Abstract
Background
Accumulating evidence suggests the presence of cognitive impairment in patients with major depressive disorder (MDD), which affects their psychosocial function and quality of life (QoL). PERFORM-J (Prospective Epidemiological Research on Functioning Outcomes Related to MDD in Japan) is an observational, multicenter study to assess longitudinal changes in depressive symptoms, psychomotor speed, subjective cognitive function, and psychosocial function.
Methods
Five hundred and eighteen Japanese outpatients with MDD initiating new antidepressant monotherapy (first-line or switch from previous drug) as part of their routine medical care participated in this study. Assessments at baseline and over the 6-month observation period included physician-rated depression severity (Montgomery–Åsberg Depression Rating Scale), psychomotor speed (Digit Symbol Substitution Test; DSST), subjective cognition (Perceived Deficits Questionnaire–Depression), psychosocial function (Sheehan Disability Scale), and QoL (EuroQol-5 Dimension-5 Level).
Results
Antidepressant treatment for 6 months improved depressive symptoms and subjective cognitive impairment (cognitive complaints), whereas psychomotor speed remained impaired (ie, DSST total score was >1 standard deviation below the norm) in 35.6% of patients at 6 months. Impairment of subjective cognition, but not psychomotor speed at month 2 was associated with poor psychosocial function and QoL at 6 months. There was a trend for higher relapse rates at 6 months in patients with greater subjective cognitive impairment at 2 months.
Conclusion
These findings highlight the importance of evaluating cognitive difficulties to predict long-term outcomes in patients with MDD. Early intervention for cognitive complaints may decrease the relapse rate, which warrants further study.
Keywords: cognition, depression, functional outcome, quality of life, Japan
Introduction
Major depressive disorder (MDD) is a common psychiatric condition with debilitating consequences for patients; the estimated 12-month prevalence of MDD in Japan is 2.2%.1,2 Patients with MDD characteristically experience depressed mood and/or lack of interest or enjoyment, in addition to other symptoms, such as changes in appetite, sleep patterns, and energy levels; difficulty thinking, concentrating, and making decisions.3 Some patients rarely or never experience remission, whereas others may have extended periods between episodes.3
During symptomatic episodes and remission phases, cognitive domains, including attention, memory processing speed, and psychomotor skills are often impaired, affecting quality of life (QoL) and psychosocial function in patients with MDD.4–7 Evidence also suggests that impaired cognitive function, particularly executive function and, to a lesser extent, psychomotor function, predicts treatment outcomes in patients with MDD.8 A study conducted in six Asian countries reported subjective memory or concentration deficits in approximately 70% of outpatients with MDD.9 In European patients, the severity of both depressive and cognitive symptoms has been found to be significantly associated with impaired health-related QoL.6 Deficits in patient-reported functioning may also persist after resolution of depressive symptoms.10 Thus, there is growing interest in the relationship between cognitive function, psychosocial function, and QoL in patients with MDD.
The Prospective Epidemiological Research on Functioning Outcomes Related to Major Depressive Disorder study (PERFORM) was a 2-year, non-interventional study conducted in Europe to evaluate the relationship between depressive episodes versus cognitive and psychosocial functions in patients with MDD.11 The results suggested an association between the severity of cognitive impairment, as measured by the 5-item Perceived Deficit Questionnaire (PDQ), and social functioning, as measured by the Sheehan Disability Scale (SDS) and the Work Productivity and Activity Impairment (WPAI) questionnaire. Results from PERFORM also suggested an association between sociodemographic and clinical characteristics versus the likelihood of remission or subsequent relapse. Specifically, residual subjective cognitive impairment, or cognitive complaints, in patients who had achieved remission at month 2 were found to be associated with an increased risk of relapse 4 months later.12 Therefore, further efforts are warranted to evaluate the risk of relapse of depressive symptoms in patients with MDD who experience persistent cognitive impairment after treatment with antidepressants.
Outside Japan, various studies linking cognitive impairment and psychosocial functioning, such as PERFORM, have been conducted in patients with MDD.4,11,13–15 However, data from these studies cannot be generalized to the Japanese population because of differences in several factors, including the prevalence and characteristics of MDD, and cultural attitudes towards it.16,17 For example, the lifetime prevalence of mental disorders in Japan is higher in men whereas persistence of any mental disorder is greater in women, unlike the patterns in Western patients.1 Additionally, the stigma associated with psychiatric disorders, such as MDD, may limit the access to mental healthcare services in Japan compared with other developed countries.1,18
To our knowledge, no studies have explored longitudinal changes in cognitive and psychosocial functioning during treatment in a sizable number of Japanese patients with MDD. Therefore, we conducted the observational, prospective, multicenter, epidemiological PERFORM-Japan study to evaluate the relationship between persistent cognitive impairment and relapse of depressive symptoms in a routine clinical setting (PERFORM-J; UMIN Clinical Trials Registry: UMIN000024320).19 The study design was modified from the original European PERFORM study.11 In PERFORM-J, the longitudinal pattern of subjective cognitive function, objectively measured psychomotor function, and depressive symptoms in Japanese patients with MDD was assessed during depressive episodes and after treatment over 6 months.20 Analysis of baseline data from PERFORM-J demonstrated a correlation between the severity of depressive symptoms and impairment of subjective cognition, both of which were significantly associated with psychosocial function.20 Here we present the results of the longitudinal analysis of the 6-month follow-up data collected in the PERFORM-J study. Our primary hypothesis was that subjective cognitive impairment (cognitive complaints) would deteriorate social function and QoL over time, and increase the risk of relapse in patients with MDD.
