Abstract
Introduction:
Obesity interventions may be most effective if they begin in the earliest stages of life, support changes across family, clinical, and public health systems, and address socio-contextual factors.
Methods:
The First 1000 Days is a systematic program starting in early pregnancy lasting through the first 24 months of infancy to prevent obesity among low-income mother-infant pairs in three community health centers in Massachusetts. The program uses a Collective Impact approach to create the infrastructure for sustained, system-wide changes for obesity prevention across early life clinical and public health services, including Obstetrics, Pediatrics, Adult Medicine, Behavioral Health, Nutrition, Community Health, the Women, Infants and Children (WIC) program, and the Maternal, Infant and Childhood Home Visiting program. Program components include 1) staff and provider training; 2) enhanced gestational weight gain and infant overweight tracking; 3) universal screening of adverse health behaviors and socio-contextual factors; 4) universal patient navigation to support individual behavior change and social needs, while strengthening integration of clinical and public health services; 5) individualized health coaching for mother-infant pairs at high risk of obesity; and 6) educational materials to support behavior change.
Results:
A quasi-experimental evaluation design will examine changes, between 2015 and 2019, in gestational weight gain and prevalence of infant overweight from 0 to 24 months of age.
Conclusions:
The First 1000 Days program will examine the effectiveness of an early life obesity prevention program for mother-infant pairs. If successful, the program could provide a model for chronic disease prevention and health promotion among vulnerable families starting in early life.
Keywords: Collective Impact, Obesity, Intervention
1. Introduction
Obesity represents a major threat to public health and results in significant excess burden of chronic diseases, health and societal costs, and adverse quality of life [1]. Evidence suggests that disparities in childhood obesity prevalence emerge in early life and can be influenced by factors in the “First 1000 Days” – pregnancy though 24 months of age [2–4]. Substantial evidence also suggests that obesity interventions may be most effective if they begin in the earliest stages of life, support changes across family, clinical, and public health systems, and address socio-contextual factors [5].
The First 1000 Days program was co-created by a diverse set of stakeholders working in early life clinical and public health services, including Obstetrics, Pediatrics, Adult Medicine, Behavioral Health, Nutrition, Community Health, the Women, Infants and Children (WIC) program, and the Maternal, Infant and Childhood Home Visiting program. The aims are to develop, implement, and evaluate a comprehensive, systematic program to prevent obesity among low-income mother-infant pairs during pregnancy and early infancy. Recognizing that system-wide changes to achieve improved health outcomes require a highly structured and collaborative effort, the program uses a “Collective Impact” approach to create the infrastructure for sustainable, systems-level changes. Collective Impact (CI) is defined as “the commitment of a group of important actors from different sectors to a common agenda for solving a specific social problem” [6–8].
The theoretical model underlying this work is the multi-dimensional society-behavior-biology nexus described by Glass & McAtee, which depicts multi-level influences on health behaviors starting in early life and which has been applied to obesity [9]. Effective interventions for addressing obesity require multi-sector strategies that invoke change in intermediary factors at the individual, family, social environment, and systems-levels [10]. The CI approach employs multidisciplinary stakeholder engagement around a common agenda, use of shared metrics of success, continuous communication, and mutually reinforcing activities. These four elements coupled with backbone support for the initiative, are conditions that together can produce true alignment of efforts and lead to sustained results. We have used the CI framework to build cross-sector collaboration and establish a common agenda of obesity prevention in early-life clinical and public health services co-located at three community health centers, which has in turn informed the design of the First 1000 Days program to reduce obesity risk factors among low-income mother-infant pairs and close the gap in obesity disparities. Table 1 describes the five CI elements and the corresponding First 1000 Days program activities.
Table 1.
