Dear Editor,
Early data during the current pandemic demonstrated worse outcome in patients with pre-existing heart disease [1]. Consequently, adults with congenital heart disease (ACHD) have been deemed at high risk of adverse outcome from Covid-19, particularly those with complex anatomy [2]. We would like to report our experience with Coronavirus disease 2019(Covid-19) among patients with Fontan circulation at our ACHD tertiary centre.
We retrospectively included all Fontan patients who were infected from the beginning of the pandemic to 14th March 2021. Informed consent was obtained from each patient. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institution's ethical committee. Statistical analysis was performed using Medcalc version 19.2.0. Continuous variables were reported as mean ± SD or median [IQR], as appropriate. Student t-test was used to compare baseline oxygen saturation values with those during infection. P-value was set to<0.05.
Over 1 year of Covid-19 pandemic, 7 patients (28 years [25.5–39.55], 57%male) out of 63 patients with Fontan circulation followed-up at the ACHD Unit of Monaldi Hospital were infected, with an estimated 1-year incidence of 11%. The main details on patients’ medical history and Covid-19 course are reported in Table 1 . Patients were followed by an ACHD-specialist via remote medicine modalities: they were periodically interrogated on their symptoms, instructed to monitor their peripheral oxygen saturation and to seek urgent medical attention in case of minimal signs of deterioration. Overall, no significant drop in the oxygen saturation value was found (mean SpO2 at baseline: 92.1 ± 3.3%, SpO2 during Covid-19: 88.4 ± 3.6%; p = 0.06). Six out of 7 patients reported spontaneous resolution of symptoms after a median of 8.5 [7–14.5] days. Patient 1 was initially admitted to our Institution and discharged home on the same day, after negative chest CT. Patient 7 was admitted to our institution for desaturation: chest CT on admission demonstrated mild bilateral lung involvement with a Chung score [3] of 2/20. The patient was successfully managed by a multidisciplinary team of pneumologists and ACHD-specialized cardiologists: she received high flow oxygen and steroids. The remaining patients did not report any complications requiring hospital admission. All patients in our cohort survived Covid-19 and made full recovery. Patients 2 and 4 were reviewed in the outpatient clinic 4 weeks after being tested negative for Covid-19: there was no significant change in their clinical status compared to baseline.
Table 1.
Previous medical history and Covid-19 course in the study population.
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Patient 7 | |
|---|---|---|---|---|---|---|---|
| Sex | M | F | F | M | M | M | F |
| Age | 24 yo | 27 yo | 40 yo | 39 yo | 56 yo | 28 yo | 23 yo |
| Diagnosis | PA IVS | AVSD | TA | DILV with TGA | Dextrocardia TA with TGA |
TA | TA |
| Physiological stage | B | C | C | C | C | C | D |
| Type of Fontan | Extracardiac conduit | Extracardiac conduit | Bjork Fontan | Extracardiac conduit | Extracardiac conduit | Lateral tunnel | Extracardiac conduit |
| Previous interventions | BT shunt Glenn Fontan |
PA banding Glenn Damus-Kaye Fenestrated Fontan Fenestration closure |
Atrial septostomy BT shunt Fontan |
BT shunt Fontan |
BT shunt (x2) Glenn Fontan |
BT shunt Glenn Fontan Stenting of Fontan conduit |
Glenn Fontan Stenting of Fontan conduit |
| NYHA class | 2 | 2 | 3 | 3 | 3 | 2 | 3 |
| Oxygen saturation | 90% | 92% | 89% | 96% | 88% | 94% | 96% |
| Arrhythmic history | NSVT | none | AF AVB |
none | NSVT | paroxysmal AF/AVB | none |
| Antiplatelet/anticoagulant | warfarin | aspirin | warfarin | edoxaban | aspirin | aspirin clopidogrel |
aspirin |
| Other medications | beta blockers | ACE-i | beta blockers diuretics flecainide |
beta blockers | sotalol ACE-i diuretics oxygen |
sotalol | beta blockers diuretics albumin |
| hospitalization for HF | none | none | none | none | none | none | 2 episodes in 2020 |
