Abstract
Rationale: How to provide advanced respiratory support for coronavirus disease (COVID-19) to maximize population-level survival while optimizing mechanical ventilator access is unknown.
Objectives: To evaluate the use of high-flow nasal cannula for COVID-19 on population-level mortality and ventilator availability.
Methods: We constructed dynamical (deterministic) simulation models of high-flow nasal cannula and mechanical ventilation use for COVID-19 in the United States. Model parameters were estimated through consensus based on published literature, local data, and experience. We had the following two outcomes: 1) cumulative number of deaths and 2) days without any available ventilators. We assessed the impact of various policies for the use of high-flow nasal cannula (with or without “early intubation”) versus a scenario in which high-flow nasal cannula was unavailable.
Results: The policy associated with the fewest deaths and the least time without available ventilators combined the use of high-flow nasal cannula for patients not urgently needing ventilators with the use of early mechanical ventilation for these patients when at least 10% of ventilator supply was not in use. At the national level, this strategy resulted in 10,000–40,000 fewer deaths than if high-flow nasal cannula were not available. In addition, with moderate national ventilator capacity (30,000–45,000 ventilators), this strategy led to up to 25 (11.8%) fewer days without available ventilators. For a 250-bed hospital with 100 mechanical ventilators, the availability of 13, 20, or 33 high-flow nasal cannulas prevented 81, 102, and 130 deaths, respectively.
Conclusions: The use of high-flow nasal cannula coupled with early mechanical ventilation when supply is sufficient results in fewer deaths and greater ventilator availability.
Keywords: high-flow nasal cannula, mechanical ventilation, COVID-19, simulation
As of August 25, 2020, the global pandemic caused by coronavirus disease (COVID-19) has resulted in more than 23 million persons known to be infected (1). The sickest require hospitalization, and of those, 8–33% require invasive mechanical ventilation (MV) for COVID-19–associated respiratory failure (2–4). Such demand for MV has prompted many institutions, professional organizations, and governments to think “outside the box” to try to expand access to MV by repurposing machines not typically used for MV (e.g., noninvasive ventilator machines and anesthesia machines) (5–7), calling on companies not normally in the business of making ventilators to assist in manufacturing (8), and even using a single ventilator to provide MV to more than one patient simultaneously (9).
Another potential solution being employed in many hospitals is the use of high-flow nasal cannula (HFNC). Before COVID-19, HFNC was found to reduce the need for MV in hypoxemic respiratory failure (10–15) and reintubation (replacement on MV) for patients liberated from MV if used prophylactically after extubation (15–17). Indeed, HFNC is recommended in guidelines on management of patients with COVID-19 and acute respiratory failure (18–20). However, the use of HFNC may potentially delay MV for patients who will ultimately need MV and, in this subgroup, has been associated with higher mortality than early MV (21). Moreover, both HFNC and MV supplies may be constrained if volume of patients with COVID-19 is high. How the use of HFNC impacts patient outcomes and resource use and how to optimally use HFNC and MV, therefore, is not straightforward and may vary by local resource availability.
In this study, we sought to evaluate the impact of differing strategies to allocate HFNC and MV on 1) hospital mortality of patients with COVID-19–associated hypoxemic respiratory failure and 2) MV availability (i.e., MV demand relative to supply) through simulation. Understanding this interplay can help inform hospital, health-system, and even regional or national recommendations on how to best deploy these two respiratory support technologies.
Methods
We conducted a simulation study of HFNC and MV use for patients hospitalized with COVID-19. The simulation model is a deterministic dynamical system that captures the underlying patient flow and resource allocation dynamics of the system. This type of modeling approach has been prevalently applied in healthcare management, including the well-known SIR (Susceptible, Infected, or Recovered) model developed for pandemic evolution (22). The institutional review board at Albert Einstein College of Medicine approved this study (#2020–11803).
Model Description
Our model was limited to hypoxemic patients “at risk for needing MV,” conceptualized as requiring ≥6 L nasal cannula to maintain adequate oxygenation (independent of need for intensive care unit admission). Patients on a ventilator before hospital admission were not considered. Noninvasive positive pressure ventilation (NIPPV) was not considered in the model for the following three reasons: 1) expert clinical guidelines for management of COVID-19 acute respiratory failure recommend use of HFNC over NIPPV and the use of NIPPV only if HFNC is not available (18–20); 2) at the limits of resource availability, NIPPV machines may be repurposed to provide MV (making them unavailable to provide NIPPV); and 3) for simplicity to allow us to focus on the relationship between HFNC and MV use.
