Abstract
Several exercise methods, such as the Shaker exercise, tongue press exercise, chin tuck against resistance (CTAR) exercise, and submandibular push exercise, have been introduced to strengthen the muscles involved in swallowing. In this study, we compared the effectiveness of the CTAR, submandibular push, and Shaker exercises for the induction of selective supra- and infrahyoid muscle contractions using surface electromyography (EMG). This study is a prospective non-randomized controlled study. Twenty-five healthy subjects and 20 patients experiencing swallowing difficulty were enrolled. During the three different types of exercises, the root mean square (RMS) values of the sternocleidomastoid (SCM), suprahyoid (anterior belly of the digastric and mylohyoid muscles), and infrahyoid (sternothyroid and thyrohyoid muscles) muscles were analyzed using surface EMG. Differences in the activity of swallowing muscles among the three different exercises were analyzed using one-way repeated measured analysis of variance. In terms of both the maximum and mean RMS values of the suprahyoid muscle, the submandibular push exercise showed a larger RMS value than the CTAR and Shaker exercises in healthy subjects (p < 0.05). In terms of both the maximum and mean RMS values of the suprahyoid muscle, the Shaker exercise and submandibular push exercise showed a larger RMS value than the CTAR exercise in patients with swallowing difficulty (p < 0.05). The submandibular push exercise may be effective as a swallowing muscle exercise owing to its superiority in inducing selective contractions of the supra- and infrahyoid muscles. The CTAR and Shaker exercises are also effective in this regard.
Subject terms: Neurological disorders, Geriatrics, Quality of life
Introduction
The swallowing process is a compound sensori-motor behavior that includes the coordinated relaxation and contraction of the muscle tissues around the tongue, mouth, pharynx, larynx, and upper esophagus1–3. Of the muscles contributing to the swallowing process, the supra- and infrahyoid muscles have been extensively reported2,4–7. The functions of the suprahyoid muscle in terms of the anterosuperior motions of the hyoid bone and the functions of the omohyoid, sternothyroid, and sternohyoid muscles and a part of the infrahyoid muscles in depressing the hyolaryngeal complex are understood8,9. The role of the thyrohyoid muscle, one of the four infrahyoid muscles, is to move the larynx antero-superiorly during the swallowing process. Moreover, the infra- and suprahyoid muscles support the opening of the upper esophageal sphincter (UES) by moving the hyoid bone anteriorly8–12.
Dysphagia or difficulty swallowing may result from various problems such as neurological impairment and physiological and anatomical derangements in any region from the mouth to the esophagus (e.g., in the muscles involved in swallowing)13–17. Various methods have been employed to treat dysphagia. Conventional treatment methods such as oropharyngeal (including the muscles involved in swallowing) exercises, compensated maneuvers, and electrical stimulation of the oropharyngeal area are widely applied in swallowing therapy11,18–21.
The muscles involved in swallowing can be strengthened using several exercise methods, such as the Shaker and tongue press exercises, chin tuck against resistance (CTAR) exercise, and submandibular push exercise20,21. In the Shaker exercise, sustained head lifts are performed with the subject in the supine position. The Shaker exercise was designed to strengthen the suprahyoid muscle, thereby assisting the opening of the UES. It can be effective in addressing swallowing difficulty caused by incomplete UES opening20. Additionally, the Shaker exercise significantly increases the antero-posterior diameter of the UES in elderly patients with and without swallowing difficulty and significantly reduces post-swallow aspiration20. However, in a previous study, it was concluded that the Shaker exercise was difficult to perform, especially for elderly patients with chronic diseases22. Hence, the CTAR exercise was recommended in previous studies21,23. In the CTAR exercise, by changing the resistances of a plastic bar or rubber ball between the chest and the chin, the exercise load can be modulated21,23. However, the superiority of the CTAR exercise over the Shaker exercise has been disputed. In a previous study, the CTAR exercise showed greater maximal values on surface electromyography (EMG) of the suprahyoid muscle than the Shaker exercise23. However, in patients with swallowing difficulty, Gao and Zhang24 reported similar effects in improving swallowing dysfunction between the CTAR and Shaker exercises.
However, both exercises involve neck flexion movement patterns, which induce unnecessary contractions of the sternocleidomastoid (SCM) muscle and may adversely affect contractions of the selective supra- and infrahyoid muscles25. To overcome the limitations of the CTAR and Shaker exercises, the submandibular push exercise was introduced in a previous study18. However, that study used visual feedback from pressure sensors. Therefore, the application of the submandibular push exercises in patients who constantly need dysphagia treatment may have some limitations. Based on these observations, we examined the effectiveness of the submandibular push exercise for the contraction of muscles involved in swallowing without a pressure sensor, in order to determine its usefulness as an at-home exercise. Based on previous research results, we postulated that compared to the CTAR and Shaker exercises, the submandibular push exercise would induce selective contraction of the supra- and infrahyoid muscles without unnecessary SCM contraction. Therefore, we assessed the effectiveness of the CTAR, submandibular push, and Shaker exercises for the induction of selective contractions of the supra- and infrahyoid muscles using a simple device, such as a plastic bar. By comparing three different exercises, we attempted to determine the effects of each of the three different exercises on each swallowing muscle in healthy subjects and patients with swallowing difficulty.
Methods
Ethics statements
This prospective case–control study was approved by the institutional review board of Daegu Fatima Hospital. All methods were performed in accordance with relevant guidelines and regulations (Declaration of Helsinki), and written informed consent was obtained from all participants. Informed consent for publication of identifying images was obtained from each relevant patient.