Collective Impact strategy and design for obesity prevention in the First 1000 Days.
| Collective impact condition | Description | First 1000 days activity |
|---|---|---|
| Common agenda | A shared vision for change that includes a common understanding of the problem and a joint approach to solving it through agreed upon actions. | ■ Stakeholders from each early life clinical and public health sectora agree on the primary goal of the initiative to improve the prevalence of obesity/overweight and obesity-related outcomes among mother-infant pairs. |
| Shared measurement system | A common system for collecting data, reporting performance, and measuring outcomes. | ■ Identify a list of measures for maternal and infant health and social outcomes, including gestational weight gain and infant weight and length |
| ■ Universal electronic health record | ||
| Mutually reinforcing activities | A set of activities that each stakeholder undertakes that supports and is coordinated with the actions of others. | ■ Develop a list of sector-specific activities that fit together and reinforce an overarching plan of obesity prevention |
| ■ Train all clinical and public health providers in early life obesity prevention | ||
| ■ Develop signage and educational materials with consistent messaging for use in prenatal and pediatric sectors | ||
| Continuous communication | Flowing communication between and within each system/sector. | ■ Regularly scheduled meetings with stakeholders to identify opportunities and strategies for early life obesity prevention |
| ■ Quarterly newsletters with program information and tracking | ||
| ■ Monthly Executive Committee meetings to inform program implementation and ensure continuous quality improvement | ||
| ■ Shared web-based file repository for all program materials | ||
| Backbone support | Separate organization and staff coordinates the entire initiative and provides supporting infrastructure. | ■ Core intervention team provides overall coordination, organizes and leads meetings and trainings, facilitates communications support, and tracks program data and progress |
Early life sectors include Obstetrics; Pediatrics; Behavioral Health; Nutrition; Community Health; the Women, Infants and Children program; and the Maternal, Infant and Childhood Home Visiting program.
2. Methods
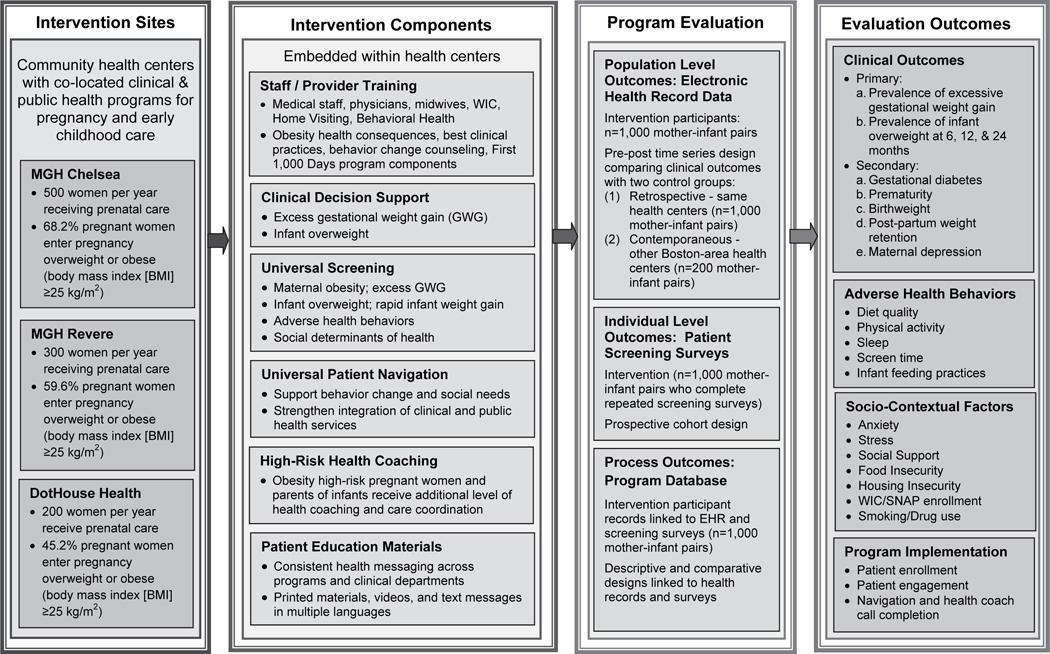
The First 1000 Days program is a systems-level initiative that engages stakeholders across clinical and public health sectors via the Collective Impact process to reduce the prevalence of obesity and obesity risk factors among low-income mother-infant pairs by addressing the levels of individual, family, and socio-contextual factors that hinder progress in obesity prevention (Fig. 1). The program’s system-wide interventions start with women seeking prenatal care in their first trimester of pregnancy and supports the mothers, their partners, and later the mother-partner/father-infant triads, throughout the first 24 months of age. Given implementation across the entire population, the program uses a combination of pre-post time series and quasi-experimental designs to evaluate whether the intervention results in improved anthropometric and behavioral outcomes among mother-infant pairs and their families during the first 1000 days. Interventions at the systems-level are purposely targeted to promote sustainability. The First 1000 Days study protocol was approved by the Partners Health-Care Institutional Review Board.
