Summary
Background
Loneliness is experienced by a third of older adults in the UK and is a modifiable potential risk factor for depressive symptoms. It is unclear how the association between loneliness and depressive symptoms persists over time, and whether it is independent of related social constructs and genetic confounders. We aimed to investigate the association between loneliness and depressive symptoms, assessed on multiple occasions during 12 years of follow-up, in a large, nationally representative cohort of adults aged 50 years and older in England.
Methods
We did a longitudinal study using seven waves of data that were collected once every 2 years between 2004 and 2017, from adults aged 50 years and older in the English Longitudinal Study of Ageing (ELSA). The exposure was loneliness at baseline (wave two), measured with the short 1980 revision of the University of California, Los Angeles Loneliness Scale (R-UCLA). The primary outcome was a score indicating severity of depression measured at six subsequent timepoints (waves three to eight), using the eight-item version of the Centre for Epidemiologic Studies Depression Scale (CES-D). Analyses were linear multilevel regressions, before and after adjusting for social isolation, social support, polygenic risk scores, and other sociodemographic and health-related confounders. The secondary outcome was depression diagnosis, measured using a binary version of the CES-D.
Findings
4211 (46%) of 9171 eligible participants had complete data on exposure, outcome, and confounders, and were included in our complete case sample. After all adjustments, a 1-point increase in loneliness score was associated with a 0·16 (95% CI 0·13–0·19) increase in depressive symptom severity score (averaged across all follow-ups). We estimated a population attributable fraction for depression associated with loneliness of 18% (95% CI 12–24) at 1 year of follow-up and 11% (3–19) at the final follow-up (wave eight), suggesting that 11–18% of cases of depression could potentially be prevented if loneliness were eliminated. Associations between loneliness and depressive symptoms remained after 12 years of follow-up, although effect sizes were smaller with longer follow-up.
Interpretation
Irrespective of other social experiences, higher loneliness scores at baseline were associated with higher depression symptom severity scores during 12 years of follow-up among adults aged 50 years and older. Interventions that reduce loneliness could prevent or reduce depression in older adults, which presents a growing public health problem worldwide.
Funding
National Institute on Aging and a consortium of UK Government departments coordinated by the National Institute for Health Research.
Introduction
Depression among older adults is common (with an estimated prevalence of 4–9% worldwide),1 potentially underdiagnosed and undertreated, and associated with substantial morbidity and mortality.1 Data from the past 15 years suggest that the prevalence of depressive illness among older adults is increasing.2 Better identification of modifiable risk factors for depression would inform public health and clinical approaches to prevention.
Loneliness is a painful emotional state caused by a discrepancy between a person's desired meaningful social relationships, and what relationships they perceive they have.3, 4 Loneliness is related to, but distinct from, other aspects of social relationships such as objective social isolation and perceived social support.3, 4 Around a third of people aged 50 years and older in the UK report loneliness,5 which might partly be due to factors such as retirement, physical and cognitive decline, bereavement, reduced social networks, and loss of social roles. There is substantial overlap between the constructs of loneliness and depression, although there is also evidence that they are distinct.6 Theoretical models suggest that loneliness has social, cognitive, and biological consequences that could increase the risk of subsequent depression.7 Potential mechanisms for this association include negative perceptions of social interactions, negative cognitive schemas (eg, low self-belief), expectations of social threat, increased stress, reduced self-esteem, and biological effects on the stress response and inflammation.7 There is also evidence that loneliness is associated with anticipated rejection and reduced reward responsiveness to positive stimuli.7
Research in context.
Evidence before this study
We searched PubMed, the American Psychological Association PsycInfo and PsycArticles, and the CINAHL databases for studies published in English from database inception to June 30, 2020, which investigated loneliness and depressive symptoms in older adults, using the approved Medical Subject Headings terms “loneliness” and “depressive disorders, major”. We also manually searched reference lists of identified studies. Many studies have examined the association between loneliness and depression but most previous studies were cross-sectional. Of the longitudinal studies, many were limited by small unrepresentative samples, single-item measures of loneliness, single follow-ups or short follow-up periods, or inadequate adjustment for confounders. Several longitudinal studies used cross-lagged panel analyses. Although these models are valuable for comparing bidirectional relationships, they often do not have follow-up periods of longer than 2–3 years and are susceptible to time-varying confounding. No previous large longitudinal study had adjusted for potential genetic confounders. Longitudinal studies which had adjusted for a broad range of social relationships that are related to, but distinct from, loneliness (such as objective isolation and social support) were also scarce.
Added value of this study
To our knowledge, this is the first large longitudinal study of the association between loneliness and subsequent depression, which used repeated measures of depressive symptoms over a long follow-up period and adjusted for other social constructs and potential genetic confounders. We found that, irrespective of other social experiences, loneliness was associated with an increased risk of subsequent depression, and this risk persisted for up to 12 years after the loneliness was reported.
Implications of all the available evidence
Clinicians should be aware that older adults who report being lonely are at increased risk of developing depressive symptoms, and approaches to reduce loneliness should be considered. Such approaches could include social prescribing, psychological therapies that target negative cognitions, social skills training, psychoeducation, and supported socialisation (offering people support and guidance to select and attend activities). From a public health perspective, our results suggest that strategies which reduce or prevent loneliness in the general population could reduce the burden of future depression among older adults.
Many studies have examined the relationship between loneliness and depression in older adults, but these studies have had limitations.8, 9 There have been several cross-sectional studies,10, 11, 12, 13, 14, 15, 16 but it is impossible to rule out reverse causation in studies with a cross-sectional design. Longitudinal studies are essential to establishing whether loneliness precedes depressive symptoms, which is a necessary condition for identifying loneliness as a potentially causal, and hence targetable, risk factor for depression.