Participants
In this study, 45 participants (25 healthy participants and 20 patients with swallowing difficulty) were enrolled (Table 1). The healthy subjects were participants without swallowing difficulty or any history of diseases that could cause swallowing difficulty (such as traumatic brain injury, spinal cord injury, and stroke). Patients with swallowing difficulty had various causative reasons and exhibited at least one symptom of swallowing difficulty, such as coughing when eating, a wet or weak voice, food sticking in the throat, globus sensations, difficulty in chewing, and drooling26,27. We excluded patients with problems that prevented them from holding an exercise tool during exercise, those with severe cognitive dysfunction (Mini-Mental Status Examination score ≤ 9), those with serious psychiatric disorders, and those aged < 20 years.
Table 1.
Characteristics of participants.
| Healthy participants | Patients with swallowing difficulty | |
|---|---|---|
| Number | 25 | 20 |
| Sex ratio (M:F) | 21:4 | 12:8 |
| Age (years) | 29.9 ± 4.1 | 70.6 ± 9.0 |
| Duration (months) | 6.2 ± 4.5 | |
| Cause of dysphagia | Hemispheric stroke (n = 14) | |
| (SICH = 1, infarction = 13) | ||
| brainstem stroke (n = 5) | ||
| (SICH = 1, infarction = 4) | ||
| TSAH (n = 1) | ||
| Symptoms of dysphagia | Protective cough with eating (n = 20) | |
| Food sticking in throat (n = 10) | ||
| Drooling (n = 3) | ||
| Having a wet or weak voice (n = 6) | ||
| Globus sensation (n = 10) | ||
| Difficulty chewing (n = 7) |
Mean ± standard deviation, M:F; male:female, TSAH; traumatic subarachnoid hemorrhage, SICH; spontaneous intra-cerebral hemorrhage.
Design
All participants were asked to consecutively perform three different types of exercises (submandibular push, CTAR, and Shaker exercises). Participants were permitted to rest between each exercise session, to prevent muscle fatigue. Before the start of each exercise, the resting muscle (supra- and infrahyoid muscles) activation levels were recorded using surface EMG.
Procedures
All participants were assessed in a quiet room. Each participant was asked to perform one trial of each exercise (10 repetitions in each trial) in the following order: (1) the Shaker exercise, (2) the CTAR exercise, and (3) the submandibular push exercise, with a 10-min rest between each exercise session to prevent fatigue of the swallowing muscles. For each exercise, the participants were instructed to maintain the end-position for 10 s21,23. The participants were instructed to keep their mouths closed during all the exercises.
Exercise maneuvers
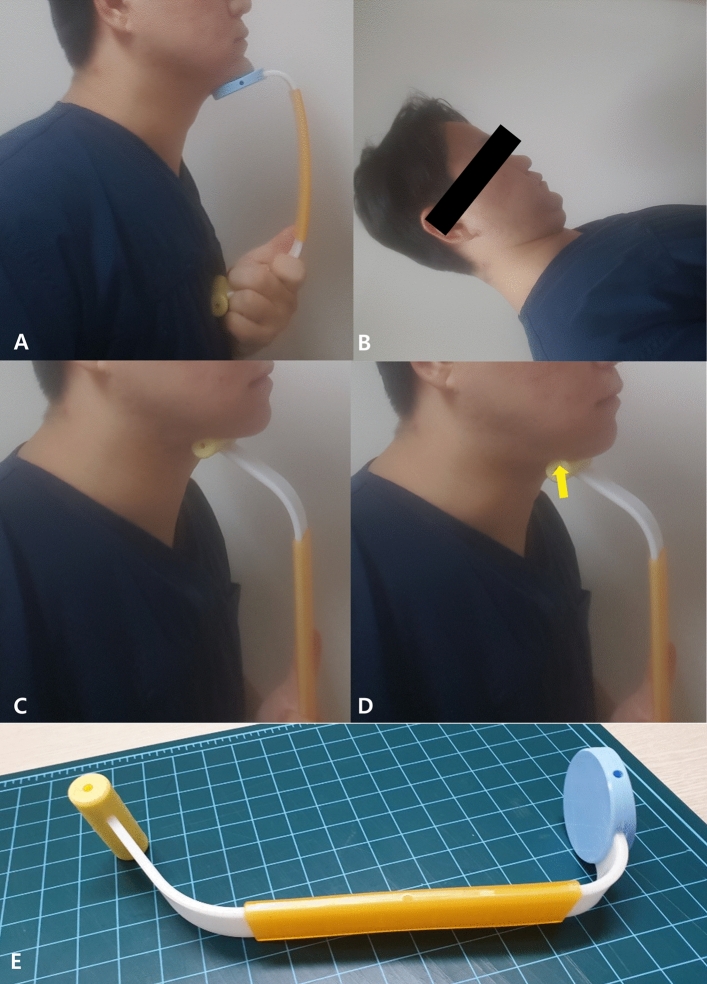
First, when performing the Shaker exercise, the healthy subjects and patients were instructed to perform the following exercise protocol: lie on the bed in the supine position, lift the head up and hold it for 10 s (Fig. 1A)18,21,23,24. Second, when performing the CTAR exercise, participants were instructed to sit on a chair and press the chin as hard as possible against a CTAR device (Renodevice, Daegu, South Korea) placed under the chin (Fig. 1B) 21,23. Lastly, when performing the submandibular push exercise, the participants were instructed to sit on a chair and increase the pressure at the submandibular area against a plastic device [Renodevice, Daegu, South Korea, (Fig. 1C,D)] without neck flexion18. The participants were instructed to maintain the end posture during the three exercises, and the surface EMG data were recorded.
Figure 1.
(A) Chin tuck against resistance (CTAR) exercise. (B) Shaker exercise. (C, D) Submandibular push exercise. Arrow, bloating change in the submandibular area during the submandibular push exercise (E) A plastic device used in this study.
