Abstract
Objectives:
To elucidate the accuracy and advantages of Multichannel intraluminal impedance-pH monitoring (MII-pH) in diagnosing gastroesophageal reflux-induced chronic cough (GERC).
Methods:
The patients with suspected GERC were recruited and underwent MII-pH, GERC was confirmed by subsequent anti-reflux treatment despite the findings of MII-pH. Its diagnostic accuracy in identifying GERC were evaluated by receiver operating characteristic (ROC) analysis and compared with that of 24-h esophageal pH monitoring.
Results:
Among 158 patients completing both MII-pH and anti-reflux therapy, GERC was diagnosed in 136 patients, including acid GERC in 96 patients (70.6%), non-acid GERC in 30 patients (22.0%), neither one of both GERC in 10 patients (7.4%). For the identification of GERC, MII-pH presented with the sensitivity of 92.6%, specificity of 63.6%, positive predictive value of 94.0%, negative predictive value of 58.3% and area under ROC curve of 0.863, which was totally superior to 24-h esophageal pH monitoring. As the essential criteria of MII-pH, esophageal acid exposure time and symptom associated probability had a limited diagnostic value when used alone, but improved greatly the diagnostic yield when used in combination, even with a suboptimal efficacy.
Conclusion:
MII-pH is a more sensitive test for identifying GERC, but with a suboptimal diagnostic efficacy.
Keywords: Esophageal acid exposure time, cough, esophageal pH monitoring, gastroesophageal reflux, symptom associated probability
Introduction
Gastroesophageal reflux-induced chronic cough (GERC) is a special gastroesophageal reflux disease (GERD) with the predominant cough and a common cause of chronic cough.1–3 Presently, ambulatory 24-h esophageal pH monitoring is a main laboratory tool employed for the diagnosis of GERC.4 However, it can only detect acid reflux but not non-acid reflux, and may easily under-diagnose GERC caused by non-acid reflux. Thus, the unmet clinical need appeals a diagnostic method for GERC with a higher sensitivity and specificity.
Multichannel intraluminal esophageal impedance-pH monitoring (MII-pH) has been recommended as an important means for detecting gastroesophageal reflux since it can effectively analyze the characters and components of refluxates including the identification of liquid and gas reflux as well as the differentiation of acid and non-acid reflux.5 However, there were only a few studies on the evaluation of MII-pH in GERC.6 In a preliminary study, we have noticed the usefulness of MII-pH in diagnosing GERC.7 Thus, we performed a prospective investigation to evaluate the efficacy of MII-pH in identifying GERC in a larger number of patients with suspected GERC.
Materials and methods
Patients
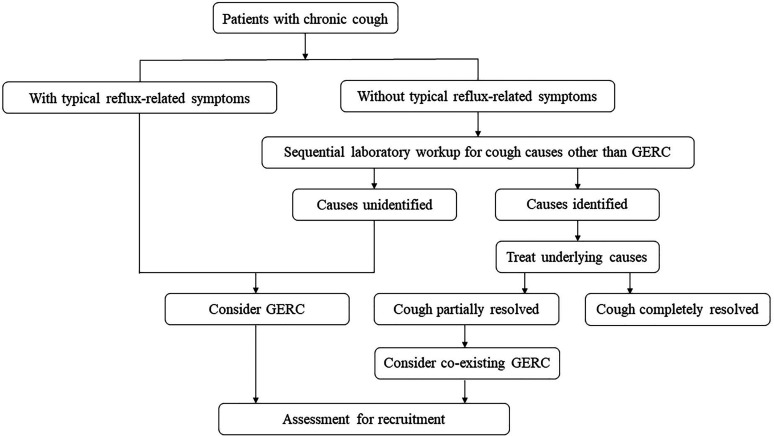
Consecutive patients with cough lasting for ≥8 weeks referred for possible GERC to our respiratory clinic were recruited into this study from July 2016 to July 2019. Inclusion criteria were anyone of followings: (1) chronic cough with co-existing typical reflux-related symptoms such as regurgitation and heartburn; (2) potential GERC was considered when the other common causes of chronic cough including cough variant asthma, upper airway cough syndrome, eosinophilic bronchitis were excluded after a sequential laboratory workup according to an established algorithm3; (3) concomitant GERC was suspected when the therapy pointed to the current cause of chronic cough could not resolve cough completely.8 Patients’ flow was shown in Figure 1 where patients would enter assessment for the study at the top of Figure 2. Exclusion criteria included: (1) refusal or intolerance to MII-pH; (2) women in pregnancy or lactation.