Existing longitudinal studies also have had limitations. Several small longitudinal studies (ie, sample sizes of less than 400 participants) have found evidence that higher levels of loneliness are associated with future depressive symptoms among older adults.17, 18, 19, 20, 21, 22 Some of these studies used clinical17, 20 or convenience21 samples, which introduces selection bias and reduces generalisability. Small studies might also not be statistically powered to produce valid and precise results.23
Several large population-based cohort studies have reported positive associations between loneliness and subsequent depression,24, 25, 26, 27, 28 although one study found no evidence of a relationship.29 Most of these studies used single-item measures of loneliness24, 25, 26, 27, 28, 29 which, compared with multi-item loneliness scales, are more susceptible to social desirability biases. Two large population-based cohort studies have found positive associations between loneliness, assessed using multi-item scales, and a single follow-up measure of depressive symptoms 2 years later.26, 27
Studies with longer follow-up periods or repeated assessments of the depression outcome are scarce,19, 27, 28, 29 but would provide evidence on how the association between loneliness and depression changes over time. This evidence would strengthen causal inferences and inform the timing of interventions to prevent depression. To our knowledge, the longest follow-up in any previous study has been 7 years, but this study found no evidence of an association between loneliness and depressive symptoms.29 The extent to which the association persists over time is therefore unclear. There have been three studies with repeated assessments of loneliness and depression, but these studies have used cross-lagged panel analyses.19, 27, 28 Although these models are valuable for comparing bidirectional relationships, they often do not have follow-up periods of longer than 2–3 years (because each outcome follows the exposure immediately before it).
Loneliness is associated with objective social isolation and perceived social support, and it is possible that associations between loneliness and depressive symptoms are confounded by these related social experiences. Only one large cohort study adjusted for a broad range of social constructs and confounders related to loneliness. An independent association between loneliness and depressive symptoms was reported, although this study used a single-item loneliness measure and a single follow-up.26 If there is an independent influence of loneliness, irrespective of other social experiences, it would suggest that interventions need to target loneliness, in addition to targeting social isolation and providing social support.
Loneliness and depression are moderately heritable.30, 31 Molecular investigations reveal substantial overlap between genes that influence loneliness and genes that influence depression.32 This overlap could introduce genetic confounding of associations between loneliness and depression which, as far as we know, has never been investigated. One way to account for possible genetic confounding is to adjust for polygenic risk scores. Gene variants are derived from genome-wide association studies and combined into a single polygenic risk score, which captures part of an individual's genetic susceptibility to the outcome (eg, depression or loneliness).33
We aimed to test the hypothesis that loneliness is associated with more severe symptoms of subsequent depression, and to build on existing evidence by using a large, nationally representative cohort of adults aged 50 years and older with a 12-year follow-up period.
Methods
Study design and participants
The English Longitudinal Study of Ageing (ELSA) began in 2002 and is an ongoing study of the health, social, and economic lives of the population aged 50 years and older in England.34 The core ELSA sample in wave one of the study was recruited from households that participated in the 1998, 1999, or 2001 Health Survey for England (HSE)—a large nationally representative annual household survey that monitors trends in the population's health. Eligibility criteria for ELSA were: belonging to a household participating in the HSE, in which at least one person agreed to be contacted; date of birth before March 1, 1952 (ie, aged 50 years or older when the study began); and living in a private household in England at the time of the first wave of fieldwork (11 578 eligible households and 18 813 individuals).34 Partners of eligible participants who were younger than 50 years of age and people who had joined households since the HSE were also invited. The household response rate was 70% and the individual response rate was 67%. The total sample of 12 099 participants at wave one of ELSA consisted of 11 391 core members, 636 partners aged younger than 50 years, and 72 new partners aged 50 years and older. The mean age of the sample was 65 years (SD 10·75).34 The ELSA sample is periodically refreshed with additional participants aged 50 years and older, drawn from other HSE waves. The wave one ELSA sample was compared with national census data and was deemed representative of the non-institutionalised general population in England aged 50 years and older.34
Participants were followed-up with a survey once every 2 years, until 2016 or 2017. Loneliness was first assessed at wave two (in 2004–05), which was used as the baseline for our study cohort (n=9432, 82·8% of the core wave one sample). ELSA data are publicly available and were downloaded from the UK Data Service. For waves one to eight, the UK Data Service contains a single ELSA data file containing the majority of variables relating to the ELSA interviewer visit.
Ethical approval for ELSA was obtained from the London Multicentre Research Ethics Committee. All participants provided informed consent.
Procedures
Depressive symptoms in the previous week were assessed at every timepoint using the eight-item version of the Centre for Epidemiologic Studies Depression Scale (CES-D). Scores ranged from 0 to 8, and higher scores indicated greater severity of depressive symptoms. The eight-item CES-D is widely used in older adults and has been validated against the 20-item version, showing good validity and reliability.35 The CES-D contains an item that asks whether respondents have felt lonely. Consistent with other studies,19, 36 we removed this item to avoid overlap with the loneliness scale, which might inflate associations. The CES-D showed good internal consistency before (α=0·78) and after (α=0·76) removing the loneliness item, at each wave. Our primary outcome was CES-D scores (using seven items, with loneliness removed) after the baseline assessment of loneliness (waves three to eight), as a repeated measure. Our secondary outcome was depression measured using a binary version of the CES-D. The recommended score cutoff approximating clinical diagnosis of depression on the eight-item CES-D (including the loneliness item) is 3 or higher.37 For our revised seven-item scale (with the loneliness item removed), we used a score cutoff of 2 or higher, which resulted in the same prevalence of depression as the cutoff of 3 or higher on the eight-item version of the CES-D.
Loneliness was measured at waves two to eight. At each of these waves the three-item short 1980 version of the University of California, Los Angeles Loneliness Scale (R-UCLA) was used.38 We used the baseline scores from wave two as the main exposure for loneliness. The scale asks “how often do you feel you lack companionship?”, “how often do you feel left out?”, and “how often do you feel isolated from others?”. Response options for each item are “hardly ever or never” (equating to a score of 1), “some of the time” (a score of 2), or “often” (a score of 3). Total scores for the scale range from 3 to 9, and higher scores indicate greater loneliness. The scale has been used extensively with older adults, with good internal reliability (α=0·78).36
We selected confounders on the basis of existing studies and theoretical assumptions. We assumed that these variables were potential alternative explanations for the association between exposure and outcome. It is possible that associations between loneliness and depressive symptoms are confounded by related social experiences.19 We therefore adjusted for measures of social network size, frequency of social contact, participation in social groups, and perceived social support. These measures were from wave two and are described in the appendix (p 3)). Consistent with other studies,36 we assumed that objective social isolation (having little social contact with others) would be captured by social network size, frequency of social contact, and participation in social groups. We also adjusted for: polygenic risk scores for loneliness and depressive symptoms, age, sex, ethnicity, marital status, level of education, employment status, wealth, long-term physical illness, mobility impairment, pain, body-mass index, waist circumference, cognitive function, and baseline depressive symptoms. Wealth is generally used as the measure of socioeconomic resources in ageing studies because of the difficulty in income measurement in retired people.36 Even among those who work, incomes are often reduced at older ages because part-time work is more common. All confounders were measured at wave two and are described in the appendix (pp 4–6).
