Abstract
The current study investigated the feasibility of telehealth-delivered diabetes self-management education and support (DSMES) for older adults with type 2 diabetes mellitus following hospital discharge. The intervention included one in-person home visit and follow-up weekly virtual DSMES for 4 additional weeks. Diabetes knowledge was measured at baseline and completion of the program. The Telehealth Usability Questionnaire was completed following the final session. Hemoglobin A1C (A1C) level was abstracted from the electronic health record at baseline and 3 months post hospital discharge. Hospital readmissions were measured at 30 days post index hospital stay. Of the 20 patients enrolled, 12 completed the intervention. The most common reason for attrition was discharge to a skilled nursing facility (3/20). Participants who completed the intervention increased their diabetes knowledge scores. A1C values decreased by 1.1%, and there were no hospital readmissions for any patient who completed the program. Participants described the program as useful and were satisfied with the program. These results suggest that it is feasible to identify and enroll patients in a telehealth education program for diabetes during hospital admission.
Patients with diabetes require daily self-care tasks to assist in achieving target blood glucose levels to prevent potential diabetes-related complications. Diabetes self-management education and support (DSMES) helps prevent or delay diabetes-related complications by focusing specifically on increasing knowledge and self-efficacy so individuals can complete recommended diabetes self-care tasks. Formal DSMES reduces overall health care costs for patients with diabetes (Boren, Fitzner, Panhalkar, & Specker, 2009) and improves glycemic control (Chrvala, Sherr, & Lipman, 2016).
Despite evidence showing the benefits of DSMES, to date, it has been severely underused. Estimates of attendance at DSMES training range from 1% to 6.8% (Strawbridge, Lloyd, Meadow, Riley, & Howell, 2015). Given the literature supporting the effectiveness of DSMES, Healthy People 2020 has made increasing the attendance of DSMES a priority (Office of Disease Prevention and Health Promotion, 2012). Interventions to achieve this goal are greatly needed. In 2018, there were only 19,584 certified diabetes educators (CDEs) (National Certification Board for Diabetes Educators [NCBDE], 2018). People with diabetes grossly exceed the capacity of CDEs to deliver education using traditional in-person methods. Therefore, a significant gap exists among the recommended guidelines, current practice, and what is even feasible.
Traditionally, DSMES is provided face-to-face in individual or group settings. Currently, Medicare covers an initial 1 hour of individual DSMES and 9 hours of group training unless there is a documented special need (Centers for Medicare & Medicaid Services [CMS], 2019). Older adults who are confined to their homes for any number of reasons, including lack of transportation, functional limitations, or medical conditions, are frequently unable to attend classes in an outpatient setting. These chronic comorbid conditions and lack of access to DSMES place older adults with diabetes at further risk for poor outcomes. Homebound older adults require alternative methods of DSMES delivery. Providing services that are accessible, convenient, and that can easily fit into patients’ schedules may improve DSMES engagement.
The American Telemedicine Association (2019) defines telehealth as “technology-enabled health and care management and delivery systems that extend capacity and access” (para. 16). The provision of DSMES via telehealth technology (i.e., the use of telecommunication to deliver education via the internet) has the potential to provide individuals with the accessibility and convenience. A recent review of the literature indicates that telehealth technologies have shown effectiveness for self-care skills, improvements in self-monitoring behaviors, and improvements in clinical outcomes among older adults with chronic conditions (Guo & Albright, 2018).
In the Balanced Budget Act of 1997, Congress mandated that the Health Care Financing Administration conduct a demonstration project using telemedicine to improve care for Medicare beneficiaries with diabetes who live in federally designated, medically underserved areas in New York City or upstate New York. This demonstration project, Informatics for Diabetes Education and Telemedicine (IDEATel), provided home diabetes education and medical monitoring. This project included a trial of 1,665 beneficiaries randomized to either receiving nurse case manager telemedicine care every 4 to 6 weeks for 2 years or usual care. At 5 years, compared to the usual care group, those who received telemedicine case management had greater improvements in hemoglobin A1C (A1C) level, low-density lipoprotein cholesterol level, and blood pressure (Shea et al., 2006).
