Abstract
Objective:
Although several effective behavioral treatments for binge-eating disorder (BED) exist, there are racial disparities in treatment access, with African-Americans and/or Black individuals having some of the lowest rates of access to care. Little is known about the experience and treatment of binge eating (BE) and BED among Black women.
Method:
This systematic review, conducted according to PRISMA guidelines, synthesizes information related to BE and BED in Black women.
Results:
A total of N=38 studies met our eligibility criteria. We did not identify any systematic risk of bias across studies. The majority of included studies used cross-sectional survey methodology, and relied on interview (EDE) and self-report measures (particularly the Binge Eating Scale, BES) for the assessment of BE. Outcomes were inconsistently measured across trials, and there are limited data on the results of evidence-based treatments for BE/BED in Black women.
Discussion:
Although Black women have similar or higher rates of BE than White women, most research on BE and BED has focused on White women, with Black individuals underrepresented in clinical trials. Future research should examine evidence-based treatments to prevent and treat BED in this population.
Keywords: Binge Eating, Binge Eating Disorder, Black, African-American women, systematic review
Introduction
Binge eating (BE) is characterized by patterns of eating more than a person would typically eat in a discrete period, while experiencing a sense of loss of control (American Psychiatric Association, 2013). Recurrent BE is a key behavior of binge-eating disorder (BED) (American Psychiatric Association, 2013), which is defined as recurrent BE (occurring at least once a week for three months) while concurrently experiencing loss of control and marked distress, in the absence of regular compensatory behaviors for weight loss (American Psychiatric Association, 2013; Udo et al., 2016). BED is the most common eating disorder across all racial and ethnic groups in the United States (Hudson, Hiripi, Pope, & Kessler, 2007; Taylor, Caldwell, Baser, Faison, & Jackson, 2007), affecting between .85% - 2.6% of the nation’s population (Kessler et al., 2013; Udo & Grilo, 2018). Moreover, BED is often comorbid with multiple somatic and psychiatric conditions, including obesity, metabolic syndrome, substance use disorders, and mood disorders (Hudson et al., 2007; Hudson et al., 2010; Taylor et al., 2007; Thornton et al., 2017; Welch et al., 2016).
Compared with White women, recent studies report similar or higher rates of BE in Black women (Lydecker & Grilo, 2016; Marques et al., 2011; Udo et al., 2016). In studies assessing BE within specific racial groups, the prevalence of this behavior among Black women was nearly 5%, compared with 2.5% in Non-Hispanic, White women (Goode, Kalarchian, Craighead, Conroy, Wallace, et al., 2018; Marques et al., 2011; Striegel-Moore, Wilfley, Pike, Dohm, & Fairburn, 2000). Furthermore, the prevalence of BE in women with obesity is even higher; estimates indicate that more than 30% of Black women with obesity also report BE (Mazzeo, Saunders, & Mitchell, 2005; Wilson et al., 2012).
Several effective behavioral treatments for BE and BED (e.g., behavioral weight loss [BWL], cognitive-behavioral therapy [CBT], interpersonal psychotherapy [IPT]) (Grilo, Masheb, Wilson, Gueorguieva, & White, 2011; Tanofsky-Kraff et al., 2013) exist. However, Black individuals have lower rates of access to care for eating disorders, compared with Non-Hispanic, Whites (Marques et al., 2011; Pike, Dohm, Striegel-Moore, Wilfley, & Fairburn, 2001; Scott, Gil-Rivas, & Cachelin, 2018). Furthermore, BE and BED may be more severe among Black women who do not access treatment; for example, in one study, Black women receiving treatment for BED demonstrated less pre-treatment BE than non-treatment seeking Black controls who also had BED (Grilo, Lozano, & Masheb, 2005; Scott et al., 2018). Early detection and intervention with this population might be a critical first step toward prevention and improvement of access to care for individuals with BE and BED (Ivezaj, Kalebjian, Grilo, & Barnes, 2014).
This article systematically reviews the empirical studies that have included Black women and addressed: (1) the prevalence of BE and BED; (2) racial differences in the nature and course of BE-pathology; (3) factors influencing the development of BE and BED; (4) evidence-based treatments; (5) access and participation in treatment for BE and BED; and (6) methodological limitations of the current scientific literature. We summarize specific challenges in the treatment of BE and BED among Black women and discuss future research opportunities and key areas for increased focus.
Methods
This systematic review was conducted in concordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Moher, Liberati, Tetzlaff, Altman, & Group, 2009).
Eligibility Criteria
Studies were independently examined for eligibility by two reviewers (R.G. and M.C.) according to the PICOS criteria (Liberati et al., 2009). To determine studies that met our inclusion and exclusion criteria, we used the PICOTS (population, interventions, comparators, outcomes, timing, settings, and study designs) approach. The desired population of interest was Black women with reported BE behaviors and/or a diagnosis of BED. We included case-control, secondary analyses, intervention studies with psychological or behavioral treatment, and cross-sectional evaluations that reported outcomes in the desired population.
