Abstract
The presence of non-odontogenic cysts associated with benign fibro-osseous lesions of the jaws has been well documented. However, literature is scant when describing benign fibro-osseous lesions with associated odontogenic cysts. This case report highlights the presence of a concurrent developmental odontogenic cyst, glandular odontogenic cyst with extensive squamous metaplasia, in a patient with florid cemento-osseous dysplasia (COD). The postulated pathogenesis of these synchronous lesions is discussed along with a review of current literature. Surgical treatment is discouraged for florid COD, however, radiological follow-up is recommended, especially in lesions with associated cysts.
Keywords: Benign fibro-osseous lesions, Florid cemento-osseous dysplasia, Odontogenic cysts, Glandular odontogenic cyst
Introduction
Benign fibro-osseous lesions are a group of conditions with overlapping radiological and histological features, characterized by a cellular fibrous stroma with scattered metaplastic bone [1, 2]. This bone may be trabeculae, cementum-like or psammomatoid. The current consensus is that the term ‘cementum’ should be reserved for bone-like substance attached to the root surface of teeth [3]. The evolution of these lesions is responsible for the radiological presentation of firstly a radiolucent lesion, then mixed radiopaque-radiolucent lesion, and finally forming a diffusely radiopaque lesion [2]. Whether or not such lesions ‘mature’ is a subject of much debate.
Cemento-osseous dysplasias (CODs) are a group of non-neoplastic lesions, associated with a strong female predominance, with three clinical and radiological presentations [4]. Focal COD is commonly seen in the mandibular first molar region in female patients in their mid-thirties. Periapical COD is noted in the anterior mandibular region associated with the apices of vital teeth in female patients of African descent. Florid COD involves teeth-bearing regions of both the mandible and maxilla, usually involving multiple quadrants [2].
Odontogenic cysts are classified as either developmental or inflammatory in origin. The glandular odontogenic cyst (GOC) is an aggressive developmental odontogenic cyst with a predilection for middle-aged males. It is common in the mandibular anterior region, where it often crosses the midline, and may present with cortical expansion, root resorption and displacement of teeth [5].
The presence of cysts associated with benign fibro-osseous lesions has been well documented in the literature. The most common cysts are non-odontogenic and non-epithelial lined cysts; i.e. simple bone cysts [6, 7] and aneurysmal bone cysts [8, 9]. Literature is scant when documenting benign fibro-osseous lesions with odontogenic cysts, with only a single case documenting this phenomenon [10]. This report highlights a case of a glandular odontogenic cyst occurring in a patient with florid cemento-osseous dysplasia, and is presented together with a review of the literature. The aim of this review is to document the scarcity of concurrent fibro-osseous lesions occurring with odontogenic cysts.
Case Details
A 43-year-old black female patient, known with retroviral disease, presented with a painless bony protrusion in the left mandibular first molar region and an expansile bony lesion involving the left posterior maxilla, associated with a painful left maxillary first molar. The patient could not recall the initial onset of the lesions. A panoramic radiograph showed multiple mixed radiopaque-radiolucent lesions involving the apices of teeth in both the mandible and maxilla, and a unilocular cystic lesion in the left posterior maxillary region (Fig. 1). Biopsies were performed from both lesions for histological assessment, the clinical diagnosis of the mandibular lesion was a benign fibro-osseous lesion and that of the maxillary cystic lesion was an odontogenic keratocyst.
Fig. 1.

Panoramic radiograph showing the mixed radiolucent/radiopaque lesions involving both the mandible and the maxilla. Additionally, a cystic lesion is noted in the left posterior maxilla
Pathological Findings
Grossly, the mandibular biopsy consisted of two fragments of bone, the largest measuring 11 × 7 × 3 mm. Histological examination showed fragments of vital bone consisting of thick curvilinear trabeculae, giving a so-called ‘ginger root’ appearance, with interspersed fibrovascular connective tissue replacing the marrow spaces (Fig. 2a). Within the fibrous stroma were oval calcifications demonstrating peripheral brush borders and scattered osteoclast-like multinucleate giant cells (Fig. 2b).
Fig. 2.