Hospitalization can provide an opportunity to assess current diabetes knowledge and engage individuals in necessary education. Teachable moments have been proposed as specific events or contexts that can lead individuals to positive behavior change (Lawson & Flocke, 2009). Prior research has used a hospitalization or emergency department visit as a teachable moment (Esler & Bock, 2004; Fonarow, 2003; Graham et al., 2016). In addition, transitions in care have been designated by the American Diabetes Association as a critical time to assess, provide, and adjust DSMES to people with diabetes (Powers et al., 2016). Using a teachable moment as a framework, the current authors identified hospitalization as a time point to directly engage patients and telemedicine as an optimal delivery system for these generally older, sicker patients.
In the current pilot study, the feasibility of DSMES through telehealth to vulnerable older adult patients with type 2 diabetes mellitus (T2DM) following a hospital admission was evaluated. Specifically, the authors sought to answer the following: (a) Can patients with T2DM be recruited during a hospital stay to a home-based telemedicine DSMES program? (b) Can a telemedicine DSMES program be successfully delivered to recently hospitalized patients with T2DM? (c) Can telehealth-delivered DSMES improve diabetes knowledge for older adults with T2DM? (d) What is the level of satisfaction and acceptability of telehealth-delivered DSMES among older adults with T2DM following a hospital admission?
METHOD
Design
A pre/post quasi-experimental study was conducted between September 2017 and March 2018. This study was approved by the University of Pennsylvania Institutional Review Board (IRB). The IRB deemed all procedures compliant with Health Insurance Portability and Accountability Act (HIPAA) guidelines.
Participants and Setting
Hospitalized older adults age ≥55 with T2DM were recruited. Eligibility criteria included admission to a medical or surgical unit for any reason, English speaking, cognitively intact, and living within a 30-mile radius of the study site (a large academic medical center within the University of Pennsylvania Health System). An advanced practice nurse/certified diabetes educator (APN/CDE; C.R.W.) conducted screening and recruitment. Patients with cognitive impairment noted during the chart review were excluded. The APN/CDE approached potential participants during their hospital admission to assess their willingness to participate in the study and obtain written consent.
Procedure
An APN/CDE provided one in-person home visit within 24 to 48 hours of hospital discharge and weekly virtual synchronous one-on-one DSMES sessions via electronic tablet supplied by the study for 4 additional weeks (Figure 1). During the initial home visit, the APN/CDE reviewed the hospital discharge instructions with the patient, completed a medication reconciliation, and provided an approved diabetes education booklet that covered “survival skills” for diabetes self-management. Electronic tablets with internet access were also provided to participants during the first home visit. Internet access was provided via cellular service. Expecting variation in levels of health and computer literacy, and using considerations outlined by prior research (Demiris, Finkelstein, & Speedie, 2001), a user interface was developed that required minimal steps and used simple plain language and large icons to connect patients to the DSMES session. Printed handouts provided step-by-step instructions with images showing where to turn on the tablet, adjust volume, how to access the appropriate icon that initiated the session, and how to conclude the session. The education was provided by an APN/CDE or a RN/CDE. The APN/CDE had 10+ years of experience providing homecare and transitional care to older adults with chronic conditions and had 5+ years as a diabetes educator. The RN/CDE (L.M.M.) had 5+ years of experience as a diabetes educator.
Figure 1.
