Abstract
Background
The spectrum of neurological involvement in COVID-19 is not thoroughly understood. To the best of our knowledge, no systematic review with meta-analysis and a sub-group comparison between severe and non-severe cases has been published. The aim of this study is to assess the frequency of neurological manifestations and complications, identify the neurodiagnostic findings, and compare these aspects between severe and non-severe COVID-19 cases.
Methods
A systematic search of PubMed, Scopus, EBSCO, Web of Science, and Google Scholar databases was conducted for studies published between the 1st of January 2020 and 22nd of April 2020. In addition, we scanned the bibliography of included studies to identify other potentially eligible studies. The criteria for eligibility included studies published in English language (or translated to English), those involving patients with COVID-19 of all age groups, and reporting neurological findings. Data were extracted from eligible studies. Meta-analyses were conducted using comprehensive meta-analysis software. Random-effects model was used to calculate the pooled percentages and means with their 95% confidence intervals (CIs). Sensitivity analysis was performed to assess the effect of individual studies on the summary estimate. A subgroup analysis was conducted according to severity. The main outcomes of the study were to identify the frequency and nature of neurological manifestations and complications, and the neuro-diagnostic findings in COVID-19 patients.
Results
44 articles were included with a pooled sample size of 13,480 patients. The mean age was 50.3 years and 53% were males. The most common neurological manifestations were: Myalgia (22.2, 95% CI, 17.2 to 28.1%), taste impairment (19.6, 95% CI, 3.8 to 60.1%), smell impairment (18.3, 95% CI, 15.4 to 76.2%), headache (12.1, 95% CI, 9.1 to 15.8%), dizziness (11.3, 95% CI, 8.5 to 15.0%), and encephalopathy (9.4, 95% CI, 2.8 to 26.6%). Nearly 2.5% (95% CI, 1 to 6.1%) of patients had acute cerebrovascular diseases (CVD). Myalgia, elevated CK and LDH, and acute CVD were significantly more common in severe cases. Moreover, 20 case reports were assessed qualitatively, and their data presented separately.
Conclusions
Neurological involvement is common in COVID-19 patients. Early recognition and vigilance of such involvement might impact their overall outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12883-021-02161-4.
Keywords: COVID-19, Coronavirus, Neurology, CNS, Clinical features, Meta-analysis, Systematic review
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread rapidly over the past year causing the Coronavirus Disease 2019 (COVID-19) pandemic. According to Johns Hopkins Coronavirus Resource Center, as of March 3, 2020, 192 nations and more than 114 million people across the globe have been affected while more than 2.5 million people died [1].
Although SARS-CoV-2 primarily affects the respiratory system causing pneumonia, multiorgan dysfunction and failure are likely to occur in severe cases [2]. There is mounting evidence that coronaviruses can invade the nervous tissue [3, 4] resulting in various neurological manifestations (NM) and neurological complications (NC) [5].
The literature about the NM of COVID-19 has been evolving with exponential increase in the number of publications. Multiple studies and case reports described the NM, which vary from being non-specific ones like headache, dizziness, and myalgias to more significant one like ataxia, seizures, anosmia, and ageusia [6–9]. Other studies reported NC of COVID-19 like acute ischemic stroke, cerebral venous sinus thrombosis, cerebral hemorrhage, and rhabdomyolysis [6, 10]. Abnormal findings in neurodiagnostic studies (ND) including neuroimaging (CT and MRI), cerebrospinal fluid (CSF) analysis, and neurophysiological studies (Electroencephalogram (EEG), Nerve Conduction Study (NCS), and Electromyography (EMG)) have also been described [6, 11, 12].
We conducted a systematic review and meta-analysis of studies addressing the neurological aspects of COVID-19 including NM, NC, and ND findings. In addition, we compared these aspects between severe and non-severe cases. Since the literature is still evolving and not many well designed studies have been published, we also performed a qualitative assessment of the case reports describing some unique NC of COVID-19.
Methods
We developed a review protocol (registration number: PROSPERO CRD42020181298) prior to commencing the study. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) were used to ensure the reporting quality of this review [13].
Literature search strategy
A broad search strategy was conducted through the following databases: PubMed, Scopus, EBSCO, Web of Science, and Google Scholar using terms related to COVID-19 and terms related to neurology; more details about the terms used in the search process are available in the appendix (Additional file 1). Primary search process and secondary search process before the final analysis included studies published between January 1st 2020 and April 22nd 2020. Moreover, additional studies referenced in selected papers were identified and included.
Inclusion and exclusion criteria
- Inclusion criteria:
- Randomized controlled trials, non-randomized controlled trials, case-control studies, cohort studies, cross sectional studies, case series, and case reports.
- Studies involving patients diagnosed with COVID-19, regardless of age.
- Studies including clinical features of COVID-19 including NM, NC, or ND studies.
- Articles published in English or are otherwise translated to English.
- Exclusion criteria:
- Articles not addressing the neurological aspects of the infection.
- Articles on cases with known neurological conditions before COVID-19 with no major neurological change during the infection (new symptoms or worsening of previous condition).
- Studies addressing any of the other five human coronaviruses.
- Studies published before 2020.
Study selection
Four reviewers screened the titles and abstracts of retrieved records for eligibility using Rayyan software [14]. Individual studies were critically appraised by applying a standardized appraisal form appropriate for the study type. Inter-rater disagreements were resolved following a discussion between the reviewers.
Data extraction
Two reviewers extracted the following information: date of publication, country, study design, age, gender, previous comorbidities, general and neurological clinical features, laboratory findings, imaging findings, neurophysiological study findings, severity and outcome of the disease. We tried to obtain unpublished missing data by contacting authors.
Risk of Bias assessment
Two reviewers assessed the risk of bias using the NIH Study Quality Assessment Tools for case series, cross sectional and cohort studies [15, 16]. Conflicts were resolved by consulting a third reviewer.
Data synthesis and analysis
We used a random effects model to calculate the pooled percentages for categorical variables and pooled means for continuous variables with their 95% confidence intervals (CIs) as the effect sizes. For data with median and inter-quartile range (IQR) or median and range, mean and standard deviation (SD) were calculated according to the equations by Luo et.al, Wan et.al, and Hozo et.al [17–19]. I2 statistic, T2 (tau-squared) test, and Cochrane Q were used to assess heterogeneity among studies. Data analysis was done using comprehensive meta-analysis software.
We assessed the existence of publication bias by the Egger’s test [20]. The existence of publication bias was determined by the degree of the funnel plot symmetry and we considered P < .05 as an evidence of the existence of publication bias.
Subgroup and sensitivity analysis
A subgroup analysis was done to compare clinical and diagnostic neurological features in patients with severe disease compared to patients with non-severe disease; this categorization was determined if the study classified them into these groups Moreover, we performed a sensitivity analysis, in which the pooled estimates for each variable was recalculated, omitting one study at a time, to ensure that none of the included studies affected the results and to examine whether the overall effect size is statistically robust.
Outcome measures
The main outcomes of this study were the frequency of NM, NC and ND findings. The main NM included but were not limited to: Headache, myalgia, weakness, dizziness, taste impairment (ageusia), smell impairment (anosmia), altered level of consciousness, behavioral changes, facial weakness, ataxia, abnormal movements (like tremor), hemiparesis, hemiplegia, vision impairment, cranial nerve dysfunction, numbness, paresthesia, and neuropathic pain. The NC included: Ischemic and hemorrhagic strokes, venous sinus thrombosis, meningitis, encephalitis, seizures, and rhabdomyolysis. The ND findings included: Laboratory findings (serum creatine kinase (CK), serum lactate dehydrogenase (LDH), neutrophil count, lymphocyte count, and monocyte count), CSF analysis, neuroimaging (MRI and CT), EEG, NCS, or EMG. Moreover, we examined the treatment associated neurological side effects or complications.
Ratings of the quality of the evidence
According to the modified rating scale of Oxford Centre for Evidence-based Medicine for ratings of individual studies [21], the evidence for most of the studies in our meta-analysis was rated as level four (case series without intervention, and cross sectional) and only two were rated as level three (retrospective cohort studies). Moreover, we included case reports in our qualitative assessment (evidence level four; case reports).
Results
Study selection results
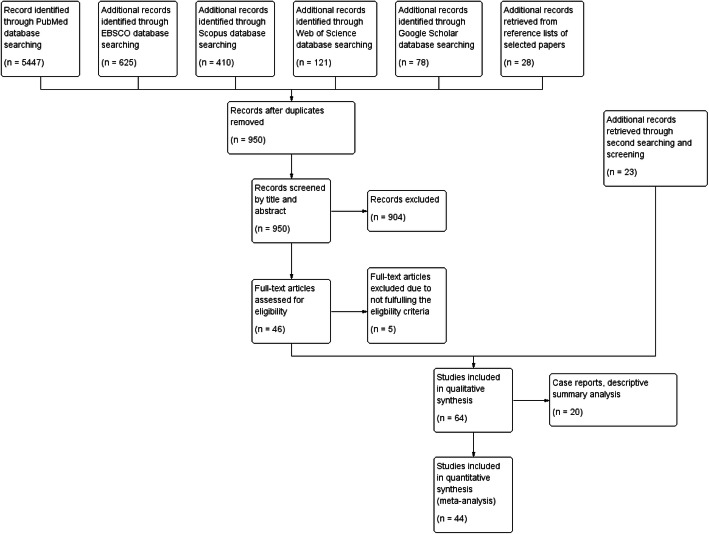
The primary search yielded 6709 articles, with 41 articles remaining after removal of duplicates and screening titles, abstracts, and full texts. As a result of the rapid growth of the COVID-19 literature, a second search was conducted yielding another 23 articles. Forty-four articles were included in the final meta-analysis and 20 case reports were included in the qualitative descriptive review (Fig. 1). Seventeen articles were available on the search databases but they were not yet published in their final form.
Fig. 1.
