Abstract
Objective:
To determine quality of antenatal care (ANC). Most literature focuses on ANC attendance and services. Less is known about quality of care (QoC).
Method:
Data were analyzed from the 2016 Kigoma Reproductive Health Survey, a population-based survey of reproductive-aged women. Women with singleton term live births were included and principal component analysis (PCA) was used to create an ANC quality index using linear combinations of weights of the first principal component. Nineteen variables were selected for the index. The index was then used to assign a QoC score for each woman and linear regression used to identify factors associated with receiving higher QoC.
Results:
A total of 3178 women received some ANC. Variables that explained the most variance in the QoC index included: gave urine (0.35); gave blood (0.34); and blood pressure measured (0.30). In multivariable linear regression, factors associated with higher QoC included: ANC at a hospital (versus dispensary); older age; higher level of education; working outside the home; higher socioeconomic status; and having lower parity.
Conclusion:
Using PCA methods, several basic components of ANC including maternal physical assessment were identified as important indicators of quality. This approach provides an affordable and effective means of evaluating ANC programs.
Keywords: Antenatal, Pregnancy, Prenatal care, Principal component analysis, Quality of care, Tanzania
1 |. INTRODUCTION
Antenatal care (ANC) is critical to promoting the health of mothers and babies. ANC is associated with increased birth weight, increased delivery with a skilled attendant, and reduced maternal mortality.1
Previously, WHO recommended initiation of ANC by 16 weeks and at least four visits for healthy women.2 In 2016, these guidelines were updated and at least eight antenatal contacts with the first occurring by 12 weeks of gestation was recommended.3 The revised guidelines also recommended a package of 39 services within the realms of nutritional interventions, maternal and fetal assessments, preventative measures, interventions for common physiologic symptoms, and health systems interventions to improve utilization and quality of ANC.3 Despite these guidelines, there remains a lack of consensus regarding what the precise make-up and delivery of ANC services should include to promote health and be cost-effective.3,4
Central to the question of the optimal components of ANC is the quality of the health care provided. There are no validated measures of quality of ANC for use in a low-resource context5 and it is believed only one instrument has been psychometrically validated in a high-resource setting.6 In the absence of standardization, multiple authors have used combinations of variables to create indices. Process measures are more easily quantified and often used as proxies for quality.7 Of the few studies regarding quality of health care from sub-Saharan Africa, the majority have created a simple quality index using unweighted averages of a combination of ANC variables.5,8–11 Though simple to implement, equal weighting constricts each variable to be as important as every other and does not adjust for correlation between variables. A single study from Indonesia used more robust statistical methods to attempt to quantify quality of ANC.12
Barriers to participation in ANC in resource-constrained countries include: low educational attainment; being unmarried; lower income; higher parity; uncomplicated prior pregnancies; undesired pregnancy; and decreased accessibility of health facilities.13–15
The aim of the present study was to add to the available literature by constructing a quality index of ANC in a low-resource setting using rigorous statistical methods to identify factors that are associated with higher quality of care (QoC).
2 |. MATERIALS AND METHODS
Data for the present study come from the 2016 Kigoma Reproductive Health Survey (KRHS), a population-based cross-sectional cluster survey of reproductive-aged women in Kigoma Region, Tanzania. The 2016 KRHS enrolled women aged 15–49 years for a face-to-face interview using a structured questionnaire. Sampling occurred in two stages. First, enumeration areas were selected with probability proportional to size. Subsequently, households within the selected enumeration area were randomly selected from a listing. The KRHS survey instrument included questions on demographic characteristics, reproductive health behaviors and attitudes, and knowledge of maternal health services including family planning, and perinatal care. A socioeconomic status (SES) variable was computed from multiple socioeconomic household variables (durable goods, dwelling characteristics, water and sanitation, crowdedness) and terciles were created from the resulting score.16 Interviews were conducted in Kiswahili and were completed in 30–60 minutes. Detailed information on study background and key findings are publicly available.16 Written consent was obtained from participants before the survey interview. Ethical approval was provided by the National Institute for Medical Research in Tanzania as one activity in the Maternal and Reproductive Health in Tanzania Project.
