Abstract
Purpose/aim:
Spatial neglect is caused by damage to neural networks critical for spatial attention. Spatial neglect without proper treatment impedes rehabilitation outcomes. Prism adaptation treatment, a visuomotor protocol, has been used with stroke survivors with spatial neglect to improve function. This case report explored the feasibility and potential effects of prism adaptation treatment in an individual with spatial neglect after glioblastoma removal.
Methods
Feasibility was designed and tested to include acceptability and implementation. Exploratory aim on the effectiveness of the intervention was determined using the Catherine Bergego Scale via the Kessler Foundation Neglect Assessment Process, star cancellation, line bisection and scene copying.
Results
The patient reported favouring the treatment. Eight sessions, one session a day, were completed over two weeks. The patient’s spatial neglect symptoms reduced on all assessments.
Conclusion
Prism adaptation treatment was feasible and effective; however, further research is needed to understand the complete benefits of prism adaptation treatment in this population.
Keywords: Unilateral spatial neglect, cognitive rehabilitation, neurorehabilitation, prism adaptation treatment, hemispatial neglect
Introduction
Spatial neglect (SN) also known as unilateral spatial neglect, results from damage to the neural networks crucial for spatial attention (Rode et al., 2017). Egocentric SN is defined as paying no or insufficient attention toward the space contralateral to the injured hemisphere, relative to the person’s midline (Rode et al., 2017). Allocentric SN is neglect of the left side of individual objects (Gossmann et al., 2013). Despite the type of SN, the deficits can disrupt basic self-care activities, impair postural balance, interfere with reading ability, impede navigation and increase fall risk (Chen et al., 2015). While SN is common after stroke, it can also occur with other types of brain injuries such as traumatic brain injury (Chen et al., 2016). The average annual incidence of glioblastoma is 11,561 or 14.7% of all tumours (Ostrom et al., 2018). Treatment, which traditionally involves surgery to extract as much of the tumour as possible, may lead to neurological consequences (Ng et al., 2019), including SN (Stone et al., 2011). Inpatient rehabilitation following glioblastoma surgery can improve outcomes and decrease hospital length of stay (Greenberg et al., 2006). While there is no rehabilitation guideline for treating SN post brain surgery, prism adaptation treatment (PAT) may be an option for ameliorating deficits related to SN that occur after glioblastoma surgery.
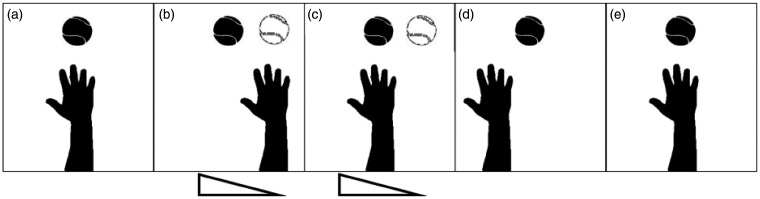
PAT is recommended for rehabilitation among stroke survivors with left-sided SN, as the treatment has been shown to decrease symptoms of SN for more than six weeks, resulting in improved activities of daily living (ADL) (Champod et al., 2018). PAT requires an individual to wear prism lenses while making arm reaching movements toward visual targets (Figure 1). Current evidence shows that PAT activates the neural networks for attention (Saj et al., 2019). After repetitive movements to targets while wearing the left-based prism goggles, adaptation and subsequent exploration of the left side of space will occur (Redding & Wallace, 2006). For individuals with left-sided neglect, prism adaptation becomes a treatment, as prism adaptation and its after-effect occur naturally, requires no effortful or conscious self-monitoring (Redding & Wallace, 2006). This case report explored the feasibility and potential effects of using PAT in an individual with SN after glioblastoma removal. This study design included data collection on the acceptability and implementation of the treatment.
Figure 1.
Illustration of an arm reaching toward a target (a) before putting on the prism, (b) at the beginning of prism exploration, (c) after multiple reaching movements and adapted to prism-shifted visual information, (d) immediately after prism removal, and (e) after multiple reaching movements and adapted back to normal vision where the target and its image are at the same location. The actual target is represented by the black ball; its prism-shifted image is the white ball.
