the relations of weather factors and air pollutants with the COVID-19 outbreak is also quite limited. Hence, the following study aimed to assess air quality and to understand and prevent the transmission of SARS-CoV-2. Here, we propose a hypothesis linking meteorological factors, the AQI, and air pollutants (CO, NO2, SO2, O3, PM10, PM2.5) with confirmed cases of COVID-19. Thus, in this study, we examined the weather condition, AQI, and air pollutant conditions with daily confirmed COVID-19 cases in the Bangkok Metropolitan Region, Thailand, and the results could have significant implications for healthcare policymakers during and after the pandemic.
2. Materials and methods
2.1. Study area
The Bangkok Metropolitan Region (BMR) is the capital of the Kingdom of Thailand (Fig. 1 ) and sits in the province in central Thailand with the coordinates of 13°45′ north latitude and 100°28′ east longitude. The city is located in the Chao Phraya River delta in the central part of the country, which extends to the Gulf of Thailand and had an estimated population of 5.67 million as of December 2019. The BMR occupies 1567.77 km2 (urban area) and has a population density of 3614 people/km2 (Administrative Strategy Division, 2019). The BMR is a tourism centre in Southeast Asia, comprising Bangkok, which is currently growing at a rate of 2.3% per year (https://worldpopulationreview.com/world-cities/bangkok-population). The Thai Meteorological Department (TMD, 2015) has divided the climate into three seasons: local summer (mid–February to mid–May), the rainy season (mid–May to mid–October), and the winter season (mid–October to mid–February). For this study, the dry season included the winter and summer seasons. The BMR has been rapidly developed, and its urbanization has accelerated environmental issues in the city, with the region experiencing air pollution for years. This study investigates air quality and the COVID-19 outbreak in Bangkok, Thailand, which represents a large, densely populated city with heavy traffic (Chirasophon and Pochanart, 2020).
Fig. 1.
Map of the Bangkok Metropolitan Region (BMR), the capital of the Kingdom of Thailand.
2.2. Data collection
The study population is considered to be the number of daily confirmed cases of COVID-19 in the Bangkok Metropolitan Administration (BMA), as officially reported by the Department of Disease Control of the Ministry of Public Health of Thailand from January 1 to March 31, 2020; these data are available at https://data.go.th/en/dataset/covid-19-daily (DDC, 2020). The daily weather data included mean temperature, relative humidity, wind speed, and air pollutant data (CO, SO2, NO, NO2, O3, PM10, and PM2.5); these datasets were collected from the Pollution Control Department of the Ministry of Natural Resources and Environment.
2.3. Calculation of absolute humidity (AH)
Absolute humidity (g/m3) is defined as the weight of water vapor per unit volume of air and is estimated using the Clausius-Clapeyron equation; it can be described as follows (Gupta et al., 2020; Kumar and Kumar, 2020; Pani et al., 2020; Qi et al., 2020):
| (1) |
where T represents the temperature in degree Celsius.
2.4. Statistical analysis
The correlations between daily confirmed COVID-19 cases and air pollutants, AQI, and meteorological factors were investigated using Spearman's and Kendall test equations (Pani et al., 2020). Hence, in the current study, the correlations between air pollutants, AQI, and meteorological parameters and the daily number of COVID-19 cases were observed using the Spearman's Rank correlation coefficient. Spearman's rank association test is a non-parametric metric, and the Spearman's rank correlation coefficient, i.e., the strength and orientation of the interactions between two graded variables, is measured by rho (). The estimation equation for Spearman's rho () is given as follows:
| (2) |
where is the difference between two parameter ranks, represents the number of alternatives, and the values and indicate perfect positive and negative associations, respectively.
Kendall rank correlation tests, another non-parametric test, were used to measure the ordinal association between two measured variables. The Kendall rank correlation coefficient, also called Kendall's tau , is used to evaluate the similarity of the ordering between two datasets and can be estimated as follows:
| (3) |
where and represent the number of concordant and discordant pairs, respectively. The value represents the number of pairs. The value of ranges from and has a similar interpretation as that of Spearman's correlation.
We used STATA (version 14.1) in this study to conduct the analysis, with numerical variables defined using descriptive statistics. Analyses of the mean differences between 1 Jan to 30 Mar 2020 and the same period in the previous year in the air pollutants, AQI, and meteorological parameters were estimated using a 95% confidence interval in two-sided t-tests paired. The daily COVID-19 cases, air pollutants, AQI, and meteorological parameters, used as datasets in the current study, were normally distributed by the Shapiro-Wilk test (see Table 1 ); thus, it was necessary to use non-parametric tests of the hypothesis, such as non-linear Spearman and Kendall correlation coefficient tests, as an empirical methodology to observe the connections between air pollutants and meteorological factors with daily confirmed COVID-19 cases in the Bangkok Metropolitan Region of Thailand. The statistical tests with results of p < 0.05 were considered statistically significant.
Table 1.
Summary of the statistical analyses of air pollution, meteorological factors, and newly confirmed COVID-19 cases between Jan 1st and Mar 30th in 2020 in the Bangkok Metropolitan Region, Thailand.
| Variables | Mean | S.D. | Median | Min | Max | Skewness | Kurtosis | Shapiro-Wilk |
|---|---|---|---|---|---|---|---|---|
| The daily confirmed of COVID-19 cases | 9.78 | 23.17 | 0.00 | 0.00 | 125.00 | 3.02 | 12.50 | 0.00001 |
| Ambient air pollutants | ||||||||
| CO (μg/m3) | 660.21 | 241.34 | 677.16 | 229.04 | 1419.05 | 0.12 | 2.91 | 0.11856a |
| NO (μg/m3) | 3.29 | 4.22 | 1.81 | 0.05 | 23.59 | 2.48 | 9.86 | 0.00001 |
| NO2 (μg/m3) | 29.07 | 19.73 | 24.05 | 6.05 | 103.33 | 0.99 | 3.84 | 0.00001 |
| SO2 (μg/m3) | 3.81 | 1.95 | 3.42 | 0.00 | 9.23 | 0.43 | 2.70 | 0.12875a |
| O3 (μg/m3) | 54.97 | 15.82 | 52.32 | 21.42 | 94.23 | 0.29 | 2.56 | 0.16407a |
| PM10 (μg/m3) | 51.70 | 24.09 | 46.00 | 20.75 | 130.33 | 0.64 | 2.68 | 0.00004 |
| PM2.5 (μg/m3) | 32.19 | 17.51 | 28.73 | 9.58 | 100.00 | 0.91 | 3.91 | 0.00003 |
| Air quality index (AQI) | 55.91 | 40.74 | 47.50 | 4.00 | 214.00 | 0.92 | 3.94 | 0.00002 |
| Meteorological parameters | ||||||||
| Temperature (°C) | 28.90 | 0.73 | 28.82 | 27.14 | 30.71 | 0.11 | 2.84 | 0.27026a |
| Relative humidity (%) | 70.44 | 11.41 | 75.31 | 39.33 | 90.28 | – 1.09 | 3.28 | 0.00001 |
| Absolute humidity (g/m3) | 19.50 | 3.30 | 21.01 | 10.86 | 23.19 | – 1.10 | 3.06 | 0.00001 |
| Wind speed (m/s) | 1.77 | 0.62 | 1.70 | 0.80 | 3.10 | 0.23 | 1.76 | 0.00036 |
| Rainfall (mm) | 0.00 | 0.02 | 0.00 | 0.00 | 0.20 | 9.33 | 88.01 | 0.00001 |
Normal distribution.