Haematoxylin and eosin (H&E)-stained section of the bone lesion showing fragments of vital bone consisting of thick curvilinear trabeculae, giving a so-called ‘ginger root’ appearance with interspersed fibrovascular connective tissue replacing the marrow spaces (a). The stroma is cellular with oval calcifications demonstrating peripheral brush borders and scattered osteoclast-like multinucleate giant cells (b)
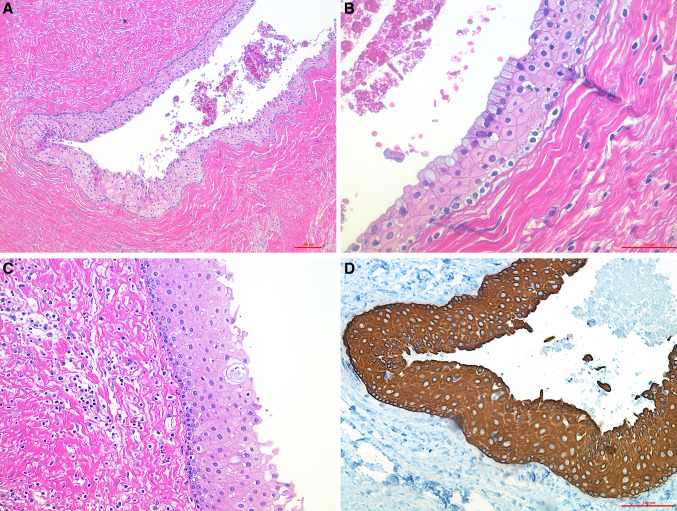
The maxillary biopsy comprised of a cyst measuring 28 × 18 mm, with an average wall thickness of 3 mm. Multiple histological sections showed a cyst lined by epithelium of varying thickness showing prominent squamous metaplasia (Fig. 3a). Within the epithelium, were scattered mucous cells and focal areas of intraepithelial duct-like structures (Fig. 3b). The superficial layer of the epithelium showed prominent hobnailing with areas of ciliated cells (Fig. 3c). This epithelium was confirmed to be odontogenic in origin via positive cytokeratin 19 (CK19) immunohistochemical staining (Fig. 3d). The wall of the cyst consisted of dense fibrous connective tissue with scattered inactive odontogenic epithelial islands. In addition, there were cementum-like bony spicules and numerous cholesterol clefts with an associated foreign body giant cell reaction. Break-apart fluorescence in-situ hybridization was negative for the MAML2 rearrangement (Z-2014-200, Zytovision, Germany) (Fig. 4).
Fig. 3.
Haematoxylin and eosin (H&E)-stained section showing the maxillary cyst lined by epithelium of varying thickness showing prominent squamous metaplasia (a). The epithelial lining shows prominent superficial hobnailing with areas of ciliated cells and scattered mucous cells (b). Intra-epithelial cyst is noted (c). Cytokeratin 19 (CK19) immunohistochemical staining of the epithelium confirming odontogenic origin (d)
Fig. 4.

Fluorescence in-situ hybridization (FISH) using MAML2 dual colour break-apart probe is negative for the MAML2 rearrangement
The combined radiological and histological features were diagnostic of florid cemento-osseous dysplasia, as it involved all four quadrants, with a concurrent glandular odontogenic cyst in the maxilla.
Discussion
The presence of cysts associated with benign fibro-osseous lesions has been well documented in the literature. The most common cysts are non-odontogenic and non-epithelial lined cysts; i.e. simple bone cysts [6, 7] and aneurysmal bone cysts [8, 9]. Literature is scant when documenting benign fibro-osseous lesions with odontogenic cysts. A PubMed (www.pubmed.org) and Google Scholar search of the English literature showed one case report of cemento-osseous dysplasia with an associated dentigerous cyst [10].
In the current case, the diagnosis of florid COD was straight-forward on radiographic and histological examination, however the cystic lesion in the maxilla prompted further exploration. Histological differential diagnoses that were considered included a glandular odontogenic cyst (GOC), squamous odontogenic tumour (SOT) with cystic degeneration, and a central mucoepidermoid carcinoma (MEC). A residual radicular cyst with mucous metaplasia was also considered due to the extracted left maxillary first molar.
The histological diagnosis of a GOC follows major and minor criteria as described by Fowler et al. [11]. In the current case, the diagnosis was based on five (5/5) major and two (2/4) minor criteria which included a squamous epithelial lining with a flat connective tissue interface lacking basal cell palisading, epithelium of varying thickness with focal luminal proliferations, hobnail cells, mucous cells, intraepithelial microcysts, ciliated cells and clear cells in the basal cell layer. These characteristic histological criteria were masked by extensive squamous metaplasia of the epithelial lining to such a degree that a squamous odontogenic tumour (SOT) was even considered as a differential diagnosis.
A SOT is a benign odontogenic neoplasm of epithelial origin with a predilection for the roots of teeth in the premolar/molar region [12]. Histologically, this tumour is characterized by islands of squamous odontogenic epithelium in a background fibrous connective tissue stroma. These epithelial islands may show cystic degeneration, however large clinically apparent cystic lesions are not described in literature.