Fig. 1.
Logic model for the First 1000 Days program.
The First 1000 Days program is being conducted in three community health centers serving predominantly low-income, racial/ethnic minority populations in Revere, Chelsea, and Dorchester, MA. All three communities have higher percentages of low-income residents than the state as a whole and childhood obesity rates substantially higher than the state-wide average (Table 2). The community health centers were selected for their patient demographics, as well as for their affiliation with Massachusetts General Hospital or the Kraft Center for Community Health, which provided a clinician champion to lead the efforts at each community health center.
Table 2.
Characteristics of population in the community health centers participating in the First 1000 Days program.
| Community demographics | Massachusetts | Revere, MA | Chelsea, MA | Dorchester, MA |
|---|---|---|---|---|
| Total population1 | 6,705,586 | 53,095 | 37,581 | 141,537 a |
| Race/ethnicity1 | ||||
| % White alone | 74.3% | 60.1% | 24.4% | 20.1% a |
| % Black or African American alone | 6.5% | 4.3% | 5.3% | 46.1% a |
| % Hispanic or Latino (any race) | 10.6% | 26.4% | 64.2% | 17.7% a |
| % High School graduate or higher1 | 89.8% | 82.2% | 65.4% | 79.5%a |
| Median family income in past 12 months for families with own children1 | $88,727 | $51,213 | $43,000 | $36,402 b |
| % Families with related children under 5 years living below poverty level1 | 12.3% | 28.3% | 22.7% | 22.3% a |
| % Children living in households with public assistance in past 12 months1 | 22.8% | 30.4% | 49.8% | 54.3% b |
| % Children under 18 years in renter-occupied housing1 | 34.5% | 52.1% | 79.1% | 75.9% b |
| % Foreign born1 | 15.5% | 34.9% | 44.0% | 32.6% a |
| % Language other than English spoken at home1 | 22.5% | 48.5% | 69.9% | 40.7% a |
| % of students in 1st, 4th, 7th, and 10th grade children with a BMI ≥ 85th percentile | 31.3%2 | 44.5%2 | 38.5%3 | Unavailable |
| Health center population demographics | ||||
| Women receiving prenatal care per year | 71,4844,c | 3245 | 5075 | 2007 |
| % Women entering pregnancy overweight or obese (body mass index [BMI] ≥25 kg/m2) | 44.8%4 | 59.6%5 | 68.2%5 | 49.2%7 |
| Women who gained adequate weight during pregnancy based on IOM guidelines and pre-pregnancy BMI, among term pregnancies | Unavailable | 34.9%4 | 35.3%4 | 33.0%7 |
| Infant Overweight Rates (weight-for-length z-score > 2SDs) | ||||
| 6 Month Well-Visit | Unavailable | 1.4%6 | 4.2%6 | 4.7%8 |
| 12 Month Well-Visit | Unavailable | 3.7%6 | 11.2%6 | 7.0%8 |
| 24 Month Well-Visit | Unavailable | 9.7%6 | 15.3%6 | 14.6%8 |
BMI: Body Mass Index; IOM: Institute of Medicine.
2011–2015 American Community Survey 5-year estimates.
Massachusetts Department of Public Health, The Status of childhood weight in Massachusetts, 2014.
Massachusetts Department of Public Health, The Status of childhood weight in Massachusetts, 2009–2011.
Massachusetts Department of Public Health, Massachusetts Births 2015.
Massachusetts General Hospital internal data, July 2012–June 2013.
Massachusetts General Hospital internal data. Includes infants whose mothers delivered at MGH, sample sizes vary by visit age.
DotHouse internal data, Jan 2013-Dec 2013.
Dothouse internal data. Includes infants born Jan 2012-Dec 2012, sample sizes vary by visit age.
Combines zip codes 02121, 02122, 02124 and 02125, weighted by population.
Combines zip codes 02121, 02124 and 02125, weighted by population of children in households. Zip code 02122 data not available.
Number of women who gave birth in 2015.