Flow diagram of study selection. Primary and secondary search processes yielded a total of 64 eligible articles. Forty-four articles were included in the final meta-analysis and 20 case reports were included in the qualitative descriptive review
Demographics and characteristics
Forty-four studies were included in the meta-analysis, 14 of which were available as pre-prints at the time of the search (Table 1). A total of 13,480 patients were included in our analysis with a mean age of 50.3 (95% CI, 47.7 to 52.9) years, and 53% (95% CI, 50.2 to 55.7%) being males. Thirty-six (81.8%) studies were from China, two (4.5%) were from Italy, and the rest being one from each of Australia, France, Japan, Netherlands, Belgium and the UK. The study sample size ranged from 13 to 6606 patients per study.
Table 1.
Characteristics of the Included Studies in the Meta-Analysis of the Neurological Features of COVID-19
| # | Author | Date (DD/MM/Y) | Journal | Study type | N | Country | Reference | Study quality |
|---|---|---|---|---|---|---|---|---|
| 1 | Chen and Wu, 2020 | 27-3-2020 | The Journal of Clinical Investigation | Case series | 21 | China | [22] | Fair |
| 2 | Liu and Zhang, 2020 | Pre-print: 13-2-2020 | The Lancet Infectious Diseases | Case series | 24 | China | [23] | Fair |
| 3 | Wang and Gao, 2020 | Pre-proof: 5-3-2020 | European Respiratory Journal | Case series | 18 | China | [24] | Fair |
| 4 | Giacomelli, 2020 | 26-3-2020 | Clinical Infectious Diseases | Cross-Sectional Study | 59 | Italy | [25] | Fair |
| 5 | Mao, 2020 | 10-4-2020 | JAMA Neurology | Case series | 214 | China | [6] | Fair |
| 6 | Xu and Yu, 2020 | 28-2-2020 | European Journal of Nuclear Medicine and Molecular Imaging | Case series | 90 | China | [26] | Fair |
| 7 | Jin, 2020 | 24-3-2020 | BMJ | Case series | 651 | China | [27] | Fair |
| 8 | Chen and Zhou, 2020 | 15-2-2020 | The Lancet | Case series | 99 | China | [28] | Fair |
| 9 | Li and Li, 2020 | Pre-print:12-2-2020 | MDrxiv | Case series | 17 | China | [29] | Fair |
| 10 | Qian, 2020 | 17-3-2020 | QJM | Case series | 91 | China | [30] | Fair |
| 11 | Xu and Wu, 2020 | 10-2-2020 | BMJ | Case series | 62 | China | [31] | Fair |
| 12 | Huang and Wang, 2020 | 24-1-2020 | Lancet | Case series | 41 | China | [32] | Fair |
| 13 | Wan, 2020 | 21-3-2020 | Journal of Medical Virology | Case Series | 135 | China | [33] | Fair |
| 14 | Yang and Yu, 2020 | 24-2-2020 | The Lancet Respiratory Medicine | Cohort - Retrospective | 52 | China | [34] | Fair |
| 15 | Liu and Fang, 2020 | 7-2-2020 | Chinese Medical Journal | Case series | 137 | China | [35] | Fair |
| 16 | Guan, 2020 | 28-2-2020 | The new england journal of medicine | Case series | 1099 | China | [2] | Fair |
| 17 | Wang and Hu, 2020 | 7-2-2020 | JAMA | Case series | 138 | China | [36] | Fair |
| 18 | Qin and Qiu, 2020 | Pre-print: 20-2-2020 | TheLancet | Case series | 89 | China | [37] | Good |
| 19 | Yang and Cao, 2020 | 26-2-2020 | The Journal of Infection | Case series | 149 | China | [38] | Fair |
| 20 | Qin and Zhou, 2020 | 12-3-2020 | Clinical Infectious Diseases | Case series | 452 | China | [39] | Fair |
| 21 | Liu and Liu, 2020 | 12-2-2020 | Preprint: medRxiv | Case series | 61 | China | [40] | Fair |
| 22 | Easom, 2020 | 29-3-2020 | Influenza Other Respir Viruses | Case series | 68 | UK | [41] | Fair |
| 23 | Deng, 2020 | 20-3-2020 | Chinese Medical Journal | Case series | 225 | China | [42] | Good |
| 24 | Huang and Tu, 2020 | 27-2-2020 | Travel Medicine and Infectious Disease | Case series | 34 | China | [43] | Fair |
| 25 | Mo, 2020 | 16-3-2020 | Clinical Infectious Diseases | Case series | 155 | China | [44] | Fair |
| 26 | Li and Wang, 2020 | Pre-print:17-3-2020 | The Lancet | Case series | 221 | China | [10] | Good |
| 27 | Zheng and Tang, 2020 | 24-3-2020 | European Review for Medical and Pharmacological Sciences | Case series | 161 | China | [45] | Fair |
| 28 | Guo, 2020 | Pre-print: 14-4-2020 | The Lancet | Case series | 118 | China | [46] | Good |
| 29 | Yan, 2020 | Pre-print: 6-4-2020 | The Lancet | Case series | 218 | China | [47] | Good |
| 30 | Chang, 2020 | 17-3-2020 | JAMA | Case series | 13 | China | [48] | Fair |
| 31 | Wang and Pan, 2020 | Pre-proof: 11-4-2020 | International Journal of Infectious Diseases | Case series | 125 | China | [49] | Fair |
| 32 | Zhou and Sun, 2020 | Pre-print: 16-3-2020 | BMC Infectious Diseases | Case series | 201 | China | [50] | Fair |
| 33 | Zheng and Xu, 2020 | 10-4-2020 | Journal of Clinical Virology | Case series | 99 | China | [51] | Fair |
| 34 | Helms, 2020 | 15-4-2020 | NEJM | Case series | 58 | France | [52] | Fair |
| 35 | Lechien, 2020 | 6-4-2020 | European Archives of Oto-Rhino-Laryngology | Cross-Sectional Study | 417 | Belgium, France, Spain, Italy | [53] | Fair |
| 36 | Chen and Chen, 2020 | Pre-print: 1-4-2020 | The Lancet | Case series | 85 | China | [54] | Fair |
| 37 | Jiang, 2020 | Pre-print: 14-4-2020 | medRxiv | Case series | 55 | China | [55] | Good |
| 38 | Zhang, 2020 | Pre-proof: 9-4-2020 | Journal of Clinical Virology | Case series | 221 | China | [56] | Fair |
| 39 | Tabata, 2020 | Pre-print: 18-3-2020 | The Lancet | Case series | 104 | Japan | [57] | Fair |
| 40 | Lei, 2020 | Pre-proof: 9-4-2020 | Travel Medicine and Infectious Disease | Case series | 20 | Guangzhou, China | [58] | Fair |
| 41 | Zhou and Yu, 2020 | 28-3-2020 | The Lancet | Cohort - Retrospective | 191 | China | [59] | Fair |
| 42 | Spinato, 2020 | 22-4-2020 | JAMA | Cross-sectional Study | 202 | Italy | [60] | Fair |
| 43 | Klok, 2020 | 10-4-2020 | Thrombosis Research | Case series | 184 | Netherlands | [61] | Fair |
| 44 | CNIRST, 2020 | 19-4-2020 | NA | Case series | 6606 | Australia | [62] | Fair |
DD/MM/Y Day, Month, Year. NA not applicable
The remaining 20 studies were included for the qualitative assessment of case reports (Table 2), three of them were available as pre-prints at the time of the search. These case reports included 57 patients with a mean age of 59.5 (± 20.2) years and 38 (67%) being males.
Table 2.
Characteristics of Included Case Reports
| # | Author | Date (DD/MM/Y) | Journal | Study type | N | Country | Reference |
|---|---|---|---|---|---|---|---|
| 1 | Moriguchi, 2020 | Pre-Print: 25-3-2020 | International Journal of Infectious Diseases | Case Report | 1 | Japan | [11] |
| 2 | Zhao and huang, 2020 | Pre-Print: 9-4-2020 | medRxiv preprint | Case Report | 1 | China | [63] |
| 3 | Lorenzo Villalba, 2020 | 3-4-2020 | European Journal of Case Reports in Internal Medicine | Case Report | 2 | France and Spain | [64] |
| 4 | Ollarves-Carrero, 2020 | 13-4-2020 | Travel Medicine and Infectious Disease | Case Report | 1 | Spain | [65] |
| 5 | Sharifi-Razavi, 2020 | 27-3-2020 | New Microbes and New Infections | Case Report | 1 | Iran | [66] |
| 6 | Marchese-Ragona, 2020 | Pre-print: 7-4-2020 | MedRxiv preprint | Case Report | 6 | Italy | [9] |
| 7 | Novi, 2020 | 9-4-2020 | Multiple sclerosis and related disorders | Case Report | 1 | Italy | [67] |
| 8 | Poyiadji, 2020 | 31-3-2020 | Radiology | Case Report | 1 | USA | [12] |
| 9 | Karimi, 2020 | 24-3-2020 | Iran Red Crescent Med J | Case Report | 1 | Iran | [68] |
| 10 | Zhao and shen, 2020 | 1-4-2020 | Lancet Neurology | Case Report | 1 | China | [69] |
| 11 | Gane, 2020 | 29-3-2020 | Rhinology | Case Report | 1 | United Kingdom | [70] |
| 12 | Hjelmesæth, 2020 | 5-4-2020 | Tidsskr Nor Legeforen | Case Report | 3 | Norway | [71] |
| 13 | Toscano, 2020 | 17-4-2020 | NEJM | Case Report | 5 | Italy | [72] |
| 14 | Filatov, 2020 | 21-3-2020 | Cureus | Case Report | 1 | USA | [8] |
| 15 | Suwanwongse, 2020 | 6-4-2020 | Cureus | Case Report | 1 | USA | [73] |
| 16 | Wang and Hajizadeh, 2020 | 08-04-2020 | Journal of Thrombosis and Haemostasis | Case Report | 3 | USA | [74] |
| 17 | Wang and Chen, 2020 | 09-02-2020 | Bioscience Trends | Case Report | 4 | China | [75] |
| 18 | Ren, 2020 | 05-05-2020 | Chinese Medical Journal | Case Report | 5 | China | [76] |
| 19 | Rothe, 2020 | 05-03-2020 | NEJM | Case Report | 1 | Germany | [77] |
| 20 | Wang and Tang, 2020 | 27-01-2020 | Journal of Medical Virology | Case Report | 17 | China | [78] |
DD/MM/Y Day, Month, Year
Risk of Bias assessment results
Of the 44 studies included in the meta-analysis, 39 were considered as case series and they were assessed for risk of bias using the NIH Quality Assessment Tool for Case Series Studies [16]. The study quality was rated as good, fair, or poor if the number of “Yes” responses were ≥ 6, 3 to 5, or ≤ 2, respectively. Of the 39-case series, 33 received a “fair” rating and 6 studies received a “good” rating.
