Abstract
AIMS:
Although research exists on parental communication in adolescents with type 1 diabetes (T1D), the role of communication by health care providers remains understudied. Grounded in Self-Determination Theory, this study examined the role of autonomy-supportive communication (i.e., providing meaningful rationale and offering choices with regard to treatment recommendations) by providers and parents, and how they interact in the prediction of diabetes outcomes.
Methods:
In this cross-sectional study, 135 adolescents (mean age 14.3 ± 2.1SD years), 171 mothers, and 121 fathers reported on autonomy-supportive communication from health care providers and parents, and on adolescent treatment adherence. HbA1c values were retrieved from the medical record.
Results:
In adolescent reports, perceived autonomy-supportive communication from providers but not from parents was positively related to treatment adherence. A significant interaction between autonomy-supportive communication from providers and parents pointed to the highest level of treatment adherence when adolescents perceived both providers and parents as autonomy-supportive. In contrast, parental reports revealed that parental autonomy-supportive communication was positively related to treatment adherence, whereas autonomy-supportive communication by providers was not.
Conclusions:
Autonomy-supportive communication by providers and parents is associated with better treatment adherence in adolescents with T1D. Interventions to improve autonomy-supportive communication by parents and providers may improve treatment adherence of adolescents (e.g., communication training).
Keywords: Type 1 diabetes, Health care providers, Adolescents, Communication, Parents, Self-Determination theory
1. Introduction
Self-management of type 1 diabetes (T1D) imposes many complex behavioral demands on the person with diabetes and their family [1,2]. Adolescents especially are a high-risk population, as they face normative physical and psychosocial changes while transitioning to more independence in life and in diabetes management [3]. During this pivotal developmental phase, relationships with parents and health care providers gradually change [4]. Decreasing parent involvement and defiance against self-care recommendations [5] may account for the fact that only a minority of youth attain recommended age-specific HbA1c goals [6,7].
Research demonstrates that diabetes self-management is most effective in the context of collaborative interpersonal relationships [8] – responsive, rather than intrusive and controlling support for diabetes management predicts better outcomes among adolescents with T1D, including better glycemic control, treatment adherence, and quality of life [5,9–11]. A key factor for diabetes outcomes in adolescents is communication by important stakeholders such as parents and health care providers from the diabetes team about the T1D treatment recommendations [5,12]. One understudied area in this respect is the specific role of autonomy-supportive communication, a concept grounded in Self-Determination Theory (SDT; [13], an encompassing framework about motivation.
Applied to T1D, the use of autonomy-supportive communication by parents and health care providers, implies that one explains the personal relevance of the recommendations for diabetes self-care to adolescents, while accepting adolescents’ perspectives rather than opposing possible negative feelings elicited by these recommendations, and while leaving room for choice and personal initiative [5,14]. Although autonomy support has been found to be beneficial for overall well-being in youth from the general population [15], few studies in T1D research have focused on autonomy-supportive communication by parents, and even fewer on autonomy-supportive communication by health care providers [5,12,16]. Moreover, to our knowledge, no studies addressed the unique and interactive role of autonomy-supportive communication by parents and by health care providers in the prediction of treatment adherence and glycemic control.
Previous work has established the relevance and importance of autonomy-supportive communication by parents [5]. However, although parents are often seen as most closely involved in the diabetes treatment, it is important not to overlook health care providers of the diabetes team [17,18]. Previous research indeed demonstrates that patient-provider communication, and satisfaction with the patient-provider relationship are essential for good health outcomes and adherence to treatment recommendations [19]. One of the few studies that focused on adolescent and parent perceptions of autonomy-supportive communication specifically by health care providers found that adolescent perception of a better health care climate (i.e., autonomy-supportive communication by providers) was associated with higher levels of self-efficacy and treatment adherence [20]. A study in young adults transitioning from pediatric to adult health care [21] revealed similar results. However, both studies examined adolescent reports, and the parent perspectives examined were mainly mothers, leaving fathers largely underrepresented. As research in related domains has established the importance of fathers for diabetes management [22,23] their perceptions of communication by the health care team may be important as well.
To date, few studies have examined autonomy-supportive communication by health care providers from a multi-informant perspective, including adolescents, and mothers as well as fathers [16]. Furthermore, although research suggests that support and communication by parents and by the health care team may mutually influence each other [12], the unique and interactive roles of autonomy-supportive communication by parents and by health care providers for adolescents with T1D remain understudied. Optimal treatment adherence and glycemic control may be achieved when both parents and health care providers are perceived as communicating in an autonomy-supportive manner. Further, support from one source may play a buffering role for the other. For example, when parents are perceived as communicating in a less autonomy-supportive way with regard to diabetes management, health care providers may play a buffering role (and vice versa).