Statistical analysis
Analyses were done using Stata 14. For descriptive analyses, we dichotomised loneliness scores (<6 or ≥6)36 and compared characteristics of these groups using means with SD or frequencies with percentages. We did not use sample weights in our main analyses because weights were derived using many of the variables used as confounders, and can lead to overadjustment.39 We included the sample weights in our multiple imputation sensitivity analysis. We defined our complete case sample as those who had data on loneliness exposure, confounders, and at least one depressive symptom severity score outcome.
We used linear multilevel regressions to examine associations between loneliness (wave two; continuous exposure) and subsequent depressive symptom severity (waves three to eight; continuous outcome). Repeated depressive symptom severity measurements were clustered within individuals, with a random intercept for individual, random slopes according to time (time defined according to wave of follow-up) and heteroscedasticity-consistent SEs. Multilevel models maximise the use of longitudinal data, adjust for the correlation between repeated measures within individuals, increase statistical power and precision (relative to traditional regression), and estimates are weighted for missing data between waves.
We built the regression model in ten stages (appendix p 7). Model one tested the univariable association between loneliness and depressive symptom severity. In model two we added continuous linear variables, and quadratic time variables were added in model three (we excluded the quadratic time variables if there was no evidence of a non-linear influence of time on depressive symptoms). In model four, we added the social variables and in model five, polygenic risk scores were added. In model six we added sociodemographic factors and, in model seven, health indicators. In model eight, we added baseline depressive symptoms. We investigated whether the association was modified by age or sex, using interaction terms. To investigate whether the association between loneliness and depressive symptoms differed according to timepoint, we calculated an interaction between loneliness and time. We calculated interactions between loneliness and linear time and quadratic time, to obtain global p values. If there was evidence of interaction, we estimated associations between loneliness and depressive symptoms at each timepoint.
As a secondary outcome, we used a binary depression variable and logistic multilevel models. We calculated the population attributable fraction (PAF; the proportion of cases of depression that could be prevented if the influence of loneliness was removed).
We did several sensitivity analyses to explore the robustness of our results. First, as depressive symptom severity scores were positively skewed, we analysed our primary outcome using a negative binomial model. Second, as loneliness is time-varying, we analysed panel data with loneliness (exposure) and depressive symptom severity (outcome) from waves two to eight, using linear multilevel regression. From this model we extracted the association between loneliness and depressive symptoms before and after adjustments, and the fixed-effect (within-person) change in depressive symptoms according to change in loneliness. Finally, we re-ran analyses of the primary and secondary outcome with the loneliness item included in the CES-D. We compared the PAF from logistic models with and without the loneliness item.
We compared the characteristics of those with complete (on all variables used in the analyses) and missing data, using independent t tests and χ2 tests. As a sensitivity analysis, we replaced missing data on confounders and outcome (missing data shown in figure) using multiple imputation with chained equations. Polygenic risk score data cannot be imputed using standard procedures due to linkage disequilibrium. We assumed data were missing at random (ie, that missing data were associated with observed data),40 and imputed 25 datasets. To predict missing values, we used all baseline characteristic variables and several auxiliary variables including tobacco smoking, alcohol use, hearing or vision impairment, household size, and whether the respondents had children, measured at wave two. We applied the population weight from wave two to the imputation model to improve representativeness of the sample to the population. Imputed datasets were combined and analyses were re-run using Rubin's rules.40
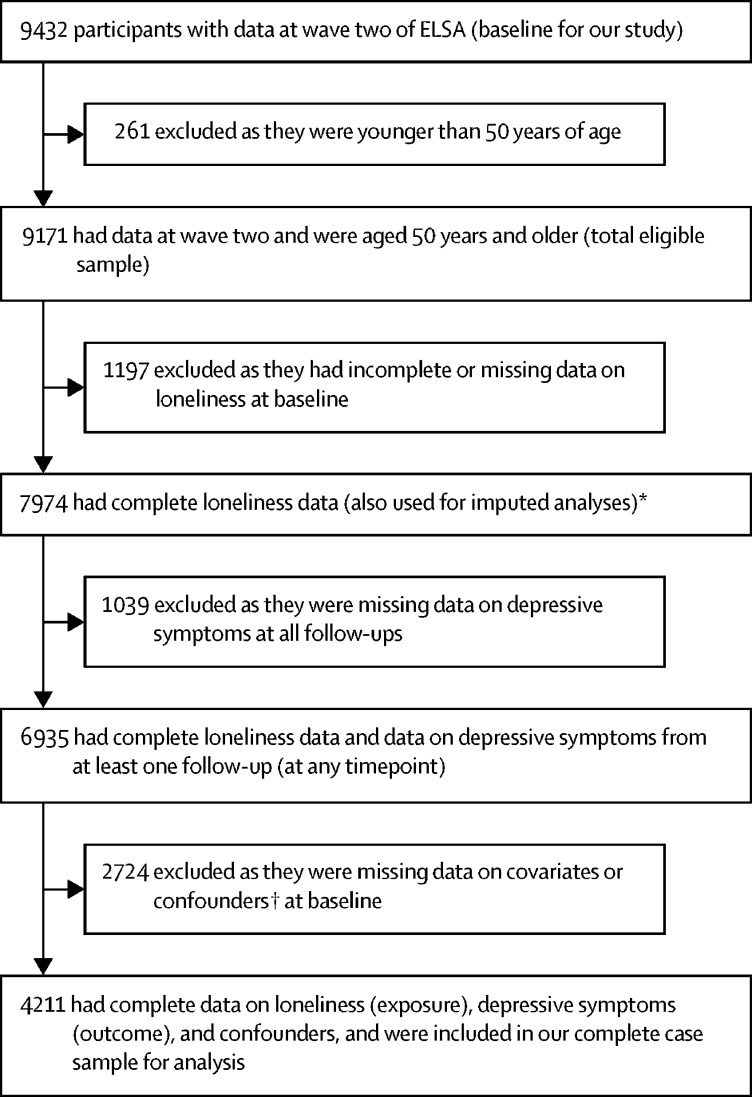
Figure.
