Highlights
-
•
Mammary Analogue Secretory Carcinoma (MASC) is a head and neck tumour that was first defined in 2010.
-
•
Only two cases of Secretory Carcinoma have reported in the sinuses.
-
•
We present a case of a Secretory Carcinoma presenting in the maxillary and ethmoid sinuses.
-
•
The tumour treated with surgical resection and re-resection and was disease free at 1 year follow up.
Keywords: Mammary analogue secretory carcinoma, Secretory carcinoma, Case report
Abstract
Introduction
Secretory Carcinoma is a recently discovered head and neck tumour. Surgical resection is generally the first line of treatment with neck dissection, radiation, and chemotherapy decided based on clinical, radiological, and histological parameters. We present a case of a Secretory Carcinoma presenting in the maxillary and ethmoid sinuses.
Case
A 39-year-old male presented with left nasal obstruction and chronic rhinosinusitis beginning after surgical repair of the mandible and maxilla due to facial trauma. A CT scan of the head showed soft tissue density in the left maxillary sinus extending through the ethmoid sinus and posterior nasal cavity. Functional endoscopic sinus surgery (FESS) was performed to remove the obstructing lesion. Biopsy was analysed and the main differential diagnosis was between a non-intestinal type adenocarcinoma of nasal origin and a salivary carcinoma.
Discussion
To our knowledge, there have only been two cases of Secretory Carcinoma reported in the sinuses: one case in the ethmoid sinus and the other in the maxillary sinus. This is the first to report follow up at 1 year.
Conclusion
Both MRI and exam showed no evidence of recurrent disease at one year follow up. This report aims to further the understanding of Secretory Carcinoma tumours in the sinuses. Our report could be used to further understand diagnostic criteria for Secretory Carcinoma in the sinuses as well as treatment outcomes for surgical resection without adjuvant treatment.
1. Introduction
Mammary Analogue Secretory Carcinoma (MASC) is a recently discovered head and neck tumour that was first defined in 2010 by Skalova et al. MASC is a carcinoma typically found in the oral cavity and major salivary glands, characterized by light microscopic and immunohistochemical features strongly reminiscent of Secretory Carcinoma (SC) of the breast and histologic features similar to Acinar Cell Carcinoma (ACC) of the salivary glands [1]. Secretory Carcinoma is now also an accepted synonym for salivary MASC and is endorsed by the WHO [2].
Secretory Carcinoma typically possesses a specific genetic marker that is also present in SC of the breast. This genetic marker is a translocation, resulting in the fusion of the ETV6 gene on chromosome 12 and the NTRK3 gene on chromosome 15. In occasional cases, ETV6 can fuse with non-NTRK3 partners. The ETV6-NTRK3 translocation allows definitive differentiation of Secretory Carcinoma from ACC and other salivary tumours with which it may be confused [1,3]. Fluorescence in situ hybridization for the ETV6 translocation is the gold standard to diagnose Secretory Carcinoma as this translocation is present in 99% of Secretory Carcinoma tumours [4]. Before its discovery, cases of Secretory Carcinoma were diagnosed generally as ACC or Adenocarcinoma not otherwise specified [5]. Many cases of Secretory Carcinoma were discovered in archived cases previously classified as ACC [6]. In a study by Bishop et al., 79% (11/14) of extraparotid gland tumours originally diagnosed as ACC were reclassified as Secretory Carcinoma [7].
Due to the rarity and novelty of Secretory Carcinoma, the incidence is still unknown, but it has been estimated that it accounts for less than 0.3% of all salivary gland tumours [8]. Secretory Carcinoma typically presents in patients between the ages of 40–60 and has been reported to be slightly higher in males [9,10]. The most common presentation is a slow-growing growing, painless nodule [6]. Seventy percent of Secretory Carcinoma tumours are found in the major salivary glands, (predominantly the parotid) and twenty percent arise from minor salivary glands [9]. Cases have been reported in the parotid gland, submandibular salivary gland, sinuses and, oral cavity, including lips, soft palate, buccal mucosa, the base of the tongue, and the skin [5,9,11]. Despite the different genetics between ACC and Secretory Carcinoma, studies have explored treatment outcomes and prognosis of Secretory Carcinoma and ACC and concluded that they can be treated similarly [9,12].