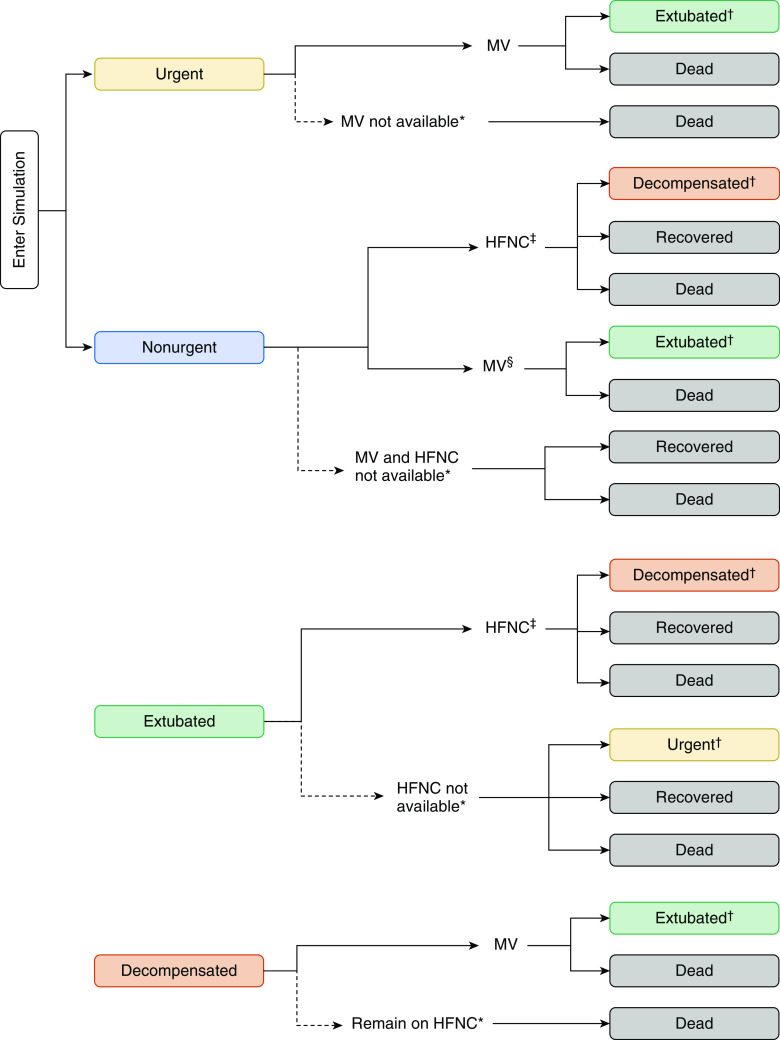
In this model (Figure 1), we first classified patients on the basis of clinical need for advanced respiratory support. Patients were stratified on entry into the simulation as “urgent” or “nonurgent.” Urgent was defined as needing MV imminently (HFNC would be insufficient) to avert death; nonurgent patients were those clinicians would believe are at high risk of needing MV but do not need it urgently (akin to those enrolled in trials of HFNC pre-MV). After initial respiratory support with MV, patients could be further categorized as “extubated” if they improved sufficiently to be liberated from MV. Nonurgent patients initially receiving HFNC could be recategorized as “decompensated” if they worsened while on HFNC and needed MV imminently. These distinctions were necessary as the rates of recovery, decompensation, and death varied across them.
Figure 1.
Model diagram of patient flow. Dotted lines represent choices made when advanced respiratory support is not available. *Able to receive advanced support available to the patient type (mechanical ventilation and/or high-flow nasal cannula) if becomes available. †Jump to new pathway. ‡For scenarios in which HFNC is available. §This state represents “early intubation” for scenarios in which it is available. HFNC = high-flow nasal cannula; MV = mechanical ventilation.
Patients from each clinical group above could receive one of the following three respiratory support modalities: HFNC, MV, or neither (if, as appropriate, HFNC or MV were not available). Urgent patients required MV immediately; if MV was unavailable, they died quickly. Nonurgent patients could obtain either HFNC or MV; if neither HFNC nor MV were available, they could remain on neither for some time before they either recovered, died, or deteriorated and became urgent patients. Finally, extubated patients were preferentially placed on HFNC (15–17, 23) but could be placed on regular oxygen if HFNC was not available.
Patients could exit the simulation as either recovered or dead. Recovered patients represented those who were at risk of respiratory failure and who survived to hospital discharge. Dead patients were those who were at risk of respiratory failure and did not survive to hospital discharge (even if their death was unrelated to respiratory failure). Our model did not pertain to patients who are not at risk of respiratory failure.
Model Inputs
Model parameters (Table 1) were estimated by consensus of the clinician authors informed by available literature for non–COVID-19 acute hypoxemic respiratory failure, national data for COVID-19 (24), and data from the care of patients with COVID-19 admitted to Montefiore Medical Center in the Bronx, New York, from March 17 to March 30, 2020. Montefiore is an urban academic healthcare system with three main hospitals, including a quaternary care center (usually 726 hospital beds), a tertiary care center (usually 431 hospital beds), and a community center (usually 360 hospital beds). During the time of data acquisition at Montefiore, the rate and duration of HFNC and MV use may have been impacted by resource constraints, and absolute survival rates were still unknown (as many patients remained hospitalized). Thus, these data were only used to inform estimates. Point estimates were used as the primary parameter estimate in each simulation; simulations were then replicated 100 times each with parameter estimates randomly drawn from within the range provided in Table 1 (assuming a truncated normal distribution with mean equal to the point estimate and standard deviation equal to half the width of the range) to create a credible range of model outputs.
Table 1.
Model parameter estimates
| Parameter | Point Estimate | Range* | Montefiore Value | Literature References |
|---|---|---|---|---|
| Proportion urgent patients, % | 33 | 16–50 | 67.3† | 34–40‡ (42, 43) |
| Probability of death, % | ||||
| Not HFNC/MV | ||||
| Nonurgent | 5 | 2–8 | 4 | 6.8–27.7§ (10–12, 14, 33, 34, 44) |
| Extubated | 10 | 6–14 | 12.5 | 2.5–6.2§ (16, 17, 23) |
| HFNC | ||||
| Nonurgent | 4 | 2–6 | 10.3 | 6.0–25.9§ (10–14, 33, 34, 44) |
| Extubated | 8 | 4–12 | 0‖ | 2.8–5.3§ (16, 17, 23) |
| MV | ||||
| Nonurgent | 15 | 10–20 | 44 | 33–40§ (43, 45) |
| Urgent | 50 | 45–55 | ||
| Decompensated | 60 | 55–65 | 60 | 38§ (45) |
| Probability of deterioration, % | ||||
| Not HFNC/MV | ||||
| Nonurgent | 65 | 55–75 | 30 | 11.2–29.2 (10–12, 14, 33, 34, 44) |
| Extubated | 15 | 10–20 | 28.1 | 8.1–15.9 (15–17, 23, 44, 46) |
| HFNC | ||||
| Nonurgent | 45 | 35–55 | 44.3 | 7.0–24.3 (10–14, 33, 34, 44, 45) |
| Extubated | 7.5 | 5–10 | 35.7 | 4.3–7.5 (15–17, 23, 47, 48) |
| Time in state before transition to next state | ||||
| Not HFNC/MV | ||||
| Nonurgent | 20 h | 15 h–25 h | 20.6 h (10.9 h–55.2 h)¶ | 15 h (5 h–39 h)¶** (44) |
| Urgent | 1 h | 0.5 h–2 h | n/a†† | — |
| Extubated | 12 h | 8 h–16 h | 1.7 h (0.1 h–14.4 h)¶ | — |
| HFNC | ||||
| Nonurgent | 48 h | 24 h–72 h | 23.7 h (8.1 h–59.0 h)¶ | 27 h (8 h–46 h)¶** (44) |
| Extubated | 18 h | 10–26 h | 18.6 h (10.1 h–35.6 h)¶ | 19 h¶** (47, 48) |
| Decompensated | 15 h | 10 h–20 h | 18.8 h (7.7 h–44.7 h)¶ | — |
| MV | ||||
| Nonurgent | 120 h (5 d) | 72 h–168 h (3–7 d) | 63.5 h (30.0 h–111.9 h)¶ | 8 d (4 d–16 d)¶** (43) |
| Urgent | 240 h (10 d) | 192 h–288 h (8–12 d) | ||
| Decompensated | 288 h (12 d) | 240 h–336 h (10–14 d) | 78.0 h (21.1 h–138.1 h)¶ | — |
Definition of abbreviations: COVID-19 = coronavirus disease; HFNC = high-flow nasal cannula; MV = mechanical ventilation; n/a = not applicable.