Electromyography
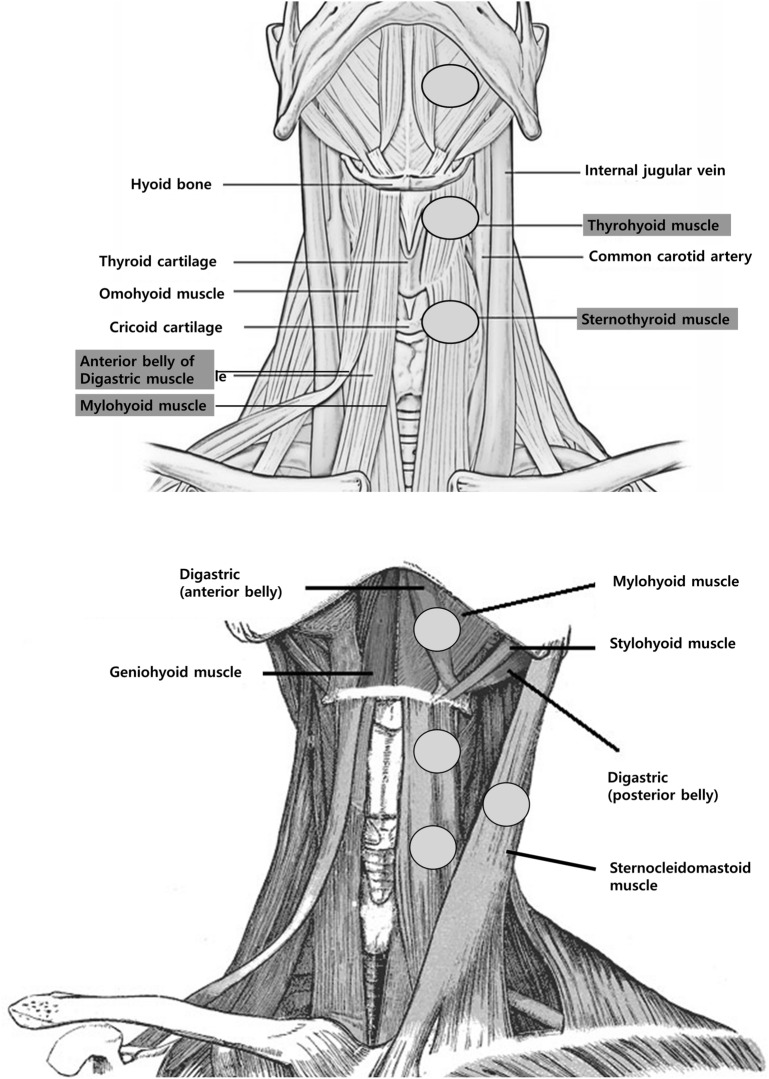
Using an EMG device and software (Medelec Synergy; CareFusion Corporation, San Diego, CA), multi-channel surface EMG was performed during each exercise2,28. The surface EMG electrode was attached to the SCM, suprahyoid muscles (mylohyoid and anterior belly of the digastric muscles), and infrahyoid muscles (sternothyroid and thyrohyoid muscles) (Fig. 2)2. To confirm the precise location of the surface EMG electrodes on the targeted muscles, ultrasonographic examinations were performed before the attachment of surface EMG electrodes. The location of the bellies of the suprahyoid, infrahyoid, and SCM muscles was examined using a 3–16- MHz linear ultrasound probe (Samsung Medison, Hongchun-gun, South Korea)2. The reference surface electrode was positioned on the anterior surface of the clavicle or mandible bone, the active surface electrode on the belly of the examined muscle, and the ground electrodes on the mandible base. To accommodate the surface EMG, all participants rested for 10 min before each exercise. During exercises involving a stick, an attempt was made to prevent contact between the stick and surface EMG electrode to reduce artifacts.
Figure 2.
Locations of the surface electromyography electrodes during the chin tuck against resistance, Shaker, and submandibular push exercises.
Data were collected at a sampling rate of 50 kHz using Medelec Synergy with the following settings: high-frequency filter, 1000 Hz; low-frequency filter, 10 Hz; 1 s/div and 100 μV/div; sweep speed and gain; and common mode rejection ratio, > 110 dB2,28,29. The EMG activity was measured using a custom-designed disposable pre-gelled 20-mm Ag/AgCl disc electrode (CareFusion, Höchberg, Germany)18.
Signal processing
The root mean square (RMS) value of EMG activity was measured 10 times with 1 s as a section18. For 10 s, the patient maintained the end-position of each exercise, and the RMS value (during 1 s as a section) was measured 10 times consecutively. Using EMG software (Medelec Synergy; CareFusion Corporation), the mean RMS of the EMG activity of each swallowing muscle during 1 s was calculated. In each exercise maneuver, a mean RMS value during 10 s was calculated18.
The resting RMS value was subtracted from the RMS value measured for each muscle to minimize bias caused by muscle contraction due to posture maintenance before exercise. Although this method is not a commonly used normalization of the EMG signal method and as it is difficult to induce maximum contraction of the swallowing muscles in patients, we used the resting RMS value of each target muscle according to the exercise posture before starting the exercise. We attempted to minimize the bias by subtracting it from the maximum RMS value of each target muscle.
The highest RMS value was defined as the maximum RMS value among the 10 RMS values (1-s section) measured for each exercise maneuver18. In addition, the average RMS value was calculated as the average of the 10 RMS values (1-s section)18.
Statistical analyses
PRISM version 8.00 (GraphPad Software, Inc., San Diego, CA, USA) and IBM SPSS version 21 (SPSS, Inc., Chicago, IL, USA) were used for all statistical analyses. Differences in the activity of the swallowing muscles among the three different exercises were analyzed using one-way repeated measured analysis of variance (ANOVA). Using repeated-measures ANOVA with the Tukey post-hoc test, the maximum and average RMS values of the 35 participants were then compared. A p value < 0.05 was considered statistically significant.