Eligible and included studies were: (1) published up to 2019; (2) written in the English language; (3) restricted to participants ≥ 18 years; (4) original articles published in peer-reviewed journals; and (5) reporting outcomes of binge eating in Black women. Exclusion criteria were: (1) case studies or studies with a sample size smaller than five; (2) and reviews, meta-analyses, commentaries, letters to the editor, books or book chapters, abstracts, and clearly irrelevant papers. Studies that included Black participants, but that did not report any outcomes or analyses with reference to race, were excluded. The decision to include or exclude studies was initially made on the basis of the article title, then its abstract, and finally the full-text article. There were no limitations on setting, or study duration.
Information Sources and Search
We conducted literature searches up to and including October 2019 in the following electronic databases: PsycINFO, PubMed, Scopus, Web of Science, MEDLINE, and Google Scholar. Search terms included “African-American,” OR “Black woman,” AND “binge eating,” OR “eating disorder,” OR “binge eating disorder,” OR “disordered eating behaviors.” Reference lists of published papers were also screened to identify additional articles meeting eligibility criteria.
Selection
The process for study selection is summarized in Figure 1. One reviewer (MC) conducted an initial search for articles based upon our inclusion/exclusion criteria based on titles and abstracts. For each study, 2 independent reviewers (M.C. and C.C.L.) rated the risks of selection, performance, attrition, detection, and outcome reporting bias. Following this search, the reviewers rated whether studies met inclusion criteria by: (1) reviewing titles and abstracts, and (2) conducting a full-text review. Disagreements were resolved by consensus discussion.
Figure 1.
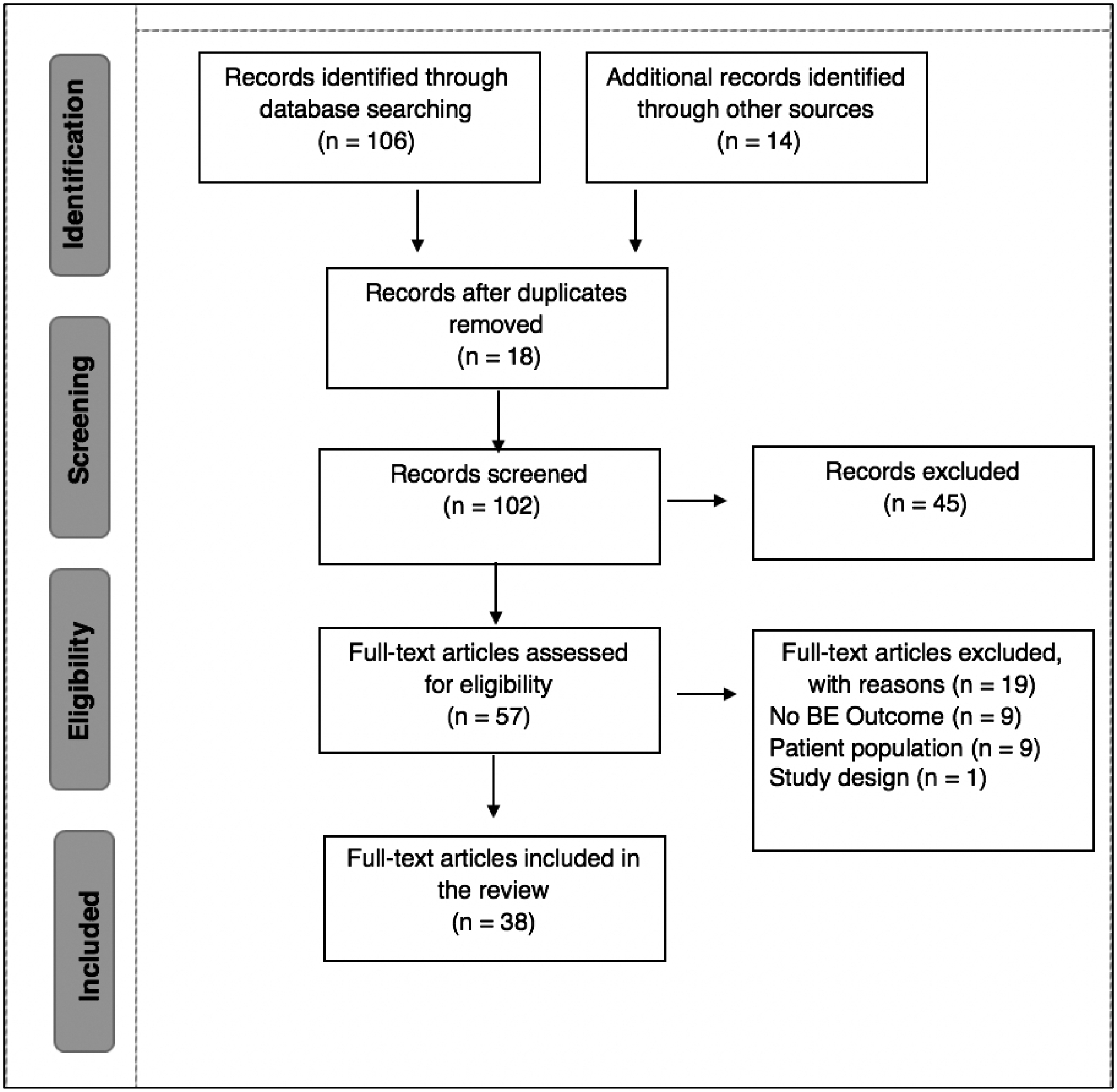
PRISMA Diagram of Systematic Review Study Selection Process; BE= binge eating
Following study selection, the following variables were extracted independently by three authors (M.C., A.F., O.O.) from each paper: study design, number of participants, mean age (SD), mean BMI (SD), percentage of Black women in the sample, prevalence of BE in Black women, sample characteristics, measurement of BE, and outcomes in Black women (Table 1).