We engaged early life clinical and public health program leaders co-located in the community health centers to participate as stakeholders in our Collective Impact approach to the design and implementation of the First 1000 Days program. The stakeholder group met biannually for Collective Impact meetings and representatives from each sector met for monthly Executive Committee meetings specific to each health center in order to provide feedback and ensure continuous quality improvement. This process generated the following program components:
(1) Staff and provider training to standardize obesity prevention across early life sectors. We held interactive, group training sessions and provided coaching to assist with implementation of evidence-informed practices within the context of each participating sector. The sessions and coaching were held at the health centers and included physicians, clinical staff such as nurses or medical assistants, administrative leaders, community health workers, and representatives from WIC and the Home Visiting programs. Training was customized by the staff or provider role, and when appropriate was delivered to multi-disciplinary groups. Training included: 1) epidemiology and health consequences of maternal obesity, excess gestational weight, infant overweight, and early life risk factors for obesity; 2) effective interventions and best practices for reducing excess gestational weight gain and accelerated infant weight gain; [5] 3) methods of encouraging health behavior change, including motivational interviewing; [11,12] and 4) orientation to the First 1000 Days pregnancy and pediatric program components and materials.
(2) Enhanced tracking of excess gestational weight gain and surveillance of infant overweight. Clinical decision supports were utilized in the electronic health records (EHRs) of the participating health centers. In pregnancy, the EHR gestational weight gain (GWG) graph plots maternal weight gain/loss against and gestational age. Based on each woman’s pre-pregnancy body mass index (BMI) category, the EHR auto-populates the GWG graph with lines showing the minimum and maximum weight gain recommended by the Institute of Medicine over the course of pregnancy [13]. The First 1000 Days program trained obstetric care providers in use of the GWG graphs as visual tools to assist with counseling prenatal patients about their personal GWG trajectory and avoiding excess GWG.
In pediatric care, growth charts plotting infant weight gain by age in months were already being utilized by the clinicians and public health programs. The First 1000 Days program added patient navigators who track at 4 and 9 months of age whether infants have crossed two or more major percentile curves since 1 month of age or attained a weight-for-length at the 97.7th percentile on the World Health Organization weight-for-length curves [14]. Navigators alert clinical providers as well as home visitors and WIC counselors about infants who meet these accelerated infancy weight gain criteria.
(3) Universal screening for health behaviors and socio-contextual factors. The First 1000 Days program instituted systematic screening in the prenatal and pediatric offices for intermediate factors influencing obesity risk – these health behaviors and socio-contextual elements were informed by literature-based evidence as well as on-the-ground experience of stakeholders familiar with the health center populations. All patients receiving obstetric care and their partners if present are offered a self-administered screening survey completed via iPad or paper at the prenatal intake visit, and at one health center again in the third trimester.
In pregnancy, domains surveyed include intake of fruit and vegetable, sugar sweetened beverages, and fast food; physical activity; screen time; sleep; food and housing security; social support; stress and pregnancy anxiety; and eligibility for WIC and the Supplemental Nutrition Assistance Program (SNAP). In pediatrics, screening is completed by the mother/father/care-giver present at the 1 month, 6 month, and 12 month well-child care visits and assesses infant feeding and sleep; behavior and temperament; developmental milestones; home visiting program participation; and parental relationship status and depression screening. Screening surveys are distributed at check-in by front desk staff, are available in English, Spanish, Vietnamese, and Arabic, and take approximately 10–15 minutes to complete. First 1000 Days Patient Navigators use the results to connect patients and partners to individualized health information, health center programs, and community resources. Survey results are transferred to the EHR to facilitate and standardize communication between the clinical providers and public health programs.
(4) Patient navigation. First 1000 Days patient navigators work with pregnant women, partners, and infant caregivers to support healthy behavior change, social needs, and strengthen integration of clinical and public health services. All women and participating partners receive a telephone call from a patient navigator in their first trimester to discuss recommendations for healthy gestational weight gain with a focus on diet, physical activity, screen time, sleep, and stress according to the individual’s screening survey responses. In infancy, the navigation calls occur at approximately 1–2 months and 6–9 months and focus on healthy infant feeding practices and infant sleep recommendations.