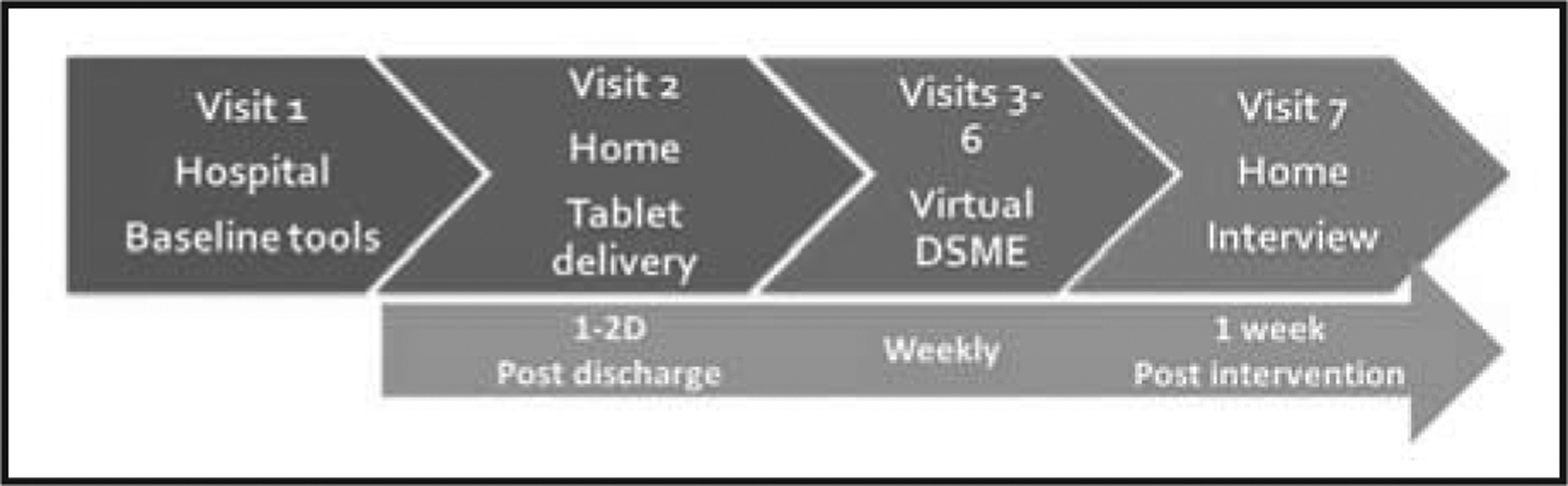
Timing of visits/assessments.
Note. DSME = diabetes self-management education.
Participants completed weekly private 30- to 60-minute virtual synchronous education sessions for a total of 4 weeks. The telehealth delivery method used Vidyo® software for synchronous videoconferencing. The software, with a screen share feature, connects participants to the CDE for a face-to-face audio/visual conference. Vidyo is HIPAA compliant.
The APN/CDE set education goals together with each patient prior to starting the online sessions. DSMES includes the American Association of Diabetes Educators 7 (AADE7®) self-care behaviors, which include healthy eating, being active, glucose monitoring, taking medication, problem solving, healthy coping, and reducing risks (AADE, 2019). Education was patient-centered and covered topics including self-management training, survival skills, general overview of pathophysiology, nutrition concepts, nutrition strategies for eating out, portion control, being active, taking medication, monitoring glucose, problem solving, healthy coping, and risk reduction for cardiovascular, renal, eye, and dental health. The APN/CDE conducted a final face-to-face home visit 1 week following the final telehealth education session to collect electronic tablets and complete questionnaires. Participants continued their usual health care throughout the study, as the telehealth visits did not replace usual care provided by medical providers.
Data Collection
Data were collected in-person at enrollment and upon completion of the program and from review of the electronic health record (EHR). The main outcomes were feasibility of the study procedures and data collection methods. Data were also collected on diabetes knowledge, A1C level, 30-day readmissions, and telehealth usability.
Sample demographic data included age, sex, race, marital status, number of comorbid conditions, education completed, and employment status. Diabetes history assessment included information regarding onset of diabetes, diabetes medications, prior DSMES, and prior hospitalizations in the past 6 months. Participants were also asked about the types of technology they have and/or use.
Primary Outcomes
Study feasibility was defined as: (a) the proportion of patients approached and enrolled versus declined, with the goal of a 75% recruitment rate; (b) the proportion of patients who completed 4 weeks of the DSMES intervention, with a goal of 80% retention; (c) the numbers and types of technical difficulties encountered; and (d) the ability to complete the study instruments and obtain A1C values pre- and postintervention, with a goal of 100%.