Table 1.
Characteristics of included studies for systematic review
| Study | Study Design | Mean age (SD) | Mean BMI (SD) | N (% or # of Black women) | Prevalence of Binge Eating among Black participants | Sample Description | Measures of Binge Eating | Binge Eating Outcomes in Black Women |
|---|---|---|---|---|---|---|---|---|
| Adamus-Leach et al., 2013 | Secondary data analysis of cross-sectional data | 44.6 (9.2) | 34.7 (7.9) | 171 (n=127) | Mean BES score: 12.7 (7.5) | Community-based sample Not clinically diagnosed with BED |
BES | Significant, positive correlation between
depressive symptoms and binge eating (r=.25). Body fat %, depressive symptoms, and weekly stress inventory impact were associated with BES score [F (4, 169) = 9.2, p<.001) |
| Assari, 2018^ | Secondary data analysis of population-based study | 42.5 (SE .56) | NR | 3516 (n= 2299; 65% female) | Mean % of BED (.06) | Community based sample National data set |
CIDI eating disorder module | Higher perceived discrimination associated with higher odds of BE. |
| Azarbad, et al., 2010 | Cross-sectional study | 40.1 (9.9) | 51.7 (9.7) | 404 (n=224) | Mean BES score: 12.0 (8.4) | Women who presented for a psychological evaluation prior to undergoing Roux-en-Y gastric bypass surgery | BES | No racial differences in BES
scores. Black women exhibited less BE symptomatology than White women Nearly 8% of Black women evidenced severe binge eating symptomatology on the BES. |
| Blostein et al., 2017^ | Secondary data analysis of population-based study | 42.3 (0.5) | NR | 5191 (100%; % female NR) | NR | African-American or Caribbean American Black participants | WHO-CIDI BES |
Body dissatisfaction was strongly associated
with binge eating (OR = 6.94, 95% CI 4.21, 11.44). Gender was not associated with binge eating. |
| Cachelin et al., 2001 | Cross-sectional study | 30.5 (range 19–43 years) | 30.2 (range 14.5–65.3) | 61 (n=12) | NR | Fulfilled clinical BED criteria as defined by the DSM-IV community-based recruitment | EDE | Though 85% of sample reported wanting help for
an ED, only 57% had ever sought treatment. Main barriers to treatment seeking were financial. |
| Fitzgibbon et al., 1998 | Cross-sectional study | 35.2 (9.5) | 30.2 (8.2) | 179 (100%) | Mean Binge Scale score: 2.8 (4.2) | Community-based sample | QEWP-R Binge Scale | Women who reported BE were heavier, more
depressed, and preferred a slimmer body ideal. BE was unrelated to body image, depression, or weight. |
| Gayle et al., 2004 | Cross-sectional study | 39.5 (9.4) | 39.6 (9.7) | 52 (n=26) | BED prevalence: 30.8% (n=8) Subclinical BED: 38.5% (n=10) |
Participants recruited from university-based eating disorders program | QEWP-R | No significant ethnic differences (between Black and White women) in the nutritional composition (e.g., protein, calories, carbohydrates) of binges. |
| Goode et al., 2018 | Randomized Control Trial | 48.8 (12.8) | 33.7 (3.9) | 31 (100% ) | Baseline BES Score: 22.6 (7.0) Monthly OBE episodes: 2.8 (5.5) Monthly LOC: 16.8 (15.5) |
Reported experiencing at least one binge
eating episode monthly (within the last 3 months) Community sample randomized to Appetite Awareness Training (AAT) or wait-list control |
EDE BES |
AAT retention was 87.5% Compared to participants in the WAIT group, AAT participants had greater decreases in binge eating scores and greater improvements in eating self-efficacy scores at the end of week 8. |
| Grilo et al., 2005 | Case-control trial | 43.9 (9.2) | 36.2 (7.4) | Clinical Sample: 337 (n=35) Community sample: 98 (n= 52) |
Black Women
(Clinic): Binge episodes per week: 4.4 (Community) Binge episodes per week: 6 |
Met DSM-IV criteria for BED Clinical Sample & community sample |
EDE EDE-Q SCID-I/P |
Black and White women did not differ
significantly on the four EDE-Q scales of BE frequency. Clinic Black women had significantly higher BMI (ES = .47), and reported lower levels of OBE (ES = −.47) than the community sample. |
| Grilo et al., 2014^ | Randomized clinical trial | 43.9 (11.2) | 38.3 (5.6) | 104 (n=36; 70% female) | NR | Met DSM-V criteria for BED Respondents for treatment study in primary care |
EDE SCID-I/P |
At 6-months, the self-help CBT group had significantly lower binge eating frequency. Race nor gender moderated or predicted clinical outcomes. |
| Harrington et al., 2006 | Cross-sectional study | 20.7 (5.13) | 25.1 (5.5) | 178 (n=93) | Mean BES: 6.79 (6.6) |
Black and White women recruited from university courses | BES | Stress (r = .21, p <.05) and discriminatory stress (r = .22, p .05) were significantly related to BES scores. |
| Harrington et al., 2010 | Cross-sectional study | 29.6 (12.8) | 28.0 (7.4) | 179 (100%) | Mean BES: 9.3 (8.0) |
Community and university-based
sample Had to experience at least 1 traumatic event Not diagnosed with BED |
BES EDDS |