Case history
Clinical observations
The patient was a 49-year-old female admitted to an inpatient rehabilitation facility after two surgeries, consisting of craniotomies to remove the glioblastoma in her right parietal and frontal lobes. The two admissions were 27 days in-between. She stayed 10 days and 16 days during the first and second admissions, respectively. The SN assessments and initial treatment were performed one-week post-surgery. This patient had a medical history that included seizure disorder, daily smoking and diabetes mellitus. Prior to her admission, the patient was independent in ADLs and ambulation, as well as employed full-time. The present study was conducted during her hospital stay and was approved by (omitted for Kessler Foundation’s) Institutional Review Board.
Outcome measures
The patient’s status was measured at baseline, after five PAT sessions and prior to discharge by study staff. The measures used were one functional measure and three paper-based tests. First was the Catherine Bergego Scale (CBS), via the Kessler Foundation Neglect Assessment Process (KF-NAP®), which is a 10-item performance-based scale that determines the presence and severity of SN through observation (). Each item is scored 0 to 3, with higher values indicating a greater severity of SN. The final score ranges from 0 to 30. Line bisection requires three 20-cm horizontal lines to be marked at the perceived centre. Performance is based on the average value of the bisections. The cutoff for left-sided SN is 6.5 mm left of the true centre of the line (Halligan et al., 1991). Star cancellation requires identification via circling of 56 printed stars. The maximum score for each side is 27. The cutoff for abnormal performance is 51. Dividing the score from the left side by the total score generates a laterality index. An index <0.48 indicates left-side SN and >0.52 indicates right-sided SN. For an index between 0.48 and 0.52, the performance is non-lateralised (Halligan et al., 1991). Scene copying test requires a five-object figure copying task (Gainotti et al., 1991). The task is to copy the scene on the lower half of the same page. Each element is scored anywhere from 2 to 0. A total score <10 is considered abnormal. In addition, we categorised a performance as egocentric SN if left-sided objects were missing, and as allocentric SN if left-sided features in a given object were missing. Also, the patient was asked to answer open-ended questions such as: ‘What do you think of the prism treatment? Why?’ These feasibility questions were intended to collect information about the patient’s experience and the acceptability of the PAT.
Intervention
The patient received PAT during occupational therapy, one session a day. Each PAT session took 10–15 minutes including 60 arm reaching movements with 20-diopter prism goggles on, which displaced the visual field horizontally rightward by 11.3 degrees of visual angle. PAT was administered by the occupational therapist who used the Kessler Foundation Prism Adaptation Treatment (KF-PAT®) Portable Kit and the Manual, which includes directions on administration of visual and proprioceptive pointing to determine a prism after-effect immediately after prism removal.
Results
The patient’s hospital length of stay was 16 days, during which she completed eight daily sessions of PAT. The KF-PAT Manual suggests 10 sessions, which was the intended goal for this patient, however after eight sessions she was scheduled to be discharged.
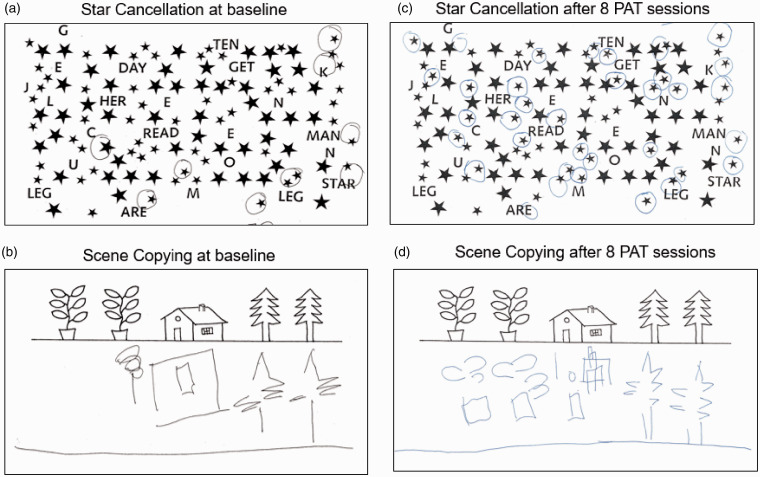
Based on her CBS scores, the patient’s SN symptoms were reduced from moderate (16.6 at admission) to mild severity (11.1 and 7, during and after PAT; Table 1 also includes each item’s score). Line bisection performance was with the normal range (deviation <6.5 mm) at baseline and during and after PAT. The star cancellation test score showed that she remained biased toward the right side (all laterality indices <0.48), but the bias during and after PAT (0.42 and 0.37, respectively) was better than that at baseline (0.16). The scene copying test showed that, the egocentric neglect improved as the score was closer to zero after treatment, but allocentric neglect did not change; see Table 1 and Figure 2.