Sample size calculation
The maximum RMS value of the suprahyoid muscle (μV) was determined using data from the 10 healthy subjects. This value was used to perform a two-tailed sample size calculation of the expected mean differences, with a standard deviation (SD) of 0.2, significance level of 0.05, and power of 80%. Therefore, the required sample size for this study was at least 12 participants in each group.
Results
Participant characteristics
Twenty-five healthy participants (male: 21, female: 4) aged 21–39 years (average, 29.9; SD, 4.1) and 20 patients with swallowing difficulty (male: 12, female: 8) aged 52–84 years (mean, 70.6; SD, 9.0) were enrolled (Table 1). The etiologies of swallowing difficulty are shown in Table 1.
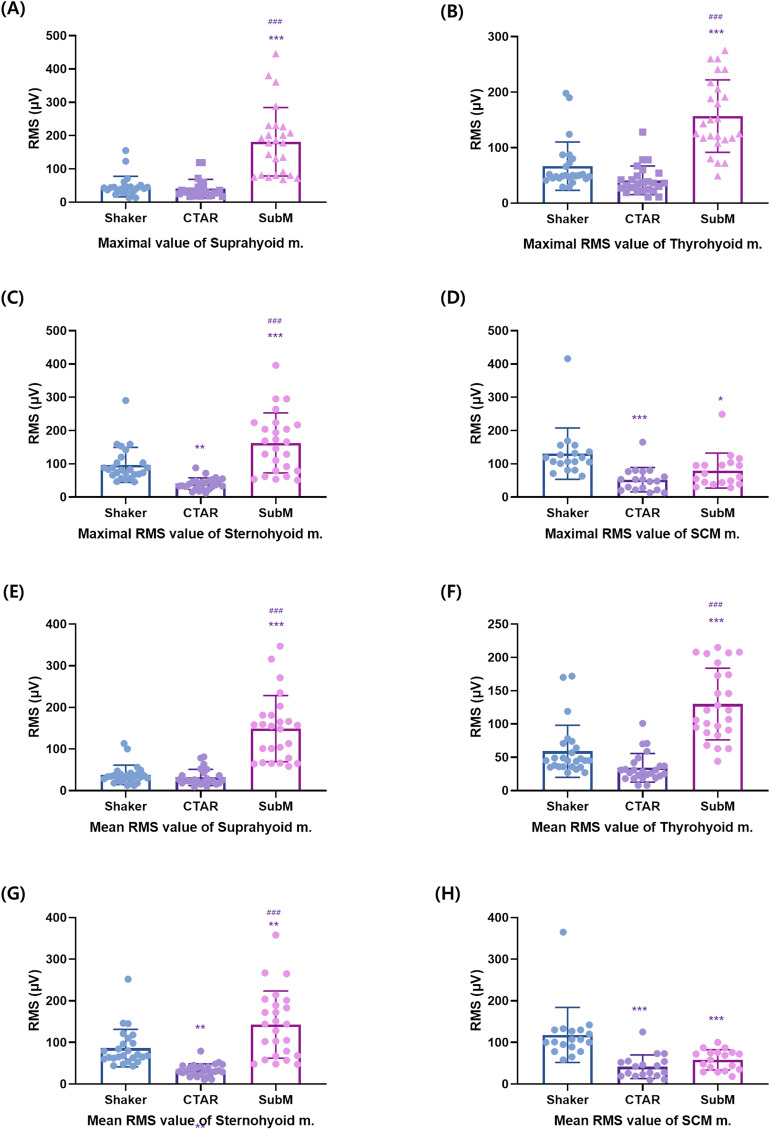
Comparison of the three different types of exercises in the healthy subjects
There were significant differences in the maximum RMS values of the suprahyoid (p < 0.001), thyrohyoid (p = 0.003), sternohyoid (p < 0.001), and SCM muscles (p < 0.001) among the three different exercises, as well as in the mean RMS values of the suprahyoid (p < 0.001), thyrohyoid (p < 0.001), sternohyoid (p < 0.001), and SCM muscles (p < 0.001). In the post-hoc analysis, the submandibular push exercise exhibited a larger RMS value than the Shaker and CTAR exercises in terms of both the maximum and mean RMS values of the suprahyoid muscle (p < 0.05, Tables 2, 3). There was no significant difference between the CTAR and Shaker exercises (p ≥ 0.05). In terms of both the maximum and mean RMS values of the thyrohyoid muscle, the submandibular exercise exhibited a larger RMS value than the Shaker and CTAR exercises (p < 0.05). However, there was no significant difference (p ≥ 0.05) between the Shaker and CTAR exercises. In terms of both the maximum and mean RMS values of the sternohyoid muscle, the submandibular push exercise showed a larger RMS value than the Shaker and CTAR exercises (p < 0.05). Moreover, between the CTAR and Shaker exercises, there were significant differences (p < 0.05). In terms of both the maximum and mean RMS values of the SCM muscle, the Shaker exercise showed a larger RMS value than the CTAR and submandibular push exercises (p < 0.001). However, there was no significant difference between the CTAR and submandibular push exercises (p < 0.05) (Fig. 3A–H).
Table 2.