Methods
Detailed methods for this study have been published previously.19 Briefly, from September 2016 to June 2017, this observational, prospective, multicenter, epidemiological study enrolled outpatients from 48 psychiatric center study sites (mainly outpatient clinics) in Japan. The study was performed in accordance with the ethical standards described in the Declaration of Helsinki and the Japanese Ethical Guideline for Clinical Research, as well as all other applicable laws and regulations. Ethical review committees approved the study protocol before commencement of the study. Patients were required to provide written informed consent and were free to withdraw from the study at any time.
Study Population
Eligible patients were outpatients aged 18–65 years with a recurrent or new diagnosis of MDD (according to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision),3 confirmed using the Mini International Neuropsychiatric Interview.21 These patients had started antidepressant monotherapy, either as a first-line treatment or had switched medication, as part of their routine medical care.
Study Design
Patients initiated their new antidepressant monotherapy (a selective serotonin reuptake inhibitor, serotonin–norepinephrine reuptake inhibitor, noradrenergic and/or serotonergic antidepressant, or tricyclic or tetracyclic antidepressant) at baseline and were then followed during an observation period of 6 months. Because this study was conducted under routine medical care, augmentation of treatment with other antidepressants and concomitant medications during the follow-up period were permitted by clinical judgment of each physician (eg, in case of insufficient response to antidepressant or occurrence of adverse events).
Assessments
Physician-and patient-reported data were obtained at baseline and 1, 2 and 6 months after patients began antidepressant monotherapy. Physician-rated assessments and patient-reported outcomes are summarized in Supplementary Table S1. Validated Japanese versions of these assessment tools were used for this study. The severity of depressive symptoms and psychomotor speed, as an objective cognitive indicator, were assessed using the physician-rated Montgomery–Åsberg Depression Rating Scale (MADRS) and Digital Symbol Substitution Test (DSST), respectively. Physicians rated the 10 items of the MADRS on a scale of 0 to 6 to give a total score between 0 and 60, with lower scores signifying less severe depressive symptoms. In the DSST, patients were required to substitute 133 digits with a simple symbol within 120 seconds, and the number of correctly placed symbols was counted, giving a total score ranging from 0 to 133, with higher scores indicating better performance. The DSST was not performed at the 1-month study visit.
Subjective (patient-reported) cognition, social function, and QoL were evaluated using self-assessment questionnaires (PDQ–Depression [PDQ-D], SDS, WPAI, and EuroQol-5 Dimension-5 Level [EQ-5D-5L]). Patients reported on the 20 items of the PDQ-D, which cover four domains (attention, retrospective memory, prospective memory and planning/organization), each of which contains five items, over the past 7 days on a scale of 0 (never) to 4 (very often), resulting in a total score of 0 to 80, where lower values correspond to fewer cognitive complaints. In the SDS, patients reported the severity of impairment across three domains (work, social life, and family life/home responsibilities) over the previous 7 days on a scale of 0 to 10, resulting in a total score of 0 (unimpaired) to 30 (highly impaired). In terms of WPAI, patients reported on work time missed (absenteeism), impairment while working (presenteeism), overall work impairment and general activity impairment because of symptoms over the past 7 days. Patients also completed the EQ-5D-5L, which comprises five items (mobility, self-care, usual activities, pain/discomfort and depression/anxiety), yielding a utility score ranging from 0 to the best possible score of 1, and a visual analog scale ranging from 0 to 100 (best overall health state).
Study Objectives
The primary study objective was to evaluate longitudinal changes in subjective cognitive function, psychomotor speed and depressive symptoms in patients with MDD over the course of 6 months, after the start of antidepressant treatment. This was assessed by determining changes from baseline in PDQ-D, DSST, and MADRS scores at each time point. Secondary objectives included evaluating multiple measures to determine the degree of cognitive impairment and depressive symptoms, and assessing the association between cognitive impairment and psychosocial function over the 6-month observation period. Evaluation of whether cognitive impairment provides a risk factor for relapse at 6 months was an exploratory objective. Remission was defined as a MADRS score at follow-up visit ≤10 points. Relapse was defined as a MADRS score of 22 or more at 6 months in patients who had achieved remission at an earlier visit (at 1 or 2 months).
Statistical Analysis
A sample size of 500 patients was estimated to ensure acceptable precision of the mean change from baseline in DSST scores at month 6. Based on two previous clinical studies which investigated the effect of vortioxetine on cognitive function in MDD,22,23 assuming a standard deviation of 8.1 and a withdrawal rate of 25% at month 6, 500 enrolled patients will ensure a value of 0.82 for the half-width of the two-sided 95% confidence interval for the change in DSST score from baseline to month 6. Analyses were conducted for patients who completed the DSST assessment at baseline. Total scores for MADRS and DSST were classified as described previously.20 When categorizing DSST total scores, the norm (normative score) was determined according to values adjusted for age using data from the general Japanese population in relation to the standardized Japanese version of the DSST.24 PDQ-D total scores were classified into four categories by quartiles at 2 months.