Study flowchart
ELSA=English Longitudinal Study of Ageing. *This was the sample size after using multiple imputation to replace data missing for confounders and outcome; exposure data were not imputed. †Confounders were social network size, social contact frequency, participation in social groups, perceived social support, age, sex, ethnicity, marital status, level of education, employment status, wealth, long-term physical illness, mobility impairment, pain, body-mass index, waist circumference, cognitive function, polygenic risk scores, and depressive symptoms at baseline (wave two).
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Of 9171 eligible participants, our complete case sample included 4211 participants (46%; figure) aged 52–101 years (mean 65·1, SD 8·9); 2310 (55%) were female, 2785 (66%) were unemployed or retired, and 4211 (100%) were white (table 1, appendix pp 8–9). The mean loneliness score at baseline (wave two) was 4·12 (SD 1·50). Mean depressive symptom severity scores increased slightly over time and were higher in the group with high loneliness scores (score of ≥6; table 2). At baseline, 17% of the sample had a depression severity score of 2 or higher on the CES-D and this was similar during follow-up. At baseline, there was a moderate positive correlation between loneliness and depression (Pearson's correlation coefficient 0·44 when including the CES-D loneliness item and 0·49 when not including the loneliness item).
Table 1.
Baseline characteristics of the complete case sample, overall and by loneliness score
| Overall (n=4211) |
Loneliness |
||||
|---|---|---|---|---|---|
| High* (n=714, 18%) | Low† (n=3497, 82%) | p value | |||
| Sex | |||||
| Female | 2310 (55%) | 460 (64%) | 1850 (53%) | <0·0001 | |
| Male | 1901 (45%) | 254 (36%) | 1647 (47%) | .. | |
| Marital status | |||||
| Married | 2954 (70%) | 309 (43%) | 2645 (76%) | <0·0001 | |
| Unmarried‡ | 1257 (30%) | 405 (57%) | 852 (24%) | .. | |
| Level of education | |||||
| Higher (degree level and higher) | 603 (14%) | 71 (10%) | 532 (15%) | <0·0001 | |
| Intermediate (school qualifications) | 2272 (54%) | 361 (51%) | 1911 (55%) | .. | |
| No formal qualification | 1336 (32%) | 282 (39%) | 1054 (30%) | .. | |
| Employment status | |||||
| Employed | 1426 (34%) | 189 (26%) | 1237 (35%) | <0·0001 | |
| Unemployed or retired | 2785 (66%) | 525 (74%) | 2260 (65%) | .. | |
| Wealth quintile | |||||
| 1 (least wealthy) | 490 (12%) | 148 (23%) | 342 (10%) | .. | |
| 2 | 742 (18%) | 151 (21%) | 591 (17%) | .. | |
| 3 | 896 (21%) | 140 (20%) | 756 (22%) | .. | |
| 4 | 1014 (24%) | 150 (21%) | 864 (25%) | .. | |
| 5 (wealthiest) | 1069 (25%) | 125 (18%) | 944 (27%) | <0·0001 | |
| Long-term physical illness | |||||
| Yes | 2297 (55%) | 467 (65%) | 1830 (52%) | ||
| No | 1914 (45%) | 247 (35%) | 1667 (48%) | <0·0001 | |
| Mobility impairment | |||||
| Present | 2313 (55%) | 487 (68%) | 1826 (52%) | <0·0001 | |
| Absent | 1898 (45%) | 227 (32%) | 1671 (48%) | ||
| Often troubled with pain | |||||
| Yes | 1140 (33%) | 350 (49%) | 1140 (33%) | .. | |
| No | 2357 (67%) | 364 (51%) | 2357 (67%) | <0·0001 | |
| Score of 2 or higher on CES-D | |||||
| Yes | 729 (17%) | 301 (42%) | 428 (12%) | ||
| No | 3482 (83%) | 413 (58%) | 3069 (88%) | <0·0001 | |
| Participation in social groups | |||||
| Yes | 960 (23%) | 188 (26%) | 772 (22%) | 0·014 | |
| No | 3251 (77%) | 526 (74%) | 2725 (78%) | .. | |
| Age, years | 65·1 (8·9) | 66·1 (9·6) | 64·9 (8·8) | 0·0010 | |
| Depressive symptom severity score at wave two (range 0–8) | 1·2 (1·6) | 2·2 (2·1) | 0·9 (1·4) | <0·0001 | |
| Social support score (range 0–36) | 23·2 (7·2) | 18·1 (6·9) | 24·2 (6·8) | <0·0001 | |
| Social network size score (range 0–30) | 7·3 (4·2) | 6·1 (3·9) | 7·5 (4·2) | <0·0001 | |
| Social contact frequency score (range 0–18) | 9·0 (3·0) | 8·2 (3·1) | 9·1 (3·0) | <0·0001 | |
| Body-mass index, kg/m2 | 26·8 (7·0) | 26·6 (7·9) | 26·9 (6·8) | 0·40 | |
| Waist circumference, cm | 93·8 (17·4) | 93·2 (18·3) | 93·9 (17·2) | 0·34 | |
| Overall cognitive function§ | 0·0 (1·0) | −0·3 (1·1) | 0·1 (1·0) | <0·0001 | |
Data are n (%) or mean (SD). CES-D=Centre for Epidemiologic Studies Depression Scale. R-UCLA=the short 1980 version of the University of California, Los Angeles Loneliness Scale.
Participants who scored 6–9 on R-UCLA.
Participants who scored less than 6 on R-UCLA.
Single, divorced, separated, or widowed.
Assessed using neuropsychological tests of immediate and delayed verbal memory, prospective memory, verbal fluency, cognitive speed and attention, and time orientation.
Table 2.