Secondary Outcomes
Change in diabetes knowledge was measured using the Diabetes Knowledge Test Version 2 (DKT2; Fitzgerald et al., 2016) to determine if the delivery of content had any effect on the goal of improving diabetes knowledge. The DKT2 comprises 23 multiple choice items; 14 items focus on general diabetes knowledge and nine items are insulin related (Fitzgerald et al., 2016). The DKT2 demonstrates reliability and validity (Fitzgerald et al., 2016). The DKT2 was administered at baseline and the final exit interview.
Change in A1C level was determined from the EHR. The baseline A1C level closest to the hospital admission within the past 6 months was abstracted. Follow-up A1C level was either self-reported or retrieved from the EHR within 3 months after discharge from the intervention. Rehospitalizations were defined as a hospital admission for any reason within 30 days of the index hospital discharge. This variable was collected via self-report and/or the EHR.
Usability of the telehealth intervention was assessed with the Technology Usability Questionnaire (TUQ) and administered during the exit interview. The TUQ is a 21-item questionnaire that uses a 7-point Likert scale from 1 = strongly disagree to 7 = strongly agree (Parmanto, Lewis, Graham, & Bertolet, 2016). The TUQ provides subscale scores for assessing usefulness, ease of use, interface and interaction quality, reliability, satisfaction, and future use. The TUQ has established reliability and validity (Parmanto et al., 2016).
Data Analysis
Means and standard deviations were calculated for continuous variables and rates were calculated for dichotomous and ordinal variables. Changes in diabetes knowledge (DKT2) and A1C level were analyzed using a one sample, paired t test. Due to the small sample size, data were reanalyzed using nonparametric Wilcoxon signed-rank test. Intention-to-treat was used for all analyses. All statistical analyses were calculated using SPSS 23. An alpha level of 0.05 was used for all tests of statistical significance.
RESULTS
Table 1 displays the sample demographics. A total of 20 patients were enrolled. Participants who enrolled in the intervention were primarily Black (n = 15; 75%) and female (n = 11; 55%). Age ranged from 55 to 83 years with an average age of 66.5 years. There was an average of five comorbid conditions. Seven (23.3%) participants attended some college and 15 (75%) were retired on disability. Forty percent (n = 8) attended prior DSMES; however, only one half indicated they completed a prior DSMES program. Seventeen (85%) participants were prescribed insulin.
TABLE 1.
Participant Characteristics (N = 20)
| Characteristic | Value |
|---|---|
| Age (years) (mean, SD, range) | 66.5 (8.62) (55 to 83) |
| Female (n, %) | 11 (55) |
| Race (n, %) | |
| Black | 15 (75) |
| White | 4 (20) |
| Asian | 1 (5) |
| Duration of diabetes (years) (mean, SD, range) | 13.8 (8.48) (1 to 30) |
| Insulin use (n, %) | |
| Yes | 17 (85) |
| No | 3 (15) |
| No. of comorbid conditions (mean, SD, range) | 8.4 (3.72) (4 to 10) |
| Prior DSMES (n, %) | 8 (40) |
| Prior DSMES completion (n, %) | 4 (20) |
| Prior technology use (n, %) | 16 (80) |
| Marital status (n, %) | |
| Single | 8 (40) |
| Married | 5 (25) |
| Widowed | 5 (25) |
| Divorced | 2 (10) |
| Education (n, %) | |
| Less than high school | 6 (30) |
| High school | 7 (23.3) |
| Some college | 7 (23.3) |
| Employment status (n, %) | |
| Retired | 9 (45) |
| Disability | 6 (30) |
| Employed | 5 (25) |
Note. DSMES = diabetes self-management education and support.