A mixed-effects model for repeated measurements was used to assess longitudinal changes in DSST, PDQ-D, and MADRS score using visit as a fixed factor, each score at baseline as a continuous covariate, and interaction between each score at baseline and at each visit. Analysis of variance (ANOVA) was used to assess the association between cognitive function (DSST or PDQ-D) at 2 months (covariate) versus psychosocial function (SDS or WPAI) or QoL (EQ-5D-5L) at 6 months (dependent variable). Other covariates included age (≤40 years/≥41 years), sex (female/male), educational level (up to and including junior college graduate level/university degree or higher), duration of the current depressive episode (<8 weeks/≥8 weeks), concomitant mental disorders (no/yes), comorbid somatic conditions (no/yes), chronic pain (no/yes), and MADRS categories (0–19/20–34/35–60). Multivariate logistic regression analysis was performed to assess relapse at 6 months according to DSST and PDQ-D scores at 2 months as indices of cognitive function. Factors listed above were also used as covariates.
Results
Patient Demographics
Overall, 523 patients were enrolled and provided informed consent. Five patients were excluded from the analysis; four due to prescription of antipsychotics or mood stabilizers at the baseline visit, and one due to a missing baseline DSST assessment. Mean age in the analysis population (n=518) was 37.3 years; 55.6% of patients were female (Table 1).20 Most patients (84.4%) were in paid employment or were self-employed; 88.3% of these patients were working full time (defined as more than 32 hours per week). At study entry, 59.8% of patients were experiencing their first episode of MDD. Of the 208 patients with MDD in relapse, 39 (18.8%) had experienced their last depressive episode within the preceding year. The antidepressants most commonly prescribed at baseline were selective serotonin reuptake inhibitors (40.3%) and serotonin–norepinephrine reuptake inhibitors (33.6%).20 A total of 337 patients completed the 6-month observation period.
Table 1.
Baseline Demographics and Clinical Characteristics
| Total (N=518) | ||
|---|---|---|
| Age, years | Mean (SD) | 37.3 (11.2) |
| Sex, n (%) | Female | 288 (55.6) |
| Education status, n (%) | University degree or higher | 250 (48.3) |
| Up to and including junior college graduate level | 268 (51.7) | |
| Employment status, n (%) | Employed/self-employed | 437 (84.4) |
| Full-time | 386 (88.3)a | |
| Part-time | 51 (11.7)a | |
| Other (unemployed, student, etc.) | 81 (15.6) | |
| History of MDD episodes, n (%) | First episode | 310 (59.8) |
| Relapse | 208 (40.2) | |
| If relapsed, onset time of previous depressive episode, n (%) | Within the last 12 months | 39 (18.8)b |
| Earlier in life | 169 (81.3)b | |
| Time since onset of current depressive episode, n (%) | <8 weeks | 170 (32.8) |
| ≥8 weeks | 348 (67.2) | |
| Antidepressant prescribed at baseline, n (%) | Tricyclic | 31 (6.0) |
| SSRI | 209 (40.3) | |
| SNRI | 174 (33.6) | |
| NaSSA | 61 (11.8) | |
| Other | 43 (8.3) |
Notes: aDenominator is 437 patients in paid employment or self-employed. Full-time was defined as working more than 32 hours per week. bDenominator is 208 patients with relapsed MDD. Adapted from J Affect Disord, Vol 258, Sumiyoshi T, Watanabe K, Noto S, et al. “Relationship of cognitive impairment with psychosocial function and relapse of depressive symptoms in patients with major depressive disorder: Analysis of longitudinal data from PERFORM-J”, 172–178, Copyright (2019), with permission from Elsevier.20
Abbreviations: MDD, major depressive disorder; NaSSA, noradrenergic and specific serotonergic antidepressant; SD, standard deviation; SNRI, serotonin–norepinephrine reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor.
Changes in Depressive Symptoms and Cognitive Function
Mean (standard deviation [SD]) baseline MADRS total score, DSST total score, and PDQ-D total score were 27.0 (8.8), 72.4 (19.2), and 32.2 (15.8), respectively.20 All three measures showed improvements from baseline over the 6-month observation period after initiation of antidepressant administration (Table 2).
Table 2.
Changes from Baseline in MADRS, DSST, and PDQ-D Scores Over 6 Months
| n | Adjusted Mean Changes from Baseline (95% CI) | |
|---|---|---|
| MADRS total score (lower values indicate less severe depressive symptoms)a | ||
| 1 month | 407 | –8.41 (–9.20, –7.62) |
| 2 months | 395 | –12.00 (–12.89, –11.10) |
| 6 months | 337 | –16.05 (–16.99, –15.12) |
| DSST total score (higher values indicate better cognitive function)b | ||
| 2 months | 392 | 6.30 (5.10, 7.50) |
| 6 months | 334 | 8.15 (6.63, 9.68) |
| PDQ-D total score (lower values indicate better cognitive function)c | ||
| 1 month | 396 | –6.78 (–7.77, –5.79) |
| 2 months | 384 | –9.06 (–10.22, –7.90) |
| 6 months | 330 | –11.99 (–13.37, –10.61) |
Notes: aMean MADRS total score was 27.0 at baseline. bMean DSST total score was 72.4 at baseline. cMean PDQ-D total score was 32.2 at baseline.
Abbreviations: CI, confidence interval; DSST, Digital Symbol Substitution Test; MADRS, Montgomery–Åsberg Depression Rating Scale; PDQ-D, Patient Deficit Questionnaire–Depression.