For the present analysis, women with a singleton term live birth were included. Data from only the most recent birth for each woman was used. Stata/SE v14.2 was used for analysis (release 14; StataCorp LP, College Station, TX, USA). First, principal component analysis (PCA) was used to create an ANC quality index using the first component loading. PCA is a multivariate statistical technique that uses correlation between multiple variables to create constructs (“components”) to attempt to identify a subset of variables that collectively represent an underlying construct (e.g. quality of ANC) that cannot be measured directly. The technique collapses a larger number of partially correlated variables into fewer uncorrelated components.17 Variables included in the index were chosen a priori on the basis of their inclusion in the WHO framework of essential components of ANC (Table 1).1 On each component, a load was calculated for each of the input variables. The sign of the load was used to assess positive or negative correlation between that variable and the component. The magnitude of the load was used to assess the contribution of the variable to the given component.
TABLE 1.
Prevalence and loadings on first component for ANC variables in a PCA model.a
| Variable | Prevalence | Loading (first component) | |
|---|---|---|---|
| Proportion explained by first principal component | 0.18 | ||
| 1 | Four or more ANC visits | 1413 (45) | 0.23 |
| 2 | Initiated care by 4 months of pregnancy | 1163 (37) | −0.22 |
| 3 | Weighed at least once | 2931 (92) | 0.23 |
| 4 | Height measured at least once | 2096 (66) | 0.27 |
| 5 | Gave urine sample at least once | 1640 (52) | 0.35 |
| 6 | Gave blood sample at least once | 2213 (70) | 0.34 |
| 7 | Tested for HIV at least once | 2885 (91) | 0.26 |
| 8 | Blood pressure checked at least once | 1506 (48) | 0.30 |
| 9 | Given injection to prevent tetanus at least once | 1767 (55) | 0.07 |
| 10 | Told about pregnancy complications | 1831 (58) | 0.23 |
| 11 | Knew severe vaginal bleeding is a serious health problem that can “endanger the life of a pregnant/postpartum woman” | 1596 (50) | 0.12 |
| 12 | Advised to develop a birth plan | 2771 (87) | 0.24 |
| 13 | Advised to identify transport for delivery | 1084 (34) | 0.20 |
| 14 | Advised to save money for delivery | 1969 (62) | 0.22 |
| 15 | Advised to identify a blood donor | 124 (4) | 0.11 |
| 16 | Advised to identify companion or support person for delivery | 1963 (62) | 0.21 |
| 17 | Advised to sleep under mosquito net treated with insecticide | 2723 (85) | 0.14 |
| 18 | Prescribed antimalarial prophylaxis | 2429 (76) | 0.22 |
| 19 | Counseled about family planning during ANC | 2150 (67) | 0.17 |
Abbreviations: ANC, antenatal care; PCA, principal component analysis.
Values are given as number (percentage).
Each woman’s quality of ANC score was then estimated from the PCA. For ease of interpretation, each quality score was multiplied by 100 and quartiles computed.
The first principal component was theorized to represent quality of ANC. This assumption was tested by examining the direction of the loadings for logical consistency and whether a higher score on the QoC index predicted delivery in a health facility. Logistic regression modeling was used with facility-based delivery as a binary outcome and quartile of ANC score as an independent variable that was forced to remain in the model. A change in estimate approach was used for model construction.18 All variables with P<0.200 in bivariate analysis were entered into a full model. Individually, non-significant variables (P<0.050) were removed from the model but retained if any of the remaining estimates changed by more than 10%. The sampling weights were computed using the inverse of the total probability of selecting a woman in a household and incorporated into the logistic regression model.
Finally, multivariable linear regression modeling was used to identify factors associated with higher quality ANC score. Model selection was performed using the same method described above for the logistic model and sampling weights were used to account for complex survey design. Goodness-of-fit of the linear model was assessed using the R2, plot of residuals, and linktest command in Stata.19 Use of sampling weights excluded estimation of some regression diagnostic parameters but also provided robustness to model misspecification.20
3 |. RESULTS
A total of 6630 households were interviewed from July to September 2016 and 94% of the 7506 eligible women residing in these households completed questionnaires. Of these, 3216 (43%) women had live births in the 5 years preceding the study interview and nearly all (3178, 99%) of these women had some ANC and were therefore included in the analysis. The median age was 28 years (interquartile range [IQR] 23–35). Only 197 (6%) had completed more education than primary school and 1035 (33%) received income (money or goods) for work outside the home in the previous year. Most (2732, 86%) were married or living as married with their partner. Other characteristics of participants are listed in Table 2.