A total of 23 patients were approached for the study; 20 consented for an acceptance rate of 86.9%. Of the 20 patients enrolled, 12 (60%) completed the intervention. Attrition was due to extended skilled nursing stays (n = 3; 15%), refusal of the intervention once they were home (n = 2; 10%); inability to be reached after hospital discharge (n = 2; 10%); and inability to complete the study due to advancing cognitive impairment, which had been missed in the screening phase (n = 1; 5%). Of the 12 participants who started the DSMES sessions, all (100%) completed four or more sessions.
There were limited technical issues. Two patients encountered difficulties initiating the software during one video session. These difficulties were determined to be due to an unknown software update. Once the update was completed, there were no additional technical issues. Another participant reported difficulty hearing the educator during the online education session. This participant was provided with a headset that enabled her to hear with improved sound quality and increased her satisfaction of the program. One caregiver requested to receive the education with her spouse during the intervention. The educator incorporated both the patient and caregiver in the education for this dyad.
For the 12 patients who completed the program, general diabetes knowledge significantly improved from 63 (SD = 20) to 78 (SD = 14) (p = 0.02), as did knowledge of insulin, which improved from 61 (SD = 28) to 81 (SD = 17) (p = 0.02). A1C level improved from 9.5% (SD = 2.3) to 8.5% (SD = 1.7%) (p = 0.22) (Table 2). At 30 days, two individuals who did not complete the program had rehospitalizations. Notably, there were no unplanned hospital readmissions for any patient who completed the program during this same timeframe. Participants indicated that overall, they were satisfied with DSMES delivery via electronic tablet following a hospital stay. All except one participant indicated they would receive future education via electronic tablet if available. Table 3 displays TUQ items and subscale scores.
TABLE 2.
Changes in Diabetes Knowledge Test (DKT2) and Hemoglobin A1C Level
| Variable | Mean (SD) (Range) | p Value | |
|---|---|---|---|
| Pretest | Posttest | ||
| DKT2a | |||
| General test | 63 (20) (18 to 90) | 78 (14) (45 to 100) | 0.018 |
| Insulin use | 61 (28) (18 to 100) | 81 (17) (45 to 100) | 0.015 |
| A1C (%) | 9.5 (2.3) (6.4 to 12.5) | 8.5 (1.7) (6.8 to 11.1) | 0.219 |
Higher score = % correct.
TABLE 3.
Telehealth Usability Questionnaire
| Item | Mean Score | Mode |
|---|---|---|
| Usefulness | ||
| Telehealth improves access to health care services | 6.3 | 7 |
| Telehealth saves me time traveling to a clinic | 6.4 | 7 |
| Telehealth provides for my health care needs | 5.8 | 7 |
| Ease of Use and Learnability | ||
| It was simple to use this system | 6.3 | 7 |
| It was easy to learn to use the system | 6.4 | 7 |
| I believe I could become productive quickly using this system | 6.6 | 7 |
| Interface Quality | ||
| The way I interact with this system is pleasant | 7 | 7 |
| I like using the system | 6.4 | 7 |
| The system is simple and easy to understand | 6.1 | 7 |
| This system is able to do everything I would want it to be able to do | 6.5 | 7 |
| Interaction Quality | ||
| I could easily talk to the clinician using the telehealth system | 6.9 | 7 |
| I could hear the clinician clearly using the telehealth system | 7 | 7 |
| I felt I was able to express myself effectively | 6.4 | 7 |
| Using the telehealth system, I could see the clinician as well as if we met in person | 7 | 7 |
| Reliability | ||
| I think the visits provided over the telehealth system are the same as in-person visits | 6.4 | 7 |
| Whenever I made a mistake using the system, I could recover easily and quickly | 6.7 | 7 |
| The system gave error messages that clearly told me how to fix problems | 6.25 | 7 |
| Satisfaction and Future Use | ||
| I feel comfortable communicating with the clinician using the telehealth system | 7 | 7 |
| Telehealth is an acceptable way to receive healthcare services | 6.7 | 7 |
| I would use telehealth services again | 6.4 | 7 |
| Overall, I am satisfied with this telehealth system | 6.8 | 7 |
Note. Item score ranges from 1 to 7, where 1 = strongly disagree and 7 = strongly agree, with higher scores indicating more positive responses (Parmanto et al., 2016).