The maximal RMS value of the suprahyoid, thyrohyoid, sternohyoid, and SCM muscles in healthy participants and patients with dysphagia.
| Max Suprahyoid RMS | Max Thyrohyoid RMS | Max Sternothyroid RMS | Max SCM RMS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Shaker (μV) | CTAR (μV) | SubM (μV) | Shaker (μV) | CTAR (μV) | SubM (μV) | Shaker (μV) | CTAR (μV) | SubM (μV) | Shaker (μV) | CTAR (μV) | SubM (μV) | ||
| HP | Mean | 47.04 | 40.64 | 181.52*# | 66.76 | 41.12 | 156.96*# | 96.80# | 40.20* | 162.88*# | 130.72# | 52.33* | 79.78* |
| SD | 30.79 | 27.73 | 102.83 | 43.58 | 25.76 | 65.28 | 52.58 | 17.45 | 90.24 | 76.99 | 36.49 | 52.37 | |
| DP | Mean | 78.95# | 35.61* | 76.24# | 100.50# | 43.39* | 69.74# | 95.85# | 37.07* | 76.87# | 98.66# | 53.64* | 54.80* |
| SD | 43.35 | 26.07 | 36.15 | 61.19 | 32.51 | 54.49 | 25.52 | 26.59 | 42.98 | 34.48 | 28.17 | 26.61 | |
RMS; root mean square, SD; standard deviation, CTAR; chin tuck against resistance, SubM; submandibular push exercise, SCM; sternocleidomastoid, Max; maximum, HP; healthy participants, DP; dysphagic patients.
versus Shaker; *p < 0.05, versus CTAR; #p < 0.05.
Table 3.
The mean RMS value of the suprahyoid, thyrohyoid, sternohyoid, and SCM muscles in healthy participants and patients with dysphagia.
| Mean Suprahyoid RMS | Mean Thyrohyoid RMS | Mean Sternothyroid RMS | Mean SCM RMS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Shaker (μV) | CTAR (μV) | SubM (μV) | Shaker (μV) | CTAR (μV) | SubM (μV) | Shaker (μV) | CTAR (μV) | SubM (μV) | Shaker (μV) | CTAR (μV) | SubM (μV) | ||
| HP | Mean | 37.64 | 31.57 | 148.91*# | 59.12 | 34.19 | 130.07*# | 86.33# | 33.42* | 142.92*# | 118.06# | 41.39* | 58.11* |
| SD | 23.43 | 19.43 | 79.41 | 39.02 | 21.43 | 53.86 | 45.22 | 15.06 | 80.76 | 66.26 | 28.53 | 24.28 | |
| DP | Mean | 62.47# | 30.05* | 67.28# | 83.31# | 34.49* | 60.30 | 86.32# | 33.06* | 67.62# | 88.23# | 42.47* | 47.24* |
| SD | 28.27 | 19.58 | 35.44 | 34.86 | 21.57 | 46.58 | 22.67 | 23.67 | 45.37 | 29.64 | 19.6 | 20.86 | |
RMS; root mean square, SD; standard deviation, CTAR; chin tuck against resistance, SubM; submandibular push exercise, SCM; sternocleidomastoid, Max; maximum, HP; healthy participants, DP; dysphagic patients.
versus Shaker; *p < 0.05, versus CTAR; #p < 0.05.
Figure 3.
The maximum (A–D) and mean (E–H) RMS values of the suprahyoid, thyrohyoid, sternohyoid, and SCM muscles in healthy participants. The graphs were drawn using GraphPad Prism 8.0. RMS, root mean square; SCM, sternocleidomastoid. Compared with the Shaker exercise: *p < 0.05, **p < 0.01, ***p < 0.001; compared with the chin tuck against resistance exercise: #p < 0.05, ##p < 0.01, ###p < 0.001.
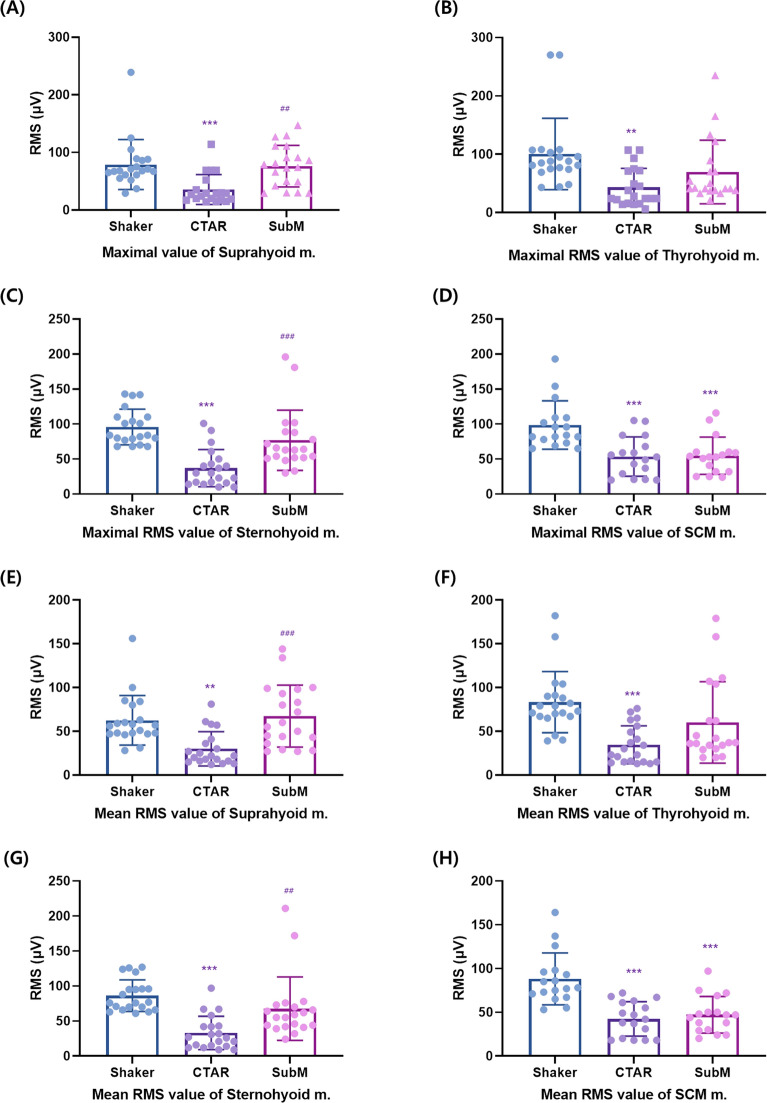
Comparison of the three different types of exercises in patients with swallowing difficulty
There were significant differences in the maximum RMS values of the suprahyoid (p < 0.001), thyrohyoid (p < 0.001), sternohyoid (p < 0.001), and SCM muscles (p < 0.001) among the three different exercises, as well as the mean RMS values of the suprahyoid (p < 0.001), thyrohyoid (p < 0.001), sternohyoid (p < 0.001), and SCM muscles (p < 0.001). In the post-hoc analysis, the Shaker and submandibular push exercises showed a larger RMS value than the CTAR exercise in terms of both the maximum and mean RMS values of the suprahyoid muscle (p < 0.05, Tables 2, 3). However, there was no significant difference between the submandibular push exercise and Shaker exercises (p ≥ 0.05). In terms of both the maximum and mean RMS values of the thyrohyoid muscle, the Shaker exercise showed a larger RMS value than the CTAR exercise (p < 0.05). However, there was no significant difference between the submandibular push and Shaker exercises (p ≥ 0.05) and between the submandibular push and CTAR exercises (p ≥ 0.05).