TABLE 2.
Unweighted characteristics of study population (n=3178).
| Variable | |
|---|---|
| Age (years) | 28 (23–35) |
| Education | |
| <Primary | 907 (29) |
| Primary | 2074 (65) |
| >Primary | 197 (6) |
| Worked outside the home | 1035 (33) |
| Married/living as married | 2732 (86) |
| Husband/partner is health decision maker | 1257 (40) |
| Live births | 4 (2–6) |
| Location of ANC | |
| Hospital | 217 (7) |
| Health center | 453 (14) |
| Dispensary | 2457 (78) |
| Other | 30 (1) |
| Delivered in a health facility | 1935 (61) |
| Attend religious services weekly or more frequently | 2580 (81) |
| Source of water | |
| Public tap | 662 (21) |
| Well | 863 (27) |
| Surface water | 1343 (42) |
| Other | 310 (10) |
| Distance to water | |
| On site/<10 min | 669 (21) |
| 10 to <30 min | 1002 (32) |
| 30 to <60 min | 846 (27) |
| +60 min | 661 (21) |
| Electricity in the home | 542 (17) |
| Owns a mobile phone | 2037 (64) |
Abbreviations: ANC, antenatal care; IQR, interquartile range.
Values are given as number (percentage) or median (IQR).
Nineteen variables selected a priori as related to quality of ANC were used in the PCA model (Table 1). There was considerable variation in prevalence of these variables in the sample: over 90% of women were tested for HIV and weighed at least once during ANC, whereas less than half initiated care by 4 months of pregnancy, had four or more ANC visits, or had their blood pressure checked.
Of the 19 variables entered into the full model, all except entry into ANC by the fourth month of pregnancy were positive, indicating positive correlation with quality of ANC score. The variables with the highest loadings on the first component included ever giving a urine or blood sample (0.35 and 0.34, respectively), having blood pressure or height measured at least once (0.30 and 0.27, respectively), being tested for HIV (0.26), and being advised to develop a birth plan (0.24). Variables with the lowest absolute value of the loading included receiving a tetanus vaccination (0.07) and being advised to identify a blood donor (0.11).
ANC quality scores were predicted for each participant from the PCA and multiplied by 100. The median value of the transformed score was 25 (IQR 115–138) and was left-skewed (Fig. 1).
FIGURE 1.

Distribution of transformed quality of care score from principal component analysis.
As a robustness check, it was determined whether the resulting ANC quality score was associated with facility-based delivery. In multivariable logistic regression modeling, ANC quality score predicted delivery in a health facility. Controlling for confounders, with the lowest quartile as the reference group, the second, third, and highest quartile had 2.00, 3.27, and 5.83 higher odds, respectively, of delivery in a health facility (P<0.001 for each group) (Table 3).
TABLE 3.
Results from two regression models.
| Model 1. Logistic regression model with facility-based delivery as outcomea | |||
|---|---|---|---|
| Variable | OR | 95% CI | P |
| Quartile of quality of ANC score computed from PCA | |||
| Lowest | Ref | ||
| Second | 2.00 | 1.55–2.56 | <0.001 |
| Third | 3.27 | 2.45–4.38 | <0.001 |
| Highest | 5.83 | 4.05–8.41 | <0.001 |
| Model 2. Linear regression model with transformed ANC quality score (from PCA) as outcomeb | |||
| Variable | Estimate | 95% CI | P |
| Location of antenatal care | |||
| Hospital | 117 | 94–140 | <0.001 |
| Health center | 52 | −7 to 111 | 0.083 |
| Dispensary | Ref | ||
| Age (1-year increase) | 5 | 3–7 | <0.001 |
| Educational level completed and participation in religious services at least weekly | |||
| No education, no weekly religious participation | −111 | −146 to −77 | <0.001 |
| Primary education, no weekly religious participation | −14 | −37 to 10 | 0.250 |
| More than primary education, no weekly religious participation | 12 | −43 to 68 | 0.657 |
| No education, yes weekly religious participation | −40 | −59 to −20 | <0.001 |
| Primary education, yes weekly religious participation | Ref | ||
| More than primary education, yes weekly religious participation | 52 | 25–79 | <0.001 |
| Worked outside the home in the previous year | 24 | 7–41 | 0.005 |
| Tercile of SES | |||
| First | Ref | ||
| Second | 32 | 17–47 | <0.001 |
| Third | 56 | 34–77 | <0.001 |
| Number of previous live births (1 birth increase) | −11 | −17 to −5 | <0.001 |
| Husband is health decision-maker | −14 | −31 to 3 | 0.110 |
Abbreviations: ANC, antenatal care; CI, confidence interval; OR, odds ratio; PCA, principal component analysis; SES, socioeconomic status.