For sensitivity analysis, each parameter is assumed to follow a truncated normal distribution, whose mean is equal to the point estimate and whose standard deviation is equal to half width of the range.
Initial support MV (of all patients ultimately requiring HFNC or MV).
No exact data available in the literature; ∼40% of non–COVID-19 acute respiratory distress syndrome develops within 48 hours of hospitalization, suggesting not all is “urgent;” ∼34% of acute respiratory failure receive MV on hospital Day 1.
Includes intensive care unit, hospital, and 28-day mortality as reported by individual studies.
Few patients extubated to HFNC who had hospital outcome determined (alive/dead) at time of analysis.
Median (interquartile range).
Time to reintubation only (not time to all “next states” combined).
Defined as patients who would not survive long without MV.
The arrival rates of patients (i.e., demand pattern) were derived from retrospective and predicted mortality data. Detailed methodology to derive the arrival rate is provided in the online supplement. The arrival rates were derived primarily from estimates from the Institute for Health Metrics and Evaluation at University of Washington (24). To check the robustness of the results to different demand patterns, results were compared across arrival rates derived from two additional projection models (24–26).
Outcomes
We had the following two coprimary outcomes: 1) the cumulative number of deaths and 2) MV unavailability, quantified as days without any available MV (i.e., all are in use). The number of deaths represents the number of patients who were at risk for needing MV at some point during their hospital stay and did not survive to hospital discharge (including deaths not related to respiratory failure).
Resource Allocation Strategies
We considered a restrictive (base case) strategy in which HFNC was not available for any patients and MV was only available for urgent patients. In this scenario, nonurgent patients remained without any advanced support—HFNC or MV—unless they deteriorated and became urgent; we termed this policy “no HFNC” (Table E1 in the online supplement).
In addition to the restrictive strategy, we considered a series of policies allowing for more liberal use of HFNC and MV. First, we allowed HFNC for both extubated and nonurgent patients; we considered prioritization of HFNC for extubated (HFNCext) or nonurgent (HFNCnonurg) patients in two separate scenarios. Second, we considered policies promoting “early intubation” (19, 27) by providing MV to nonurgent patients when available MV supply exceeded a threshold (MV20 denoted ≥20% of total MV capacity, and MV10 denoted ≥10%). In these scenarios, nonurgent patients received MV preferentially over HFNC. This resulted in consideration of the following six additional policies: no HFNC + MV20; HFNCext + MV20; HFNCnonurg + MV20; no HFNC + MV10; HFNCext + MV10; and HFNCnonurg + MV10. In all cases, access to MV was prioritized for urgent patients over those clinically decompensated on HFNC.
Simulated Scenarios
We modeled the outbreak from February 4, 2020, through November 1, 2020 (in line with Institute for Health Metrics and Evaluation models) (24).
First, we simulated the impact of each resource allocation strategy at the national level. We allowed MV availability to range from 3,000–60,000 ventilators (28, 29), and, we considered HFNC capacity in ratios of MV:HFNC of 3:1, 5:1, and 8:1. We then focused on major cities that were substantially impacted by COVID-19 (Detroit, Miami, New Orleans, New York City, and Phoenix). Because the exact number of ventilators available in each city was not readily attainable, we estimated that each city had access to a fraction of the corresponding state’s MV supply (30), in which the proportion was equal to the city:state cumulated deaths ratio (as of August 2, 2020; see online supplement). As a robustness check, we also conducted analyses across varying levels of ventilator supply in each city. The policy associated with the fewest deaths across these scenarios was identified as the recommended policy.
We then focused on a more local, hospital-based view. First, we compared the recommended policy with the most restrictive policy (no HFNC) across hospitals of several sizes (100, 250, 500, and 1,000 beds); in each hospital, various MV and HFNC capacity levels were analyzed (MV: 25, 50, 100, 150, 200, and 250; MV:HFNC ratio: 3:1, 5:1, and 8:1). Second, to understand the circumstances necessary for HFNC use to be beneficial, we conducted a series of tipping-point experiments in which we considered a range of possible values for the following two critical parameters: 1) the probability of decompensation of nonurgent patients on HFNC and 2) the excess duration of MV for nonurgent patients who decompensated and required MV (vs. direct placement on MV). For this analysis, we considered a 250-bed hospital with 100 mechanical ventilators and 20 HFNC (5:1 ratio).
Lastly, we assessed the robustness of the performance of the recommended policy compared with no HFNC to variations in all parameter estimates over their full ranges in Table 1.
All simulations were performed using python. For reproducibility purposes, we have made the code and data openly available via https://github.com/YueHu-CU/Use-of-HFNC-in-COVID-19.
Results
National Scale
The number of cumulative deaths decreased for all strategies as MV capacity increased until MV availability was plentiful (Figures 2 and E1). Overall mortality decreased with HFNC use; the magnitude of this effect was heightened when HFNC capacity was greater. HFNCext + MV10 and HFNCnonurg + MV10 consistently outperformed other policies, resulting in up to 20,000–80,000 fewer deaths than no HFNC. HFNCext + MV10 was identified as the recommended policy.
