Pediatric asthma exacerbations frequently result in emergency department (ED) visits (1). To mitigate the rapid spread of coronavirus disease (COVID-19) (1, 2), Massachusetts declared a state of emergency on March 10, schools and childcare facilities closed by March 15 and 18, respectively, and a “stay-at-home” order went into effect on March 24, 2020 (3). The Boston Children’s Hospital ambulatory clinics, ED, and hospital remained open for urgent visits, and all other medical care was provided via telehealth. Patients with asthma were advised to adhere to their controller medications (4). Although viral illness is a frequent cause of asthma exacerbation (5), the effects of social distancing and school closure on pediatric asthma are unknown. We aimed to determine the impact of these measures on frequency of asthma-related pediatric ED visits. We hypothesized that ED visits would be lower following the 2020 “shutdown.”
Methods
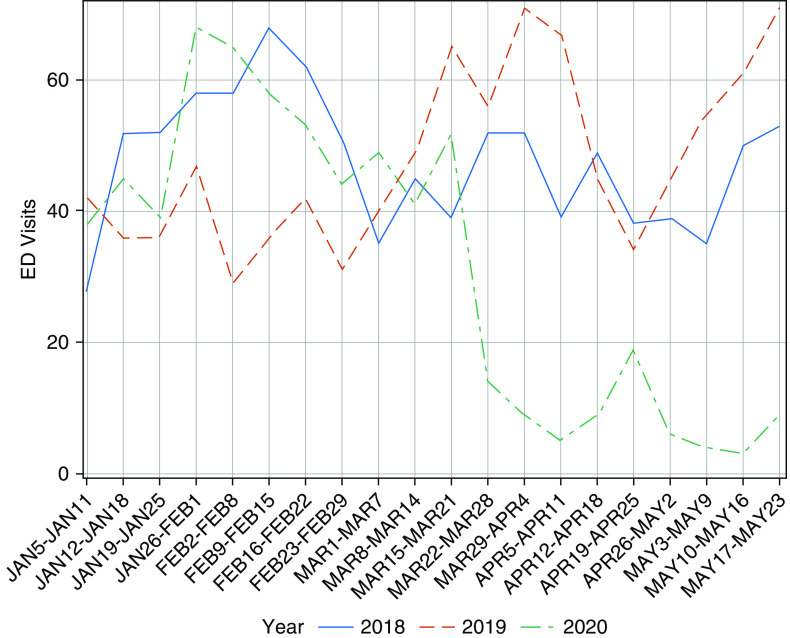
This retrospective cohort study was deemed exempt by the institutional review board. The Boston Children’s Hospital Data Repository linked to the electronic health record was queried to identify children ages 2–22 years with ED visits for asthma (diagnosis codes J45.XX), who received at least one asthma-related medication (albuterol, ipratropium, levalbuterol, or albuterol–ipratropium) between January 5 and May 23 in 2018, 2019, and 2020. Children with other chronic heart or lung diseases were excluded. Patient characteristics were compared with chi-squared tests. Based on visual inspection of run charts (Figure 1), pre- and post-COVID-19 shutdown was defined as January 5 to March 21 and March 22 to May 23, respectively, and applied to each year. Interrupted time-series design with a negative binomial regression model assessed weekly ED visits with regard to time (weeks elapsed since January 5), COVID-19 shutdown (pre- vs. post-), and year (2018, 2019, and 2020). A three-way interaction term between time, COVID-19, and year indicated no difference in slope in the pre- versus post-COVID-19 time period across years (P = 0.3702) and was subsequently dropped in favor of a more parsimonious model. Regression coefficients were exponentiated to derive incidence rate ratios (IRRs). Results were considered significant for P values <0.05 (SAS Institute).
Figure 1.
Run chart of asthma ED visits from January 5 to May 23 in 2018, 2019, and 2020 (n = 2,543). ED = emergency department.
Results
Across the 3 years, 2,543 total ED asthma visits occurred between January 5 and May 23. There were significantly fewer and a lower proportion of asthma ED visits in 2020 compared with 2019 and 2018 (Figure 1). Only ethnicity varied by year. The percentage of asthma exacerbations requiring admission to the hospital was not significantly higher in 2020 compared with 2018 but was higher than 2019 (Table 1).
Table 1.