Other model covariates include: location of ANC, age, level of education, SES tercile, number of previous livebirths, distance to nearest health facility in minutes. Sampling weights used.
Sampling weights used.
Finally, in multivariable linear regression modeling with ANC quality score as the outcome, having received ANC in a hospital (versus dispensary), increasing age, working outside the home in the previous year, higher socioeconomic status, and lower numbers of live births were all associated with higher ANC quality score (Table 3). There was a statistically significant interaction between level of education and participation in religious services at least weekly. In comparison to women who completed primary school and attended religious services at least weekly, those with no education had lower scores, regardless of attendance at religious services. By contrast, of the women who received more than a primary education, only those who also attended weekly services had a higher score. There were no other significant interaction terms.
Model R2 was 0.14. On assessment of residuals, graphically they appeared approximately normally distributed but slightly right-skewed without severe outliers (Fig. 2). Link test revealed non-significant prediction squared, indicating adequate model specification.
FIGURE 2.
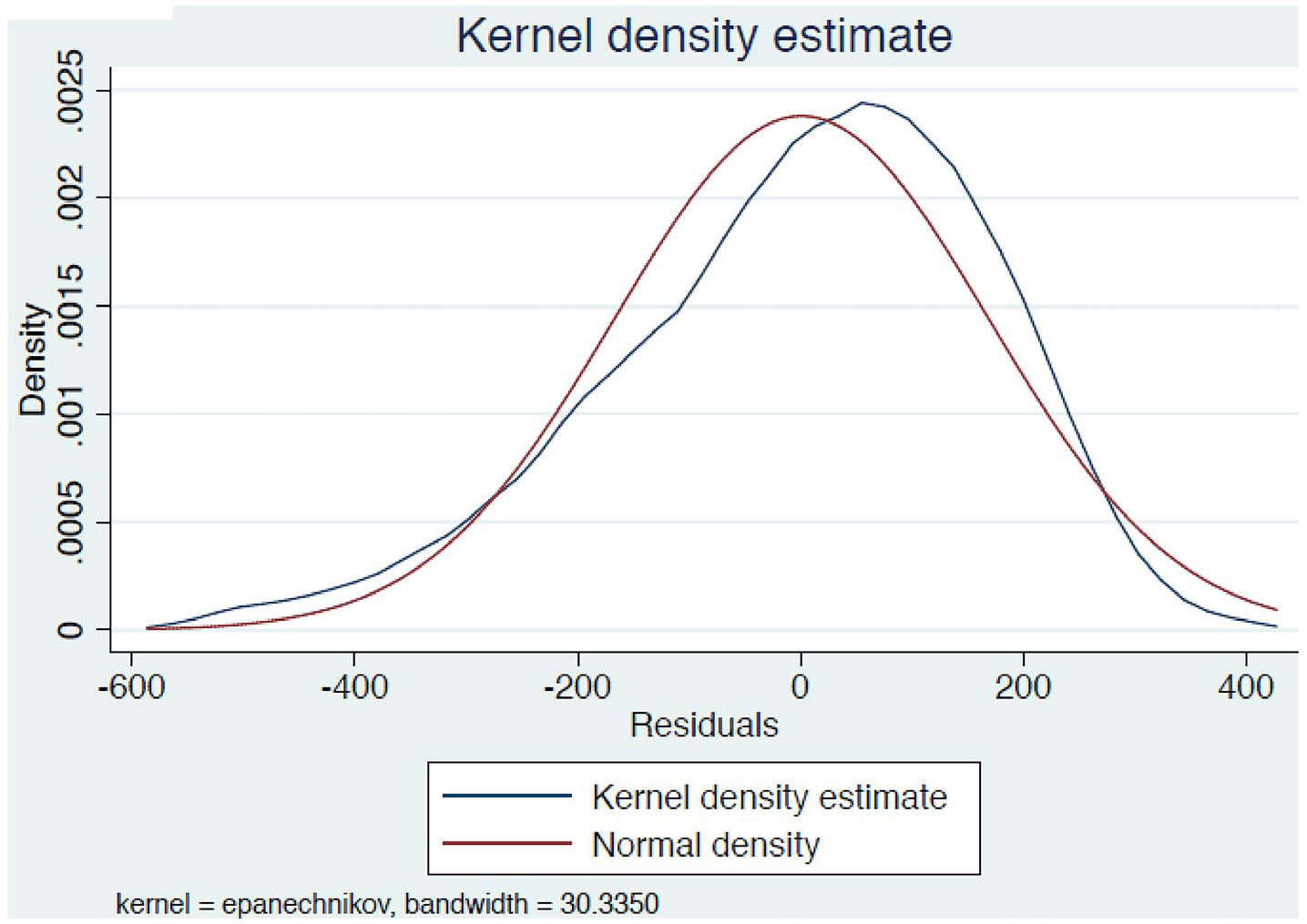
Kernel density estimate.
4 |. DISCUSSION
The present study utilized a robust statistical technique with existing data to create a measure of ANC quality in a low-resource setting and used this measure to identify factors associated with higher quality of ANC score. It was found that multiple basic services, including providing a urine and blood sample and having blood pressure checked, were most associated with higher quality ANC score. Number of visits and timing of initiation of care, having height and weight measured, being tested for HIV, receiving malarial prophylaxis, and reporting receiving key counseling messages about pregnancy complications and birth preparation were also important components of quality. Conversely, receiving a tetanus vaccination, receiving counseling about family planning, and sleeping under a mosquito net were less related to quality of ANC score. This mix of variables differs somewhat from a study12 constructing a quality index using Demographic and Health Survey (DHS) data from Indonesia, which found counseling messages, especially advice related to pregnancy complications and discussion of transportation and place and payment for delivery, had the highest loadings on a quality index. This difference highlights that the mix of individual variables included in a PCA quality model will be unique for each dataset and will vary by region and practice environment. Nevertheless, the PCA methodology may be applied in each individual circumstance to derive quality estimates.