In terms of both the maximum and mean RMS values of the sternohyoid muscle, the Shaker and submandibular push exercises showed a larger RMS value than the CTAR exercise (p < 0.05). However, there was no significant difference between the Shaker and submandibular push exercises, (p ≥ 0.05). In terms of both the maximum and mean RMS values of the SCM muscle, the Shaker exercise showed a larger RMS value than the CTAR and submandibular push exercises (p < 0.001). However, there was no significant difference (p < 0.05, Fig. 4A–H) between the CTAR and submandibular push exercises.
Figure 4.
The maximum (A–D) and mean (E–H) RMS values of the suprahyoid, thyrohyoid, sternohyoid, and SCM muscles in patients with swallowing difficulty. The graphs were drawn using GraphPad Prism 8.0. RMS, root mean square; SCM, sternocleidomastoid. Compared with the Shaker exercise: *p < 0.05, **p < 0.01, ***p < 0.001; compared with the chin tuck against resistance exercise: #p < 0.05, ##p < 0.01, ###p < 0.001.
Discussion
To the best of our knowledge, this is the first study to compare the effects of these three exercises (Shaker, CTAR, and submandibular push exercises) on the swallowing-related muscles using a plastic bar. The importance of this study is the knowledge of how each of the three different exercises affects each swallowing muscle in healthy subjects and patients with swallowing difficulty.
In the present study, both the maximum and mean RMS values of all the examined muscles showed significant differences according to the three different exercises in both healthy subjects and patients with swallowing difficulty. However, the muscle contraction patterns during the three different exercises showed slightly different results between healthy subjects and patients with swallowing difficulty. In the healthy young age group (20–40-year-old participants), the submandibular push exercise using a plastic bar induced stronger supra- and infrahyoid muscle contractions than the CTAR and Shaker exercises. The CTAR and Shaker exercises induced similar SCM, suprahyoid, and infrahyoid muscle contractions in healthy subjects, possibly because both these exercises included neck flexion movement patterns. The overall muscle contraction was higher in the Shaker exercise group than in the CTAR group. This is potentially because the Shaker exercise is performed with neck flexion against gravity.
In patients with swallowing difficulty, the degree of supra- and infrahyoid muscle contraction with the submandibular push exercise was higher than that with the CTAR exercise but similar to that with the Shaker exercise. However, in patients with swallowing difficulty, the submandibular push exercise exhibited less SCM muscle contraction than supra- and infrahyoid muscle contraction, unlike the other two exercise methods. The different contraction patterns of the swallowing muscles between healthy subject and patients with swallowing difficulty may be attributed to the following reasons: First, the difficulty in performing the submandibular push exercise. In a previous study, although the submandibular push exercise was performed with the help of visual feedback from a pressure sensor, patients experienced difficulty in understanding the submandibular push exercise18. Moreover, in our study, unlike healthy subjects who were in their 20 s and 30 s, the mean age of patients with dysphagia was 70 years; this discrepancy could be the cause of the difference in the effects of the submandibular push exercise between the two groups. Second, most patients with dysphagia often have weakness of the swallowing muscles such as the supra- and infrahyoid muscles, which decrease the degree of supra- and infrahyoid muscle contractions during the submandibular push exercise that requires a relatively high degree of swallowing muscle contraction6. However, in patients with swallowing difficulty, the submandibular push exercise along with the Shaker exercise induced the most supra- and infrahyoid muscle contractions.
Although the Shaker exercise can induce powerful contractions of muscles involved in swallowing, it may be inefficient from the perspective of selective contraction of muscles involved in swallowing (supra- and infrahyoid muscles)30. However, in patients with swallowing difficulty, the submandibular push exercise has been shown to induce powerful supra- and infrahyoid contractions similar to those induced by the Shaker exercise. In addition, in healthy subjects, the submandibular push exercise has been shown to induce more powerful supra- and infrahyoid muscle contractions than the Shaker exercise. Moreover, the submandibular push exercise can induce selective supra- and infrahyoid muscle contractions, considering the relatively lower degree of SCM muscle contraction. In a previous study, in terms of contraction of the SCM muscles in the CTAR and Shaker exercises, the CTAR exercise resulted in less activation of the SCM muscles than the Shaker exercise22. Although there may be a different degree of neck flexion movement, both the CTAR and Shaker exercises, unlike the submandibular push exercise, have a neck flexion component during exercise. These results demonstrate that the effects of the submandibular push exercise on both the supra- and infrahyoid muscle may be greater or equivalent to those of the CTAR or Shaker exercise without the induction of unnecessary SCM muscle contraction.