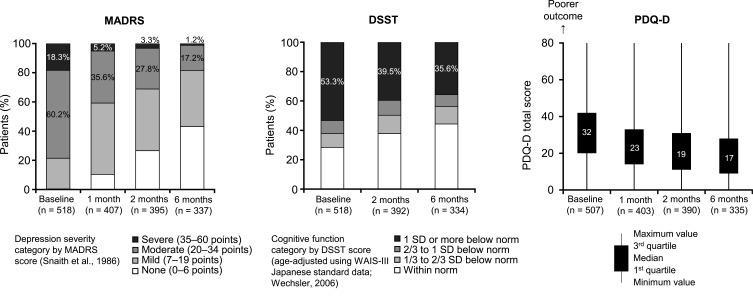
The proportion of patients with a MADRS total score of ≥20 (indicating at least moderate depressive symptoms) was 78.6% at baseline, 40.8% at 1 month, 31.1% at 2 months, and 18.4% at 6 months (Figure 1). Similarly, the proportion of patients with a DSST total score of 1 SD or more below norm decreased from 53.3% at baseline to 39.5% at 2 months and 35.6% at 6 months. Median PDQ-D total scores also decreased from baseline at 1, 2, and 6 months, representing a reduction in cognitive complaints.
Figure 1.
Distributions of MADRS,34 DSST,24 and PDQ-D scores at baseline, and at 1, 2, and 6 months.
Abbreviations: DSST, Digital Symbol Substitution Test; MADRS, Montgomery–Åsberg Depression Rating Scale; PDQ-D, Patient Deficit Questionnaire–Depression; SD, standard deviation; WAIS-III, Wechsler Adult Intelligence Scale-III.
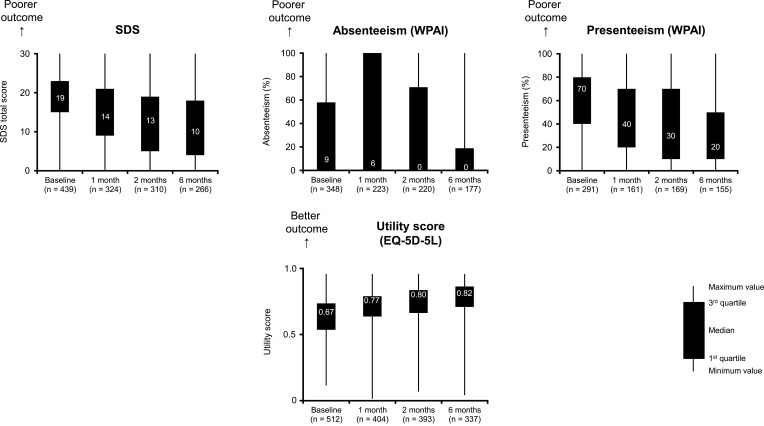
Changes in Psychosocial Function and QoL
Figure 2 shows median baseline scores of the SDS, WPAI (absenteeism and presenteeism), and EQ-5D-5L, as well as changes in these scores over the 6-month observation period after initiation of antidepressant administration. Changes in all four scores indicate a trend for improved outcome over the 6-month period.
Figure 2.
Distribution of scores for psychosocial function and QoL at baseline, and at 1, 2, and 6 months.
Abbreviations: EQ-5D-5L, EuroQol-5 Dimension-5 Level; QoL, quality of life; SDS, Sheehan Disability Scale; WPAI, Work Productivity and Activity Impairment.
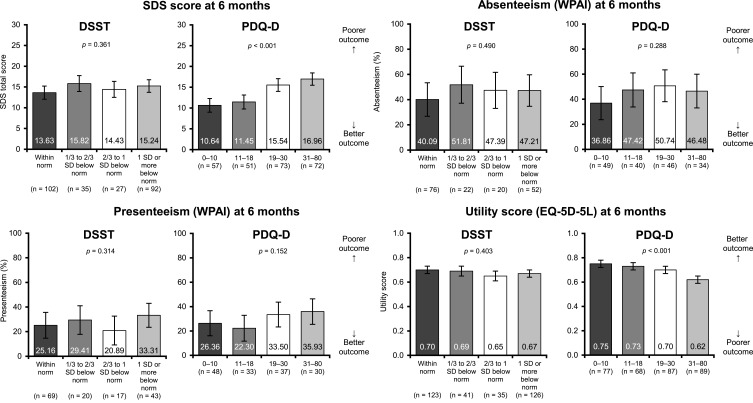
Relationship Between Cognitive Impairment and Psychosocial Function/QoL
The relationship between cognitive difficulties (assessed by DSST and PDQ-D) at 2 months, and psychosocial function and QoL (assessed by SDS, WPAI, and EQ-5D-5L) at 6 months was evaluated by multivariate ANOVA (Figure 3). When adjusting for depression severity and other factors, PDQ-D total score at 2 months was found to predict scores of the SDS (p<0.001) and EQ-5D-5L (p<0.001) at 6 months.
Figure 3.
Relationship between cognitive function (DSST and PDQ-D) at 2 months and psychosocial function (SDS and WPAI) and QoL (EQ-5D-5L) at 6 months. Bars show adjusted means; error bars show standard error. The following factors were used in ANOVA: age, sex, educational level, time since start of current depressive episode, concomitant mental disorders, comorbid somatic conditions, chronic pain, and MADRS scores at baseline, and DSST/PDQ-D total scores at 2 months.
Abbreviations: ANOVA, analysis of variance; DSST, Digital Symbol Substitution Test; EQ-5D-5L, EuroQol-5 Dimension-5 Level; MADRS, Montgomery–Åsberg Depression Rating Scale; PDQ-D, Patient Deficit Questionnaire–Depression; QoL, quality of life; SD, standard deviation; SDS, Sheehan Disability Scale; WPAI, Work Productivity and Activity Impairment.