Demographic and clinical characteristics of ED visits for an asthma exacerbation in 2018, 2019, and 2020 (n = 2,543)
| January to May 2018 (n = 955) | January to May 2019 (n = 958) | January to May 2020 (n = 630) | P Value | |
|---|---|---|---|---|
| N (%) of total ED visits | 955/17,973 (5.3) | 958/18,626 (5.1) | 630/13,715 (4.6) | 0.0117 |
| N (%) of total ED visits March to May* | 526/10,180 (5.2) | 659/11,404 (5.8) | 220/5,675 (3.9) | <0.0001 |
| N (%) of asthma exacerbations requiring admission | 490 (51.3) | 417 (43.5) | 335 (53.2) | 0.0001 |
| Age, yr, n (%) | 0.3602 | |||
| 0–4 | 295 (30.9) | 278 (29.0) | 187 (29.7) | |
| 5–11 | 378 (39.6) | 399 (41.6) | 235 (37.3) | |
| 12–18 | 229 (24.0) | 237 (24.7) | 165 (26.2) | |
| 19+ | 53 (5.5) | 44 (4.6) | 43 (6.8) | |
| Ethnicity, n (%) | 0.0003 | |||
| Hispanic | 141 (14.8) | 193 (20.1) | 86 (13.7) | |
| Non-Hispanic | 713 (74.7) | 635 (66.3) | 451 (71.6) | |
| Missing | 101 (10.6) | 130 (13.6) | 93 (14.8) | |
| Race, n (%) | 0.0636 | |||
| White | 261 (27.3) | 225 (23.5) | 168 (26.7) | |
| Black | 328 (34.3) | 303 (31.6) | 188 (29.8) | |
| Asian | 19 (2.0) | 18 (1.9) | 14 (2.2) | |
| Other | 310 (32.5) | 376 (39.2) | 212 (33.7) | |
| Missing | 37 (3.9) | 36 (3.8) | 48 (7.6) | |
| Insurance, n (%) | 0.2496 | |||
| Private | 377 (39.5) | 356 (37.2) | 267 (42.4) | |
| Public (Medicaid) | 561 (58.7) | 584 (61.0) | 345 (54.8) | |
| International | 11 (1.2) | 12 (1.3) | 6 (1.0) | |
| Missing | 6 (0.6) | 6 (0.6) | 12 (1.9) |
Definition of abbreviation: ED = emergency department.
Subset of data set reflecting N (%) of total ED visits for March 1 to May 23.
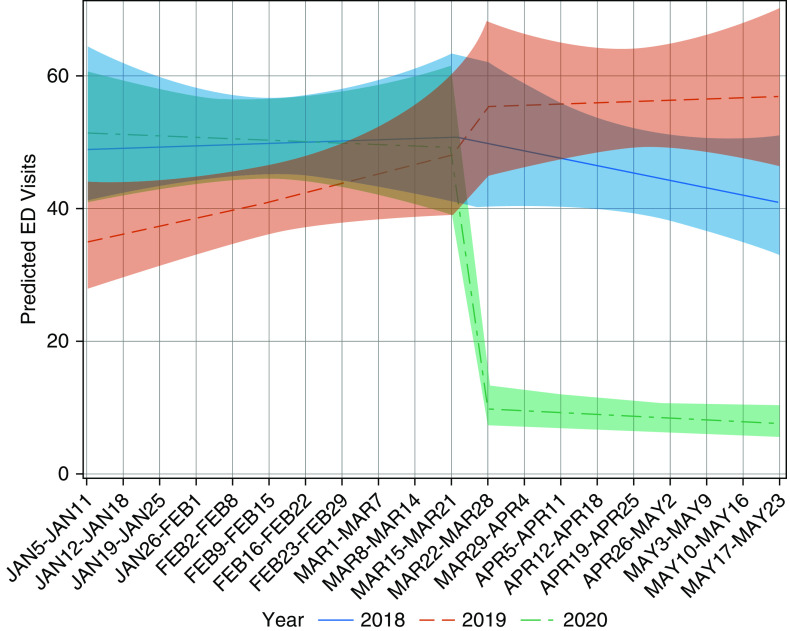
After adjusting for year, weeks, and time period (before or after shutdown), we found a significantly decreased incidence of ED visits after the shutdown in 2020 compared with 2018 (IRR, 0.21; 95% confidence interval [95% CI], 0.11–0.37; P < 0.0001) and 2019 (IRR, 0.18; 95% CI, 0.10–0.32; P < 0.0001) but not between 2018 and 2019 (P = 0.6250) (see Table E1 in the online supplement). For the week of March 15 to March 21, the rate of ED visits was similar across years. However, the following week, the rate of ED visits decreased by 80% (IRR, 0.20; 95% CI, 0.14–0.28) and 82% (IRR, 0.18; 95% CI, 0.13–0.25) in 2020 relative to 2018 and 2019, respectively (P < 0.0001), which continued through May 23 (82% and 87% reduction compared with 2018 and 2019, respectively, Figure 2).
Figure 2.
Multivariable model of weekly incidence of asthma ED visits from January 5 to May 23 in 2018, 2019, and 2020 (n = 2,543). ED = emergency department.
Owing to significant differences in patient ethnicity by year, the primary model was stratified by Hispanic (n = 420) and non-Hispanic (n = 1,799). Each subgroup demonstrated significantly lower ED rates after COVID-19 in 2020 than in previous years, consistent with the overall findings.
