Abstract
Introduction
The gold standard for reconstruction is the microvascular free flaps, whereas pedicled flaps are generally employed as a rescue procedure. Pectoralis major myocutaneous flap (PMMC) flap being a reliable flap is associated with high rate of complication. So, the purpose of this study was to check and assess the predictability of PMMC Flap and its clinical outcome in 168 Indian patients.
Materials and method
We conducted a retrospective study of PMMC flap which was harvested in 168 Indian oral cancer patients in 3 years time span. Patients were kept on follow up for 1–3 years. Rate of complication were documented for flap necrosis and wound dehiscence; and patient related data like neck bulk acceptance and range of motion were recorded. Gender comparison of complications were also documented.
Results
The most common complication was wound dehiscence in 11 (6.5%) patients. Partial flap necrosis was observed in 3 (1.8%) female patients. There was no case of total flap necrosis. Questionare method was used for patients to record neck bulk acceptance. Range of motion was evaluated during follow up period. Follow up period of all the patients was 1–3 years.
Conclusion
PMMC flap is still a well founded ‘workhorse’ flap for reconstruction in head and neck cancer patients and can be used successfully with acceptable morbidity.
Keywords: PMMC Flap, Post-operative complications, Neck bulk acceptance, Range of motion
1. Introduction
Head and neck cancer is found most commonly in Indian population. In accordance to the Indian Council of scientific studies (ICMR) Atlas, every 12 months kind of 2 lakhs new head and neck cancer patients are identified.1 Oral cavity forms an imperative element and plays critical function in a person’s life. Respiratory, speech, chewing and esthetics are some functions performed by oral cavity.2 Oral carcinoma is an evil affecting more and more large numbers of populace worldwide. The most effective way to save one from most cancers is its early detection and counseling.3
A benchmark for reconstruction in oral carcinoma patients is the microvascular free flaps, at the same time pedicled flaps are typically employed as a rescue approach.3,4 Due to harzards of microvascular reconstruction techniques like it demands higher anesthetic threat for seriously ill patients, and also lack of understanding and facilities, huge procedural cost and extended working time.3,5
Earlier than the advent of microvascular free flaps, Ariyan in 1980 described the pectoralis major myocutaneous flap (PMMC) as a ‘‘Workhorse Flap’‘.2,6 The PMMC flap is labeled as type 5 flap primarily based on the classification system given with the aid of Mathes and Nahai in 1981. This flap has a dominant pedicle and accessory segmental vascular pedicles.2 The flap is said to be the workhorse flap as there are many advantages like extremely good vascular supply, proximity to head and neck vicinity, ease of harvesting and protecting critical structures of neck.7
The present research become advocated to verify the predictability of Pectoralis Major Myocutaneous Flap (PMMC) and its scientific final outcomes in 168 Indian patients.
2. Materials and methods
A total of 168 PMMC flap reconstructions have been accomplished in the department of Oral and Maxillofacial Surgery all through the year 20017–2019 following institutional ethical clearance. This is the Retrospective Study where patients had been evaluated primarily based on history, clinical, radiological, histopathological findings, and ordinary blood examination prior to treatment making plans. The scientific staging become accomplished in accordance to TNM category (UICC 2002 criteria).
Inclusion criteria turned into- 1. Patients diagnosed with oral carcinoma confirmed after histopathology; 2. Patients willing to be a part of the scientific research; 3. Cases in which the defect need reconstruction with local flap, PMMC flap. 4. Compromised patient status where free flaps are contraindicated.
Exclusion criteria- 1. Patients not willing to be a part of the study. 2. Cases where the defect size would need reconstruction with free flap.
Parameters included in our study had been post-operative complications of PMMC flap in terms of (1) flap necrosis-complete and partial (2) wound dehiscence (3) neck bulk acceptance (4) range of motion.
Informed consent was signed prior to the scientific study. Under all aseptic precautions neck dissection and tumor resection was done.
2.1. Surface markings of vascular pedicle of PMMC flap
First Line- A line is marked connecting a shoulder tip to the xiphisternum.
Second Line- A line drawn perpendicular from the middle of the clavicle to divide the first line.