Figure 2.
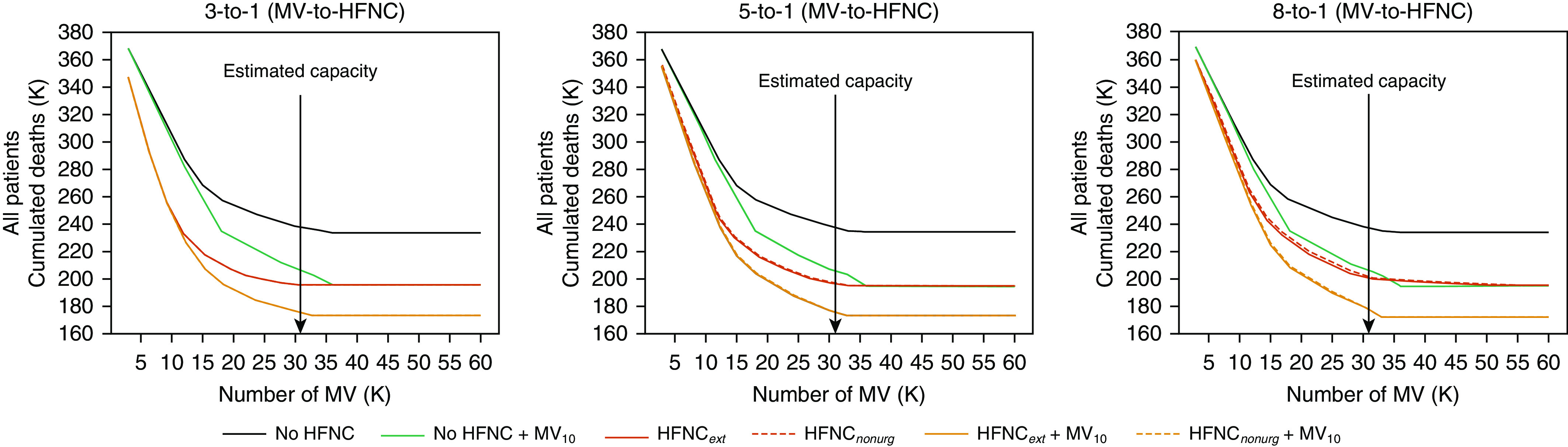
Impact of use of high-flow nasal cannula on mortality in the United States. MV available for nonurgent patients as “early intubation” when ≥20% of total MV capacity is available scenarios are not included on plots for simplicity; in general, they performed less well than equivalent MV10 scenarios. HFNC = high-flow nasal cannula; HFNCext = HFNC prioritized for extubated (over nonurgent) patients; HFNCnonurg = HFNC prioritized for nonurgent (over extubated) patients; MV = mechanical ventilation; MV10 = MV available for nonurgent patients as “early intubation” when ≥10% of total MV capacity is available.
The eight policies were practically indistinguishable in terms of MV use when MV capacity was either limited (e.g., ≤20,000) or abundant (≥40,000; Figure E2); with an MV capacity of 20,000, there were 43 days (15.7%) during the epidemic with no available MV. With midrange MV capacity (25,000–35,000), HFNCext + MV10 had notably fewer days with no MV available—up to 25 days—compared with no HFNC. No meaningful difference was observed in MV use between HFNC use preferentially before intubation (HFNCnonurg) or after extubation (HFNCext).
Identical directional trends with small variations in the magnitude of cumulative lives saved and reduction in days without MV were obtained using two alternative prediction models (Figures E3–E5).
Regional Scale
Similar to the national scale, HFNCext + MV10 consistently resulted in the fewest deaths in each city (Figure E6). With an MV:HFNC ratio of 5:1, HFNCext + MV10 averted 319 deaths in Detroit, 1,033 deaths in Miami, 3,094 deaths in New York City, 200 deaths in New Orleans, and 1,088 deaths in Phoenix. Moreover, HFNCext + MV10 reduced the period with no available MV by 5 days in Detroit, 14 days in Miami, 7 days in New York City, 8 days in New Orleans, and 9 days in Phoenix (Table 2). In all cities, the difference between HFNCext + MV20 and HFNCext + MV10 in terms of MV use was barely distinguishable (data not shown).
Table 2.
Impact of use of recommended policy on mortality in major cities
| City | Cumulative Deaths |
Days with No Available MV |
||||
|---|---|---|---|---|---|---|
| No HFNC* | HFNCext + MV10† | Difference | No HFNC* | HFNCext + MV10† | Difference | |
| Detroit | 1,710 | 1,391 | −319 | 34 | 29 | −5 |
| Miami | 4,763 | 3,730 | −1,033 | 49 | 35 | −14 |
| New Orleans | 856 | 656 | −200 | 32 | 24 | −8 |
| New York City | 24,843 | 21,749 | −3,094 | 41 | 37 | −7 |
| Phoenix | 6,086 | 4,998 | −1,088 | 57 | 48 | −9 |
Definition of abbreviations: HFNC = high-flow nasal cannula; MV = mechanical ventilation.
No HFNC = HFNC was not available for any patients, and MV was only available for urgent patients.
HFNCext + MV10 = HFNC for nonurgent and extubated patients (extubated prioritized) with MV for nonurgent patients as “early intubation” when ≥10% of total MV capacity is available.
