Abstract
Few studies have derived data-driven dietary patterns in youth in the United States (US). This study examined data-driven dietary patterns and their associations with BMI measures in predominantly low-income, racial/ethnic minority US youth. Data were from baseline assessments of the four Childhood Obesity Prevention and Treatment Research (COPTR) Consortium trials: NET-Works (N=534; 2–4-year-olds), GROW (N=610; 3–5-year-olds), GOALS (N=241; 7–11-year-olds), and IMPACT (N=360; 10–13-year-olds). Weight and height were measured. Children/adult proxies completed 3 24-hour dietary recalls. Dietary patterns were derived for each site from 24 food/beverage groups using k-means cluster analysis. Multivariable linear regression models examined associations of dietary patterns with BMI and percentage of the 95th BMI percentile. Healthy (produce and whole grains) and Unhealthy (fried food, savory snacks, and desserts) patterns were found in NET-Works and GROW. GROW additionally had a dairy and sugar-sweetened beverage based pattern. GOALS had a similar Healthy pattern and a pattern resembling a traditional Mexican diet. Associations between dietary patterns and BMI were only observed in IMPACT. In IMPACT, youth in the Sandwich (cold cuts, refined grains, cheese, and miscellaneous [e.g., condiments]) compared to Mixed (whole grains and desserts) cluster had significantly higher BMI [β=0.99 (95% CI: 0.01, 1.97)] and percentage of the 95th BMI percentile [β=4.17 (95% CI: 0.11, 8.24)]. Healthy and Unhealthy patterns were the most common dietary patterns in COPTR youth, but diets may differ according to age, race/ethnicity, or geographic location. Public health messages focused on healthy dietary substitutions may help youth mimic a dietary pattern associated with lower BMI.
Keywords: dietary patterns, cluster analysis, youth, BMI, ethnic minority
INTRODUCTION
The prevalence of obesity among 2–19-year-olds in the United States (US) is 18.5%, with ethnic/racial minority youth facing the highest burden of obesity(1). Diet is a known contributor to risk for obesity(2), but associations based on individual foods or nutrients are less consistent than those for dietary patterns(3). Examining dietary patterns instead of individual foods/nutrients is advantageous because it allows researchers to measure the totality of individuals’ dietary intake and the complex, multidimensional nature of diets(4). Dietary patterns may also better predict risk for cardiometabolic diseases because they can capture both over- and under-consumption of key nutrients or foods over time(3,5).
Dietary patterns can be operationalized with various dietary quality indices and scores. For example, children’s diet quality has been examined using the Healthy Eating Index-2010 (HEI-2010)(6), Dietary Approaches to Stop Hypertension (DASH) scores(7), and the Mediterranean Diet Quality Index for children and adolescents (KIDMED)(8,9). These scores are based on recommended “healthy” dietary patterns that have been defined a priori. While these scores are useful for studying the quality of diets and associations with health outcomes, the optimal utility of a priori defined dietary patterns in epidemiological studies is limited to populations with a broad distribution of scores for a given index. Often the scores in a given sample are not well distributed, and thus an alternative approach is needed.
For example, in the four randomized controlled trials (RCTs) within the Childhood Obesity Prevention and Treatment Research (COPTR) Consortium(10)—which examined predominantly low-income, racial/ethnic minority youth aged 2-5 or 7-13 years—HEI-2010 scores in each study were narrowly distributed. Specifically, out of a possible score of 100, the mean and 95% confidence intervals (CIs) for each study were: 63.7 (95% CI: 62.8, 64.7), 64.5 (95% CI: 63.6, 65.4), 47.9 (95% CI: 46.8, 49.0), and 61.7 (95% CI: 60.3, 63.2)(6). Further, an HEI-2010 score ≥81 indicated good dietary quality(6), but only 0.3-8.1% of participants met this criterion across the four COPTR studies. Such a narrow range of scores does not allow for accurate examination of associations between HEI-2010 scores and outcomes like body mass index (BMI).
An alternative approach to using a priori defined dietary patterns is using data-driven methodology, including k-means cluster analysis(11). K-means cluster analysis identifies groups of individuals with similar dietary intakes(12). By design, cluster analysis is exploratory and sample-specific, and it relies on the researcher making informed decisions on topics ranging from food groupings to the number of clusters to examine(12,13). However, cluster analysis has a distinct benefit over a priori approaches because it allows researchers to search for the patterns that actually occur in a given sample, regardless of distributions of a priori scores or of overall dietary quality(14). Previous reviews have examined data-driven dietary patterns in young children (aged 1 to 5 years)(15) and wider age ranges of children/adolescents (aged 2 to 19 years)(16). The derived dietary patterns in youth are often named “Healthy” and “Unhealthy”, with some studies identifying a third, culture-specific dietary pattern called a “Traditional” pattern(15,16). For example, a Traditional pattern in a cohort of youth from the United Kingdom (UK) was typified by high consumption of meat/meat pies, potatoes, fried fish, dairy, cakes/buns, and puddings(17).
To our knowledge, only three previous studies have derived overall dietary patterns using cluster analysis in US children(18–20). While these studies have included racially/ethnically diverse groups, with one specifically deriving dietary patterns for Black adolescents(19), none of these studies included samples that were predominantly Hispanic and two of the studies used data collected during the late 1980s and 1990s(18,19). Given changes in US children’s dietary intake from the 1980s to 2010(21) and evidence that dietary patterns differ according to race and ethnicity(19,22), there is a need to derive dietary patterns using recent data for multi-ethnic US youth. This is especially needed among samples that are predominantly Hispanic and non-Hispanic Black, populations with a higher prevalence of childhood obesity than non-Hispanic White youth (25.8% and 22.0% vs. 14.1%, respectively)(1). Further, no studies in US children have examined associations between data-driven dietary patterns and BMI measures, with only one study having examined this association in adolescents(19). There is a particular need to examine the association between dietary patterns and BMI in Mexican American youth, given inconsistent findings in the association between a Traditional Mexican dietary pattern (i.e., high intake of tortillas, beans, squash, tomato, chile, and onion)(23) and risk for obesity in adults(24,25). Notably, the one study conducted in the US actually indicated that adults following a Traditional Mexican dietary pattern trended towards a higher BMI(24).
In this study, our objective was to fill these gaps by deriving data-driven dietary patterns and examining the associations of these patterns with baseline BMI and percentage of the 95th BMI percentile in low-income, racial/ethnic minority children enrolled in the four trials of the COPTR Consortium(10). We hypothesized that Healthy and Unhealthy patterns would be derived for each study and that a Traditional Mexican pattern representing Mexican food culture would be derived for studies with a high percentage of Mexican American participants. We expected an inverse association between the Healthy pattern and BMI measures and a positive association between the Unhealthy and Traditional dietary patterns and BMI measures, based on previous literature.
METHODS
Research population.