Trauma exposure and distress predict greater internalization of “Strong Black Women ideology”, which is associated with emotional inhibition/regulation difficulties, eating for psychological reasons, and binge eating. |
| Higgins et al., 2015 | Cross-sectional study | 19.0 (1.6) | 22.2 (2.8) | 276 (n=97) | Mean frequency of BE= .95 (2.9) | Participants were 276 women attending a Midwestern university in the United States | BUILT-R EDE-Q |
High body shame and high impulsivity was associated with increased binge eating. |
| Hrabosky & Grilo, 2007 | Cross-sectional study | 34.8 (9.7) | 30.5 (8.3) B: 31.0 (8.9) |
120 (n= 67) | OBE: 1.3 (3.0) EDE-Q: Shape: 2.5 (1.9) Weight: 2.1 (1.8) Restraint: 1.1 (1.5) Eating Concern: .95 (1.2) |
Community Sample of Black and Hispanic women | EDE-Q QEWP-R |
Higher weight associated with binge
eating. No significant differences were observed between Black and Hispanic women in BMI, body image attitudes or distress, eating attitudes or behavior, teasing experience, or depressive affect. |
| Jarosz et al., 2007 | Cross-sectional study | 40.6 (10.8) | 40.9 (7.1) | 96 (n=88) | NR | Sample recruited from four urban clinic sites | QEWP-R | Approximately 6.4% of sample reported recurrent binge eating, and 18.9% reported night eating syndrome. |
| Kelly, Cotter, & Mazzeo, 2012 | Cross-sectional study | 19.6 (3.7) | 24.8 (5.9) | 395 (100%) | EDE-Q Scores: Global: 1.5 (1.3) Restraint: 1.1 (2.3) Eating: 0.8 (1.1) Shape: 2.1 (1.6) Weight: 2.2 (1.8) |
Black, undergraduate women Recruited from psychology classes at a public university in the southeastern United States |
EDE-Q | Black women reported engaging in regular
subjective binge eating, self-induced vomiting, and laxative/diuretic
misuse. Participants reported levels of ED symptoms comparable to White community members, but lower than White undergraduate peers. |
| Kelly et al., 2012 | Secondary data analysis of a cross-sectional study | 19.7 (3.85) | 25.6 (5.5) | 2,208 (n=741) | Mean BES score: 8.7 (6.8) | Undergraduate women recruited from a large,
public university in the southeastern United States, No formal ED diagnosis |
BES EDDS EAT-26 |
Black women had higher BMI and were less
likely than White women to endorse eating disorder symptomatology, including body dissatisfaction. Current measures of disordered eating were developed and validated with primarily White samples, and may overemphasize risk factors such as dieting, body dissatisfaction, and internalization of the thin-ideal, which may not be as relevant for Black women. |
| Lydecker et al., 2016^ | Cross-sectional study | 45.3 (9.8) | 38.5 (6.9) | 238 (n=119; 83.2% female) |
EDE: OBE: 21.2 (16.3) SBE: 9.2 (16.0) OOE: 3.3 (6.6) EDE-Q OBE: 12.0 (8.3) SBE: 5.7 (7.8) OOE: 15.5 (10.7) |
Participants were treatment-seeking adults with DSM-IV-TR defined BED | EDE EDE-Q SCID-IV |
EDE and EDE-Q scores are correlated on BE,
eating disorder psychopathology scales, and weight
variables. Correlations were similar between Black and White patients. |
| Lydecker & Grilo, 2016^ | Cross-sectional study | 45.4 (.89) | 40.2 (SE=.59) | 775 (n=100; 82.6% female) |
Mean (SE) OBE: 21.6 (1.1) EDE global score: 2.7 (.08) Restraint: 1.8 (.12) Eating: 1.9 (.12) Shape: 3.7 (.10) Weight: 3.2 (.09) |
Treatment-seeking adults with
DSM-IV–defined BED who self-identified as Black, Hispanic, or
White |
EDE | Black participants had a higher BMI, and
reported more frequent binge eating episodes compared to White
participants. ED psychopathology did not differ across racial/ethnic groups. Developmental trajectory of BED is more rapid for Black participants than White participants |
| Lydecker et al., 2019^ | Secondary data analysis of randomized clinical trials | 46.4 (9.6) | 37.6 (6.2) | 592 (n=93; 82.3% female) | Mean BE frequency: 11.45 (8.0) |
Participants were patients in psychological and pharmacological RCTs for BED | SCID EDE EDE-Q |
Black participants had fewer-BE episodes and
had less depression Greater proportion of Black participants achieved BE remission across time points Lower % of Black participants achieved WL |
| Mama et al., 2015 | Secondary data analysis of randomized clinical trial | 47.2 (8.4) | 34.7 (8.0) | 180 (n=131) | NR | Community-based recruitment of Black and
Hispanic women from Houston, TX Participated in two-arm lifestyle intervention: 1) physical activity; 2) dietary habits |
BES | Over 1/4 (27.8%) of participants were
classified as binge eaters at baseline. Women classified as binge eaters who participated in the physical activity intervention reported greater decreases in BES score than non-binge eaters in the dietary habits intervention. |
| Marcus et al., 2007 | Secondary data analysis of population-based longitudinal study | 45.7 (2.5) | 31.3 (7.1) | 589 (n=157) | NR | Participants from the Study of Women’s Health across the Nation (SWAN) | Bulimia Test-Revised (BULIT-R) | Nearly 13.4% of Black women endorsed use of