Hospital Level
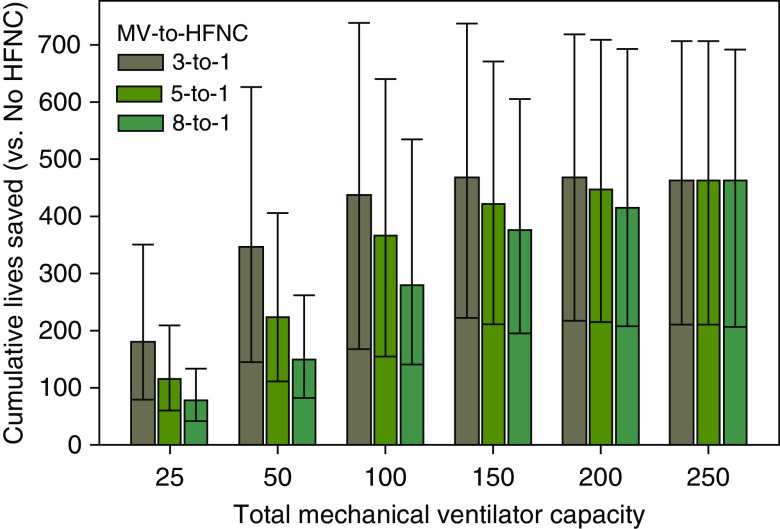
At the hospital level, HFNCext + MV10 consistently led to fewer deaths than no HFNC. For example, in a 250-bed hospital with capacity for 100 MV and 20 HFNC (5:1 ratio), 367 deaths were avoided (Figures 3 and E7). Greater relative availability of HFNC resulted in more lives saved (281 for 8:1 and 439 for 3:1), yet the magnitude of this difference in lives saved decreased with greater MV availability. For fixed bed:MV:HFNC ratios, the number of lives saved increased proportionally to the hospital size (Figure E8).
Figure 3.
Impact of use of recommended policy on mortality across hospital scenarios with differing resource constraints. Modeled using a 250 bed hospital; comparing recommended policy, HFNCext + MV10 (HFNC for nonurgent and extubated patients [extubated prioritized] with MV for nonurgent patients as “early intubation” when ≥10% of total MV capacity is available), versus restrictive policy, No HFNC (HFNC was not available for any patients and MV was only available for urgent patients). Columns = point estimates based on point estimates for parameters from Table 1; bars = the 95% credible range (2.5%–97.5% percentile) of performance derived from 100 simulations using parameters randomly sampled from their full range, assuming a truncated normal distribution whose mean is equal to the point estimate and whose standard deviation is equal to half the width of the range (Table 1). HFNC = high flow nasal cannula; MV = mechanical ventilation.
Time with no MV available under no HFNC ranged from 0 to 224 days depending on the hospital environment. HFNCext + MV10 resulted in shorter durations (a reduction of 4–64 d) of full MV use.
Tipping Points
As the probability of decompensation and the excess duration of MV upon decompensation increased, the reduction in number of deaths of HFNCext + MV10 over no HFNC decreased (Figure E9A). In the case with 0.35 probability of decompensation and 5 days excess MV duration upon decompensation, HFNCext + MV10 averted 466 deaths when compared with no HFNC for a 250-bed hospital with 100 MV and 20 HFNC (5:1 ratio). However, in an extreme scenario (0.7 probability of decompensation and 15 d excess MV duration upon decompensation), HFNCext + MV10 resulted in 86 more deaths when compared with no HFNC. Similarly, the number of days with no MV available was not consistently decreased by use of HFNCext + MV10 (Figure E9B). When the probability of decompensation and excess MV duration were small, HFNCext + MV10 reduced time without MV availability by up to 88 days; however, with higher likelihoods of decompensation and/or longer MV durations for those who decompensated, HFNCext + MV10 led to up to 56 additional days without MV availability.
Sensitivity Analysis
In a series of simulations using the full ranges of parameter estimates, HFNCext + MV10 always resulted in fewer deaths than no HFNC across the credible ranges of performance, although the reduction magnitude varied (Table E2). The impact of HFNCext + MV10 on MV use was less consistently positive.
Discussion
Our simulations suggest that at the national, regional, and hospital levels, the use of HFNC for patients with respiratory failure due to COVID-19 will result in increased population-level survival and increased availability of mechanical ventilators across almost all scenarios. Moreover, we found that adding an early intubation strategy to HFNC when there is at least 10% ventilator supply not in use can save lives without significantly decreasing systemwide MV availability. Notably, the use of an early intubation strategy without the use of HFNC provided less mortality benefit than using HFNC alone unless MV capacity was very high (greater than 40,000 nationally). Finally, across plausible ranges of both risk of decompensating on HFNC and excess days of MV for those who decompensated, use of HFNC resulted in at least a reduction of 1.6 days (0.6% of d) with no available MV.
Our findings suggest that it is of paramount importance for clinicians to gain comfort with HFNC. Moreover, administrators and policymakers must consider amending protocols to not only allow, but actually advocate for, the use of HFNC for patients with COVID-19 with significant hypoxemia who, without this option, would be placed on MV. Much press has appropriately surrounded concerns over insufficient MV capacity (31, 32). Relatively little light has been shown on capacity constraints for HFNC, however. Institutions should consider acquiring more HFNC set-ups, which, anecdotally, exist in far fewer numbers than ventilators at most hospitals.
The value of HFNC for use in acute hypoxemic respiratory failure (unrelated to COVID-19) has been extensively studied. Of eight meta-analyses published since 2017, five concluded that HFNC was associated with reduced rates of MV compared with conventional oxygen therapy or NIPPV in the setting of acute hypoxemic respiratory failure (10, 12, 14, 15, 33), whereas the remaining three found no difference in the rates of subsequent MV (11, 13, 34). Those meta-analyses that evaluated death consistently found no difference with the use of HFNC (10, 11, 13, 33, 34). Four meta-analyses evaluated the use of HFNC after liberation from MV (15–17, 23); all but one demonstrated a reduction in the need for reintubation and reinitiation of MV (23). No meta-analysis of HFNC use, either before or after MV, found HFNC to be associated with worse outcomes.
Use of HFNC in patients without COVID-19 is likely less common than the evidence would suggest it should be for several reasons. First, there is concern that if HFNC causes delays in initiation of MV, such delays might be associated with higher odds of mortality (21). Second, in many institutions, use of HFNC requires investment of additional resources (e.g., involvement of a respiratory therapist and/or admission to an intensive or intermediate care unit). Finally, many hospitals simply do not have enough HFNC set-ups to use it for all patients with hypoxemia. With infectious pathogens with droplet or airborne spread, concern exists about potential exposure risk associated with using HFNC. However, newer evidence should alleviate this worry (35, 36), and, as such, institutions that initially disallowed use of HFNC for COVID-19–associated respiratory failure have begun to permit it (37).