We present a case of a Secretory Carcinoma presenting in the maxillary and ethmoid sinuses.
This work has been reported in line with the SCARE criteria [15].
2. Case presentation
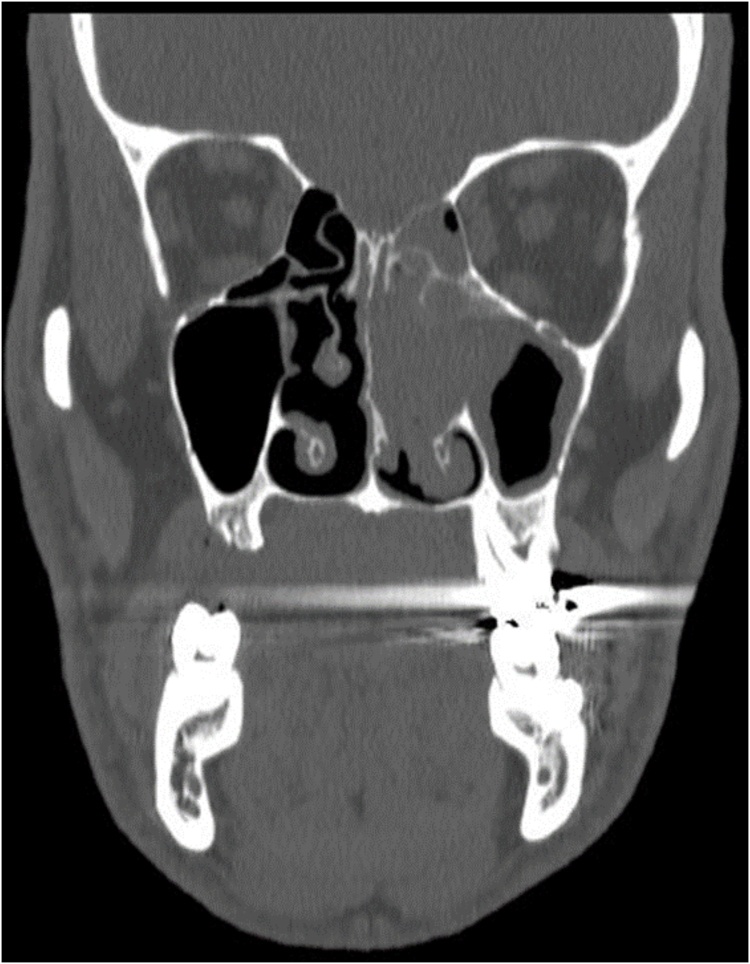
A 39-year-old male was referred to outpatient otolaryngology-head and neck surgery clinic with left nasal obstruction and chronic rhinosinusitis, reported to be present after surgical repair of the mandible and maxilla due to facial trauma. Past medical history was significant for a 25 pack-year history of smoking and daily cannabis use. A CT scan of the head showed soft tissue density in the left maxillary sinus extending through the ethmoid sinus and posterior nasal cavity. The patient was booked for functional endoscopic sinus surgery (FESS) to remove the lesion and this was performed by the staff surgeon. During surgery, an erythematous, lobulated mass arising from middle turbinate was noted with extenstion to the lateral nasal wall, posterior nasal choanae, and up into sphenoid rostrum was removed. Significant debulking and biopsies were taken from the left ethmoid cavity and left posterior choana (Fig. 1).
Fig. 1.
Coronal CT image of head showing soft tissue density in left maxillary sinus extending through the ethmoid sinus and posterior nasal cavity.