Two studies were considered cohort studies and three were considered cross-sectional studies. They were assessed using the NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [15]. The study quality was rated as good, fair, or poor if the number of “Yes” responses were ≥ 9, 4 to 8, or ≤ 3, respectively. All of the five included cohort and cross-sectional studies were given a “fair” rating.
Moreover, some questions of the previous quality assessment tools were not applicable to all studies. A more detailed illustration of the risk of bias assessment for each study is attached as a table in the supplementary appendix (Additional files 2 and 3).
Clinical features and laboratory findings
The frequency of NM in COVID-19 patients was as follows: Myalgia (22.2, 95% CI, 17.2 to 28.1%), taste impairment (19.6, 95% CI, 3.8 to 60.1%), smell impairment (18.3, 95% CI, 15.4 to 76.2%), headache (12.1, 95% CI, 9.1 to 15.8%), dizziness (11.3, 95% CI, 8.5 to 15.0%), encephalopathy or cognitive dysfunction (9.4, 95% CI, 2.8 to 26.6%), and ataxia or abnormal gait (2.1, 95% CI, 0.2 to 23.7%). Nearly, 2.5% (95% CI, 1 to 6.1%) of COVID-19 patients had acute cerebrovascular diseases (CVD); which included ischemic stroke (IS), intracerebral hemorrhage (ICH), and cerebral venous sinus thrombosis (CVT) (Table 3, additional file 4).
Table 3.
Meta-analysis of the clinical characteristics of the study subjects
| Pooled effect size (95% CI) |
Heterogeneity | Tau squared | # of studies | |||
|---|---|---|---|---|---|---|
| Q value | P value | I Squared | ||||
| Mean age (Years) | 50.3 (47.7–52.9) | 2872.2 | < .001 | 98.50 | 72.58 | 44 |
| Male | 53.0 (50.2–55.7) % | 180.71 | < .001 | 77.31 | 8.97 | 42 |
| Clinical features | ||||||
| Headache | 12.1 (9.1–15.8) % | 989.99 | < .001 | 96.26 | 0.824 | 38 |
| Myalgia | 22.2 (17.2–28.1) % | 621.55 | < .001 | 94.85 | 0.740 | 33 |
| Taste impairment | 19.6 (3.8–60.1) % | 431.04 | < .001 | 99.30 | 3.405 | 4 |
| Smell impairment | 18.3 (1.54–76.2) % | 853.88 | < .001 | 99.64 | 7.254 | 4 |
| Dizziness | 11.3 (8.5–15.0) % | 27.85 | .001 | 67.68 | 0.156 | 10 |
| Features of encephalopathy or cognitive dysfunction | 9.4 (2.8–26.6) % | 133.92 | < .001 | 95.51 | 2.70 | 7 |
| Ataxia or abnormal gait | 2.1 (0.2–23.7) % | 6.59 | .010 | 84.83 | 3.18 | 2 |
| Fever | 80.6 (74.9–85.3) % | 1604.55 | < .001 | 97.44 | 1.05 | 42 |
| Cough | 64.1 (59.9–68.0) % | 575.30 | < .001 | 93.04 | 0.26 | 41 |
| Neurological complications a | 3.0 (0.9–9.6) % | 50.01 | < .001 | 92.00 | 1.66 | 5 |
| Acute CVD | 2.5 (1.0–6.1) % | 15.3 | 0.004 | 74.41 | 0.72 | 5 |
| Laboratory findings | ||||||
| Serum CK (U/L) | 85.5 (73.8–97.3) | 369.93 | < .001 | 96.21 | 434.78 | 15 |
| Serum LDH (U/L) | 263.4 (234.6–292.3) | 648.50 | < .001 | 97.84 | 3026.56 | 15 |
| Lymphocyte (a10^9/L) | 1.08 (1.02–1.14) | 549.37 | < .001 | 95.08 | 0.024 | 28 |
| Neutrophils (a10^9/L) | 3.44 (3.21–3.68) | 214.45 | < .001 | 90.67 | 0.244 | 21 |
| Monocytes (a10^9/L) | 0.39 (0.37–0.42) | 42.66 | < .001 | 78.90 | 0.001 | 10 |
| Severe COVID-19 | 31.1 (21.9–42.2) % | 739.23 | < .001 | 97.02 | 1.16 | 23 |
| ICU admission | 20.6 (14.1–29.0) % | 231.12 | < .001 | 91.34 | 0.81 | 21 |
| Comorbidities | ||||||
| Any previous comorbidity | 37.4 (33.1–41.9) % | 274.90 | < .001 | 89.08 | 0.231 | 31 |
| Diabetes Mellitus | 10.3 (8.3–12.8) % | 265.15 | < .001 | 88.68 | 0.360 | 31 |
| Hypertension | 20.4 (17.0–24.2) % | 196.73 | < .001 | 87.292 | 0.253 | 26 |
| Heart diseases | 9.7 (7.2–12.9) % | 426.59 | < .001 | 93.201 | 0.706 | 30 |
| Neurological diseases | 5.7 (3.3–9.7) % | 175.60 | < .001 | 90.319 | 1.213 | 18 |
| Malignancy | 2.7 (2.0–3.6) % | 61.429 | < .001 | 59.303 | 0.319 | 26 |
| Pulmonary diseases | 3.4 (2.2–5.0) % | 260.24 | < .001 | 89.240 | 0.973 | 29 |
| Chronic kidney disease | 2.3 (1.3–3.9) % | 75.189 | < .001 | 81.380 | 0.858 | 15 |
| Chronic liver disease | 3.5 (2.6–4.7) % | 32.726 | .005 | 54.165 | 0.187 | 16 |
| Smoking | 9.2 (6.4–13.0) % | 146.643 | < .001 | 89.771 | 0.501 | 16 |
aNeurological complications include: Cerebrovascular diseases (ischemic stroke, cerebral hemorrhage, and venous sinus thrombosis), rhabdomyolysis, and seizures
P < .05 indicates the presence of heterogeneity
About a third of COVID-19 patients were severely affected (31.1, 95% CI, 21.9 to 42.2%) and 20.6% (95% CI, 14.1 to 29.0%) were admitted to intensive care units. About 37.4% (95% CI, 33.1 to 41.9%) had a pre-existing comorbidity, and 5.7% (95% CI, 3.3 to 9.7%) had a preexisting neurological disease. Detailed characteristics of the pre-existing comorbidities are presented in (Table 3, additional file 5).
Regarding laboratory abnormalities (Table 3, additional file 6), the mean values were as follows: CK: 85.57 U/L (Normal range; 40–200 U/L), LDH: 263.49 U/L (Normal range; 120–250 U/L). The mean lymphocyte, neutro0phil, and monocyte count were 1.08, 3.44, and 0.39 (*10^9/L), respectively.
No published data regarding COVID-19 treatment related neurological side effects and complications were found.
Publication Bias
According to Egger et.al [20], publication bias assessment is only reliable for 10 or more pooled studies. Therefore, we presented the results of publication bias for variables that were discussed in 10 or more studies (Additional file 7). Publication bias was observed in the following variables: fever (p < .001), headache (p < .001), serum LDH (p = .0015), Diabetes Mellitus (DM) (p = .0089), pre-existing neurological diseases (p = .0089), malignancy (p = .031), and chronic kidney disease (CKD) (p = .044).
Sensitivity analysis
A sensitivity analysis, in which the meta-analysis was serially repeated after the exclusion of each study, demonstrated that no individual study affected the overall prevalence for each variable except for the following: Taste impairment prevalence was reduced from 19.6 to 10.9% when the study by Spinato et.al was excluded [60]; smell impairment prevalence was reduced from 18.3 to 7.5% when the study by Lechien et.al was excluded [53], and increased to 35.2% when the study by Mao et.al was removed [6]. After excluding the study conducted by Guan et.al, the reported frequency of NC increased from 3 to 5.8% [2]. More details can be found in additional file 8.
Subgroup analysis
When comparing severe to non-severe COVID-19 patients, the severe group included older patients [mean age 60 vs 44.7 years-old, p < .001] and more males [60.3% vs 48.6%, p = .001] than the non-severe group. Myalgia [34.9% vs 4.1%, p = .045], acute CVD [34.9% vs 4.1%, p = .045], higher CK value [324.9 vs 121.2 U/L, p = .01], and higher LDH value (247.6 vs 83.0 U/L, p = .012) were more likely in the severe group. While encephalopathy and cognitive dysfunction were more frequent in the severe group [16.9% vs 1.9%, p = .054], this was not statistically significant. There was no significant difference for the rest of the variables evaluated (Table 4). Heterogeneity was significant for all the variables and was not resolved by subgroup analysis.
Table 4.