Factors Associated with Relapse at 6 Months
Relapse was observed in 28 patients at 6 months among 188 patients with remission at 2 months. Table 3 shows the results of multivariate logistic regression analysis of relapse rates at 6 months according to cognitive symptoms (assessed by DSST and PDQ-D) at 2 months. There was a trend for higher rates of relapse at 6 months in patients with higher PDQ-D scores (ie, more severe cognitive complaints) at 2 months. When adjusting for depression severity and other factors, psychomotor speed at 2 months was not associated with relapse rate at 6 months.
Table 3.
Relapse Rate at 6 Months by Degree of Cognitive Function, as Assessed by DSST and PDQ-D at 2 Months
| n | Relapse at 6 Months, n (%) | Multivariate Logistic Regression Analysis | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p value | |||
| DSST total score (2 months) | ||||
| Within norm | 87 | 14 (16.1) | 1 | |
| 1/3 to 2/3 SD below norm | 22 | 3 (13.6) | 0.73 (0.17, 3.12) | 0.670 |
| 2/3 to 1 SD below norm | 24 | 4 (16.7) | 0.73 (0.17, 3.02) | 0.659 |
| 1 SD or more below norm | 54 | 7 (13.0) | 0.92 (0.30, 2.78) | 0.883 |
| PDQ-D total score (2 months) | ||||
| 0–10 | 70 | 4 (5.7) | 1 | |
| 11–18 | 58 | 7 (12.1) | 2.13 (0.53, 8.58) | 0.286 |
| 19–30 | 41 | 11 (26.8) | 4.72 (1.25, 17.90) | 0.022 |
| 31–80 | 17 | 6 (35.3) | 4.95 (0.93, 26.45) | 0.061 |
Notes: The following factors were used in multivariate logistic regression analysis: baseline age, sex, educational level, time since start of current depressive episode, concomitant mental disorders, comorbid somatic conditions, chronic pain, MADRS, and DSST/PDQ-D total scores at 2 months.
Abbreviations: CI, confidence interval; DSST, Digital Symbol Substitution Test; MADRS, Montgomery–Åsberg Depression Rating Scale; PDQ-D, Patient Deficit Questionnaire–Depression; SD, standard deviation.
Discussion
This analysis of longitudinal data for a sizable number of Japanese patients with MDD showed that depressive symptoms and cognitive difficulties improved over 6 months after initiation of treatment with antidepressants. Specifically, changes were evident in subjective cognitive symptoms, or cognitive complaints. Our findings are consistent with those of the Prospective Research Observation to Assess Cognition in Treated patients with MDD (PROACT) study conducted in China,13 which reported improvements in depressive symptoms, as assessed by the 17-item Hamilton Depression Rating Scale and PDQ-D over 6 months after initiation of new antidepressant monotherapy. The improvement in psychomotor speed in the PROACT study appeared less pronounced compared with the improvements seen in other cognitive, depressive, and functional domains over the same timeframe.13 This latter finding from the PROACT study is comparable to the persistent psychomotor dysfunction (DSST total score of 1 SD or more below norm at 6 months) seen in approximately one-third of patients in our study. Our observations are also consistent with the findings of Conradi et al,25 who reported the presence of residual objective cognitive and psychomotor problems even during remission from depressive symptoms in a proportion of patients with MDD.
In the PERFORM-J study, psychomotor speed at 2 months was not associated with psychosocial function or QoL at 6 months. By contrast, subjective cognitive symptoms at 2 months were found to significantly affect both psychosocial function and QoL at 6 months. Similarly, the PROACT study demonstrated that subjective cognitive symptoms at month 2 predicted subsequent functional decline, as assessed by the SDS and WPAI, as well as poor QoL, as assessed by the EQ-5D, at month 6.13 In contrast, psychomotor speed at month 2 only predicted absenteeism and QoL. Our findings also reflect those of the original PERFORM study, which reported a strong association between the severity of subjective cognitive symptoms and functional impairment.11 Furthermore, results from the cross-sectional data of the PERFORM-K (Epidemiological Research on Functioning Outcomes Related to Major depressive disorder in South Korea) study support a relationship between subjective cognition and functional outcomes.4 Taken together, these observations suggest that persistent subjective cognitive problems after 2 months of antidepressant treatment may decrease the likelihood of functional recovery.
The selective association between psychosocial function/QoL and subjective cognition, rather than performance on certain objective measures of cognition, such as psychomotor speed, is in line with previous observations.13,26,27 Compared with subjective assessments of cognition, performance on the DSST may represent different aspects of clinical manifestations in MDD, and appears to be relatively independent of depressive symptoms.20 In contrast, the PDQ-D is a patient-reported questionnaire that focuses on self-perceived changes in cognitive performance in the past week, which tends to be affected by depressive symptoms.20 Given that the SDS, WPAI, and EQ-5D-5L are also subjective patient-reported measures, it would be reasonable to assume that their scores may relate more closely to those of the PDQ-D compared with performance on the DSST.20 Furthermore, whereas the primary symptom of MDD is mood disturbance, which patients recognize subjectively,20 impaired psychomotor function appears to be indicative of a melancholic subtype of MDD.8,28 In general, patients with MDD display a wide range of cognitive deficits,7,8 so evaluation of other domains of cognition, eg, memory and executive function, in addition to attention/psychomotor speed, would have provided us with more comprehensive information to predict functional outcomes.
