Abstract
Aims:
To analyze the association between colchicine prescription and COVID-19-related hospital admissions in patients with rheumatic and musculoskeletal diseases (RMDs).
Methods:
Patients attending a rheumatology outpatient clinic from a tertiary care center in Madrid, Spain, from 1 September 2019 to 29 February 2020 were included. Patients were assigned as exposed or unexposed based on whether they were prescribed with colchicine in their last visit to the clinic during the 6 months before the start of the observation period. Treatment changes during the observation period were also considered. The primary outcome was COVID-19-related hospital admissions between 1 March and 20 May 2020. Secondary outcome included COVID-19-related mortality. Several weighting techniques for data balancing, based and non-based on the propensity score, followed by Cox regressions were performed to estimate the association of colchicine prescription on both outcomes.
Discussion:
The number of patients entered in the study was 9379, with 406 and 9002 exposed and unexposed follow-up periods, respectively. Generalized Boosted Models (GBMs) and Empirical Balancing Calibration Weighting (EBCW) methods showed the best balance for COVID-19-related hospital admissions. Colchicine prescription did not show a statistically significant association after covariable balancing (p-value = 0.195 and 0.059 for GBM and EBCW, respectively). Regarding mortality, the low number of events prevented a success variable balancing and analysis.
Conclusion:
Colchicine prescription does not play a significant protective or risk role in RMD patients regarding COVID-19-related hospital admissions. Our observations could support the maintenance of colchicine prescription in those patients already being treated, as it is not associated with a worse prognosis.
Plain language title:
Colchicine influence in COVID-19-related hospital admissions
Keywords: colchicine, COVID-19, hospital admission, survival analysis, weighting techniques
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes a myriad of clinical signs and symptoms, together with typical laboratory abnormalities that manifest as the disease COVID-19.1 The severity of COVID-19 symptoms can range from very mild to severe, with a variable disease progression among patients. Although the progression is usually characterized by symptoms such as fever, fatigue, dry cough or loss of taste or smell, in severe cases the course of the disease can be fatal, with pneumonia, ischemic events, or kidney complications.
RNA viruses, such as SARS-CoV-2, trigger the innate immune system by destroying epithelial barriers, triggering the complement system response, and activating the toll-like receptors. In severe cases, an excessive immune response can lead to high levels of pro-inflammatory cytokines promoting a “cytokine storm” by overstimulating inflammatory-related genes. Pro-inflammatory circulating cytokines and chemokines are increased in SARS-CoV-2.2 One of the immediate effects of this excessive response is the respiratory system’s inflammation inducing respiratory failure.
In order to prevent or modulate this exaggerated inflammatory response, several clinical trials with already approved and well known therapeutic agents3 that inhibit the inflammatory response, such as hydroxicloroquine4 or tocilizumab,5 are being carried out. However, none of these drugs, often used in the management of patients with rheumatic and musculoskeletal diseases (RMDs), seems to achieve the desired results when treating COVID-19.
Colchicine, a drug employed in rheumatology to treat diseases such as gout, Behçet’s disease or other autoinflammatory syndromes, inhibits multiple pro-inflammatory mechanisms, mediating an anti-inflammatory response.6 Colchicine effects have also been broadly discussed in cardiovascular disease prevention.7 Together with its anti-inflammatory properties, colchicine’s extensive clinical experience supports its potential theoretical application to help manage COVID-19. Several clinical trials to assess this drug’s efficacy are under way,8 although no result has been published at the time of this manuscript submission.
The aim of our study was to analyze whether colchicine prescription plays a role in COVID-19 severity (defined as COVID-19-related hospital admission and mortality following admission) when affecting patients with RMDs.
Patients and methods
Study setting and design
The study was carried out at the Hospital Clínico San Carlos (HCSC), a public tertiary care center of Madrid, Spain, with a catchment area of nearly 400,000 subjects. We performed a longitudinal retrospective observational study from 1 March 2020 (when the first COVID-19-related hospital admission was reported at the HCSC) to 20 May 2020.
Patients
Eligible patients were selected from the HCSC-COVID-19 cohort, a cohort of patients with RMDs seen at least once at the HCSC rheumatology outpatient clinic between 1 March 2019 and 1 March 2020.9,10 In addition, patients had to fulfill the following criteria:
1. HCSC rheumatology outpatient clinic attendance at least once during the 6 months before the observation period (i.e. 1 September 2019 to 29 February 2020).
2. Patient’s clinical information regarding hospital admissions and discharge had to be accessible from the Hospital Information System (HIS).
3. The patient had not been admitted, due to COVID-19, before the beginning of the observation period (1 March 2020).
4. For the analysis of COVID-19-related to mortality, the patient had to be admitted at the HCSC due to COVID-19.
HCSC Ethics Review Board approval was obtained as a retrospective study and waiver of informed consent was obtained for the use of de-identified clinical records. Furthermore, the study was conducted in accordance with the Declaration of Helsinki.
Data sources
Demographical and clinical data of relevance were retrieved from a departmental electronic health record (EHR; Penelope), from the HCSC Rheumatology Department. Outcomes data were extracted from the HIS. SARS-CoV-2 polymerase chain reaction (PCR) diagnostic assays results were obtained from the HCSC Microbiology Service.
Outcomes
The primary outcome, COVID-19-related hospital admission, was defined as an admission to the HCSC during the observation period due to COVID-19 compatible symptoms, and a positive SARS-CoV2 PCR test, regardless of the duration of the admission or the department where the patient was admitted.
The secondary outcome, COVID-19-related mortality, was defined as the decease of a subject previously admitted to the HCSC due to COVID-19 compatible symptoms and a positive SARS-CoV2 PCR test. Decease had to occur during admission or in the 30 days after discharge. All deceases in these patients were considered related to COVID-19.
Covariables
The main covariable was “colchicine prescription”: a patient was considered as having received a colchicine prescription if in the most recent visit registered in the EHR of the 6 months before the observation period, or during any visit of the observation period, they had:
Received by their attending rheumatologist a Spanish Drug and Medical Products Agency code for colchicine (703194 and 733204), and/or
Received a prescription with colchicine as a concomitant treatment, meaning that it had been prescribed by another physician (such as primary care physician).
