Abstract
By employing the city-level data from China during the spring of 2020, this study investigates the relationship between city-level resilience against the outbreak of COVID-19 pandemics and its affecting factors, including the inflow risk pressure of COVID-19 virus (population inflow from the epicenter), city agglomeration characteristics (urban population density and city size), healthcare resource adequacy, among others. The results reveal that, while managing COVID-19 inflow risk pressure plays a critical role in the city’s pandemic disaster resilience, city agglomeration characteristics also matters. To be exact, we find that large and high-density cities with high inter and intra-city mobility flows have more difficulties in containing the epidemic spread, but improving healthcare infrastructure adequacy and urban governance capacity can increase time efficacy of pandemic control and then improve the city’s resilience against pandemic. Although our analysis is based on the performance of Chinese cities in the case of COVID-19, the research framework can be applied in understanding COVID-19 control performance of cities in other countries and the findings can be useful for improving health-related urban resilience and sustainability.
Keywords: COVID-19, Public health, Urban resilience, Population density, Urban governance
1. Introduction
Coronavirus disease 2019 (COVID-19), assessed by the United Nations as the biggest challenge facing the whole human since the World War II, has triggered extensive scientific research from various perspectives (OECD, 2020; The Lancet, 2020b; WHO, 2020b). Urban characteristics, such as city size, density, geographic distance to the domestic epicenter and health infrastructure, have large impacts on resilience of a city against the outbreak of COVID-19 pandemic (Florida, 2020; Glaeser, 2020; The Lancet, 2020b). While infectious diseases has occurred with increasing frequencies in cities in recent decades (Zarocostas, 2020, Jones et al., 2008), there is still significant knowledge shortage concerning the role of urban characteristics in city’s epidemic resilience.
In an urban resilience perspective, urban preparedness and emergency governance for infectious diseases has shown many loopholes and difficulties facing the challenge of COVID-19 (Acuto, 2020; Florida, 2020; Kraemer et al., 2020; Tian et al., 2020). Deeper understanding of urban resilience for health urgency events can not only help to guide post-disaster socioeconomic recovery, but also inform key factors and issues necessary to be taken care of for the next coming pandemic disasters. Different with natural disasters whose durations are usually not in the hand of human control, pandemic disaster impacts vary greatly in time duration depending on urban preparedness and intervention measures (Lee et al., 2020; Peak et al., 2020; The Lancet, 2020b). The differences can be attributed to factors including population density and connectivity, emergency data and governance capability, information validation and dissemination, as well as citizen and community engagement (Lee et al., 2020). Thus, comparative studies of COVID-19 situation across cities can add knowledge to resilience framework regarding pandemic mitigation measures. Such evaluations would help city planners, policy-makers, and managers to understand better the current resilience level of cities against pandemic disasters (Fastiggi, Meerow, & Miller, 2020; Hernantes, Maraña, Gimenez, Sarriegi, & Labaka, 2019; Scott, 2020).
To provide timely-needed empirical knowledge on factors that affecting a city’s pandemic disaster resilience, this paper analyzes the relationship between a set of key urban characteristics and varibles, including COVID-19 inflow risk pressure from the epicenter, economic activity scale and population density, and healthcare burden, of 120 prefecture-level cities in China and the time these cities spent to contain the outbreak of COVID-19 disease in spring of 2020. The paper primarily measures the time to contain the outbreak of COVID-19 virus by the length of the days from the day with the first confirmed case of COVID-19 to the day after three successive days without any single confirmed COVID-19 case, with other alternative measures for robustness checks. Besides controlling for the inflow risk pressure of virus transmission by using the amount of population inflow from Chinese first reported epicenter of COVID-19 (Wuhan city), the paper explores the roles of several factors including the proximity to the domestic epicenter, characteristics of urban agglomeration e.g. city size and city density, economic development levels, healthcare resource adequacy in the emergency status, and experience in previous major infectious diseases.
This study contributes to the existing literatures on urban resilience that so far mostly focusing on natural disaster (Biggs et al., 2012; Turner et al., 2003; Zou, Lam, Cai, & Qiang, 2018; Qiang, Huang, & Xu, 2020). Moreover, this paper studies the duration time to put disease outbreak under control instead of socioeconomic consequences of diseases that commonly investigated in previous literature, contributing to expanding the knowledge of urban disaster preparedness that can be used to improve urban planning and emergency governance strategies from the novel viewpoint of time efficiency of outbreak control. Practically, this study provides policy-makers and urban planners with useful empirical evidence and takeaways regarding preparations for future pandemic disasters.
The paper will be organized into the following sections. The second section first reviews related works and then develop the main hypotheses to be empirically tested in the paper. The third section explains the data sources, discusses variable definition and presents the empirical approach of this paper. Section 4 presents the econometric model results, robustness checks and discussions of findings. Finally, the paper concludes with policy recommendations in section 5.
2. Literature review and hypothesis development
The research work of this paper is situated at the intersection point of several strands of literature, including urban resilience, emergency management, urban governance, healthcare provision, and social epidemiology research. Below, the paper first briefly reviews theoretical literatures on urban resilience, and how the framework can and should further incorporate empirical evidence on resilience against pandemic disasters. Then, previous studies on key factors related to resilience against pandemic disasters are examined, including a city’s geographic proximity to the domestic epicenter, population inflow from the epicenter, city density, urban economic activity scale, healthcare resources adequacy, and previous pandemic experiences. These reviews and discussions form the theoretical mechanisms underlining the main hypotheses to be tested in the paper.
2.1. Urban resilience
The term resilience was by Holling (1973) initially introduced the term resilience as a determinant of how system relationships are persistant and how systems absorb changes of their variables (Ribeiro & Gonçalves, 2019). Among myriads of definiations of resilience, this study focuses on the maintenance, resistance, and recovery perspective of resilience (Allenby & Fink, 2005; Zhou, Wan, & Jia, 2010). In the urban resilience perspective, the adopted definition of resilience focuses on how a city can absorb and adapt to external pressures during any crisis, hazards or disasters (Rus, Kilar, & Koren, 2018; Zhu, Li, & Feng, 2019). Specifically, Meerow, Newell, and Stults, 2016, page 39) define urban resilience as how an urban system can “maintain or rapidly return to desired functions in the face of a disturbance, to adapt to change, and to quickly transform systems that limit current or future adaptive capacity” (Cariolet, Vuillet, & Diab, 2019).
Resilience has gained increasing interests in urban studies due to its applicability to better understand and improve governance for urban disasters and emergencies (Fastiggi et al., 2020; Godschalk, 2003; Wardekker et al., 2020). Urban resilience is used as de facto framework for enhancing emergency preparedness, response, and recovery (Cutter, Ash, & Emrich, 2014). However, resilience research faces several issues that hinder its usefulness and applicability in guiding planning and intervention practices, which include the lack of clear-cut definition (2008, Cutter et al., 2014; Wardekker et al., 2020), and dearth of empirical data in a disaster conditions to quantify the impacts of key determination factors of resilience (Chen & Zhang, 2020; Sherrieb, Norris, & Galea, 2010; Qiang et al., 2020).
2.2. Resilience and pandemic emergency governance
The ongoing global spread of COVID-19 pandemic presents challenges to urban emergency governance as well as opportunities and empirical data to study urban disaster resilience. First, as a health disaster, the study of COVID-19 adds to the existing resilience literatures that mostly focus on environmental disasters (Shamsuddin, 2020; Zou et al., 2018). Recent decades witness many emerging infectious diseases occurring at an increasing scale and frequency, such as Ebola virus disease, severe acute respiratory syndrome (SARS), avian and pandemic influenza, Middle-East respiratory syndrome (MERS), and the most recent COVID-19 (Jones et al., 2008; McCloskey, Dar, Zumla, & Heymann, 2014; The Lancet, 2020b). As the outbreaks of contagious diseases typically struck the cities without any early warning and resulted in wide-ranging negative socioeconomic shocks, there is an increasing call for health disaster preparedness to be crucially included in the design of urban resilience frameworks (Kruk et al., 2017; Lee et al., 2020; McCloskey et al., 2020). Especially, Jovanović et al. (2020) propose that future solutions to pandemic disasters (such as COVID-19) should use resilience indicators that are adopted and adapted from other critical infrastructure evaluation. Some urban resilience and vulnerability frameworks have been proposed for COVID-19. For example, Mishra, Gayen, and Haque (2020) devised a COVID Vulnerability Index using Analytic Hierarchy Process for India including variables such as population density, residential building quality, and distance from drinking water. Peters (2020) creates a COVID‐19 susceptibility scale at the county level, USA with indicators including population density, percentage of elderly population, and COVID-19-related disease mortality. Our study aims to fill in the research gap to provide further solid empirical evidence for pandemic disaster resilience framework.