In the context of a pandemic such as COVID-19, our priorities must shift slightly. No longer can our focus be solely on how to help an individual patient survive and thrive. We must also consider how potentially constrained resources (e.g., ventilators) should be allocated. The benefits of providing a ventilator to one patient must be balanced against the risks that that ventilator will not be usable by the next patient. As such, any strategy that can extend the availability of ventilators without negatively impacting the outcomes of treated patients must be considered. Notably, we found that the relationship between ventilator availability and cumulative deaths is nonlinear; specifically, at low MV capacity, the addition of a few ventilators has great impact on population-level survival, whereas when capacity is already substantial, adding more ventilators produces less benefit. Moreover, different ratios of HFNC:MV capacity shift these nonlinear relationships. Knowing where a given community is in both the MV and the HFNC capacity continua is essential to allowing optimal determination of the clinical and cost-effectiveness of procuring additional machines.
Although not explicitly investigated in our simulations, there are some potential downstream benefits of increasing use of HFNC for COVID-19. A simulation study of HFNC both before and after MV in the United Kingdom demonstrated significant cost savings associated with its use (38). Similarly, simply avoiding MV is likely to produce cost and resource savings. First, medications required to facilitate MV (e.g., analgesics and anxiolytics) have a direct monetary cost that would be avoided; moreover, shortages of sedatives are a concern that could be mitigated against by lowering demand for these products. Second, complications of MV, such as delirium, are known to be associated with increased financial costs (39, 40). Third, it is known that patients with COVID-19 who require intensive care unit admission have longer hospital lengths of stay than patients who do not. Because MV use is a central reason for intensive care unit admission in this epidemic (41), it is plausible that the avoidance of MV through the use of HFNC may allow for shorter hospital lengths of stay. As such, financial costs may be reduced, and resources may be more appropriately allocated.
The strengths of our study stem from its reliance on evidence-based parameter estimates revised by clinicians with firsthand knowledge of the trajectory and prognosis of patients with COVID-19–associated respiratory failure. However, these parameter estimates also represent our study’s largest potential limitation. Despite the use of best available evidence coupled with thoughtful adjustment, it is possible that one or more of our estimates deviates substantially from their true values. The robustness of our findings across the range of considered values, however, lessens the likelihood that our results are grossly inaccurate. In addition, our simulation is limited by its simplicity; inclusion of the use of NIPPV as an alternative to HFNC or MV may have changed our findings and would represent a more complete picture of the impact of deploying any and all available resources as they were intended to be used. Similarly, factors such as time to turnover of ventilators (between patients) and availability of clinicians to readily assess patients for deterioration, which may vary between hospitals, were not included. Finally, several limitations related to our model parameter estimates exist. First, as access to ventilators likely varies substantially across the United States, our estimates of available ventilators in each of the cities simulated is assuredly imperfect. Second, as our estimation of MV supply was based on local mortality rates, we must consider the possibility that mortality rates were impacted by either actual or perceived mechanical ventilator scarcity. Third, we allowed clinicians’ willingness to use MV early (in, for example, the HFNCext + MV10 scenario) to be constant irrespective of patient severity of illness or how much MV capacity remained; this assumption likely represents a simplification of the impact of scarcity.
Using a range of plausible parameter estimates, we found that the use of HFNC was associated with improved population-level patient survival and availability of ventilators. These findings held true at the national level and across hospitals of 100–1,000 beds with access to 25–250 ventilators. Administrators and policymakers both nationally and at the individual hospital level should focus efforts on increasing the availability of HFNC and on advocating for its use for COVID-19–associated respiratory failure.
Footnotes
Supported by National Science Foundation grant CMMI-1762544 (J.D.); U.S. National Institutes of Health grants UO1 HL122998 (M.N.G.), UH2 HL125119 (M.N.G.), UO1 HL123009 (M.N.G.), and UO1 HL143453 (M.N.G.); and Agency for Healthcare Research and Quality grant R18 HS026188 (M.N.G.).
Author Contributions: Design of work: all authors. Data acquisition: J.-T.C. Analysis: Y.H., J.D., and C.W.C. Interpretation of results: all authors. Drafting the manuscript: H.B.G. Revision of manuscript for critically important intellectual content: all authors. Final approval of version to be published: all authors. Agreement to be accountable for all aspects of the work: H.B.G.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Coronavirus Resource Center. Baltimore, MD: Johns Hopkins University; 2020. COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) [accessed 2020 Jun 1]. Available from: https://coronavirus.jhu.edu/map.html. [Google Scholar]
- 2.Feng Y, Ling Y, Bai T, Xie Y, Huang J, Li J, et al. COVID-19 with different severities: a multicenter study of clinical features. Am J Respir Crit Care Med. 2020;201:1380–1388. doi: 10.1164/rccm.202002-0445OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Northwell COVID-19 Research Consortium. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, et al. Clinical characteristics of covid-19 in New York city. N Engl J Med. 2020;382:2372–2374. doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Society of Anesthesiologists; Anesthesia Patient Safety Foundation APSF/ASA guidance on purposing anesthesia machines as ICU ventilators Schaumburg, Illinois: American Society of Anesthesiologists; 2020[accessed 2020 Aug 17]. Available from: https://www.asahq.org/in-the-spotlight/coronavirus-covid-19-information/purposing-anesthesia-machines-for-ventilators [Google Scholar]
- 6.Dosch M. Using the anesthesia workstation as a ventilator for critically ill patients: technical considerations. American Association of Nurse Anesthetists Journal. 2020:13–17.