3. Results and discussion
3.1. Air quality changes during 90 days of the COVID-19 outbreak
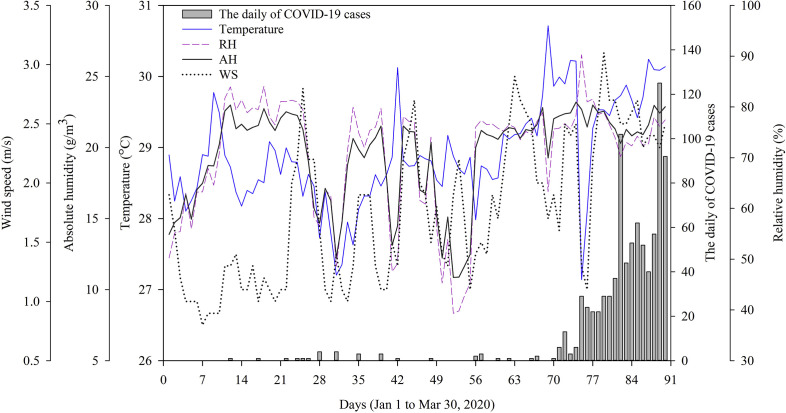
The study results showed the temporal patterns of daily COVID-19 cases, meteorological factors, air pollutants, and the AQI in the Bangkok Metropolitan Region during the study period. Fig. 2 shows the daily air pollutants (CO, NO, NO2, SO2, O3, PM10, and PM2.5), AQI, and daily COVID-19 cases between Jan 1 and Mar 30, 2020. The average daily meteorological data included the temperature, relative humidity, absolute humidity, wind speed, and daily COVID-19 cases between Jan 1 and Mar 30, 2020, as shown in Fig. 3 .
Fig. 2.
Panels (a), (b), (c), (d), (e), (f), (g), and (h) show the temporal patterns of the daily average of CO, NO, NO2, SO2, O3, PM10, PM2.5, and AQI, respectively, with the daily number of confirmed COVID-19 cases (Jan 1 to Mar 30, 2020).
Fig. 3.
Daily meteorological parameters and COVID-19 cases from January 1 to March 30, 2020, in the Bangkok Metropolitan Region.
3.1.1. Carbon monoxide (CO)
Table 2 presents the sources of carbon monoxide emissions (CO), a critical air pollution tracer. The results showed that the average CO concentration in the same period of the 2019 was 536.74 μg/m3. During the COVID-19 outbreak, the average CO of the same period in 2020 reached 660.21 μg/m3 and was observed to be significantly increased (p < 0.01) in Bangkok (23.00%). CO is one of the gaseous pollutant and characterized as colourless, non-irritating, odourless, and tasteless. It originates from natural sources such as forest wildfires and anthropogenic sources which account for the majority of CO emissions. Therefore, those who experience excessive CO exposure, as defined by exposure to concentrations higher than the limits designated by the WHO, can be at risk to the reaction of blood haemoglobin molecules to produce carboxyhaemoglobin (COHb), a significant outcome of the effects of CO exposure that reduces the supply of oxygen to the brain and other body organs (Fazlzadeh et al., 2015).
Table 2.
Descriptive statistics of the air pollutants, AQI, and meteorological factors in the BMR during the COVID-19 outbreak between Jan 1st and Mar 30th in 2020.
| Parameter | Bangkok Metropolitan Region (BMR) |
|||
|---|---|---|---|---|
| COVID-19 outbreak (2020) | The same period of the previous year (2019) | Mean difference (95% CI) | % Difference | |
| Ambient air parameters | ||||
| CO (μg/m3) | 660.21 | 536.74 | 123.47 (43.59, 203.34) | +23.00** |
| NO (μg/m3) | 3.29 | 6.03 | – 2.74 (– 5.09, −0.39) | – 45.44** |
| NO2 (μg/m3) | 29.07 | 20.91 | 8.15 (3.52, 12.79) | +39.02** |
| SO2 (μg/m3) | 3.81 | 2.68 | 1.13 (0.30, 1.97) | +42.16** |
| O3 (μg/m3) | 54.97 | 54.96 | 0.01 (– 4.63, 4.65) | +0.02 |
| PM10 (μg/m3) | 51.70 | 50.11 | 1.59 (– 4.90, 8.08) | +3.17 |
| PM2.5 (μg/m3) | 32.19 | 27.18 | 5.01(– 0.38, 9.65) | +18.43* |
| Air quality index (AQI) | 55.91 | 63.22 | – 7.31(– 16.67, 2.05) | – 11.56 |
| Meteorological | ||||
| Temperature (°C) | 28.90 | 28.58 | 0.32 (0.11, 0.54) | +1.12** |
| Relative humidity (%) | 70.44 | 72.23 | – 1.79 (– 4.81, 1.22) | – 2.48 |
| Absolute humidity (g/m3) | 19.50 | 20.00 | – 0.50 (– 1.33, 0.33) | – 2.50 |
| Wind speed (m/s) | 1.77 | 1.77 | 0.01 (– 0.14, 0.12) | 0.00 |
| Rainfall (mm) | 0.00 | 0.04 | – 0.04 (– 0.10, 0.03) | – 100.00 |
* Statistically significant at p < 0.05.
** Statistically significant at p < 0.01.
+ Air pollutants, AQI, and meteorological parameters increased as the percentage of the difference increased.
– Air pollutants, AQI, and meteorological parameters decreased percent differences.
3.1.2. Nitrogen monoxide (NO) and nitrogen dioxide (NO2)
According to Table 2, the results showed high nitrogen monoxide (NO) concentrations between Jan 1 and Mar 30, 2019. The average NO concentration reached 6.03 μg/m3 in 2019, and the average NO concentration during the COVID-19 outbreak from Jan 1 to Mar 30, 2020 was 3.29 μg/m3. A significant reduction (p < 0.01) in the average concentration of NO was observed in Bangkok; the concentration dropped noticeably (45.44%). The NO2 concentrations (μg/m3) in the same period in 2019 and during the COVID-19 outbreak from Jan 1 to Mar 30, 2020 were 20.91 and 29.07 μg/m3, respectively. The average concentration of NO2 significantly increased from 2019 to 2020 (p < 0.01) by 39.02%. The concentration of NO2 increased during the COVID-19 outbreak, which may also cause adverse health effects. Furthermore, a short-term increase in outdoor NO2 concentration can significantly increase upper respiratory tract infection risk. As an atmospheric pollutant, NO2 has many associated activities. It is a toxic gas that triggers major airway inflammation at short-term 1-h mean concentrations above 200 μg/m3 (WHO, 2018).