| MELD-XI score | 5.25 | not available | 4.41 | 8.18 | 13.44 | 5.67 | 23.25 |
| Other comorbidities | none | none | dysthyroidism Hepatitis C |
none | Restrictive lung disease | none | PLE AKI currently on dialysis Recent hemoperitoneum |
| Ventricular function | Normal (EF = 55%) | Normal (EF = 55%) | Normal (EF = 55%) | Normal (EF = 65%) | Mildly impaired (EF = 50%) | Normal (EF = 57%) | Low-normal (EF = 52%) |
| AV valve(s) regurgitation | Mild | Severe | Moderate | Mild | Moderate | Moderate | Moderate |
| Other echo findings | Normal TCPC flow | Normal TCPC flow | Grossly dilated RA Normal flow in Fontan circuit |
Moderate subaortic obstruction Normal TCPC flow |
Moderate aortic regurgitation | Normal flow in Fontan circuit | Mild residual obstruction of Fontan circuit |
| Peak VO2 | 23.4 | 25.8 | Not available | 24.3 | 10.3 | 11.2 | Not available |
| VE/VCO2 | 34 | 37.4 | Not available | 24 | 41 | 26 | Not available |
| Pro BNP nt (pg/ml) |
75 |
100 |
509 |
296 |
5411 |
140 |
570 |
| Covid-19 course | |||||||
| Symptoms | Malaise Fatigue Sore throat Cough |
Fever Sore throat Loss of smell Cough |
Fever Fatigue Myalgia Diarrhoea Cough |
Fever Fatigue |
Fever Cough Dyspnoea |
Fever Cough Myalgia Headache |
Fever Malaise Fatigue Cough Dyspnoea |
| Symptoms duration | 7 days | 10 days | 25 days | 2 days | 16 days | 7 days | not available |
| Reason for testing | Contact with a case | Symptoms | Contact with a case | Screened at work | Symptoms | Symptoms | Symptoms |
| Diagnosis | PCR test | PCR test | PCR test | Serological test | PCR test | PCR test | PCR test |
| Lowest SpO2 peak | 89% | 92% | 86% | 93% | 83% | 90% | 86% |
| Treatment | azithromycin | none | azithromycin | none | azithromycin | azithromycin | high flow oxygen steroids azithromycin |
| Outcome | Full recovery | Full recovery | Full recovery | Full recovery | Full recovery | Full recovery | Hospitalization required |
AKI = acute kidney injury, AVB = atrioventricular block, AF = atrial fibrillation, AVSD = atrioventricular septal defect, Covid-19 = Coronavirus disease 2019, CT = computed tomography, DILV = double inlet left ventricle, EF = ejection fraction, HF = heart failure, MELD-XI = Model for End-stage Liver Disease excluding INR, NSVT = non-sustained ventricular tachycardia, PA IVS = pulmonary atresia with intact ventricular septum, PMK = pacemaker, TA = tricuspid atresia, TCPC = total cavopulmonary connection, TGA = transposition od the great arteries, PCR = polymerase chain reaction, PLE = protein losing enteropathy RA = right atrium, SpO2 = peripheral oxygen saturation.
Covid-19 may have multiple peculiar implications in patients with Fontan circulation due to their complex physiology and unique hemodynamic characteristics:
-
-
Potential complications: Covid-19-related interstitial pneumonia may raise the pulmonary vascular resistance with deleterious effects on the pulmonary blood flow and, ultimately, on the preload-dependent cardiac output. Moreover, positive-pressure ventilatory support might interfere with the systemic venous return with devastating effects. Systemic inflammation might easily trigger supraventricular arrhythmia in this susceptible population. Additionally, Covid-19 might induce a hypercoagulable state in Fontan patients who are already prone to thromboembolic events. Covid-19 has also been associated with myocardial injury, a particularly worrisome complication in patients with univentricular heart. Another common manifestation in patients with mild forms of Covid-19 is diarrhoea, which may intensify fluid and electrolyte imbalance in patients on chronic diuretic treatment. Finally, a small number of patients may present the uncommon Covid-19-induced hepatic damage [4], which may superimpose on a Fontan associated liver disease causing acute liver dysfunction, with potential negative impact on the outcome [5].
The main potential consequences of Covid-19 in patients with Fontan circulation are graphically summarized in Fig. 1 .