Subgroup analysis between severe and non-severe groups
| Study | Subgroup | Pooled effect size (95% CI) |
Heterogeneity | Tau squared | Mixed effects analysis | |||
|---|---|---|---|---|---|---|---|---|
| Q value | Df (Q) | P value † | I Squared | P value | ||||
| Age (Years) | Total | 56.9 (55.1–58.8) | 1443.18 | 34 | < .001 | 97.64 | 107.603 | < .001 |
| Non severe | 44.4 (40.1–48.7) | 585.98 | 16 | < .001 | 97.26 | 77.40 | ||
| Severe | 60.0 (57.9–62.1) | 78.77 | 17 | < .001 | 78.418 | 13.35 | ||
| Male | Total | 53.1 (49.5–56.6) % | 108.58 | 31 | < .001 | 71.45 | 0.104 | .001 |
| Non severe | 48.6 (44.2–53.1) % | 54.23 | 15 | < .001 | 72.34 | 0.082 | ||
| Severe | 60.3 (54.7–65.7) % | 36.90 | 15 | .001 | 59.36 | 0.104 | ||
| Clinical features | ||||||||
| Headache | Total | 14.8 (12.4–17.5) % | 187.25 | 30 | < .001 | 83.97 | 0.474 | .308 |
| Non severe | 12.2 (7.9–18.2) % | 170.26 | 15 | < .001 | 91.19 | 0.730 | ||
| Severe | 15.4 (12.7–18.5) % | 16.27 | 14 | .296 | 14.003 | 0.025 | ||
| Myalgia | Total | 24.4 (18.2–32.0) % | 167.89 | 18 | < .001 | 89.279 | 0.468 | .045 |
| Non severe | 19.4 (13.1–27.9) % | 102.34 | 9 | < .001 | 91.206 | 0.463 | ||
| Severe | 34.9 (22.3–49.9) % | 58.061 | 8 | < .001 | 86.221 | 0.651 | ||
| Dizziness | Total | 11.9 (8.7–16.0) % | 16.073 | 7 | 0.024 | 56.449 | 0.106 | .506 |
| Non severe | 10.9 (7.4–16.1) % | 10.27 | 4 | 0.036 | 61.076 | 0.145 | ||
| Severe | 13.5 (8.2–21.5) % | 5.619 | 2 | 0.06 | 64.409 | 0.152 | ||
| Features of Encephalopathy / cognitive dysfunction | Total | 3.2 (1.2–8.4) % | 116.97 | 6 | < .001 | 94.87 | 4.753 | .054 |
| Non severe | 1.9 (0.6–5.8) % | 2.266 | 2 | .322 | 11.743 | 0.167 | ||
| Severe | 16.9 (2.4–62.3) % | 83.34 | 3 | < .001 | 96.4 | 4.342 | ||
| Fever | Total | 79.8 (71.6–86.2) % | 560.33 | 31 | < .001 | 94.46 | 1.159 | .213 |
| Non severe | 76.9 (66.3–85.0) % | 313.83 | 15 | < .001 | 95.22 | 0.912 | ||
| Severe | 86.5 (72.6–93.9) % | 238.40 | 15 | < .001 | 93.708 | 2.63 | ||
| Cough | Total | 59.2 (52.8–65.3) % | 285.48 | 30 | < .001 | 89.49 | 0.402 | .094 |
| Non severe | 55.8 (48.2–63.2) % | 141.37 | 15 | < .001 | 89.39 | 0.302 | ||
| Severe | 67.4 (55.9–77.2) % | 135.46 | 14 | < .001 | 89.66 | 0.734 | ||
| Neurological Complications | Total | 3.8 (1.3–10.0) % | 82.532 | 7 | < .001 | 91.518 | 2.274 | .212 |
| Non severe | 1.3 (0.2–8.8) % | 17.178 | 2 | < .001 | 88.35 | 2.663 | ||
| Severe | 5.6 (1.7–17.1) % | 37.55 | 4 | < .001 | 89.34 | 1.607 | ||
| Acute CVDa | Total | 2.6 (1.1–5.8) % | 33.02 | 7 | < .001 | 78.91 | 1.42 | .045 |
| Non severe | 0.6 (0.1–3.1) % | 4.578 | 2 | 0.101 | 56.319 | 1.299 | ||
| Severe | 4.1 (1.6–10.0) % | 15.38 | 4 | 0.004 | 74.00 | 0.797 | ||
| Laboratory findings | ||||||||
| Serum CK | Total | 91.5 (79.3–103.7) | 90.95 | 15 | < .001 | 83.505 | 377.38 | .01 |
| Non severe | 83.0 (69.1–96.8) | 53.346 | 7 | < .001 | 86.87 | 276.03 | ||
| Severe | 121.2 (95.4–147.1) | 18.80 | 7 | < .001 | 62.76 | 633.03 | ||
| Serum LDH | Total | 270.6 (243.1–298.1) | 494.931 | 15 | < .001 | 96.969 | 3099.14 | .012 |
| Non severe | 247.6 (214.8–280.4) | 272.42 | 7 | < .001 | 97.43 | 1997.9 | ||
| Severe | 324.9 (274.4–375.4) | 66.42 | 7 | < .001 | 89.462 | 4195.36 | ||
| Preexisting neurological diseases | Total | 4.5 (2.8–7.0) % | 101.58 | 20 | < .001 | 80.31 | 1.055 | .072 |
| Non severe | 2.6 (1.2–5.5) % | 36.692 | 9 | < .001 | 78.19 | 0.970 | ||
| Severe | 6.2 (3.5–10.9) % | 42.959 | 11 | < .001 | 74.39 | 0.772 | ||
aCVD (Cerebrovascular diseases): Ischemic stroke, cerebral hemorrhage, and venous sinus thrombosis
† P < .05 indicates the presence of heterogeneity
Qualitative assessment
Twenty case reports (57 patients) were identified and their details are summarized in Table 5. Six (10.5%) patients were diagnosed with GBS 5–10 days after the onset of respiratory symptoms [69, 72]. Their neurological symptoms included numbness, weakness, dysphagia, and facial weakness; four patients (7.0%) had facial weakness including one (1.8%) with facial diplegia. All of these patients had abnormal NCS/EMG findings consistent with an axonal variant in three patients and a demyelinating variant in two.
Table 5.
Patients characteristics and findings of the included case reports
| Variable | N (%) or Mean ± SD | Variable | N (%) or Mean ± SD | ||
|---|---|---|---|---|---|
| Number | Cases | 57 | Clinical features | Fever | 41 (71.9%) |
| Articles | 20 | Cough | 34 (59.6%) | ||
| Countries of the cases reported | China | 28 (49.1%) | Fatigue | 14 (25.6%) | |
| Italy | 12 (21.0%) | Myalgia | 12 (21.0%) | ||
| USA | 6 (10.5%) | Headache | 5 (8.8%) | ||
| Norway | 3 (5.3%) | Dizziness | 2 (3.5%) | ||
| Iran | 2 (3.5%) | Taste impairment | 11 (19.3%) | ||
| Spain | 2 (3.5%) | Smell impairment | 13 (22.8%) | ||
| France | 1 (1.8%) | Encephalopathy features | 5 (8.8%) | ||
| Germany | 1 (1.8%) | Weakness/ paralysis | 7 (12.3%) | ||
| Japan | 1 (1.8%) | Altered reflexes | 3 (5.3%) | ||
| UK | 1 (1.8%) | Altered sensationc | 5 (8.8%) | ||
| Age (Years) | 59.5 ± 20.2 | Ataxia or abnormal gait | 1 (1.8%) | ||
| Gender | Male | 38 (66.6%) | Facial weakness | 4 (7%) | |
| Female | 19 (33.3%) | Neck pain/ rigidity | 2 (3.5%) | ||
| Comorbidities | Any | 24 (42.1%) | Number of neurological manifestations | None | 20 (35.0%) |
| DM | 7 (12.3%) | 1–2 | 27 (47.3%) | ||
| Hypertension | 13 (22.8%) | > 3 | 10 (17.5%) | ||
| Cardiovascular diseases | 9 (15.7%) | Neurological complications | Any | 12 (21.0%) | |
| Neurological diseases | 8 (14.0%) | GBS | 6 (10.5%) | ||
| Chronic liver diseases | 3 (5.2%) | Encephalitis | 2 (3.5%) | ||
| Pulmonary diseases | 5 (8.8%) | Seizure | 2 (3.5%) | ||
| Malignancy or cancer | 1 (1.8%) | Cerebral Hemorrhage | 1 (1.8%) | ||
| Chronic kidney disease | 4 (7%) | Myelitis | 1 (1.8%) | ||
| ICU | Yes | 16 out of 28 (57.1%) | Rhabdomyolysis | 1 (1.8%) | |
| No | 12 out of 28 (42.8%) | Onset (Days)a | 7.25 ± 2.43 | ||
| Onset (Days) a | 7.7 ± 2.9 | Imaging | CT/MRI changes | 6 (10.5%) | |
| Ventilator | Yes | 11 out of 31 (35.4%) | CSF | Increased protein | 5 (8.8%) |
| No | 20 out of 31 (64.5%) | SARS-CoV-2 RNA in CSF | 1 (1.8%) | ||
| Onset (Days) a | 7 ± 2.49 | EEG | Temporal slowing and sharp waves | 1 (1.8%) | |
| Severity of COVID-19 | Asymptomatic | 3 (5.3%) | Nerve conduction study/EMG | Demyelinating or Axonal patterns | 6 (10.5%) |
| Non-severe | 19 (33.3%) | Neurology-related management | 12 (21%) | ||
| Severe | 30 (52.6%) | Neurological outcome | Morbidity/ disability | 4 out of 16(25%) | |
| COVID-19 disease outcome | Death | 20 out of 45(44.4%) | Recovery/ Improvement | 10 out of 16(62.5%) | |
| Discharged/ Recovery | 18 out of 45(40%) | Still hospitalized | 2 out of 16(12.5%) | ||
| Still hospitalized | 7 out of 45(15.5%) | Onset (Days)a,b | 15.5 (2.5) |
Some data are missing or not reported. All patients in the aforementioned case reports were confirmed to have COVID-19
GBS Guillain–Barré Syndrome
a Onset in relation to the onset of COVID-19 symptoms
bReported as median and IQR
c Altered sensation included paresthesia, numbness, loss of pain, temperature, or tactile sensations of the lower limbs, upper limbs, or trunk
Besides the above-mentioned EMG/NCS abnormalities, ND findings included neuro-imaging, CSF, and EEG findings. Neuro-imaging utilized were head CT, brain MRI and spinal MRI. Six patients had significant neuroimaging findings, including two patients with cerebral hemorrhage [12, 66], one patient with encephalitis/ventriculitis [11], two GBS patients with enhancement of the caudal nerve roots [72], and one GBS patient with bilateral enhancement of facial nerves [72]. Besides, six (10.5%) patients had CSF changes; mainly increased protein in five [8, 69, 72], and only one with SARS-CoV-2 RNA detected in CSF using RT-PCR assay [11]. Lastly, one patient had EEG changes consisting of bilateral and focal slowing in the left temporal region with left temporal sharp waves [8].