A further description of the identification of patients under colchicine therapy can be found in the Supplemental material file “Colchicine exposure assessment” online.
These patients were allocated to the “Exposed group”. Those that did not fulfill these criteria were allocated to the “Unexposed group”. Treatment changes during the observation period were considered. Therefore, these patients were analyzed considering two (or more) distinct follow-up periods, as exposed and as unexposed.
Demographic and clinical-related variables collected during the patient’s visits using our EHR were also included. For both outcomes, covariable data were taken from the most recent visit before the beginning of the time at risk for each outcome: for the primary outcome, covariable data were taken from the patient’s last visit of the 6 months before the observation period and from the visits during the observation period when colchicine treatment was modified. For the secondary outcome, covariable data were taken from the last patient’s visit before the COVID-19-related hospital admission (regardless of whether it took place in the last 6 months before the observation period or during the observation period).
The covariables considered are described in the Supplemental file “Covariables”.
Statistical analysis
Continuous variables were summarized using median and interquartile range (IQR) and categorical variables using proportions.
COVID-19-related admissions and mortality crude incident rates and 95% confidence intervals (CI) were presented as the number of events per 100 patient-years and were estimated by dividing the number of events that occurred during follow-up by the number of person-years of exposure.
For COVID-19-related admissions, the total follow-up time comprised the elapsed time from 1 March 2020 until 20 May 2020. Patients contributed risk time until any of the following censoring points: (a) a change in the colchicine treatment, including the prescription of colchicine in a patient not treated with this drug, regardless of the cause, or colchicine discontinuation, also regardless of the cause; or (b) hospital admission at the HCSC. This means that for those who were admitted, the follow-up time would be defined as the elapsed time between the beginning of the study (1 March 2020) and the hospital admission. For those who were not admitted, the follow-up time would be defined as the elapsed time between the beginning of the study and the end of the study (20 May 2020). Those changing treatment had the same follow-up and they contributed to the group of exposed or unexposed depending on whether they were prescribed or not with colchicine.
For COVID-19-related mortality, the total follow-up time comprised the elapsed time from the beginning of COVID-19-related hospital admission (which took place between 1 March 2020 and 20 May 2020) until the end of the study (20 June 2020). Patients contributed risk time until any of the following censoring points: (a) death; or (b) 30 days after discharge.
Kaplan–Meier cumulative incidence curves were estimated to account for COVID-19-related admissions and mortality.
Cox regression models were fitted to estimate the influence of colchicine prescription in the hazard of COVID-19-related admissions and mortality. We considered the influence of other covariables: those with a prevalence ⩾5% in the “exposed group” and a percentage difference between both groups ⩾30%; those covariables already associated with prognosis and/or mortality risk [such as hypertension, diabetes, cancer, dyslipidemia, cardiovascular, lung (interstitial lung disease/chronic obstructive lung disease) or thyroid diseases], regardless of their prevalence or percentage difference; and those covariables related to the use of disease-modifying antirheumatic drugs. For diagnoses and treatments covariables with a prevalence <5%, we combined those that were related to similar pathologies or treatments, in order to achieve this criterion. Supplemental Excel file “Initial variables” summarizes all of the initially considered variables and the merging process into groups. Details on the methods used to balance the distribution of variables can be found in the Supplemental file “Statistical analyses”.
Finally, Cox regression models including the variable “Colchicine prescription” were calculated and adjusted by the variables that remained unbalanced. We limited the number of variables in the multivariable model following the rule of 10 events per variable.11–13 Our null hypothesis was that there was not association, in our cohort, between colchicine prescription and our primary endpoints. Results from the Cox models were expressed as hazard ratios (HRs) with 95% CIs. In order to verify if the proportional hazards assumption held for our variable of interest, the Schoenfeld residuals and the scaled Schoenfeld residuals were used.
Statistical analyses were performed with R version 4.0.2 and WeightIt14 and Cobalt15 R packages.
Results
Cohort description
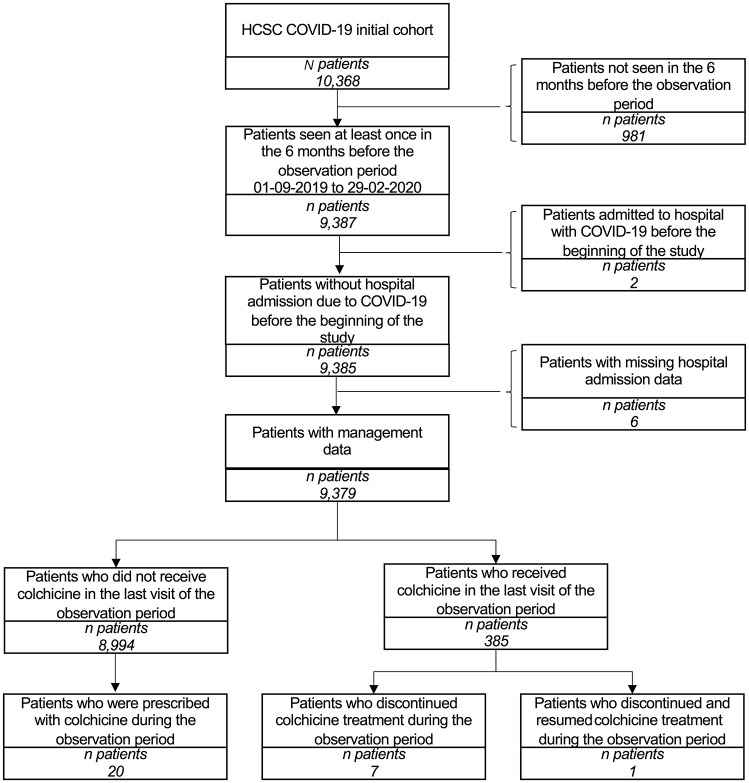
Figure 1 shows the inclusion criteria and patient flow. By 1 March 2020, 9379 patients (385 exposed and 8994 unexposed) were identified. During the observation period, 28 patients underwent a medication change (20 were prescribed with colchicine, seven discontinued the treatment, and one suspended and then resumed the medication). We considered that these patients had two/three follow-up periods, as exposed and as unexposed. None of the patients were readmitted to the HCSC during the following-up period.