Figure 1.
Patients’ flow diagram for the recruitment. GERC: gastroesophageal reflux-induced chronic cough.
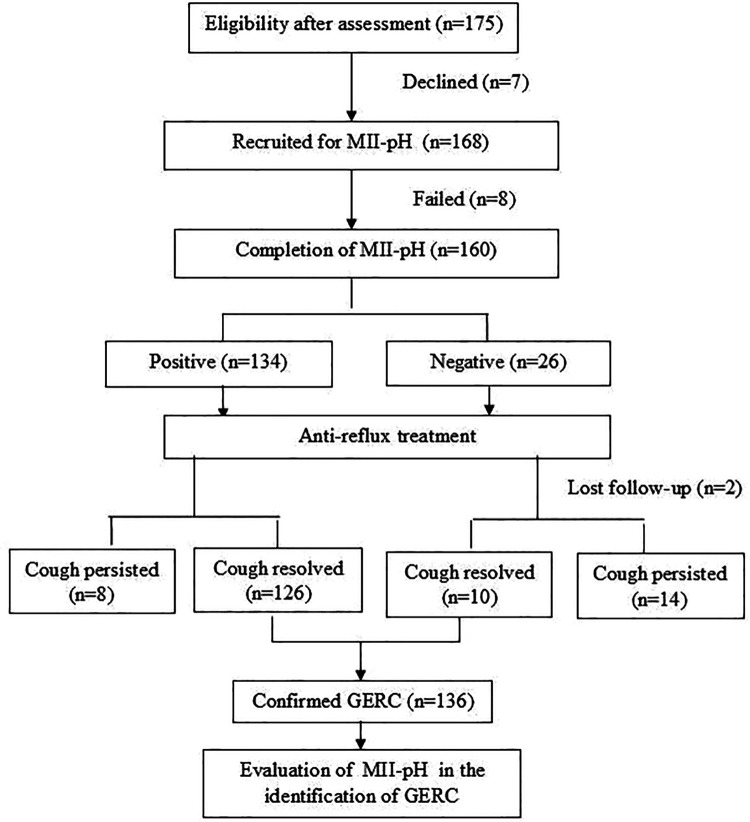
Figure 2.
Consort flow diagram of the study. GERC: gastroesophageal reflux-induced chronic cough; MII-pH: multichannel intraluminal impedance-pH monitoring.
It is a single-center observational study. The protocol was approved by the Ethics Committee of Tongji Hospital (No. K-1017-019). Written informed consent was obtained from each participant before enrollment.
MII-pH
MII-pH was conducted off acid suppression for at least one week as described previously.9 On the testing day, the patients appeared to the esophageal laboratory in our hospital after an overnight fasting and were asked to keep in a sitting or supine position. After the location of lower esophageal sphincter by previous esophageal manometry (Solar GI, Medical Measurement System B.V., Netherlands), a 2.1-mm diameter combined MII-pH catheter consisting of six impedance channel amplifiers (K6011-E10632, Unisensor, Switzerland) and an antimony pH probe (819100, Medical Measurement System B.V., Netherlands) was transnasally inserted into the esophagus, with impedance channel amplifiers located at 3, 5, 7, 9, 15 and 17 cm above the manometrically determined lower esophageal sphincter, and pH probe positioned 5 cm above the proximal border of lower esophageal sphincter. Prior to the procedure, the pH probe was calibrated at pH 4.0 and 7.0 according to the manufacturer’s instructions. The catheter was connected to a portable data logger (Ohmega, Medical Measurement System B.V. Netherlands) that collects the data from all seven channels with 50 Hz frequency over 24 h. The patients were instructed to maintain their usual life style, and keep a diary to record the timing of the start and end of meals, changes in position and symptoms.