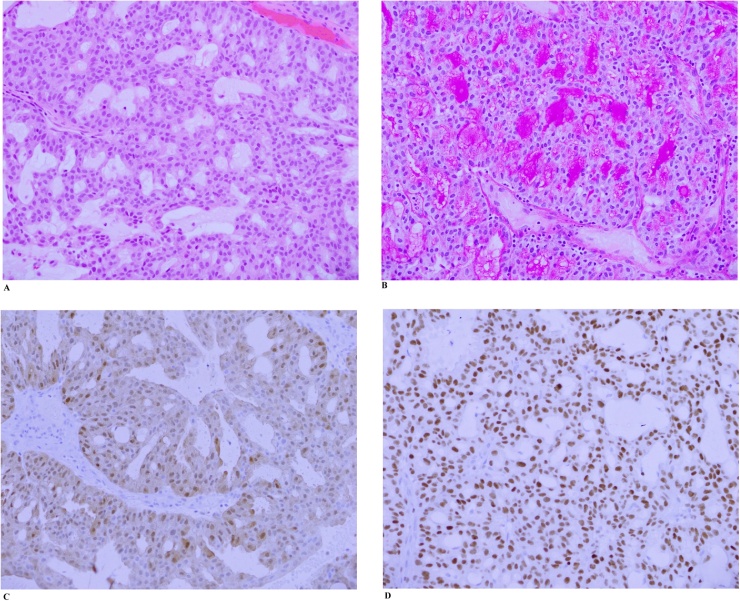
The biopsy specimens contained multiple fragments of adenocarcinoma with a cribriform growth pattern, replacing most of the tissue (Fig. 2A). There was confluent tumour necrosis in some areas. The tumour cells had eosinophilic to slightly vacuolated cytoplasm, mild nuclear pleomorphism, and easily identified mitotic figures (up to 7/10 high power fields). Abundant mucin production was noted with a PAS stain (Fig. 2B). Immunohistochemistry showed positivity for CK7, CK19, vimentin, gross cystic disease fluid protein (GCDFP), S100 (Fig. 2C), and GATA3 (Fig. 2D). About 50% of cells were weakly to moderately p63 positive. There was focal weak mammaglobin staining. CK20, CK5/6, TTF-1, calponin, and CDX2 were negative.
Fig. 2.
A. Hematoxylin and eosin stained image (200×) showing the tumour with a cribriform glandular pattern and fairly uniform oval to round nuclei.
B. PAS stain showing abundant mucin production.
C. S100 immunostain showing nuclear and weak cytoplasmic positivity.
D. GATA3 immunostain showing diffuse positivity.
The initial impression was of an adenocarcinoma, which in the nasal cavity could be of the salivary or non-salivary type or be metastatic from another primary site. Non-salivary adenocarcinomas are either intestinal or non-intestinal type. An intestinal type adenocarcinoma was excluded by immunohistochemistry (lack of staining for CK20 or CDX2) and similarly, the morphology was not typical of common metastatic sources (e.g. lung). The main differential diagnosis was between a non-intestinal type adenocarcinoma of nasal origin and a salivary carcinoma. Although the combination of immunohistochemistry and morphology was not typical of most salivary tumours, Secretory Carcinoma was a consideration.
Molecular cytogenetic studies were positive for rearrangement of the ETV6 (12p13) locus in 92% of 100 interphase cells analyzed. This finding, in combination with the morphology and immunohistochemistry, was consistent with Secretory Carcinoma. There was a greater degree of cytologic atypia and necrosis than in most Secretory Carcinoma from other sites (e.g. parotid or oral cavity). The impact of this finding on the patient’s prognosis is unclear.
A more extensive endoscopic re-resection and medial maxillectomy was performed approximately three months after initial resection. All the specimens were negative for residual Secretory Carcinoma.
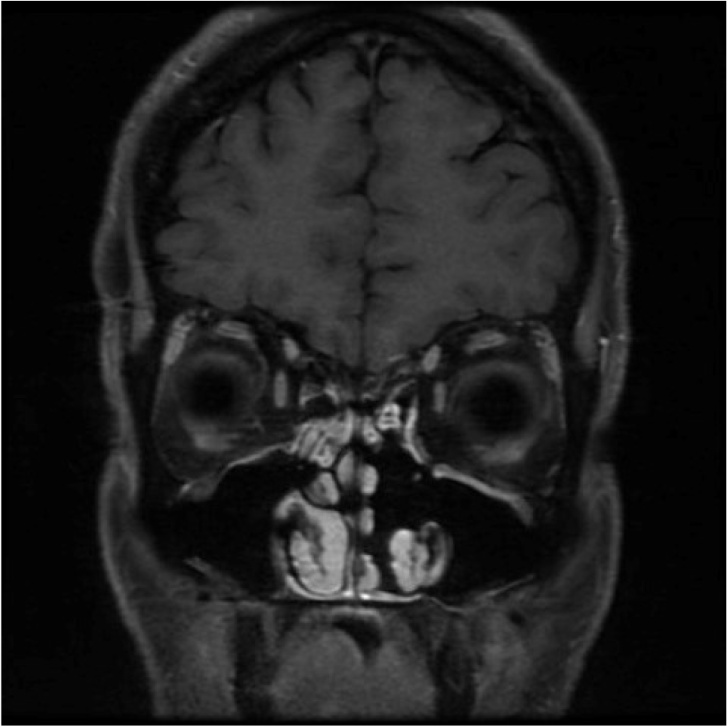
The patient’s case was reviewed post-operatively by the tumour board. As there were no signs of residual disease, the tumour board recommended endoscopic observation in three months, MRI in six months, and no additional adjuvant therapy. The patient was discharged with a prescription for nasal steroids. The patient returned for endoscopic observation three months later that showed no signs of recurrent disease. The six-month MRI was delayed due to COVID-19. Instead, the patient received the MRI at his one year follow up. Both MRI and exam showed no evidence of recurrent disease (Fig. 3).