During the phone calls, patient navigators refer participants to health center programs that support healthy behaviors and social-emotional health and community resources to address social determinants of health such as food and housing insecurity. All patients are sent a personalized resource guide by mail or email summarizing the information discussed on the phone call and any additional resources that may be of assistance to the family. Navigators make a follow up call approximately two weeks after the initial call to assess referral completion and if any further education or support resources are indicated. Calls are summarized in the EHR, enabling coordination of care across providers and programs.
(5) Individual health coaching. First 1000 Days patient navigators also provide additional health coaching for mother-infant pairs with increased risk of excess GWG and/or infant overweight. Any woman with a pre-pregnancy BMI ≥ 30 or with high weight gain in early pregnancy is flagged as high-risk for excess GWG and receives up to two additional health coach calls during pregnancy, as well as calls when their child is approximately 2 months, 4 months, and 9 months old to continue supporting the family health environment after pregnancy. In infancy, children are flagged as high-risk after their 4 or 9 month well-child care visits if they are overweight (weight-for-length ≥ 97.7th percentile) or have rapid weight gain (crossing 2 or more major growth percentiles) [15]. The caregivers of these infants receive health coaching calls, which review recommendations around healthy infant weight using a motivational interviewing approach to develop behavior change goals, create a plan, and address barriers to success. Health coaches follow up with patients to evaluate their progress and make any necessary adjustments to the patient’s goals. These calls are also summarized in the EHR.
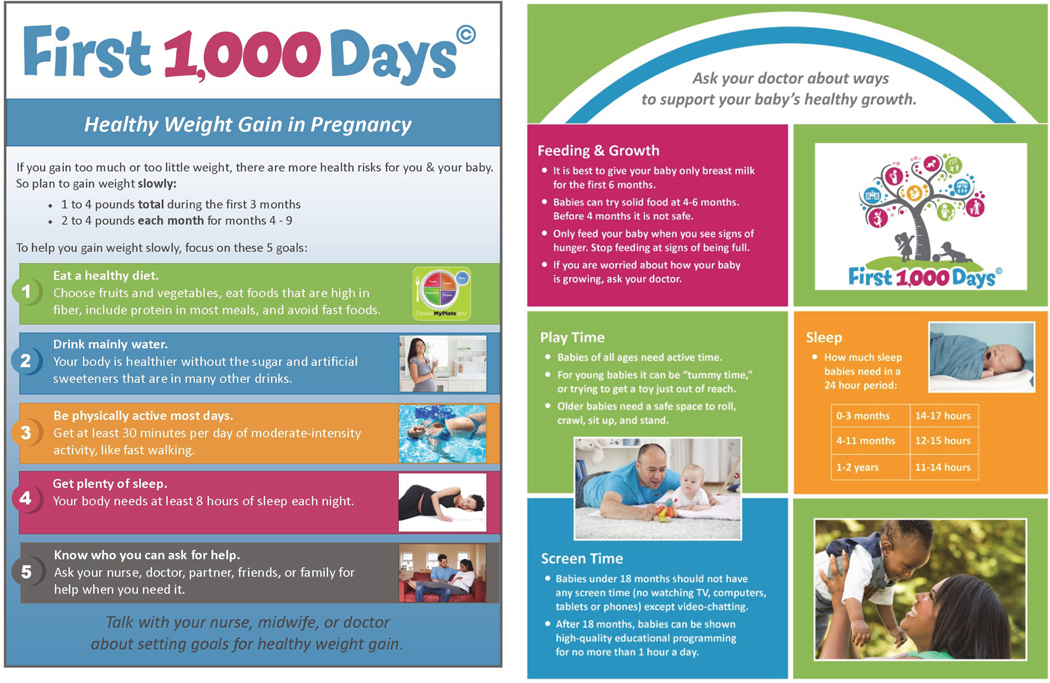
(6) Multi-media health education and support. The First 1000 Days Program focuses on five healthy behavior targets during pregnancy: 1) eat a healthy diet, 2) drink mainly water, 3) be physically active most days, 4) get plenty of sleep, and 5) reduce stress. In infancy, behavioral targets focus on healthful feeding habits, soothing techniques, age-appropriate sleep and screen time, and developmentally appropriate play and parent engagement. Feeding recommendations include: 1) breastfeed exclusively for 6 months, 2) if giving any formula, measure formula accurately as directed on the label, and 3) recognize hunger and satiety cues and feed accordingly.