Subjective cognitive impairment at 2 months tended to predict higher rates of relapse at 6 months, irrespective of depression severity. This finding is consistent with results from another PERFORM study that showed an association between residual subjective cognitive symptoms in patients who achieved remission at month 2 and elicited an increased risk of relapse at month 6.12 Similarly, the PROACT study demonstrated an association between subjective cognitive problems at month 2 and a greater risk of relapse at month 6.13 Collectively, these findings highlight the importance of identifying subjective cognitive symptoms to prevent relapse in patients with MDD. This is relevant not only to the wellbeing but also overall economic burden, which worsens on relapse or recurrence.29
The strength of the PERFORM studies, including PERFORM-J, relates to the real-world settings and longitudinal follow-up procedures. Specifically, data in the PERFORM-J were obtained through assessments of both subjective cognition and objectively assessed psychomotor speed,20 unlike the European PERFORM study, where only subjective components of cognition were evaluated.11 As physician-rated and patient-reported measures may represent different aspects of cognition,30–32 evaluation of both types of cognitive difficulties is desirable to obtain the comprehensive views of functional outcomes. Secondly, all study sites in PERFORM-J were psychiatric centers, allowing both physicians and patients to report clinical symptoms. Lastly, as the Japanese version of the DSST has been standardized,24,33 it was possible to quantify psychomotor performance in relation to that of the general population in the current study. This is in contrast to other PERFORM studies and clinical trials which investigated the impact of antidepressants on psychomotor speed assessed by the DSST, where data on population norms were not available.
As outlined previously,19,20 one of the limitations of this study is that only outpatients were recruited, most of whom had relatively high levels of prior educational attainment, which precludes generalization of the results to Japanese patients with MDD as a whole. Also, patients in this study had started antidepressant monotherapy as part of their routine medical care. As such, administration of concomitant medications, including additional antidepressants, was permitted, which may have influenced cognitive function.
Conclusions
In conclusion, the longitudinal data from the PERFORM-J study indicate the presence of persistent impairment of psychomotor speed in most Japanese patients with MDD. Antidepressant therapy improved depressive symptoms and, to a lesser extent, cognitive complaints (subjective cognitive symptoms). Subjective cognitive symptoms during the initial phase of treatment were associated with poor psychosocial function and QoL at 6 months, whereas a similar relationship between psychomotor speed and psychosocial function was not evident. Impaired subjective cognition at 2 months also tended to increase relapse rates at 6 months. These findings in the real-world setting highlight the importance of identifying subjective cognitive disturbances to predict long-term outcomes in patients with MDD.
Acknowledgments
The authors acknowledge the patients participating in this study and their families, as well as staff at all investigational sites. The authors are also grateful to Takuma Endo, Shuichi Okamoto, Katsuhito Murase, Kentaro Yamato, and Izumi Mishiro at Takeda Pharmaceutical Company Limited for their support with conception of the work, interpretation of the data, or analysis, and to Kristin Hui Xian Tan at Lundbeck Singapore Pte Limited for support with the statistical analysis. Medical writing support was funded by Takeda Pharmaceutical Company Limited, and was provided by Philippa Lloyd and Jenny Wilkinson of FireKite, an Ashfield company, part of UDG Healthcare plc; in accordance with Good Publication Practice 3 ethical guidelines (Battisti et al. Ann Intern Med 2015).
Funding Statement
This study was funded by Takeda Pharmaceutical Company Limited and Lundbeck Japan KK. They were involved in the design of this study and contributed to the development and approval of the present manuscript.
Abbreviations
ANOVA, analysis of variance; CI, confidence interval; DSST, Digital Symbol Substitution Test; EQ-5D-5L, EuroQol-5 Dimension-5 Level; MADRS, Montgomery–Åsberg Depression Rating Scale; MDD, major depressive disorder; NaSSA, noradrenergic and specific serotonergic antidepressant; PDQ-D, Patient Deficit Questionnaire–Depression; PERFORM, Prospective Epidemiological Research on Functioning Outcomes Related to Major Depressive Disorder; PROACT, Prospective Research Observation to Assess Cognition in Treated patients with MDD; QoL, quality of life; SD, standard deviation; SDS, Sheehan Disability Scale; SNRI, serotonin–norepinephrine reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; WAIS-III, Wechsler Adult Intelligence Scale-III; WPAI, Work Productivity and Activity Impairment.
Data Sharing Statement
Takeda makes patient-level, de-identified data sets and associated documents available after applicable marketing approvals and commercial availability have been received, an opportunity for the primary publication of the research has been allowed, and other criteria have been met as set forth in Takeda’s Data Sharing Policy (see www.TakedaClinicalTrials.com for details). To obtain access, researchers must submit a legitimate academic research proposal for adjudication by an independent review panel, who will review the scientific merit of the research and the requestor’s qualifications and conflict of interest that can result in potential bias. Once approved, qualified researchers who sign a data-sharing agreement are provided access to these data in a secure research environment.