1.1. The current study
The current study is one of the first to assess the relationship of diabetes-related autonomy supportive communication by parents and by health care providers, both separately and in interaction with each other, to adolescent treatment adherence and glycemic control. Given the surge of evidence in diabetes research illustrating the importance of applying a multi-informant family perspective [23–25], in the current study we have included adolescents, mothers, and fathers, rather than using the classic dyadic mother-adolescent approach.
Utilizing this multi-informant approach, two main research objectives were addressed. First, we aimed to explore differences and similarities across respondents in their reports on autonomy-supportive communication provided by parents and by health care providers. Given the dearth of literature about autonomy-supportive communication in adolescents with T1D from a multi-informant family perspective, we did not put forward specific hypotheses in this regard. Second, we aimed to examine the unique and combined effects of autonomy-supportive communication by parents and by health care providers for adolescent treatment adherence and glycemic control. Based on prior studies [5,12] investigating autonomy-supportive communication by parents and by health care providers separately, we hypothesized that both autonomy-supportive communication by providers and by parents would be uniquely positively related to treatment adherence and glycemic control. We also expected that the most optimal levels of treatment adherence and glycemic control would be attained when both health care providers and parents were perceived as autonomy-supportive. Furthermore, we hypothesized a buffering effect of autonomy-supportive communication by health care providers on diabetes outcomes when parents would be perceived as communicating in a less autonomy-supportive manner. In turn, when health care providers are perceived as less autonomy supportive, parental autonomy-supportive communication may play a buffering role towards diabetes outcomes.
2. Method
2.1. Participants and procedure
Adolescents with T1D meeting the following criteria participated in the study: (1) diagnosed with T1D for at least six months, (2) aged 11–18 years, and (3) Dutch-speaking. Exclusion criteria were other severe somatic (e.g., cystic fibrosis), psychiatric or developmental (e.g., autism) diagnoses. Recruitment of adolescents and parents took place at seven hospitals in Belgium through e-mail with a link to the online questionnaires using a secured web survey. Of 360 contacted families, a total of 135 (37.5%) adolescents, 171 (47.5%) mothers, and 121 (33.6%) fathers participated. Participation in the study was individually possible for each adolescent, mother, and father of the contacted families. In 38.4% of the participating families, adolescent as well as mother and father responded, while in other cases one or two family members of the same family participated.
An online informed assent or consent form was signed by all participants and parents gave active informed consent for their adolescent’s participation. The study was approved by central and local Institutional Review Boards of participating centers prior to implementation of any study procedures.
2.2. Measures
2.2.1. Demographic and diabetes-related characteristics
Adolescents and parents provided information on age, sex, ethnicity, family structure and level of education and profession. After obtaining informed consent and/or assent from parents and/or adolescents, data on duration of T1D, treatment (injection vs. pump), and glycemic control in terms of HbA1c (reported in % and mmol/mol) value were retrieved from medical records. The HbA1c-value closest to the date of the survey completion (i.e., ±3 months) was used. In Belgium, all clinical sites have similar assays to measure HbA1c in order to guarantee continuity and quality of HbA1c results.
2.2.2. Diabetes-related autonomy-supportive communication by health care providers
Adolescent and parent perceived autonomy support was measured with the short six item version of the Brief Health Care Climate Questionnaire [26], after rigorous translation and back translation into Dutch. The Brief Health Care Climate Questionnaire measures persons’ perspectives of the degree to which they perceive their health care team as communicating in an autonomy–supportive manner, i.e., by providing a rationale, and an empathic and open-minded perspective (e.g., “I feel that my diabetes team provides me with options and choices.”). Both adolescents and parents rated all items on a 7-point Likert scale (‘strongly disagree’ to ‘strongly agree’). In the current study, reliability of the adolescent and parent measures for autonomy supportive health care climate was excellent: α = 0.91 and α = 0.91/95 (adolescent report and mother/father report).
2.2.3. Diabetes-related autonomy-supportive communication by parents
To assess the degree to which one perceives parents to communicate in an autonomy-supportive manner, a previously validated measure was adapted to a diabetes-related version [5,14,27]. After four statements describing maternal and paternal expectations about diabetes self-management, including measuring blood glucose values, injecting insulin, healthy eating, and physical activity (e.g., ‘To what degree does your mother have clear expectations about how often you should measure your blood sugar values’), adolescents were asked about the quality of parental communication (i.e., autonomy supportive or psychologically controlling) across these four self-care areas. For the current study, only the autonomy-supportive scale was used, reflecting parental provision of a rationale, and an empathic and open-minded perspective (4 items, e.g., ‘My father gives me a meaningful explanation for why he considers this to be important for me.’). Similarly, mothers and fathers reported upon their own diabetes-related autonomy support. For parent self-reports, the items were adapted (e.g., “I would be open to my adolescent’s point of view and ask if my adolescent could find another way to change something in his self-care behavior”). Participants rated all items on a 5-point Likert scale (‘totally disagree’ to ‘fully agree’). The measures are available for the Reader upon request. Reliability of the adolescent and parent measures for diabetes-related autonomy support was good: α = 0.87 and α = 0.87 for adolescent-reports about mothers and fathers, respectively, and α = 0.70, and α = 0.60, for mothers’ and fathers’ self-reports, respectively.