A central mucoepidermoid carcinoma (MEC) shows similar histological features to a GOC and is therefore considered an important differential diagnosis. Low grade MEC may present as a cyst or multicystic lesion lined by epithelium comprising of mucous cells, epidermoid cells and intermediate cells. However, in this case the histological features did not fit the criteria for the diagnosis; CK19 immunohistochemistry was used to confirm odontogenic origin. Although many have speculated that a GOC is a precursor lesion to central MEC, these theories have been discredited by Bishop et al. [13] who showed that GOC lacked the MAML2 gene rearrangements seen in MEC.
GOCs are postulated to arise from the epithelial cell rests of Serres, however the exact mechanism of development is not clear [5]. The pathogenesis of COD is unfortunately not documented, however the designation of the term ‘cemento’ and the fact that these lesions are located in radicular regions may suggest odontogenic origin from the periodontal ligament [4]. Other studies have documented fibro-osseous-like lesions with odontogenic tumours including adenomatoid odontogenic tumour (AOT) [14, 15] and odontomas [16–18].
In these studies, the AOT was associated with COD-like [15] and ossifying fibroma-like lesions [14]. Li et al. [14] postulated the fibro-osseous-like proliferations to be metaplastic ossification in the wall of the AOT, instead of collision of two separate entities. Whilst Prodromidis et al. [17] postulated that the presence of the benign fibro-osseous-like lesion may be due to the presence of COD-like features in an odontoma, coincidental association of two distinct lesions, or a common developmental origin for both lesions.
The difference between the current case and cases in the literature [14, 15, 17] is that our case showed two clear distinct radiological and pathological entities, whilst those reported in the literature showed a fibro-osseous proliferation in the wall of an odontogenic tumour or cyst. The case report by Zameer et al. [19] was excluded in this review as it was diagnosed as focal COD of the mandible and separate a radicular cyst in the maxilla. The only case in literature similar to the current case is that of Sanjai et al. [10] whereby florid COD was seen in conjunction with a dentigerous cyst. An interesting observation was that majority of these lesions occurred in females, as summarised by Table 1.
Table 1.
Summary of cases of benign fibro-osseous lesion and odontogenic lesions in the literature
| Author (s) | Year published | Number of cases | Age (years)/ gender | Location of both lesions | Benign fibro-osseous lesion | Odontogenic lesion (s) |
|---|---|---|---|---|---|---|
| Iida et al. [18] | 2006 | 1 | 37 F | Max L | OD-like | Odontoma |
| Sanjai et al. [10] | 2010 | 1 | 20 F | Man L | FCOD | Dentigerous cyst |
| Prodromidis et al. [17] | 2011 | 1 | 36 F | Man L | COD-like | Odontoma |
| Li et al. [14] | 2013 | 1 | 22 F | Max R | OF-like | AOT |
| Naidu et al. [15] | 2016 | 2 |
34 F 23 F |
Max R Max R |
OF-like | AOT |
| Reddy et al. [16] | 2019 | 1 | 12 M | Man L | BFOL-like | Odontoma |
| Current case | 1 | 43 F | Max L | FCOD | GOC |
Man mandible, Max maxilla, L left, R right, BFOL benign fibro-osseous lesion, OF ossifying fibroma, OD osseous dysplasia, COD cemento-osseous dysplasia, FCOD florid cemento-osseous dysplasia, AOT adenomatoid odontogenic tumour, GOC Glandular odontogenic cyst
To the authors’ knowledge, this is the second case documenting florid COD with an odontogenic cyst, and the first concurrent GOC with extensive squamous metaplasia. We postulate that the concurrent presentation of these two lesions may be from the same pluripotent cells or from synchronous development from activation of odontogenic sources. This requires further elucidation with molecular studies.