Fig. 3.
Coronal MRI image from the T1 FLAIR with contrast at one year follow up showing no sign of recurrent disease.
3. Discussion
We presented a case of a Secretory Carcinoma presenting in the maxillary and ethmoid sinuses. To our knowledge, there have only been two cases of Secretory Carcinoma reported in the sinuses: one case in the ethmoid sinus and the other in the maxillary sinus [5,11]. The ethmoid sinus case was diagnosed post surgical resection and did not provide details regarding recurrence, survival, or adjuvant therapies [5]. The maxillary sinus case received adjuvant radiation therapy post surgical resection due to a positive resection margin. This patient had no signs of recurrence eight months after resection [11].
The guidelines for surgical treatment, chemoradiation, and follow up have not yet been standardized, due to the rarity and novelty of the disease [9,13]. Surgical resection is generally the first line of treatment with neck dissection, radiation, and chemotherapy decided based on clinical, radiological, and histological parameters [6,9,3]. A contemporary review by Sethi et al. reviewed the treatment of 86 Secretory Carcinoma cases who received some form of surgical resection for the primary tumour and roughly 22% (19/86) received adjuvant therapy. In this review 21 patients underwent neck dissections, 17 patients received adjuvant radiation, and 2 patients received adjuvant chemoradiation [6]. The review also showed a 5% (4/91) disease-related mortality and the mean disease‐free survival, using death or recurrence as the end‐point, was 92 months (95% CI, 71–115) [6]. A different study followed nine patients and three developed local recurrence at a time ranging from 10 to 101 months [14].
Our case was the first case of Secretory Carcinoma in the sinuses to report follow up after 1 year. We showed that surgical resection without adjuvant treatment was adequate to prevent recurrence in the first year post operatively. Potential limitations to our study include only having follow up at 1 year mark and not following the patient longer. In addition, larger sample sizes will be required to further assess the effectiveness of surgical resection without adjuvant treatment for Secretory Carcinoma in the sinuses. Our report could be used to further understand diagnostic criteria for Secretory Carcinoma in the sinuses as well as treatment outcomes for surgical resection without adjuvant treatment.
4. Conclusion
Secretory Carcinoma is a recently described tumour that commonly presents as a slow-growing painless nodule. It has been reported in multiple head and neck subsites but only reported twice in the sinuses. Fluorescence in situ hybridization for the ETV6 translocation is the gold standard for the diagnosis of Secretory Carcinoma. To date, surgical excision is the mainstay of therapy, and consideration of adjuvant therapy is done on a case by case basis depending on risk factors.
We presented a case of a 39-year-old with Secretory Carcinoma in his maxillary and ethmoid sinus. The patient is disease-free one year post-operatively. This report aims to further the understanding of Secretory Carcinoma tumours in the sinuses
Declaration of Competing Interest
The authors report no declarations of interest.
Sources of funding
None.
Ethical approval
Exempt.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Kurt Willis – Author of manuscript.
Dr. Rigby and Dr.Bullock – clinical care of patient, clinical expertise and editing.
Registration of research studies
Not applicable.