All data were collected between 2012 and 2014 during baseline examinations of the four COPTR Consortium studies. The COPTR Consortium included two obesity prevention randomized controlled trials (RCTs; University of Minnesota, Now Everyone Together for Healthy and Amazing Kids [NET-Works](26) and Vanderbilt University, Growing Right Onto Wellness [GROW](27)), two obesity treatment RCTs (Stanford University, GOALS(28) and Case Western Reserve University, Ideas Moving Parents and Adolescents to Change Together [IMPACT](29)), and a Research Coordinating Unit (The University of North Carolina at Chapel Hill)(10). These studies recruited predominantly low-income, racial/ethnic minority populations for three-year multi-level obesity interventions(10,26–29). Each study had different intervention protocols, sample sizes, and eligibility criteria. Preschool-aged children were recruited for the NET-Works (N=534 2- to 4-year-olds ≥50th BMI percentile) and GROW (N=610 3- to 5-year-olds ≥50th and <95th BMI percentile) studies(26,27). Pre-adolescent and adolescent children with overweight or obesity were recruited for the GOALS (N=241 7- to 11-year-olds ≥85th BMI percentile) and IMPACT (N=360 rising 6th graders ≥85th BMI percentile, resulting in recruitment of 10- to 13-year-olds) studies(28,29). Additional details of the COPTR Consortium and each intervention study have previously been published(10,26–29).
The COPTR studies were conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects/patients were approved by the University of Minnesota (NET-Works), Vanderbilt University Medical Center (GROW), Stanford University Administrative Panel on Human Subjects in Medical Research (GOALS), and the University Hospitals of Cleveland Human Subjects (IMPACT). Written informed consent was obtained from parents in all COPTR studies; children additionally provided written assent in GOALS and IMPACT. A data and safety monitoring board appointed by the National Heart, Lung, and Blood Institute approved all study protocols and monitored participant safety and protocol adherence throughout the trials.
Dietary assessment.
Dietary intake of each child was assessed using three 24-hour dietary recalls collected via the Nutrition Database System for Research (NDSR) software (versions 2011-2013) developed by the Nutrition Coordinating Center, University of Minnesota, Minneapolis, Minnesota(10,30). All dietary recalls were conducted in English or Spanish, and each study aimed to collect data from participants on both weekends and weekdays(26–29). Dietary recalls were collected either in person or by telephone. Respondents were provided with two-dimensional food portion aids to assist in identifying portion sizes for each recall(26–29).
In the GOALS and IMPACT studies, the child self-reported their dietary intake with parental/guardian assistance as needed(28,29). Because children in NET-Works and GROW were younger, a parent/guardian served as a proxy for the child(26,27). For children in childcare, food records were given to the childcare provider, and the completed form was used by the parent/guardian to aid in dietary recall completion(26,27). For the purpose of analysis, intake was measured in terms of number of servings, and individual foods/beverages were collapsed into 24 food groups (Supplementary Table 1). Intake was averaged across recalls within child.
Outcome assessment.
Weight and height were measured with the child in light clothing without shoes using a standardized protocol across all studies(26–29). Weight was measured to the nearest 0.1 kg, and height was measured to the nearest 0.1 cm(26–29). BMI was calculated as weight in kilograms divided by height in meters squared. Age- and sex-specific BMI percentiles were calculated using the Centers for Disease Control and Prevention (CDC) SAS program(31) (based on the CDC growth charts) to determine site-specific eligibility. However, the highest percentile estimated in the CDC growth charts was the 97th percentile, and thus using this program to estimate the BMI percentile for an individual with a very high BMI is not recommended and has been shown to be inaccurate(31–33). The CDC recommends that, if a large portion of youth in an analysis has severe obesity (as was the case in COPTR), that all BMIs should be expressed relative to the 95th percentile (“percentage of the 95th BMI percentile”)(31). This variable is a better measure of adiposity for these youth and can be interpreted as in the following example: if the percentage of the 95th BMI percentile is equal to 160, the child would have a BMI equal to 1.6 times the CDC-defined age- and sex-specific 95th BMI percentile. Percentage of the 95th BMI percentile was thus calculated for all youth using the CDC SAS program(31).
Covariate assessment.
The primary parent/guardian completed questionnaires in their language of choice (English or Spanish) to assess the following variables: race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, multi-racial, or other) of the child, age and sex of the child, employment status (full-time, part-time, or not working for pay), highest household education (<high school, high school or equivalent, or at least some college), Supplemental Nutrition Assistance Program (SNAP) participation (yes/no), and marital status (single or married/living as married)(26–29). Regarding Hispanic ethnicity, parents were asked to indicate whether the child was of “Hispanic, Latino/a, or Spanish” origin. If they selected “yes”, they then indicated (selecting all that applied) whether the child was Mexican American, Chicano/a; Puerto Rican; Cuban; or another Hispanic, Latino/a, or Spanish origin(26–29). Parent’s height and weight were also measured by trained examiners using a standardized protocol across all studies(26–29). Parent’s weight status was determined according to existing standards: underweight (BMI<18.5 kg/m2), normal weight (BMI 18.5-24.9 kg/m2), overweight (BMI 25.0-29.9 kg/m2), or obese (BMI≥30 kg/m2)(34). Due to few individuals being classified as underweight in each study, the underweight and normal weight groups were combined for analysis.
Statistical analysis.
To derive dietary patterns, a k-means cluster analysis(11) was conducted for each study separately among children with at least two dietary recalls (n=1 from GROW was excluded due to having only 1 dietary recall; analytic sample sizes as follows: NET-Works [N=534], GROW [n=609], GOALS [N=241], and IMPACT [N=360]). Each cluster analysis was based on energy-adjusted, standardized versions of the 24 dietary variables. Specifically, each of the dietary variables was energy-adjusted by dividing intake (average servings) by average total daily caloric intake and subsequently multiplying by 1000 to create a variable of “servings/1000 calories”(35). Each variable was then standardized using z-scores to calibrate for the magnitude across variables(35). Cluster solutions with 2 to 10 clusters were examined, and each analysis was run for a maximum of 1000 iterations. Seeds containing less than or equal to 5% of the sample were removed during each iteration to ensure adequate sample sizes in the resulting clusters(36). The best solution was selected according to the pseudo-F statistic(11,37).
To examine the predictors of dietary patterns and associations between dietary patterns and measures of BMI, participants with missing socio-demographic and anthropometric data were further excluded. Individuals were excluded for missing primary parent/guardian employment status (GROW n=1), SNAP participation (NET-Works n=1; GROW n=2; GOALS n=1), primary parent/guardian marital status (GROW n=2; IMPACT n=2), and primary parent/guardian’s weight status (NET-Works n=6; IMPACT n=17). This corresponded to excluding the following percentages of each study: 1% of NET-Works and GROW, <1% of GOALS, and 5% of IMPACT. The final analytic sample sizes were as follows: NET-Works (n=527), GROW (n=604), GOALS (n=240), and IMPACT (n=341).
Multiple logistic or multinomial logistic regression models were used to examine the odds of cluster membership according to socio-demographic and anthropometric characteristics. Multivariable linear regression models were used to examine associations between cluster membership and BMI or percentage of the 95th BMI percentile. Covariates in these models included child’s age, child’s sex, highest household education, primary parent/guardian employment, SNAP participation, primary parent/guardian marital status, and primary parent/guardian weight status. Significance was set at p<0.05 for all analyses. All analyses were conducted using SAS version 9.4 (Cary, NC).