With the increasing availability of big data and advanced information technology, unprecedentedly close monitoring of population mobility has been placed during COVID-19 outbreak and different public health intervention measures have been implemented (Beria & Lunkar, 2021; OECD, 2020; Peak et al., 2020; WHO, 2020a). With new means of syndromic surveillance, more prompt execution of travel prohibit and stricter enforcement of quarantine of infected people and their contacts (Bauch & Anand, 2020; Chinazzi et al., 2020; The Lancet, 2020a), the correlation between urban agglomeration characteristics and COVID-19 transmission speed may have different patterns as compared to previous major. With advancement of information technology, extensive surveillance systems that installed in high-density areas can assist the public authority to put the mobility of infected cases or potential virus carriers under closer monitoring and more prompt to limit their contagion risks (Wilder-Smith & Freedman, 2020). Meanwhile, high-density areas may facilitate the spread of epidemic information, health knowledge as well as news of health policy intervention measures (The Lancet, 2020a). Further, quarantine of patients, people screening, proactive testing, travel restrictions to the extent of complete lockdown, and other forms of prevention and control measures would be more likely to be implemented in urban areas (Bauch & Anand, 2020; Chinazzi et al., 2020; The Lancet, 2020b). In addition, the community coordination of public health intervention would be more effective in urban areas (Jia et al., 2020). These advantages of higher density would be especially true in the case of China, where the state has high authority power to control population mobility and has installed extensive surveillance systems everywhere in the downtowns of major cities (Kupferschmidt & Cohen, 2020; WHO, 2020a). Nonetheless, even taking into account of all these new technology developments, big and high-denser cities still intuitively appear to be more vulnerable to the outbreak of health disaster due to the high population mobility, high frequency of travels and economic activities (Florida, 2020; Glaeser, 2020).
In summary, the research of urban resilience is extensive but still needs clear-defined empirical and practical studies to solidify its contribution to urban emergency governance and planning management practices. With respect to urban resilience against epidemic outbreak, the existing literature has generally investigated connections between the spread of the infection in cities and certain urban agglomeration characteristics. However, yet no study has explored how the urban agglomeration characteristics correlate with a city’s time efficiency of containing the outbreak of virus, the indicator that can reflect a city’s resilience against epidemic outbreak. This paper sets out to bridge this gap.
2.3. Hypothesis development
To address the ongoing debate, we develop 3 hypotheses mainly concerning whether cities with higher population inflow risk pressure from the epicenter, larger economic activity scale and higher population density, or healthcare burden would suffer prolonged or shorter time of disease control. This paper chooses to study the time length to brake the spread of COVID-19 virus rather than the peak number of COVID-19 infection case, as the former indicator can better reflect the initial stage of a city’s resilience for preparedness when struck by the sudden outbreak of a pandemic. Our 3 hypotheses are present as below:
H1
The time that a city spent to contain the epidemic outbreak is longer when there is higher population inflow risk pressure from the first reported domestic epicenter to this city.
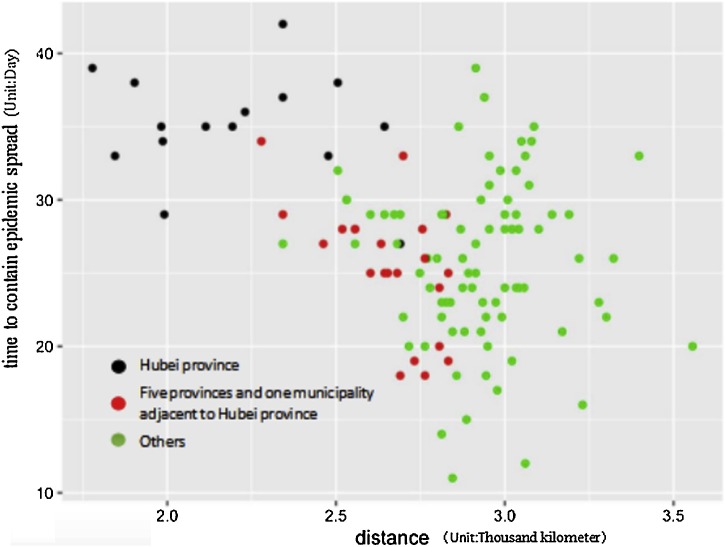
Geographic proximity to the domestic epicenter is widely suspected to have great influence on the between-city transmission of disease. An earlier literature has proposed that closeness to the first epicenter (Wuhan) could be a significant independent predictor of the number of confirmed COVID-19 cases in Chinese cities, especially in the immediate stage after the outbreak of pandemic (Liu, 2020; Qiu, Chen, & Shi, 2020) (Fig. 1 ). Liu (2020) estimated that 1% closer of the distance to Wuhan city is associated with 0.96 % higher the confirmed infection number in the city (Liu, 2020). We thus expect that higher number of inflow population from the domestic epicenter in proportion to the city total population results in prolonged length of contagious disease control.
H2
The time that a city spent to contain the spread of epidemic is longer when the city has a large economic activity scale and a higher population density.
Fig. 1.
The time to contain epidemic spread and distance to Wuhan.
Higher population density can create vulnerability to natural and pandemic disasters (Connolly et al., 2020; Prashar, Shaw, & Takeuchi, 2012). Emerging infectious diseases are either reported to originate in urban settings (such as COVID-19), or rapidly propagate in urban areas (such as SARS Zika virus) (Cho et al., 2016; Metsky et al., 2017). An analysis of a database of 335 emerging infectious diseases (EID) 'events' (origins of EIDs) between 1940 and 2004 suggests that human population density was a common significant independent predictor of EID events in all categories (Jones et al., 2008). Bhadra, Mukherjee, and Sarkar (2020) have found moderate association between Covid-19 spread (measured by infection and mortality rate) and population density in India. However, so far there is no widely-accepted consensus on the role of city size and population density in the infection and mortality rate of infectious diseases. For example, a study of the 1918 influenza pandemic in the U.S cities find that factors such as, population size or density, were not significantly correlated with city-level excess deaths in 1918–1919 (Bootsma & Ferguson, 2007). Sun, Zhang, Yang, Wan, and Wang (2020) that population density cannot affect COVID-19 spreading under strict lockdown policies in China. A recent study of COVID-19 finds that both urban area and population density are negatively correlated with the city-level confirmed COVID-19 cases in urban China (Liu, 2020). The author suspected that this “counter-intuitive finding” was largely due to a special reason that population outflows from Wuhan city during the “spring rush” that mainly inflowed to small cities or even rural areas (Liu, 2020).1
Big cities with higher scale of economic activities are usually associated with higher propensity of social contact and transmission from various factors including crowded indoor and outdoor living, closely packed public transport systems, higher difficulties for isolation and social distancing, they thus intuitively appear to has less resilience against the outbreak of epidemic (Block et al., 2020; Chu et al., 2020; Florida, 2020; Glaeser, 2020; Lai, Webster, Kumari, & Sarkar, 2020; Peak et al., 2020). Florida (2020) identifies 3 types of cities that are most severely hit by COVID-19, which include: 1) large dense superstar cities (New York and London), which are vulnerable due to large flow of people; 2) industrial centers (Wuhan, Detroit and Northern Italy), which are connected through supply chain; and 3) tourist meccas (ski slopes of Italy, Switzerland, and cities in the Colorado Rockies). In general, these are places with high population density and/or economic activity scales. We thus propose cities with higher population density and economic activity scales would have more difficulties to achieve a timely containment of COVID-19 spread.