Twelve patients received neurology-related management including IVIG in eight patients, and four who used one or more of the following therapies: ceftriaxone, vancomycin, acyclovir, ganciclovir, steroids, levetiracetam, phenytoin, plasma exchange, or vitamin B12.
Of note, some NM and ND findings were reported by a few studies, out of the 44 studies, and were insufficient to be included in the meta-analysis. These included manifestations like visual impairment [6], nerve pain [6], and diffuse corticospinal tract signs with enhanced tendon reflexes, ankle clonus, and bilateral extensor plantar reflexes [52]. CSF findings included positive oligoclonal bands with the same pattern in serum, elevated CSF IgG and CSF protein levels, and low albumin level [52]. Head CT findings included ischemic stroke, cerebral hemorrhage, and cerebral venous sinus thrombosis [6, 10]. Brain MRI findings included leptomeningeal enhancement, bilateral frontotemporal hypoperfusion, and acute and subacute ischemic strokes [52]. EEG findings included nonspecific changes and slowing consistent with encephalopathy [52].
Discussion
A total of 13,480 COVID-19 patients were included in the meta-analysis. NM were frequent with around 20% of patients reporting myalgia, taste impairment, or smell impairment; and around 10% complaining of headache, dizziness, or encephalopathy. Ataxia or abnormal gait was the least reported NM. Five studies reported NC (CVD, seizures, and rhabdomyolysis). CVDs (IS, ICH, CVT) occurred in 2.5% of patients. For those who were tested, high levels of CK and LDH as markers of muscle injury were found, especially in the severe subgroup. About one third of patients included in this study had severe disease course and one fifth of them were admitted to the ICU.
There is a mounting evidence that Angiotensin Converting Enzyme 2 (ACE 2) receptors are expressed throughout the central nervous system, primarily on the surface of neurons [79], and SARS-CoV-2 might use these receptors to gain entry into the nervous system [3, 4, 80]. The result of direct neuronal invasion could explain manifestations such as headache, dizziness, ataxia and encephalopathy, while neuronal death and inflammation could explain complications like meningitis/encephalitis [11, 81], as well as seizures or even refractory status epilepticus [82–84]. Interestingly, direct invasion of the respiratory centers in the brainstem was proposed as a contributing factor to the respiratory failure in COVID-19 patients [3, 85].
Viral entry into the CNS is debatable. This could happen via a hematogenous route in which the virus passes through the blood brain barrier (BBB) by transcytosis or infects endothelial or epithelial cells to cross the BBB [4, 11, 86]. Alternatively, the virus could infect and get transported by leukocytes into the CNS, as was shown for SARS-CoV [87].
Moreover, ACE 2 receptor is heavily expressed on the epithelial cells of the mucosa of the oral cavity [88] and a trans-neural transmission of SARS-CoV through the olfactory bulb was seen in a mice model [89]. Sungnak et al. surveyed expression of SARS-CoV-2 viral entry-associated genes in multiple tissues from healthy human donors and found these genes highly expressed in nasal epithelial cells [90]. These findings could explain the occurrence of anosmia and ageusia in COVID-19 patients, which at times can be the only presenting features or the very early symptoms of COVID 19 [53, 91].
Myalgia and occasionally clinically significant muscle injury in severe disease, as evidenced by elevated CK and LDH, can be either a direct response of viral invasion of the skeletal muscles, which are also known to express ACE2 receptor [80], or an indirect response to the systemic inflammatory reaction manifested by a cytokine storm, subsequently causing muscle injury [92–94].
Multiple mechanisms could explain the increased risk of ischemic strokes and venous sinus thrombosis [95, 96]; these include hypercoagulability [6, 97], high systemic inflammatory response or “cytokine storm” [98], vascular endothelial injury [59], and cardiac injury resulting in cerebral embolism [99]. It is worth-mentioning there were anecdotal reports of decline in stroke admission rates in certain communities, possibly due to the anxiety surrounding this pandemic which discourages patients, especially those with mild stroke symptoms, from seeking emergency medical services [100–104]. There is a need for clear guidelines for the neuroradiology departments on how to safely and effectively perform urgent neuro-diagnostic images and emergent neuro-interventional procedures [100, 105, 106]. Implementing such guidelines are critical to streamline the management of COVID-19 patients presenting with neurological complications such as stroke, and to maintain a high-quality standard workflow.
According to our analysis, myalgia and evidence of muscle injury “elevated CK and LDH” as well as CVD were more likely to occur with severe disease. This might be related to the degree of the inflammatory response and the reported cytokine release syndrome [107] as well as the prothrombotic state [108] that occur with severe cases of COVID-19 and contribute to the multiorgan failure [22, 109].
Congruent with what Mao et al. [6] reported in the first retrospective observational case series describing the NM of COVID-19 in 214 hospitalized patients in Wuhan-China, our meta-analysis shows that myalgia or skeletal muscle injury (with elevated LDH and CK) and acute CVDs are predominantly associated with severe COVID-19.
A recent systematic review of 8 studies [110], not including a meta-analysis, suggested that some patients, particularly those with severe illness, have CNS involvement and NM, which is supported by the results of our study. Montalvan et al. [111] concluded that symptoms of hyposmia, headaches, weakness, and altered consciousness, and complications like encephalitis, demyelination, neuropathy, and stroke were associated with coronaviruses infections. Those results are congruent with our findings, although we looked at SARS-CoV-2 exclusively, while they evaluated other human coronaviruses in addition. The authors also suggested that trans-synaptic extension through the cribriform plate and olfactory bulb represents the main mechanism of neuro-invasion, and that invasion of the medulla could contribute to the respiratory failure in critically ill COVID-19 patients. A group from the National Hospital, Queen Square described five major categories of NM and NC associated with COVID-19, including: (i) encephalopathies with delirium/psychosis in the absence of characteristic MRI or CSF abnormalities; (ii) inflammatory CNS syndromes including encephalitis, acute disseminated encephalomyelitis which many times was hemorrhagic, and myelitis; (iii) ischemic strokes (half of them with pulmonary embolism); (iv) peripheral neuropathies including Guillain-Barré Syndrome (GBS) and brachial plexopathy; and (v) miscellaneous central nervous system disorders [112]. Ahmad et al. [113] in a narrative literature review reported that neurological features could occur before the classical features of COVID-19 like fever and cough, and accordingly a high index of suspicion is needed for a timely diagnosis and isolation of cases.
In the 20 case reports we evaluated, the most common NM included fatigue, myalgia, and smell and taste impairment, which is quite similar to our meta-analysis results. NC included GBS (6 cases), encephalitis, seizures, ICH, IS, myelitis and rhabdomyolysis. GBS associated with COVID-19 indicates that SARS CoV-2 can potentially induce an immune response that results in a delayed neurological complication [114]. This association between coronaviruses and GBS was reported before [114, 115]. In these case reports, the neurological outcome was variable, but one fourth of patients were left with residual deficits after 2 weeks of COVID-19 disease onset, indicating potential severity of the neurological injury.
Quality of the evidence
We believe that the evidence generated from our meta-analysis is reliable since it is based on fair to good quality studies and well-defined search methods and eligibility criteria. More than 40 studies in varied populations have been included in the final meta-analysis, with emphasis on avoiding overlapping data. In addition, we performed a subgroup analysis to test if there is an association between neurological manifestations of COVID-19 and severity of the disease. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist to prepare this study [13].
Limitations
Limitations of our analysis include the heterogeneity among the studies being considerably high both in the overall population and following the subgroup analysis. This is due to the large variation in the sample size among studies, the different study designs and methodologies, lack of uniformity in collecting and reporting of data, and possibly reflecting a true variation between different populations. Sensitivity analysis was conducted to explore the heterogeneity. Moreover, random effect model was set a priori since significant heterogeneity was expected. Besides, most of the included studies collected the data retrospectively. Finally, egger test indicated that there is a possible publication bias among the following variables: Fever, headache, serum LDH, DM, pre-existing neurological diseases, malignancy, and CKD. There is a possibility that some unpublished studies were not identified as our meta-analysis was limited to studies published in English-language and since many studies were not yet published at the time of screening. However, we tried to avoid publication bias by including studies translated into English as well as including pre-prints and contacting authors.
Conclusion
In this meta-analysis on the neurological features of COVID-19, we found that several NM and NC are associated with COVID-19, and certain features, such as CVD, muscle injury, and probably encephalopathy, might be associated with severe disease status. Healthcare professional dealing with COVID-19, neurologists, and the general public should be aware of the neurological involvement of the disease. Patients of possible COVID-19 presenting with the previously mentioned neurological features should trigger clinical suspicion. Further studies are required to assess the prevalence of the neurological aspects of COVID-19 in different populations and to directly compare them between severe and non-severe subgroups. More pathophysiological analysis and studies are required as well in order to understand the exact mechanism through which the virus affects the nervous system.