RESULTS
Table 1 presents the socio-demographic and anthropometric characteristics for each COPTR study. All studies except IMPACT were predominantly Hispanic, with IMPACT being predominantly non-Hispanic Black. Hispanic individuals in NET-Works, GROW, and GOALS primarily reported being Mexican American/Chicano/a (74%, 70%, and 85%, respectively; data not shown in Table 1). Parents in each study most frequently reported not working for pay, and the majority of households in GROW (75.5%) and IMPACT (70.6%) were SNAP participants.
Table 1.
Characteristics of child and primary parent/guardian in the analytic sample for each COPTR study
| Prevention studies |
Treatment studies |
|||||||
|---|---|---|---|---|---|---|---|---|
| NET-Works (N=534) | GROW (n=609) | GOALS (N=241) | IMPACT (N=360) | |||||
| n or mean | % or SD | n or mean | % or SD | n or mean | % or SD | n or mean | % or SD | |
| Child’s sex (n and %) | ||||||||
| Male | 262 | 49.1 | 294 | 48.3 | 107 | 44.4 | 152 | 42.2 |
| Female | 272 | 50.9 | 315 | 51.7 | 134 | 55.6 | 208 | 57.8 |
| Parent’s sex (n and %) | ||||||||
| Male | 44 | 8.3 | 10 | 1.6 | 12 | 5.0 | 20 | 5.6 |
| Female | 489 | 91.7 | 599 | 98.4 | 229 | 95.0 | 339 | 94.4 |
| Missing | 1 | - | - | - | - | - | 1 | - |
| Child’s age, years (Mean and SD) | 3.4 | 0.7 | 4.3 | 0.9 | 9.5 | 1.4 | 11.6 | 0.6 |
| Child’s race/ethnicity (n and %) | ||||||||
| Non-Hispanic White | 67 | 12.5 | 6 | 1.0 | 0 | 0.0 | 14 | 3.9 |
| Non-Hispanic Black | 98 | 18.4 | 36 | 5.9 | 4 | 1.7 | 276 | 76.7 |
| Hispanic | 312 | 58.4 | 554 | 91.0 | 236 | 97.9 | 59 | 16.4 |
| Multiracial/Other | 57 | 10.7 | 13 | 2.1 | 1 | 0.4 | 11 | 3.1 |
| Highest household education (n and %) | ||||||||
| <High school | 178 | 33.3 | 316 | 51.9 | 153 | 63.5 | 65 | 18.1 |
| High school or GED | 118 | 22.1 | 157 | 25.8 | 41 | 17.0 | 101 | 28.1 |
| ≥Some higher education | 238 | 44.6 | 136 | 22.3 | 47 | 19.5 | 194 | 53.9 |
| Parent employment (n and %) | ||||||||
| Not working for pay | 227 | 42.5 | 381 | 62.7 | 105 | 43.6 | 160 | 44.4 |
| Part time | 148 | 27.7 | 119 | 19.6 | 58 | 24.1 | 64 | 17.8 |
| Full time | 159 | 29.8 | 108 | 17.8 | 78 | 32.4 | 136 | 37.8 |
| Missing | - | - | 1 | - | - | - | - | - |
| SNAP participant (n and %) | ||||||||
| Yes | 229 | 43.0 | 458 | 75.5 | 98 | 40.8 | 254 | 70.6 |
| No | 304 | 57.0 | 149 | 24.5 | 142 | 59.2 | 106 | 29.4 |
| Missing | 1 | - | 2 | - | 1 | - | 1 | - |
| Parent marital status (n and %) | ||||||||
| Married/Living as married | 367 | 68.7 | 503 | 82.9 | 207 | 85.9 | 119 | 33.2 |
| Single | 167 | 31.1 | 104 | 17.1 | 34 | 14.1 | 239 | 66.8 |
| Missing | - | - | 2 | - | - | - | 2 | - |
| Child’s BMI, kg/m2 (Mean and SD) | 17.6 | 1.8 | 16.7 | 0.8 | 25.1 | 4.0 | 27.1 | 4.9 |
| Child’s BMI percentile* (Mean and SD) | 81.7 | 14.3 | 77.2 | 13.0 | 96.5 | 3.2 | 95.7 | 3.7 |
| Child’s %95th BMI percentile† (Mean and SD) | 96.5 | 9.8 | 92.0 | 4.3 | 114.0 | 17.9 | 111.7 | 20.2 |
| Parent weight status‡ (n and %) | ||||||||
| Under-/Normal weight | 128 | 24.2 | 121 | 19.9 | 31 | 12.9 | 34 | 9.9 |
| Overweight | 162 | 30.7 | 239 | 39.2 | 77 | 32.0 | 60 | 17.5 |
| Obesity | 238 | 45.1 | 249 | 40.9 | 133 | 55.2 | 249 | 72.6 |
| Missing | 6 | - | - | - | - | - | 17 | - |
COPTR, Childhood Obesity Prevention and Treatment Research; NET-Works, Now Everyone Together for Healthy and Amazing Kids; GROW, Growing Right Onto Wellness; IMPACT, Ideas Moving Parents and Adolescents to Change Together; GED, General Equivalency Diploma; SNAP, Supplemental Nutrition Assistance Program, BMI, body mass index
Child’s BMI percentile refers to age- and sex-specific BMI percentiles calculated using the Centers for Disease Control and Prevention SAS macro
Child’s %95th BMI percentile refers to the percentage of the age- and sex-specific 95th BMI percentile calculated using the Centers for Disease Control and Prevention SAS macro
Parent’s weight status classified as follows: underweight/normal weight (BMI<25 kg/m2), overweight (BMI 25-29 kg/m2), obesity (BMI≥30 kg/m2)
Table 2 provides an overview of the k-means cluster analysis results. Two dietary patterns were derived for all studies except GROW, which had three patterns. Patterns were named based on the food groups that loaded highly on each cluster and in accordance with existing knowledge of diet quality and previously derived dietary patterns(15,16). The NET-Works and GROW studies each had dietary patterns labeled “Healthy” and “Unhealthy,” reflecting the degree of adherence to US dietary guidelines. A third pattern was derived for GROW called “Dairy/Sugar-sweetened beverage (SSB),” named solely after the foods groups with the highest intake. The GOALS study also had a similar “Healthy” pattern and a pattern labeled “Semi-Traditional,” reflecting intake of some, but not all, foods/beverages typical of a Traditional Mexican diet. The two patterns for the IMPACT study were distinct from those derived in the other three COPTR studies and were labeled “Mixed,” indicating adherence to some aspects of healthy and unhealthy diets, and “Sandwich,” due to this pattern containing high intake of food groups typically found in a sandwich. The most prevalent dietary pattern was the Healthy cluster for NET-Works children (59.7%), the Dairy/SSB cluster for GROW children (51.7%), the Semi-Traditional cluster for GOALS adolescents (62.2%), and the Mixed cluster for IMPACT adolescents (51.7%). The odds of belonging to each cluster according to socio-demographic characteristics are provided in Supplementary Tables 2 and 3.
Table 2.