3.1.3. Sulphur dioxide (SO2)
The average SO2 concentration (μg/m3) in Bangkok from January 1 to March 30, 2019 was 2.68 μg/m3. In the same period in 2020 during the COVID-19 outbreak, the daily SO2 concentration increased slightly, and the average SO2 concentration reached 3.81 μg/m3, representing a significant (p < 0.01) increase during the COVID-19 outbreak (42.16%). The levels of SO2 were found to be below the WHO limit of 20 μg/m3 (24-h mean) (WHO, 2018) because the BMR represents an urban city with a high population density located near neighbouring industry perimeters, e.g., Samut Prakan Province, Phra Nakhon Si Ayutthaya Province, Pathum Thani Province, and Samut Sakhon Province. The emission sources of SO2 may include power generation, the manufacturing of chemicals, petroleum refineries, metal industries, transportation, and community services (Pervaiz et al., 2020).
3.1.4. Ozone (O3)
The average daily O3 (μg/m3) concentration in Bangkok from January 1 to March 30, 2019 was 54.96 μg/m3. In the same period in 2020 during the COVID-19 outbreak, the daily O3 concentration increased slightly; the average O3 concentration reached 54.97 μg/m3 and was observed to non-significantly increase by 0.02%. In general, increases in atmospheric O3 are associated with lowered nitrogen monoxide levels (Quan et al., 2014), which demonstrates that lower concentrations of NO will promote increases in O3 concentrations in the atmosphere (Collivignarelli et al., 2020). Previous studies have reported that an observed rise in the O3 concentration was related to its increased rate of production (Zheng et al., 2020). Moreover, the concentration of O3 rose dramatically in those studies, causing the ozone layer to have a healing effect (Srivastava, 2021). Additionally, a rise in O3 concentrations was correlated with a decrease in the concentration of NO2 in a study in Baghdad, Iraq (Hashim et al., 2021). When the emission of NO is sufficiently high, NO releases a large fraction of O3 into NO2 in the atmosphere (Monks et al., 2015).
3.1.5. PM10 and PM2.5
The average concentrations of PM10 (μg/m3) in BMR from Jan 1 to Mar 30, 2019 and in the same period in 2020 during the COVID-19 outbreak were 50.11 μg/m3 and 51.70 μg/m3, respectively. The change in the average PM10 concentration was found to be non-significant and slightly increased (3.17%). The mean concentration of PM10 from Jan 1 to Mar 30, 2020 indicated an exceedance of the recommended Air Quality Guideline of the WHO, i.e., the daily reference value of 50 μg/m3 for PM10 (WHO, 2018). In contrast, the daily concentration of PM2.5 (μg/m3) showed a significant increase (p < 0.05) of 18.43% between 2019 and 2020. The results showed that the average PM2.5 concentration from Jan 1 to Mar 30 in 2019 was 27.18 μg/m3. During the COVID-19 outbreak in the same period in 2020, the average PM2.5 concentration increased to 32.19 μg/m3. This shows that the PM2.5 concentration exceeded the WHO's 24-h standard, namely, a 24-h mean of 25 μg/m3 (WHO, 2018). The percent difference increases in the PM10 and PM2.5 concentrations observed in the BMR can be attributed to the different meteorological factors, particularly in terms of rainfall. The study period is considered a dry season, which thus does not receive sufficient rainfall to wash out various atmospheric pollutants, especially PM10 and PM2.5. The potential sources of PM10 and PM2.5 in Metropolitan Bangkok are dust soil, industrial emissions, construction, and soil re-suspension (Wimolwattanapun et al., 2011), while the major sources of PM2.5 emissions are biomass burning and transportation (Narita et al., 2019; Wimolwattanapun et al., 2011). It could be possible that during long-range transport, pollution sources, particularly biomass burning, indicate that the pollution source and preferred pathway could originate could be from north-eastern Thailand or father in the north-east direction (Wimolwattanapun et al., 2011). The resulting study found that the AQI decreased in the BMR from the period spanning Jan 1 to Mar 30, 2019 to the same period in 2020, during which the COVID-19 outbreak occurred; the results showed that the average AQIs were 63.22 and 55.91 during these periods, respectively. The average difference in the AQI was found to be non-significant and decreasing (11.56%).
Overall, the COVID-19 outbreak in Bangkok exhibited decreased NO and AQI values, whereas air pollutants (CO, NO2, SO2, O3, PM10, PM2.5) were found to increase in concentration; these pollutants were still sourced from anthropogenic activities such as transportation, construction, and industrial operations because during the study period, the Thai government had not yet officially announced a lockdown in Bangkok. In comparison, our study found that the average of Air Quality Index: AQI in a study period was moderately ranged (51–100) as 56 scores following Air Quality Index of Thailand. In addition, extreme health threats can occur not only from particulate matter (PM) emissions but also from O3, NO2, and SO2 exposure, particularly in urban areas. Moreover, nitrogen dioxide and sulphur dioxide may also play a role in asthma, bronchial effects, lung inflammation, and diminished lung function (WHO, 2018), especially during the COVID-19 pandemic, causing illness due to air pollution issues and possibly instigating an increased risk of infection.
3.1.6. Meteorological factors
Among the observed weather factors, only the average temperature (°C) was found to significantly increase in Bangkok; the average temperature increased by 1.12%, with p < 0.01. On the other hand, the RH, AH, WS, and rainfall underwent non-significant decreases of −2.48%, −2.50%, −0.00%, and −100%, respectively, as shown in Table 2.
3.2. Association between meteorological factors, air pollutants and AQI parameters and daily confirmed COVID-19 cases
The average daily of weather conditions, air pollutants, and the air quality index (AQI) with daily COVID-19 cases in the Bangkok Metropolitan Region (BMR) from January 1 to March 30, 2020 (90 days) were used to investigate the association between weather variables, air pollutants, AQI and daily confirmed COVID-19 cases. This investigation was carried out by using Spearman and Kendall rank correlation tests. The results of the empirical investigation of the air pollutants, AQI, and weather factors associated with daily confirmed COVID-19 cases in the BMR revealed that CO, NO2, SO2, O3, PM10, PM2.5, and AQI have a negative association with daily confirmed COVID-19 cases. On the other hand, the temperature, RH, AH, and WS showed a positive significant association with the daily number of COVID-19 cases in both Spearman and Kendall correlation tests, as shown in Table 3 . We then investigated the Spearman correlation between the daily number of COVID-19 cases and air pollutants in Bangkok as described in Sections 3.2.1, 3.2.2. However, in Spearman's rank correlation measure, the analysis and the exhibited correlation coefficient are higher than those obtained with Kendall's correlation.
Table 3.
Empirical results of the associations of air pollutants, AQI, and weather factors with daily confirmed COVID-19 cases from 1 January to 30 March 2020 in the BMR, Thailand.
| Type of correlation coefficients | Parameters | Daily of COVID-19 cases |
|---|---|---|
| Spearman's rank correlation coefficients | CO (μg/m3) | – 0.582* |
| NO (μg/m3) | – 0.062 | |
| NO2 (μg/m3) | – 0.525* | |
| SO2 (μg/m3) | – 0.599* | |
| O3 (μg/m3) | – 0.330* | |
| PM10 (μg/m3) | – 0.506* | |
| PM2.5 (μg/m3) | – 0.460* | |
| Air quality index (AQI) | – 0.458* | |
| Temperature (°C) | 0.431* | |
| Relative humidity (%) | 0.244* | |
| Absolute humidity (g/m3) | 0.453* | |
| Wind speed (m/s) | 0.487* | |
| Rainfall (mm) | – 0.088 | |
| Kendall's rank correlation coefficients | CO (μg/m3) | – 0.445* |
| NO (μg/m3) | – 0.049 | |
| NO2 (μg/m3) | – 0.415* | |
| SO2 (μg/m3) | – 0.473* | |
| O3 (μg/m3) | – 0.230* | |
| PM10 (μg/m3) | – 0.397* | |
| PM2.5 (μg/m3) | – 0.360* | |
| Air quality index (AQI) | – 0.359* | |
| Temperature (°C) | 0.318* | |
| Relative humidity (%) | 0.171* | |
| Absolute humidity (g/m3) | 0.335* | |
| Wind speed (m/s) | 0.381* | |
| Rainfall (mm) | – 0.080 |
* Statistically significant at p < 0.05.