Figure 1.
Flow chart of included patients.
HCSC, Hospital Clínico San Carlos.
For the primary outcome COVID-19-related hospital admissions, 9408 treatment periods were analyzed.
The median (IQR) number of days that exposed patients were under colchicine prescription by 1 March 2020 was 413 (7–1379) days. Discontinuations in the treatment of less than 3 months, taking place before the observation period, were disregarded. More than half of the patients had been taking colchicine for more than a year (204, 53%); one-quarter had been recently prescribed (⩽7 days; 99, 26%); the other quarter had been using colchicine for less than a year (82, 21%).
Demographic and clinical-related variables at the last rheumatology outpatient visit in the 6 months before the observation period or at the visit during the observation period when colchicine treatment was modified can be found in Table 1.
Table 1.
Clinical characteristics before the observation period and when colchicine prescription was modified.
| Variable | Unexposed n = 9002 |
Exposed n = 406 |
Total N = 9408 |
Percentage difference |
|---|---|---|---|---|
| Women, n (%) | 6535 (72.59) | 203 (50) | 6738 (71.62) | |
| Age, median (IQR) | 60.84 (49.58, 74.36) | 67.83 (55.88, 78.64) | 61.16 (49.71,74.73) | |
| Diagnoses, n (%) | ||||
| Other inflammatory diseases | 2335 (25.94) | 64 (15.76) | 2399 | 64.59 |
| Rheumatoid arthritis | 1408 (15.64) | 36 (8.87) | 1444 | 76.32 |
| Knee osteoarthritis | 619 (6.88) | 55 (13.55) | 674 | 49.23 |
| Hand osteoarthritis | 450 (5) | 80 (20.69) | 534 | 75.83 |
| Monoarthritis | 95 (1.06) | 24 (5.91) | 119 | 82.06 |
| Behçet’s disease | 19 (0.21) | 23 (5.67) | 42 | 96.3 |
| Gout | 200 (2.22) | 195 (48.03) | 395 | 95.38 |
| Treatment, n (%) | ||||
| Analgesic | 1900 (21.11) | 57 (14.04) | 1957 | 50.36 |
| NSAIDs | 1303 (14.47) | 34 (8.37) | 1337 | 72.88 |
| DMARDs | 1047 (11.63) | 34 (8.37) | 1081 | 38.95 |
| Corticosteroid oral | 862 (9.58) | 78 (19.21) | 940 | 50.13 |
| Comorbidities, n (%) | ||||
| Hypertension | 2138 (23.75) | 130 (32.02) | 2268 | 25.83 |
| Dyslipidemia | 1840 (20.44) | 93 (22.91) | 1933 | 10.78 |
| Thyroid disease | 862 (9.58) | 35 (8.62) | 896 | 10.9 |
| Diabetes mellitus | 714 (7.93) | 35 (8.62) | 749 | 8 |
| Cancer | 664 (7.38) | 36 (8.87) | 700 | 16.8 |
| Vascular disease | 527 (5.85) | 47 (11.58) | 574 | 49.48 |
| Lung disease – ILD/COPD | 459 (5.1) | 28 (6.9) | 487 | 26.09 |
| Cardiovascular disease | 401 (4.45) | 31 (7.64) | 432 | 41.75 |
| Rosser index, median (IQR)* | 0.99 (0.97, 0.99) | 0.99 (0.97, 0.99) | 0.99 (0.97, 0.99) | |
| Days from visit until the start of the study, median (IQR) | 73.00 (30.00, 115.00) | 66.00 (25.25, 104.00) | 73.00 (27.00, 115.00) | |
Rosser index was not used for data balancing.
COPD, chronic obstructive pulmonary disease; DMARD, disease-modifying anti-rheumatic drug; ILD, interstitial lung disease; IQR, interquartile range; NSAID, non-steroidal anti-inflammatory drug.
We identified 132 COVID-19-related hospital admissions (at the HCSC): 12 (2.96%) in patients from the exposed group and 120 (1.34%) in patients from the unexposed group. The median (IQR) time to event (TTE) for COVID-19-related hospital admission (time elapsed from 1 March until outcome or censoring) was 28.5 (20–38) days; 28.5 (20–38) days in the unexposed and 28 (19.5–36.5) days in the exposed groups. The median (IQR) length-of-stay of admitted patients was 9 (5–16) days; 8.5 (5–15.25) and 15 (7.75–20.25) days in the unexposed and exposed groups, respectively.
Demographic and clinical-related variables at the last visit before COVID-19-related hospital admission can be found in Table 2.
Table 2.
Clinical characteristics at the most recent before a COVID-19-related admission at the Hospital Clínico San Carlos.