Using specific software (Database soft, 8.7 version, Medical Measurement System B.V., Netherlands), the data were automatically analyzed but manually reviewed for reflux episodes, which are classified as liquid, gas and mixed reflux on the basis of impedance values, and categorized into acidic (pH < 4.0) and non-acidic consisting of weakly acidic (pH 4.0–7.0) and weakly alkaline reflux (pH > 7.0).10 Symptom association probability (SAP) for acid and non-acid reflux was calculated to establish the temporal association between cough and MII-detected liquid-containing reflux.6,11 Briefly, the entire recording was divided into consecutive 2-min time widows and evaluated for the presence of reflux. Combined with cough time and number recorded on diary cards, each time widow of the recording was classified into reflux alone, reflux followed by cough, only cough but no reflux and neither reflux nor cough. When a cough occurred in the 2-min time widow after the start of a reflux event, it was considered “associated to reflux.” The probability (P-value) that the observed association between reflux (acid or nonacid) and cough occurred by chance, was calculated from the contingency table containing the number of the above different types of 2-min widows with Fisher’s exact test. The SAP was expressed as (1.0-P) ×100%. Esophageal acid exposure time (AET) was expressed as total time percentage of esophageal pH < 4 over the whole monitoring time and used as a global measure of esophageal acid exposure. Abnormal reflux was defined as AET > 6% and/or SAP for acid and nonacid reflux ≥ 95%5 and used for the diagnostic criteria of GERC.
For the comparison with pure 24-h esophageal pH monitoring, the data of MII-pH in the same patients were re-analyzed by ignoring the tracings of impedance channel sensors and only reviewing the recordings of pH to simulate and collect the data of 24-h esophageal pH monitoring, with AET >6% and/or SAP for acid reflux ≥95% as the positive criteria of abnormal acid reflux.
Diagnostic criteria of GERC
The diagnosis of GERC were confirmed when the patients met all the following criteria: (1) the presence of chronic cough, with or without typical reflux symptoms; (2) MII-pH revealed abnormal acid (for acid GERC) or nonacid reflux (for nonacid GERC), defined by a positive AET and/or SAP for acid or nonacid reflux as described above; (3) cough disappeared or substantially improve with medical anti-reflux therapy.5,9
Studying procedures
Initial assessment of patients included the collection of general information, the recording of cough severity and performance of MII-pH. Cough severity was evaluated by the validated Chinese version12 of cough symptom score described by Hsu et al.13 Despite the findings of MII-pH, all the patients received an 8 weeks of standard anti-reflux therapy comprising omeprazole, 20 mg twice daily 30 min before meals, and domperidone, 10 mg three times daily. When the initial treatment failed and MII-pH revealed the abnormal reflux, the patients were given an augmented anti-reflux trial, either by doubling the dose of omeprazole to 80 mg daily or replacing domperidone with baclofen 20 mg three times daily14 or gabapentin 300 mg three times daily.15 The patients received follow-ups every 2 weeks, and their response to therapy and cough symptom score were recorded at each time. GERC was definitely confirmed when cough was completely resolved or significantly improved (cough symptom score decreased by >50%) in response to the anti-reflux treatment.15 Patients with abnormal acid reflux were diagnosed as acid GERC while these with abnormal non-acid reflux were defined as non-acid GERC.16
Statistical analysis
Data with normal distribution were expressed as mean ± SD, whereas those with skewed distribution were expressed as medians (25%, 75% interquartile). Receiver operating characteristic (ROC) analysis was employed to evaluate the efficacy of AET and SAP in identifying GERC. The diagnostic efficacy of MII-pH and 24-h esophageal pH monitoring was compared by chi square test. The consistence of diagnosis was evaluated with Kappa test. SPSS 14.0 software (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. A P-value <0.05 was accepted as statistically significant.