H3
The time that a city spent to contain the spread of epidemic is shorter when the city has a higher adequacy of healthcare facilities and previous pandemic disease experiences.
The ratio of COVID-19 cases to health-care resource availability and accessibility (such as the number of hospitals in a city) have been used to measure adequacy of healthcare facilities (Ji, Ma, Peppelenbosch, & Pan, 2020), and experiences for handling previous pandemics (such as SARS) represent previous pandemic disease experiences (Fang et al., 2012). Previous research has found the critical importance of healthcare resource in mitigating the transmission risk of epidemic (Fang et al., 2012; Ji et al., 2020). Some early studies on COVID-19 containment clearly indicate high impacts of healthcare resource adequacy and healthcare burden on COVID-19 mortality rates and mitigation. Ji et al. (2020) postulated that higher mortality rates in the epicenter of China (Wuhan and Hubei) is likely to be related to an insufficiency of health-care resources facing the rapid escalation in the number of infections. They showed a significant positive correlation between mortality and health-care burden (numbers of infections in a given population). Evidence have suggested that insufficient healthcare resources could lead to more likely crash of healthcare system and higher mortality (Ji et al., 2020). Inequalities of healthcare facility accessibility further place certain population in excessively high health risks and disproportionate impacts of COVID-19 pandemic (Kraemer et al., 2020; Lee et al., 2020; Peak et al., 2020).
We also concern the impacts of past experiences of infectious diseases to the epidemic preparedness. It has been suggested that infectious disease experiences may enhance preparedness of cities against coming pandemics (The Lancet, 2020b). For example, as post-hoc pandemic reaction, many authorities in urban areas worldwide have developed infectious disease surveillance systems that make use of digital and web-based information, or have established contingency and emergency plans (Tang, Bie, Park, & Zhi, 2018). For China, the last nationwide pandemic was SARS in 2003. Therefore, experiences for handling SARS may be useful against COVID-19 outbreak. Specifically, the Chinese Government established the public health system for emergent and novel infectious diseases after SARS in 2003, which played a significant role in outbreak prevention and control of H1N1 in 2009 (Fang et al., 2012). Our final hypothesis thus postulates that higher adequacy of healthcare facilities and previous pandemic disease coping experiences in a city can help cities mitigating growth of disease case in shorter periods.
3. Data description and empirical strategy
This section first elaborates the empirical identification strategy of this study, and then explains the data sources, sample construction and variable selection to be used in the regression models.
3.1. Empirical model
This study employs multiple linear regression for quantitative measurement with 120 prefecture-level cities in China as analytical units. The cities are selected subject to the data availability of key variables. Multiple linear regression (MLR), also known simply as multiple regression, is a statistical technique that uses several explanatory variables to predict the outcome of a response variable. The goal of multiple linear regression (MLR) is to model the linear relationship between the explanatory (independent) variables and response (dependent) variable. MLR is used extensively in econometrics and financial inference. Our study aims to investigate the relationship between city-level resilience against the outbreak of COVID-19 pandemics and its affecting factors, including the inflow risk pressure of COVID-19 virus (population inflow from the epicenter), city agglomeration characteristics (urban population density and city size), healthcare resource adequacy, among others. Therefore, MLR is applicable.
The details of data source and variable explanations are available in Table 1 with data source introduced in Section 3.2. Assuming COVID-19 inflow risk pressure, the city economic activity size, population density, GDP per capita would correlate the time to contain the epidemic spread in logarithm form and the rest variables would correlate in linear form, we construct the econometric model as following:
| (1) |
Table 1.
Variable definition and descriptive statistics.
| Variable | Definition | Unit | Mean | Variance | Minimum | Maximum | obs |
|---|---|---|---|---|---|---|---|
| Time: Time to contain the epidemic spread (reach plateau stage) | Days from the day with first case to the day after three consecutive days of zero case | Day | 26.802 | 5.907 | 11 | 42 | 126 |
| Inflow | Population inflow from Wuhan during the 2020 spring rush | 10,000 persons | 4.220 | 11.308 | .033 | 79.665 | 124 |
| Inflow ratio | Population inflow from Wuhan during the 2020 spring rush/local population | % | 0.973 | 2.955 | 0.004 | 21.817 | 120 |
| Lninflow | Log of inflow | – | −.037 | 1.608 | −3.421 | 4.378 | 124 |
| popu | City’s urban population (2017) | 10,000 persons | 260.39 | 310.450 | 28 | 2450 | 124 |
| GDP | City’s GDP (2017) | 0.1 billion Yuan | 2931.6 | 4805.90 | 184.64 | 28178.65 | 119 |
| GDPp | GDP per capita (2017) | Yuan | 75200 | 34529.15 | 20003 | 167411 | 117 |
| Garbage | Total waste treatment amount (2017) | 10,000 ton | 103.64 | 145.066 | 11.650 | 924.770 | 124 |
| Density | Urban population /Urbanized area of the city (2017) | 10,000 persons/ km2 |
1.2143 | 0.5286 | 0.0523 | 2.946 | 126 |
| med | Number of Medical practitioners/Number of confirmed cases as of March 9, 2020 | Person/ Persons |
170.80 | 186.386 | 0.520 | 980.300 | 120 |
| Hospital bed | Hospital bed number/Number of confirmed cases as of March 9, 2020 | Bed Number/ Persons |
318.26 | 347.096 | 1.309 | 2244.787 | 120 |
| Hospital | Hospitals/Number of confirmed cases as of March 9,2020 | Hospital number/ Persons |
1.417 | 1.609 | 0.006 | 9.571 | 120 |
| SARS | Provincial-level SARS confirmed cases in 2003 | Person | 127.13 | 408.059 | 0 | 2521 | 124 |
3.2. Data source and variable explanation
Data used in this paper is collected from various sources, including China City Statistics Yearbook, Baidu migration index database, online government information, news reports and professional reports. Data of city scale (including population size, annual GDP and annual size of waste management), population density, the city’s annual GDP per capita, healthcare resource is referring to the year of 2017 and obtained from China City Statistical Yearbook. The year of 2017 is the latest year that these data are publicly available for most sample cities. We assume that socioeconomic variables have stayed consistenly from 2017 to early 2020 at city-level in China, as the economy in this period was undergoing steady growth with no major disturbances or fluactuation. Below we explain the construction of dependent variable and key control variables.
3.2.1. Time to contain the epidemic spread
The stage with no further growth of cases is referred as the stage of epidemic plateau in this paper (plateau). Data related to COVID-19 in this study are all from the information disclosed by the National Health Commission of China (NHCC, 2020) and local health commission agencies as of March 9, 2020. We suppose the time to reach the epidemic plateau, reflecting the time efficacy of epidemic containment, can well exemplify the city’s resilience against epidemic outbreak. In the case of COVID-19, we use the day after three consecutive days without new case to identify epidemic plateau. More details of the cutoff date and plateau time selection is available in Appendix A, and the results are documented in Appendix Table C3.
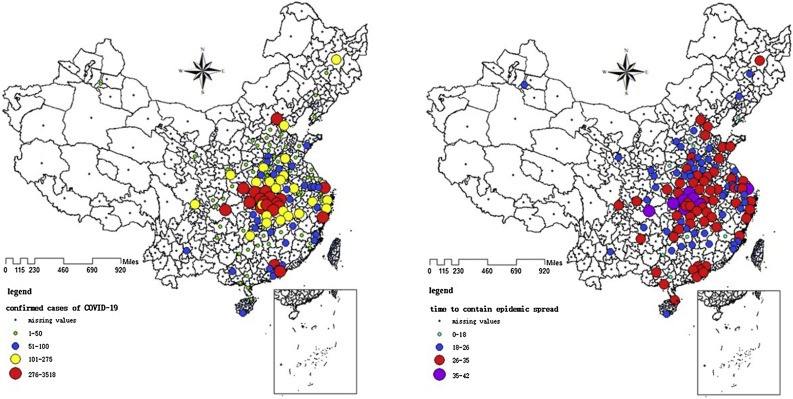
Fig. 2 shows spatial distribution of city-level accumulated COVID-19 confirmed cases as well as the time to control COVID-19 outbreak as of March 9. The time which Chinese cities spent to contain the epidemic spread shows less weight in spatial concentration to the proximity of Wuhan City and Hubei Province. Six out of the eight cities with the longest days spent are from Hubei Province, including Jingmen, Xiaogan, Ezhou, Yichang, Suizhou, and Jingzhou. These cities took more than 35 days to brake the epidemic spread. The remaining two cities are Shanghai and Chongqing, which are followed by another two cities in Hubei Province. Outside Hubei Province, Hangzhou and Beijing also took significantly longer time to put the epidemic under good containment.