- 7.Libassi M. Manhasset, NY: Feinstein Institutes for Medical Research; 2020. Northwell converts BiPAP machines into ventilators for hospitalized COVID-19 patients, uses 3D printed adapter. [accessed 2020 Aug 17]. Available from: https://feinstein.northwell.edu/news/the-latest/northwell-converts-bipap-machines-into-ventilators-for-hospitalized-covid-19-patients-uses-3d-printed-adapter. [Google Scholar]
- 8.Wayland MGE. Englewood Cliffs, NJ: CNBC; 2020. Ford sign $336 million federal contract to make ventilators for coronavirus outbreak. [accessed 2020 Aug 17]. Available from: https://www.cnbc.com/2020/04/16/ge-ford-sign-336-million-federal-contract-for-ventilator-production.html. [Google Scholar]
- 9.Beitler JR, Mittel AM, Kallet R, Kacmarek R, Hess D, Branson R, et al. Ventilator sharing during an acute shortage caused by the COVID-19 pandemic. Am J Respir Crit Care Med. 2020;202:600–604. doi: 10.1164/rccm.202005-1586LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhao H, Wang H, Sun F, Lyu S, An Y. High-flow nasal cannula oxygen therapy is superior to conventional oxygen therapy but not to noninvasive mechanical ventilation on intubation rate: a systematic review and meta-analysis. Crit Care. 2017;21:184. doi: 10.1186/s13054-017-1760-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leeies M, Flynn E, Turgeon AF, Paunovic B, Loewen H, Rabbani R, et al. High-flow oxygen via nasal cannulae in patients with acute hypoxemic respiratory failure: a systematic review and meta-analysis. Syst Rev. 2017;6:202. doi: 10.1186/s13643-017-0593-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ou X, Hua Y, Liu J, Gong C, Zhao W. Effect of high-flow nasal cannula oxygen therapy in adults with acute hypoxemic respiratory failure: a meta-analysis of randomized controlled trials. CMAJ. 2017;189:E260–E267. doi: 10.1503/cmaj.160570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Monro-Somerville T, Sim M, Ruddy J, Vilas M, Gillies MA. The effect of high-flow nasal cannula oxygen therapy on mortality and intubation rate in acute respiratory failure: a systematic review and meta-analysis. Crit Care Med. 2017;45:e449–e456. doi: 10.1097/CCM.0000000000002091. [DOI] [PubMed] [Google Scholar]
- 14.Ni YN, Luo J, Yu H, Liu D, Liang BM, Liang ZA. The effect of high-flow nasal cannula in reducing the mortality and the rate of endotracheal intubation when used before mechanical ventilation compared with conventional oxygen therapy and noninvasive positive pressure ventilation: a systematic review and meta-analysis. Am J Emerg Med. 2018;36:226–233. doi: 10.1016/j.ajem.2017.07.083. [DOI] [PubMed] [Google Scholar]
- 15.Xu Z, Li Y, Zhou J, Li X, Huang Y, Liu X, et al. High-flow nasal cannula in adults with acute respiratory failure and after extubation: a systematic review and meta-analysis. Respir Res. 2018;19:202. doi: 10.1186/s12931-018-0908-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ni YN, Luo J, Yu H, Liu D, Liang BM, Yao R, et al. Can high-flow nasal cannula reduce the rate of reintubation in adult patients after extubation? A meta-analysis. BMC Pulm Med. 2017;17:142. doi: 10.1186/s12890-017-0491-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang HW, Sun XM, Shi ZH, Chen GQ, Chen L, Friedrich JO, et al. Effect of high-flow nasal cannula oxygen therapy versus conventional oxygen therapy and noninvasive ventilation on reintubation rate in adult patients after extubation: a systematic review and meta-analysis of randomized controlled trials. J Intensive Care Med. 2018;33:609–623. doi: 10.1177/0885066617705118. [DOI] [PubMed] [Google Scholar]
- 18.Poston JT, Patel BK, Davis AM. Management of critically ill adults with COVID-19. JAMA. 2020;323:1839–1841. doi: 10.1001/jama.2020.4914. [DOI] [PubMed] [Google Scholar]
- 19.Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving Sepsis Campaign: Guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19) Crit Care Med. 2020;48:e440–e469. doi: 10.1097/CCM.0000000000004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Institutes of Health Care of critically ill patients with COVID-19 2020[accessed 2020 May 13]. Rockville, MD: National Institutes of Health. Available from: https://www.covid19treatmentguidelines.nih.gov/critical-care/.
- 21.Kang BJ, Koh Y, Lim CM, Huh JW, Baek S, Han M, et al. Failure of high-flow nasal cannula therapy may delay intubation and increase mortality. Intensive Care Med. 2015;41:623–632. doi: 10.1007/s00134-015-3693-5. [DOI] [PubMed] [Google Scholar]
- 22.Calafiore GC, Novara C, Possieri C. A time-varying SIRD model for the COVID-19 contagion in Italy. Annu Rev Control. 2020;50:361–372. doi: 10.1016/j.arcontrol.2020.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhu Y, Yin H, Zhang R, Ye X, Wei J. High-flow nasal cannula oxygen therapy versus conventional oxygen therapy in patients after planned extubation: a systematic review and meta-analysis. Crit Care. 2019;23:180. doi: 10.1186/s13054-019-2465-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Institute for Health Metrics and Evaluation. COVID-19 projections. Seattle, WA: Institute for Health Metrics and Evaluation; 2020 [accessed 2020 May 13]. Available from: https://covid19.healthdata.org/united-states-of-america.
- 25.Chhatwal J, Ayer T, Linas B, Dalgic O, Mueller P, Adee M, et al. COVID-19 simulator. doi: 10.1001/jamahealthforum.2022.0760. Boston, MA: MGH Institute for Technology Assessment; 2020 [accessed 2020 Aug 17]. Available from: https://covid19sim.org/ [DOI] [PMC free article] [PubMed]
- 26.Zou D, Wang L, Xu P, Chen J, Zhang W, Gu Q. Epidemic model guided machine learning for Covid-19 forecasts in the United States [preprint] medRxiv; 2020 [accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.05.24.20111989v1. [Google Scholar]
- 27.Phua J, Weng L, Ling L, Egi M, Lim CM, Divatia JV, et al. Asian Critical Care Clinical Trials Group. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020;8:506–517. doi: 10.1016/S2213-2600(20)30161-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rubinson L, Vaughn F, Nelson S, Giordano S, Kallstrom T, Buckley T, et al. Mechanical ventilators in US acute care hospitals. Disaster Med Public Health Prep. 2010;4:199–206. doi: 10.1001/dmp.2010.18. [DOI] [PubMed] [Google Scholar]
- 29.Kobokovich A. Ventilator stockpiling and availability in the US. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health; 2020 [accessed 2021 Jan 3]. Available from: https://www.centerforhealthsecurity.org/resources/COVID-19/COVID-19-fact-sheets/200214-VentilatorAvailability-factsheet.pdf.