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- EEG
Electroencephalography
- EMG
Electromyography
- CK
Creatine Kinase
- CNS
Central Nervous System
- COVID-19
Coronavirus Disease 2019
- CSF
Cerebrospinal Fluid
- CT
Computed Tomography
- LDH
Lactate Dehydrogenase
- MRI
Magnetic Resonance Imaging
- NCS
Nerve Conduction Study
- SARS-CoV-2
Severe Acute Respiratory Syndrome Coronavirus 2
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- BBB
Blood Brain Barrier
- NM
Neurological Manifestations
- NC
Neurological Complications
- ND
Neurodiagnostic
Authors’ contributions
AY designed the study, searched the literature, screened the records, assessed the risk of bias, and drafted and revised the manuscript. MN designed the study, searched the literature, extracted and synthesized the data, undertook statistical analyses and interpretation, and drafted the manuscript. AS designed the study, searched the literature, assessed the risk of bias, extracted and synthesized the data, and drafted the manuscript. KA screened the records, interpreted the data, and drafted and revised the manuscript. KE screened the records, interpreted the data, and drafted and revised the manuscript. OS undertook statistical analyses and interpretation, and revised the manuscript. MA screened the records, assessed the risk of bias, and drafted and revised the manuscript. Qualifications: AY is an Assistant Professor of Neurology and Neurology Residency Program Director at Jordan University of Science and Technology/ King Abdullah University Hospital. He did his Neurology residency and Clinical Neurophysiology and Epilepsy fellowships in the United States. He has the American Boards in Neurology, Clinical Neurophysiology, Epilepsy and Medical Quality. MN graduated from the Medical School of The University of Jordan in 2019, ranking in the top 5th percentile. He finished his internship from the Royal Medical Services and is pursuing to do his residency training in Ophthalmology at the United Kingdom next year. At the same time, he is an active researcher with expertise in conducting meta-analysis and collaborates with Faculty members from different Jordanian universities in multiple research projects. AS graduated from the Medical School of The University of Jordan in 2019, ranking in the top 5th percentile. He finished his internship from the Royal Medical Services. He is currently a researcher at King Hussein Cancer Center and is pursuing to do his residency training in Neurology at the United States next year. He is an active researcher with vast skills in conducting systematic reviews and meta-analysis and collaborates with neurologists from different Jordanian institutions in multiple research projects. KA is an Associate Professor of Neurology and Neurosurgery, Director of EEG Department, and Neurocritical Care Fellowship Program Director at the University of Tennessee Health Science Center - Methodist University Hospital. He has American Boards in Neurology, Epilepsy, and Neurocritical Care Medicine. KE is a Professor of Neurology and Vice President of Jordan University of Science and Technology. He did his Neurology residency and Clinical Neurophysiology and Neuromuscular fellowships in the United States. He has the American Boards in Neurology, Clinical Neurophysiology and Neuromuscular Medicine. He is a Fellow of the American Academy of Neurology (FAAN). OS is an Assistant Professor of Community Medicine and Public Health at Yarmouk University in Jordan. She earned her PhD in Clinical Sciences/ Health Services research track from Preventive Medicine and Community Health School at University of Texas Medical Branch/Galveston-TX-USA. MA is an Assistant Professor of Neurology at The George Washington University. He has American Boards in Neurology, Clinical Neurophysiology and Epilepsy. He is the Director of Continuing Medical Education (CME) in the Department of Neurology and Co-Director of the Transcranial Magnetic Stimulation (TMS Unit. He is also a research associate at the Department of Anatomy and Regenerative Medicine. The author(s) read and approved the final manuscript.
Funding
No funding was obtained.
Availability of data and materials
All data synthesized and analyzed are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ahmed Yassin, Mohammed Nawaiseh, and Ala Shaban contributed equally and are co-first authors.
References
- 1.Johns Hopkins. Corona Virus Resource Center. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins. Available at: https://coronavirus.jhu.edu/map.html.
- 2.Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, Liu L, Shan H, Lei CL, Hui DSC, du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS, China Medical Treatment Expert Group for Covid-19 Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Y-C, Bai W-Z, Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol. 2020;92(6):552–555. doi: 10.1002/jmv.25728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Desforges M, Le Coupanec A, Dubeau P, Bourgouin A, Lajoie L, Dubé M, et al. Human coronaviruses and other respiratory viruses: underestimated opportunistic pathogens of the central nervous system? Viruses. 2020;12(1):14. doi: 10.3390/v12010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pleasure SJ, Green AJ, Josephson SA. The spectrum of neurologic disease in the severe acute respiratory syndrome coronavirus 2 pandemic infection: neurologists move to the frontlines: neurologists move to the frontlines. JAMA Neurol. 2020;77(6):679–680. doi: 10.1001/jamaneurol.2020.1065. [DOI] [PubMed] [Google Scholar]
- 6.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, Miao X, Li Y, Hu B. Neurologic manifestations of hospitalized patients with Coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xiang P, Xu XM, Gao LL, Wang HZ, Xiong HF, Li RH. First case of 2019 novel coronavirus disease with encephalitis. ChinaXiv. 2020;202003:00015. [Google Scholar]
- 8.Filatov A, Sharma P, Hindi F, Espinosa PS. Neurological Complications of Coronavirus Disease (COVID-19): Encephalopathy. Cureus. 2020;12(3):e7352. Published 2020 Mar 21. 10.7759/cureus.7352. [DOI] [PMC free article] [PubMed]
- 9.Marchese-Ragona R, Ottaviano G, Piero N, Vianello A, Miryam C. Sudden hyposmia as a prevalent symptom of COVID-19 infection. medRxiv. 2020; Available from: 10.1101/2020.04.06.20045393.
- 10.Li Y, Wang M, Zhou Y, Chang J, Xian Y, Mao L, et al. Acute cerebrovascular disease following COVID-19: A single center, retrospective, observational study. SSRN Electron J. 2020; Available from. 10.2139/ssrn.3550025. [DOI] [PMC free article] [PubMed]
- 11.Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, Ueno M, Sakata H, Kondo K, Myose N, Nakao A, Takeda M, Haro H, Inoue O, Suzuki-Inoue K, Kubokawa K, Ogihara S, Sasaki T, Kinouchi H, Kojin H, Ito M, Onishi H, Shimizu T, Sasaki Y, Enomoto N, Ishihara H, Furuya S, Yamamoto T, Shimada S. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis. 2020;94:55–58. doi: 10.1016/j.ijid.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Poyiadji N, Shahin G, Noujaim D, Stone M, Patel S, Griffith B. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: imaging features. Radiology. 2020;296(2):E119–E120. doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 14.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1) Available from:. 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed]
- 15.Health NI of. National Heart Lung, and Blood Institute . Quality assessment tool for observational cohort and cross-sectional studies. 2014. [Google Scholar]
- 16.Health NI of. Quality Assessment tool for case series studies . The National Heart, Lung, and Blood Institute. 2017. [Google Scholar]
- 17.Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27(6):1785–1805. doi: 10.1177/0962280216669183. [DOI] [PubMed] [Google Scholar]
- 18.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14(1):135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Group OL of EW . The Oxford levels of evidence 2: Oxford centre for evidence-based medicine. University of Oxford. 2011. [Google Scholar]
- 22.Chen G, Wu D, Guo W, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130(5):2620–9. 10.1172/JCI137244. [DOI] [PMC free article] [PubMed]
- 23.Liu YS, Zhang D, Tang S, Chen H, Chen L, He X, Tong M, Liu M, Lin Y, Zhu B, Su X The Epidemiological and Clinical Characteristics of 2019 Novel Coronavirus Infection in Changsha, China. 2020. Available at SSRN: https://ssrn.com/abstract=3537093 or 10.2139/ssrn.3537093.
- 24.Wang L, Gao YH, Lou LL, Zhang GJ. The clinical dynamics of 18 cases of COVID-19 outside of Wuhan, China. Eur Respir J. 2020;55(4):2000398. Published 2020 Apr 23. 10.1183/13993003.00398-2020. [DOI] [PMC free article] [PubMed]
- 25.Giacomelli A, Pezzati L, Conti F, Bernacchia D, Siano M, Oreni L. Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study. Clin Infect Dis. 2020;71(15):889–890. doi: 10.1093/cid/ciaa330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xu X, Yu C, Qu J, Zhang L, Jiang S, Huang D, Chen B, Zhang Z, Guan W, Ling Z, Jiang R, Hu T, Ding Y, Lin L, Gan Q, Luo L, Tang X, Liu J. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging. 2020;47(5):1275–1280. doi: 10.1007/s00259-020-04735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jin X, Lian J-S, Hu J-H, Gao J, Zheng L, Zhang Y-M, Hao SR, Jia HY, Cai H, Zhang XL, Yu GD, Xu KJ, Wang XY, Gu JQ, Zhang SY, Ye CY, Jin CL, Lu YF, Yu X, Yu XP, Huang JR, Xu KL, Ni Q, Yu CB, Zhu B, Li YT, Liu J, Zhao H, Zhang X, Yu L, Guo YZ, Su JW, Tao JJ, Lang GJ, Wu XX, Wu WR, Qv TT, Xiang DR, Yi P, Shi D, Chen Y, Ren Y, Qiu YQ, Li LJ, Sheng J, Yang Y. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69(6):1002–1009. doi: 10.1136/gutjnl-2020-320926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J', Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li J, Li S, Cai Y, Liu Q, Li X, Zeng Z, et al. Epidemiological and clinical characteristics of 17 hospitalized patients with 2019 novel Coronavirus infections outside Wuhan, China. medRxiv. 2020. Available from. 10.1101/2020.02.11.20022053.
- 30.Qian G-Q, Yang N-B, Ding F, Ma AHY, Wang Z-Y, Shen Y-F, et al. Epidemiologic and clinical characteristics of 91 hospitalized patients with COVID-19 in Zhejiang, China: a retrospective, multi-Centre case series. QJM. 2020;113(7):474–481. doi: 10.1093/qjmed/hcaa089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu X-W, Wu X-X, Jiang X-G, Xu K-J, Ying L-J, Ma C-L, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. [published correction appears in BMJ. 2020 Feb 27;368:m792]. BMJ. 2020;368:m606. Published 2020 Feb 19. [DOI] [PMC free article] [PubMed]
- 32.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wan S, Xiang Y, Fang W, Zheng Y, Li B, Hu Y, Lang C, Huang D, Sun Q, Xiong Y, Huang X, Lv J, Luo Y, Shen L, Yang H, Huang G, Yang R. Clinical features and treatment of COVID-19 patients in Northeast Chongqing. J Med Virol. 2020;92(7):797–806. doi: 10.1002/jmv.25783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu K, Fang Y-Y, Deng Y, Liu W, Wang M-F, Ma J-P, Xiao W, Wang YN, Zhong MH, Li CH, Li GC, Liu HG. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J. 2020;133(9):1025–1031. doi: 10.1097/CM9.0000000000000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan. China. Jama. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Qin X, Qiu S, Yuan Y, Zong Y, Tuo Z, Li J, et al. Clinical Characteristics and Treatment of Patients Infected with COVID-19 in Shishou, China. 2020. Available at SSRN: https://ssrn.com/abstract=3541147 or 10.2139/ssrn.3541147.