3.2.1. The association between meteorological factors and daily COVID-19 cases
Our results found a positive association between temperature and the daily number of COVID-19 cases (, p < 0.05). According to, several studies have shown that temperature is associated with the number of COVID-19 cases. A study of the daily number of new cases of COVID-19 showed a positive association with the maximum temperature in Norway, with an average temperature of 4.76 °C (Menebo, 2020). Tantrakarnapa and Bhopdhornangkul (2020) found that the average daily temperature was associated with the daily cumulative number of COVID-19 cases in Thailand. Similarly, a study in Singapore found that average temperature was significantly associated with the numbers of new cases and total cases (Pani et al., 2020); another study found that only the average temperature was significantly positively associated with the COVID-19 pandemic (Tosepu et al., 2020). In contrast, the minimum temperature has also been found to be associated with the number of active COVID-19 cases. Additionally, the maximum and average temperatures were inversely correlated with COVID-19 cases in Mumbai, India (Kumar and Kumar, 2020). In addition, temperature was found to be constantly well-correlated with COVID-19 incidence in both Wuhan and XiaoGan but had an anti-correlation (Li et al., 2020). Additionally, the results of another study showed that temperature was negatively associated with daily new cases. It has been reported that a 1 °C increase in temperature was related to a 3.08% reduction in daily new cases (Wu et al., 2020b) and to a drop of −14.2% in the number of confirmed cases (Islam et al., 2020b); in Brazil, this temperature increase was linked to a drop of −4.90% in the number of daily COVID-19 cases (Prata et al., 2020). It has recently been reported that no evidence could be found to support the hypothesis that temperature can reduce the transmission of COVID-19 cases (To et al., 2021). Our results showed a positive association between the temperature with the daily confirmed number of COVID-19 cases (which was statistically significant), so that higher temperature resulted in a greater number of COVID-19 cases. On the other hand, the results of a study conducted in Canada, ambient temperature was not statistically significantly associated with COVID-19 incidence (To et al., 2021). In addition, a study of the association between weather factors and global transmission of SARS-CoV-2 reported a negative association between the average temperature per country and the number of cases of SARS-CoV-2 infection (Sobral et al., 2020). We believe our current result could not fully represent the potency of the influence of temperature on SARS-CoV-2 transmission due to the relatively limited study period and location. Thus, we cannot conclude the influence of temperature on the spread of COVID-19 based on the current data. Future studies are needed to accurately determine the effects of this parameter.
This study found that RH (%), AH (g/m3) and WS (m/s) had a positive association with the number of COVID-19 cases that was statistically significant showed positive associations with daily COVID-19 cases: RH ( p < 0.05), AH ( p < 0.05) and WS ( p < 0.05). Currently, few studies have reported a correlation between humidity and COVID-19 cases. In addition, a meta-analysis found that each rise in AH of 1 g/m3 was substantially correlated with a decrease in reported cases (Liu et al., 2020). In Turkey, it was discovered that the correlation between humidity and the number of cases was strong. In contrast, the association was negative, indicating a decline in the number of cases due to a rise in humidity (Şahin, 2020). In addition, Wu et al. (2020b), relative humidity was negatively associated with daily new COVID-19 cases. Another study produced experimental data showing that lower relative humidity favours influenza virus spread, further confirming this weather effect (Gardner et al., 2019). The stability of SARS coronavirus at low humidity may facilitate its spread in communities in subtropical climates (such as Hong Kong) during the spring (Chan et al., 2011). Therefore, Asian countries in tropical zones with high relative humidity values did not have major community outbreaks of SARS (Chan et al., 2011). Additionally, in dry indoor places of <40% RH, airborne transmission of SARS-COV-2 was found to be higher than that when the humidity was 90% (Ahlawat et al., 2020).
Whereas WS does not seem to be a significant role player in affecting the number of COVID-19 cases (Bashir et al., 2020a). So far, there have been few studies conducted on the topic. However, we conducted analyses of wind speed in this study. Interestingly, our study finds that wind speed showed positive significant association with the confirmed daily number of COVID-19 cases. According to the results of a study conducted in Iran, it was observed that the correlation is significant during outbreaks at low wind speeds (Ahmadi et al., 2020). Research in Turkey found that the average wind speed over 14 days is most associated with the number of cases of COVID-19 compared with other meteorological variables (Şahin, 2020). Additionally, WS was significantly associated with Middle East Respiratory Syndrome (MERS) cases occurring 5–6 days after the measured wind speed (Gardner et al., 2019). A study in the USA reported that WS did not significantly play a role in the spread of the virus (Bashir et al., 2020a), and other studies found that WS had a negative association with the number of COVID-19 cases (Rosario et al., 2020). However, wind speed is also a potential factor that suppresses SARS-CoV-2 transmission (Rosario et al., 2020). Previous study results showed that the most appropriate time span to study the effects of wind speed is 14 days. It indicates that it is imperative to consider wind speed to analyse its connection with the COVID-19 situation observed after 14 days (Şahin, 2020; Srivastava, 2021). Additionally, based on a study on the respiratory exhalation flow in an indoor environment, the size of the droplets that were carried 2 m away and evaporated before falling were between 60 and 100 μm. Expelled large droplets, on the other hand, were carried more than 6 m away by exhaled air at a velocity of 50 m/s (sneezing), more than 2 m away at a velocity of 10 m/s (coughing), and less than 1 m away at a velocity of 1 m (breathing) (Xie et al., 2007). Therefore, meteorological factors, especially WS, may potentially affect SARS-CoV-2 among symptomatic and asymptotic cases due to sneezing and coughing in population-dense areas such as airports, shopping malls, markets, public transportation, immigration borders, and places of entertainment such as pubs, clubs, bars, and other public places, which may lead to more infections.
Although few studies have been limited to the association between rainfall and daily confirmed COVID-19 cases, it has been reported that countries with higher precipitation measurements saw positive associations, with increased spread of disease. A rise of 56.01 cases a day was determined for each average inch of rainfall per day (Sobral et al., 2020). Thus, it may be possible that Thailand, due to the dry season occurring during the studied period, experienced a daily number of cases that was not massive compared with those of countries that had rainfall in the same period. These results suggest that this correlation needs to be studied in an equatorial climate, especially during rainy months with COVID-19 outbreaks. Therefore, datasets considered in further studies on the relationship between rainfall and the number of cases should cover all seasons in each country.