vigorous exercise, strict dieting, and/or purging to keep from gaining
weight. Black women had significantly higher BE scores than did Hispanic women, and similar scores to White women. |
| Marques et al., 2011^ | Secondary data analysis of population-based study | NR | NR | 11,222 (n= 5,381; % female NR) | 1.5% (SE=.24) lifetime BED prevalence | Pooled data from the NIMH Collaborative
Psychiatric Epidemiological Studies Examined 12-month and lifetime prevalence of 12-month and lifetime prevalence of AN, BN, and any binge eating |
WMH-CIDI | Lifetime prevalence of any binge eating was greater and mental health service utilization was less in Black participants (overall, and by gender) in comparison to Non-Hispanic, Whites. |
| Mazzeo et al., 2005 | Cross-sectional study | 39.9 (10.8) | 47.9 (7.9) | 388 (n=147) | BES: 22.8 (9.7) Met criteria for BED: 33.3% Severe Binge Eaters: 35.8% |
All participants were bariatric candidates | QEWP BES |
Black women had higher BMIs, higher
self-esteem, and less depression than White women. There were no significant racial differences in rates of binge eating or BED. |
| Mitchell & Mazzeo, 2004 | Cross-sectional study | 20.4 (5.3) | 26.2 (5.8) | 259 (n = 73) | Mean BES: 7.8 (6.9) | Community-based sample | EDDS BES |
Depression, anxiety, and alexithymia
associated with BES scores No significant difference in BE prevalence between Black and White women |
| Munn-Chernoff et al., 2015 | Secondary data analysis of population-based longitudinal study | Median = 22 years (range = 19–24 years) | NR | 3755 (n=547) | 10.23% of Black women reported any lifetime overeating (OE) or BE | Participants were part of the Missouri Adolescent Female Twin Study | Lifetime Overeating-Binge Eating (OE-BE) was based on the endorsement of two questions | No significant differences in overeating or BE in Black (10.2%) compared with White women (7.4) (p=.07). |
|
Pike et al.,
2001 |
Case-control study | 31.4 (5.7) | 36.3 (7.4) | 150 (n=52) |
Binges/week: 6.0 (4.2) | Participants recruited as part of the New
England’s Health Study 150 women with BED matched with community-based sample of 150 women without BED. |
SCID EDE EDE-Q |
Black women had significantly higher binging
episodes per week, 5.99 v. 3.88 [F=15.7, df = 1, 148, p <.001]. Black women significantly less likely than White women to be treated for BED [7.7% (n=4) vs. 22.4% (n=22); X2 = 5.2; p < .03). |
| Scott et al., 2018 | Qualitative Research | 38.1 (12.5) | 36.1 (12.7) | 16 (100%) | Reported 5.3 (5.0) binge eating episodes in
the last 28-day period EDE-Q Total Score= 3.2 (0.9) |
Recruited from local university and community organizations in two southeastern urban areas | EDE-Q | Nearly one-quarter of participants felt they
had never had a problem with eating. While several participants
currently (37.5%; n = 6) or previously (37.5%; n = 6) wanted help for
eating problems, only one individual had ever received any treatment for
an eating concern. Key focus group theme revealed lack of awareness of BE and BED. |
| Smith et al., 1998^ | Secondary data analysis of population-based longitudinal study | 34.5 (3.9) | 30.0 (7.9) | 5,115 (n=1101; 65% female); | Prevalence of BED = 2.2% | Participants from the Coronary Artery Risk Development in Young Adults (CARDIA) Study | QEWP-R | Comparable rates of BED in Black (2.2%) and White women (2.0%), despite substantial differences in obesity and depression between these groups. |
| Shuttlesworth & Zotter, 2011 | Cross-sectional study | 20.0 (4.0) | NR | 301 (n=119) HBCU: 88 (100%) PWU: 213 (n=31) |
HBCU (Black): BES: 24.0 (7.0) EAT-26: 52.1 (14.5) |
Undergraduate students from a) mid-Atlantic,
historically Black, public university; b) mid-Atlantic, predominately White, public university |
BES EAT-26 |
Low levels of ethnic identity represent a risk factor and increase the likelihood of binge eating and bulimic pathology. |
| Striegel-Moore et al., 2000 | Cross sectional study | 28.3 (5.0) | 27.0 (6.0) | 7369 (n=1628) | Binge eating at least once in the last 3
months: 8.4% (n=136) |
Community sample of Black and White women recruited from Northeastern United States participating in a telephone survey. | EDE | Black women were as likely as White women to
report that they had engaged in the behaviors of binge eating and
self-induced vomiting during the preceding 3 months. In addition, more Black women than White women reported that they had used laxatives, diuretics, or fasting to control their weight. Almost twice as many Black women as White women were identified as probable eating disorder cases. |
| Striegel-Moore, et al., 2002 | Case-Control Study | 30.1 (5.8) | NR | 520 (n = 166) | NR | Participants from the New England Women’s Health Project | EDE | All categories of physical abuse, reports of being bullied by peers, and reports of sexual abuse and repeated sexual abuse were more common among Black women with BED than Black women in healthy and psychiatric groups. |