| Variable | Unexposed n = 120 |
Exposed n = 12 |
Total N = 132 |
Percentage difference |
|---|---|---|---|---|
| Women, n (%) | 79 (65.83) | 5 (41.67) | 84 (63.64) | |
| Age, median (IQR) | 72.34 (57.72, 82.66) | 74.19 (67.22, 84.47) | 72.34 (59.10, 83.17) | |
| Diagnoses, n (%) | ||||
| Rheumatoid arthritis | 22 (18.33) | 1 (8.33) | 23 | 120.05 |
| Knee osteoarthritis | 13 (10.83) | 2 (16.67) | 15 | 35.03 |
| Osteoarthritis | 10 (8.33) | 3 (25) | 13 | 66.68 |
| Tendinitis (lower extremities) | 5 (4.17) | 1 (8.33) | 6 | 49.94 |
| Osteoporosis | 5 (4.17) | 1 (8.33) | 6 | 49.94 |
| Monoarthritis | 0 (0) | 3 (25) | 3 | 100 |
| Gout | 4 (3.33) | 8 (66.67) | 12 | 95.01 |
| Treatment, n (%) | ||||
| DMARDs | 13 (10.83) | 1 (8.33) | 14 | 30.01 |
| SYSADOA | 0 (0) | 1 (8.33) | 1 | 100 |
| Comorbidities, n (%) | ||||
| Hypertension | 41 (34.17) | 7 (58.33) | 48 | 41.42 |
| Dyslipidemia | 24 (20) | 4 (33.33) | 28 | 39.99 |
| Lung disease – ILD/COPD | 18 (15) | 2 (16.67) | 20 | 10.02 |
| Diabetes mellitus | 19 (15.83) | 1 (8.33) | 20 | 90.04 |
| Vascular disease | 11 (9.17) | 5 (41.67) | 16 | 77.99 |
| Cancer | 14 (11.67) | 0 (0) | 14 | – |
| Thyroid disease | 8 (6.67) | 1 (8.33) | 9 | 19.93 |
| Cardiovascular disease | 7 (5.83) | 1 (8.33) | 8 | 30.01 |
| Obesity | 7 (5.83) | 1 (8.33) | 8 | 30.01 |
| Gastroesophageal reflux disease | 4 (3.33) | 2 (16.67) | 6 | 80.02 |
| Rosser index, median (IQR)* | 0.99 (0.96, 0.99) | 0.99 (0.94, 0.99) | 0.99 (0.96, 0.99) | |
| Days from inclusion visit until the start of the study, median (IQR) | 73.50 (35.50, 120.25) | 87.00 (47.00, 114.75) | 73.50 (36.75, 120.25) | |
Rosser index was not used for data balancing.
COPD, chronic obstructive pulmonary disease; DMARD, disease-modifying antirheumatic drug; ILD, interstitial lung disease; IQR, interquartile range; NSAID, non-steroidal anti-inflammatory drug; SYSADOA, symptomatic slow action drugs for osteoarthritis.
Regarding COVID-19-related deaths, 34 were identified; four (0.99%) and 30 (0.33%) in the exposed and unexposed groups, respectively. The median (IQR) TTE for COVID-19-related mortality following hospital admission (time elapsed from admission until outcome or censoring) was 6 (2–9.75) days; 6 (2.25–9.75) days in the unexposed group and 4.5 (0.75–10.5) days in the exposed group. There was only one patient with a COVID-19-related decease 19 days after discharge.
Influence of colchicine prescription in COVID-19-related hospital admissions
Supplemental Tables S1 and S2 show the mean differences for the selected covariables, unadjusted and balanced (adjusted, trimmed, and stabilized) using different methods based and not based on the Propensity Score (PS), respectively. For the methods based on the PS, Generalized Boosted Models (GBMs) showed the lowest number of unbalanced variables (n = 3). In addition, we selected the stabilized weights as they showed the lowest coefficient of variation 0.296. Regarding non-PS methods, the three tested were able to balance all variables. We selected the Empirical Balancing Calibration Weighting, as it showed the lowest maximum mean difference compared with the other two methods. In addition, we selected the stabilized weighting as it showed the lowest coefficient of variation 5.706.
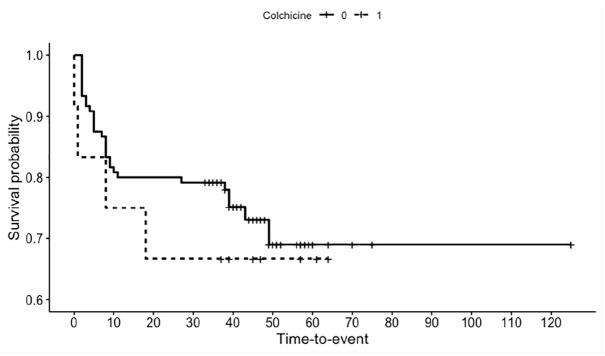
In the unbalanced analysis, colchicine prescription was associated with a statistically significant higher hazard of COVID-19-related hospital admission [HR (95% CI) = 2.237 (1.236–4.049), p-value = 0.008]. Kaplan–Meier curves for COVID-19-related hospital admission can be found in Figure 2.
Figure 2.
Kaplan–Meier cumulative incidence curves representing COVID-19-related hospital admissions.
Table 3 shows the association of colchicine prescription and COVID-19 after balancing using PS and non-PS based methods with stabilized weights. Proportional hazard assumption test results are shown through the Schoenfeld residuals p-values. As can be seen, all models fulfilled the proportional hazard assumption (p-value > 0.05).
Table 3.
Cox models analyzing the association of colchicine prescription in COVID-19-related hospital admissions after covariates balancing.
| Adj. | Trim. | Stab. | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Method | HR | 95% CI | p-value | p-value* | HR | CI | p-value | p-value* | HR | CI | p-value | p-value* |
| GLMs | 3.32 | 1.10–10.04 | 0.033 | 0.869 | 2.59 | 0.95–7.08 | 0.064 | 0.868 | 2.67 | 0.94–7.55 | 0.064 | 0.84 |
| GBMs | 2.77 | 0.76–10.159 | 0.124 | 0.854 | 2.15 | 0.89–5.22 | 0.090 | 0.834 | 2.37 | 0.64–8.73 | 0.195 | 0.82 |
| CBPS | 3.27 | 1.08–9.87 | 0.035 | 0.867 | 2.50 | 0.86–7.26 | 0.093 | 0.858 | 2.61 | 0.96–7.11 | 0.061 | 0.838 |
| NPCBPS | 1.98 | 0.68–5.75 | 0.212 | 0.826 | 2.71 | 1.06–6.91 | 0.037 | 0.848 | 1.97 | 0.67–5.76 | 0.217 | 0.825 |
| MLPS | 1.96 | 0.81–4.78 | 0.137 | 0.828 | 1.98 | 0.84–4.67 | 0.117 | 0.827 | 1.95 | 0.88–4.29 | 0.099 | 0.818 |
| EBAL | 3.11 | 0.96–10.12 | 0.059 | 0.844 | 2.56 | 0.97–6.72 | 0.057 | 0.842 | 3.10 | 0.96–10.04 | 0.059 | 0.843 |
| EBCW | 3.11 | 0.96–10.12 | 0.059 | 0.844 | 2.56 | 0.97–6.72 | 0.057 | 0.842 | 3.10 | 0.96–10.04 | 0.059 | 0.843 |
| OBW | 3.30 | 1.06–10.25 | 0.039 | 0.848 | 2.68 | 0.96–7.46 | 0.06 | 0.832 | 3.29 | 1.06–10.22 | 0.039 | 0.848 |
Schoenfeld test p value.