Overview of cluster solutions for each COPTR study
| Prevention studies,
n (%) |
Treatment studies,
n (%) |
|||
|---|---|---|---|---|
| NET-Works (N=534) | GROW (n=609) | GOALS (N=241) | IMPACT (N=360) | |
| Healthy | 319 (59.7) | 162 (26.6) | 91 (37.8) | |
| Unhealthy | 215 (40.3) | 132 (21.7) | ||
| Dairy/SSB | 315 (51.7) | |||
| Semi-Traditional | 150 (62.2) | |||
| Mixed | 186 (51.7) | |||
| Sandwich | 174 (48.3) | |||
COPTR, Childhood Obesity Prevention and Treatment Research; NET-Works, Now Everyone Together for Healthy and Amazing Kids; GROW, Growing Right Onto Wellness; IMPACT, Ideas Moving Parents and Adolescents to Change Together; SSB, sugar-sweetened beverages
Specific food groups that characterized the Healthy and Unhealthy clusters in NET-Works and GROW differed slightly between studies (Figures 1 and 2, respectively). However, the Healthy cluster was generally characterized by high consumption of fruits, vegetables, legumes, whole grains, eggs, seafood, and poultry, and the Unhealthy cluster was characterized by high consumption of fried foods, snacks, desserts, and sweetened milk. The Healthy cluster in the GOALS study (Figure 3) was similar to the Healthy clusters in NET-Works and GROW except it was largely characterized by high milk intake and did not include high vegetable or poultry intake. For the IMPACT study (Figure 4), the Mixed cluster was characterized by high intake of fruits, vegetables, whole grains, milk, and poultry but also by high intakes of desserts, fruit juice, and sweetened milk.
Figure 1.
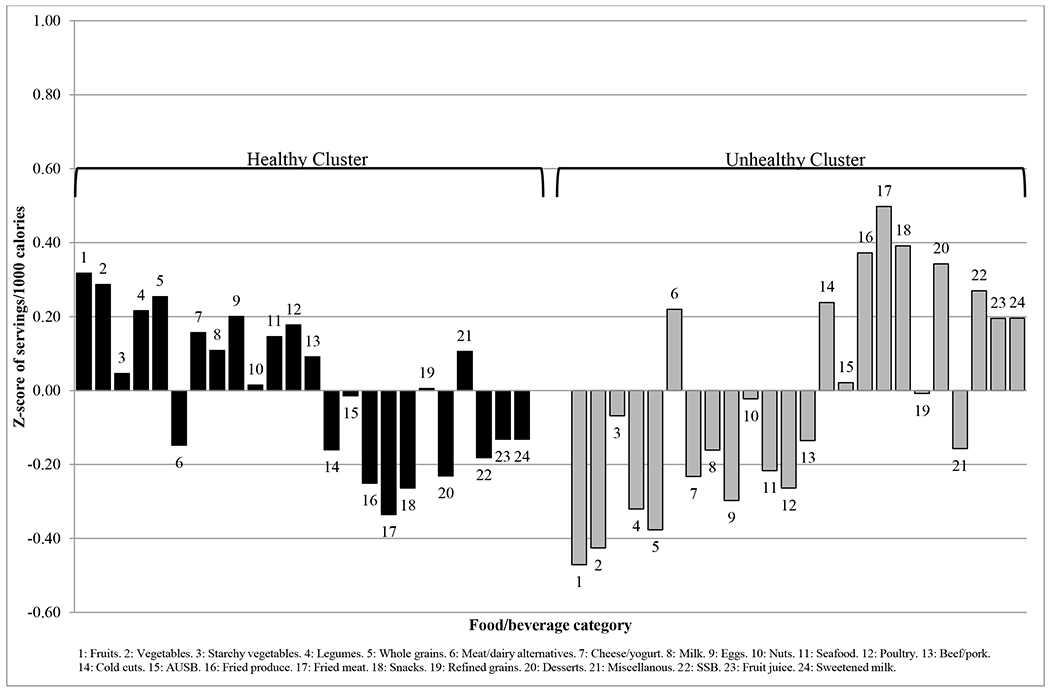
Mean z-score of each food/beverage group servings per 1000 calories for the selected k-means cluster solution for NET-Works (N=534).
AUSB, artificially and unsweetened beverages; SSB, sugar-sweetened beverages
Figure 2.
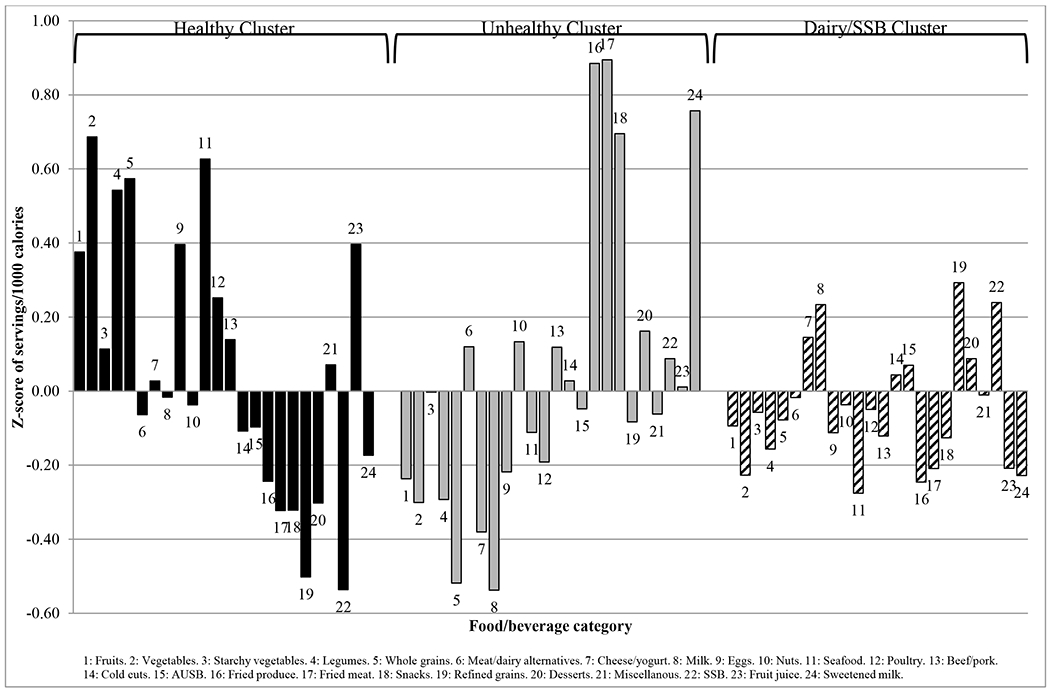
Mean z-score of each food/beverage group servings per 1000 calories for the selected k-means cluster solution for GROW (n=609).
AUSB, artificially and unsweetened beverages; SSB, sugar-sweetened beverages
Figure 3.
