Abstract
We present a case of an isolated open bronchus rupture following blunt thoracic trauma. Tracheobronchial injuries (TBI) following blunt chest trauma are a rare but possibly life-threatening condition. Though typically associated with additional injuries, high-energy blunt trauma led to perforating chest wound alone. A bronchial injury has not been seen neither in preoperative CT scan nor intraoperatively. This underlines the strong need for bronchoscopy in chest trauma as the only definitive diagnostic in bronchial lesions.
Keywords: Bronchus rupture, Blunt chest trauma, Bronchoscopy, Thoracic trauma, Tracheobronchial injury
Case presentation
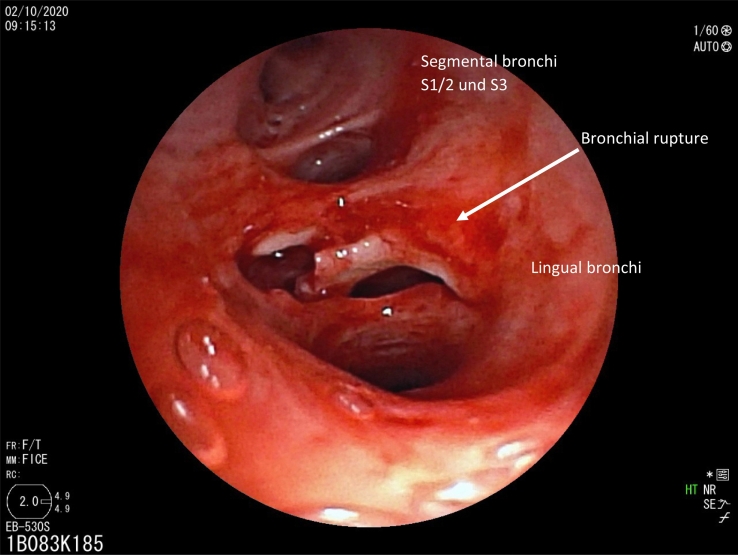
A 57-year-old male smith suffered a major chest trauma during open die forging of glowing steel. A 200-degree Celsius hot pliers lost its grip and was catapulted to his chest causing an about 4 cm long, left parasternal wound penetrating pleura. Patient suffered from severe pain and dyspnoea, but was awake and haemodynamically stable. Despite of small superficial lacerations on forehead and lower leg, no other injuries were found. CT scan showed displaced fracture of second rib with nondisplaced fracture of sternum. After trauma room assessment, patient was directly admitted to the operation theatre for video-assisted thoracoscopy. Apart from cardiac contusion with haemorrhagic pericardial effusion, hiliar vessels impressed skeletonized up until segmental bronchi, while not ruptured. A bronchial injury has not been seen neither in preoperative CT scan nor intraoperatively. Due to massive bronchial secretion, intraoperative bronchoscopy was necessary. After bronchial evacuation of large amounts of blood clots, a bronchial lesion between upper lobe and lingula got visible (Fig. 1). Via thoracotomy, rupture was treated with interrupted 4-0 monofilament absorbable suture and covered with pediculated pericardial patch. Underwater testing showed no air leakage. Patient recovered well from the operation and was discharged from hospital on tenth post-operative day.
Fig. 1.
Bronchial rupture between upper lobe and lingua.
Discussion
We present a case of an isolated open bronchus rupture following blunt thoracic trauma. Tracheobronchial injuries (TBI) following blunt chest trauma are a rare but possibly life-threatening condition [1]. While improved ambulant services reduced number of patients dying before reaching the hospital, most patients suffering from TBI die immediately [[1], [2], [3], [4]]. Blunt trauma is typically associated with additional injuries for example of abdomen, head, vocal cords or spine [5]. This is due to typical mechanism of blunt chest trauma. One can differentiate between three usual ways of trauma: 1) “explosive rupture” by high intraluminal pressure during thoracic compression while glottis is closed; 2) deceleration trauma leading to shear stress on fixed points, e.g. carina; 3) tension on carinal tissue during extensive anterior-posterior thorax compression [6,7]. In our case, high-energy blunt trauma led to perforating wound with no other injuries. Even costal violation was small. Typically, TBI from penetrating traumas are located in the cervical site [5]. In blunt trauma, TBI is most often located within the first 2 cm of the right main bronchus [6]. Reasons for that may be the shorter right bronchus carrying the heavier right lung as well as higher exposure due to fewer surrounding tissue [6]. In our patient, subcarina between upper lobe and lingula may have been a predetermined breaking point from the accentuated collision directly on the left hemithorax.
Bronchoscopy remains the gold standard and only definitive diagnostic in bronchus lesions [5,8]. In our case, bronchus rupture was diagnosed via bronchoscopy alone. This underlines the strong need for bronchoscopy in chest trauma even if CT scan and thoracoscopic examination were unsuspicious.
Conclusion
Isolated TBI is an exceedingly rare trauma with the need for urgent interdisciplinary treatment. Bronchoscopy should be performed in all perforating chest trauma for safe evaluation of tracheobronchial tree.
Acknowledgments
Acknowledgments
We acknowledge support from Leipzig University for Open Access Publishing.
References
- 1.van Roozendaal Lori M., van Gool Matthijs H., Sprooten Roy T.M., Maesen Bart A.E., Poeze Martijn, Hulsewé Karel W.E. Surgical treatment of bronchial rupture in blunt chest trauma: a review of literature. Journal of Thoracic Disease. 2018;10(9):5576–5583. doi: 10.21037/jtd.2018.08.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bertelsen S., Howitz P. Injuries of the trachea and bronchi. Thorax. 1972;27(2):188–194. doi: 10.1136/thx.27.2.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kirsh Marvin M., Orringer Mark B., Behrendt Douglas M., Sloan Herbert. Management of tracheobronchial disruption secondary to nonpenetrating trauma. Ann. Thorac. Surg. 1976;22(1):93–101. doi: 10.1016/S0003-4975(10)63961-6. [DOI] [PubMed] [Google Scholar]
- 4.Taskinen Seppo O., Salo Jarmo A., Halttunen Paavo E.A., Sovijärvi Anssi R.A. Tracheobronchial rupture due to blunt chest trauma: a follow-up study. Ann. Thorac. Surg. 1989;48(6):846–849. doi: 10.1016/0003-4975(89)90683-8. [DOI] [PubMed] [Google Scholar]
- 5.Altinok Tamer, Can Atilla. Management of tracheobronchial injuries. Eurasian J. Med. 2014;46(3):209–215. doi: 10.5152/eajm.2014.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kiser Andy C., O’Brien Sean M., Detterbeck Frank C. Blunt tracheobronchial injuries: treatment and outcomes. Ann. Thorac. Surg. 2001;71(6):2059–2065. doi: 10.1016/s0003-4975(00)02453-x. [DOI] [PubMed] [Google Scholar]
- 7.Prokakis Christos, Koletsis Efstratios N., Dedeilias Panagiotis, Fligou Fotini, Filos Kriton, Dougenis Dimitrios. Airway trauma: a review on epidemiology, mechanisms of injury, diagnosis and treatment. J. cardiothorac. Surg. 2014;9:117. doi: 10.1186/1749-8090-9-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Symbas Panagiotis N., Justicz Alexander G., Ricketts Richard R. Rupture of the airways from blunt trauma: treatment of complex injuries. Ann. Thorac. Surg. 1992;54(1):177–183. doi: 10.1016/0003-4975(92)91177-B. [DOI] [PubMed] [Google Scholar]