Adj., adjusted; CBPS, covariate balancing method; CI, confidence interval; EBAL, entropy balancing; EBCW, Empirical Balancing Calibration Weighting; GBM, Generalized Boosted Model; GLM, generalized linear model; HR: hazard ration; MLPS, machine learning propensity score based methods; NPCBPS, non-parametric covariate balancing method; OBW, optimization-based weighting; Stab., stabilized; Trim., trimmed.
In the selected balancing methods, we observed that colchicine prescription was still associated with a higher HR although statistical significance was lost. Supplemental Table S3 shows the complete models, including the unbalanced covariables.
Influence of colchicine prescription in COVID-19-related mortality
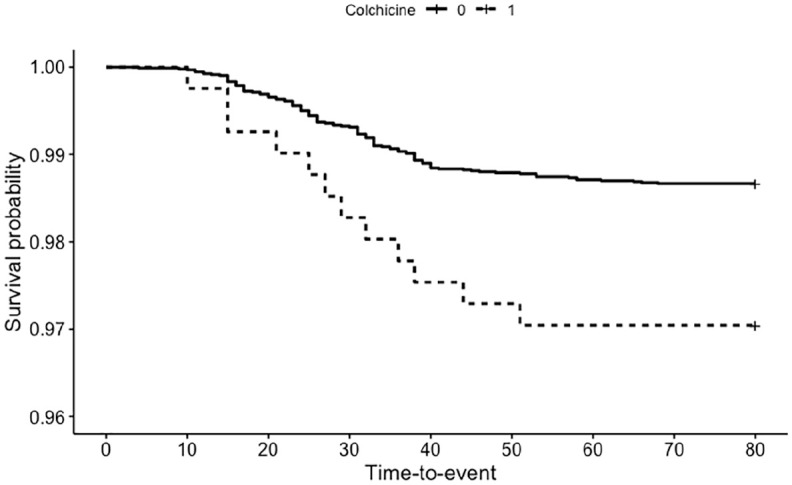
In the unbalanced analysis, colchicine prescription was not associated with a statistically significant higher hazard of COVID-19-related decease [HR (95% CI) = 1.371 (0.482–3.899), p-value = 0.554]. Kaplan–Meier curves for COVID-19-related death can be found in Figure 3.
Figure 3.
Kaplan–Meier cumulative incidence curves representing COVID-19-related mortality following hospital admission.
Supplemental Table S4 shows the mean differences for the selected covariables, unadjusted and balanced (adjusted, trimmed, and stabilized) using different methods based on PS. Singularity and convergence issues appeared when testing non-PS based methods, likely due to the low number of events (n = 34 deaths). After balancing, the number of unbalanced variables was much higher, compared with the primary outcome analysis. The method able to balance the highest number of variables was the trimmed GBM, leaving 13 covariables unbalanced. The overall number of events and the number of covariables that would have to be included in the multivariate analysis11–13 prevented us from carrying out a proper analysis of the secondary outcome.
Discussion
Our study aimed to assess the role that colchicine could play in a cohort of RMD patients in terms of COVID-19-related hospital admission and mortality. In this setting, colchicine prescription was not associated with a statistically significant higher hazard of admission after covariable balancing. Regarding COVID-19-related mortality, the number of unbalanced covariables remained too high with regard to the number of events, and, therefore, the colchicine effect was not analyzed for this outcome.
Colchicine is one of the several drugs that are being currently tested for efficacy in COVID-1916,17 due to its anti-inflammatory effects: colchicine is able to inhibit the microtubule polymerization, interfering with inflammatory pathways related to the innate immune system, such as neutrophil recruitment and adhesion, superoxide production, and inflammasome, rho-associated protein kinase or NF-κB protein complex activation.6 Several observational or uncontrolled studies have shown a beneficial effect of colchicine when used with the intention to treat COVID-19. Sandhu et al.18 showed a lower mortality, a lower rate of intubations, and a higher number of discharges among hospitalized patients who received colchicine (n = 53) compared with standard of care (n = 144). In addition, Scarsi et al.19 also observed a better survival rate in 122 patients admitted with severe COVID-19 (pneumonia and acute respiratory distress syndrome) and treated with colchicine, compared with 140 patients treated with standard of care. Brunetti et al.20 performed a propensity score matched comparison of admitted patients receiving colchicine (n = 33) versus standard care (n = 33). Those receiving colchicine showed a lower 28-days all-cause mortality compared with those not receiving this medication. Although in the three studies the allocation of colchicine was not random, both the intervention and control groups were comparable. Colchicine has also been used in a community setting: Della-Torre et al.21 reported a favorable outcome in an uncontrolled case series of nine domiciliary consecutive COVID-19 patients treated with this drug. In addition, data from two randomized controlled trials has been released: Lopes et al.22 presented an interim analysis of a single-center randomized, double-blinded, placebo-controlled clinical trial including 35 patients (18 placebo and 17 colchicine). Subjects in the colchicine group showed a shorter time of need for supplemental oxygen, shorter hospitalization time, and a higher discharge rate. Finally, the results from the COLCORONA study have been released,17 apparently showing a significant reduction in mortality.