| Striegel-Moore et al., 2003 | Secondary data analysis from a population-based longitudinal study | 21.5 (0.7) | NR | 2046 (n=1,061) | BED prevalence in the sample: 1.4% (n=27) |
Participants were recruited from the 10-year longitudinal NHLBI Growth and Health Study. | Screening Interview for Eating
Disorder EDE SCID-IV |
Significantly less Black women met criteria
for BED than White women. Among those who reported a history of ED (n=76), few women ever received treatment: B (n=1); W (n=16). |
| Striegel-Moore et al., 2005 | Case-control study | 30.7 (6.0) | 36.7 (9.3) | 162 (n=60) | NR | Participants from the New England Women’s Health Project, sampled to determine risk factors for BED in a community sample of Black and White women. | SCID EDE |
Childhood obesity and familial eating problems
are specific risk factors for BED. Race did not moderate risk for BED. |
| Taylor et al., 2007^ | Secondary data analysis of population-based study | NR | NR | 5191 (100%) | Lifetime prevalence of any BE: (n=174;
5.8%) 12-month prevalence of any BE: (n=84; 1.5%) |
Participants from the National Survey for
American Life (NSAL) |
WMH-CIDI-WHO | Binge eating was the most prevalent eating
disorder among adults and adolescents. The average age of onset for BE was significantly higher than AN. Women had higher lifetime prevalence of any binge eating and 12-month prevalence of BN, and BED than men. |
| Thompson-Brenner et al., 2013^ | Secondary analysis of randomized controlled trials | NR | NR | 1073 (n=78) 85% of sample was female |
Baseline: OBE: 19.6 (Range: 16.9, 22.2) Post-treatment OBE 4.8 (Range: 2.6, 7.1) |
Data aggregated from eleven, randomized, controlled trials of psychosocial treatments for BED | EDE | Black participants were more likely to drop
out than White participants. (OR = 2.3, p <.01) Black participants demonstrated a greater reduction in EDE global score, compared to White participants (d = .21, p <.05). |
| Udo et. al., 2016 | Cross Cross-sectional study |
43.6 (10.7) | 39.3 (6.0) | 109 (n=56) | OBE: 17.4 (13.7) SBE: 9.9 (13.8) OOE: 4.4 (9.1) |
articipants were obese (BMI ≥ 30
kg/m 2 ) and m et DSM-5 criteria thresholds for BED Participants responded to advertisements for treatment and had obesity (BMI greater than 30) and met the DSM-5 criteria thresholds for BED |
EDE | Caucasian women reported
significantly earlier onset of becoming overweight, beginning binge eating, and dieting, and a greater number of times on a diet Black women reported significantly later onset of becoming overweight, beginning binge eating and dieting, and 50% less times being on a diet, compared to White women. No significant difference in by race in ED psychopathology |
| Wilson et al., 2012 | Secondary data analysis of cross-sectional data | 45.8 (9.2) | 34.5 (9.2) | 283 (n=192) | NR | Recruited to the HIP study through media, brochures, churches, and internet communication. | BES | Higher BMI was associated with increased fat
consumption and binge eating. Negative correlation between BES scores and fruit consumption. |
Black men were also included in the sample.
BE = Binge Eating; BED = Binge Eating Disorder; AN = Anorexia Nervosa; BN = Bulimia Nervosa; ED= Eating Disorder; NR= not reported; OBE = Objective Bulimic Episode; SBE = Subjective Bulimic Episode; OOE = Objective Overeating; ES = Effect Size; BES = Binge Eating Scale; EDE = Eating Disorder Examination; EDE-Q = Eating Disorder Examination-Questionnaire; SCID = Structured Clinical Interview for DSM-IV; EAT-26 = Eating Attitudes Test; QEWP-R = Questionnaire on Eating and Weight Patterns-Revised ; WMH-CIDI or WHO-CIDI = World Health Organization Composite International Diagnostic Interview
Risk of Bias in Individual Studies.
We conducted a quality rating to assess the risk of bias in individual studies that met eligibility criteria by using the Kmet form for quantitative analysis (Kmet, Lee, & Cook, 2004). This tool assesses the quality of studies on 11 different criteria in relation to the study design, methods, reporting of results, and study conclusions. For each criteria, every study was given a score of 0, 1, or 2, with a maximum score of 22 (see supporting information 1).
Results
Fifty-seven articles met the outlined inclusion criteria. Nineteen of these were subsequently excluded due to the lack of a BE outcome (n = 9), patient population (e.g., not reporting outcomes in Black women) (n = 9), and study design (n = 1). In total, 38 studies were included in the systematic review. Studies were summarized based on the following categories: authors, study aim/design, sample size/characteristics, BE measurement, and outcomes related to BE (Table 1).