DISCUSSION
The current study found the telemedicine DSMES intervention for recently hospitalized older adults with T2DM to be feasible. The study had high rates of acceptance of the program, few technical difficulties, and high rates of completion for those who started the program. Rates of initiation after enrollment were not as high as targeted, mostly due to some individuals who enrolled in the program being discharged to a skilled nursing facility and not home. Improvements were found in overall diabetes knowledge and insulin knowledge after participating in the program, as well as a clinically significant lowering in A1C level >1% (Lisi, 2018). However, given the small sample size, this reduction in A1C level was not statistically significant. Finally, participants, who were all older adults, reported the technology was easy to use and indicated they would use telehealth for DSMES delivery in the future.
This is the first study to provide diabetes telehealth-delivered education to older adults with T2DM immediately post-discharge from the hospital, a time when patients are at higher risk for rehospitalization. The immediate post-discharge period has been identified as a teachable moment and may be a time to engage and enhance patient activation, which has been associated with a decrease in hospital readmissions (Mitchell et al., 2014). Beginning contact with patients during hospitalization presents an opportunity to assess patients’ knowledge and understanding of their ability for self-management. In addition, the education provided in the home via telehealth can reinforce education provided in the hospital and may lead to improved outcomes, including decreased readmissions. In a retrospective analysis of a large dataset, Healy, Black, Harris, Lorenz, and Dungan (2013) found that patients who were provided with diabetes education during hospitalization had less frequent hospitalizations than those who were not provided education. In fact, the patient population enrolled in the current study had poor baseline diabetes knowledge with a mean DKT2 score of 63, which is lower than baseline scores reported for similar populations (Fitzgerald et al., 2016). This critical transition period provides opportunity to refer patients for DSMES, which can then be continued at home. Efforts to reduce barriers to delivery of DSMES among homebound older adults need to be explored. Diabetes education delivered via telehealth has the potential to reduce hospitalizations while also increasing diabetes knowledge.
Provision of education provided by CDEs has shown improved blood glucose control, decreased A1C level, decreased weight, and improved diabetes empowerment scores (Bollyky, Bravata, Yang, Williamson, & Schneider, 2018; Siminerio, Ruppert, & Gabbay, 2013). In the current pilot study, it was important to maintain a patient-centered approach to provide one-on-one education to older adults who were unable to access DSMES in a group setting. This model of online education and training provides many benefits including the ability to individualize education sessions, flexibility in timing of sessions, and ease of accessibility. A 100% retention rate was demonstrated in individuals who started the program, which contrasts to the 20% who indicated they completed a past DSMES program. This high completion rate may be due to taking advantage of a teachable moment when intrinsic motivation is high, but also to being able to deliver the education in the person’s home and tailoring the content to the patient’s specific needs. Of note, this tailoring extended beyond just the patient when one patient’s spouse requested to participate with the enrolled participant. When caregivers receive appropriate services tailored to their needs—such as care consultation, education, and training—improved outcomes can be achieved for the caregiver and care recipient (Feinberg & Houser, 2012).
Many stereotypes exist regarding older adults and their acceptance and use of technology. In the current study, there was a broad range of prior technology use, from no use to everyday use. An easy to use technology designed for older adults was provided; therefore, even patients who reported a low comfort level with technology were satisfied with the mode of DSMES delivery and how easy the tablet was to use. Participants also reported increased convenience by completing the education online in their home.