3.2.2. The relations of air pollution and the AQI with the daily confirmed number of COVID-19 cases
Currently, studies of the relationship between CO and SO2 are very limited. The present study found that CO (μg/m3) and SO2 (μg/m3) had significantly negative associations with daily COVID-19 cases ( p < 0.05 and p < 0.05, respectively). The CO and SO2 increases were associated with decreases in the daily number of COVID-19 cases. Recently, it has been reported that 1 μg/m3 CO is associated with a 15.11% increase in the daily count of confirmed COVID-19 cases (Zhu et al., 2020). The SO2 concentration of 10 μg/m3 was accompanied by a 7.79% decrease in the daily number of confirmed cases in China's 120 cities (Zhu et al., 2020). Therefore, in the current study, there is insufficient evidence for conclusive findings for CO and SO2 due to these factors being both negatively and positively associated with SARS-CoV-2 transmission.
The concentration of nitrogen dioxide (NO2) had a significantly negative association ( p < 0.05) with daily COVID-19 cases. Similarly, another study on the association between environmental pollution and the COVID-19 pandemic determined a significantly negative association between nitrogen dioxide and COVID-19 in California (Bashir et al., 2020b). In contrast, a study on the association between short-term exposure to air pollution and COVID-19 infection in China by Generalized Additive Modell (GAM) found that a 10 μg/m3 NO2 increase (lag0-14) was connected to a reported 6.94% increase in daily confirmed new cases (Zhu et al., 2020). Additionally, a death analysis percentage found that 83% of fatal COVID-19 cases were associated with NO2 > 100 μmol/m2 (Ogen, 2020). However, NO2 has not been found to be positively associated to COVID-19 cases (Zhu et al., 2020). Therefore, exposure to high ambient NO2 may be responsible for the extensive lung injuries seen in COVID-19 pneumonia, which are associated with worse outcomes (Frontera et al., 2020a), especially in urban areas. According to Frontera et al. (2020a), long-term lung exposure to NO2 may lead to viral injuries and local damage induced by oxidative stress, reduced macrophage function, and adaptive immune response.
The present study found that PM was a significant negative association with daily COVID-19 cases, both for PM10 ( p < 0.05) and PM2.5 ( p < 0.05). Similarly, a study in Dhaka, Bangladesh, found that PM10 and PM2.5 were negatively associated with the number of new COVID-19 cases (Pavel et al., 2020). In contrast, PM2.5 was positively associated with virus transmission in Italy (Lolli et al., 2020). A study in Milan, Italy, found that all confirmed daily new COVID-19 cases were positively associated with the average surface air PM2.5 and the daily maximum PM10 (Zoran et al., 2020). Additionally, viral replication in the respiratory system is enhanced by the negative effects of PM on the integrity of human respiratory barriers (Li et al., 2020; Xian et al., 2020). Wu et al. (2020a) investigated the effect of PM2.5 and suggested that increases of 1 μg/m3 in long-term exposure are associated with a 11% increase in the COVID-19 death rate and that increases of 10 μg/m3 in PM10 and PM2.5 have been associated with 2.24% and 1.76% increases in daily confirmed cases (Zhu et al., 2020). In particular, exposure to high concentrations of PM2.5 particles induces chronic respiratory conditions favourable to infective agents (Mehmood et al., 2020). This result supports the idea of Frontera et al. (2020a), in which the evidence reported that chronic exposure, especially to PM2.5, correlates with overexpression of the alveolar ACE-2 receptor, which can increase the viral load in patients exposed to PM (Domingo et al., 2020) and lead to more serious infection with COVID-19. However, it remains unclear whether ambient air pollutants, especially PM2.5, could assist in SARS-CoV-2 transmission (Li et al., 2020).
Our study showed that the AQI has a negatively significant association ( p < 0.05) with daily COVID-19 cases. Similarly, a study in Dhaka, Bangladesh, found that the AQI was negatively associated with the number of new COVID-19 cases and the total number of cases (Pavel et al., 2020). There was no correlation found between the number of new COVID-19 cases and the AQI in 12 cities in China during the pandemic (Huang et al., 2020). In contrast, a study of the incidence numbers in Wuhan and XiaoGan, China reported that the AQI was positively associated with daily COVID-19 incidence (Li et al., 2020). Similarly, a study in Milan, Italy, showed that the AQI was positively associated with daily COVID-19 cases (Zoran et al., 2020), indicating the significant role the AQI plays in SARS-CoV-2 spread.
However, the results of the present study found that the concentrations of NO were not significantly negatively associated with daily COVID-19 cases. However, the decreases may be related to NO released in the atmosphere converting to O3 (Hashim et al., 2021; Sicard et al., 2020). While our study of ozone (O3) has a negatively significant association (= −0.330, p < 0.05) with the daily COVID-19 case. In contrast, the studies in Milan, Italy has found that ground levels of ozone (O3) positively related with daily of COVID-19 cases (Zoran et al., 2020). The findings of this study demonstrate that level ozone possible acts as a SARS-CoV-2, being negatively associated with the daily of COVID-19 cases. In a recent study on the role of tropospheric O3 in flagging the COVID-19 pandemic transmission in metropolitan areas in Italy, the researchers observed that higher tropospheric ozone concentrations contribute to the slowing down of the COVID-19 pandemic-related infections (Lolli and Vivone, 2020). Thus, the higher concentrations of O3 in the troposphere, which has already been proven effective against viruses and microbial contaminants, is also considered to play a role in flagging SARS-CoV-2 transmission (Lolli and Vivone, 2020). This result indicates that O3 is a powerful oxidant and virucide and is sufficient to have a diminishing effect against bacteria, viruses, and protozoans under oxidizing agent reactions (Hudson et al., 2009).
3.2.3. Limitations of the study and suggestions
This study also has some limitations. The air pollutant data and meteorological parameters were taken from one monitor station, affecting the data and statistical analyses. Additionally, the study period was relatively short compared to other epidemiology studies (Li et al., 2020), and the seasonal variability of COVID-19 incidence has been suggested as a potentially significant variable of the pandemic (Meyer et al., 2020). Future studies should consider meta-analysis and a lag of incubation period between pollution and meteorological factors with COVID-19 cases to find relationships in each country in a given climatic zone, and individual, social, and economic factors should be involved in the study. In addition, more data on air pollutants, seasons, latitudes (such as subtropical, temperate, and tropical climates), and meteorological conditions should be considered from multiple monitoring stations to represent information for validation in the study region. Another important issue is that SARS-CoV-2 transmission is influenced by the number of foreign tourists (Tantrakarnapa et al., 2020), which affects the population density (Brown et al., 2008, Wu et al., 2020b), and the terrain and geography of each country are involved the landscape climate of different zones. Socioeconomic and industrial development may cause concentrations of air pollution, and the relationships between daily climate factors and the spread of COVID-19 may change. Notably, such data are associated with the SARS-CoV-2 outbreak, since COVID-19 is infectious and mainly influenced by population genetics, health infrastructure, the adherence of people to social distancing and social isolation measures, and the immunity and resistance of people (Pani et al., 2020); thus, different analyses considering age, gender, nationality, underlying conditions, occupation, vulnerable groups (e.g., persons with asthma, diabetes, chronic obstructive pulmonary disease (COPD), tuberculosis (TB), or cardiovascular diseases) should be conducted, and several factors are needed to conduct a comprehensive study. However, physical distancing, frequent handwashing, and personal protective equipment are still needed during this outbreak, and protection, especially face masks, should be worn when going to do activities outside the home, such as going to shopping malls, markets, mass transit systems, areas with high-density populations, and public areas. Thus, safety measures shall be suggested to residents for SARS-CoV-2 protection in the worst weather cases and in highly polluted areas. This study is limited to the presently available facts during the international worldwide pandemic and does not claim to report any potential seasonal pattern for SARS-CoV-2.