Comparing these results with those in our study, we did not observe a significant difference in the crude mortality rate among those exposed and unexposed to colchicine. This finding could be related to the fact that we were not able to properly balance the baseline characteristics of those exposed and unexposed to colchicine for this outcome, and, therefore, the propensity score analysis could not be carried out. On the other hand, we did not use colchicine as a specific treatment for COVID-19, and therefore it may have been discontinued after admission. Unfortunately, we do not have data regarding who continued treatment or who did not. We want to point out that the use of this drug was not included in the COVID-19 treatment protocols used at our center, and therefore its prescription during admission was not promoted. Finally, it is possible that colchicine’s positive effect is related to the use of higher dosages, similar to those used to treat gout flares (⩾1 mg/day). In our case, most patients were receiving a lower dosage (0.5–0.6 mg/day) when outpatients, and among those who were admitted and continued their treatment, it is very likely that colchicine was not prescribed at higher dosages, and patients just continued with their previous dosages.
Other studies have shown that the chronic use of colchicine was not associated with a higher risk of severe COVID-19: in a cohort of patients with familial Mediterranean fever,23 a similar proportion of severe SARS-CoV-2 infection compared with the general population was reported. Furthermore, a group of five patients with iatrogenic allogenosis24 seemed to present with a milder COVID-19 course compared with their close contacts who also developed the disease. In our study, analyzing the association between colchicine and COVID-19 in terms of chronic exposure (at least for most of the patients that had been receiving this medication by 1 March 2020), we observed similar results, in the sense that colchicine use was not associated with a significantly different COVID-19 prognosis (in our case defined as COVD19-related admission) compared with those patients not receiving this drug. As previously mentioned for COVID-19-related mortality, we could hypothesize that the dosage used by those patients taking colchicine was not high enough to improve COVID-19 prognosis.
Although the published American College of Rheumatology guidelines25 do not mention nor provide colchicine-related recommendations, based on our results and previous evidence we suggest not discontinuing colchicine therapy in patients who were prescribed with this drug, as the previous use of colchicine does not seem to constitute a risk factor for severe COVID-19. This recommendation may be of particular relevance for patients with vascular disease, since COVID-19 affectation and severity in this group of patients has been demonstrated and discussed since the beginning of the pandemic.26–28 The unjustified colchicine discontinuation could negatively affect the patient’s health and render them prone to potential rheumatic flares or ischemic complications. Regarding the former, we have to take into account the possible ramifications of a flare in a quiescent or controlled disease considering the current situation due to the pandemic. Not only were our healthcare systems almost at full capacity (emergency departments and hospitalizations) and with reduced or even at times suspended outpatient care, but also citizens were subjected to sometimes stringent limitations of movement (including home confinement).29 As an example, if we consider autoinflammatory syndromes, flares can be associated with very severe and life-threatening manifestations. In addition, typically they are associated with fever, one of the more common symptoms of COVID-19. In other diseases, such as gout, an otherwise mild flare could be associated with severe limitations, as patients are unable to access healthcare and/or family caregivers are not able to provide support.
Our study has a series of limitations, the main one being its retrospective nature. Treatment allocation was not carried out at random, and although we carried out different methods to increase the comparability of both groups, prescription bias cannot be completely compensated. However, we observed similar results regardless of the method used to balance the covariables between patients prescribed or not with colchicine, which increases our confidence regarding the validity of our results. On the other hand, the weighting strategies employed do not prevent bias from unmeasured confounders. Some studies have highlighted different ways to reduce this bias in observational studies, such as doing sensitivity analyses with external validation data.30,31 Although the considered variables in our study were only those accessible in our outpatient EHR, and we did not carry out an external validation, our results were in line with previously published observations in populations chronically exposed to colchicine.
Another limitation is that the outcome data were extracted from a single center. On the one hand, there is the issue of the generalizability of the results, being obtained from a homogeneous group of patients with RMDs from a tertiary care center. It is important to consider that the effect of colchicine may be different in patients with other diseases that are also chronically exposed to this drug. On the other hand, patients may have been admitted to other hospitals due to COVID-19, or they may have died of COVID-19 also in other centers or before attending the HCSC. Because we do not have access to those data, we may have wrongfully classified patients as not having developed the outcomes. This may also have introduced a selection bias in our study, as we cannot assess whether the characteristic of those admitted to the HCSC and those that may have been admitted to other centers were similar or not. Furthermore, due to the same reasons, readmissions of the studied population in other hospitals during the follow-up period could not be assessed.
Another limitation of our study is that patient adherence to colchicine treatment was not assessed. We were able to analyze prescription, but not use, and we assumed that those prescribed with colchicine were taking the medication. Furthermore, we have prescription data at the time of the visits from the EHR. Colchicine treatment may have been discontinued or initiated, but not registered at the EHR.
Nevertheless, our study also presents several strengths: we have included patients with a board spectrum of RMDs, reflecting the clinical practice from our health area. In addition, more than 400 episodes of colchicine treatment were analyzed, and several weighting techniques applied, with consistent results.
Conclusion
Our results suggest that colchicine does not play a significant protective either a risk role in COVID-19 severity, in a population of RMD patients. Whereas in the unbalanced analysis colchicine prescription was associated with a statistically significant higher hazard of COVID-19-related hospital admission, in the balanced analyses, the statistical significance was lost. Therefore, we conclude that there is no significant association between colchicine exposure and COVID-19 severity.
These results should be interpreted as an initial approach to the possible role that colchicine could play in a COVID-19 exposed population. In light of our observations, colchicine treatment seems safe in these circumstances, and it likely should be continued in RMD patients.