Fig. 2.
Total COVID-19 confirmed cases of Chinese cities and city-level variations of the time to contain the epidemic spread.
3.2.2. Measurement of COVID-19 inflow risk pressure
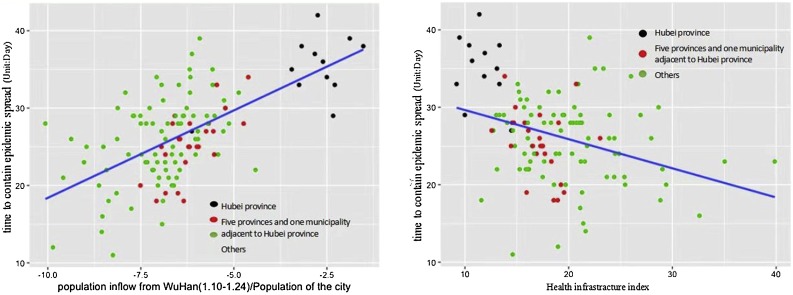
The estimate of population inflow from Wuhan is constructed using data from three sources, including the open source intercity travel indicators from Baidu Migration (an online migration database created by the largest Chinese internet search engine, Baidu), the passenger train schedule of Wuhan Railway Bureau, and inter-region migration data from previous years. This study estimates the approximate population inflow from Wuhan to each sample city between the period of January 10–24, 2020. The 15-day span is selected because the traditional Spring Festival travel rush started on January 10 in the year of 2020 and population outflow from Wuhan was banned on January 23, 2020 due to the lockdown of Wuhan city (WHO, 2020a). The details of processing Baidu Migration data, along with other dataset, is available in Appendix B, and the results are documented in Appendix Table C1. In the left panel of Fig. 3 , we employ the indicator of population inflow from Wuhan as a proportion of local population, and find it has a strong positive relationship with the time to contain the spread of COVID-19 virus. It thus provides an intuitive support for Hypothesis 1. The right panel on Fig. 3 shows that cities with higher healthcare infrastructure index spend shorter time in reaching the containment of epidemic spread, barring other controls.
Fig. 3.
Correlations between COVID-19 inflow risk pressure, health infrastructure and the time to contain the epidemics spread.
3.2.3. Population density and economic activity size
The indicator of city’s population density is computed by population per area of urbanized land in the city. Therefore, compared with the population density calculated by dividing total population in the city’s jurisdiction (often including rural population) by administrative area, population density used in this study reflects population aggregation of cities in a more accurate and authentic manner. For economic activity size, this study selects waste treatment amount as the proxy variable of city economic activity size to mitigate collinearity that other key independent variables are closely associated with city economic activity size.
3.2.4. Healthcare infrasutructre adequecy
Because COVID-19 was a major public health emergency, the commonly used per capita healthcare resource indicator may not reflect the healthcare resource adequacy at the urgent time. Therefore, in addition to per capita indicators of healthcare resources, this study also measures healthcare resource adequacy by dividing healthcare resources by the number of accumulated cases by March 9, 2020. Healthcare resources indicators in this paper refer to medical practitioners, hospital beds and hospitals. In order to improve the robustness of healthcare resource adequacy indicator, we use, referring to the report of Ni and Li’s (2020) healthcare infrastructure index. This study adopts the total confirmed cases of SARS at province-level as the proxy indicator for the experience a city accumulated in responding to major public health emergencies, and the data source is from China’s Public Health Data Center2 , since confirmed cases of SARS were disclosed only at province-level, and the provincial government in China plays a leading role in building public health system.
3.2.5. Other control variables
To cities in Hubei Province, population inflow from Wuhan was also much larger than that to cities outside Hubei Province (cf. Appendix C: Table C2). Therefore, we add the dummy variable, “Hubei: whether the city is in Hubei”, into the regressions and compare the econometric results with and without cities of Hubei Province. In addition, to migrate estimation bias due to regional clustering, we divide31 provinces, of mainland China into seven regions. Detailed designation of provinces in a given regional clustering is given in Appendix C: Table C4. Clustering robust standard errors are estimated based on these seven geographic regions.
4. Empirical results and discussion
4.1. Regression results
This study constructs multiple linear regression model to quantify the correlations between the time for cities to reach epidemic plateau with a number of city characteristics. Benchmark regression results are shown in Table 2 . We first explore the effects of COVID-19 inflow risk pressure on urban epidemic control efficacy. The results demonstrate that COVID-19 inflow risk pressure is positively correlated to the time for cities to reach epidemic plateau when population density, healthcare infrastructure index, city economic activity size (especially when indicated by waste treatment amount) are controlled. Regression coefficients remain stable under various model settings. Specifically, according to the results of Table 2, COVID-19 inflow risk pressure significantly prolongs the time to reach COVID-19 case plateau. At the mean value of the samples, 100 % increase in COVID-19 inflow risk pressure (population inflow from Wuhan as proportion of local population) postpones the average time for reaching epidemic plateau by 1.03–1.18 day. Then, we also anticipate that city economic activity size increase difficulty in epidemic control significantly. According to column (4) and (5) of Table 2, at the mean value of the samples, 100 % increase in city economic activity size (i.e. waste treatment amount) postpones the average time for reaching epidemic plateau by 2.8–2.93 days when other conditions remain constant.
Table 2.
Factors that correlated with a city’s time to contain the spread of COVID-19 (benchmark results).
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| VARIABLES | time | time | time | time | time |
| lninflow | 1.033*** | 1.074** | 1.180*** | 1.150*** | 1.048** |
| (0.223) | (0.332) | (0.265) | (0.255) | (0.342) | |
| lnpopu | 3.574*** | 3.217** | |||
| (0.679) | (1.154) | ||||
| lnGDP | 3.226*** | 1.240 | |||
| (0.868) | (1.171) | ||||
| lngarbage | 2.798*** | 2.934*** | |||
| (0.671) | (0.594) | ||||
| lndensity | 0.628 | 2.322*** | 2.152*** | −0.084 | |
| (0.855) | (0.522) | (0.410) | (1.195) | ||
| lnGDPp | −2.206 | 0.987 | 0.713 | ||
| (1.795) | (1.055) | (0.947) | |||
| bidoctor | −0.012*** | −0.012*** | −0.012*** | −0.012*** | −0.013** |
| (0.003) | (0.003) | (0.002) | (0.002) | (0.003) | |
| hubei | 6.771*** | 6.791*** | 6.819*** | 6.537*** | |
| (0.729) | (1.393) | (1.152) | (1.254) | ||
| SARS | −0.071 | ||||
| (0.146) | |||||
| Constant | 0.169 | 13.608 | −26.972* | −22.605* | −10.930 |
| (2.329) | (22.903) | (13.828) | (11.030) | (20.716) | |
| Observations | 119 | 117 | 117 | 106 | 109 |
| R-squared | 0.627 | 0.653 | 0.635 | 0.531 | 0.633 |
Notes: (1) The t value in parentheses is calculated by using the Chinese 7 major geographic regions level clustering robust standard error; (2) *, **, *** are statistically significant at the 10 %, 5%, and 1% levels, respectively.
Besides, we investigate the effects of population density on urban epidemic control efficacy. The results demonstrate that population density is positively correlated to the time for cities to reach epidemic plateau. at the mean value of the samples, 100 % increase in city population density postpones the average time for reaching epidemic plateau by 2.15–2.32 day, suggesting that COVID-19 outbreak is harder to contain in cities with higher population density.