2.2.4. Treatment adherence
For assessment of treatment adherence, the previously validated Diabetes Self-Management Profile-Self-Report and Parent-Report surveys (DSMP-SR and -PR; [28] were used after rigorous forward and backward translation into Dutch. These 24-item surveys quantify adolescent self-management behaviors over the previous three months (e.g., “If you think you are having a low blood sugar, how often do you check your blood sugar before treating?”). Item responses included 2, 3 or 4-point Likert response scales. Internal consistency reliability in the current study was adequate: α = 0.77 and α = 0.71/0.68 (adolescent self-report and mother/father proxy report).
2.3. Statistical analyses
Analyses using SPSS v.26 were conducted in three steps. To address the first research question, paired samples t-tests were performed to investigate mean level differences in adolescent treatment adherence, and in autonomy-supportive communication by parents and by health care providers, across the three respondents (adolescent, mother, father). Bivariate Pearson correlations among the variables were calculated as well. To address the second research question, four sets of regression analyses were conducted: (1) adolescent-reported autonomy-supportive communication by mother, and by health care providers predicting adolescent reported adherence and glycemic control, (2) adolescent-reported autonomy-supportive communication by father, and by health care providers predicting adolescent reported adherence and glycemic control, (3) mother-reported autonomy-supportive communication by mother, and by health care providers predicting mother-reported adherence and glycemic control, and (4) father-reported autonomy-supportive communication by father, and by health care providers predicting father-reported adherence and glycemic control. Before calculating interaction terms, all independent variables – except for sex (0 = male, 1 = female) and type of insulin administration (0 = injections, 1 = pump) – were standardized [29]. In Step 1, we added sex, age, and illness duration as control variables. In Step 2, we added autonomy-supportive communication by parents and from health care providers. In Step 3, the two-way interaction term was added, and significant interaction terms were interpreted if the chunk test indicated a significant increase in R2 [30].
3. Results
3.1. Sample characteristics
Adolescents had a mean age of 14.3 ± 2.1 years, had a mean diabetes duration of 6.2 ± 3.9 years, and the majority were female (52%). Mean HbA1c was 7.5 ± 1.1% (58 mmol/mol) and only 24% were on pump therapy. Further, the majority of families were intact (80.8%), and had the Belgian nationality (96.8%). Most adolescents were receiving secondary education (82.8%) while a minority received primary (11.5%) or higher education (5.7%). Most parents had a college or university degree (66.4% of mothers and 61.3% of fathers) and had a job (93.7% of mothers and 96% of fathers).
3.2. Mean level analyses
Table 1 presents means and standard deviations of all variables in the lower panel of the table. To address the first exploratory research question, paired sample t-tests revealed that mothers reported higher perceived autonomy-supportive communication by the health care providers than adolescents (t(1 0 5) = −3.03, p = .003) and fathers (t(87) = 2.94, p = .004). Paired sample t-tests also showed no difference between adolescent and father reports of autonomy-supportive communication by the health care providers. With regard to perceived parental autonomy-supportive communication, adolescents perceived their mothers as more autonomy-supportive than their fathers (t(1 3 2) = 2.66, p = .009), and both mothers and fathers reported themselves as being more autonomy-supportive than their adolescents perceived them (t(1 0 2) = 4.76, p < .0001 and t(94) = 5.37, p < .0001), respectively). With regard to adolescent treatment adherence, no differences emerged among the three respondents.