Participants of Included Studies
Among all 38 included studies, sample sizes ranged from 16 to 11,222, and percentage of included Black women varied (ranging from 7–40% (n = 18), and ≥40%, n = 20). Participants’ mean age was 35.3 years (SD=9.6), and mean Body Mass Index (BMI) was 34.4 kg/m2 (SD=7.1). Of the studies that reported BMI (n=29), two (7%) included participants with a mean BMI < 25 kg/m2, six studies (21%) had participants with a mean BMI > 25–30 kg/m2, and the remaining 21 articles (72%) included participants with a mean BMI ≥30 kg/m2. Recruited participants included those from clinical settings (n = 5), community-based samples (n = 18), or undergraduate student populations (n = 7).
Design of Included Studies
Most studies reported cross-sectional findings (n = 17; 44.7%) (Azarbad, Corsica, Hall, & Hood, 2010; Cachelin, Rebeck, Veisel, & Striegel-Moore, 2001; Fitzgibbon et al., 1998; Gayle, Fitzgibbon, & Martinovich, 2004; Harrington, Crowther, Henrickson, & Mickelson, 2006; Harrington, Crowther, & Shipherd, 2010; Higgins, Lin, Alvarez, & Bardone-Cone, 2015; Hrabosky & Grilo, 2007; Jarosz, Dobal, Wilson, & Schram, 2007; Kelly, Cotter, & Mazzeo, 2012; Lydecker & Grilo, 2016; Lydecker, White, & Grilo, 2016; Mazzeo et al., 2005; Mitchell & Mazzeo, 2004; Shuttlesworth & Zotter, 2011; Striegel-Moore et al., 2000; Udo et al., 2016). Additional studies included secondary data analyses of cross-sectional data (n = 3; 7.8%) (Adamus-Leach et al., 2013; Kelly, Mitchell, et al., 2012; Wilson et al., 2012), secondary data analyses of population-based longitudinal studies (n=4; 10.5%) (Marcus, Bromberger, Wei, Brown, & Kravitz, 2007; Munn-Chernoff et al., 2015; Smith, Marcus, Lewis, Fitzgibbon, & Schreiner, 1998; Striegel-Moore et al., 2003); secondary analyses of large, representative data sets of Black respondents (n = 4; 10.5%) (Assari, 2018; Blostein, Assari, & Caldwell, 2017; Marques et al., 2011; Taylor et al., 2007), and secondary analyses of RCT’s (n = 3; 7.8%) (Lydecker, Gueorguieva, Masheb, White, & Grilo, 2019; Mama et al., 2015; Thompson-Brenner et al., 2013). The remaining studies were: (a) a focus group study (Scott et al., 2018); (b) case-control design studies (n = 4; 10.3%) (Grilo et al., 2005; Pike et al., 2001; Striegel-Moore, Dohm, Pike, Wilfley, & Fairburn, 2002; Striegel-Moore et al., 2005); and (c) randomized clinical trials (n = 2; 5.3%) examining the change in BE over time (Goode, Kalarchian, Craighead, Conroy, Wallace, et al., 2018; Grilo et al., 2014).
Binge-Eating Measures Used
To assess the prevalence and severity of BE among Black women, investigators frequently used the Eating Disorder Examination (EDE) (n = 14) (Fairburn & Cooper, 1993), Binge Eating Scale (n = 13) (Gormally, Black, Daston, & Rardin, 1982), Eating Disorder Examination – Questionnaire (EDE-Q) (Celio, Wilfley, Crow, Mitchell, & Walsh, 2004) (n = 8), and the Structured Clinical Interview for DSM-IV (n = 7) (First, Spitzer, Gibbon, & Williams, 2002). Other less commonly used measures included the Questionnaire on Eating and Weight Patterns-Revised (Spitzer, Yanovski, & Marcus, 1994) (n = 6), and the World Health Organization Composite International Diagnostic Interview (Kessler & Ustun, 2004) (n = 3).
Prevalence of BE and BED
In total, 30 of the 38 studies (79%) reported information on the prevalence of BE and/or BED among Black participants (Adamus-Leach et al., 2013; Assari, 2018; Azarbad et al., 2010; Fitzgibbon et al., 1998; Gayle et al., 2004; Goode, Kalarchian, Craighead, Conroy, Wallace, et al., 2018; Grilo et al., 2005; Harrington et al., 2006; Harrington et al., 2010; Higgins et al., 2015; Hrabosky & Grilo, 2007; Kelly, Cotter, et al., 2012; Kelly, Mitchell, et al., 2012; Lydecker & Grilo, 2016; Lydecker et al., 2016; Marques et al., 2011; Mazzeo et al., 2005; Mitchell & Mazzeo, 2004; Munn-Chernoff et al., 2015; Pike et al., 2001; Scott et al., 2018; Shuttlesworth & Zotter, 2011; Smith et al., 1998; Striegel-Moore et al., 2003; Striegel-Moore et al., 2002; Striegel-Moore et al., 2000; Taylor et al., 2007; Thompson-Brenner et al., 2013; Wilson et al., 2012). In studies that reported BE prevalence in Black women, estimates ranged from 1.5–36% (Kelly, Mitchell, et al., 2012; Mazzeo et al., 2005; Scott et al., 2018; Striegel-Moore et al., 2000; Taylor et al., 2007). In addition, BED prevalence ranged from .06% - 2.2% (Assari, 2018; Marques et al., 2011; Smith et al., 1998; Striegel-Moore et al., 2003). Seven of the 30 studies (23%) reported no significant differences in the prevalence of BE between Black and White participants (Fitzgibbon et al., 1998; Gayle et al., 2004; Grilo et al., 2005; Marcus et al., 2007; Mazzeo et al., 2005; Mitchell & Mazzeo, 2004; Udo et al., 2016). In contrast, five of the 30 studies (17%) indicated that White women had significantly higher BE or lifetime BED prevalence than Black women (Azarbad et al., 2010; Harrington et al., 2006; Kelly, Mitchell, et al., 2012; Lydecker et al., 2019; Striegel-Moore et al., 2003) and four of the 30 studies (13%) reported that Black women had a significantly higher prevalence of BE than White women (Lydecker & Grilo, 2016; Marques et al., 2011; Pike et al., 2001; Striegel-Moore et al., 2000).