- 38.Yang W, Cao Q, Qin L, Wang X, Cheng Z, Pan A, Dai J, Sun Q, Zhao F, Qu J, Yan F. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19):a multi-center study in Wenzhou city, Zhejiang, China. J Infect. 2020;80(4):388–393. doi: 10.1016/j.jinf.2020.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, Xie C, Ma K, Shang K, Wang W, Tian DS. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis. 2020;71(15):762–768. doi: 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu J, Liu Y, Xiang P, Pu L, Xiong H, Li C, et al. Neutrophil-to-lymphocyte ratio predicts severe illness patients with 2019 novel Coronavirus in the early stage. bioRxiv. 2020. Available from:. 10.1101/2020.02.10.20021584.
- 41.Easom N, Moss P, Barlow G, Samson A, Taynton T, Adams K, Ivan M, Burns P, Gajee K, Eastick K, Lillie PJ. Sixty-eight consecutive patients assessed for COVID-19 infection: experience from a UK regional infectious diseases unit. Influenza Other Respir Viruses. 2020;14(4):374–379. doi: 10.1111/irv.12739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Deng Y, Liu W, Liu K, Fang Y-Y, Shang J, Wang K, et al. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 (COVID-19) in Wuhan, China: a retrospective study. Chin Med J. 2020;133(11):1261–1267. doi: 10.1097/CM9.0000000000000824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huang Y, Tu M, Wang S, Chen S, Zhou W, Chen D, et al. Clinical characteristics of laboratory confirmed positive cases of SARS-CoV-2 infection in Wuhan, China: A retrospective single center analysis. Travel Med Infect Dis. 2020;36:101606. doi: 10.1016/j.tmaid.2020.101606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mo P, Xing Y, Xiao Y, Deng L, Zhao Q, Wang H, et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis. 2020. 10.1093/cid/ciaa270. Online ahead of print.
- 45.Zheng F, Tang W, Li H, Huang YX, Xie YL, Zhou ZG. Clinical characteristics of 161 cases of corona virus disease 2019 (COVID-19) in Changsha. Eur Rev Med Pharmacol Sci. 2020;24(6):3404–3410. doi: 10.26355/eurrev_202003_20711. [DOI] [PubMed] [Google Scholar]
- 46.Guo T-M, Tong Y, Chen J, Huang L, Cheng B, Zhoue J. Clinical features predicting mortality risk in older patients with COVID-19. SSRN Electron J. 2020; Available from:. 10.2139/ssrn.3569846. [DOI] [PubMed]
- 47.Yan X, Wang C, Peng D, Han X, Fan Y, Fang Z, et al. Clinical features, treatment and outcomes of 218 patients with COVID-19: A retrospective, multicenter study based on clinical classification. SSRN Electron J. 2020; Available from:. 10.2139/ssrn.3559594.
- 48.Chang D, Lin M, Wei L, Xie L, Zhu G, Cruz CSD, et al. Epidemiologic and clinical characteristics of novel coronavirus infections involving 13 patients outside Wuhan, China. Jama. 2020;323(11):1092–1093. doi: 10.1001/jama.2020.1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang R, Pan M, Zhang X, Fan X, Han M, Zhao F, et al. Epidemiological and clinical features of 125 hospitalized patients with COVID-19 in Fuyang, Anhui, China. Int J Infect Dis. 2020;95:421–428. doi: 10.1016/j.ijid.2020.03.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhou J, Sun J-J, Cao Z-Q, Wang W-C, Huang K, Zheng F, et al. Epidemiological and clinical features of 201 COVID-19 patients in Changsha, China. Research Square. 2020. Available from:. 10.21203/rs.3.rs-17313/v1. [DOI] [PMC free article] [PubMed]
- 51.Zheng Y, Xu H, Yang M, Zeng Y, Chen H, Liu R, Li Q, Zhang N, Wang D. Epidemiological characteristics and clinical features of 32 critical and 67 noncritical cases of COVID-19 in Chengdu. J Clin Virol. 2020;127:104366. doi: 10.1016/j.jcv.2020.104366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Helms J, Kremer S, Merdji H, Clere-Jehl R, Schenck M, Kummerlen C, Collange O, Boulay C, Fafi-Kremer S, Ohana M, Anheim M, Meziani F. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020;382(23):2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lechien JR, Chiesa-Estomba CM, De Siati DR, Horoi M, Le Bon SD, Rodriguez A, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. 2020;277(8):2251–2261. doi: 10.1007/s00405-020-05965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen W, Chen C, Huang L, Ye K, Lv L, Qin Z, et al. Clinical Characteristics of 85 Patients Infected by SARS-CoV-2 in Guangxi, China. 2020. [Google Scholar]
- 55.Jiang X, Tao J, Wu H, Wang Y, Zhao W, Zhou M, et al. Clinical features and management of severe COVID-19: A retrospective study in Wuxi, Jiangsu Province, China. medRxiv. 2020. Available from:. 10.1101/2020.04.10.20060335.
- 56.Zhang G, Hu C, Luo L, Fang F, Chen Y, Li J, Peng Z, Pan H. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. J Clin Virol. 2020;127:104364. doi: 10.1016/j.jcv.2020.104364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tabata S, Imai K, Kawano S, Ikeda M, Kodama T, Miyoshi K, et al. The clinical characteristics of COVID-19: a retrospective analysis of 104 patients from the outbreak on board the Diamond Princess cruise ship in Japan. medRxiv. 2020. Available from:. 10.1101/2020.03.18.20038125.
- 58.Lei Z, Cao H, Jie Y, Huang Z, Guo X, Chen J, Peng L, Cao H, Dai X, Liu J, Li X, Zhu J, Xu W, Chen D, Gao Z, He JR, Lin BL. A cross-sectional comparison of epidemiological and clinical features of patients with coronavirus disease (COVID-19) in Wuhan and outside Wuhan, China. Travel Med Infect Dis. 2020;35:101664. doi: 10.1016/j.tmaid.2020.101664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. [published correction appears in lancet. 2020 mar 28;395(10229):1038] [published correction appears in lancet. 2020 mar 28;395(10229):1038] Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Spinato G, Fabbris C, Polesel J, Cazzador D, Borsetto D, Hopkins C, Boscolo-Rizzo P. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. JAMA. 2020;323(20):2089–2090. doi: 10.1001/jama.2020.6771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers D, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: an updated analysis. Thromb Res. 2020;191:148–150. doi: 10.1016/j.thromres.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.COVID-19 National Incident Room Surveillance Team. COVID-19, Australia: Epidemiology Report 12 (Reporting week to 23:59 AEST 19 April 2020). Commun Dis Intell (2018). 2020;44. Available from. 10.33321/cdi.2020.44.36. [DOI] [PubMed]
- 63.Zhao K, Huang J, Dai D, Feng Y, Liu L, Nie S. Acute myelitis after SARS-CoV-2 infection: a case report. medRxiv. 2020. Available from:. 10.1101/2020.03.16.20035105.
- 64.Villalba NL, Maouche Y, Ortiz MBA, Sosa ZC, Chahbazian JB, Syrovatkova A, et al. Anosmia and dysgeusia in the absence of other respiratory diseases: should COVID-19 infection be considered? Eur J Case Rep Intern Med. 2020;7:001641. 10.12890/2020_001641. [DOI] [PMC free article] [PubMed]
- 65.Ollarves-Carrero MF, Rodriguez-Morales AG, Bonilla-Aldana DK, Rodriguez-Morales AJ. Anosmia in a healthcare worker with COVID-19 in Madrid, Spain. Travel Med Infect Dis. 2020;35:101666. doi: 10.1016/j.tmaid.2020.101666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sharifi-Razavi A, Karimi N, Rouhani N. COVID-19 and intracerebral haemorrhage: causative or coincidental? New Microbes New Infect. 2020;35(100669):100669. doi: 10.1016/j.nmni.2020.100669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Novi G, Mikulska M, Briano F, Toscanini F, Tazza F, Uccelli A, Inglese M. COVID-19 in a MS patient treated with ocrelizumab: does immunosuppression have a protective role? Mult Scler Relat Disord. 2020;42(102120):102120. doi: 10.1016/j.msard.2020.102120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Karimi N, Sharifi Razavi A, Rouhani N. Frequent convulsive seizures in an adult patient with COVID-19: A case report. Iran Red Crescent Med J. 2020;22(3) Available from:. 10.5812/ircmj.102828.