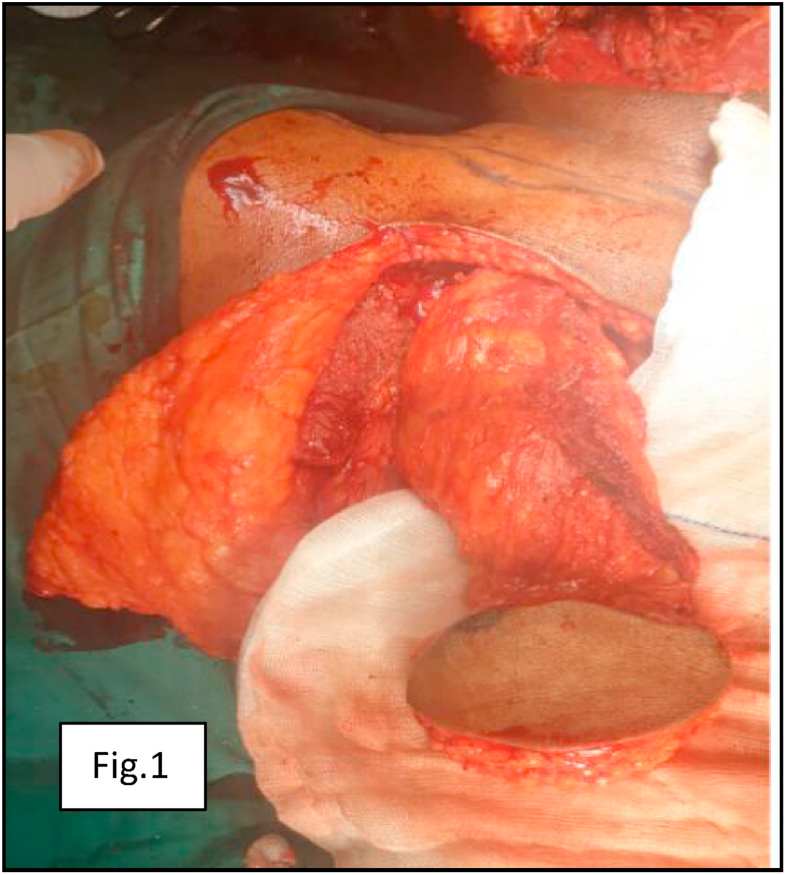
Flap harvesting method-The design of the flap and the skin paddle have been based on the size, site and form of the defect. The design of the skin paddle being commonly medial and beneath to the nipple. In case of females the paddle is placed in inframammary crease. The dissection is extended onto the pectoralis major muscle with the skin incised around the skin paddle. The skin paddle have to be bevelled radially so as to encompass as many myocutaneous perforators as possible that supply the skin paddle and have to be tacked with sutures to minimise the theat of shearing damage to the perforators. The distance between the superior aspect of the skin paddle and the inferior aspect of the clavicle ought to equal or exceed the distance among the recipient site for the flap and the inferior aspect of the clavicle in order to make sure that the pedicle is of adequate length. The flap was extended up as far as the coracoid process wherein the pedicle was narrowed and laterally up to the deltopectoral groove. Further elevation was permitted with division of muscle medially and laterally with extra arc of rotation. The lateral pectoral vessels were left intact or divided relying on the extent of the flap required (Fig. 1). Flap was passed above the clavicle to the recipient site through a prepared tunnel of skin. The sutures secured to the flap were then removed and the skin of the flap was sutured to the mucosal defect. The incision of neck was closed over the vascular pedicle and muscle. The chest skin was mobilized drastically and closed in all cases. For neck and chest, separate closed suction drains No. 16 have been utilized. Nasogastric tubes had been inserted in all sufferers for feeding. All the specimens have been dispatched for histopathological restaging following surgical procedure. Length of the cutaneous paddle, gender comparison of postoperative complications associated to flap like flap necrosis-complete and partial, wound dehiscence; and patient related like neck bulk acceptance and range of motion have been documented. All cases were often observed up postoperatively for 1–3 years and carefully reviewed for recurrence.
Fig. 1.
PMMC Flap alongwith pedicle.
3. Results
On assessment of the collected data, it was found that amongst 168 patients 121 were males and 47 females, between age group of 30–70 years with median age at the time of surgery as 53.6 years. All patients had biopsy confirmed malignancy of oral cavity. These patients underwent resection of primary lesion and reconstruction with PMMC flap. Larger number of cases showed squamous cell carcinoma involving right buccal mucosa (34.5%), followed by left buccal mucosa with floor of mouth (18.5%), left buccal mucosa (13.6%), right alveolus (8.3%), right RMT (6.5%), left mandible and left RMT with same frequency (4.8%), left alveolus (1.8%) and right buccal mucosa with RMT (1.2%). Average size of skin paddle of PMMC was 6.5 × 8.7 cm with a range of 5 cm × 7 cm–14 cm × 12 cm. Some were bipedicled flap whose skin paddle was greater in size. 12 (9.9%) male patients underwent bipedicle flap while 7 (14.9%) were female patients. Nutrition was maintained through nasogastric tube for a minimum of 15 days. All documented complications of the study are presented in Table 1. Complications were compared with regard to patient gender with respect to flap necrosis and wound dehiscence (Fig. 2). Patients who developed complications were managed conservatively by routinely change in dressing and irrigation of reconstruction site. Majority of our patients received postoperative radiotherapy, however none of them advanced any hassle associated to healing. Patients were kept for follow up postoperatively every 2 months up to 1–3 years depending on duration. Final functional outcome and esthetics was acceptable in all cases. At last the treated cases were referred to the Department of Maxillofacial Prosthodontics for evaluation and prosthodontic rehabilitation(See. Table 2).