Depressive symptom severity score at each follow-up in the sample overall and by loneliness score
| Overall |
Loneliness |
|||
|---|---|---|---|---|
| High* | Low† | p value‡ | ||
| Wave three (n=4060) | 1·16 (1·64) | 2·25 (2·15) | 0·94 (1·41) | <0·0001 |
| Wave four (n=3651) | 1·13 (1·64) | 2·09 (2·09) | 0·93 (1·46) | <0·0001 |
| Wave five (n=3387) | 1·26 (1·70) | 2·21 (2·08) | 1·07 (1·54) | <0·0001 |
| Wave six (n=3142) | 1·14 (1·63) | 2·06 (2·07) | 0·96 (1·46) | <0·0001 |
| Wave seven (n=2751) | 1·17 (1·59) | 2·13 (2·04) | 0·98 (1·41) | <0·0001 |
| Wave eight (n=2449) | 1·14 (1·53) | 2·06 (1·96) | 0·97 (1·37) | <0·0001 |
Data are mean (SD). The number of participants with complete data on all variables at each wave varies because there were a different number of people with depression data at each wave (due to attrition). R-UCLA=the short 1980 version of the University of California, Los Angeles Loneliness Scale.
Participants who scored 6–9 on R-UCLA.
Participants who scored less than 6 on R-UCLA.
Obtained from independent t tests.
Compared with those with low loneliness scores (score of <6), participants with high loneliness scores (≥6) were on average older and a higher proportion were female, unmarried, unemployed, and had lower level of education and wealth (table 1). The group with high loneliness scores also had more physical illnesses, mobility impairment, and pain, as well as more severe depressive symptoms, lower levels of social support, smaller social network sizes, and less frequent social contact. However, participation in social groups was more common in the group with high loneliness scores (table 1).
Participants with missing data were older than those in the complete case sample and more likely to be unmarried, from an ethnic minority, and of lower socioeconomic status (appendix pp 8–9). Participants with missing data also had higher scores on loneliness, depressive symptoms, and social isolation, and were more likely to have experienced mobility impairment or be often troubled with pain (appendix pp 8–9).
In the univariable model (model one), a 1-point increase in loneliness was associated with a 0·38 (95% CI 0·35–0·41) increase in depressive symptoms on average across all follow-ups (table 3). There was evidence of a small increase in depressive symptoms over time (model two, p=0·0016) and no evidence that this was non-linear (model three, p=0·55). There was little change in the association between loneliness and depressive symptoms after adjusting for other social experiences and polygenic risk scores. The association remained but was attenuated after further adjustment for sociodemographic and health-related confounders (0·29 [95% CI 0·26–0·32]; model seven, table 3). Adjusting for baseline depressive symptoms reduced the effect estimate by around half, but evidence for the association remained (0·16 [0·13–0·19]; model eight, table 3). There was no evidence that the association between loneliness and depression was modified by age (p=0·33) or sex (p=0·24). Effect estimates for social experiences related to loneliness, and polygenic risk scores, are reported in the appendix (p 12)).
Table 3.
Mean change in depressive symptom severity score per 1-point increase in loneliness score, using repeated measures of depressive symptoms from waves three to eight
| Change in depressive symptom severity score (95% CI) | p value | |
|---|---|---|
| Model one: univariable association | 0·38 (0·35–0·41) | <0·0001 |
| Model two: model one plus continuous linear time variable | 0·38 (0·35–0·41) | <0·0001 |
| Model three: model two plus continuous quadratic time variable* | 0·38 (0·35–0·41) | <0·0001 |
| Model four: model two adjusted for social experiences related to loneliness† | 0·36 (0·33–0·40) | <0·0001 |
| Model five: model four adjusted for polygenic risk scores‡ | 0·36 (0·32–0·39) | <0·0001 |
| Model six: model five adjusted for sociodemographic factors§ | 0·33 (0·29–0·36) | <0·0001 |
| Model seven: model six adjusted for health indicators¶ | 0·29 (0·26–0·32) | <0·0001 |
| Model eight: model seven adjusted for depressive symptoms at baseline‖ | 0·16 (0·13–0·19) | <0·0001 |
Time squared was subsequently excluded from models because of no evidence of departure from linearity.
Social network size, social contact frequency, participation in social groups, and perceived social support.
Polygenic risk scores for depressive symptoms and loneliness.
Age, sex, ethnicity, marital status, level of education, employment status, and wealth.
Long-term physical illness, mobility impairment, pain, body-mass index, waist circumference, and cognitive function.
Interactions between loneliness and time and loneliness and time squared were added to model eight; results for interaction terms are reported in the text.
The magnitude of the association between loneliness and depressive symptoms reduced as follow-up progressed (interaction term coeffecient −0·01 [95% CI −0·019 to −0·009]; p=0·031; table 4). Evidence of the association remained at wave eight, representing a 12-year interval between loneliness and depressive symptoms (table 4). We found no evidence for a non-linear influence of time on the association between loneliness and depressive symptoms (p=0·40; from interaction between loneliness and quadratic time).
Table 4.
Unadjusted and adjusted change in mean depressive symptom severity score per 1-point increase in loneliness score, according to timepoint
|
Unadjusted |
Fully adjusted* |
|||
|---|---|---|---|---|
| Change in mean score (95% CI) | p value | Change in mean score (95% CI) | p value | |
| Wave three (n=4060) | 0·41 (0·38–0·45) | <0·0001 | 0·19 (0·15–0·23) | <0·0001 |
| Wave four (n=3651) | 0·37 (0·33–0·42) | <0·0001 | 0·15 (0·11–0·19) | <0·0001 |
| Wave five (n=3387) | 0·38 (0·33–0·42) | <0·0001 | 0·16 (0·11–0·20) | <0·0001 |
| Wave six (n=3142) | 0·36 (0·31–0·40) | <0·0001 | 0·14 (0·09–0·18) | <0·0001 |
| Wave seven (n=2751) | 0·37 (0·32–0·41) | <0·0001 | 0·14 (0·10–0·19) | <0·0001 |
| Wave eight (n=2449) | 0·35 (0·01–0·40) | <0·0001 | 0·13 (0·08–0·18) | <0·0001 |
Associations were drawn from multilevel models. The number of participants with complete data on all variables at each wave varies because there were a different number of people with depression data at each wave (due to attrition).
Adjusted for social network size, social contact frequency, participation in social groups, social support, age, sex, ethnicity, marital status, level of education, employment status, wealth, long-term illness, mobility impairment, pain, body-mass index, waist circumference, cognitive function, and depressive symptoms at baseline (wave two).