Table 1 –
Summary of Pearson intercorrelations, means and standard deviations for scores on autonomy-supportive communication by parents, and by health care providers, and on treatment adherence and HbA1c.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.Autonomy-supportive Communication Mother AR | - | ||||||||||
| 2. Autonomy-supportive Communication Father AR | 0.54** | - | |||||||||
| 3. Autonomy-supportive Communication Mother PR | 0.27** | 0.25* | - | ||||||||
| 4. Autonomy-supportive Communication Father PR | 0.25** | 0.22* | 0.29** | - | |||||||
| 5. Autonomy-supportive Communication Health Care Providers AR | 0.44** | 0.40** | 0.16 | 0.21* | - | ||||||
| 6. Autonomy-supportive Communication Health Care Providers MR | 0.11 | 0.13 | 0.23** | 0.13 | 0.26** | - | |||||
| 7. Autonomy-supportive Communication Health Care Providers FR | 0.14 | 0.14 | −0.05 | 0.20* | 0.23* | 0.18 | - | ||||
| 8.Treatment adherence AR | 0.08 | 0.12 | 0.11 | 0.14 | 0.30** | 0.01 | 0.05 | - | |||
| 9.Treatment adherence MR | 0.06 | 0.06 | 0.14 | 0.12 | 0.24* | 0.04 | 0.03 | 0.60** | - | ||
| 10. Treatment adherence FR | 0.06 | 0.05 | 0.12 | 0.42** | 0.20 | 0.22* | 0.22* | 0.41** | 0.51** | - | |
| 11. HbAlc | 0.00 | −0.19* | −0.03 | −0.24** | −0.16 | −0.09 | −0.10 | −0.46** | −0.34** | −0.27** | - |
| M | 4.0 | 3.7 | 4.5 | 4.4 | 33.4 | 35.3 | 34.1 | 58.6 | 60.0 | 60.5 | 7.5 |
| SD | 1.0 | 1.0 | 0.5 | 0.5 | 6.8 | 6.1 | 6.8 | 10.3 | 8.8 | 8.3 | 1.1 |
Note. AR = adolescent report; PR = parent report; MR = mother report; FR = father report.
p ≤ 0.05.
p ≤ 0.01.
p ≤ 0.001
3.3. Correlation analyses
Table 1 presents the correlations in the top panel of the table. Adolescent-reported maternal and paternal autonomy-supportive communication correlated significantly with mother- and father-reported autonomy-supportive communication respectively, and there was a positive correlation between mother- and father-reported parental autonomy-supportive communication. Further, adolescent-, mother-and father-reported autonomy-supportive communication by parents, related positively to adolescent-, mother- and father-reported autonomy-supportive communication by health care providers, respectively. Higher adolescent and father-reported autonomy-supportive communication by health care providers was associated with higher adolescent and father-reported treatment adherence, respectively, while no correlation was found between mother-reported autonomy-supportive communication by providers and mother-reported treatment adherence. Lastly, father-reported but not mother- or adolescent-reported parental autonomy support related negatively to HbA1c, and better treatment adherence reported by all three respondents correlated consistently to lower HbA1c. No associations emerged between HbA1c and autonomy support from providers.
3.4. Regression analyses
Table 2 (adolescent reports) and Table 3 (parent reports) present standardized betas and R2 values of the regression analyses.
Table 2 –
Standardized beta coefficients from the hierarchical regression analyses for adolescent reports.
| Predictor | Treatment AdherenceAadherence | HbA1c |
|---|---|---|
| Step 1 (R2) | 0.07*/0.08* | 0.10**/0.09** |
| Sex (0 = male; 1 = female) | 0.20*/0.21* | −0.11/−0.11 |
| Age | −0.11/−0.14 | 0.10/0.08 |
| Illness duration | −0.09/−0.08 | 0.24**/0.25** |
| Step 2 (change R2) | 0.14**/0.15** | 0.11**/0.12** |
| Autonomy-Supportive Communication by ParentsCommunication | −0.05/−0.01 | 0.03/−0.14 |
| Autonomy-SupportiveCommunication by Health Care Providers | 0.30**/0.27** | −0.12/−0.06 |
| Step 3 (change R2) | 0.17***/0.18*** | 0.13*/0.12** |
| Autonomy-SupportiveCommunication by Parents × AutonomySupportive | 0.20*/0.18* | −0.15+/−0.05 |
| Communication by Health CareProviders | ||
Note. The coefficient before the slash is for adolescent-reports about mother; the coefficient after the slash is for adolescent-reports about father.
p ≤ 0.10.
p ≤ 0.05.
p ≤ 0.01.
p ≤ 0.001.