However, our results were inconsistent with those of some previous studies that reported the superiority of the CTAR exercise over other exercises such as the Shaker exercise with regard to the degree of suprahyoid muscle contraction22,23. This inconsistency may be due to the difference in devices used in the CTAR exercise. In previous investigations, soft balls were used in the CTAR exercise, whereas in our study, a plastic bar was used22,23. We thought that if devices with different elasticity were used in the CTAR and submandibular push exercises, this could create a bias in comparing the effects of the CTAR and submandibular push exercises. Therefore, to reduce bias due to differences in elasticity of the device, a plastic bar that can be used in both these exercises was applied to compare the effects of these two exercises.
Limitations
There were several limitations in our study. First, we analyzed the degrees of supra- and infrahyoid muscle contractions in one session of each exercise. In addition, at least 2–3 months of training is necessary to cause functional changes in neuro-muscular tissue31. Functional changes such as the strengthening or thickening of muscle tissues in the supra- and infrahyoid muscles are difficult to prove, based on the results of this study. However, considering that the degree of muscle activation is proportional to the amount of exercise, the results of our study may reflect the possibility of actual strengthening of swallowing muscles. To confirm the improvement of dysphagia by the submandibular push exercise, a further study with > 2–3 months of exercise training is necessary31. Second, the order of execution of the three exercises was the same. To exclude bias caused by the order of exercise execution, future studies including a protocol with a random order of exercise execution would be necessary. Fourth, in this study, we used surface EMG; therefore, the effect of volume contraction cannot be completely excluded. In addition, artifacts due to the use of sticks may also affect the results of the three different exercises. Fifth, a standard EMG processing procedure was not used in this study. We calculated the RMS value of each muscle by subtracting the resting RMS value from the RMS value measured for each muscle. However, this study did not aim to compare the degree of contraction of several muscles according to each exercise. We only compared the RMS values to determine the activity induced by the three exercises in each muscle. For example, this study did not investigate the ratio of activation of the suprahyoid, infrahyoid, and SCM muscles with the three different exercises. We compared the RMS values of the Shaker, CTAR, and submandibular push exercises in one muscle of the same individuals. Therefore, although we did not use a standard EMG processing procedure, if we compare the degree of contraction in each participant using the same measurement method in one muscle, we believe that the results of this study. However, to investigate the exact RMS values of swallowing-related muscles, a further study with standard EMG processing would be required. Lastly, despite the use of surface EMG analysis, not all the muscles involved in swallowing were evaluated. Further studies investigating all the muscles involved in swallowing are warranted to investigate the exact mechanism and effects of the submandibular push exercise.
Conclusions
Although the Shaker and CTAR exercises can induce powerful contractions of muscles involved in swallowing, they may be inefficient from the perspective of selective contraction of the supra- and infrahyoid muscles because of unnecessary contraction of the SCM muscle. Considering its superiority in inducing selective supra- and infrahyoid muscle contractions, the submandibular push exercise may be an effective exercise method in both healthy subjects and patients with swallowing difficulty. To confirm the improvement of dysphagia by using the submandibular push exercise, further studies with > 3 months of exercise training are warranted.
Author contributions
M.C.C.: Editing the manuscript. S.P.: Acquisition of clinical data. J.Y.C.: Acquisition of clinical data. B.J.L.: Acquisition of clinical data. J.-M.H.: Editing the manuscript. K.K.: making a device. D.P.: Writing article, concept of study design, critical editing the manuscript.
Funding
This research was funded by Gyeongsan Medichallenger program. The present study was supported by a National Research Foundation of Korea grant funded by the Korean government (grant no. NRF-2019M3E5D1A02069399).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ertekin C, Aydogdu I. Neurophysiology of swallowing. Clin. Neurophysiol. 2003;114:2226–2244. doi: 10.1016/s1388-2457(03)00237-2. [DOI] [PubMed] [Google Scholar]
- 2.Park D, et al. Normal contractile algorithm of swallowing related muscles revealed by needle EMG and its comparison to videofluoroscopic swallowing study and high resolution manometry studies: A preliminary study. J. Electromyogr. Kinesiol. 2017;36:81–89. doi: 10.1016/j.jelekin.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 3.Park D, Shin CM, Ryu JS. Effect of different viscosities on pharyngeal pressure during swallowing: a study using high-resolution manometry. Arch. Phys. Med. Rehabil. 2017;98:487–494. doi: 10.1016/j.apmr.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 4.Kim SJ, Han TR. Effect of surface electrical stimulation of suprahyoid muscles on hyolaryngeal movement. Neuromodulation. 2009;12:134–140. doi: 10.1111/j.1525-1403.2009.00200.x. [DOI] [PubMed] [Google Scholar]
- 5.Humbert IA, et al. The effect of surface electrical stimulation on hyolaryngeal movement in normal individuals at rest and during swallowing. J. Appl. Physiol. 2006;101:1657–1663. doi: 10.1152/japplphysiol.00348.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hara K, Tohara H, Minakuchi S. Treatment and evaluation of dysphagia rehabilitation especially on suprahyoid muscles as jaw-opening muscles. Jpn. Dent. Sci. Rev. 2018;54:151–159. doi: 10.1016/j.jdsr.2018.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sun SF, et al. Combined neuromuscular electrical stimulation (NMES) with fiberoptic endoscopic evaluation of swallowing (FEES) and traditional swallowing rehabilitation in the treatment of stroke-related dysphagia. Dysphagia. 2013;28:557–566. doi: 10.1007/s00455-013-9466-9. [DOI] [PubMed] [Google Scholar]
- 8.Paik NJ, et al. Movement of the hyoid bone and the epiglottis during swallowing in patients with dysphagia from different etiologies. J. Electromyogr. Kinesiol. 2008;18:329–335. doi: 10.1016/j.jelekin.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen, J. & Duong, H. in StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK546659/ (2020).