4. Conclusion
This study aims to assess air pollutants, the AQI, and weather variables and their parameter associations with the daily number of confirmed COVID-19 cases in the Bangkok Metropolitan Region (BMR) during the outbreak using descriptive statistical analyses and Spearman and Kendall correlation coefficient tests. The results showed that nitrogen monoxide (NO) and the AQI decreased during the COVID-19 outbreak. In contrast, it was found that CO, NO2, SO2, O3, PM2.5, and temperature significantly increased during the COVID-19 outbreak compared to the same period of the previous year. Our study found that the RH, AH, WS, and rainfall decreased during the same period. The results revealed that the temperature, RH, AH and WS have positively associated with daily confirmed COVID-19 cases, while the CO, NO2, SO2, O3, PM10, PM2.5, and AQI are negative associated with the daily number of confirmed COVID-19 cases in the BMR. These variables can potentially enhance SARS-CoV-2 sustained transmission. This study presents new insights into the association of daily weather variables, the AQI, and air pollutants with confirmed COVID-19 cases in the BMR. These data may support the Department of Public Health, local hospitals and government policymakers. The specifics of this study could help to establish a meteorological warning or alarm system as well as a prediction model to encourage a timely response to the SARS-CoV-2 activity upsurge (Chakraborty and Ghosh, 2020; Chong et al., 2020; Pani et al., 2020; Petropoulos and Makridakis, 2020).
CRediT author statement
Sarawut Sangkham: Conceptualization, Methodology, Software, Validation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing, Visualization. Sakesun Thongtip: Writing – review & editing. Patipat Vongruang: Software, Validation, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to thank the Air Quality and Noise Management Bureau, Pollution Control Department (PCD), Ministry of Natural Resources and Environment for the secondary data of air pollutants and meteorological parameter data; the dataset of the updated daily number of confirmed COVID-19 cases was obtained from the official webpage of the Department of Disease Control (DDC), Ministry of Public Health, Thailand. The authors would also like to acknowledge the editors and two anonymous reviewers, who contributed immensely to improving this publication's quality.
References
- Administrative Strategy Division Statical profile of Bangkok metropolitan administration. 2019. Available at: http://www.bangkok.go.th/pipd/page/sub/18654.
- Ahlawat A., Wiedensohler A., Mishra S.K. An overview on the role of relative humidity in airborne transmission of SARS-CoV-2 in indoor environments. Aerosol Air Qual. Res. 2020;20(9):1856–1861. http://doi:10.4209/aaqr.2020.06.0302 [Google Scholar]
- Ahmadi M., Sharifi A., Dorosti S., Jafarzadeh Ghoushchi S., Ghanbari N. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci. Total Environ. 2020;729:138705. doi: 10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., Ma B., Bilal Komal B., Bashir M.A., Tan D., Bashir M. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci. Total Environ. 2020;728:138835. doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., Ma B.J., Bilal Komal B., Bashir M.A., Farooq T.H., et al. Correlation between environmental pollution indicators and COVID-19 pandemic: a brief study in Californian context. Environ. Res. 2020;187:109652. doi: 10.1016/j.envres.2020.109652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedi J.S., Dhaka P., Vijay D., Aulakh R.S., Gill J.P.S. Assessment of air quality changes in the four metropolitan cities of India during COVID-19 pandemic lockdown. Aerosol Air Qual. Res. 2020;20(10):2062–2070. http://doi:10.4209/aaqr.2020.05.0209 [Google Scholar]
- Brown H.E., Childs J.E., Diuk-Wasser M.A., Fish D. Ecologic factors associated with west nile virus transmission, Northeastern United States. Emerg. Infect. Dis. 2008;14(10):1539. doi: 10.3201/eid1410.071396. http://doi:10.3201/eid1410.071396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Q.-C., Lu J., Xu Q.-F., Guo Q., Xu D.-Z., Sun Q.-W., et al. Influence of meteorological factors and air pollution on the outbreak of severe acute respiratory syndrome. Publ. Health. 2007;121(4):258–265. doi: 10.1016/j.puhe.2006.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakraborty T., Ghosh I. Real-time forecasts and risk assessment of novel coronavirus (COVID-19) cases: a data-driven analysis. Chaos, Solit. Fractals. 2020;135:109850. doi: 10.1016/j.chaos.2020.109850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan K.H., Peiris J.S.M., Lam S.Y., Poon L.L.M., Yuen K.Y., Seto W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv. Virol. 2011:734690. doi: 10.1155/2011/734690. http://doi:10.1155/2011/734690 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan A., Singh R.P. Decline in PM2.5 concentrations over major cities around the world associated with COVID-19. Environ. Res. 2020;187:109634. doi: 10.1016/j.envres.2020.109634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. 10223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chirasophon S., Pochanart P. The long-term characteristics of PM10 and PM2.5 in Bangkok, Thailand. Asian J. Atmos. 2020;14(1):73–83. doi: 10.5572/ajae.2020.14.1.073. [DOI] [Google Scholar]
- Chong K.C., Lee T.C., Bialasiewicz S., Chen J., Smith D.W., Choy W.S.C., et al. Association between meteorological variations and activities of influenza A and B across different climate zones: a multi-region modelling analysis across the globe. J. Infect. 2020;80(1):84–98. doi: 10.1016/j.jinf.2019.09.013. [DOI] [PubMed] [Google Scholar]
- Coker E.S., Cavalli L., Fabrizi E., Guastella G., Lippo E., Parisi M.L., et al. The effects of air pollution on COVID-19 related mortality in Northern Italy. Environ. Resour. Econ. 2020;76(4):611–634. doi: 10.1007/s10640-020-00486-1. http://doi:10.1007/s10640-020-00486-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collivignarelli M.C., Abbà A., Bertanza G., Pedrazzani R., Ricciardi P., Carnevale Miino M. Lockdown for CoViD-2019 in Milan: what are the effects on air quality? Sci. Total Environ. 2020;732:139280. doi: 10.1016/j.scitotenv.2020.139280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020;261:114465. doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui Y., Zhang Z.-F., Froines J., Zhao J., Wang H., Yu S.-Z., Detels R. Air pollution and case fatality of SARS in the People's Republic of China: an ecologic study. Environ. Health: Glob. Access Sci. Source. 2003;2(1) doi: 10.1186/1476-069X-2-15. http://doi:10.1186/1476-069X-2-15 15-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DDC 2020. https://data.go.th/dataset/covid-19-daily Accessed date:
- Domingo J.L., Marquès M., Rovira J. Influence of airborne transmission of SARS-CoV- 2 on COVID-19 pandemic. A review. Environ. Res. 2020;188:109861. doi: 10.1016/j.envres.2020.109861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutheil F., Baker J.S., Navel V. COVID-19 as a factor influencing air pollution? Environ. Pollut. 2020;263:114466. doi: 10.1016/j.envpol.2020.114466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazlzadeh M., Rostami R., Hazrati S., Rastgu A. Concentrations of carbon monoxide in indoor and outdoor air of Ghalyun cafes. Atmos. Pollut. Res. 2015;6(4):550–555. doi: 10.5094/APR.2015.061. [DOI] [Google Scholar]