-
-
Overestimation of respiratory involvement severity: Fontan patients' oxygen saturation may range between 90 and 95%. Lower values are expected in those with right-to-left shunt. During initial urgent assessment of a Covid-19-positive Fontan patient, a low SpO2 value might trigger a proactive and likely harmful invasive approach from medical staff with no experience in ACHD. The absolute SpO2 value should therefore be considered in the context of the patient's previous medical history.
-
-
Management strategy: Covid-19-positive Fontan patients should be admitted early to an ACHD centre in presence of signs of respiratory or cardiovascular impairment. For those requiring intensive assistance, a multidisciplinary management involving intensivists and ACHD-specialized cardiologists might improve the outcome.
Fig. 1.
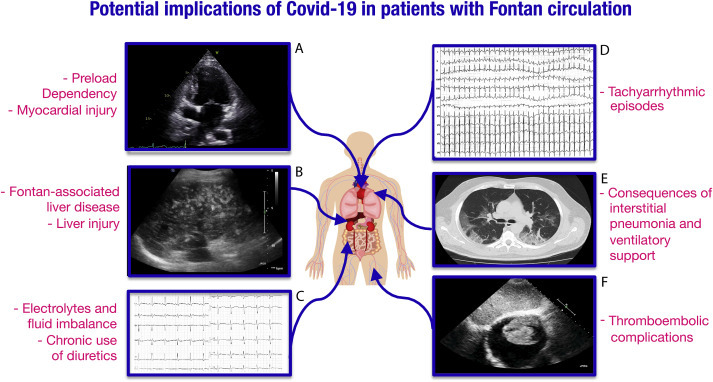
Main potential implications of Coronavirus disease 2019 in patients with Fontan circulation.
Patients with Fontan circulation have a complex physiology and may present multiorgan complications in case of infection. Covid-19-related interstitial pneumonia may raise pulmonary vascular resistance with deleterious effects on pulmonary blood flow in these patients. Moreover, respiratory support techniques including both non-invasive positive-pressure ventilation and mechanical ventilation may reduce the systemic venous return leading to impaired cardiac output in a preload-dependent circulation. Covid-19-related myocardial injury may further interfere the Fontan hemodynamics. Systemic inflammation might easily trigger arrhythmic events in this susceptible population. Gastrointestinal disorders may exacerbate fluid and electrolyte imbalance especially in those on chronic diuretic treatment and trigger arrhythmias. Fontan patients are prone to thromboembolic complication, which are also a known adverse event in Covid-19 patients. Finally, Covid-19-related hepatic damage may superimpose on a Fontan-associated liver disease.
A. Echocardiographic 4-chamber view in a patient with tricuspid atresia palliated with total cavopulmonary connection.
B. Liver fibrosis in a patient with Fontan circulation.
C. ECG of a patient with Fontan circulation and severe hypokaliemia.
D. ECG showing supraventricular tachycardia with a heart rate of 250 bpm in a patient with Fontan circulation.
E. Chest CT in patient with Covid-19 related interstitial pneumonia demonstrating multiple areas of ground glass opacity.
F. Right atrial thrombus in a patient with tricuspid atresia and atrio-pulmonary connection.
To the best of our knowledge, this is the first European report of Covid-19 in Fontan circulation. Surprisingly, in our cohort no one presented severe manifestations from Covid-19. Our data are in line with the positive outcome described in 10 Fontan patients in a single-centre US study [6]. These results may be partially explained with the observation that, despite the above-described multiple implications of Covid-19, patients with single-ventricle might be protected by younger age, patients’ education to self-isolation and chronic treatment with anticoagulants/antiplatelets, which were showed to improve the outcome [7,8]. Interestingly, according to the 2018 ACC/AHA ACHD guidelines [9], out of 7 patients in our study had an advanced physiological stage, which was reported as a risk factor of adverse outcome in ACHD patients [6]. Patients with failing Fontan or unstable haemodynamics may be at higher risk of complications from Covid-19. In our cohort, patient 7 was recently admitted for acute heart failure and had undergone abdominal surgery for hemoperitoneum following ovarian cyst rupture, which was complicated by acute kidney injury requiring dialysis shortly before contracting Covid-19.