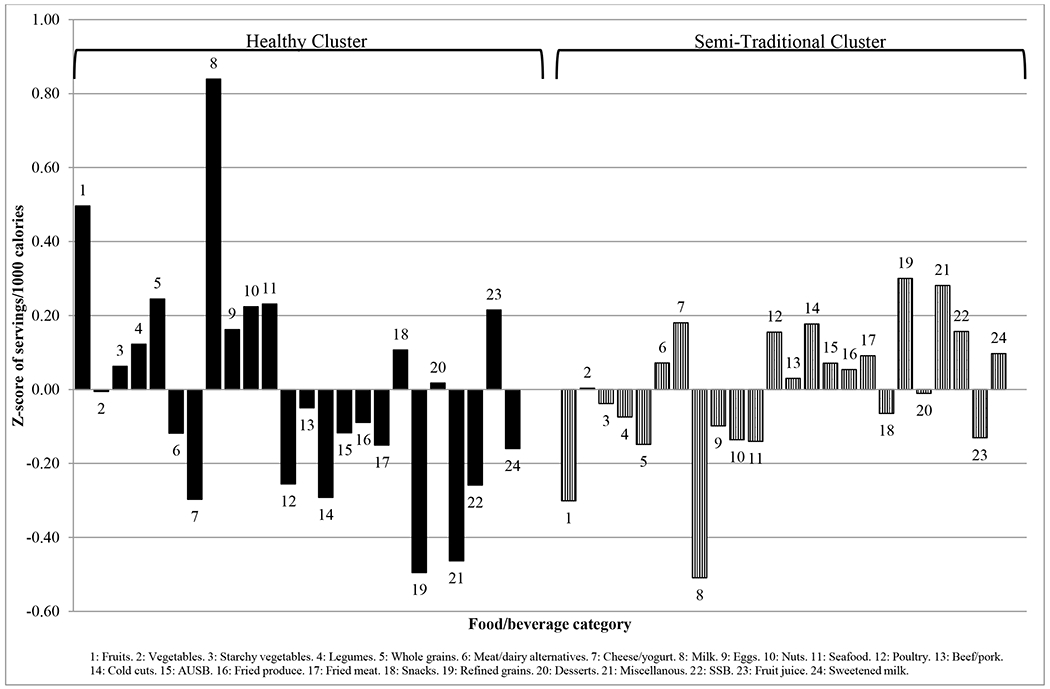
Mean z-score of each food/beverage group servings per 1000 calories for the selected k-means cluster solution for GOALS (N=241).
AUSB, artificially and unsweetened beverages; SSB, sugar-sweetened beverages
Figure 4.
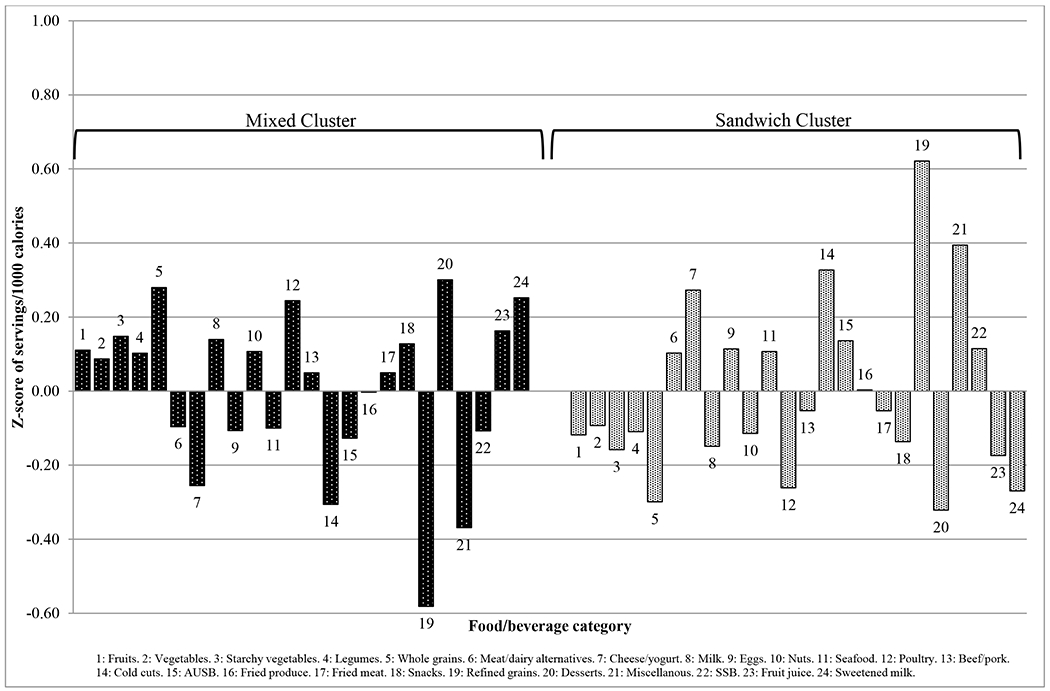
Mean z-score of each food/beverage group servings per 1000 calories for the selected k-means cluster solution for IMPACT (N=360).
AUSB, artificially and unsweetened beverages; SSB, sugar-sweetened beverages
Foods that characterized the remaining clusters differed across studies. The Dairy/SSB cluster in the GROW study was typified by high intake of refined grains, milk, cheese/yogurt, and SSBs. The Semi-Traditional cluster in GOALS was defined by high intake of refined grains, poultry, cold cuts, cheese/yogurt, miscellaneous, and SSBs. Lastly, the Sandwich pattern in IMPACT was characterized by high intake of refined grains, cold cuts, miscellaneous, and cheese/yogurt.
Table 3 shows the association between cluster membership and BMI and percentage of the 95th BMI percentile. All associations were null with the exception of the IMPACT study. For the IMPACT study, belonging to the Sandwich compared to Mixed cluster was associated with a 0.99 kg/m2 (95% CI: 0.01, 1.97) higher BMI and being 4.17 (95% CI: 0.11, 8.24) percentage points greater than the average percentage of the 95th BMI percentile.
Table 3.
Associations between cluster membership and BMI and percentage of the 95th BMI percentile for each COPTR study†
| Prevention studies, β
(95% CI) |
Treatment studies, β
(95% CI) |
|||
|---|---|---|---|---|
| NET-Works (n=527) | GROW (n=604) | GOALS (n=240) | IMPACT (n=341) | |
| BMI | ||||
| Healthy | Ref. | Ref. | Ref. | - |
| Unhealthy | −0.24 (−0.55, 0.07) | −0.11 (−0.29, 0.06) | - | - |
| Dairy/SSB | - | −0.01 (−0.15, 0.14) | - | - |
| Semi-Traditional | - | - | −0.37 (−1.34, 0.61) | - |
| Mixed | - | - | - | Ref. |
| Sandwich | - | - | - | 0.99 (0.01, 1.97)* |
| %95th BMI percentile‡ | ||||
| Healthy | Ref. | Ref. | Ref. | - |
| Unhealthy | −1.39 (−3.11, 0.33) | −0.64 (−1.62, 0.34) | - | - |
| Dairy/SSB | - | −0.08 (−0.89, 0.73) | - | - |
| Semi-Traditional | - | - | −1.57 (−6.01, 2.87) | - |
| Mixed | - | - | - | Ref. |
| Sandwich | - | - | - | 4.17 (0.11, 8.24)* |
CI, confidence interval
Models adjusted for child’s age, child’s sex, highest household education, primary parent/guardian employment, SNAP participation, primary parent /guardian marital status, and primary parent/guardian weight status
%95th BMI percentile refers to the percentage of the child’s age- and sex-specific 95th BMI percentile calculated using the Centers for Disease Control and Prevention SAS macro
p<0.05
DISCUSSION
This is one of the few studies to examine dietary patterns in low-income, racial/ethnic minority children and adolescents in the US and the first US study (that we are aware of) to derive dietary patterns in samples of predominantly Hispanic youth. Additionally, this study is the first to our knowledge to examine associations between data-driven dietary patterns and BMI in young US children. Consistent with our hypothesis, 2-3 dietary patterns described overall dietary intake for each COPTR study. Healthy and Unhealthy patterns were found in both the NET-Works and GROW studies, and a similar Healthy pattern was observed in the GOALS study. A Semi-Traditional pattern was only identified for the GOALS study. Across studies, associations with BMI were largely null, but having a Sandwich compared to a Mixed dietary pattern in the IMPACT study was associated with a greater BMI and percentage of the 95th BMI percentile.