LIMITATIONS
The current study had several limitations. Enrollment was from one academic medical center in Philadelphia, Pennsylvania. Results therefore cannot be generalized to the greater population. The final sample was small for this limited feasibility study. There was no comparison group; thus, whether these outcomes would have improved without the DSMES is unknown. However, there is evidence of improvements in diabetes knowledge following participation in DSMES (Baradaran, Knill-Jones, Wallia, & Rodgers, 2006; Steinsbekk, Rygg, Lisulo, Rise, & Fretheim, 2012). There was some variability regarding the length of time among individual sessions. Most participants completed the 1-hour sessions; however, one individual requested shorter sessions due to fatigue and inability to focus attention after long periods. Many participants received concurrent home health care. Although it is possible that home health care alone may improve outcomes, it is important to acknowledge that due to the complexity of multiple comorbid conditions and recent hospitalization, home care use in this population could not be controlled. A majority of participants were taking insulin for T2DM management. Although proper dosage of medication can improve A1C level, only one participant had an escalation of insulin dosage at the time of hospital discharge. Finally, it is unknown whether these results would persist and if there would be sustained improvements in knowledge and A1C level over time.
CONCLUSION
The current pilot study supports that DSMES delivered via telehealth is a feasible and acceptable method to provide diabetes education and support to older adults with T2DM during transitions in care. This research provides necessary information for recruitment, retention, and feasibility of providing virtual DSMES to older adults as they are discharged from the acute care setting. Future longitudinal and experimental work with a larger sample is needed to investigate the efficacy of post-discharge diabetes telehealth education to improve meaningful clinical outcomes for this at-risk population with diabetes. Additional studies should also investigate the costs associated with telehealth education implementation.
Acknowledgments
This work was supported by the Penn Nursing Tyson Family Endowment for Gerontological Research and the Ruth L. Kirschstein National Research Service Award for Institutional Research Training (T32) Individualized Care for At Risk Frail Elders (T32NR009356) at the NewCourtland Center for Transitions and Health at the University of Pennsylvania School of Nursing.
Footnotes
The authors have disclosed no potential conflicts of interest, financial or otherwise.
REFERENCES
- American Association of Diabetes Educators. (2019). AADE7 Self-Care Behaviors®. Retrieved from https://www.diabeteseducator.org/living-with-diabetes/aade7-self-care-behaviors
- American Telemedicine Association. (2019). Telehealth basics. Retrieved from https://www.americantelemed.org/resource/why-telemedicine
- Baradaran HR, Knill-Jones RP, Wallia S, & Rodgers A (2006). A controlled trial of the effectiveness of a diabetes education programme in a multi-ethnic community in Glasgow [ISRCTN28317455]. BMC Public Health, 6(1), 134. 10.1186/1471-2458-6-134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollyky JB, Bravata D, Yang J, Williamson M, & Schneider J (2018). Remote lifestyle coaching plus a connected glucose meter with certified diabetes educator support improves glucose and weight loss for people with type 2 diabetes. Journal of Diabetes Research, 2018, 3961730. 10.1155/2018/3961730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boren SA, Fitzner KA, Panhalkar PS, & Specker JE (2009). Costs and benefits associated with diabetes education: A review of the literature. The Diabetes Educator, 35(1), 72–96. 10.1177/0145721708326774 [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. (2019). Medicare benefit policy manual: Chapter 15—Covered medical and other health services. Retrieved from https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c15.pdf
- Chrvala CA, Sherr D, & Lipman RD (2016). Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Education and Counseling, 99(6), 926–943. 10.1016/j.pec.2015.11.003 [DOI] [PubMed] [Google Scholar]
- Demiris G, Finkelstein SM, & Speedie SM (2001). Considerations for the design of a web-based clinical monitoring and educational system for elderly patients. Journal of the American Medical Informatics Association, 8(5), 468–472. 10.1136/jamia.2001.0080468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esler JL, & Bock BC (2004). Psychological treatments for noncardiac chest pain: Recommendations for a new approach. Journal of Psychosomatic Research, 56(3), 263–269. 10.1016/S0022-3999(03)00515-4 [DOI] [PubMed] [Google Scholar]