Results
General information
A total of 175 patients with suspected GERC met the inclusion criteria, accounting for 29.8% of 587 patients with chronic cough referred during the study period. Except for seven patients who declined and eight patients who failed to undergo MII-pH because of intolerance to intubation, 160 patients received MII-pH examination. Two patients lost to follow-up after the initiation of anti-reflux treatment. Finally, 158 patients completed both MII-pH and anti-reflux therapy (Table 1, Figure 2).
Table 1.
General information of the patients.
| Items | Value |
|---|---|
| Case number (male/female) | 158 (70/88) |
| Age (years, x ± s) | 44.3 ± 14.6 |
| Cough duration (months) | 12 (6, 48) |
| Cough symptom score | |
| Daytime | 3 (3, 4) |
| Nighttime | 1 (1, 2) |
| FEV1 (% predictive value) | 100.0 ± 13.6 |
| FVC (% predictive value) | 100.9 ± 14.1 |
| FEV1/FVC | 86.5 ± 10.4 |
FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity.
Cough duration and cough symptom score were expressed as medium (interquartile).
Etiological diagnosis
One hundred thirty-six patients (86.1%) favorably responded to anti-reflux therapy and were conclusively diagnosed as having GERC, including acid GERC in 96 patients (70.6%), non-acid GERC in 30 patients (22.0%), and mixed acid with non-acid GERC in 10 patients (7.4%). Their cough was relieved in response to the therapy containing omeprazole in 101 patients (74%), baclofen in 26 patients (19%) and gabapentin in 9 patients (7%), respectively. Among 22 patients failing to anti-reflux treatment and recruited by inclusion criteria one, their cough was finally explained by cough variant asthma in six, eosinophilic bronchitis in four, atopic cough in three and psychogenic cough in two. In the remaining seven patients, no etiology could be identified.
MII-pH in identifying GERC
One hundred thirty-four (84.8%) patients had a positive finding of MII-pH, including the purely increased AET in 69 (51.5%) patients, only positive SAP for acid reflux in 10 (7.5%) patients, only positive SAP for non-acid reflux in 30 (22.4%) patients and both positive AET and SAP in 25 (18.6%) patients. Finally, GERC were confirmed in 126 (94.0%) patients. Among the remaining 24 patients with normal MII-pH, cough was favorably responsive to empirical anti-reflux treatment in 10 (41.7%) patients (Figure 2).
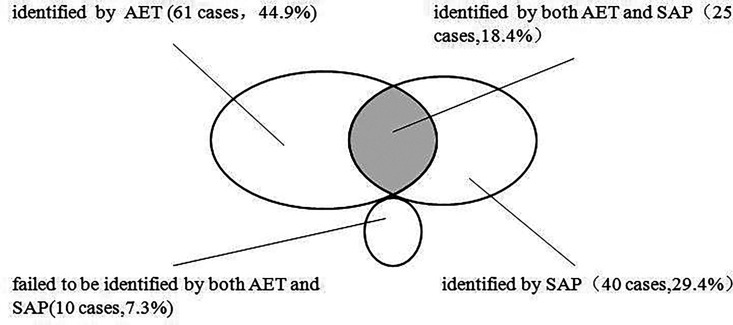
Totally, 18.4% GERC (25 cases) was overlapped identified by both AET and SAP, 44.9% GERC (61 cases) exclusively identified by AET, and 29.4% GERC (40 cases) exclusively identified by SAP. 7.3% GERC (10 cases) failed to be identified by either AET or SAP (Figure 3).