Table 1.
Complications: Flap related and Patient related.
| Sr. N. | Flap related | Sex N (%) | Total N (%) | |
|---|---|---|---|---|
| M | F | |||
| 1. | Partial Flap necrosis | 0 | 3 (6.4) | 3 (1.8) |
| 2. | Complete Flap necrosis | 0 | 0 | 0 |
| 3. | Wound Dehiscence | 5 (4.1) | 6 (12.8) | 11 (6.5) |
Male; F- Female; N- Number; %- Percentage; Sr- Serial.
Fig. 2.
Partial flap necrosis with wound dehiscence.
Table 2.
Complications: Flap related and Patient related.
| Sr. N. | Patient related | Sex N (%) | Total N (%) | |
|---|---|---|---|---|
| M | F | |||
| 1. | Neck bulk acceptance | |||
| Accepted | 82 (67.8) | 34 (72.3) | 116 (69) | |
| Not accepted | 39 (32.2) | 13 (27.7) | 52 (31) | |
| 2. | Range of Motion | |||
| Affected | 35 (28.9) | 11 (23.4) | 46 (27.4) | |
| Not affected | 86 (71.1) | 36 (76.6) | 122 (72.6) | |
Male; F- Female; N- Number; %- Percentage; Sr- Serial.
4. Discussion
With the advent of improved knowledge, scientific capabilities and availability of higher infrastructure, free flap reconstruction remains the benchmark and the first preference of reconstruction of the head and neck physician. In case of failure of free flaps, PMMC flaps are kept reserved for rescue technique and compromised patient status.3,8,9 Saito et al. stated that the most important benefit of PMMC flap is survival and that complete flap necrosis was absent in their patients. Partial flap necrosis occurred in 4 patients (33%) out of 12 patients. Wound dehiscence was observed in 1 patient. Overall microvascular free flap loss may be visible even in the hands of professional surgeons. But PMMC flap failure is very uncommon due to its reliable vascularity.8
In our literature, we observed a complication rate of 1.8% occurrence of partial flap necrosis with no documented complete flap necrosis. All the partial flap necrosis failures was seen in female patients. Our results are comparable to those with Vartanian et al.9 who reported least complication rate for complete and partial flap necrosis of 2.4% and 9.7% respectively in 371 cases. According to Jena et al.10 more complications were found in female patients when PMMC flap was harvested in the defect because of high amount of adipose tissue and due to interposition of breast tissue between the muscle and the skin paddle.
Rikimaru et al. pointed out that positioning the skin island simply medially to the nipple, over the 4th, 5th and 6th intercostal spaces, is important and if placed below the 7th rib will increase the threat of flap loss.11 In our cases, we did not look for this entity; for this reason it’s contribution to flap necrosis in our study is not known.
El-Marak by reported 2 cases (8%) of total flap necrosis amongst 25 patients and partial flap necrosis in 3 patients (12%).12 According to Baek et al., in 1982 total flap necrosis in 133 patients was 1.5%.13 This contrasting difference between these studies and present study can be attributed by careful handling of pedicle, avoiding kinking of vascular pedicle and avoiding closure of the flap under tension by prior planning for proper reconstruction.
Wound dehiscence was present more in females; 6 (12.8%) than in males; 5 (4.1%). The most common complication which accounted in 11 (6.5%) patients. Wound dehiscence can be prevented by avoiding over tight closure of wound that can lead to reduced blood supply of skin margins. Dehiscence can also be prevented by post operative regular dressing of sutured margins which is pivotal in managing wound dehiscence at neck region. This was managed by resuturing the site and changing the dressing regularly.
Information collection from patients was performed with questionare method for the acceptance of neck bulk. 52 (31%) patients did not accepted the neck bulk of PMMC flap from which 39 (32.2%) were male and 13 (27.7%) were female patients. This can be avoided by dividing a portion of the clavicular fibers of the muscle to accommodate only the neurovascular pedicle.6
Patients have been evaluated for range of motion during follow up period. 46 (27.4%) patients were affected with 35 (28.9%) male and 11 (23.4%) female patients.
Due to the fact of its simplicity, ease of approach, versatility, and reliability, reconstruction with the PMMC Flap seems to be safe and effective with desirable range of complications in patients. According to our study, PMMC flap is a superb choice in restrained resources and where microvascular reconstruction facilities are no longer available.