Table 3 –
Standardized beta coefficients from the hierarchical regression analyses for parent-reports.
| Predictor | Treatment Adherence AdAdhadherence | HbA1c |
|---|---|---|
| Step 1 (R2) | 0.06*/0.08* | 0.06*/0.09* |
| Sex (0 = male; 1 = female) | 0.05/0.04 | −0.14+/−0.04 |
| Age | −0.07/−0.01 | 0.11/0.11 |
| Illness duration | −0.21**/−0.27* | 0.14+/0.23* |
| Step 2 (change R2) | 0.08*/0.23*** | 0.06+/0.12* |
| Autonomy-SupportiveCommunication by Parents | 0.14+/0.34*** | 0.01/−0.17+ |
| Autonomy-SupportiveCommunication by Health Care Providers | −0.04/0.15+ | −0.03/−0.07 |
| Step 3 (change R2) | 0.08*/0.23*** | 0.07+/0.14* |
| Autonomy-Supportive | 0.09/−0.05 | −0.10/−0.13 |
| Communication by Parents × Autonomy | ||
Note. The coefficient before the slash is for mother-reports; the coefficient after the slash is for father-reports.
p ≤ 0.10.
p ≤ 0.05.
p ≤ 0.01.
p ≤ 0.001
3.4.1. Adolescent reports
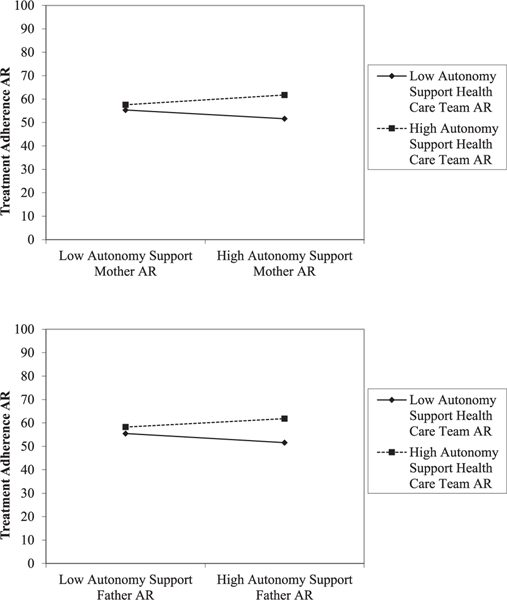
In step 1, sex was significantly related to treatment adherence, indicating that girls tended to have better treatment adherence than boys. Illness duration was significantly related to HbA1c, indicating that longer illness duration was associated with higher HbA1c. In step 2, perceived autonomy-supportive communication by health care providers was uniquely related to treatment adherence, whereas autonomy-supportive communication by parents was not. No associations were found with HbA1c. In step 3, a significant interaction emerged between perceived autonomy-supportive communication by parents, and by health care providers. This indicates that the combination of more perceived parental autonomy-supportive communication and more perceived autonomy-supportive communication by health care providers was associated with more optimal outcomes in terms of treatment adherence. With HbA1c as the outcome, the interaction effect between autonomy-supportive communication by health care providers and from mothers was in the expected direction, albeit not statistically significant (p < .10). Fig. 1 shows a graphical depiction of the significant interaction effects in adolescent reports.
Fig. 1 –
Significant interaction effects.
3.4.2. Parent reports
In step 1, illness duration was negatively related to treatment adherence, and the association with HbA1c was in the expected direction, but not statistically significant. Hence, similar to findings in adolescent reports, longer diabetes duration was related to worse treatment adherence and higher HbA1c. In step 2, contrary to adolescent reports, no unique effect was found of perceived autonomy-supportive communication by health care providers. Father reports of autonomy-supportive communication were uniquely related to treatment adherence, and mother reports of autonomy-supportive communication were in the same direction, albeit not significant (p < .10). Further, there was a tendency towards significance for father-reported of autonomy support and HbA1c (p < .10). In step 3, none of the interaction effects reached significance.
4. Discussion
Grounded in Self-Determination Theory (SDT) [13], this cross-sectional study investigated the unique and interactive role of autonomy-supportive communication by parents and health care providers for treatment adherence and glycemic control in adolescents with type 1 diabetes (T1D). In doing so, we applied a multi-informant family approach, involving adolescents, mothers, and fathers. Several theoretically meaningful and clinically relevant findings emerged, pointing to the importance of autonomy-supportive communication by important stakeholders.
First, with regard to differences and similarities across the three respondents, adolescents perceived their mothers as communicating in a more autonomy-supportive way than their fathers. This finding is in line with previous research in youth with T1D, affirming mothers -who are most often the primary caregivers- as more closely involved [31,32] and as more supportive in the daily management of their adolescents’ T1D [5,32]. Similar to previous research [12], mothers also tended to report higher perceived autonomy-supportive communication by health care providers than adolescents and fathers did. One explanation for the latter finding may be that, in addition to being more closely involved in the daily diabetes care of their adolescent, mothers may also interact more closely with health care providers. In turn, this interaction may provoke more autonomy-supportive communication by health care providers towards mothers. The finding that adolescent reports of autonomy-supportive communication by health care providers correlated most strongly with adolescent reports of autonomy-supportive communication by mothers, seems to be in line with this as well. This is consistent with longitudinal research by Baker and colleagues in young adults [12], who found that high perceived quality in the maternal relationship sets the stage for higher perceived autonomy-supportive communication by health care providers (referred to as patient-centered communication).