- Feinberg L, & Houser A (2012). Assessing family caregiver needs: Policy and practice considerations. Retrieved from https://www.caregiving.org/wp-content/uploads/2010/11/AARP-caregiver-fact-sheet.pdf
- Fitzgerald JT, Funnell MM, Anderson RM, Nwankwo R, Stansfield RB, & Piatt GA (2016). Validation of the Revised Brief Diabetes Knowledge Test (DKT2). The Diabetes Educator, 42(2), 178–187. 10.1177/0145721715624968 [DOI] [PubMed] [Google Scholar]
- Fonarow GC (2003). In-hospital initiation of statins: Taking advantage of the ‘teachable moment.’ Cleveland Clinic Journal of Medicine, 70(6), 502–502, 504–506. 10.3949/ccjm.70.6.502 [DOI] [PubMed] [Google Scholar]
- Graham HL, Copello A, Griffith E, Freemantle N, McCrone P, Clarke L,…Birchwood M (2016). Pilot randomised trial of a brief intervention for comorbid substance misuse in psychiatric in-patient settings. Acta Psychiatrica Scandinavica, 133(4), 298–309. 10.1111/acps.12530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, & Albright D (2018). The effectiveness of telehealth on self-management for older adults with a chronic condition: A comprehensive narrative review of the literature. Journal of Telemedicine and Telecare, 24(6), 392–403. 10.1177/1357633X17706285 [DOI] [PubMed] [Google Scholar]
- Healy SJ, Black D, Harris C, Lorenz A, & Dungan KM (2013). Inpatient diabetes education is associated with less frequent hospital readmission among patients with poor glycemic control. Diabetes Care, 36(10), 2960–2967. 10.2337/dc13-0108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawson PJ, & Flocke SA (2009). Teachable moments for health behavior change: A concept analysis. Patient Education and Counseling, 76(1), 25–30. 10.1016/j.pec.2008.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisi DM (2018). Applying recent A1C recommendations in clinical practice. Retrieved from https://www.uspharmacist.com/article/applying-recent-a1c-recommendations-in-clinical-practice
- Mitchell SE, Gardiner PM, Sadikova E, Martin JM, Jack BW, Hibbard JH, & Paasche-Orlow MK (2014). Patient activation and 30-day post-discharge hospital utilization. Journal of General Internal Medicine, 29(2), 349–355. 10.1007/s11606-013-2647-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Certification Board for Diabetes Educators. (2018). Count* by state of health professionals holding the certified Diabetes Educator® credential. Retrieved from https://www.ncbde.org/assets/1/7/StateCount0418.pdf
- Office of Disease Prevention and Health Promotion. (2012). Healthy people 2020: Diabetes. Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/diabetes/objectives
- Parmanto B, Lewis AN Jr., Graham KM, & Bertolet MH (2016). Development of the Telehealth Usability Questionnaire (TUQ). International Journal of Telerehabilitation, 8(1), 3–10. 10.5195/IJT.2016.6196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH,…Vivian E (2016). Diabetes self-management education and support in type 2 diabetes: A joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Clinical Diabetes: A Publication of the American Diabetes Association, 34(2), 70–80. 10.2337/diaclin.34.2.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shea S, Weinstock RS, Starren J, Teresi J, Palmas W, Field L,…Lantigua RA (2006). A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus. Journal of the American Medical Informatics Association, 13(1), 40–51. 10.1197/jamia.M1917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siminerio L, Ruppert KM, & Gabbay RA (2013). Who can provide diabetes self-management support in primary care? Findings from a randomized controlled trial. The Diabetes Educator, 39(5), 705–713. 10.1177/0145721713492570 [DOI] [PubMed] [Google Scholar]
- Steinsbekk A, Rygg LØ, Lisulo M, Rise MB, & Fretheim A (2012). Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus: A systematic review with meta-analysis. BMC Health Services Research, 12(1), 213. 10.1186/1472-6963-12-213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strawbridge LM, Lloyd JT, Meadow A, Riley GF, & Howell BL (2015). Use of Medicare’s diabetes self-management training benefit. Health Education & Behavior: The Official Publication of the Society for Public Health Education, 42(4), 530–538. 10.1177/1090198114566271 [DOI] [PubMed] [Google Scholar]