5. Conclusion
The outcomes of our study simply demonstrate that the PMMC flap still remains the ‘workhorse’ of reconstruction in head and neck cancer patients. The usual complication rates are properly within desirable range and most can be managed conservatively. However, reconstruction in younger women is challenging and prior warning and counseling must be encouraged. Donar site may also need revision plastic surgical operation. PMMC flaps are kept reserved for rescue technique in case of failure of free flaps. PMMC flaps are best used in compromised patient status, or if planned as soft tissue filler in combination with free flaps.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Limitations of the study
-
1.
Quality of life have not been addressed.
-
2.
Comparison of flap complications according to the subsite of oral cavity have not been outlined.
Declaration of competing interest
Authors have no conflict of interest to disclose.
References
- 1.Trivedi N.P., Kekatpure V.D., Trivedi N.N., Kuriakose M.A. Head and neck cancer in India: need to formulate uniform national treatment guideline? Indian J Canc. 2012 Jan-Mar;49(1):6–10. doi: 10.4103/0019-509X.98907. [DOI] [PubMed] [Google Scholar]
- 2.Anehosur V., Dikhit P.S., Nagraj N., Jayade B., Kumar N. PMMC flap revisited and its clinical outcome in 150 patients. J Maxillofac Oral Surg. 2020 Mar;19(1):26–31. doi: 10.1007/s12663-019-01228-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhanja A., D’Souza D.S., Roy C., Poddar R.N. Reliability of the pectoralis major myocutaneous flap in reconstructive oral cancer surgery in developing countries: our experience. Med J Armed Forces India. 2016 Dec;72:1–7. doi: 10.1016/j.mjafi.2016.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Novakovic D., Patel R.S., Goldstein D.P., Gullane P.J. Salvage of failed free flaps used in head and neck reconstruction. Head Neck Oncol. 2009 Aug 21;1:33. doi: 10.1186/1758-3284-1-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chaudhary R., Akhtar M.S., Bariar L.M., Khurram M.F. Use of pectoralis major myocutaneous flap for resurfacing the soft tissue defects of head and neck. J Orofac Sci. 2014 Oct;6(2):88–93. [Google Scholar]
- 6.Tripathi M., Parshad S., Karwasra R.K., Singh V. Pectoralis major myocutaneous flap in head and neck reconstruction: an experience in 100 consecutive cases. Natl J Maxillofac Surg. 2015 Jan-Jun;6(1):37–41. doi: 10.4103/0975-5950.168225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leite A.K., de Matos L.L., Belli M. Pectoralis major myocutaneous flap for head and neck reconstruction: risk factors for fistula formation. Acta Otorhinolaryngol Ital. 2014 Dec;34(6):389–393. [PMC free article] [PubMed] [Google Scholar]
- 8.Saito A., Minakawa H., Saito N., Nagahashi T. Indications and outcomes for pedicled pectoralis major myocutaneous flaps at a primary microvascular head and neck reconstructive center. Mod Plast Surg. 2012;2:103–107. [Google Scholar]
- 9.Vartanian J.G., Carvalho A.L., Carvalho S.M.T., Mizobe L., Magrin J., Kowalski L.P. Pectoralis major and other myofascial/myocutaneous flaps in head and neck cancer reconstruction: experience with 437 cases at a single institution. Head Neck. 2004 Dec;26(12):1018–1023. doi: 10.1002/hed.20101. [DOI] [PubMed] [Google Scholar]
- 10.Jena Amitabh, Patnayak Rashmi, Sharan Rajeev, Kumar Reddy Siva, Manilal Banoth, Chandrasekhar Rao Leela Mohan. Outcomes of pectoralis major myocutaneous flap in female patients for oral cavity defect reconstruction. J Oral Maxillofac Surg. 2014 Jan;72(1):222–231. doi: 10.1016/j.joms.2013.06.205. [DOI] [PubMed] [Google Scholar]
- 11.Rikimaru H., Kiyokawa K., Inoue Y., Tai Y. Three-dimensional anatomical vascular distribution in the pectoralis major myocutaneous flap. Plast Reconstr Surg. 2005 April;115(5):1342–1352. doi: 10.1097/01.prs.0000156972.66044.5c. [DOI] [PubMed] [Google Scholar]
- 12.El Marakby H. The reliability of pectoralis major myocutaneous flap in head and neck reconstruction. J Egypt Natl Canc Inst. 2006 Mar;18(1):41–50. [PubMed] [Google Scholar]
- 13.Baek S., Lawson W., Biller H. An analysis of 133 pectoralis major myocutaneous flaps. Plast Reconstr Surg. 1982 Mar;69(3):460–469. doi: 10.1097/00006534-198203000-00010. [DOI] [PubMed] [Google Scholar]