Second, with regard to adolescent and parent perspectives on the unique and interactive role of autonomy-supportive communication by parents and health care providers for adolescent treatment adherence and glycemic control, differences emerged between adolescent and parent perspectives. Notably, from the adolescent perspective, perceived autonomy-supportive communication by health care providers but not by parents was uniquely positively related to treatment adherence. Although replication of these findings in a longitudinal design is needed to clarify directionality of effects, adolescents may take daily parental autonomy-supportive communication (or lack thereof) for granted, while autonomy-supportive communication by their health care providers may be of more importance for how they deal with their T1D. In turn, adolescents displaying better self-management, may provoke more autonomy-supportive communication from providers.
The opposite pattern of findings emerged from the perspective of parents – self-perceived autonomy-supportive communication by parents but not by health care providers was uniquely positively related to treatment adherence. More specifically, findings stemming from fathers’ perspectives were more robust than from mothers’ perspectives, which may point to different roles parents attribute themselves. Parents, and fathers especially, may overestimate the importance of their own autonomy-supportive communication for their adolescents’ self-management, and may therefore attach less importance to the health care team’s autonomy-supportive communication. Further, the interaction effect between autonomy-supportive communication by parents and by health care providers in adolescent reports, may point to an accumulating effect of autonomy supportive communication by different stakeholders. When adolescents experience both parents and providers as communicating in an autonomy supportive manner, they may be more inclined to adhere to the self-management recommendations. Lastly, the finding that no significant associations were found with glycemic control deserves attention. Indeed, in diabetes research it is generally more common to find associations with the more subjective self- or proxy-reported assessments of treatment adherence, than with the more objective measure of glycemic control (although some exceptions break this rule, e.g., [24]). Several explanations for the current finding are possible, such as the indirect link between perceptions of communication, and glycemic control through better adherence.
4.1. Limitations and avenues for future research
Several limitations must be acknowledged and represent avenues for future research. First, given the cross-sectional design, causality cannot be inferred. Although we hypothesize a beneficial effect of autonomy-supportive communication by important stakeholders for adolescent self-management, this link is likely to have a bidirectional component. Thus, carefully designed longitudinal studies are needed to understand directionality of effects, and to disentangle the complex pathways between stakeholder communication and adolescent diabetes outcomes. For example, youth displaying more optimal self-management and glycemic control may experience more positive clinic visits, since there are fewer problems to address, and may elicit more responsive and autonomy-supportive communication. Second, the current sample was Belgian, and generally had relatively good glycemic control (mean HbA1c = 7.5%, or 58 mmol/mol). Hence, generalizability of findings to families in the US and other parts of the world, and to adolescents who are not meeting targets for glycemic control may be limited. Further, parents were relatively highly educated. All of these factors might be indicative of a relatively high functioning research sample. Future research should target youth with a broader range of glycemic control, while also paying attention to educational and ethnic diversity, particularly since a study of minority youth with T1D found that adolescents reported significantly lower levels of satisfaction with the patient-provider relationship than parents [19]. Future longitudinal research may also benefit from investigating whether the importance of autonomy-supportive communication differs according to adolescents’ glycemic control. It may be that perceived autonomy-supportive communication by important stakeholders has a more tangible impact in adolescents with optimal glycemic control (≤7.0%). Adolescents with suboptimal glycemic control may be less inclined to be influenced by an autonomy-supportive approach (and in the latter group of adolescents, parents and health care providers may, out of a sense of helplessness, be less inclined to take on an autonomy-supportive attitude). Third, the current study is specifically focused on the concept of autonomy-supportive communication, one of many behavioral constructs of importance to adolescents with T1D. Future multi-informant research on the role of autonomy-supportive communication could also benefit from including a broader set of biopsychosocial and behavioral parameters. For example, including concepts such as diabetes-related family responsibilities and conflicts would allow for exploration of potential interactions of these parameters with autonomy-supportive communication. Also, including concepts such as diabetes-related self-efficacy, and adolescents’ sense of perceived competence might be beneficial, as these concepts may function as mediators in the association between autonomy-supportive communication and diabetes-related outcomes [12,33,34]. Fourth, only a minority of participating families included data from adolescent as well as mother and father as respondents. Although this did not impact our within-respondent analyses, future research may benefit from efforts to include all three respondents within families, such that more comparative hypotheses can be explored. Lastly, given the importance of a multi-informant approach which adds richness to interpreting results, it may be interesting for future research to include providers’ perspectives as well.