Ethics Approval and Consent to Participate
The study was conducted in accordance with the ethical principles described in the Declaration of Helsinki and the Japanese Ethical Guideline for Clinical Research, as well as all other applicable laws and regulations. Ethical review committees were constituted according to the regulations and approved the study protocol at each site before commencement of the study. Ethical review and approval were conducted by the following committees: The Joint Ethical Review Board (Kochi, Japan), the Ethical Review Board of Akita University Graduate School of Medicine and Faculty of Medicine (Akita, Japan), and the Ethical Review Board of Warakukai (Tokyo, Japan). Patients were required to provide written informed consent and were free to withdraw from the study at any time.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
T.S. reports honoraria received for advisory boards/lectures/papers and/or research funding from Takeda Pharmaceutical Company Limited, Sumitomo Dainippon Pharma, Meiji Seika Pharma, Otsuka Pharmaceutical Company Limited, Lundbeck, Ono Pharmaceutical Company Limited, Janssen Pharma, Shionogi Co. Ltd., and VeraSci Inc. K.W. reports consultancies undertaken for Eli Lilly, Otsuka Pharmaceutical Company Limited, Sumitomo Dainippon Pharma, Taisho Toyama Pharmaceutical Company Limited, and Takeda Pharmaceutical Company Limited, honoraria received from Daiichi Sankyo, Eisai, Eli Lilly, GSK, Janssen, Meiji Seika Pharma, Mitsubishi Tanabe Pharma, Mochida Pharmaceutical Company Limited, MSD, Otsuka Pharmaceutical Company Limited, Pfizer, Shionogi, Sumitomo Dainippon Pharma, Tsumura Pharmaceutical Company Limited, and Yoshitomi Pharmaceutical Company Limited, and grants received from Daiichi Sankyo, Eisai, MSD, Mitsubishi Tanabe Pharma, Meiji Seika Pharma, Otsuka Pharmaceutical Company Limited, Sumitomo Dainippon Pharma, and Takeda Pharmaceutical Company Limited. S.N. reports research grants received from Crecon Medical Assessment Inc. S.S. and J.F. are employees of Takeda Pharmaceutical Company Limited. J.F. holds restricted shares from GSK and Takeda Pharmaceutical Company Limited. Y.M. is an employee of Lundbeck Japan KK. L.H-H. is an employee of H. Lundbeck A/S. The authors report no other conflicts of interest in this work.
References
- 1.Ishikawa H, Kawakami N, Kessler RC, the World Mental Health Japan Survey Collaborators. Lifetime and 12-month prevalence, severity and unmet need for treatment of common mental disorders in Japan: results from the final dataset of World Mental Health Japan Survey. Epidemiol Psychiatr Sci. 2016;25(3):217–229. doi: 10.1017/S2045796015000566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. 2013;34(1):119–138. doi: 10.1146/annurev-publhealth-031912-114409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013. doi: 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- 4.Kim JM, Chalem Y, Di Nicola S, Hong JP, Won SH, Milea D. A cross-sectional study of functional disabilities and perceived cognitive dysfunction in patients with major depressive disorder in South Korea: the PERFORM-K study. Psychiatry Res. 2016;239:353–361. doi: 10.1016/j.psychres.2016.01.022 [DOI] [PubMed] [Google Scholar]
- 5.Lam RW, Kennedy SH, McIntyre RS, Khullar A. Cognitive dysfunction in major depressive disorder: effects on psychosocial functioning and implications for treatment. Can J Psychiatry. 2014;59(12):649–654. doi: 10.1177/070674371405901206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saragoussi D, Christensen MC, Hammer-Helmich L, Rive B, Touya M, Haro JM. Long-term follow-up on health-related quality of life in major depressive disorder: a 2-year European cohort study. Neuropsychiatr Dis Treat. 2018;14:1339–1350. doi: 10.2147/NDT.S159276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Semkovska M, Quinlivan L, O’Grady T, et al. Cognitive function following a major depressive episode: a systematic review and meta-analysis. Lancet Psychiatry. 2019;6(10):851–861. doi: 10.1016/S2215-0366(19)30291-3 [DOI] [PubMed] [Google Scholar]
- 8.Groves SJ, Douglas KM, Porter RJ. A systematic review of cognitive predictors of treatment outcome in major depression. Front Psychiatry. 2018;9:382. doi: 10.3389/fpsyt.2018.00382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Srisurapanont M, Bautista D, Chen C-H, Wang G, Udomratn P, Eurviriyanukul K. Subjective memory and concentration deficits in medication-free, non-elderly Asians with major depressive disorder: prevalence and their correlates. J Affect Disord. 2015;171:105–110. doi: 10.1016/j.jad.2014.09.007 [DOI] [PubMed] [Google Scholar]
- 10.IsHak WW, James DM, Mirocha J, et al. Patient-reported functioning in major depressive disorder. Ther Adv Chronic Dis. 2016;7(3):160–169. doi: 10.1177/2040622316639769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hammer-Helmich L, Haro JM, Jönsson B, et al. Functional impairment in patients with major depressive disorder: the 2-year PERFORM study. Neuropsychiatr Dis Treat. 2018;14:239–249. doi: 10.2147/NDT.S146098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saragoussi D, Touya M, Haro JM, et al. Factors associated with failure to achieve remission and with relapse after remission in patients with major depressive disorder in the PERFORM study. Neuropsychiatr Dis Treat. 2017;13:2151–2165. doi: 10.2147/NDT.S136343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang G, Si T-M, Li L, et al. Cognitive symptoms in major depressive disorder: associations with clinical and functional outcomes in a 6-month, non-interventional, prospective study in China. Neuropsychiatr Dis Treat. 