Supplemental Material
Supplemental material, sj-docx-1-tab-10.1177_1759720X211002684 for Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis by Alfredo Madrid-García, Inés Pérez, José Ignacio Colomer, Leticia León-Mateos, Juan A Jover, Benjamín Fernández-Gutiérrez, Lydia Abásolo-Alcazar and Luis Rodríguez-Rodríguez in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-docx-2-tab-10.1177_1759720X211002684 for Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis by Alfredo Madrid-García, Inés Pérez, José Ignacio Colomer, Leticia León-Mateos, Juan A Jover, Benjamín Fernández-Gutiérrez, Lydia Abásolo-Alcazar and Luis Rodríguez-Rodríguez in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-docx-3-tab-10.1177_1759720X211002684 for Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis by Alfredo Madrid-García, Inés Pérez, José Ignacio Colomer, Leticia León-Mateos, Juan A Jover, Benjamín Fernández-Gutiérrez, Lydia Abásolo-Alcazar and Luis Rodríguez-Rodríguez in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-docx-4-tab-10.1177_1759720X211002684 for Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis by Alfredo Madrid-García, Inés Pérez, José Ignacio Colomer, Leticia León-Mateos, Juan A Jover, Benjamín Fernández-Gutiérrez, Lydia Abásolo-Alcazar and Luis Rodríguez-Rodríguez in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-docx-5-tab-10.1177_1759720X211002684 for Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis by Alfredo Madrid-García, Inés Pérez, José Ignacio Colomer, Leticia León-Mateos, Juan A Jover, Benjamín Fernández-Gutiérrez, Lydia Abásolo-Alcazar and Luis Rodríguez-Rodríguez in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-xlsx-6-tab-10.1177_1759720X211002684 for Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis by Alfredo Madrid-García, Inés Pérez, José Ignacio Colomer, Leticia León-Mateos, Juan A Jover, Benjamín Fernández-Gutiérrez, Lydia Abásolo-Alcazar and Luis Rodríguez-Rodríguez in Therapeutic Advances in Musculoskeletal Disease
Footnotes
Author contributions: LRR and LAA conceived and designed the study. IP, JIC, LLM, JAJ, and BFG collected data. AMG, LAA, and LRR performed the data analysis and interpreted the data. All of the authors were involved in the drafting and/or revising of the manuscript.
Conflict of interest statement: The authors declare that there is no conflict of interest.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Instituto de Salud Carlos III (ISCIII), Ministry of Health, Spain (CPII17/00014; PI18/01188; CP16/00916; and RD16/0012/0014) and cofounded by el Fondo Europeo de Desarrollo Regional (FEDER). Funders had no role in the design, collection, management, analyses, interpretation of the data, preparation, review, approval or decision to submit the manuscript for publication.
Data availability statement: Data are available upon reasonable request.
Ethics statement: The study was approved by the Hospital Clínico San Carlos Ethics Committee (approval number 20/268-E-BS). This study was conducted according to the principles of the Declaration of Helsinki.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
ORCID iDs: Alfredo Madrid-García  https://orcid.org/0000-0002-1591-0467
https://orcid.org/0000-0002-1591-0467
Benjamín Fernández-Gutiérrez  https://orcid.org/0000-0002-6126-8786
https://orcid.org/0000-0002-6126-8786
Luis Rodríguez-Rodríguez  https://orcid.org/0000-0002-2869-7861
https://orcid.org/0000-0002-2869-7861
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Alfredo Madrid-García, Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, Madrid, Spain; Escuela Técnica Superior de Ingenieros de Telecomunicación (ETSIT), Universidad Politécnica de Madrid, Madrid, Spain.
Inés Pérez, Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, Madrid, Spain.
José Ignacio Colomer, Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, Madrid, Spain.
Leticia León-Mateos, Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, Madrid, Spain.
Juan A Jover, Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, Madrid, Spain.
Benjamín Fernández-Gutiérrez, Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, Madrid, Spain.
Lydia Abásolo-Alcazar, Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, Madrid, Spain.
Luis Rodríguez-Rodríguez, Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, c\ Prof. Martin Lagos s/n, Madrid, 28040, Spain.
References
- 1. Fernandez-Gutierrez B. COVID-19 with pulmonary involvement. An autoimmune disease of known cause. Reumatol Clin 2020; 16: 253–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Coperchini F, Chiovato L, Croce L, et al. The cytokine storm in COVID-19: an overview of the involvement of the chemokine/chemokine-receptor system. Cytokine Growth Factor Rev 2020; 53: 25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shaffer L. 15 drugs being tested to treat COVID-19 and how they would work. Nat Med. Epub ahead of print 15 May 2020. DOI: 10.1038/d41591-020-00019-9. [DOI] [PubMed] [Google Scholar]
- 4. Geleris J, Sun Y, Platt J, et al. Observational study of hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med 2020; 382: 2411–2418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Xu X, Han M, Li T, et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci U S A 2020; 117: 10970–10975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Terkeltaub RA. Colchicine update: 2008. Semin Arthritis Rheum 2009; 38: 411–419. [DOI] [PubMed] [Google Scholar]
- 7. Hemkens LG, Ewald H, Gloy VL, et al. Colchicine for prevention of cardiovascular events. Cochrane database Syst Rev 2016; 1: CD011047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. ClinicalTrials.gov. Studies covid19 and colchicine, https://clinicaltrials.gov/ct2/results?cond=Covid19&term=colchicine&cntry=&state=&city=&dist= (accessed 19 October 2020).
- 9. Fernandez-Gutierrez B, Leon L, Madrid A, et al. Hospital admissions in inflammatory rheumatic diseases during the COVID-19 pandemic: incidence and role of disease modifying agents. medRxiv 2020. DOI: 2020.05.21.20108696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Freites Nuñez DD, Leon L, Mucientes A, et al. Risk factors for hospital admissions related to COVID-19 in patients with autoimmune inflammatory rheumatic diseases. Ann Rheum Dis 2020; 79: 1393–1399. [DOI] [PubMed] [Google Scholar]
- 11. Concato J, Peduzzi P, Holford TR, et al. Importance of events per independent variable in proportional hazards analysis. I. Background, goals, and general strategy. J Clin Epidemiol 1995; 48: 1495–501. [DOI] [PubMed] [Google Scholar]
- 12. Peduzzi P, Concato J, Feinstein AR, et al. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J Clin Epidemiol 1995; 48: 1503–1510. [DOI] [PubMed] [Google Scholar]
- 13. Peduzzi P, Concato J, Kemper E, et al. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 1996; 49: 1373–1379. [DOI] [PubMed] [Google Scholar]
- 14. Greifer N. WeightIt: weighting for covariate balance in observational studies, https://cran.r-project.org/package=WeightIt (accessed 24 October 2020).
- 15. Greifer N. cobalt: covariate balance tables and plots, https://cran.r-project.org/package=cobalt (accessed 24 October 2020).