Printed educational materials were created with the primary purpose of providing consistent messaging across health center sectors around healthy behaviors during pregnancy and infancy (Fig. 2). Materials included posters throughout health center clinical and public health offices and individual booklets provided to patients – available in English, Spanish, Vietnamese, and Arabic with health information relevant to distribution at first and third trimester prenatal visits, the 6-week postpartum visit, and at the 0–1 month, 2–4 month, 4–6 month, 6–9 month, 9–12 month, and 12–24 month well-child care visits – to promote health behavior targets and goal-setting.
Fig. 2.
Waiting room and exam room posters for Obstetrics and Pediatrics.
The First 1000 Days program created a text message library to provide additional health education and support between health center visits. Women and their partners are offered enrollment in the text message campaign during prenatal care or at the child’s 1 month well-child visit. The text message program sends 2–3 automated text messages per week during pregnancy and the child’s first 2 years of life. Topics include the health behavior targets described above, encouragements for positive behavior changes, and links to social and community resources. Infancy messages include links to the Boston Basics [16]. Messages are sent using Mobile Commons, a web-based platform, and are available in English and Spanish [17].
Additionally, we developed over 50 short informational videos (Vidscrips®) in English and Spanish to reinforce program health messages, and weblinks to the videos were provided to women and partners throughout the program. The videos provide answers to common questions around pregnancy weight gain, diet, exercise, etc., as well as maternal depression, smoking, and gestational diabetes. Public health program staff are featured in videos focusing on resources such as WIC, farmers markets, behavioral health, and support services specific to fathers. Videos for infancy include topics such as sleep, feeding (breastfeeding, formula, and introduction of solids), hunger and satiety cues, screen time, soothing, and active time for infants.
During implementation of the program components described above, modifications and enhancements were made in response to stakeholder and health center staff feedback provided as part of the Collective Impact process.
3. Results
The impact of the First 1000 Days program on prevention of obesity in mother-infant pairs during pregnancy and the first 2 years of infancy is strengthened by its multifactorial, systems-level approach, however these methods also create challenges for program evaluation, as there may be effects both on the entire health center population through changed systems, as well as on individual participants utilizing specific components of the program. The First 1000 Days program evaluation seeks to assess the implementation and impact of the overall program and its components at the individual (maternal-child) level and the health center population level, using clinical and program databases from 2015 to 2019, and a set of analytic study designs.
The First 1000 Days evaluation addresses three inter-related questions: 1) Is the implementation of First 1000 Days program associated with improvements of maternal and infant obesity-related outcomes at the level of the health center population?; 2) Is participation in the First 1000 Days program’s targeted activities associated with individual level improvements in self-reported maternal and infant health, obesogenic behaviors, and obesogenic social environments?; And 3) Can the multi-faceted First 1000 Days maternal and infant early life obesity prevention program be successfully implemented and achieve a high level of sustained participation? Three distinct study designs and separate databases will address these three inter-related questions.
First, we will evaluate the impact of the program on clinical measures using a quasi-experimental, longitudinal pre-post time series design with non-treatment comparison controls. Clinical measures from all pregnant women and their infants who receive prenatal or pediatric care at the program’s three health centers will be compared with the same measures from two distinct populations: a retrospective comparison with mothers and infants at the same health centers just prior to the program onset, and a contemporaneous comparison of mothers and infants at two similar non-intervention Boston-area health centers. Maternal and infant obesity-related clinical information is routinely recorded during patient visits in the EHR used at both the intervention and comparison sites. The two primary clinical outcome measures for evaluation are the prevalence of excess GWG and infant overweight.
Second, we will evaluate the impact of the program on individual participants’ maternal and infant health, obesogenic health behaviors, and socio-contextual factors using a prospective cohort study design, exploring variations in intra-program participation. Women and participating partners at the intervention health centers will be asked to complete a screening survey in early and late pregnancy, and at 1 month, 6 months, and 12 months after the birth of their infant. We will use these repeated assessments to examine changes in individual-level behavior and socio-context over time, monitor continued programmatic participation/adherence, as well as ascertain participant perceptions/satisfaction with the First 1000 Days program and its components.