Identification of Healthy and Unhealthy patterns across the two COPTR studies of young children is consistent with a recent review of 17 studies that identified these two patterns as the most common dietary patterns in young children (aged 1 to 5 years) in developed countries(15). Similar to COPTR, the specific foods that characterized these patterns varied across studies, but Healthy patterns were generally characterized by high intake of fruits, vegetables, and whole grains, and Unhealthy patterns were typified by high intake of SSBs, chips, and sweets(15). The findings for the NET-Works and GROW studies are also similar to those of the three previous studies that derived dietary patterns using cluster analysis in US youth(18–20). Specifically, two of the aforementioned studies identified a Healthy pattern(19,20) and one study additionally reported an Unhealthy pattern(20).
It should also be noted that a third pattern was derived for the GROW study that was labeled the Dairy/SSB pattern, and the majority of children in GROW (51.7%) belonged to this cluster. While this finding was unexpected, a similar pattern has been derived for 4- to 8-year-old low-income children in the US called “Big Eaters – Dairy and non-whole grains style”(18). The Big Eaters – Dairy and non-whole grains style was also relatively common among youth (second most prevalent pattern) and was characterized by high caloric intake, specifically high intake of refined grains, milk, cheese, and added sugars(18). However, researchers should interpret this Dairy/SSB pattern with caution given 1) it was unique to the GROW study and 2) there was substantial overlap of the Dairy/SSB cluster with both the Healthy and Unhealthy cluster in exploratory analyses using principal components analysis (data not shown).
It was hypothesized that Healthy and Unhealthy patterns would also be observed in the GOALS and IMPACT studies, given they are the most commonly derived patterns among adolescents(16). However, a Healthy pattern was only observed for the GOALS study. While the Mixed pattern in IMPACT encompassed some components of healthy intake, such as whole grains and poultry, the lack of a Healthy pattern for the IMPACT study is consistent with the one previous examination of dietary patterns in US Black adolescents(19).
A second dietary pattern was identified in the GOALS and IMPACT studies that was unique to each study. In the GOALS study, the second dietary pattern identified was the Semi-Traditional pattern, and the majority of youth belonged to this cluster (62.2%). While similar to the Unhealthy patterns from NET-Works and GROW (in that the Semi-Traditional pattern was also typified by low intake of fruits, milk, and lean proteins), it was considered a distinct pattern because it was not characterized by high intake of fried foods, snacks, or desserts. Nearly 98% of the GOALS study was Hispanic, of which 85% were Mexican American or Chicano/a (the remaining 15% were of “other Hispanic, Latino/a, or Spanish ethnicity”). Thus, it is plausible that this dietary pattern represents dietary intake characteristic of Mexican culture.
It is important to note that, while the majority of Hispanics in GOALS were of Mexican descent, the definition of a “traditional” dietary pattern varies across Hispanic/Latino backgrounds as a result of cultural heritage and country of origin(38). Traditional diets in Mexican American adults have been described as high in intake of refined grains (in the form of tortillas)(24,38,39), meat(38,40), legumes(24,39,40), tomatoes(24,38–40), cheese(40), and sweetened drinks(24,38). However, the GOALS pattern was not characterized by high intake of tomatoes and legumes, and thus this dietary pattern is labeled only as Semi-Traditional. Dietary acculturation may provide a potential explanation for the lack of a true Traditional Mexican dietary pattern, particularly with respect to the low intake of tomatoes and other produce. Notably, Mexican American individuals have been shown to consume fewer fruits and vegetables and more fast food with greater acculturation (41–43). It is also possible that the Semi-Traditional dietary pattern is not a true Traditional Mexican dietary pattern due to the presence of multiple Hispanic/Latino backgrounds in our sample.
The second pattern identified in the IMPACT study was the Sandwich pattern. The observation that both dietary patterns for IMPACT were distinct from those derived in other COPTR studies is similar to previous research in COPTR which identified distinct snack-occasion-specific dietary patterns for IMPACT compared to the other COPTR studies(44). Interestingly, the Sandwich pattern in IMPACT was similar to another pattern called “Packed Lunch” that was previously observed at 7, 10, and 13 years of age in the Avon Longitudinal Study of Parents and Children (ALSPAC) in England(45). Specifically, the Packed Lunch pattern was characterized by high consumption of white bread, ham and bacon, miscellaneous items (i.e., margarine, sweet spreads, salty flavorings), crisps (chips), biscuits (cookies), and artificially and unsweetened beverages (i.e., diet squash [fruit-flavored beverage], tea, and coffee)(45).
Contrary to our hypotheses, associations between dietary patterns and BMI or percentage of the 95th BMI percentile were null with the exception that the Sandwich compared to the Mixed dietary pattern was associated with a higher BMI and percentage of the 95th BMI percentile. This finding for the IMPACT study is similar to findings for the Packed Lunch pattern in ALSPAC(46). Specifically, compared to a Healthy dietary pattern, a Packed Lunch pattern at 7 years of age was associated with a significantly greater odds of being in the top 10% for BMI at 7 years of age. However, significant cross-sectional associations were not observed between the Packed Lunch pattern and BMI at age 10 or 13 years(46).
A potential explanation for the null associations of dietary patterns with BMI and percentage of the 95th BMI percentile in this study is the cross-sectional design of the analysis. For example, individuals with a Healthy dietary pattern could have 1) adopted or reported a healthy diet as a result of having a higher BMI and a desire to lose weight or 2) followed a healthy diet to maintain their already normal BMI. This combination of individuals within one group may have prevented the detection of a significant association. Of course, it is possible that our derived dietary patterns were not associated with BMI and that other factors were more strongly associated with adiposity in these youth.
Strengths and Limitations
The present analysis has several strengths, including the use of data-driven methodology to derive clusters. This methodology allows for the detection of dietary patterns unique to each population and does not rely on previously validated scores or indices(14). This type of approach is especially useful in populations like the COPTR cohorts in which the distributions of a priori scores like HEI-2010 are narrow(6). Another strength is the diversity in age and in race/ethnicity in the COPTR populations with multiple 24-hour recalls collected per child.
This study is limited by the self-reported dietary data. While repeated 24-hour recalls were used to obtain valid reports of dietary intake, it remains a challenge to collect dietary data that is valid and precise, particularly in children(47). Additionally, although comparisons were made between healthier and unhealthier dietary patterns, the patterns labeled Healthy did not meet all required dietary standards. For example, vegetable intake in the GOALS Healthy pattern was low, while the two Healthy patterns derived from the obesity prevention studies were low in milk intake. The lack of a Healthy diet pattern that meets the dietary recommendations for youth reflects a limitation of data-derived dietary patterns, in that the defined patterns are not reflective of evidence-based dietary quality.