Figure 3.
Identifying proportion of GERC by AET and SAP. AET: esophageal acid exposure time; GERC: gastroesophageal reflux-induced chronic cough; SAP: symptom association probability.
By using AET or SAP as a diagnostic criteria, the efficacy of MII-pH in identifying GERC was shown in Table 2. AET presented with a moderate sensitivity, specificity and area under curve, a high positive predictive value and a low negative predictive value and Kappa value. In contrast, all of total SAP, SAP for acid reflux or non-acid reflux had a low sensitivity, negative predictive value and Kappa value, a high specificity and positive predictive value, and a moderate area under curve. However, the combination of AET with SAP (either one was positive) obviously improved the diagnostic accuracy of MII-pH in identifying GERC.
Table 2.
Diagnostic efficacy of MII-pH in diagnosing GERC.
| Parameters | Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) | Kappa | Area under ROC curve |
|---|---|---|---|---|---|---|
| AET and SAP | 92.6 | 63.6 | 94.0 | 58.3 | 0.512 | 0.863 |
| AET | 63.2 | 63.6 | 91.5 | 21.9 | 0.149 | 0.657 |
| SAP for acidic reflux | 25.7 | 100 | 100 | 17.9 | 0.088 | 0.721 |
| SAP for non-acidic reflux | 22.1 | 100 | 100 | 17.2 | 0.073 | 0.714 |
AET: esophageal acid exposure time; GERC: gastroesophageal reflux-induced chronic cough; MII-pH: multichannel intraluminal esophageal impedance-pH monitoring; ROC: receiver operating curve; SAP: symptom association probability.
Comparison of MII-pH with 24-h esophageal pH monitoring in identifying GERC
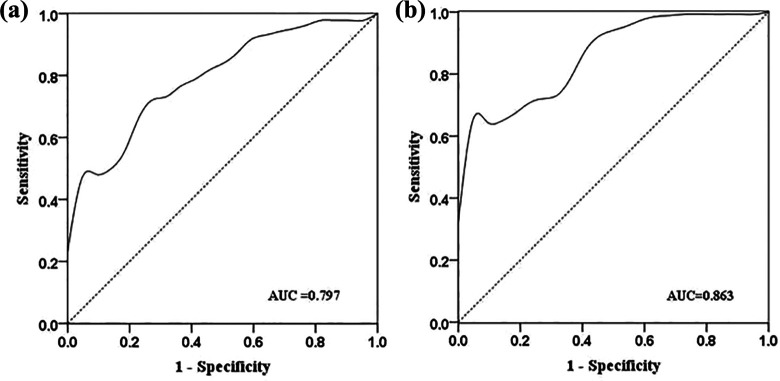
MII-pH had a higher sensitivity, positive predictive value, Kappa value and area under than those of pure 24-h esophageal pH monitoring, with a similar specificity and negative predictive value (Table 3, Figure 4).
Table 3.
Comparison on the efficacy between MII-pH and 24-h esophageal pH monitoring in identifying GERC.
| Method | Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) | Kappa |
|---|---|---|---|---|---|
| MII-pH | 92.6 | 63.6 | 94.0 | 58.3 | 0.542 |
| 24-h esophageal pH monitoring | 70.6 | 63.6 | 92.3 | 25.9 | 0.213 |
| X2 value | 25.9 | …. | 0.277 | 7.583 | — |
| P-value | 0.000 | …. | 0.599 | 0.006 | All <0.01 |
GERC: gastroesophageal reflux-induced chronic cough; MII-pH: multichannel intraluminal esophageal impedance-pH monitoring.
Figure 4.
Receiver operating curve (ROC) of multichannel intraluminal impedance-pH monitoring (MII-pH) and 24-h esophageal pH monitoring in identifying gastroesophageal reflux-induced chronic cough (GERC). AUC: area under the curve, sensitivity and 1-specificity by positive esophageal acid exposure time and symptom association probability (SAP) (A: MII-pH; B: 24-h esophageal pH monitoring).