The present analysis goes beyond isolated components of the provision of ANC to consider the larger context of individual, correlated elements. This method may be an inexpensive and comparatively simple way for government and program officials to use existing data to follow quality of ANC at the national or sub-national level. Although some statistical expertise would be required for implementation, most low- and middle-income countries have conducted and analyzed DHS data, which routinely use PCA in the estimation of the wealth index, a key background variable. Furthermore, PCA may be implemented in major statistical packages including SAS, Stata, and SPSS.
The prevalence of the individual quality indicators was variable. Nearly all women report being tested for HIV at least once, but only one-quarter of women both initiated care by 4 months and had at least four visits. Just half of women ever had their blood pressure checked and one-third were advised to identify transport at the time of delivery. Factors identified as having a positive association with ANC quality score included having higher SES and working outside the home. A lower level of education was associated with a lower quality score, but higher educational attainment was only associated with a higher quality score among the subset of women who attended religious services weekly. Previous studies21,22 have found religious affiliation to be associated with utilization of ANC or facility-based delivery but such studies do not typically take into account frequency of attendance. A recent analysis23 of quality of ANC in 91 low- and middle-income countries defined quality as having blood pressure checked and receiving blood and urine testing. In that analysis, among women in low-income countries, 85% had blood pressure measured, 72% had blood sample taken, and 62% had urine samples taken. The authors found sub-national region, urban/rural residence, maternal age and education, and number of ANC visits accounted for much of the variation in QoC. These data and those of the present study indicate opportunities for improvement on basic, fundamental components of ANC and highlight important contributions to variation in quality.