Third, we will evaluate the implementation process and sustainability of the program as an innovative maternal and infant obesity prevention initiative, as well as for the program’s continuous quality management. Detailed process measures are collected and maintained by program staff in a database, which include demographic information, mother-child linkage identifiers, dates of First 1000 Day participation, screening survey completion, participation in program components (text messages, health coaching, etc.), clinical notes of the patient navigators, and a final survey assessing satisfaction with the program overall and its individual components.
Data from the study participant’s EHR and screening survey results are automatically transferred into and linked with the master program database, allowing for analyses across the three evaluative domains described above. Each of the three evaluation approaches will also be examined by subpopulations (socio-demographic groups, initial high or low obesogenic risk, and site of care), and where appropriate, by extent of participation in the First 1000 Days program (duration, intensity, and plurality of programmatic components participation). As such, the integrated comprehensive First 1000 Days program evaluation plan, with its three core study questions and three distinct data bases, is an integral part of the overall First 1000 Days intervention.
4. Discussion
Evidence suggests that reducing the prevalence of obesity risk factors during pregnancy, infancy and early childhood could help close the gap in obesity disparities in mid-childhood [3,18]. We have used the Collective Impact collaborative process to design multi-factorial system-level obesity prevention interventions that operate across early life clinical and public health services at community health centers with high-risk populations for development of childhood obesity.
The First 1000 Days Program is innovative in several ways. First, all intervention components, implementation of systems changes, and monitored outcomes are directly informed by key stakeholders from the early life clinical and public health programs operating at the program’s health centers. The use of a Collective Impact approach to design and implement the program allowed us to identify specific needs and barriers raised by the participating clinicians and programs that interface directly with vulnerable families, and this information was then used to shape and unify broad changes in the health center systems. Second, rather than focus solely on individual lifestyle interventions, our program utilized a life course approach and aimed from its conception to influence obesity risk factors at systems-, family- and individual-levels to achieve maximal impact. Third, few prior interventions have focused specifically on the earliest stages of life – the first 1000 days – to begin obesity prevention efforts, and none have taken a family-focused approach that includes fathers. Fourth, our program leverages existing clinical health information technology to link families across clinical disciplines and public health programs, resulting in more effective, efficient, and coordinated care for families around early life health care. Finally, the Collective Impact model for stakeholder engagement and systems change sets the foundation for sustainability and continued evolution of the First 1000 Days program in the future.
4.1. Limitations
Despite the strengths of the program, there are also limitations. By intention, the First 1000 Days interventions are implemented across a variety of health center clinical and public health programs and providers, which inevitably includes some degree of variability in program component administration and utilization. Given the many life stressors in low-resource populations, even a multi-factorial and multi-level program cannot address all risk factors or barriers they experience. A randomized controlled study design was not feasible given the program objective for system-wide changes, thus our chosen analytic approaches are necessarily subject to confounding in evaluating program impact, yet may be more representative of real-world conditions for program implementation.
5. Conclusion
The First 1000 Days program used a Collective Impact approach to develop, refine, and implement an intervention that leverages early life clinical systems and public health resources to improve obesity prevention among vulnerable family units. The multi-faceted intervention components of the First 1000 Days program provide the foundation for a model of early life obesity prevention that could be widely disseminated as we strive to improve health outcomes for children and their families most at risk in Massachusetts and across the US.
Acknowledgements
We thank the institutions, research staff and students for their dedication to the First 1,000 Days Program.
Research reported in this publication was supported by The Boston Foundation, Massachusetts General Hospital for Children, and the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number K24DK105989. The content is solely the responsibility of the authors and does not necessarily represent the official views of the sponsors.
All authors contributed to the conception and design of the study. Tiffany Blake-Lamb drafted the article, with significant contributions by Elsie Taveras, Etna Tiburcio, Brianna Roche, Meghan Perkins, Sarah Price, and Milton Kotelchuck. Alexy Arauz Boudreau, Sarah Matathia and Derri Shtasel revised the article for important intellectual content.
This study is registered at www.clinicaltrials.gov NCT03191591.
No financial disclosures were reported by the authors of this paper.