Table 1.
Outcome measures repeated over the course of PAT.
| Outcome measure | Baseline | After five PAT sessions | After eight PAT sessions |
|---|---|---|---|
| CBS via KF-NAP | |||
| Dressing | 3 | 1 | 1 |
| Grooming | 1 | 1 | 1 |
| Leftward gaze | 2 | 2 | 2 |
| Limb awareness | 3 | 2 | 1 |
| Auditory attention | 0 | 0 | 0 |
| Collision | N/A | N/A | 0 |
| Navigation | 1 | 1 | 0 |
| Personal belongings | 2 | 0 | 0 |
| Eating | 2 | 2 | 1 |
| Cleaning after meals | 1 | 1 | 1 |
| Total scores | 15 | 10 | 7 |
| Adjusted scores | 16.6 | 11.1 | 7 |
| Line bisection | |||
| Total score in millimetres; positive = right-sided deviation | –0.33 | 1.67 | –0.67 |
| Star cancellation | |||
| Total score | 6 | 19 | 30 |
| Laterality index | 0.16 | 0.42 | 0.37 |
| Scene copying | |||
| Total score | 4 | 4.5 | 6.5 |
| Egocentric; positive = right-sided bias | 2 | 2.5 | 0.5 |
| Allocentric; positive = right-sided bias | 1 | 2.5 | 1.5 |
PAT: prism adaptation treatment; CBS: Catherine Bergego Scale; KF-NAP: Kessler Foundation Neglect Assessment Process.
Figure 2.
The patient’s performance in star cancellation and scene copying at baseline (a, c) and after prism adaptation treatment (PAT) (b, d).
PAT: prism adaptation treatment.
The patient mentioned looking forward to receiving the PAT and reported a sense of success when completing the treatment. Specifically, the patient said ‘I am excited for this therapy. I think am good at PAT’ and ‘I like using prisms because they are straightforward and not overwhelming.’
Discussion
The present study demonstrated the use of PAT with an individual experiencing SN after glioblastoma removal, integrating the treatment into her regular occupational therapy sessions. This case reported successful implementation of eight daily PAT sessions, delivered over 16 days. As mentioned in the results, the intended 10 sessions noted in the KF-PAT Manual were only not able to be completed due to a scheduled discharge during the treatment completion. There were no adverse events or issues prohibiting continuation. Thus, even though the proposed dose via KF-PAT manual guidelines was not met, eight sessions can be interpreted as a successful implementation of the protocol because it was more than the suggested minimal dose (Goedert et al., 2015).
Also, the case demonstrated the potential effect of PAT on symptoms of SN and possibly on functional improvement. Consistent with previous studies focused on stroke survivors, PAT improved the patient’s egocentric SN but not allocentric SN (Gossmann et al., 2013). It is hypothesised that the treatment effects of PAT result from increased functional activities of the dorsal neural networks critical to spatial attention operated in the egocentric, body-centred frame of references (Saj et al., 2019). In addition, the patient showed greater apparent improvement in the functional assessment than in the paper and pencil-based tests, which aligns with previous reported group-level observations (Goedert et al., 2015).
Prism adaptation and its after-effects occur without explicit effort. In other words, patients are not required to memorise or learn a specific strategy. This may be the reason why the patient ‘liked’ the treatment. Her subjective reports suggested a good level of acceptability.