Guarantor
Dr. Matthew Rigby.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Skálová A., Vanecek T., Sima R., Laco J., Weinreb I., Perez-Ordonez B., Starek I., Geierova M., Simpson R.H., Passador-Santos F., Ryska A., Leivo I., Kinkor Z., Michal M. Mammary analogue secretory carcinoma of salivary glands, containing the etv6-ntrk3 fusion gene: a hitherto undescribed salivary gland tumor entity. Am. J. Surg. Pathol. 2010;34:599–608. doi: 10.1097/PAS.0b013e3181d9efcc. [DOI] [PubMed] [Google Scholar]
- 2.J.N. Eble, G. Sauter, J.I. Epstein, S.I.A. Eds, W. Health, WHO Classification of Head and Neck Tumors 2017, 2017.
- 3.Skalova A., Michal M., Simpson R.H. Newly described salivary gland tumors mammary analog secretory carcinoma. Nat. Publ. Gr. 2017;30:27–43. doi: 10.1038/modpathol.2016.167. [DOI] [PubMed] [Google Scholar]
- 4.Skalova A. Mammary analogue secretory carcinoma of salivary gland origin: an update and expanded morphologic and immunohistochemical spectrum of recently described entity. Head Neck Pathol. 2013;7:30–36. doi: 10.1007/s12105-013-0455-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lurquin E., Jorissen M., Debiec-Rychter M., Hermans R., Hauben E. Mammary analogue secretory carcinoma of the sinus ethmoidalis. Histopathology. 2015;67:749–751. doi: 10.1111/his.12702. [DOI] [PubMed] [Google Scholar]
- 6.Sethi R., Kozin E., Remenschneider A., Meier J., VanderLaan P., Faquin W., Deschler D., Frankenthaler R. Mammary analogue secretory carcinoma: update on a new diagnosis of salivary gland malignancy. Laryngoscope. 2014;124:188–195. doi: 10.1002/lary.24254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bishop J.A., Yonescu R., Batista D., Eisele D.W., Westra W.H. Most nonparotid “acinic cell carcinomas” represent mammary analog secretory carcinomas. Am. J. Surg. Pathol. 2013;37:1053–1057. doi: 10.1097/PAS.0b013e3182841554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zardawi I.M., Hook P. Mammary analogue secretory carcinoma of minor salivary glands. Pathology. 2014;46:667–669. doi: 10.1097/PAT.0000000000000179. [DOI] [PubMed] [Google Scholar]
- 9.Bishop J.A. Unmasking MASC: bringing to light the unique morphologic, immunohistochemical and genetic features of the newly recognized mammary analogue secretory carcinoma of salivary glands. Head Neck Pathol. 2013;7:35–39. doi: 10.1007/s12105-013-0429-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mariano F.V., dos Santos H.T., Azañero W.D., da Cunha I.W., Coutinho-Camilo C.M., de Almeida O.P., Kowalski L.P., Altemani A. Mammary analogue secretory carcinoma of salivary glands is a lipid-rich tumour, and adipophilin can be valuable in its identification. Histopathology. 2013 doi: 10.1111/his.12192. n/a–n/a. [DOI] [PubMed] [Google Scholar]
- 11.Xu B., Aryeequaye R., Wang L., Katabi N. Sinonasal secretory carcinoma of salivary gland with high grade transformation: a case report of this under-recognized diagnostic entity with prognostic and therapeutic implications. Head Neck Pathol. 2018;12:274–278. doi: 10.1007/s12105-017-0855-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stevens T.M., Parekh V. Mammary analogue secretory carcinoma. Arch. Pathol. Lab. Med. 2016;140:997–1001. doi: 10.5858/arpa.2015-0075-RS. [DOI] [PubMed] [Google Scholar]
- 13.Sun L., Thorson T., Zhu R., Huo J., Tong J., Rodgers W.H., Shemen L. A case report of parotid mammary analogue secretory carcinoma and reviews. Int. J. Surg. Case Rep. 2019;55:88–91. doi: 10.1016/j.ijscr.2019.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jung M.J., Song J.S., Kim S.Y., Nam S.Y., Roh J.L., Choi S.H., Kim S.B., Cho K.J. Finding and characterizing mammary analogue secretory carcinoma of the salivary gland. Korean J. Pathol. 2013;47:36–43. doi: 10.4132/KoreanJPathol.2013.47.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]