In 2016, WHO published comprehensive recommendations for ANC3 that were adopted by the Tanzanian Ministry of Health in 2018.24 A number of the recommended interventions (or a proxy)— including HIV screening, provision of malaria prophylaxis, screening for asymptomatic bacteriuria, measurement of hemoglobin, and provision of tetanus vaccine—were included in the quality index in the present study and all of these, with the exception of tetanus vaccination, were predictive of a higher quality score.
The updated guidance also recommended eight ANC visits. We chose to use the previous recommendation of four visits because 75% of the births in the present study occurred before the updated guidance and less than 1% of women in the sample had eight or more contacts. In a comment published in The Lancet, Weeks and Temmerman25 suggest, especially in resource-constrained settings, there may be a tension between implementing an aspirational recommendation (such as eight contacts) and improving quality, which is less tangible. There will be continued opportunity to understand how each of these recommendations from WHO contribute to QoC and the methods in the present study could assist policy makers determine their utility in individual settings.
The present study has several limitations. The primary data collection tool did not include data on all ANC components recommended by WHO. All measures of quality were process measures and were self-reported. The proportion of variance explained by the first component was modest at 14%. However, this may be reasonable in light of typical R2 values obtained for PCA utilized in other common scenarios. For example, in a review26 of PCA for creating SES indices, the first component explained 12%–27% of the total variation. Further, the construction of the quality index assumes the first component represents QoC and this cannot be tested empirically, although the PCA model did have logical consistency (with signs of all loadings in the anticipated direction) and was associated with delivery in a health facility. Finally, any index or global measure will necessarily be a simplification of the true underlying construct of quality, which is complex and multifaceted. Nevertheless, the current formulation hopes to improve on even more simplistic earlier representations of ANC quality.
Strengths include the population-based sample and use of data comparable to that collected in the DHS and therefore potentially applicable to a wide range of settings.
Overall, the results from the present study highlight the opportunity to improve ANC and the opportunity to address QoC as a whole rather than as merely discrete components. In a population-based sample of women in western Tanzania, basic components of ANC were identified as drivers of quality. High-quality ANC is one important component in the effort to improve perinatal outcomes for mothers and babies.
ACKNOWLEDGMENTS
We would like to acknowledge the donors (Bloomberg Philanthropies, Fondation H&B Agerup), Dr. Paul Chaote, Kigoma Regional Medical Officer, Ministry of Health, Community Development, Gender, Elderly and Children, Tanzania, CDC/DRH staff Alicia Ruiz and Fernando Carlosama; AMCA Tanzania staff Abdulaziz Ali Msuya and Rose Rusibamayila and their dedicated field work interviewers, and all the women who participated in the study.
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest.
REFERENCES
- 1.Lincetto O, Mothebesoane-Anoh S, Gomez P, Munjanja S. Opportunities for Africa’s Newborns: Practical Data, Policy, and Programmatic Support for Newborn Care in Africa. Cape Town: 2006. www.who.int/pmnch/media/publications/aonsectionIII_2.pdf. Accessed July 29, 2020. [Google Scholar]
- 2.World Helath Organization. Standards for Maternal and Neonatal Care. Geneva, Switzerland: 2007. https://apps.who.int/iris/bitstream/handle/10665/69735/a91272.pdf?sequence=1. Accessed July 29, 2020. [Google Scholar]
- 3.World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva, Switzerland: 2016. https://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-eng.pdf;jsessionid=6807C5A4148CA9AA402A82389486525C?sequence=1. Accessed July 29, 2020 [PubMed] [Google Scholar]
- 4.Carroli G, Rooney C, Villar J. How effective is antenatal care in pre-venting maternal mortality and serious morbidity? An overview of the evidence. Paediatr Perinat Epidemiol. 2001;15(Suppl.1):1–42. [DOI] [PubMed] [Google Scholar]