- 69.Zhao H, Shen D, Zhou H, Liu J, Chen S. Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol. 2020;19(5):383–384. doi: 10.1016/S1474-4422(20)30109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gane SB, Kelly C, Hopkins C. Isolated sudden onset anosmia in COVID-19 infection. A novel syndrome? Rhinology. 2020;58(3):299–301. doi: 10.4193/Rhin20.114. [DOI] [PubMed] [Google Scholar]
- 71.Hjelmesæth J, Skaare D. Loss of smell or taste as the only symptom of COVID-19. Tidsskr Nor Laegeforen. 2020;140(7) Available from:. 10.4045/tidsskr.20.0287. [DOI] [PubMed]
- 72.Toscano G, Palmerini F, Ravaglia S, Ruiz L, Invernizzi P, Cuzzoni MG, Franciotta D, Baldanti F, Daturi R, Postorino P, Cavallini A, Micieli G. Guillain-Barré syndrome associated with SARS-CoV-2. N Engl J Med. 2020;382(26):2574–2576. doi: 10.1056/NEJMc2009191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Suwanwongse K, Shabarek N. Rhabdomyolysis as a Presentation of 2019 Novel Coronavirus Disease. Cureus. 2020;12(4):e7561. 10.7759/cureus.7561. [DOI] [PMC free article] [PubMed]
- 74.Wang J, Hajizadeh N, Moore EE, McIntyre RC, Moore PK, Veress LA, et al. Tissue plasminogen activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): a case series. J Thromb Haemost. 2020;18(7):1752–1755. doi: 10.1111/jth.14828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang Z, Chen X, Lu Y, Chen F, Zhang W. Clinical characteristics and therapeutic procedure for four cases with 2019 novel coronavirus pneumonia receiving combined Chinese and Western medicine treatment. Biosci Trends. 2020;14(1):64–68. doi: 10.5582/bst.2020.01030. [DOI] [PubMed] [Google Scholar]
- 76.Ren L-L, Wang Y-M, Wu Z-Q, Xiang Z-C, Guo L, Xu T, Jiang YZ, Xiong Y, Li YJ, Li XW, Li H, Fan GH, Gu XY, Xiao Y, Gao H, Xu JY, Yang F, Wang XM, Wu C, Chen L, Liu YW, Liu B, Yang J, Wang XR, Dong J, Li L, Huang CL, Zhao JP, Hu Y, Cheng ZS, Liu LL, Qian ZH, Qin C, Jin Q, Cao B, Wang JW. Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chin Med J. 2020;133(9):1015–1024. doi: 10.1097/CM9.0000000000000722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, Zimmer T, Thiel V, Janke C, Guggemos W, Seilmaier M, Drosten C, Vollmar P, Zwirglmaier K, Zange S, Wölfel R, Hoelscher M. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wang W, Tang J, Wei F. Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan, China. J Med Virol. 2020;92(4):441–447. doi: 10.1002/jmv.25689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chen R, Wang K, Yu J, Howard D, French L, Chen Z, et al. The spatial and cell-type distribution of SARS-CoV-2 receptor ACE2 in human and mouse brain. bioRxiv. 2020. Available from:. 10.1101/2020.04.07.030650. [DOI] [PMC free article] [PubMed]
- 80.Hamming I, Timens W, Bulthuis MLC, Lely AT, Navis GJ, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ye M, Ren Y, Lv T. Encephalitis as a clinical manifestation of COVID-19. Brain Behav Immun. 2020;88:945–946. doi: 10.1016/j.bbi.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Robinson CP, Busl KM. Neurologic Manifestations of Severe Respiratory Viral Contagions. Crit Care Explor. 2020;2(4):e0107. Published 2020 Apr 29. 10.1097/CCE.0000000000000107. [DOI] [PMC free article] [PubMed]
- 83.Sohal S, Mossammat M. COVID-19 Presenting with Seizures. IDCases. 2020. p. e00782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Vohora D, Jain S, Tripathi M, Potschka H. COVID-19 and seizures: is there a link? Epilepsia. 2020;61(9):1840–1853. doi: 10.1111/epi.16656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nath A. Neurologic complications of coronavirus infections. Neurology. 2020;94(19):809–810. doi: 10.1212/WNL.0000000000009455. [DOI] [PubMed] [Google Scholar]
- 86.Paniz-Mondolfi A, Bryce C, Grimes Z, Gordon RE, Reidy J, Lednicky J, Sordillo EM, Fowkes M. Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) J Med Virol. 2020;92(7):699–702. doi: 10.1002/jmv.25915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gu J, Gong E, Zhang B, Zheng J, Gao Z, Zhong Y, Zou W, Zhan J, Wang S, Xie Z, Zhuang H, Wu B, Zhong H, Shao H, Fang W, Gao D, Pei F, Li X, He Z, Xu D, Shi X, Anderson VM, Leong ASY. Multiple organ infection and the pathogenesis of SARS. J Exp Med. 2005;202(3):415–424. doi: 10.1084/jem.20050828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Xu H, Zhong L, Deng J, Peng J, Dan H, Zeng X, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12(1):1–5. doi: 10.1038/s41368-019-0067-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol. 2008;82(15):7264–7275. doi: 10.1128/JVI.00737-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sungnak W, Huang N, Bécavin C, Berg M, Queen R, Litvinukova M, et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. 2020;26(5):681–687. doi: 10.1038/s41591-020-0868-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sedaghat AR, Gengler I, Speth MM. Olfactory dysfunction: a highly prevalent symptom of COVID-19 with public health significance. Otolaryngol Head Neck Surg. 2020;163(1):12–15. doi: 10.1177/0194599820926464. [DOI] [PubMed] [Google Scholar]
- 92.Cabello-Verrugio C, Morales MG, Rivera JC, Cabrera D, Simon F. Renin-angiotensin system: an old player with novel functions in skeletal muscle. Med Res Rev. 2015;35(3):437–463. doi: 10.1002/med.21343. [DOI] [PubMed] [Google Scholar]
- 93.Ding Y, He L, Zhang Q, Huang Z, Che X, Hou J, Wang H, Shen H, Qiu L, Li Z, Geng J, Cai J, Han H, Li X, Kang W, Weng D, Liang P, Jiang S. Organ distribution of severe acute respiratory syndrome (SARS) associated coronavirus (SARS-CoV) in SARS patients: implications for pathogenesis and virus transmission pathways. J Pathol. 2004;203(2):622–630. doi: 10.1002/path.1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Disser NP, De Micheli AJ, Schonk MM, Konnaris MA, Piacentini AN, Edon DL, et al. Musculoskeletal consequences of COVID-19. J Bone Joint Surg Am. 2020;102(14):1197–1204. doi: 10.2106/JBJS.20.00847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zakeri A, Jadhav AP, Sullenger BA, Nimjee SM. Ischemic stroke in COVID-19-positive patients: an overview of SARS-CoV-2 and thrombotic mechanisms for the neurointerventionalist. J Neurointerv Surg. 2021;13(3):202–206. doi: 10.1136/neurintsurg-2020-016794. [DOI] [PubMed] [Google Scholar]
- 96.Devreese KMJ, Linskens EA, Benoit D, Peperstraete H. Antiphospholipid antibodies in patients with COVID-19: a relevant observation? J Thromb Haemost. 2020;18(9):2191–2201. doi: 10.1111/jth.14994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mankad K, Perry MD, Mirsky DM, Rossi A. COVID-19: a primer for Neuroradiologists. Neuroradiology. 2020;62(6):647–648. doi: 10.1007/s00234-020-02437-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Akhmerov A, Marbán E. COVID-19 and the heart. Circ Res. 2020;126(10):1443–1455. doi: 10.1161/CIRCRESAHA.120.317055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Temporary emergency guidance to US stroke centers during the coronavirus disease 2019 (COVID-19) pandemic: on behalf of the American Heart Association/American Stroke Association stroke council leadership. Stroke. 2020;51(6):1910–2. 10.1161/STROKEAHA.120.030023. [DOI] [PubMed]
- 101.Siegler JE, Heslin ME, Thau L, Smith A, Jovin TG. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis. 2020;29(8):104953. doi: 10.1016/j.jstrokecerebrovasdis.2020.104953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sharma M, Lioutas V-A, Madsen T, Clark J, O’Sullivan J, Elkind MSV, et al. Decline in stroke alerts and hospitalisations during the COVID-19 pandemic. Stroke Vasc Neurol. 2020;5(4):403–405. doi: 10.1136/svn-2020-000441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020;51(7):1996–2001. doi: 10.1161/STROKEAHA.120.030225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Aguiar de Sousa D, Sandset EC, Elkind MSV. The curious case of the missing strokes during the COVID-19 pandemic. Stroke. 2020;51(7):1921–1923. doi: 10.1161/STROKEAHA.120.030792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cerase A, Guazzi G, Mazzei MA. Letter by Cerase et al regarding article, “temporary emergency guidance to US stroke centers during the COVID-19 pandemic”. Stroke. 2020;51(7):e139–e140. doi: 10.1161/STROKEAHA.120.030147. [DOI] [PubMed] [Google Scholar]
- 106.Siddiqui J, Bala F, Sciacca S, Falzon AM, Benger M, Matloob SA, Miller FNAC, Simister RJ, Chatterjee I, Sztriha LK, Davagnanam I, Booth TC. COVID-19 stroke apical lung examination study: a diagnostic and prognostic imaging biomarker in suspected acute stroke. AJNR Am J Neuroradiol. 2021;42(1):138–143. doi: 10.3174/ajnr.A6832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Moore JB, June CH. Cytokine release syndrome in severe COVID-19. Science. 2020;368(6490):473–474. doi: 10.1126/science.abb8925. [DOI] [PubMed] [Google Scholar]
- 108.Spiezia L, Boscolo A, Poletto F, Cerruti L, Tiberio I, Campello E, Navalesi P, Simioni P. COVID-19-related severe hypercoagulability in patients admitted to intensive care unit for acute respiratory failure. Thromb Haemost. 2020;120(6):998–1000. doi: 10.1055/s-0040-1710018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(5):846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Asadi-Pooya AA, Simani L. Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci. 2020;413(116832):116832. doi: 10.1016/j.jns.2020.116832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Montalvan V, Lee J, Bueso T, De Toledo J, Rivas K. Neurological manifestations of COVID-19 and other coronavirus infections: a systematic review. Clin Neurol Neurosurg. 2020;194(105921):105921. doi: 10.1016/j.clineuro.2020.105921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Paterson RW, Brown RL, Benjamin L, Nortley R, Wiethoff S, Bharucha T, Jayaseelan DL, Kumar G, Raftopoulos RE, Zambreanu L, Vivekanandam V, Khoo A, Geraldes R, Chinthapalli K, Boyd E, Tuzlali H, Price G, Christofi G, Morrow J, McNamara P, McLoughlin B, Lim ST, Mehta PR, Levee V, Keddie S, Yong W, Trip SA, Foulkes AJM, Hotton G, Miller TD, Everitt AD, Carswell C, Davies NWS, Yoong M, Attwell D, Sreedharan J, Silber E, Schott JM, Chandratheva A, Perry RJ, Simister R, Checkley A, Longley N, Farmer SF, Carletti F, Houlihan C, Thom M, Lunn MP, Spillane J, Howard R, Vincent A, Werring DJ, Hoskote C, Jäger HR, Manji H, Zandi MS. The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings. Brain. 2020;143(10):3104–3120. doi: 10.1093/brain/awaa240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ahmad I, Rathore FA. Neurological manifestations and complications of COVID-19: a literature review. J Clin Neurosci. 2020;77:8–12. doi: 10.1016/j.jocn.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kim J-E, Heo J-H, Kim H, Song S, Park S-S, Park T-H, Ahn JY, Kim MK, Choi JP. Neurological complications during treatment of Middle East respiratory syndrome. J Clin Neurol. 2017;13(3):227–233. doi: 10.3988/jcn.2017.13.3.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sharma K, Tengsupakul S, Sanchez O, Phaltas R, Maertens P. Guillain–Barré syndrome with unilateral peripheral facial and bulbar palsy in a child: A case report. SAGE Open Med Case Rep. 2019;7:2050313X19838750. doi: 10.1177/2050313X19838750. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data synthesized and analyzed are included in this published article.