Clinical trials
The First 1000 Days Program: Maternal-Child Obesity Prevention in Early Life (NCT03191591), June 2017. This study is supported by The Boston Foundation (G2015-0007), Massachusetts General Hospital for Children, and the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health. Partners Human Research Committee (P2016P000801), approved 5/12/2016.
Conflict of interest statement
This research was funded by The Boston Foundation and the NIH. The sponsors had no role in the study design; collection, analysis and interpretation of data; writing of report; or decision to submit for publication. The authors have no individual conflicts of interest to report.
Footnotes
Financial disclosure
The authors have no financial disclosures to report.
References
- [1].Collaborators TGO. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med0(0):null. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Taveras EM, Gillman MW, Kleinman K, Rich-Edwards JW, Rifas-Shiman SL, Racial/ethnic differences in early-life risk factors for childhood obesity, Pediatrics 125 (4) (April 2010) 686–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Taveras EM, Gillman MW, Kleinman KP, Rich-Edwards JW, Rifas-Shiman SL, Reducing racial/ethnic disparities in childhood obesity: the role of early life risk factors, JAMA Pediatr. 167 (8) (August 01 2013) 731–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Woo Baidal JA, Locks LM, Cheng ER, Blake-Lamb TL, Perkins ME, Taveras EM, Risk factors for childhood obesity in the first 1,000 days: a systematic review, Am. J. Prev. Med 50 (6) (February 8 2016) 761–779. [DOI] [PubMed] [Google Scholar]
- [5].Blake-Lamb TL, Locks LM, Perkins ME, Woo Baidal JA, Cheng ER, Taveras EM, Interventions for Childhood Obesity in the First 1,000 Days A Systematic Review, Am. J. Prev. Med 50 (6) (2016. February 8) 780–789 pii: S0749–3797(15)00750–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Kania J, Kramer M, Collective impact, Stanf. Soc. Innov. Rev 9 (1) (2011) 36–41. [Google Scholar]
- [7].Hanleybrown F, Kania J, Kramer M, Channeling change: making collective impact work, Stanf. Soc. Innov. Rev (2012), https://ssir.org/articles/entry/channeling_change_making_collective_impact_work. [Google Scholar]
- [8].Boyce B, Collective impact: aligning organizational efforts for broader social change, J. Acad. Nutr. Diet 113 (4) (April 2013) 495–497. [DOI] [PubMed] [Google Scholar]
- [9].Glass TA, McAtee MJ, Behavioral science at the crossroads in public health: ex-tending horizons, envisioning the future, Soc. Sci. Med 62 (7) (April 2006) 1650–1671. [DOI] [PubMed] [Google Scholar]
- [10].Huang T, Glass T, Transforming research strategies for understanding and preventing obesity, JAMA 300 (15) (October 15, 2008) 1811–1813. [DOI] [PubMed] [Google Scholar]
- [11].Miller WR, Rollnick S, Motivational Interviewing- Motivational Enhancement Therapy, (2002). [Google Scholar]
- [12].Rollnick S, Miller William R, Butler CC, Motivational Interviewing in Health Care: Helping Patients Change Behavior, Taylor & Francis Group; (2008). [Google Scholar]
- [13].Institute of Medicine, Weight Gain during Pregnancy: Reexamining the Guidelines, National Academies Press, Washington DC, 2009. [PubMed] [Google Scholar]
- [14].World Health Organization, WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development. Geneva, Switzerland, (2006). [Google Scholar]
- [15].Institute of Medicine, Early Childhood Obesity Prevention Policies, The National Academies Press, Washington, DC, 2011. [Google Scholar]
- [16].The Boston Basics, The Boston Basics, http://boston.thebasics.org/en/ (Accessed: June 20, 20172017).
- [17].Price S, Ferisin S, Sharifi M, et al. , Development and implementation of an interactive text messaging campaign to support behavior change in a childhood obesity randomized controlled trial, J. Health Commun 20 (7) (2015) 843–850. [DOI] [PubMed] [Google Scholar]
- [18].Reis JP, Loria CM, Lewis CE, et al. , Association between duration of overall and abdominal obesity beginning in young adulthood and coronary artery calcification in middle age, JAMA 310 (3) (July 17, 2013) 280–288. [DOI] [PMC free article] [PubMed] [Google Scholar]