We must also note that while there was consistency in dietary patterns across COPTR studies, dietary patterns derived using cluster analysis are, by design, sample-specific(12). Thus, these patterns may not be applicable to other populations. Further, while the use of cluster analysis to examine dietary patterns is commonplace in nutritional epidemiology(48–50), this approach does not allow investigators to delineate dissimilarities in dietary intake among individuals within a given group(13). Additional limitations of this study include that unmeasured variables may explain differences in clusters despite our attempt to adjust for plausible determinants of cluster membership. Further, while this is one of the first studies to examine dietary patterns in minority race/ethnic groups, sample size within each COPTR study prevented the examination of dietary patterns specific to each race or Hispanic ethnic group.
Implications
Several potential intervention targets emerged from our analysis. Based on the association of the Sandwich compared to the Mixed dietary pattern with a higher BMI in the IMPACT study, potential intervention targets could be substitution of refined grains for whole grains and of cold cuts and cheese for poultry (given that poultry was the main source of protein in the Mixed dietary pattern). Despite null associations with BMI in the other COPTR studies, other potential intervention targets can be suggested based on how intakes of types of foods grouped together within each study’s patterns. For example, the Unhealthy dietary patterns were defined by high intake of fried foods as well as low intake of fruits and vegetables. The way these foods group together suggests that programs and policies that promote fruit and vegetable intake, for example, may be associated with decreased fried food consumption, which would make the diets of children in the Unhealthy cluster more similar to diets of children in the Healthy cluster. Similarly, patterns defined by high intake of sweetened beverages (i.e., Unhealthy, Semi-Traditional, and Sandwich patterns) were also defined by low intake of milk. Making milk, or plain water (which was not used to derive dietary patterns), the default choice for children may also help improve overall diet quality.
CONCLUSIONS
The specific foods that defined the dietary patterns varied across studies, and some dietary patterns were specific to each COPTR study. Dietary intakes of low-income, racial/ethnic minority preschool children largely cluster into Healthy and Unhealthy dietary patterns, while older age groups had dietary patterns consistent with other reports of food intake in the literature. This suggests that dietary patterns in youth may differ according to age, race/ethnicity, or geographic location. No dietary patterns were associated with BMI except for the Sandwich pattern in the IMPACT study. Findings from the four COPTR studies suggest that all dietary patterns of low-income, racial/ethnic minority children can be improved in terms of diet quality, and that public health messages focused on healthy substitutions, such as replacing refined grains with whole grains or cold cuts with poultry, may help youth mimic a dietary pattern associated with lower BMI.
Supplementary Material
Acknowledgements:
Financial support: This research was supported by grants U01 HL103561, U01 HL103620, U01 HL103622, U01 HL103629, U01 HD068890, UL 1RR024989, and NIH DK56350 from the National Heart, Lung, and Blood Institute and the Eunice Kennedy Shriver National Institute of Child Health and Development and the Office of Behavioral and Social Sciences Research. The content expressed in this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, And Blood Institute, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institutes of Health, or the U.S. Department of Health and Human Services. The National Heart, Lung, And Blood Institute, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institutes of Health, and the U.S. Department of Health and Human Services had no role in the design, analysis, or writing of this article. Support for MNL was provided by a National Heart, Lung, and Blood Institute training grant (T32 HL144456).
Footnotes
Conflict of interest: None.
References
- 1.Hales CM, Carroll MD, Fryar CD, et al. (2017) Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS Data Brief, no 288. Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- 2.Kumar S, Kelly AS (2017) Review of Childhood Obesity: From Epidemiology, Etiology, and Comorbidities to Clinical Assessment and Treatment. Mayo Clin Proc 92, 251–65. [DOI] [PubMed] [Google Scholar]
- 3.Ambrosini GL (2014) Childhood dietary patterns and later obesity: a review of the evidence. Proc Nutr Soc 73, 137–46. [DOI] [PubMed] [Google Scholar]
- 4.Ocké MC (2013) Evaluation of methodologies for assessing the overall diet: dietary quality scores and dietary pattern analysis. Proc Nutr Soc 72, 191–9. [DOI] [PubMed] [Google Scholar]
- 5.Schulze MB, Hoffmann K (2006) Methodological approaches to study dietary patterns in relation to risk of coronary heart disease and stroke. Br J Nutr 9, 860–9. [DOI] [PubMed] [Google Scholar]
- 6.Truesdale KP, Matheson DM, JaKa MM, et al. (2019) Baseline diet quality of predominantly minority children and adolescents from households characterized by low socioeconomic status in the Childhood Obesity Prevention and Treatment Research (COPTR) Consortium. BMC Nutr 5, 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Golpour-Hamedani S, Mohammadifard N, Khosravi A, et al. (2017) Dietary approaches to stop hypertension diet and obesity: A cross-sectional study of Iranian children and adolescents. ARYA Atheroscler 13, 7–13. [PMC free article] [PubMed] [Google Scholar]
- 8.Labayen Goñi I, Arenaza L, Medrano M, et al. (2018) Associations between the adherence to the Mediterranean diet and cardiorespiratory fitness with total and central obesity in preschool children: the PREFIT project. Eur J Nutr 57, 2975–83. [DOI] [PubMed] [Google Scholar]
- 9.Iaccarino Idelson P, Scalfi L, Valerio G (2017) Adherence to the Mediterranean Diet in children and adolescents: A systematic review. Nutr Metab Cardiovasc Dis 27, 283–99. [DOI] [PubMed] [Google Scholar]
- 10.Pratt CA, Boyington J, Esposito L, et al. (2013) Childhood Obesity Prevention and Treatment Research (COPTR): interventions addressing multiple influences in childhood and adolescent obesity. Contemp Clin Trials 36, 406–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caliński T, Harabasz J (1974) A dendrite method for cluster analysis. Commun Stat 3:1–27. [Google Scholar]
- 12.Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology (2002). Curr Opin Lipidol 13, 3–9. [DOI] [PubMed] [Google Scholar]
- 13.Reedy J, Wirfàlt E, Flood A, et al. Comparing 3 Dietary Pattern Methods—Cluster Analysis, Factor Analysis, and Index Analysis—With Colorectal Cancer Risk (2010). Am J Epidemiol 171, 479–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miller PE, Lazarus P, Lesko SM, et al. (2010) Diet index-based and empirically derived dietary patterns are associated with colorectal cancer risk. J Nutr 140, 1267–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smithers LG, Golley RK, Brazionis L, et al. (2011) Characterizing whole diets of young children from developed countries and the association between diet and health: a systematic review. Nutr Rev 69, 449–67. [DOI] [PubMed] [Google Scholar]