Meanwhile, we find that adequacy of medical practitioners significantly shortens the time for reaching epidemic plateau. As shown in Table 2, increasing one doctor per patient shortens the time for reaching epidemic by around 0.012−0.013 days. On the other hand, the impacts of SARS confirmed cases in 2003 in Table 2 is not significant. Based on the above results, it can be summarized that the time to reach epidemic plateau is subject to COVID-19 inflow risk pressure, city economic activity size, population density, and adequacy of medical practitioners. Inflow risk pressure and city activity size (identified by volume of garbage treatment per day) are also consistently positive and significant, which are expected in our hypothesis.
4.2. Robustness tests
To examine the robustness of the results of Table 2, several alternative models have been conducted several for robustness tests. First, we explore alternative model variables including ratio of population inflow from Wuhan the city’s population, logarithm of per capita GDP (directly taken from China City Statistical Yearbook (lnGDPp) and our own calculation based on GDP within city ministration boundary divided by population within city ministration boundary(lnGDP/pop)), and alternative measures of health infrastructure adequacy (hospital bed per patient and health infrastructure index explained in section 3.2(3)). The result in Table 3 demonstrates that the effects of population density, COVID-19 inflow risk pressure, adequacy of medical practitioners, and city economic activity size have robust effects to the length of days to reach COVID-19 case plateau. Moreover, inflow population ratio, adequacy of hospital beds, and healthcare infrastructure index also demonstrate expected effects with similar direction to their alternative variables (total COVID inflow risk pressure and medical practitioner adequacy, respectively).
Table 3.
Factors that correlated with a city’s time to contain the spread of COVID-19 (robustness checks).
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| VARIABLES | time | time | time | time |
| lninflow | 1.211*** | 1.222*** | 1.283*** | |
| (0.271) | (0.268) | (0.186) | ||
| lngarbage | 2.555*** | 3.574*** | 2.621*** | 3.117*** |
| (0.669) | (0.745) | (0.676) | (0.646) | |
| lnGDP/pop | 1.438 | 0.466 | ||
| (0.919) | (1.097) | |||
| lndensity | 2.880*** | 2.426*** | 2.213*** | 2.374*** |
| (0.732) | (0.505) | (0.542) | (0.568) | |
| bidoctor | −0.012*** | −0.015*** | ||
| (0.002) | (0.002) | |||
| hubei | 6.625*** | 9.508*** | 6.612*** | 5.303*** |
| (1.141) | (0.628) | (1.242) | (0.879) | |
| inflowratio | 21.789*** | |||
| (3.135) | ||||
| lnGDPp | 0.962 | 0.939 | ||
| (1.167) | (1.206) | |||
| Hospital bed | −0.006*** | |||
| (0.001) | ||||
| medicalindex | −0.442*** | |||
| (0.066) | ||||
| Constant | −36.668* | −14.505 | −25.446 | −22.735 |
| (15.390) | (13.712) | (14.709) | (15.616) | |
| Observations | 119 | 119 | 117 | 118 |
| R-squared | 0.641 | 0.606 | 0.628 | 0.623 |
Notes: (1) The t value in parentheses is calculated by using the Chinese 7 major geographic regions level clustering robust standard error; (2) *, **, *** are significant at the 10 %, 5%, and 1% levels, respectively; (3) Samples in the table only include cities outside Hubei Province.
We further explore factors affecting the time for cities to reach epidemic plateau by adding different interaction terms. Column (2) and (3) of Table 4 demonstrate that effects of population and city economic activity size has varied effects with respect to different COVID-19 inflow risk pressure. Higher density actually mitigates higher inflow risk pressure, while larger economic activity size actually multiplies the effects of higher COVID-19 inflow risk pressure. Column (4) shows that higher number of medical practitioners per patient has diminishing effects when city grows in economic activity sizes. Contrarily, column (6) shows that that higher number of medical practitioners per patient has increasing effects in shortening days to reach epidemic plateau in when city population density is higher.
Table 4.
Factors that correlated with a city’s time to contain the spread of COVID-19 (interaction term: moderating effects).
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| VARIABLES | time | time | time | time | time | time |
| lninflow | 1.344*** | −5.660** | 3.469*** | 0.526*** | 1.002*** | 1.043*** |
| (0.267) | (1.775) | (0.693) | (0.139) | (0.222) | (0.187) | |
| lngarbage | 3.188*** | 3.169*** | 9.195*** | 1.972*** | 18.870* | 3.124*** |
| (0.414) | (0.460) | (1.447) | (0.387) | (8.653) | (0.401) | |
| lndensity | 1.923*** | −4.522* | 1.853** | 2.181*** | 8.451* | 3.574*** |
| (0.511) | (1.892) | (0.524) | (0.429) | (3.776) | (0.710) | |
| bidoctor | 0.004 | −0.012*** | −0.014*** | −0.069*** | −0.012*** | 0.087** |
| (0.011) | (0.002) | (0.002) | (0.006) | (0.002) | (0.030) | |
| hubei | 6.357*** | 7.464*** | 5.771*** | 7.361*** | 7.648*** | 7.443*** |
| (1.021) | (0.851) | (0.778) | (0.599) | (0.906) | (0.754) | |
| Doctor*inflow | −0.002 | |||||
| (0.001) | ||||||
| Density*inflow | 0.721*** | |||||
| (0.179) | ||||||
| Garbage*inflow | −0.633*** | |||||
| (0.159) | ||||||
| Doctor*garbage | 0.011*** | |||||
| (0.001) | ||||||
| Density*garbage | −1.707 | |||||
| (0.920) | ||||||
| Density*Doctor | −0.011** | |||||
| (0.003) | ||||||
| Constant | −15.180** | 47.481** | −34.569*** | −4.493 | −72.321* | −27.674*** |
| (5.559) | (18.127) | (9.142) | (3.990) | (35.056) | (6.959) | |
| Observations | 119 | 119 | 119 | 119 | 119 | 119 |
| R-squared | 0.636 | 0.637 | 0.650 | 0.671 | 0.641 | 0.644 |
Notes: (1) The t value in parentheses is calculated by using the Chinese 7 major geographic regions level clustering robust standard error; (2) *, **, *** are significant at the 10 %, 5%, and 1% levels, respectively; (3) Samples in the table only include cities outside Hubei Province.
4.3. Discussion
4.3.1. Factors for city resilience against epidemic outbreak
In this paper, we test 3 hypotheses related to the factors for cities against COVID-19 pandemics in China. The findings for each hypothesis is shown below:
-
•
The first hypothesis (H1) is that the time that a city spent to contain the epidemic outbreak is longer when there is higher population inflow risk pressure from the first reported domestic epicenter to this city. The model results substantiate this intuitive hypothesis as 100 % increase in COVID-19 inflow risk pressure (population inflow from Wuhan as proportion of local population) postpones the average time for reaching epidemic plateau by 1.03–1.18 day. Our results also complement previous finding that closeness to the first epicenter (Wuhan) could be a significant independent predictor of the number of confirmed COVID-19 cases in Chinese cities (Liu, 2020). Though population inflow from Wuhan is obviously correlated with closeness to Wuhan, measuring inflow would more likely highlight the challenges of some megacities (such as Shanghai, Shenzhen, Beijing) that may not be geographically close to Wuhan but still have large amount of inter-city population mobility.
-
•
The second hypothesis (H2) is that the time that a city spent to contain the spread of epidemic is longer when the city has a large economic activity scale and a higher population density. The model results consistently validate this hypothesis as in all models higher volume of garbage treatment in a city prolongs the time to contain the disease case number. This provides empirical evidence for Lai et al. (2020) who argue that the difficulty in controlling infectious disease outbreak is much higher in large cities. In term of population density, the model results largely validate this hypothesis, except for the models that include GDP as control variables (in which case, the coefficients for density is not significant). Nonetheless, density or GDP can both represent intra-city mobility of social or economic activities, which could spur spread of infectious diseases (Dalziel, Pourbohloul, & Ellner, 2013). Thus, our findings can be seen as empirical evidence for Glaeser’s (2020) argument that density and urban proximity is usually deemed to “enable the spread of illness.” Hypothesis 1 and 2 highlight two aspects that highlight the challenges facing cities for pandemic control—inter- and intra-city mobility. Furthermore, when modeling the interaction term of higher population inflow risk pressure and population density, they contribute to marginal increase of disease control time effects of each other.