- 30.Adelman D. Thousands of lives could be saved in the US during the COVID-19 pandemic if states exchanged ventilators. Health Aff (Millwood) 2020;39:1247–1252. doi: 10.1377/hlthaff.2020.00505. [DOI] [PubMed] [Google Scholar]
- 31.Kliff S, Satariano A, Silver-Greenberg J, Kulish N. New York, NY: The New York Times; 2020. There aren’t enough ventilators to cope with the coronavirus. [accessed 2020 Apr 8]. Available from: https://www.nytimes.com/2020/03/18/business/coronavirus-ventilator-shortage.html. [Google Scholar]
- 32.Rowland C. Washington, DC: The Washington Post; 2020. More lifesaving ventilators are available: hospitals can’t afford them. [accessed 2020 Mar 19]. Available from: https://www.washingtonpost.com/health/2020/03/18/ventilator-shortage-hospital-icu-coronavirus/ [Google Scholar]
- 33.Rochwerg B, Granton D, Wang DX, Helviz Y, Einav S, Frat JP, et al. High flow nasal cannula compared with conventional oxygen therapy for acute hypoxemic respiratory failure: a systematic review and meta-analysis. Intensive Care Med. 2019;45:563–572. doi: 10.1007/s00134-019-05590-5. [DOI] [PubMed] [Google Scholar]
- 34.Lin SM, Liu KX, Lin ZH, Lin PH. Does high-flow nasal cannula oxygen improve outcome in acute hypoxemic respiratory failure? A systematic review and meta-analysis. Respir Med. 2017;131:58–64. doi: 10.1016/j.rmed.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 35.Iwashyna TJ, Boehman A, Capelcelatro J, Cohn AM, Cooke JM, Costa DK, et al. Variation in aerosol production across oxygen delivery devices in spontaneously breathing human subjects [preprint] medRxiv; 2020 [accessed Dec 29 2020]. Available from: https://www.medrxiv.org/content/10.1101/2020.04.15.20066688v1. [Google Scholar]
- 36.Gaeckle NT, Lee J, Park Y, Kreykes G, Evans MD, Hogan CJ., Jr Aerosol generation from the respiratory tract with various modes of oxygen delivery. Am J Respir Crit Care Med. 2020;202:1115–1124. doi: 10.1164/rccm.202006-2309OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Griffin KM, Karas MG, Ivascu NS, Lief L. Hospital preparedness for COVID-19: a practical guide from a critical care perspective. Am J Respir Crit Care Med. 2020;201:1337–1344. doi: 10.1164/rccm.202004-1037CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eaton Turner E, Jenks M. Cost-effectiveness analysis of the use of high-flow oxygen through nasal cannula in intensive care units in NHS England. Expert Rev Pharmacoecon Outcomes Res. 2018;18:331–337. doi: 10.1080/14737167.2018.1411804. [DOI] [PubMed] [Google Scholar]
- 39.Milbrandt EB, Deppen S, Harrison PL, Shintani AK, Speroff T, Stiles RA, et al. Costs associated with delirium in mechanically ventilated patients. Crit Care Med. 2004;32:955–962. doi: 10.1097/01.ccm.0000119429.16055.92. [DOI] [PubMed] [Google Scholar]
- 40.Vasilevskis EE, Chandrasekhar R, Holtze CH, Graves J, Speroff T, Girard TD, et al. The cost of ICU delirium and coma in the intensive care unit patient. Med Care. 2018;56:890–897. doi: 10.1097/MLR.0000000000000975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Institute for Health Metrics and Evaluation. Seattle, WA: Institute for Health Metrics and Evaluation; 2020. COVID-19: what’s new for April 5, 2020. Main updates on US COVID-19 predictions since April 2, 2020. [accessed 2020 Apr 22]. Available from: http://www.healthdata.org/sites/default/files/files/Projects/COVID/Estimation_update_040520.pdf. [Google Scholar]
- 42.Gajic O, Dabbagh O, Park PK, Adesanya A, Chang SY, Hou P, et al. U.S. Critical Illness and Injury Trials Group: Lung Injury Prevention Study Investigators (USCIITG-LIPS) Early identification of patients at risk of acute lung injury: evaluation of lung injury prediction score in a multicenter cohort study. Am J Respir Crit Care Med. 2011;183:462–470. doi: 10.1164/rccm.201004-0549OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. LUNG SAFE Investigators; ESICM Trials Group. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 44.Frat JP, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, et al. FLORALI Study Group; REVA Network. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372:2185–2196. doi: 10.1056/NEJMoa1503326. [DOI] [PubMed] [Google Scholar]
- 45.Nagata K, Morimoto T, Fujimoto D, Otoshi T, Nakagawa A, Otsuka K, et al. Efficacy of high-flow nasal cannula therapy in acute hypoxemic respiratory failure: decreased use of mechanical ventilation. Respir Care. 2015;60:1390–1396. doi: 10.4187/respcare.04026. [DOI] [PubMed] [Google Scholar]
- 46.Miltiades AN, Gershengorn HB, Hua M, Kramer AA, Li G, Wunsch H. Cumulative probability and time to reintubation in U.S. ICUs. Crit Care Med. 2017;45:835–842. doi: 10.1097/CCM.0000000000002327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hernández G, Vaquero C, Colinas L, Cuena R, González P, Canabal A, et al. Effect of postextubation high-flow nasal cannula vs noninvasive ventilation on reintubation and postextubation respiratory failure in high-risk patients: a randomized clinical trial. JAMA. 2016;316:1565–1574. doi: 10.1001/jama.2016.14194. [DOI] [PubMed] [Google Scholar]
- 48.Hernández G, Vaquero C, González P, Subira C, Frutos-Vivar F, Rialp G, et al. Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in low-risk patients: a randomized clinical trial. JAMA. 2016;315:1354–1361. doi: 10.1001/jama.2016.2711. [DOI] [PubMed] [Google Scholar]