- Frontera A., Cianfanelli L., Vlachos K., Landoni G., Cremona G. Severe air pollution links to higher mortality in COVID-19 patients: the “double-hit” hypothesis. J. Infect. 2020;81(2):255–259. doi: 10.1016/j.jinf.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frontera A., Martin C., Vlachos K., Sgubin G. Regional air pollution persistence links to COVID-19 infection zoning. J. Infect. 2020;81(2):318–356. doi: 10.1016/j.jinf.2020.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner E.G., Kelton D., Poljak Z., Van Kerkhove M., von Dobschuetz S., Greer A.L. A case-crossover analysis of the impact of weather on primary cases of Middle East respiratory syndrome. BMC Infect. Dis. 2019;19(1):113. doi: 10.1186/s12879-019-3729-5. http://doi:10.1186/s12879-019-3729- 5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S., Raghuwanshi G.S., Chanda A. Effect of weather on COVID-19 spread in the US: a prediction model for India in 2020. Sci. Total Environ. 2020;728:138860. doi: 10.1016/j.scitotenv.2020.138860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanaoka T., Masui T. Exploring effective short-lived climate pollutant mitigation scenarios by considering synergies and trade-offs of combinations of air pollutant measures and low carbon measures towards the level of the 2 °C target in Asia. Environ. Pollut. 2020;261:113650. doi: 10.1016/j.envpol.2019.113650. [DOI] [PubMed] [Google Scholar]
- Hashim B.M., Al-Naseri S.K., Al-Maliki A., Al-Ansari N. Impact of COVID-19 lockdown on NO2, O3, PM2.5 and PM10 concentrations and assessing air quality changes in Baghdad. Iraq. Sci. Total Environ. 2021;754:141978. doi: 10.1016/j.scitotenv.2020.141978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoang T., Tran T.T.A. Ambient air pollution, meteorology, and COVID-19 infection in Korea. J. Med. Virol. 2020;1–8 doi: 10.1002/jmv.26325. http://doi:10.1002/jmv.26325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang H., Liang X., Huang J., Yuan Z., Ouyang H., Wei Y., Bai X. Correlations between meteorological indicators, air quality and the COVID-19 pandemic in 12 cities across China. J. Environ. Health Sci. Eng. 2020 doi: 10.1007/s40201-020-00564-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson J.B., Sharma M., Vimalanathan S. Development of a practical method for using ozone gas as a virus decontaminating agent. Ozone Sci. Eng. 2009;31(3):216–223. http://doi:10.1080/01919510902747969 [Google Scholar]
- Islam A.R.M.T., Hasanuzzaman M., Azad M.A.K., Salam R., Toshi F.Z., Khan M.S.I., et al. Effect of meteorological factors on COVID-19 cases in Bangladesh. Environ. Dev. Sustain. 2020 doi: 10.1007/s10668-020-01016-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam A.R.M.T., Hasanuzzaman M., Shammi M., Salam R., Bodrud-Doza M., Rahman M.M., et al. Are meteorological factors enhancing COVID-19 transmission in Bangladesh? Novel findings from a compound Poisson generalized linear modeling approach. Environ. Sci. Pollut. Res. 2020 doi: 10.1007/s11356-020-11273-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ju M.J., Oh J., Choi Y.H. Changes in air pollution levels after COVID-19 outbreak in Korea. Sci. Total Environ. 2021;750:141521. doi: 10.1016/j.scitotenv.2020.141521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar G., Kumar R.R. A correlation study between meteorological parameters and COVID-19 pandemic in Mumbai, India. Diabetes Metab. Syndr. 2020;14(6):1735–1742. doi: 10.1016/j.dsx.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H., Xu X.L., Dai D.W., Huang Z.Y., Ma Z., Guan Y.J. Air pollution and temperature are associated with increased COVID-19 incidence: a time series study. Int. J. Infect. Dis. 2020;97:278–282. doi: 10.1016/j.ijid.2020.05.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Zhou J., Yao J., Zhang X., Li L., Xu X., et al. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci. Total Environ. 2020;726:138513. doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lolli S., Chen Y.C., Wang S.H., Vivone G. Impact of meteorological conditions and air pollution on COVID-19 pandemic transmission in Italy. Sci. Rep. 2020;10(1):16213. doi: 10.1038/s41598-020-73197-8. http://doi:10.1038/s41598-020-73197-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lolli S., Vivone G. The role of tropospheric ozone in flagging COVID-19 pandemic transmission. Bull. Atmos. Sci. Technol. 2020 doi: 10.1007/s42865-020-00026-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martelletti L., Martelletti P. Air pollution and the novel Covid-19 disease: a putative disease risk factor. SN Compr. Clin. Med. 2020;2(4):383–387. doi: 10.1007/s42399-020-00274-4. http://doi:10.1007/s42399-020- 00274-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehmood K., Saifullah Iqbal M., Abrar M.M. Can exposure to PM2.5 particles increase the incidence of coronavirus disease 2019 (COVID-19)? Sci. Total Environ. 2020;741:140441. doi: 10.1016/j.scitotenv.2020.140441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menebo M.M. Temperature and precipitation associate with Covid-19 new daily cases: a correlation study between weather and Covid-19 pandemic in Oslo, Norway. Sci. Total Environ. 2020;737:139659. doi: 10.1016/j.scitotenv.2020.139659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer A., Sadler R., Faverjon C., Cameron A.R., Bannister-Tyrrell M. Evidence that higher temperatures are associated with a marginally lower incidence of COVID-19 cases. Front. Public Health. 2020;8(367) doi: 10.3389/fpubh.2020.00367. http://doi:10.3389/fpubh.2020.00367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monks P.S., Archibald A.T., Colette A., Cooper O., Coyle M., Derwent R., et al. Tropospheric ozone and its precursors from the urban to the global scale from air quality to short-lived climate forcer. Atmos. Chem. Phys. 2015;15(15):8889–8973. http://doi:10.5194/acp-15-8889-2015 [Google Scholar]
- Narita D., Oanh N.T.K., Sato K., Huo M., Permadi D.A., Chi N.N.H., et al. Pollution characteristics and policy actions on fine particulate matter in a growing Asian economy: the case of Bangkok Metropolitan Region. Atmosphere. 2019;10(5):227. [Google Scholar]
- Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. Sci. Total Environ. 2020;726:138605. doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pani S.K., Lin N.H., RavindraBabu S. Association of COVID-19 pandemic with meteorological parameters over Singapore. Sci. Total Environ. 2020;740:140112. doi: 10.1016/j.scitotenv.2020.140112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavel M.R.S., Salam A., Yesmin M., Ahsan N., Zaman S.U., Jeba F. medRxiv; 2020. Impact and Correlation of Air Quality and Climate Variables with COVID-19 Morbidity and Mortality in Dhaka, Bangladesh.http://doi:10.1101/2020.09.12.20193086 [Google Scholar]