-
•
The third hypothesis (H3) is that the time that a city spent to contain the spread of epidemic is shorter when the city has a higher adequacy of healthcare facilities and previous pandemic disease experiences. This factor is arguably a more controllable factor by urban planning and governance. Our results, with various healthcare resource adequacy factors tested (including adequacy of medical practitioners, hospital beds, or composite index of healthcare infrastructure), consistently suggest that better healthcare resource adequacy can significant shorten the time for cities to contain the spread of epidemic. Increasing one doctor per patient shortens the time for reaching epidemic by around 0.012−0.013 days It echoes with previous research’s findings about critical importance of healthcare resource in mitigating the transmission risk of epidemic (Fang et al., 2012; Ji et al., 2020). However, we do not find any correlation between previous pandemic disease experience at the city-level and the time to contain the COVID-19 outbreak. It is likely that COVID-19 is much different to any past major epidemic, e.g. characterized with most infected cases are having mild symptoms or even symptomless.
In general, our results alarm the challenges of extended urbanization facing infectious diseases, echoing arguments by Connolly, Keil, and Ali (2020). From the perspective of human activities in cities, urbanization increases intra-city (related to the economy activity size and density variables) and inter-city mobility (related to the inflow risk pressure variable) (Dalziel et al., 2013), which are key drivers of infectious disease dynamics for cities. From the perspective of urban governance, healthcare infrastructure and governance capacity inadequacy in the fast-growing urbanization potentially increase vulnerability to infectious diseases in peri- or suburban areas (Connolly et al., 2020). The interaction term’s coefficients in our model show that increased adequacy of medical practitioners are still insufficient to address marginal increase in disease control difficulty for cities with large economic activity sizes.
The results of this study complement the current framework of urban resilience that mostly focus on environmental, socioeconomic, or natural disaster resilience (Shamsuddin, 2020; Zou et al., 2018). Especially, this study uses empirical data in a pandemic disaster to understand key Ex Ante factors for urban disaster resilience which includes urban economy activity size, population density, and healthcare infrastructure. On one hand, the results highlight key vulnerabilities of worldwide cities against pandemic disasters. On the other hand, the results of single indicators as well as their interactions provide basic data for resilience indicators for urban pandemic resilience. For example, our results show that increased adequacy of medical practitioners can mitigate pandemic disaster vulnerability in high density cities (shown by the negative coefficients for the interaction term), but cannot achieve the similar effects for large-scale economic activity. Moreover, how urban characteristics interplay with other socioeconomic factors (including poverty and income) that have strong influence on severety of outbreak and how these factors should be considered in urban planning, design and governance, are subject to future investigation (Das et al., 2021; Sannigrahi, Pilla, Basu, Basu, & Molter, 2020; Silva et al., 2021; Wang, 2021).
4.3.2. Takeaway for practice
Our results provide several takeaways for urban planning and governance practices. First, higher urban density has been recognized more sustainable development pattern as it saves land resource as well as associates with less carbon emissions per capita (Chen and Zhang, 2020; Egidi, Salvati, & Vinci, 2020; Yi, Dong, & Li, 2019). However, the principle of compact and smart urban planning and development needs to be re-evaluated due to its potential issues in pandemic control.
Second, adequacy of healthcare infrastructure has been shown to be the key determinants of city-level pandemic control during COVID-19 outbreak in China. Avoiding healthcare system collapse can avoid many more disease cases as well as economic losses (McKee & Stuckler, 2020). Healthcare resource demand during COVID-19 outbreak is increasingly enormous worldwide. Edejer et al. (2020) projected that the global healthcare cost estimate for the COVID-19 response in the status quo scenario was US$52·45 billion per month during the outbreak. Avoiding the burden during pandemics and conserving resources require intuiting early and comprehensive measures to improve city resilience for pandemic emergency governance. Furthermore, the most per capita disease burden and relative healthcare system demand may be highest away from major population centers, such as small cities and peri-urban areas (Connolly et al., 2020; Miller, Becker, Grenfell, & Metcalf, 2020).
Finally, our results also highlight the importance of urban governance capacity during pandemic disasters. Controlling inflow risk pressure from the epicenter are found to be a key factor for infectious disease control, while the epicenter cannot be predicted before the pandemic outbreak. Thus, controlling inter-city population flow during pandemics need not only immediate governance responses following health expert suggestions, but also coordination between multiple cities.
5. Conclusions
Based on China’s city-level data during the initial stage of COVID-19 pandemic outbreak, this study investigates the relationship between a city’s pandemic resilience and its affecting factors, including the inflow risk pressure of COVID-19 virus (population inflow from the epicenter), city agglomeration characteristics (urban population density and economic activity size), healthcare resource adequacy, and experience of local government in handling major epidemics. The results in this paper reveal that, while managing the import of virus inflow risk pressure is critical in determining a city’s pandemic resilience, city’s urban characteristics also matters.
Large and high-density cities with high inter and intra-city mobility flows have more difficulties in containing the epidemic spread. Healthcare infrastructure adequacy is the key for preparing for such disasters, while previous pandemic disease handling experiences do not factor into city resilience against COVID-19. On the other hand, economic activity size appears to as the major multiplier for inflow pressure and healthcare resource burden to postpone the control of COVID-19, as higher frequencies of travel and business meetings create more opportunities for the pandemics to spread. Cities with lower population density should also take caution as they are more sensitive to high inflow risk pressure due to the small cities’ lack of capacity in dealing with such pressure.
Although our analysis is based on the performance of Chinese cities in the case of COVID-19, the research framework is universally applicable and can be applied in understanding COVID-19 control performance of cities in other countries as well as control efficacy of other epidemics. It calls for more comprehensive understanding of urban resilience and sustainability framework especially for re-evaluation of factors including healthcare infrastructure, city size and population density. As density and city economic activity size have been found significant in this study, it is important to further understand their relationship between inter- and intra-city mobility. Mobility could be the key mechanism of accelerated infectious disease transmission and becomes a bliss-and-curse for global megacities. The use of new sources of big data, such as mobile phone and public transport check-in data, would make such research extensions possible.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
National Natural Science Foundation of China (NSFC71974125, NSFC52000130, NSFC71661137004, NSFC71573166); Shanghai Municipal Health Commission (GWV-9.4).
Footnotes
“Spring rush” or “Spring festival travel rush” is referring to the phenomena that Chinese would go back to their hometowns to reunite with their family members remaining there during the most important festival——spring festival, just like people in the western world do during the Christmas holiday. With billions of passengers travelled during the roughly 1.5 month season, it is arguably the largest-scale annual human migration of human being history (Hu, 2019).
Source: China’s Public Health Data Center http://www.phsciencedata.cn/Share/index.jsp.