Discussion
Laboratory tests available for GERC include barium esophagography, esophagoscopy and 24-h esophageal pH monitoring.17 Since barium esophagography and esophagoscopy only reveal the positive findings in only 35–50% patients with GERC,18,19 they are not recommended as the first-line choice in identifying GERC. 24-h esophageal pH monitoring, a preferred test for diagnosing GERC, has a higher sensitivity and specificity than barium esophagography and esophagoscopy.17 Nevertheless, it cannot identify non-acid and gas reflux as well as the moving direction of intraesophageal liquids and alimentary bolus, and thus have no ability to recognize the cough due to non-acid reflux.10
The study has demonstrated that MII-pH is superior to 24-h esophageal pH monitoring in identifying GERC. Nevertheless, its specificity and negative predictive value was the same as those of 24-h esophageal pH monitoring. These findings are consistent with the previous observations of our preliminary report with a small sample size that MII-pH additionally identifies non-acid GERC when keeping the same ability to measure acid reflux as 24-h esophageal pH monitoring,7 regardless of a slightly higher sensitivity but lower specificity in the present study. Therefore, MII-pH may make up the defects of 24-h esophageal pH monitoring in lacking the ability to detect non-acid reflux, and present with a better diagnostic accuracy for GERC in clinical practices.
The diagnosis of GERC depends essentially on AET and SAP according to the current guideline for the management of chronic cough.4,5 This study has demonstrated that both AET and SAP have their own merits in predicting GERC, with a moderate sensitivity and specificity in AET and a low sensitivity but high specificity in SAP. Therefore, these parameters present with a limited efficacy alone and are unable to meet the needs for the diagnosis of GERC. However, when either positive AET or SAP is used in combination as the objective criteria of GERC, the diagnostic yield has been greatly improved and the shortcomings of single indicator have been maximally compensated.
Despite its advantages over 24-h esophageal pH monitoring, MII-pH has its inherent limitations, with a suboptimal sensitivity and specificity in identifying GERC. Currently, there is no general consensus on how to best interpret the results of MII-pH. AET has nothing to do with the non-acid reflux. SAP only reflects the cough within two-minute time widow after the occurrence of reflux episodes, which only accounts for 56–81% of the total count of cough.20 During MII-pH, the patients often forget to record the cough events or mislabel the cough time, leading to the inaccuracy in the calculation of SAP.21 The positive rate of SAP was only 35% in the patients with suspected GERC,22 could be only increased to 48–71% even MII-pH was combined with synchronous esophageal manometry or cough frequency recording.23 In the situation that GERC is highly probable by clinical manifestation but with a negative MII-pH, the empirical anti-reflux therapy is still necessary to be instituted to minimize the misdiagnosis and under-diagnosis.24 In the study, 10 patients with the negative findings of MII-pH were finally confirmed to suffer from GERC with subsequent empirical anti-reflux treatment.
In the present study, the favorable response to anti-reflux therapy was set as the gold standard for definite GERC. Despite its advantage on verifying the cause-effect relation between reflux and cough, the failure to anti-reflux therapy cannot exclude the possibility that the patients with positive findings of MII-pH still had GERC since some patients with abnormal reflux (especially with non-acid reflux) were resistant to antireflux medicinal treatment but might have responded to anti-reflux surgery.25 Therefore, it is predictable that the diagnostic efficacy and accuracy of MII-pH for potential GERC might be underestimated by the means of outcome assessment used in the study.