We found the same pattern of association between loneliness and depression when using a binary depression variable (appendix p 10). The PAF for depression associated with loneliness was estimated to be 18% (95% CI 12–24) at the first follow-up (wave three) and 11% (3–19) at the final follow-up (wave eight).
In the sensitivity analysis, primary outcome results were similar when using a negative binomial model (appendix pp 13–14). In panel analyses using a time-varying loneliness exposure, primary outcome results were similar, though the association was stronger and there was no evidence that it reduced with time (appendix p 15). Primary and secondary outcomes remained similar when including the CES-D loneliness item (appendix pp 16–19). 95% CIs overlapped with those in the primary analysis but PAFs were slightly higher when including the CES-D loneliness item (23% [95% CI 17–28] at the first follow-up and 16% [8–22] at the final follow-up). In the multiple imputation analyses, results were similar and we found the same pattern of the association remaining but attenuating as follow-up progressed (appendix pp 20–21).
Discussion
In this large, prospective cohort of adults aged 50 years and older, loneliness was associated with increased severity of depressive symptoms over a 12-year follow-up period, independent of objective social isolation, social support, and other potential confounders including polygenic risk scores. The size of the association reduced as follow-up progressed, but loneliness remained associated with increased severity of depressive symptoms 12 years later.
To our knowledge, this study is the first large, longitudinal investigation with multiple waves of follow-up and a nationally representative sample of older adults to adjust for a broad range of social experiences related to, but distinct from, loneliness. We adjusted for polygenic risk scores along with other confounders which, as far as we know, most previous studies have not accounted for. The repeated assessments of depression every 2 years allowed us to investigate the persistence of associations between loneliness and depression over a 12-year follow-up period.
We used self-reported depression measures, which could lead to more measurement error than clinical interviews. However, we would expect such measurement error to be random with respect to our hypotheses. Depressive symptoms exist as a continuum and symptom measures capture variation in severity, as well as increasing statistical power and reducing observer bias. The CES-D has shown high sensitivity and specificity in similar community samples.35 There are also potential limitations in how we assessed loneliness. For example, there are distinctions between emotional and social loneliness, and it is possible the R-UCLA scale focuses on emotional loneliness.3 Alternative scales such as the De Jong Gierveld scale can be separated into social and emotional loneliness factors, allowing comparisons between the two.3
Attrition is a limitation of all cohort studies. Our complete case sample with data on all variables differed systematically from the overall sample, which could lead to bias. In sensitivity analyses using multiple imputations our findings were unaltered, suggesting they were unlikely to be due to selection bias. Although we cannot be certain that data were missing at random (an assumption of multiple imputation), the large amount of data in ELSA allowed us to identify several variables associated with missingness, supporting the plausibility of the missing-at-random assumption. We cannot exclude the possibility that data were missing not at random, which could lead to biases not corrected by multiple imputation. For example, if participants with more severe loneliness and depressive symptoms were more likely to drop out over time, and this was not corrected in imputations, it could have reduced the size of our associations or accounted for the decline in the association over time. Systematic attrition would affect the representativeness of the sample. In our imputations we used a population weight to increase representativeness, and this did not change our findings. Although broadly representative of the population of England, the proportion of ethnic-minority participants in ELSA was small, and in the sample we used for analyses, all participants were white. ELSA is also not representative of the institutionalised population of England.
Although we adjusted for a wide range of confounders, as with any observational study, we cannot exclude the possibility of residual confounding. Polygenic risk scores for depression and loneliness account for a modest proportion of genetic variance, and although our adjustment for these scores is a methodological advancement, we cannot exclude the possibility of residual genetic confounding. Another potential limitation is that some variables that were adjusted for at baseline, such as depressive symptoms and physical health problems, could have been mediators rather than confounders, which might have resulted in underestimation of associations between exposure and outcome. Adjusting for variables that might follow loneliness (and share common causes with depression) might also cause collider bias. However, collider bias is most likely to induce spurious associations or reverse the direction of associations, and we found no indications of this.
Although robust to adjustments, our effect sizes were modest and it is difficult to judge their potential clinical importance. Small effect sizes are, however, likely to be of clinical and public health importance when exposures and outcomes are common. We estimated a PAF for depression related to loneliness of 18% at the 1-year follow-up. This is noteworthy when the complexity of effect sizes is considered. Finally, although we were interested in the long-term association between loneliness and subsequent depression (to inform preventive interventions for depression, which are urgently needed), there is evidence of a bidirectional relationship between loneliness and depression.22, 27, 28 This bidirectional relationship has implications for mechanisms and interventions, and further work on this issue is needed.
Our finding that loneliness is associated with increased risk of subsequent depressive symptoms is consistent with most other large population-based cohort studies.19, 25, 26, 27, 28 The finding is inconsistent with one study, which used a 7-year follow-up, although the cohort studied was relatively small and could have been statistically underpowered.29
Little is known about causal mechanisms underlying the association between loneliness and depression. Our observation that loneliness remained associated with depressive symptoms 12 years later could have arisen because the adverse consequences of loneliness persist, because loneliness persists, or because depressive symptoms are often chronic. Loneliness is thought to involve a perceived absence of companionship, meaningful connections, sense of belonging, or empathic understanding. There is evidence that loneliness can lead to cognitive malfunctions, for example increased vigilance towards threatening social stimuli and negative cognitive biases.7 People who are lonely are more likely to anticipate negative social interactions, recall negative social memories, and make negative evaluations of themselves and the social context. Loneliness could be associated with the development of negative beliefs about one's self, which are associated with depression. Experiences of companionship, belongingness, and meaningful connections are usually rewarding, and reduced experience of social rewards has been associated with depression.41 Loneliness might also have biological effects on the stress response that might increase risk of depression, for example impaired immune function or hypothalamic–pituitary–adrenal axis activity.