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.scs.2021.102892.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Acuto M. COVID-19: Lessons for an urban (izing) world. One Earth. 2020;2(4):317–319. doi: 10.1016/j.oneear.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allenby B., Fink J. Toward inherently secure and resilient societies. Science. 2005;309(5737):1034–1036. doi: 10.1126/science.1111534. [DOI] [PubMed] [Google Scholar]
- Bauch C.T., Anand M. COVID-19: When should quarantine be enforced? The Lancet Infectious Diseases. 2020 doi: 10.1016/S1473-3099(20)30428-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beria P., Lunkar V. Presence and mobility of the population during the first wave of Covid-19 outbreak and lockdown in Italy. Sustainable Cities and Society. 2021;65 doi: 10.1016/j.scs.2020.102616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhadra A., Mukherjee A., Sarkar K. Impact of population density on Covid-19 infected and mortality rate in India. Modeling Earth Systems and Environment. 2020 doi: 10.1007/s40808-020-00984-7. https://link.springer.com/article/10.1007/s40808-020-00984-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biggs R., Schlüter M., Biggs D., Bohensky E.L., BurnSilver S., Cundill G.…West P.C. Toward principles for enhancing the resilience of ecosystem services. Annual Review of Environment and Resources. 2012;37(1):421–448. doi: 10.1146/annurev-environ-051211-123836. [DOI] [Google Scholar]
- Block P., Hoffman M., Raabe I.J., Dowd J.B., Rahal C., Kashyap R.…Mills M.C. Social network-based distancing strategies to flatten the COVID-19 curve in a post-lockdown world. Nature Human Behaviour. 2020;4:588–596. doi: 10.1038/s41562-020-0898-6. [DOI] [PubMed] [Google Scholar]
- Bootsma M.C.J., Ferguson N.M. The effect of public health measures on the 1918 influenza pandemic in U.S. cities. Proceedings of the National Academy of Sciences. 2007;104(18):7588–7593. doi: 10.1073/pnas.0611071104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cariolet J.M., Vuillet M., Diab Y. Mapping urban resilience to disasters–A review. Sustainable Cities and Society. 2019;51 [Google Scholar]
- Chen Y., Zhang D. Evaluation of city sustainability using multi-criteria decision-making considering interaction among criteria in Liaoning province China. Sustainable Cities and Society. 2020;59 doi: 10.1016/j.scs.2020.102211. [DOI] [Google Scholar]
- Chinazzi M., Davis J.T., Ajelli M., Gioannini C., Litvinova M., Merler S.…Vespignani A. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020 doi: 10.1126/science.aba9757. eaba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho S.Y., Kang J.-M., Ha Y.E., Park G.E., Lee J.Y., Ko J.-H.…Kim Y.-J. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: An epidemiological outbreak study. Lancet. 2016;388(10048):994–1001. doi: 10.1016/S0140-6736(16)30623-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu D.K., Akl E.A., Duda S., Solo K., Yaacoub S., Schünemann H.J.…Hajizadeh A. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet. 2020;395(10424):1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connolly C., Keil R., Ali S.H. Extended urbanisation and the spatialities of infectious disease: Demographic change, infrastructure and governance. Urban Studies. 2020 doi: 10.1177/0042098020910873. [DOI] [Google Scholar]
- Cutter S.L., Ash K.D., Emrich C.T. The geographies of community disaster resilience. Global Environmental Change Part A. 2014;29:65–77. doi: 10.1016/j.gloenvcha.2014.08.005. [DOI] [Google Scholar]
- Cutter S.L., Barnes L., Berry M., Burton C., Evans E., Tate E.…Webb J. A place-based model for understanding community resilience to natural disasters. Global Environmental Change Part A. 2008;18(4):598–606. doi: 10.1016/j.gloenvcha.2008.07.013. [DOI] [Google Scholar]
- Dalziel B.D., Pourbohloul B., Ellner S.P. Human mobility patterns predict divergent epidemic dynamics among cities. Proceedings of the Royal Society B: Biological Sciences. 2013;280(1766) doi: 10.1098/rspb.2013.0763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das A., Ghosh S., Das K., Basu T., Dutta I., Das M. Living environment matters: Unravelling the spatial clustering of COVID-19 hotspots in Kolkata megacity. India. Sustainable Cities and Society. 2021;65 doi: 10.1016/j.scs.2020.102577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edejer T.T.T., Hanssen O., Mirelman A., Verboom P., Lolong G., Watson O.J.…Soucat A. Projected health-care resource needs for an effective response to COVID-19 in 73 low-income and middle-income countries: A modelling study. The Lancet Global Health. 2020;8(11):e1372–e1379. doi: 10.1016/S2214-109X(20)30383-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egidi G., Salvati L., Vinci S. The long way to tipperary: City size and worldwide urban population trends, 1950–2030. Sustainable Cities and Society. 2020;60 doi: 10.1016/j.scs.2020.102148. [DOI] [Google Scholar]
- Fang L.-Q., Wang L.-P., Vlas S.J. de, Liang S., Tong S.-L., Li Y.-L.…Cao W.-C. Distribution and risk factors of 2009 pandemic influenza a (H1N1) in Mainland China. American Journal of Epidemiology. 2012;175(9):890–897. doi: 10.1093/aje/kwr411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fastiggi M., Meerow S., Miller T.R. Governing urban resilience: Organisational structures and coordination strategies in 20 North American city governments. Urban Studies. 2020 doi: 10.1177/0042098020907277. [DOI] [Google Scholar]
- Florida R. 2020. The geography of coronavirus.https://www.citylab.com/equity/2020/04/coronavirus-spread-map-city-urban-density-suburbs-rural-data/609394/ Retrieved April 3, 2020, from CityLab website: [Google Scholar]
- Glaeser E.L. Cities and pandemics: A long history. City Journal. 2020 https://www.city-journal.org/cities-and-pandemics-have-long-history Retrieved from. [Google Scholar]
- Godschalk D.R. Urban hazard mitigation: Creating resilient cities. Natural Hazards Review. 2003;4(3):136–143. doi: 10.1061/(ASCE)1527-6988(2003)4:3(136). [DOI] [Google Scholar]
- Hernantes J., Maraña P., Gimenez R., Sarriegi J.M., Labaka L. Towards resilient cities: A maturity model for operationalizing resilience. Cities. 2019;84(1):96–103. doi: 10.1016/j.cities.2018.07.010. [DOI] [Google Scholar]
- Holling C.S. Resilience and stability of ecological systems. Annual Review of Ecology and Systematics. 1973;4(1):1–23. doi: 10.1146/annurev.es.04.110173.000245. (1973) [DOI] [Google Scholar]
- Hu M. Visualizing the largest annual human migration during the Spring Festival travel season in China. Environment and Planning A: Economy and Space. 2019;51(8):1618–1621. doi: 10.1177/0308518X19845908. [DOI] [Google Scholar]
- Ji Y., Ma Z., Peppelenbosch M.P., Pan Q. Potential association between COVID-19 mortality and health-care resource availability. The Lancet Global Health. 2020;8(4):e480. doi: 10.1016/S2214-109X(20)30068-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia J.S., Lu X., Yuan Y., Xu G., Jia J., Christakis N.A. Population flow drives spatio-temporal distribution of COVID-19 in China. Nature. 2020 doi: 10.1038/s41586-020-2284-y. [DOI] [PubMed] [Google Scholar]
- Jones K.E., Patel N.G., Levy M.A., Storeygard A., Balk D., Gittleman J.L.…Daszak P. Global trends in emerging infectious diseases. Nature. 2008;451:990–993. doi: 10.1038/nature06536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jovanović A., Klimek P., Renn O., Schneider R., Øien K., Brown J.…Rosen T. Assessing resilience of healthcare infrastructure exposed to COVID-19: Emerging risks, resilience indicators, interdependencies and international standards. Environment Systems & Decisions. 2020:1–35. doi: 10.1007/s10669-020-09779-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer M.U.G., Yang C.-H., Gutierrez B., Wu C.-H., Klein B., Pigott D.M.…Scarpino S.V. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020 doi: 10.1126/science.abb4218. eabb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruk M.E., Ling E.J., Bitton A., Cammett M., Cavanaugh K., Chopra M.…Warnken H. Building resilient health systems: A proposal for a resilience index. BMJ. 2017 doi: 10.1136/bmj.j2323. j2323. [DOI] [PubMed] [Google Scholar]
- Kupferschmidt K., Cohen J. Can China’s COVID-19 strategy work elsewhere? Science. 2020;367(6482):1061–1062. doi: 10.1126/science.367.6482.1061. [DOI] [PubMed] [Google Scholar]