- Pervaiz S., Javid K., Zafar Khan F., Zahid Y., Akram M.A.N. Preliminary assessment of air during COVID-19 lockdown: an unintended benefit to environment. Environ. Nat. Resour. J. 2020;18(4):363–375. [Google Scholar]
- Petropoulos F., Makridakis S. Forecasting the novel coronavirus COVID-19. PloS One. 2020;15(3) doi: 10.1371/journal.pone.0231236. http://doi:10.1371/journal.pone.0231236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata D.N., Rodrigues W., Bermejo P.H. Temperature significantly changes COVID- 19 transmission in (sub)tropical cities of Brazil. Sci. Total Environ. 2020;729:138862. doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi L., Gao Y., Yang J., Ding X.B., Xiong Y., Su K., et al. The burden of influenza and pneumonia mortality attributable to absolute humidity among elderly people in Chongqing, China, 2012–2018. Sci. Total Environ. 2020;716:136682. doi: 10.1016/j.scitotenv.2020.136682. [DOI] [PubMed] [Google Scholar]
- Quan J., Tie X., Zhang Q., Liu Q., Li X., Gao Y., Zhao D. Characteristics of heavy aerosol pollution during the 2012–2013 winter in Beijing, China. Atmos. Environ. 2014;88:83–89. doi: 10.1016/j.atmosenv.2014.01.058. [DOI] [Google Scholar]
- Reboul C., Thireau J., Meyer G., André L., Obert P., Cazorla O., Richard S. Carbon monoxide exposure in the urban environment: an insidious foe for the heart? Respir. Physiol. Neurobiol. 2012;184(2):204–212. doi: 10.1016/j.resp.2012.06.010. [DOI] [PubMed] [Google Scholar]
- Rosario D.K.A., Mutz Y.S., Bernardes P.C., Conte-Junior C.A. Relationship between COVID-19 and weather: case study in a tropical country. Int. J. Hyg Environ. Health. 2020;229:113587. doi: 10.1016/j.ijheh.2020.113587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Şahin M. Impact of weather on COVID-19 pandemic in Turkey. Sci. Total Environ. 2020;728:138810. doi: 10.1016/j.scitotenv.2020.138810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setti L., Passarini F., De Gennaro G., Barbieri P., Licen S., Perrone M.G. Potential role of particulate matter in the spreading of COVID-19 in Northern Italy: first observational study based on initial epidemic diffusion. BMJ Open. 2020;10(9) doi: 10.1136/bmjopen-2020-039338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sicard P., De Marco A., Agathokleous E., Feng Z., Xu X., Paoletti E., et al. Amplified ozone pollution in cities during the COVID-19 lockdown. Sci. Total Environ. 2020;735:139542. doi: 10.1016/j.scitotenv.2020.139542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobral M.F.F., Duarte G.B., da Penha Sobral A.I.G., Marinho M.L.M., de Souza Melo A. Association between climate variables and global transmission of SARS-CoV- 2. Sci. Total Environ. 2020;729:138997. doi: 10.1016/j.scitotenv.2020.138997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastava A. COVID-19 and air pollution and meteorology-an intricate relationship: a review. Chemosphere. 2021;263:128297. doi: 10.1016/j.chemosphere.2020.128297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan J., Mu L., Huang J., Yu S., Chen B., Yin J. An initial investigation of the association between the SARS outbreak and weather: with the view of the environmental temperature and its variation. J. Epidemiol. Community Health. 2005;59(3):186. doi: 10.1136/jech.2004.020180. http://doi:10.1136/jech.2004.020180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tantrakarnapa K., Bhopdhornangkul B. Challenging the spread of COVID-19 in Thailand. One Health. 2020;100173 doi: 10.1016/j.onehlt.2020.100173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tantrakarnapa K., Bhopdhornangkul B., Nakhaapakorn K. Influencing factors of COVID- 19 spreading: a case study of Thailand. J. Public Health. 2020 doi: 10.1007/s10389-020-01329-5. http://doi:10.1007/s10389- 020-01329-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- TMD The climate of Thailand. 2015. Available at: https://www.tmd.go.th/en/archive/thailand_climate.pdf.
- To T., Zhang K., Maguire B., Terebessy E., Fong I., Parikh S., Zhu J. Correlation of ambient temperature and COVID-19 incidence in Canada. Sci. Total Environ. 2021;750:141484. doi: 10.1016/j.scitotenv.2020.141484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tosepu R., Gunawan J., Effendy D.S., Ahmad L.O.A.I., Lestari H., Bahar H., Asfian P. Correlation between weather and covid-19 pandemic in Jakarta, Indonesia. Sci. Total Environ. 2020;725:138436. doi: 10.1016/j.scitotenv.2020.138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travaglio M., Yu Y., Popovic R., Selley L., Leal N.S., Martins L.M. Links between air pollution and COVID-19 in England. Environ. Pollut. 2021;268:115859. doi: 10.1016/j.envpol.2020.115859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO WHO guidelines for indoor air quality: selected pollutants. 2010. Available at: https://www.euro.who.int/__data/assets/pdf_file/0009/128169/e94535.pdf. [PubMed]
- WHO Ambient (outdoor) air pollution. 2018. https://www.who.int/news-room/fact- sheets/detail/ambient-(outdoor)-air-quality-and-health Available at:
- Wimolwattanapun W., Hopke P.K., Pongkiatkul P. Source apportionment and potential source locations of PM2.5 and PM2.5–10 at residential sites in metropolitan Bangkok. Atmos. Pollut. Res. 2011;2(2):172–181. doi: 10.5094/APR.2011.022. [DOI] [Google Scholar]
- Wu X., Nethery R.C., Sabath M.B., Braun D., Dominici F. Air pollution and COVID- 19 mortality in the United States: strengths and limitations of an ecological regression analysis. Sci. Adv. 2020;6(45):eabd4049. doi: 10.1126/sciadv.abd4049. http://doi:10.1126/sciadv.abd4049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., Jing W., Liu J., Ma Q., Yuan J., Wang Y., et al. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci. Total Environ. 2020;729:139051. doi: 10.1016/j.scitotenv.2020.139051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xian M., Ma S., Wang K., Lou H., Wang Y., Zhang L., et al. Particulate matter 2.5 causes deficiency in barrier integrity in human nasal epithelial cells. Allergy Asthma Immunol Res. 2020;12(1):56–71. doi: 10.4168/aair.2020.12.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724:138201. doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X., Li Y., Chwang A.T., Ho P.L., Seto W.H. How far droplets can move in indoor environments--revisiting the Wells evaporation-falling curve. Indoor Air. 2007;17(3):211–225. doi: 10.1111/j.1600-0668.2007.00469.x. http://doi:10.1111/j.1600-0668.2007.00469.x [DOI] [PubMed] [Google Scholar]
- Zheng H., Kong S., Chen N., Yan Y., Liu D., Zhu B., et al. Significant changes in the chemical compositions and sources of PM2.5 in Wuhan since the city lockdown as COVID-19. Sci. Total Environ. 2020;739:140000. doi: 10.1016/j.scitotenv.2020.140000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727:138704. doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoran M.A., Savastru R.S., Savastru D.M., Tautan M.N. Assessing the relationship between surface levels of PM2.5 and PM10 particulate matter impact on COVID-19 in Milan. Italy. Sci. Total Environ. 2020;738:139825. doi: 10.1016/j.scitotenv.2020.139825. [DOI] [PMC free article] [PubMed] [Google Scholar]