Clinicians should be aware of loneliness as a potential risk factor for depression, assess for signs of loneliness in older adults, and consider strategies to address this loneliness. Such strategies could include social prescribing, psychological therapies which target negative cognitions, social skills training, psychoeducation, and supported socialisation (offering people support and guidance to select and attend activities).4 Many primary care clinicians feel that depression among older adults is attributable to loneliness or social isolation and that strategies to address this are scarce.42 There is evidence that psychological therapies for loneliness are effective, especially those that target cognitive biases or attributional styles, although more evidence is needed.4
From a public health perspective, our findings suggest that interventions that reduce loneliness could prevent depressive symptoms or make them less severe in older adults. Such public health strategies include approaches that can be delivered to whole communities by local authorities, community-sector organisations, or charities. The approach might involve building community resources, strengthening networks within neighbourhoods, community connectors in primary care, or arts and sports-based approaches embedded in communities.4 There is also evidence that new technologies and community-engaged arts interventions could be promising tools to reduce loneliness in older populations.43 Our evidence suggests that building relationships and meaningful connections should be a key part of these strategies.
In conclusion, loneliness was associated with increased risk of subsequent depression or increased depressive symptom severity, independent of other aspects of social relationships (ie, even among people who were not socially isolated or who felt socially supported), and that this increased risk persisted for up to 12 years after loneliness was reported. Interventions that target social isolation and social support could reduce loneliness by improving the quality of relationships and increasing companionship, meaningful connections, belongingness, and empathic understanding. Although tackling loneliness effectively will be a complex task, it has important potential to reduce or even prevent future depressive symptoms in older adults.
Data sharing
ELSA data, including individual participant data and data dictionaries, are publicly available. Researchers can download de-identified ELSA data from all waves, including the Health Survey for England, from the UK Data Service.
Acknowledgments
Acknowledgments
ELSA was developed by a team of researchers based at University College London, NatCen Social Research, the Institute for Fiscal Studies, and the University of Manchester. The data were collected by NatCen Social Research. The study is funded by the National Institute on Aging (grant R01AG17644) and by a consortium of UK Government departments coordinated by the NIHR. EP, SJ, GeL, FM, AP, FS, ASo, and GlL receive funding from the NIHR University College London Hospitals Biomedical Research Centre; EP, SJ, and AP are funded by the UKRI Loneliness and Social Isolation in Mental Health Network. The views expressed in this publication are those of the authors and not necessarily those of the National Health Service, NIHR, or Department of Health and Social Care.
Contributors
GeL, SLL, and EP conceptualised the manuscript, with input from all authors. GeL and SLL designed the study and wrote the statistical analysis plan, with input from all authors. GeL and SLL analysed the data and drafted the first version of the manuscript. All authors read, drafted, and critically revised the whole report. GeL acts as guarantor for the manuscript.
Declaration of interests
GeL, AP, and SJ report grants from the UK Research and Innovation (UKRI) Loneliness and Social Isolation in Mental Health Network, outside the submitted work. ASo reports grants from Wellcome Trust, outside the submitted work. OA is funded by the National Institute for Health Research (NIHR; post-doctoral fellowship 2018-11-ST2-020). All other authors declare no competing interests.
Supplementary Material
References
- 1.Rodda J, Walker Z, Carter J. Depression in older adults. BMJ. 2011;343 doi: 10.1136/bmj.d5219. [DOI] [PubMed] [Google Scholar]
- 2.Yu B, Zhang X, Wang C, Sun M, Jin L, Liu X. Trends in depression among adults in the United States, NHANES 2005–2016. J Affect Disord. 2020;263:609–620. doi: 10.1016/j.jad.2019.11.036. [DOI] [PubMed] [Google Scholar]
- 3.Wang J, Lloyd-Evans B, Giacco D. Social isolation in mental health: a conceptual and methodological review. Soc Psychiatry Psychiatr Epidemiol. 2017;52:1451–1461. doi: 10.1007/s00127-017-1446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mann F, Bone JK, Lloyd-Evans B. A life less lonely: the state of the art in interventions to reduce loneliness in people with mental health problems. Soc Psychiatry Psychiatr Epidemiol. 2017;52:627–638. doi: 10.1007/s00127-017-1392-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Victor CR, Yang K. The prevalence of loneliness among adults: a case study of the United Kingdom. J Psychol. 2012;146:85–104. doi: 10.1080/00223980.2011.613875. [DOI] [PubMed] [Google Scholar]
- 6.Russell DW. UCLA Loneliness Scale (version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66:20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- 7.Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40:218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Erzen E, Çikrikci Ö. The effect of loneliness on depression: a meta-analysis. Int J Soc Psychiatry. 2018;64:427–435. doi: 10.1177/0020764018776349. [DOI] [PubMed] [Google Scholar]
- 9.Luanaigh CÓ, Lawlor BA. Loneliness and the health of older people. Int J Geriatr Psychiatry. 2008;23:1213–1221. doi: 10.1002/gps.2054. [DOI] [PubMed] [Google Scholar]
- 10.Barger SD, Messerli-Bürgy N, Barth J. Social relationship correlates of major depressive disorder and depressive symptoms in Switzerland: nationally representative cross sectional study. BMC Public Health. 2014;14:273. doi: 10.1186/1471-2458-14-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beutel ME, Klein EM, Brähler E. Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry. 2017;17:97. doi: 10.1186/s12888-017-1262-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carandang RR, Shibanuma A, Kiriya J. Determinants of depressive symptoms in Filipino senior citizens of the community-based ENGAGE study. Arch Gerontol Geriatr. 2019;82:186–191. doi: 10.1016/j.archger.2019.02.014. [DOI] [PubMed] [Google Scholar]