One may criticize the therapeutic gain of anti-reflux therapy was mainly due to placebo effect since it is an uncontrolled treatment with omeprazole and domperidone. It is true that the placebo effect cannot be excluded, which might contribute up to 50% of the therapeutic efficacy in the study26 and limit the strength of conclusions. However, the purpose of the study is to demonstrate the diagnostic accuracy and yield of MII-pH by observing the antireflux response in the patients with potential GERC and not to verify the efficacy of anti-reflux medicinal therapy. Moreover, anti-reflux medicinal therapy employed in the study are logically expected to be effective for GERC when considering their benefits in the treatment of gastroesophageal reflux disease.4,5 We do not believe placebo effects of omeprazole and domperidone can completely explain the high therapeutic success rate (81.6%) in the cohort of the patients with chronic cough.
In conclusion, MII-pH is a more reliable and sensitive test currently available for identification of GERC, and can recognize non-acid GERC failing to be detected by 24-h esophageal pH monitoring. It improves the diagnostic yield of GERC and is gradually replacing 24-h esophageal pH monitoring for the identification of GERC in clinical practice. However, MII-pH has its inherent limitations similar to 24-h esophageal pH monitoring with suboptimal diagnostic efficacy. For the suspected GERC patients with a negative MII-pH, the implementation of empirical anti-reflux is a remedy to avoid the misdiagnosis and under- diagnosis of GERC.
Footnotes
Authors’ note: Na Li and Qiang Chen contributed equally as co-first authors.
Author contributions: Na Li had full access to the data in the study and was responsible for data integrity and the accuracy of the data analysis. Na Li and Qiang Chen were in charge of case collection, processing and statistical analysis of data, interpretation of the results and writing the manuscript. Qiang Chen also participated the critical review of the manuscript. Siwan Wen, Mengru Zhang, Ran Dong, Xianghuai Xu and Li Yu participated in case collection and critical review of the manuscript. Zhongmin Qiu was in charge of study design, program coordination, and review and correction of the manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the grants from the National Natural Science Foundation of China (No. 81670092), the Project of Science and Technology Commission of Shanghai Municipality (No. 20Y11902500) and Tongji Hospital (No. ITJ(ZD)2006 and TJ1801).
ORCID iD: Zhongmin Qiu  https://orcid.org/0000-0002-6612-7413
https://orcid.org/0000-0002-6612-7413
References
- 1. Kahrilas PJ. Chronic cough and gastroesophageal reflux disease: new twists to the riddle. Gastroenterology 2010; 139: 716–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lai K, Chen R, Lin J. et al. A prospective, multicenter survey on causes of chronic cough in China. Chest 2013; 143: 613–620. [DOI] [PubMed] [Google Scholar]
- 3. Wei W, Yu L, Lu H. et al. Comparison of cause distribution between elderly and non-elderly patients with chronic cough. Respiration 2009; 77: 259–264. [DOI] [PubMed] [Google Scholar]
- 4. Kahrilas PJ, Altman KW, Chang AB. et al. Chronic cough due to gastroesophageal reflux in adults: CHEST guideline and expert panel report. Chest 2016; 150: 1341–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gyawali CP, Kahrilas PJ, Savarino E. et al. Modern diagnosis of GERD: the Lyon Consensus. Gut 2018; 67: 1351–1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sifrim D, Dupont L, Blondeau K. et al. Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, and impedance monitoring. Gut 2005; 54: 449–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Liu B, Yu L, Qiu ZH. et al. The diagnostic value of multichannel intraluminal esophageal impedance and pH monitoring in gastroesophageal reflux-related cough. Zhonghua Nei Ke Za Zhi 2012; 51: 867–870. [PubMed] [Google Scholar]