2019;15:1723–1736. doi: 10.2147/NDT.S195505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al Jarad A, Al Hadi A, Al Garatli A, et al. Impact of cognitive dysfunction in the middle east depressed patients: the ICMED study. Clin Pract Epidemiol Ment Health. 2018;14(1):270–283. doi: 10.2174/1745017901814010270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manit S, Yee Ming M, Yen Kuang Y, et al. Cognitive dysfunction in Asian patients with depression (CogDAD): a cross-sectional study. Clin Pract Epidemiol Ment Health. 2017;13(1):185–199. doi: 10.2174/1745017901713010185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kanehara A, Umeda M, Kawakami N, the World Mental Health Japan Survey Group. Barriers to mental health care in Japan: results from the World Mental Health Japan Survey: barriers to mental health care in Japan. Psychiatry Clin Neurosci. 2015;69(9):523–533. doi: 10.1111/pcn.12267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ohtsuki T, Inagaki M, Oikawa Y, et al. Multiple barriers against successful care provision for depressed patients in general internal medicine in a Japanese rural hospital: a cross-sectional study. BMC Psychiatry. 2010;10(1):30. doi: 10.1186/1471-244X-10-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kasahara-Kiritani M, Matoba T, Kikuzawa S, et al. Public perceptions toward mental illness in Japan. Asian J Psychiatr. 2018;35:55–60. doi: 10.1016/j.ajp.2018.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sumiyoshi T, Watanabe K, Noto S, Sakamoto S, Moriguchi Y, Okamoto S. Prospective epidemiological research on functioning outcomes related to major depressive disorder in Japan (PERFORM-J): protocol for a prospective cohort study. JMIR Res Protoc. 2018;7(6):e161. doi: 10.2196/resprot.9682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sumiyoshi T, Watanabe K, Noto S, et al. Relationship of cognitive impairment with depressive symptoms and psychosocial function in patients with major depressive disorder: cross-sectional analysis of baseline data from PERFORM-J. J Affect Disord. 2019;258:172–178. doi: 10.1016/j.jad.2019.07.064 [DOI] [PubMed] [Google Scholar]
- 21.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33;quiz 34–57. [PubMed] [Google Scholar]
- 22.Mahableshwarkar AR, Zajecka J, Jacobson W, Chen Y, Keefe RS. A randomized, placebo-controlled, active-reference, double-blind, flexible-dose study of the efficacy of vortioxetine on cognitive function in major depressive disorder. Neuropsychopharmacology. 2015;40(8):2025–2037. doi: 10.1038/npp.2015.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McIntyre RS, Lophaven S, Olsen CK. A randomized, double-blind, placebo-controlled study of vortioxetine on cognitive function in depressed adults. Int J Neuropsychopharmacol. 2014;17(10):1557–1567. doi: 10.1017/S1461145714000546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wechsler D. Wechsler Adult Intelligence Scale. 3rd ed. Nihon Bunka Kagakusha Co. Ltd.; 2006. [Google Scholar]
- 25.Conradi HJ, Ormel J, de Jonge P. Presence of individual (residual) symptoms during depressive episodes and periods of remission: a 3-year prospective study. Psychol Med. 2011;41(6):1165–1174. doi: 10.1017/S0033291710001911 [DOI] [PubMed] [Google Scholar]
- 26.Ott CV, Bjertrup AJ, Jensen JH, et al. Screening for cognitive dysfunction in unipolar depression: validation and evaluation of objective and subjective tools. J Affect Disord. 2016;190:607–615. doi: 10.1016/j.jad.2015.10.059 [DOI] [PubMed] [Google Scholar]
- 27.Potvin S, Charbonneau G, Juster R-P, Purdon S, Tourjman SV. Self-evaluation and objective assessment of cognition in major depression and attention deficit disorder: implications for clinical practice. Compr Psychiatry. 2016;70:53–64. doi: 10.1016/j.comppsych.2016.06.004 [DOI] [PubMed] [Google Scholar]
- 28.Lin K, Xu G, Lu W, et al. Neuropsychological performance in melancholic, atypical and undifferentiated major depression during depressed and remitted states: a prospective longitudinal study. J Affect Disord. 2014;168:184–191. doi: 10.1016/j.jad.2014.06.032 [DOI] [PubMed] [Google Scholar]
- 29.Gauthier G, Mucha L, Shi S, Guerin A. Economic burden of relapse/recurrence in patients with major depressive disorder. J Drug Assess. 2019;8(1):97–103. doi: 10.1080/21556660.2019.1612410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Serra-Blasco M, Torres IJ, Vicent-Gil M, et al. Discrepancy between objective and subjective cognition in major depressive disorder. Eur Neuropsychopharmacol. 2019;29(1):46–56. doi: 10.1016/j.euroneuro.2018.11.1104 [DOI] [PubMed] [Google Scholar]
- 31.Srisurapanont M, Suttajit S, Eurviriyanukul K, Varnado P. Discrepancy between objective and subjective cognition in adults with major depressive disorder. Sci Rep. 2017;7(1):3901. doi: 10.1038/s41598-017-04353-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Svendsen AM, Kessing LV, Munkholm K, Vinberg M, Miskowiak KW. Is there an association between subjective and objective measures of cognitive function in patients with affective disorders? Nord J Psychiatry. 2012;66(4):248–253. doi: 10.3109/08039488.2011.626870 [DOI] [PubMed] [Google Scholar]
- 33.Wechsler D. Wechsler Adult Intelligence Scale. 3rd ed. Psychological Corporation; 1997. [Google Scholar]
- 34.Snaith RP, Harrop FM, Newby DA, Teale C. Grade scores of the Montgomery—Åsberg Depression and the Clinical Anxiety Scales. Br J Psychiatry. 1986;148(5):599–601. doi: 10.1192/bjp.148.5.599 [DOI] [PubMed] [Google Scholar]