- 16.Hinnig P de F, Monteiro JS, de Assis MAA, et al. (2018) Dietary Patterns of Children and Adolescents from High, Medium and Low Human Development Countries and Associated Socioeconomic Factors: A Systematic Review. Nutrients 10, 436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith AD a. C, Emmett PM, Newby PK, et al. (2011) A comparison of dietary patterns derived by cluster and principal components analysis in a UK cohort of children. Eur J Clin Nutr 65, 1102–9. [DOI] [PubMed] [Google Scholar]
- 18.Knol LL, Haughton B, Fitzhugh EC (2005) Dietary patterns of young, low-income US children. J Am Diet Assoc 105, 1765–73. [DOI] [PubMed] [Google Scholar]
- 19.Ritchie LD, Spector P, Stevens MJ, et al. (2007) Dietary patterns in adolescence are related to adiposity in young adulthood in black and white females. J Nutr 137, 399–406. [DOI] [PubMed] [Google Scholar]
- 20.Hidaka BH, Kerling EH, Thodosoff JM, et al. (2016) Dietary patterns of early childhood and maternal socioeconomic status in a unique prospective sample from a randomized controlled trial of Prenatal DHA Supplementation. BMC Pediatr 16, 191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ford CN, Slining MM, Popkin BM (2013) Trends in dietary intake among US 2- to 6-year-old children, 1989-2008. J Acad Nutr Diet 113, 35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin H, Bermudez OI, Tucker KL (2003) Dietary patterns of Hispanic elders are associated with acculturation and obesity. J Nutr 133, 3651–7. [DOI] [PubMed] [Google Scholar]
- 23.Valerino-Perea S, Lara-Castor L, Armstrong MEG, Papadaki A. (2019) Definition of the traditional Mexican diet and its role in health: A systematic review. Nutrients 11, E2803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carrera PM, Gao X, Tucker KL. (2007) A study of dietary patterns in the Mexican-American population and their association with obesity. J Am Diet Assoc 107, 1735–42. [DOI] [PubMed] [Google Scholar]
- 25.Flores M, Macias N, Rivera M, Lozada A, Barquera S, Rivera-Dommarco J, et al. (2010) Dietary patterns in Mexican adults are associated with risk of being overweight or obese. J Nutr 140, 1869–73. [DOI] [PubMed] [Google Scholar]
- 26.Sherwood NE, French SA, Veblen-Mortenson S, et al. (2013) NET-Works: Linking families, communities and primary care to prevent obesity in preschool-age children. Contemp Clin Trials 36, 544–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Po’e EK, Heerman WJ, Mistry RS, et al. (2013) Growing Right Onto Wellness (GROW): a family-centered, community-based obesity prevention randomized controlled trial for preschool child-parent pairs. Contemp Clin Trials 36, 436–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robinson TN, Matheson D, Desai M, et al. (2013) Family, community and clinic collaboration to treat overweight and obese children: Stanford GOALS-A randomized controlled trial of a three-year, multi-component, multi-level, multi-setting intervention. Contemp Clin Trials 36, 421–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moore SM, Borawski EA, Cuttler L, et al. (2013) IMPACT: a multi-level family and school intervention targeting obesity in urban youth. Contemp Clin Trials 36, 574–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schakel SF, Sievert YA, Buzzard IM (1988) Sources of data for developing and maintaining a nutrient database. J Am Diet Assoc 88, 1268–71. [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention, US Department of Health & Human Services (2019) A SAS program for the CDC growth charts. http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm (accessed Aug 2019).
- 32.Kuczmarski R, Ogden C, Guo S, et al. (2002) 2000 CDC Growth Charts for the United States: Methods and development. National Center for Health Statistics. Vital Health Stat 11, 246:1–190. [PubMed] [Google Scholar]
- 33.Flegal KM, Wei R, Ogden CL, et al. (2009) Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr 90, 1314–20. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention (2017) Defining Adult Overweight and Obesity. https://www.cdc.gov/obesity/adult/defining.html (accessed Aug 2019).
- 35.Austin GL, Adair LS, Galanko JA, et al. (2007) A diet high in fruits and low in meats reduces the risk of colorectal adenomas. J Nutr 137, 999–1004. [DOI] [PubMed] [Google Scholar]
- 36.Everitt BS, Landau S, Leese M, et al. (2011) Cluster Analysis (Wiley Series in Probability and Statistics), 5th ed. London: John Wiley & Sons, Ltd. [Google Scholar]
- 37.Milligan GW, Cooper MC (1985) An examination of procedures for determining the number of clusters in a data set. Psychometrika 50, 159–79. [Google Scholar]
- 38.Siega-Riz AM, Sotres-Alvarez D, Ayala GX, et al. (2014) Food-group and nutrient-density intakes by Hispanic and Latino backgrounds in the Hispanic Community Health Study/Study of Latinos. Am J Clin Nutr 99, 1487–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sofianou A, Fung TT, Tucker KL (2011) Differences in diet pattern adherence by nativity and duration of US residence in the Mexican-American population. J Am Diet Assoc 111, 1563–1569.e2. [DOI] [PubMed] [Google Scholar]
- 40.Murtaugh MA, Sweeney C, Giuliano AR, et al. (2008) Diet patterns and breast cancer risk in Hispanic and non-Hispanic white women: the Four-Corners Breast Cancer Study. Am J Clin Nutr 87, 978–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ayala GX, Baquero B, Klinger S. (2008) A systematic review of the relationship between acculturation and diet among Latinos in the United States: implications for future research. J Am Diet Assoc 108, 1330–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Unger JB, Reynolds K, Shakib S, Spruijt-Metz D, Sun P, Johnson CA. (2004) Acculturation, physical activity, and fast-food consumption among Asian-American and Hispanic adolescents. J Community Health 29, 467–81. [DOI] [PubMed] [Google Scholar]
- 43.Liu J-H, Chu YH, Frongillo EA, Probst JC. (2012) Generation and acculturation status are associated with dietary intake and body weight in Mexican American adolescents. J Nutr 142, 298–305. [DOI] [PubMed] [Google Scholar]
- 44.LeCroy MN, Truesdale KP, Matheson DM, et al. (2019) Snacking characteristics and patterns and their associations with diet quality and body mass index in the Childhood Obesity Prevention and Treatment Research Consortium. Public Health Nutr 22, 3189–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Northstone K, Smith ADAC, Newby PK, et al. (2013) Longitudinal comparisons of dietary patterns derived by cluster analysis in 7- to 13-year-old children. Br J Nutr 109, 2050–8. [DOI] [PubMed] [Google Scholar]
- 46.Bull CJ, Northstone K (2016) Childhood dietary patterns and cardiovascular risk factors in adolescence: results from the Avon Longitudinal Study of Parents and Children (ALSPAC) cohort. Public Health Nutr 19, 3369–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Burrows T, Golley RK, Khambalia A, et al. (2012) The quality of dietary intake methodology and reporting in child and adolescent obesity intervention trials: a systematic review. Obes Rev 13, 1125–38. [DOI] [PubMed] [Google Scholar]
- 48.Togo P, Osler M, Sørensen TI, Heitmann BL. Food intake patterns and body mass index in observational studies (2001). Int J Obes Relat Metab Disord 25, 1741–51. [DOI] [PubMed] [Google Scholar]
- 49.Newby PK, Tucker KL. Empirically derived eating patterns using factor or cluster analysis: a review (2004). Nutr Rev 62, 177–203. [DOI] [PubMed] [Google Scholar]
- 50.Evidence Analysis Library Division, Center for Nutrition Policy and Promotion, US Department of Agriculture (2014) A Series of Systematic Reviews on the Relationship Between Dietary Patterns and Health Outcomes. https://nesr.usda.gov/dietary-patterns-systematic-reviews-project-0
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