4.2. Conclusions and clinical implications
The current study provides evidence for the importance of autonomy-supportive communication for adolescents with T1D, and sheds light on significant similarities and differences according to adolescent, mother or father perspectives.
Important implications for clinical care can be drawn from this research. In line with suggestions from previous research [5,12], a focus on autonomy-supportive communication by parents, and by health care providers may be an important avenue for future interventions, especially as communication can be considered modifiable. Moreover, given the likely potentially accumulating effect for adolescent self-management of both parents and health care providers applying autonomy-supportive communication, it may be beneficial to raise awareness in clinicians for the importance of how they communicate with adolescents and parents, as their influence may be twofold. First, health care providers may be a model for parents in how they communicate to adolescents about the recommendations for diabetes self-management (e.g., by adopting an accepting rather than opposing attitude towards adolescents’ possible negative feelings elicited by the treatment, and by developing a compassionate dialogue with the adolescent about alternatives) [5,35]. Further, in line with the substantial body of evidence in diabetes research illustrating the importance of collaborative, responsive, and autonomy-supportive parental communication (e.g., [36]), having clinicians integrate attention for parental communication skills into routine diabetes care, and ideally into clinical interventions, may be beneficial as well. Second, health care providers themselves may be of influence through their autonomy-supportive attitude and communication towards adolescents with T1D. Therefore, in line with contemporary training recommendations for health care providers [37], integrating attention to provider communication and style of communication into routine diabetes care may be useful. This can be accomplished through the possibility of communication training for providers [38].
Acknowledgements
The authors gratefully acknowledge the willingness of the families to participate in this study. We are highly indebted to all seven participating diabetes centers across Belgium for their help in collecting the data. Most specifically we would like to thank the following colleagues: Susanne Böhler, Karen De Winter, Marian De Wulf, Elke Dello, Michel Kruth, Jolien Laridaen, Lynn Van Hecke & Shana Van Impe. This work was partially conducted with support from Harvard Catalyst.
Funding
Dr. Goethals’ work on this project was supported by the Clinical Research Fund of the University Hospital Leuven, the Vlaamse Diabetescentra voor Kinderen en Adolescenten (VDKA), the Belgian American Educational Foundation (BAEF), and a Mary K. Iacocca Research Fellowship provided by the Iacocca Family Foundation.
Footnotes
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
R E F E R E N C E S
- [1].Hilliard ME, Harris MA, Weissberg-Benchell J. Diabetes resilience: a model of risk and protection in type 1 diabetes. Curr Diab Rep 2012;12(6):739–48. [DOI] [PubMed] [Google Scholar]
- [2].American Diabetes Association. 13. children and adolescents: standards of medical care in diabetes-2019. Diabetes Care 2019;42(Suppl 1):S148–64. [DOI] [PubMed] [Google Scholar]
- [3].Raymond JK. Models of care for adolescents and young adults with type 1 diabetes in transition: shared medical appointments and telemedicine. Pediatr Ann 2017;46(5): e193–7. [DOI] [PubMed] [Google Scholar]
- [4].Wiebe DJ et al. Developmental processes associated with longitudinal declines in parental responsibility and adherence to type 1 diabetes management across adolescence. J Pediatr Psychol 2014;39(5):532–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Goethals ER et al. “Let’s talk about it” The role of parental communication in adolescents’ motivation to adhere to treatment recommendations for type 1 diabetes. Pediatr Diabetes 2019;20(7):1025–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Foster NC et al. State of type 1 diabetes management and outcomes from the T1D exchange in 2016–2018. Diabetes Technol Ther 2019;21(2):66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].DeSalvo DJ et al. Continuous glucose monitoring and glycemic control among youth with type 1 diabetes: International comparison from the T1D Exchange and DPV Initiative. Pediatr Diabetes 2018;19(7):1271–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Wiebe DJ, Helgeson V, Berg CA. The social context of managing diabetes across the life span. Am Psychol 2016;71 (7):526–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Goethals ER et al. Parenting and treatment adherence in type 1 diabetes throughout adolescence and emerging adulthood. J Pediatr Psychol 2017;42(9):922–32. [DOI] [PubMed] [Google Scholar]