Conclusion
PAT was successfully integrated into the occupational therapy plan of care for treating SN in a patient who had received craniotomies to remove a glioblastoma. PAT was considered acceptable by this patient and the protocol was able to be implemented. Consistent with the literature on stroke survivors, the patient’s SN symptoms improved. This is an important finding because the treatment can be used with multiple patient populations, which allows for more inclusivity. Limitations to this report include a lack of follow-up testing, and because this was not a randomised controlled trial, the improvement may or may not be due to PAT. Further clinical research is necessary to investigate the application of PAT to rehabilitative therapies among patients with acquired brain injuries other than stroke.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Kimberly Hreha https://orcid.org/0000-0002-8277-3992
References
- Champod A.C., Frank R.C., Taylor K., Eskes G.A. (2016). The effects of prism adaptation on daily life activities in patients with visuospatial neglect: a systematic review. Neuropsychological Rehabilitation, 28(4), 491–514. [DOI] [PubMed] [Google Scholar]
- Chen P., Hreha K., Fortis P., Goedert K. M., Barrett A. M. (2012). Functional assessment of spatial neglect: A review of the Catherine Bergego Scale and an introduction of the Kessler Foundation Neglect assessment process. Topics in Stroke Rehabilitation, 19(5), 423–435. 10.1310/tsr1905-423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen P., Hreha K., Kong Y., Barrett A. M. (2015). Impact of spatial neglect in stroke rehabilitation: Evidence from the setting of an inpatient rehabilitation facility. Archives of Physical Medicine and Rehabilitation, 96(8), 1458–1466. 10.1016/j.apmr.2015.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen P., Ward I., Khan U., Liu Y., Hreha K. (2016). Spatial neglect hinders success of inpatient rehabilitation in individuals with traumatic brain injury: A retrospective study. Neurorehabilitation and Neural Repair, 30(5), 451–460. 10.1177/1545968315604397 [DOI] [PubMed] [Google Scholar]
- Gainotti G., D’Erme P., Bartolomeo P. (1991). Early orientation of attention toward the half space ipsilateral to the lesion in patients with unilateral brain damage. Journal of Neurology, Neurosurgery, and Psychiatry, 54(12), 1082–1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goedert K. M., Zhang J. Y., Barrett A. M. (2015). Prism adaptation and spatial neglect: The need for dose-finding studies. Frontiers in Human Neuroscience, 9, 243. 10.3389/fnhum.2015.00243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gossmann A., Kastrup A., Kerkhoff G., López-Herrero C., Hildebrandt H. (2013). Prism adaptation improves ego-centered but not allocentric neglect in early rehabilitation patients. Neurorehabilitation and Neural Repair, 27(6), 534–541. 10.1177/1545968313478489 [DOI] [PubMed] [Google Scholar]
- Greenberg E., Treger I., Ring H. (2006). Rehabilitation outcomes in patients with brain tumors and acute stroke: Comparative study of inpatient rehabilitation. American Journal of Physical Medicine and Rehabilitation, 85(7), 568–573. 10.1097/01.phm.0000223218.38152.53 [DOI] [PubMed] [Google Scholar]
- Halligan, P.W., Cockburn, J. & Wilson, B.A. (1991) The Behavioural Assessment of Visual Neglect. Neuropsychological Rehabilitation, 1, 5–32.
- Ng J. C. H., See A. A. Q., Ang T. Y., Tan L. Y. R., Ang B. T., King N. K. K. (2019). Effects of surgery on neurocognitive function in patients with glioma: a meta-analysis of immediate post-operative and long-term follow-up neurocognitive outcomes. Journal of Neuro-Oncology, 141(1), 167–182. 10.1007/s11060-018-03023-9 [DOI] [PubMed] [Google Scholar]
- Ostrom Q. T., Gittleman H., Truitt G., Boscia A., Kruchko C., Barnholtz-Sloan J. S. (2018). CBTRUS statistical report: Primary brain and other central nervous system tumors diagnosed in the United States in 2011–2015. Neuro-oncology, 20(Suppl. 4), iv1–iv86. 10.1093/neuonc/noy131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redding G. M., Wallace B. (2006). Prism adaptation and unilateral neglect: Review and analysis. Neuropsychologia, 44(1), 1–20. 10.1016/j.neuropsychologia.2005.04.009 [DOI] [PubMed] [Google Scholar]
- Rode G., Pagliari C., Huchon L., Rossetti Y., Pisella L. (2017). Semiology of neglect: An update. Annals of Physical and Rehabilitation Medicine, 60(3), 177–185. 10.1016/j.rehab.2016.03.003 [DOI] [PubMed] [Google Scholar]
- Saj A., Cojan Y., Assal F., Vuilleumier P. (2019). Prism adaptation effect on neural activity and spatial neglect depend on brain lesion site. Cortex, 119, 301–311. 10.1016/j.cortex.2019.04.022 [DOI] [PubMed] [Google Scholar]
- Stone J. J., Reynolds M. R., Leuthardt E. C. (2011). Transient hemispatial neglect after surgical resection of a right frontal lobe mass. World Neurosurgery, 76(3–4), 361.e7–361.e10. 10.1016/j.wneu.2010.03.018 [DOI] [PubMed] [Google Scholar]