- 8. Xu X, Chen Q, Liang S. et al. Comparison of gastroesophageal reflux disease questionnaire and multichannel intraluminal impedance pH monitoring in identifying patients with chronic cough responsive to antireflux therapy. Chest 2014; 145: 1264–1270. [DOI] [PubMed] [Google Scholar]
- 9. Qiu Z, Yu L, Xu S. et al. Cough reflex sensitivity and airway inflammation in patients with chronic cough due to non-acid gastro-oesophageal reflux. Respirology 2011; 16: 645–652. [DOI] [PubMed] [Google Scholar]
- 10. Sifrim D, Castell D, Dent J. et al. Gastro-oesophageal reflux monitoring: review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Gut 2004; 53: 1024–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Blondeau K, Dupont LJ, Mertens V. et al. Improved diagnosis of gastro-oesophageal reflux in patients with unexplained chronic cough. Aliment Pharmacol Ther 2007; 25: 723–732. [DOI] [PubMed] [Google Scholar]
- 12. Zhao T, Qiu Z, Wang L. et al. Validation of the reliability and clinical value of the simplified cough score. Zhonghua Quan Ke Yi Shi Za Zhi 2012; 11: 273–276. [Google Scholar]
- 13. Hsu JY, Stone RA, Logan-Sinclair RB. et al. Coughing frequency in patients with persistent cough: assessment using a 24 hour ambulatory recorder. Eur Respir J 1994; 7: 1246–1253. [DOI] [PubMed] [Google Scholar]
- 14. Xu X, Lv H, Yu L. et al. A stepwise protocol for the treatment of refractory gastroesophageal reflux-induced chronic cough. J Thorac Dis 2016; 8: 178–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dong R, Xu X, Yu L. et al. Randomised clinical trial: gabapentin vs baclofen in the treatment of suspected refractory gastro-oesophageal reflux-induced chronic cough. Aliment Pharmacol Ther 2019; 49: 714–722. [DOI] [PubMed] [Google Scholar]
- 16. Xu X, Yang Z, Chen Q. et al. Comparison of clinical characteristics of chronic cough due to non-acid and acid gastroesophageal reflux. Clin Respir J 2015; 9: 196–202. [DOI] [PubMed] [Google Scholar]
- 17. Irwin RS. Chronic cough due to gastroesophageal reflux disease: ACCP evidence-based clinical practice guidelines. Chest 2006; 129: 80s–94s. [DOI] [PubMed] [Google Scholar]
- 18. Ott DJ. Gastroesophageal reflux: what is the role of barium studies? AJR Am J Roentgenol 1994; 162: 627–639. [DOI] [PubMed] [Google Scholar]
- 19. Vakil N, van Zanten SV, Kahrilas P. et al. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 2006; 101: 1900–1920; quiz 1943. [DOI] [PubMed] [Google Scholar]
- 20. Vela MF. Multichannel intraluminal impedance and pH monitoring in gastroesophageal reflux disease. Expert Rev Gastroenterol Hepatol 2008; 2: 665–672. [DOI] [PubMed] [Google Scholar]
- 21. Kavitt RT, Higginbotham T, Slaughter JC. et al. Symptom reports are not reliable during ambulatory reflux monitoring. Am J Gastroenterol 2012; 107: 1826–1832. [DOI] [PubMed] [Google Scholar]
- 22. Wunderlich AW, Murray JA. Temporal correlation between chronic cough and gastroesophageal reflux disease. Dig Dis Sci 2003; 48: 1050–1056. [DOI] [PubMed] [Google Scholar]
- 23. Smith JA, Decalmer S, Kelsall A. et al. Acoustic cough-reflux associations in chronic cough: potential triggers and mechanisms. Gastroenterology 2010; 139: 754–762. [DOI] [PubMed] [Google Scholar]
- 24. Yu L, Xu X, Hang J. et al. Efficacy of sequential three-step empirical therapy for chronic cough. Ther Adv Respir Dis 2017; 11: 225–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Novitsky YW, Zawacki JK, Irwin RS. et al. Chronic cough due to gastroesophageal reflux disease: efficacy of antireflux surgery. Surg Endosc 2002; 16: 567–571. [DOI] [PubMed] [Google Scholar]
- 26. Eccles R. The powerful placebo effect in cough: relevance to treatment and clinical trials. Lung 2020; 198: 13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]