- [10].Gruhn MA, Lord JH, Jaser SS. Collaborative and overinvolved parenting differentially predict outcomes in adolescents with type 1 diabetes. Health Psychol 2016;35(7):652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Young MT et al. Good cop, bad cop: quality of parental involvement in type 1 diabetes management in youth. Curr Diab Rep 2014;14(11):546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Baker AC et al. Structural model of patient-centered communication and diabetes management in early emerging adults at the transfer to adult care. J Behav Med 2019;42 (5):831–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ryan RM, Deci EL. Self-determination theory : basic psychological needs in motivation, development, and wellness. New York: Guilford Press; 2017. [Google Scholar]
- [14].Van Petegem S et al. When do adolescents accept or defy to maternal prohibitions? The role of social domain and communication style. J Youth Adolesc 2017;46(5):1022–37. [DOI] [PubMed] [Google Scholar]
- [15].van der Kaap-Deeder J et al. Children’s daily well-being: the role of mothers’, teachers’, and siblings’ autonomy support and psychological control. Dev Psychol 2017;53(2):237–51. [DOI] [PubMed] [Google Scholar]
- [16].Croom A et al. Adolescent and parent perceptions of patient-centered communication while managing type 1 diabetes. J Pediatr Psychol 2011;36(2):206–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Patel NJ, Datye KA, Jaser SS. Importance of patient-provider communication to adherence in adolescents with type 1 diabetes. Healthcare (Basel) 2018;6(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Datye KA et al. A review of adolescent adherence in type 1 diabetes and the untapped potential of diabetes providers to improve outcomes. Curr Diab Rep 2015;15(8):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Taylor CJ et al. Satisfaction with the health care provider and regimen adherence in minority youth with type 1 diabetes. J Clin Psychol Med Settings 2016;23(3):257–68. [DOI] [PubMed] [Google Scholar]
- [20].Wysocki T, Gavin L. Paternal involvement in the management of pediatric chronic diseases: associations with adherence, quality of life, and health status. J Pediatr Psychol 2006;31 (5):501–11. [DOI] [PubMed] [Google Scholar]
- [21].Taylor SE et al. Systematic review of father involvement and child outcomes in pediatric chronic illness populations. J Clin Psychol Med Settings 2020;27(1):89–106. [DOI] [PubMed] [Google Scholar]
- [22].Prikken S et al. A triadic perspective on control perceptions in youth with type 1 diabetes and their parents: associations with treatment adherence and glycemic control. Diabetes Res Clin Pract 2019;150(1):264–73. [DOI] [PubMed] [Google Scholar]
- [23].Berg CA et al. Adolescents’, mothers’, and fathers’ reports of adherence across adolescence and their relation to HbA1c and daily blood glucose. J Behav Med 2016;39 (6):1009–19. [DOI] [PubMed] [Google Scholar]
- [24].Czajkowska Z et al. Validation of the English and french versions of the brief health care climate questionnaire. Health Psychol Open 2017;4(2). 2055102917730675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Vansteenkiste M et al. Longitudinal associations between adolescent perceived degree and style of parental prohibition and internalization and defiance. Dev Psychol 2014;50 (1):229–36. [DOI] [PubMed] [Google Scholar]
- [26].Wysocki T et al. Validation of a self-report version of the diabetes self-management profile. Pediatr Diabetes 2012;13 (5):438–43. [DOI] [PubMed] [Google Scholar]
- [27].Cohen J et al. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. Mahwah, NJ: Lawrence Erlbaum; 2003. [Google Scholar]
- [28].Jaccard J, Turrisi R. Interaction effects in multiple regression. Vol. 72; 2003. Sage. [DOI] [PubMed] [Google Scholar]
- [29].Seiffge-Krenke I. Diabetic adolescents and their families: Stress, coping, and adaptation. Cambridge: University Press; 2001. [Google Scholar]
- [30].Berg CA et al. Adolescent disclosure to parents and daily management of type 1 diabetes. J Pediatr Psychol 2016;42 (1):75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Williams GC et al. Reducing the health risks of diabetes: how self-determination theory may help improve medication adherence and qualityof life.Diabetes Educ 2009;35(3):484–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Ng JY et al. Self-determination theory applied to health contexts: a meta-analysis. Perspect Psychol Sci 2012;7 (4):325–40. [DOI] [PubMed] [Google Scholar]
- [33].Tanenbaum ML et al. Adapting and validating a measure of diabetes-specific self-compassion. J Diabetes Complications 2018;32(2):196–202. [DOI] [PubMed] [Google Scholar]
- [34].Nansel TR et al. A multisite trial of a clinic-integrated intervention for promoting family management of pediatric type 1 diabetes: feasibility and design. Pediatr Diabetes 2009;10(2):105–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].van Zanten M et al. Assessing the communication and interpersonal skills of graduates of international medical schools as part of the United States Medical Licensing Exam (USMLE) Step 2 Clinical Skills (CS) Exam. Acad Med 2007;82(10 Suppl):S65–8. [DOI] [PubMed] [Google Scholar]
- [36].Resnicow K, McMaster F. Motivational Interviewing: moving from why to how with autonomy support. Int J Behav Nutr Phys Act 2012;9:19. [DOI] [PMC free article] [PubMed] [Google Scholar]