After 1-year of observation, we found a relatively low rate of infection among our Fontan patients. The effects of our stringent preventive policy, which has already been described elsewhere [10], might have protected ACHD patients from exposure. However, due to the small number of cases, the real impact of Covid-19 might have been underestimated in our study. Multicentre studies in larger cohorts are warranted to establish the effect of Covid-19 in this population.
In conclusion, Covid-19 might severely undermine the complex Fontan circulation physiology with multiple mechanisms. In our cohort, however, Covid-19 was associated with mild respiratory symptoms and patients were mainly managed remotely. Fontan patients with unstable haemodynamics and multiorgan dysfunction or protein losing enteropathy may be more vulnerable to the effects of Covid-19. Despite our reassuring data, Covid-19-positive Fontan patients should be managed with a multidisciplinary approach involving ACHD-specialists.
Funding statement
The authors received no specific funding for this study.
Declaration of competing interest
The authors declare no conflicts of interest to report regarding the present study.
Footnotes
All the authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
References
- 1.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavius-infected pneumonia in Wuhan, China. J Am Med Assoc. 2020 Mar 17;323(11):1061–1069. doi: 10.1001/jama.2020.1585. PMID: 32031570; PMCID: PMC7042881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diller G.P., Gatzoulis M.A., Broberg C.S. Coronavirus disease 2019 in adults with congenital heart disease: a position paper from the ESC working group of adult congenital heart disease, and the International Society for Adult Congenital Heart Disease. Eur Heart J. 2020 Dec 12 doi: 10.1093/eurheartj/ehaa960. Epub ahead of print. PMID: 33313664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chung M., Bernheim A., Mei X., Zhang N., Huang M., Zeng X., Cui J., Xu W., Yang Y., Fayad Z.A., Jacobi A., Li K., Li S., Shan H. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020 Apr;295(1):202–207. doi: 10.1148/radiol.2020200230. Epub 2020 Feb 4. PMID: 32017661; PMCID: PMC7194022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bangash M.N., Patel J., Parekh D. COVID-19 and the liver: little cause for concern. Lancet Gastroenterol Hepatol. 2020 Jun;5(6):529–530. doi: 10.1016/S2468-1253(20)30084-4. Epub 2020 Mar 20. PMID: 32203680; PMCID: PMC7270582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang Q., Davis P.B., Xu R. COVID-19 risk, disparities and outcomes in patients with chronic liver disease in the United States. EClinicalMedicine. 2021 Jan;31:100688. doi: 10.1016/j.eclinm.2020.100688. Epub 2020 Dec 22. PMID: 33521611; PMCID: PMC7834443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lewis M.J., Anderson B.R., Fremed M. Impact of coronavirus disease 2019 (COVID-19) on patients with congenital heart disease across the lifespan: the experience of an academic congenital heart disease center in New York city. J Am Heart Assoc. 2020 Dec;9(23) doi: 10.1161/JAHA.120.017580. Epub 2020 Oct 14. PMID: 33196343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tang N., Bai H., Chen X., Gong J., Li D., Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemostasis. 2020;18(5):1094-1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ouyang Y., Wang Y., Liu B., Ma X., Ding R. Effects of antiplatelet therapy on the mortality rate of patients with sepsis: a meta-analysis. J Crit Care. 2019;50:162–168. doi: 10.1016/j.jcrc.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 9.Stout K.K., Daniels C.J., Aboulhosn J.A. AHA/ACC guideline for the management of adults with congenital heart disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol. 2018;73(12):e81–e192. doi: 10.1016/j.jacc.2018.08.1029. 2019 Apr 2. Epub 2018 Aug 16. Erratum in: J Am Coll Cardiol. 2019 May 14;73(18):2361-2362. PMID: 30121239. [DOI] [PubMed] [Google Scholar]
- 10.Scognamiglio G., Fusco F., Merola A., Palma M., Correra A., Sarubbi B. Caring for adults with CHD in the era of coronavirus disease 2019 pandemic: early experience in an Italian tertiary centre. Cardiol Young. 2020 Oct;30(10):1405–1408. doi: 10.1017/S1047951120002085. Epub 2020 Jul 6. PMID: 32624052; PMCID: PMC7399145. [DOI] [PMC free article] [PubMed] [Google Scholar]