Discussion
We observed a significant decrease in pediatric ED visits for asthma during the Massachusetts shutdown in the setting of the COVID-19 pandemic. Additionally, the percentage of total ED visits that were due to asthma was lower in 2020 compared with 2018 and 2019, suggesting that the effect was not just due to an overall avoidance of the ED.
ED visits dropped precipitously the week of March 22, days after school and day care closures and coinciding with the state shutdown. There are several potential contributors to this decrease, including increased adherence to asthma medications, avoidance of the healthcare setting due to fear of contracting COVID-19, improved air quality due to work-from-home implementation, decreased participation in sports and exercise, decreased exposure to outdoor aero-allergens, and decreased viral exposure due to school and day care closure. Interestingly, rather than a gradual decline, which would be more indicative of improved medication adherence, there was a dramatic decline, suggestive of a sudden change in exposure, which occurred in conjunction with the stay-at-home order and school closure. Our findings are consistent with—although more drastic than—asthma exacerbation trends previously noted to decrease during the summer months in association with school vacation (5, 6). Furthermore, these results are similar to those recently reported by Kenyon and colleagues (7). Similarly, Hatoun and colleagues have demonstrated significant declines in several other pediatric infectious diseases in the setting of social distancing measures, including bronchiolitis and the common cold (8). It is also possible that the decrease in ED visits could be explained by a simultaneous increase in outpatient or home management of asthma exacerbations, including via telehealth, which became available at our institution during the state of emergency.
In contrast to Kenyon and colleagues, we found no change in the admission rate (7). Although this might indicate that asthma ED visits during the shutdown were not necessarily more acute, it is also possible that other factors, such as desired avoidance of admission, also contributed to the admission rate remaining the same. Additional exposure to in-home triggers and allergens may have also contributed to the similar admission rate. These findings raise important questions for future studies, such as contribution of viral infection for those requiring admission, and concomitant in home exposures. Additionally, we identified ethnic differences across the study period that did not influence the main findings. Nevertheless, it will be important for future studies to specifically assess racial/ethnic variation in healthcare use. Although provocative, these findings are limited to a single large pediatric ED and warrant validation in other institutions and ambulatory settings. If true, this phenomenon offers lessons to be learned and several areas for future investigation of this complex issue, serving as a framework for future prevention of childhood asthma exacerbations.
Footnotes
Supported by U.S. National Institutes of Health grant R01 ES030100 (J.M.G.).
Author Contributions: T.S., K.N., and J.M.G. conceptualized and designed the study. T.S. drafted the initial manuscript. K.N. and J.M.G. reviewed and revised the manuscript. A.H. participated in the study design, developed the database queries, extracted the data set, cleaned the data set, and reviewed and revised the manuscript. K.F.G. participated in the study design, performed the statistical analyses, drafted the methods and results sections, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
This letter has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395:931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Coronavirus disease 2019 (COVID-2019): situation report-51 SITUATION IN NUMBERS total and new cases in last 24 hoursMarch 11, 2020 [accessed 2020 Jun 5]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10
- 3.Baker C, Polito K.Updates, emergency orders, and guidance associated with the COVID-19 state of emergency 2020[accessed 2020 Jun 5]. Available from: https://www.mass.gov/doc/march-15-2020-school-closure-order/download
- 4.Moore A.COVID-19 and asthma: what patients need to knowDecember 15, 2020 [accessed 2020 Jun 7]. Available from: https://www.aaaai.org/conditions-and-treatments/library/asthma-library/covid-asthma
- 5.Johnston SL, Pattemore PK, Sanderson G, Smith S, Campbell MJ, Josephs LK, et al. The relationship between upper respiratory infections and hospital admissions for asthma: a time-trend analysis. Am J Respir Crit Care Med. 1996;154:654–660. doi: 10.1164/ajrccm.154.3.8810601. [DOI] [PubMed] [Google Scholar]
- 6.Johnston NW, Johnston SL, Norman GR, Dai J, Sears MR. The September epidemic of asthma hospitalization: school children as disease vectors. J Allergy Clin Immunol. 2006;117:557–562. doi: 10.1016/j.jaci.2005.11.034. [DOI] [PubMed] [Google Scholar]
- 7.Kenyon CC, Hill DA, Henrickson SE, Bryant-Stephens TC, Zorc JJ. Initial effects of the COVID-19 pandemic on pediatric asthma emergency department utilization. J Allergy Clin Immunol Pract. 2020;8:2774–2776, e1. doi: 10.1016/j.jaip.2020.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hatoun J, Correa ET, Donahue SMA, Vernacchio L. Social distancing for COVID-19 and diagnoses of other infectious diseases in children. Pediatrics. 2020;146:e2020006460. doi: 10.1542/peds.2020-006460. [DOI] [PubMed] [Google Scholar]