- Lai K.Y., Webster C., Kumari S., Sarkar C. The nature of cities and the Covid-19 pandemic. Current Opinion in Environmental Sustainability. 2020;46:27–31. doi: 10.1016/j.cosust.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee V.J., Aguilera X., Heymann D.L., Wilder-Smith A., Lee V.J., Aguilera X.…Yeo W.Q. Preparedness for emerging epidemic threats: A lancet infectious diseases commission. The Lancet Infectious Diseases. 2020;20(1):17–19. doi: 10.1016/S1473-3099(19)30674-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L. Emerging study on the transmission of the Novel Coronavirus (COVID-19) from urban perspective: Evidence from China. Cities. 2020;103 doi: 10.1016/j.cities.2020.102759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCloskey B., Dar O., Zumla A., Heymann D.L. Emerging infectious diseases and pandemic potential: Status quo and reducing risk of global spread. The Lancet Infectious Diseases. 2014;14(10):1001–1010. doi: 10.1016/S1473-3099(14)70846-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCloskey B., Zumla A., Ippolito G., Blumberg L., Arbon P., Cicero A.…Borodina M. Mass gathering events and reducing further global spread of COVID-19: A political and public health dilemma. Lancet. 2020;395(10230):1096–1099. doi: 10.1016/S0140-6736(20)30681-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee M., Stuckler D. If the world fails to protect the economy, COVID-19 will damage health not just now but also in the future. Nature Medicine. 2020;26(5):640–642. doi: 10.1038/s41591-020-0863-y. [DOI] [PubMed] [Google Scholar]
- Meerow S., Newell J.P., Stults M. Defining urban resilience: A review. Landscape and Urban Planning. 2016;147:38–49. doi: 10.1016/j.landurbplan.2015.11.011. [DOI] [Google Scholar]
- Metsky H.C., Matranga C.B., Wohl S., Schaffner S.F., Freije C.A., Winnicki S.M.…Sabeti P.C. Zika virus evolution and spread in the Americas. Nature. 2017;546(7658):411–415. doi: 10.1038/nature22402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller I.F., Becker A.D., Grenfell B.T., Metcalf C.J.E. Disease and healthcare burden of COVID-19 in the United States. Nature Medicine. 2020;26(8):1212–1217. doi: 10.1038/s41591-020-0952-y. [DOI] [PubMed] [Google Scholar]
- Mishra S.V., Gayen A., Haque S.M. COVID-19 and urban vulnerability in India. Habitat International. 2020;103 doi: 10.1016/j.habitatint.2020.102230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHCC . 2020. The NHCC’s daily briefing webiste of COVID-19 in China.http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml Retrieved June 25, 2020, from The Official Website of National Health Commission of China (NHCC) website: [Google Scholar]
- Ni P., Li B. National Academy of Economic Strategy, Research Center for City and Competitiveness in Chinese Academy of Social Sciences; Beijing: 2020. Special report on the environmental competitiveness of China’s urban medical hardware: China’s urban medical resources and service capabilities under the impact of COVID-19. [Google Scholar]
- OECD . The website of OECD. 2020. AI-powered COVID-19 watch.https://oecd.ai/covid Retrieved from. [Google Scholar]
- Peak C.M., Kahn R., Grad Y.H., Childs L.M., Li R., Lipsitch M.…Buckee C.O. Individual quarantine versus active monitoring of contacts for the mitigation of COVID-19: A modelling study. The Lancet Infectious Diseases. 2020 doi: 10.1016/S1473-3099(20)30361-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters D.J. Community susceptibility and resiliency to COVID‐19 across the rural‐urban continuum in the United States. The Journal of Rural Health. 2020;36(3):446–456. doi: 10.1111/jrh.12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prashar S., Shaw R., Takeuchi Y. Assessing the resilience of Delhi to climate-related disasters: A comprehensive approach. Natural Hazards. 2012;64(2):1609–1624. doi: 10.1007/s11069-012-0320-4. [DOI] [Google Scholar]
- Qiang Y., Huang Q., Xu J. Observing community resilience from space: Using nighttime lights to model economic disturbance and recovery pattern in natural disaster. Sustainable Cities and Society. 2020;57:102115. [Google Scholar]
- Qiu Y., Chen X., Shi W. Impacts of social and economic factors on the transmission of coronavirus disease 2019 (COVID-19) in China. Journal of Population Economics. 2020 doi: 10.1007/s00148-020-00778-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro P.J.G., Gonçalves L.A.P.J. Urban resilience: A conceptual framework. Sustainable Cities and Society. 2019;50 [Google Scholar]
- Rus K., Kilar V., Koren D. Resilience assessment of complex urban systems to natural disasters: A new literature review. International Journal of Disaster Risk Reduction. 2018;31:311–330. [Google Scholar]
- Sannigrahi S., Pilla F., Basu B., Basu A.S., Molter A. Examining the association between socio-demographic composition and COVID-19 fatalities in the European region using spatial regression approach. Sustainable Cities and Society. 2020;62 doi: 10.1016/j.scs.2020.102418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott M. Covid-19, place-making and health. Planning Theory & Practice. 2020;21(3):343–348. doi: 10.1080/14649357.2020.1781445. [DOI] [Google Scholar]
- Shamsuddin S. Resilience resistance: The challenges and implications of urban resilience implementation. Cities. 2020;103 doi: 10.1016/j.cities.2020.102763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherrieb K., Norris F.H., Galea S. Measuring capacities for community resilience. Social Indicators Research. 2010;99(2):227–247. doi: 10.1007/s11205-010-9576-9. [DOI] [Google Scholar]
- Silva J.C.S., de Lima Silva D.F., Neto A.D.S.D., Ferraz A., Melo J.L., Júnior N.R.F.…de Almeida Filho A.T. A city cluster risk-based approach for Sars-CoV-2 and isolation barriers based on anonymized mobile phone users’ location data. Sustainable Cities and Society. 2021;65 doi: 10.1016/j.scs.2020.102574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Z., Zhang H., Yang Y., Wan H., Wang Y. Impacts of geographic factors and population density on the COVID-19 spreading under the lockdown policies of China. The Science of the Total Environment. 2020;746 doi: 10.1016/j.scitotenv.2020.141347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang L., Bie B., Park S.-E., Zhi D. Social media and outbreaks of emerging infectious diseases: A systematic review of literature. American Journal of Infection Control. 2018;46(9):962–972. doi: 10.1016/j.ajic.2018.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Lancet COVID-19: Fighting panic with information. Lancet. 2020;395(10224):537. doi: 10.1016/S0140-6736(20)30379-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Lancet COVID-19: Learning from experience. Lancet. 2020;395(10229):1011. doi: 10.1016/S0140-6736(20)30686-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian H., Liu Y., Li Y., Wu C.-H., Chen B., Kraemer M.U.G.…Dye C. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020 doi: 10.1126/science.abb6105. eabb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner B.L., Kasperson R.E., Matson P.A., McCarthy J.J., Corell R.W., Christensen L.…Schiller A. A framework for vulnerability analysis in sustainability science. Proceedings of the National Academy of Sciences. 2003;100(14):8074–8079. doi: 10.1073/pnas.1231335100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J. Vision of China’s future urban construction reform: In the perspective of comprehensive prevention and control for multi disasters. Sustainable Cities and Society. 2021;64 doi: 10.1016/j.scs.2020.102511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardekker A., Wilk B., Brown V., Uittenbroek C., Mees H., Driessen P.…Runhaar H. A diagnostic tool for supporting policymaking on urban resilience. Cities. 2020;101 doi: 10.1016/j.cities.2020.102691. [DOI] [Google Scholar]
- WHO . Vol. 2019. 2020. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19)https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf (WHO website). Retrieved from. [Google Scholar]
- WHO . 2020. WHO collection for Coronavirus disease (COVID-19) outbreak.https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Retrieved June 15, 2020, from WHO Website website: [Google Scholar]
- Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: Pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. Journal of Travel Medicine. 2020;27(2):1–4. doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi P., Dong Q., Li W. Evaluation of city sustainability using the deviation maximization method. Sustainable Cities and Society. 2019;50 doi: 10.1016/j.scs.2019.101529. [DOI] [Google Scholar]
- Zarocostas J. How to fight an infodemic. Lancet. 2020;395(10225):676. doi: 10.1016/S0140-6736(20)30461-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou H., Wan J., Jia H. Resilience to natural hazards: A geographic perspective. Natural Hazards. 2010;53(1):21–41. [Google Scholar]
- Zhu S., Li D., Feng H. Is smart city resilient? Evidence from China. Sustainable Cities and Society. 2019;50 [Google Scholar]
- Zou L., Lam N.S.N., Cai H., Qiang Y. Mining twitter data for improved understanding of disaster resilience. Annals of the American Association of Geographers. 2018;108(5):1422–1441. doi: 10.1080/24694452.2017.1421897. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.