- 5.McNabb M, Chukwu E, Ojo O, et al. Assessment of the quality of antenatal care services provided by health workers using a mobile phone decision support application in northern Nigeria: A pre/post-intervention study. PLoS One. 2015;10:e0123940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heaman MI, Sword WA, Akhtar-Danesh N, et al. Quality of prenatal care questionnaire: Instrument development and testing. BMC Pregnancy Childbirth. 2014;14:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blanc AK, Diaz C, McCarthy KJ, Berdichevsky K. Measuring progress in maternal and newborn health care in Mexico: Validating indicators of health system contact and quality of care. BMC Pregnancy Childbirth. 2016;16:255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tetui M, Ekirapa EK, Bua J, Mutebi A, Tweheyo R, Waiswa P. Quality of Antenatal care services in eastern Uganda: Implications for interventions. Pan Afr Med J. 2012;13:27. [PMC free article] [PubMed] [Google Scholar]
- 9.Nesbitt RC, Lohela TJ, Manu A, et al. Quality along the continuum: A health facility assessment of intrapartum and postnatal care in Ghana. PLoS One. 2013;8:e81089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diamond-Smith N, Sudhinaraset M, Montagu D. Clinical and perceived quality of care for maternal, neonatal and antenatal care in Kenya and Namibia: The service provision assessment. Reprod Health. 2016;13:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hodgins S, D’Agostino A. The quality-coverage gap in antenatal care: Toward better measurement of effective coverage. Glob Health Sci Pract. 2014;2:173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dettrick Z, Gouda HN, Hodge A, Jimenez-Soto E. Measuring quality of maternal and newborn care in developing countries using demographic and health surveys. PLoS One. 2016;11:e0157110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simkhada B, Teijlingen ER, Porter M, Simkhada P. Factors affecting the utilization of antenatal care in developing countries: Systematic review of the literature. J Adv Nurs. 2008;61:244–260. [DOI] [PubMed] [Google Scholar]
- 14.Fagbamigbe AF, Idemudia ES. Barriers to antenatal care use in Nigeria: Evidences from non-users and implications for maternal health programming. BMC Pregnancy Childbirth. 2015;15:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muhwava LS, Morojele N, London L. Psychosocial factors associated with early initiation and frequency of antenatal care (ANC) visits in a rural and urban setting in South Africa: A cross-sectional survey. BMC Pregnancy Childbirth. 2016;16:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Kigoma Reproductive Health Survey. Kigoma Region, Tanzania; 2016. http://ghdx.healthdata.org/record/tanzania-kigoma-reproductive-health-survey-2016. Accessed December 1, 2018. [Google Scholar]
- 17.Joliffe IT, Morgan BJ. Principal component analysis and exploratory factor analysis. Stat Methods Med Res. 1992;1:69–95. [DOI] [PubMed] [Google Scholar]
- 18.Modeling Greenland S. and variable selection in epidemiologic analysis. Am J Public Health. 1989;79:340–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Z Residuals and regression diagnostics: Focusing on logistic regression. Ann Transl Med. 2016;4:195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li J, Valliant R. Linear regression diagnostics in cluster samples. J Off Stat. 2015;31:61–75. [Google Scholar]
- 21.Mekonnen Y, Mekonnen A. Factors influencing the use of maternal healthcare services in Ethiopia. J Health Popul Nutr. 2003;21:374–382. [PubMed] [Google Scholar]
- 22.Onah HE, Ikeako LC, Iloabachie GC. Factors associated with the use of maternity services in Enugu, southeastern Nigeria. Soc Sci Med. 2006;63:1870–1878. [DOI] [PubMed] [Google Scholar]
- 23.Arsenault C, Jordan K, Lee D, et al. Equity in antenatal care quality: An analysis of 91 national household surveys. Lancet Glob Health. 2018;6:e1186–e1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.United Republic of Tanzania Ministry of Health, Community Development, Gender, Elderly and Children: Antenatal Care Guidelines. 2018. Available by request.
- 25.Weeks A, Temmerman M. New WHO antenatal care model-quality worth paying for? Lancet. 2016;388:2574–2575. [DOI] [PubMed] [Google Scholar]
- 26.Vyas S, Kumaranayake L. Constructing socio-economic status indices: How to use principal components analysis. Health Policy Plan. 2006;21:459–468. [DOI] [PubMed] [Google Scholar]