- 16. Varshney AS, Wang DE, Bhatt AS, et al. Characteristics of clinical trials evaluating cardiovascular therapies for coronavirus disease 2019 registered on ClinicalTrials.gov: a cross sectional analysis. Am Heart J. Epub ahead of print 26 October 2020. DOI: 10.1016/j.ahj.2020.10.065. [DOI] [PMC free article] [PubMed]
- 17. Colchicine Coronavirus SARS-CoV2 Trial (COLCORONA) (COVID-19), https://clinicaltrials.gov/ct2/show/NCT04322682 (accessed 25 January 2021).
- 18. Sandhu T, Tieng A, Chilimuri S, et al. A case control study to evaluate the impact of colchicine on patients admitted to the hospital with moderate to severe COVID-19 infection. Can J Infect Dis Med Microbiol 2020; 2020: 8865954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Scarsi M, Piantoni S, Colombo E, et al. Association between treatment with colchicine and improved survival in a single-centre cohort of adult hospitalised patients with COVID-19 pneumonia and acute respiratory distress syndrome. Ann Rheum Dis 2020; 79: 1286–1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Brunetti L, Diawara O, Tsai A, et al. Colchicine to weather the cytokine storm in hospitalized patients with COVID-19. J Clin Med. Epub ahead of print 14 September 2020. DOI: 10.3390/jcm9092961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Della-Torre E, Della-Torre F, Kusanovic M, et al. Treating COVID-19 with colchicine in community healthcare setting. Clin Immunol 2020; 217: 108490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lopes MIF, Bonjorno LP, Giannini MC, et al. Beneficial effects of colchicine for moderate to severe COVID-19: an interim analysis of a randomized, double-blinded, placebo controlled clinical trial. medRxiv 2020. DOI: 2020.08.06.20169573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bourguiba R, Delplanque M, Vinit C, et al. Clinical course of COVID-19 in a cohort of 342 familial Mediterranean fever patients with a long-term treatment by colchicine in a French endemic area. Ann Rheum Dis. Epub ahead of print 2 November 2020. DOI: 10.1136/annrheumdis-2020-218707. [DOI] [PubMed] [Google Scholar]
- 24. Montealegre-Gómez G, Garavito E, Gómez-López A, et al. [Colchicine: a potential therapeutic tool against COVID-19. Experience of 5 patients]. Reumatol Clin. Epub ahead of print 16 May 2020. DOI: 10.1016/j.reuma.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mikuls TR, Johnson SR, Fraenkel L, et al. American College of Rheumatology guidance for the management of rheumatic disease in adult patients during the COVID-19 pandemic: Version 2. Arthritis Rheumatol. Epub ahead of print 30 July 2020. DOI: 10.1002/art.41437. [DOI] [PubMed] [Google Scholar]
- 26. Zheng YY, Ma YT, Zhang JY, et al. COVID-19 and the cardiovascular system. Nat Rev Cardiol 2020; 17: 259–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Clerkin KJ, Fried JA, Raikhelkar J, et al. COVID-19 and cardiovascular disease. Circulation 2020; 141: 1648–1655. [DOI] [PubMed] [Google Scholar]
- 28. López-Otero D, López-Pais J, Antúnez-Muiños PJ, et al. Asociación entre el daño miocárdico y el pronóstico de pacientes hospitalizados por COVID-19 con y sin cardiopatía. Registro CARDIOVID. Rev Española Cardiol. Epub ahead of print 16 September 2020. DOI: 10.1016/j.recesp.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. López-Medina C, Ladehesa-Pineda L, Gómez-García I, et al. Treatment adherence during the COVID-19 pandemic and the impact of confinement on disease activity and emotional status: a survey in 644 rheumatic patients. Joint Bone Spine 2020; 88: 105085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Stürmer T, Schneeweiss S, Avorn J, et al. Adjusting effect estimates for unmeasured confounding with validation data using propensity score calibration. Am J Epidemiol 2005; 162: 279–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Schneeweiss S. Sensitivity analysis and external adjustment for unmeasured confounders in epidemiologic database studies of therapeutics. Pharmacoepidemiol Drug Saf 2006; 15: 291–303. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-tab-10.1177_1759720X211002684 for Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis by Alfredo Madrid-García, Inés Pérez, José Ignacio Colomer, Leticia León-Mateos, Juan A Jover, Benjamín Fernández-Gutiérrez, Lydia Abásolo-Alcazar and Luis Rodríguez-Rodríguez in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-docx-2-tab-10.1177_1759720X211002684 for Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis by Alfredo Madrid-García, Inés Pérez, José Ignacio Colomer, Leticia León-Mateos, Juan A Jover, Benjamín Fernández-Gutiérrez, Lydia Abásolo-Alcazar and Luis Rodríguez-Rodríguez in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-docx-3-tab-10.1177_1759720X211002684 for Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis by Alfredo Madrid-García, Inés Pérez, José Ignacio Colomer, Leticia León-Mateos, Juan A Jover, Benjamín Fernández-Gutiérrez, Lydia Abásolo-Alcazar and Luis Rodríguez-Rodríguez in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-docx-4-tab-10.1177_1759720X211002684 for Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis by Alfredo Madrid-García, Inés Pérez, José Ignacio Colomer, Leticia León-Mateos, Juan A Jover, Benjamín Fernández-Gutiérrez, Lydia Abásolo-Alcazar and Luis Rodríguez-Rodríguez in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-docx-5-tab-10.1177_1759720X211002684 for Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis by Alfredo Madrid-García, Inés Pérez, José Ignacio Colomer, Leticia León-Mateos, Juan A Jover, Benjamín Fernández-Gutiérrez, Lydia Abásolo-Alcazar and Luis Rodríguez-Rodríguez in Therapeutic Advances in Musculoskeletal Disease
Supplemental material, sj-xlsx-6-tab-10.1177_1759720X211002684 for Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis by Alfredo Madrid-García, Inés Pérez, José Ignacio Colomer, Leticia León-Mateos, Juan A Jover, Benjamín Fernández-Gutiérrez, Lydia Abásolo-Alcazar and Luis Rodríguez-Rodríguez in Therapeutic Advances in Musculoskeletal Disease