- 13.Richard A, Rohrmann S, Vandeleur CL, Schmid M, Barth J, Eichholzer M. Loneliness is adversely associated with physical and mental health and lifestyle factors: results from a Swiss national survey. PLoS One. 2017;12 doi: 10.1371/journal.pone.0181442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh A, Misra N. Loneliness, depression and sociability in old age. Ind Psychiatry J. 2009;18:51–55. doi: 10.4103/0972-6748.57861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peltzer K, Pengpid S. Loneliness correlates and associations with health variables in the general population in Indonesia. Int J Ment Health Syst. 2019;13:24. doi: 10.1186/s13033-019-0281-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Theeke LA. Sociodemographic and health-related risks for loneliness and outcome differences by loneliness status in a sample of U.S. older adults. Res Gerontol Nurs. 2010;3:113–125. doi: 10.3928/19404921-20091103-99. [DOI] [PubMed] [Google Scholar]
- 17.Gan P, Xie Y, Duan W, Deng Q, Yu X. Rumination and loneliness independently predict six-month later depression symptoms among Chinese elderly in nursing homes. PLoS One. 2015;10 doi: 10.1371/journal.pone.0137176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tiikkainen P, Heikkinen R-L. Associations between loneliness, depressive symptoms and perceived togetherness in older people. Aging Ment Health. 2005;9:526–534. doi: 10.1080/13607860500193138. [DOI] [PubMed] [Google Scholar]
- 19.Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging. 2010;25:453–463. doi: 10.1037/a0017216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holvast F, Burger H, de Waal MMW, van Marwijk HWJ, Comijs HC, Verhaak PFM. Loneliness is associated with poor prognosis in late-life depression: longitudinal analysis of the Netherlands study of depression in older persons. J Affect Disord. 2015;185:1–7. doi: 10.1016/j.jad.2015.06.036. [DOI] [PubMed] [Google Scholar]
- 21.McHugh Power J, Hannigan C, Hyland P, Brennan S, Kee F, Lawlor BA. Depressive symptoms predict increased social and emotional loneliness in older adults. Aging Ment Health. 2020;24:110–118. doi: 10.1080/13607863.2018.1517728. [DOI] [PubMed] [Google Scholar]
- 22.Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol Aging. 2006;21:140–151. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- 23.Button KS, Ioannidis JPA, Mokrysz C. Power failure: why small sample size undermines the reliability of neuroscience. Nat Rev Neurosci. 2013;14:365–376. doi: 10.1038/nrn3475. [DOI] [PubMed] [Google Scholar]
- 24.Sjöberg L, Östling S, Falk H, Sundh V, Waern M, Skoog I. Secular changes in the relation between social factors and depression: a study of two birth cohorts of Swedish septuagenarians followed for 5 years. J Affect Disord. 2013;150:245–252. doi: 10.1016/j.jad.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 25.Beutel ME, Brähler E, Wiltink J. New onset of depression in aging women and men: contributions of social, psychological, behavioral, and somatic predictors in the community. Psychol Med. 2019;49:1148–1155. doi: 10.1017/S0033291718001848. [DOI] [PubMed] [Google Scholar]
- 26.Domènech-Abella J, Mundó J, Haro JM, Rubio-Valera M. Anxiety, depression, loneliness and social network in the elderly: longitudinal associations from The Irish Longitudinal Study on Ageing (TILDA) J Affect Disord. 2019;246:82–88. doi: 10.1016/j.jad.2018.12.043. [DOI] [PubMed] [Google Scholar]
- 27.Luo Y, Hawkley LC, Waite LJ, Cacioppo JT. Loneliness, health, and mortality in old age: a national longitudinal study. Soc Sci Med. 2012;74:907–914. doi: 10.1016/j.socscimed.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hsueh YC, Chen CY, Hsiao YC, Lin CC. A longitudinal, cross-lagged panel analysis of loneliness and depression among community-based older adults. J Elder Abuse Negl. 2019;31:281–293. doi: 10.1080/08946566.2019.1660936. [DOI] [PubMed] [Google Scholar]
- 29.Stessman J, Rottenberg Y, Shimshilashvili I, Ein-Mor E, Jacobs JM. Loneliness, health, and longevity. J Gerontol A Biol Sci Med Sci. 2014;69:744–750. doi: 10.1093/gerona/glt147. [DOI] [PubMed] [Google Scholar]
- 30.Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry. 2000;157:1552–1562. doi: 10.1176/appi.ajp.157.10.1552. [DOI] [PubMed] [Google Scholar]
- 31.Boomsma DI, Willemsen G, Dolan CV, Hawkley LC, Cacioppo JT. Genetic and environmental contributions to loneliness in adults: the Netherlands twin register study. Behav Genet. 2005;35:745–752. doi: 10.1007/s10519-005-6040-8. [DOI] [PubMed] [Google Scholar]
- 32.Day FR, Ong KK, Perry JRB. Elucidating the genetic basis of social interaction and isolation. Nat Commun. 2018;9 doi: 10.1038/s41467-018-04930-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lewis CM, Vassos E. Polygenic risk scores: from research tools to clinical instruments. Genome Med. 2020;12:44. doi: 10.1186/s13073-020-00742-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Steptoe A, Breeze E, Banks J, Nazroo J. Cohort profile: the English longitudinal study of ageing. Int J Epidemiol. 2013;42:1640–1648. doi: 10.1093/ije/dys168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Briggs R, Carey D, O'Halloran AM, Kenny RA, Kennelly SP. Validation of the 8-item Centre for Epidemiological Studies Depression Scale in a cohort of community-dwelling older people: data from The Irish Longitudinal Study on Ageing (TILDA) Eur Geriatr Med. 2018;9:121–126. doi: 10.1007/s41999-017-0016-0. [DOI] [PubMed] [Google Scholar]
- 36.Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci USA. 2013;110:5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. Int Psychogeriatr. 1999;11:139–148. doi: 10.1017/s1041610299005694. [DOI] [PubMed] [Google Scholar]
- 38.Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Miratrix LW, Sekhon JS, Theodoridis AG, Campos LF. Worth weighting? How to think about and use weights in survey experiments. Polit Anal. 2018;26:275–291. [Google Scholar]
- 40.Sterne JAC, White IR, Carlin JB. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338 doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lewis G, Kounali DZ, Button KS. Variation in the recall of socially rewarding information and depressive symptom severity: a prospective cohort study. Acta Psychiatr Scand. 2017;135:489–498. doi: 10.1111/acps.12729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Frost R, Beattie A, Bhanu C, Walters K, Ben-Shlomo Y. Management of depression and referral of older people to psychological therapies: a systematic review of qualitative studies. Br J Gen Pract. 2019;69:e171–e181. doi: 10.3399/bjgp19X701297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Poscia A, Stojanovic J, La Milia DI. Interventions targeting loneliness and social isolation among the older people: an update systematic review. Exp Gerontol. 2018;102:133–144. doi: 10.1016/j.exger.2017.11.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
ELSA data, including individual participant data and data dictionaries, are publicly available. Researchers can download de-identified ELSA data from all waves, including the Health Survey for England, from the UK Data Service.