- 10.Ferdjallah M, Wertsch JJ, Shaker R. Spectral analysis of surface electromyography (EMG) of upper esophageal sphincter-opening muscles during head lift exercise. J. Rehabil. Res. Dev. 2000;37:335–340. [PubMed] [Google Scholar]
- 11.Park D, Suh JH, Kim H, Ryu JS. The effect of four-channel neuromuscular electrical stimulation on swallowing kinematics and pressures: a pilot study. Am. J. Phys. Med. Rehabil. 2019;98:1051–1059. doi: 10.1097/PHM.0000000000001241. [DOI] [PubMed] [Google Scholar]
- 12.Park D, Oh Y, Ryu JS. Findings of abnormal videofluoroscopic swallowing study identified by high-resolution manometry parameters. Arch. Phys. Med. Rehabil. 2016;97:421–428. doi: 10.1016/j.apmr.2015.10.084. [DOI] [PubMed] [Google Scholar]
- 13.Yu KJ, Park D. Clinical characteristics of dysphagic stroke patients with salivary aspiration: A STROBE-compliant retrospective study. Medicine (Baltimore) 2019;98:e14977. doi: 10.1097/MD.0000000000014977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee DH, Kim JM, Lee Z, Park D. The effect of radionuclide solution volume on the detection rate of salivary aspiration in the radionuclide salivagram: a STROBE-compliant retrospective study. Medicine (Baltimore) 2018;97:e11729. doi: 10.1097/MD.0000000000011729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park D, et al. The correlation between clinical characteristics and radionuclide salivagram findings in patients with brain lesions: a preliminary study. Ann. Rehabil. Med. 2017;41:915–923. doi: 10.5535/arm.2017.41.6.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang MC, Park JS, Lee BJ, Park D. Effectiveness of pharmacologic treatment for dysphagia in Parkinson's disease: a narrative review. Neurol. Sci. 2020 doi: 10.1007/s10072-020-04865-w. [DOI] [PubMed] [Google Scholar]
- 17.Lee JT, Park E, Hwang JM, Jung TD, Park D. Machine learning analysis to automatically measure response time of pharyngeal swallowing reflex in videofluoroscopic swallowing study. Sci. Rep. 2020;10:14735. doi: 10.1038/s41598-020-71713-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park S, et al. Effect of the submandibular push exercise using visual feedback from pressure sensor: an electromyography study. Sci. Rep. 2020;10:11772. doi: 10.1038/s41598-020-68738-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Byeon H. Effect of the Masako maneuver and neuromuscular electrical stimulation on the improvement of swallowing function in patients with dysphagia caused by stroke. J. Phys. Ther. Sci. 2016;28:2069–2071. doi: 10.1589/jpts.28.2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Easterling C, Grande B, Kern M, Sears K, Shaker R. Attaining and maintaining isometric and isokinetic goals of the Shaker exercise. Dysphagia. 2005;20:133–138. doi: 10.1007/s00455-005-0004-2. [DOI] [PubMed] [Google Scholar]
- 21.Yoshida M, Groher ME, Crary MA, Mann GC, Akagawa Y. Comparison of surface electromyographic (sEMG) activity of submental muscles between the head lift and tongue press exercises as a therapeutic exercise for pharyngeal dysphagia. Gerodontology. 2007;24:111–116. doi: 10.1111/j.1741-2358.2007.00164.x. [DOI] [PubMed] [Google Scholar]
- 22.Sze WP, Yoon WL, Escoffier N, Rickard Liow SJ. Evaluating the training effects of two swallowing rehabilitation therapies using surface electromyography-chin tuck against resistance (CTAR) exercise and the shaker exercise. Dysphagia. 2016;31:195–205. doi: 10.1007/s00455-015-9678-2. [DOI] [PubMed] [Google Scholar]
- 23.Yoon WL, Khoo JK, Rickard Liow SJ. Chin tuck against resistance (CTAR): new method for enhancing suprahyoid muscle activity using a Shaker-type exercise. Dysphagia. 2014;29:243–248. doi: 10.1007/s00455-013-9502-9. [DOI] [PubMed] [Google Scholar]
- 24.Gao J, Zhang HJ. Effects of chin tuck against resistance exercise versus Shaker exercise on dysphagia and psychological state after cerebral infarction. Eur. J. Phys. Rehabil. Med. 2017;53:426–432. doi: 10.23736/S1973-9087.16.04346-X. [DOI] [PubMed] [Google Scholar]
- 25.Bordoni, B. & Varacallo, M. in StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK493232/ (2020).
- 26.Jones D, Prowse S. Globus pharyngeus: an update for general practice. Br. J. Gener. Pract. J. R. Coll. Gener. Pract. 2015;65:554–555. doi: 10.3399/bjgp15X687193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kang JH, et al. The effect of bedside exercise program on stroke patients with Dysphagia. Ann. Rehabil. Med. 2012;36:512–520. doi: 10.5535/arm.2012.36.4.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aksoy F, et al. Role of nasal muscles in nasal valve collapse. Otolaryngol. Head Neck Surg. 2010;142:365–369. doi: 10.1016/j.otohns.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 29.Lim SH, Hong BY, Oh JH, Lee JI. Effects of joint effusion on quadriceps muscles in patients with knee osteoarthritis. Phys. Ther. Sport. 2016;17:14–18. doi: 10.1016/j.ptsp.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 30.Kilinc HE, Arslan SS, Demir N, Karaduman A. The effects of different exercise trainings on suprahyoid muscle activation, tongue pressure force and dysphagia limit in healthy subjects. Dysphagia. 2020;35:717–724. doi: 10.1007/s00455-019-10079-w. [DOI] [PubMed] [Google Scholar]
- 31.Maeo S, Yoshitake Y, Takai Y, Fukunaga T, Kanehisa H. Neuromuscular adaptations following 12-week maximal voluntary co-contraction training. Eur. J. Appl. Physiol. 2014;114:663–673. doi: 10.1007/s00421-013-2801-x. [DOI] [PubMed] [Google Scholar]