Acknowledgements
We wish to acknowledge Dr. GJ Richter, MChD (Maxillofacial and Oral Surgery), for the radiograph and biopsy specimens.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by the University of Pretoria, Faculty of Health Sciences Research Ethics Committee (Reference No.: 712/2019). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institution and/or the National Research Committee and the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Eversole R, Su L, ElMofty S. Benign fibro-osseous lesions of the craniofacial complex a review. Head Neck Pathol. 2008;2(3):177–202. doi: 10.1007/s12105-008-0057-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.El-Mofty SK. Fibro-osseous lesions of the craniofacial skeleton: an update. Head Neck Pathol. 2014;8(4):432–444. doi: 10.1007/s12105-014-0590-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCarthy EF. Fibro-osseous lesions of the maxillofacial bones. Head Neck Pathol. 2013;7(1):5–10. doi: 10.1007/s12105-013-0430-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Speight PM, Takata T. New tumour entities in the 4th edition of the World Health Organization Classification of Head and Neck tumours: odontogenic and maxillofacial bone tumours. Virchows Arch. 2018;472(3):331–339. doi: 10.1007/s00428-017-2182-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin L, Speight PM. Odontogenic cysts. Diagn Histopathol. 2015;21(9):359–369. doi: 10.1016/j.mpdhp.2015.07.005. [DOI] [Google Scholar]
- 6.Mahomed F, Altini M, Meer S, Coleman H. Cemento-osseous dysplasia with associated simple bone cysts. J Oral Maxillofac Surg. 2005;63(10):1549–1554. doi: 10.1016/j.joms.2005.05.322. [DOI] [PubMed] [Google Scholar]
- 7.Horner K, Forman G. Atypical simple bone cysts of the jaws. II: a possible association with benign fibro-osseous (cemental) lesions of the jaws. Clin Radiol. 1988;39(1):59–63. doi: 10.1016/S0009-9260(88)80344-1. [DOI] [PubMed] [Google Scholar]
- 8.Wojno KJ, McCarthy EF. Fibro-osseous lesions of the face and skull with aneurysmal bone cyst formation. Skeletal Radiol. 1994;23(1):15–18. doi: 10.1007/BF00203695. [DOI] [PubMed] [Google Scholar]
- 9.Speight PM, Carlos R. Maxillofacial fibro-osseous lesions. Curr Diagn Pathol. 2006;12(1):1–10. doi: 10.1016/j.cdip.2005.10.002. [DOI] [Google Scholar]
- 10.Sanjai K, Kumarswamy J, Kumar VK, Patil A. Florid cemento osseous dysplasia in association with dentigerous cyst. J Oral Maxillofac Pathol. 2010;14(2):63–68. doi: 10.4103/0973-029X.72503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fowler CB, Brannon RB, Kessler HP, Castle JT, Kahn MA. Glandular odontogenic cyst: analysis of 46 cases with special emphasis on microscopic criteria for diagnosis. Head Neck Pathol. 2011;5(4):364–375. doi: 10.1007/s12105-011-0298-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elmuradi S, Mair Y, Suresh L, DeSantis J, Neiders M, Aguirre A. Multicentric squamous odontogenic tumor: a case report and review of the literature. Head Neck Pathol. 2017;11(2):168–174. doi: 10.1007/s12105-016-0753-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bishop JA, Yonescu R, Batista D, Warnock GR, Westra WH. Glandular odontogenic cysts (GOCs) lack MAML2 rearrangements: a finding to discredit the putative nature of GOC as a precursor to central mucoepidermoid carcinoma. Head Neck Pathol. 2014;8(3):287–290. doi: 10.1007/s12105-014-0534-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li B-B, Xie X-Y, Jia S-N. Adenomatoid odontogenic tumor with fibro-osseous reaction in the surrounding tissue. J Craniofac Surg. 2013;24(1):e100-e1. doi: 10.1097/SCS.0b013e3182799005. [DOI] [PubMed] [Google Scholar]
- 15.Naidu A, Slater LJ, Hamao-Sakamoto A, Waters P, Kessler HP, Wright JM. Adenomatoid odontogenic tumor with peripheral cemento-osseous reactive proliferation: report of 2 cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122(3):e86–e92. doi: 10.1016/j.oooo.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Reddy R, Jagtap R, Kashtwari D, Hambrook CC, Freburg-Hoffmeister DL, Islam MN, et al. Benign fibro-osseous lesion and odontoma of the mandible: a report of a rare, hybrid lesion and review of literature. J Oral Maxillofac Surg Med Pathol. 2019;31(6):415–419. doi: 10.1016/j.ajoms.2019.05.002. [DOI] [Google Scholar]
- 17.Prodromidis GI, Tosios KI, Koutlas IG. Cemento-osseous dysplasia-like lesion and complex odontoma associated with an impacted third molar. Head Neck Pathol. 2011;5(4):401–404. doi: 10.1007/s12105-011-0261-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iida S, Kishino M, Sakai T, Ishida H, Okura M, Toyosawa S, et al. Multiple osseous dysplasia arising from impacted teeth: report of a case associated with odontogenic lesions. J Oral Pathol Med. 2006;35(7):402–406. doi: 10.1111/j.1600-0714.2006.00414.x. [DOI] [PubMed] [Google Scholar]
- 19.Zameer P, Sulabha A, Choudhari S. Concomitant occurrence of infected cemento-osseous dysplasia and radicular cyst in young Indian female: an unusual case report. J Oral Maxillofac Radiol. 2013;1(2):75–79. doi: 10.4103/2321-3841.120124. [DOI] [Google Scholar]