Racial Differences in the Nature and Course of Eating Disorder Psychopathology
Nine studies examined racial differences in eating disorder pathology (e.g., concerns about weight, shape, restraint, as measured by the EDE) (Blostein et al., 2017; Grilo et al., 2005; Hrabosky & Grilo, 2007; Kelly, Cotter, et al., 2012; Kelly, Mitchell, et al., 2012; Lydecker & Grilo, 2016; Shuttlesworth & Zotter, 2011; Striegel-Moore et al., 2000; Udo et al., 2016). In four of the nine studies (44%), no racial differences in ED psychopathology were observed, and Black and White women reported similar concerns about weight, shape, and eating (Grilo et al., 2005; Lydecker & Grilo, 2016; Striegel-Moore et al., 2000; Udo et al., 2016). For example, in one study, Black women were as likely as White women to report BE and self-induced vomiting during the previous 3 months (Striegel-Moore et al., 2000). However, two of the nine studies (22%) found that Black participants were less likely to report eating disorder symptomatology, including engaging in regular subjective BE (i.e., sense of loss of control but the amount of food was not unusually large), self-induced vomiting, and laxative/diuretic misuse) (Kelly, Cotter, et al., 2012; Kelly, Mitchell, et al., 2012). In two other studies (22%), few racial differences in the clinical presentation of eating disorder symptomatology emerged; however Black women did have higher BMIs compared with Non-Hispanic, White women (Grilo et al., 2005; Lydecker & Grilo, 2016).
Age of BE and BED Onset
There were five studies that examined the age of onset of BE and/or BED among Black women. In three of the five studies (60%), investigators reported significant differences in the age of onset for BE in Black women compared with White women (Lydecker & Grilo, 2016; Striegel-Moore et al., 2005; Udo et al., 2016). For example, in Udo et al. (2016) mean age of BE onset was 30.0 ± 13.3 years, compared with 22.7 ± 12.2 years for White women (p<.01). Similarly, Lydecker et al. (2016) reported the mean age of onset of BE to be 26.92 years (SE=1.22) (Black), compared with 22.46 years (SE =.54) (White) (p=.002). Three studies reported age of onset of BED (Lydecker & Grilo, 2016; Smith et al., 1998; Taylor et al., 2007), with ages ranging from 18–28.5 years for Black individuals, compared to 14–26.7 (.58) years for those identifying as White.
Factors Associated with BE
Thirteen studies investigated correlates of BE in Black women (Adamus-Leach et al., 2013; Assari, 2018; Azarbad et al., 2010; Blostein et al., 2017; Harrington et al., 2006; Harrington et al., 2010; Higgins et al., 2015; Mazzeo et al., 2005; Mitchell & Mazzeo, 2004; Shuttlesworth & Zotter, 2011; Striegel-Moore et al., 2002; Striegel-Moore et al., 2005; Wilson et al., 2012). Four of the 13 studies (31%) reported a positive association between depressive symptoms and BE (Adamus-Leach et al., 2013; Azarbad et al., 2010; Mazzeo et al., 2005; Mitchell & Mazzeo, 2004). Two of the 13 studies (15%) reported high levels of body shame and/or dissatisfaction were associated with increased binge eating (Blostein et al., 2017; Higgins et al., 2015). Additionally, higher levels of ethnic identity were associated with lower levels of BE in Black, undergraduate college women (Shuttlesworth & Zotter, 2011). Other factors positively associated with BE among Black women include perceived discrimination (Assari, 2018); physical and sexual abuse (Striegel-Moore et al., 2002); consumption of dietary fat (r=.23) (Wilson et al., 2012); trauma (r=.22) (Harrington et al., 2006); stress (r=.36) and discriminatory stress (r=.22) (Harrington et al., 2006); childhood obesity (d=.64) and family overeating/BE (d=.82) (Striegel-Moore et al., 2005).
Evidence-Based Treatments
Several treatment studies included Black participants, and either reported outcomes by race, or reported outcomes specifically in Black individuals. First, Grilo et al. (2014) examined the effectiveness of 4-month intervention of self-help CBT and an anti-obesity medication (sibutramine), alone and in combination, in a sample that included 36 Black participants (34.6% of the total sample) with BED. At the 6 month-follow-up only, participants randomized to the self-help CBT group had significantly lower binge-eating frequency. Self-help CBT and sibutramine did not demonstrate long-term effectiveness relative to placebo for treating BED, and there were no significant differences in BE outcomes between treatments by the end of the study (16-months). Race did not moderate or predict clinical outcomes.
Two published studies report outcomes in Black women in an RCT targeting BE (Goode, Kalarchian, Craighead, Conroy, Wallace, et al., 2018; Mama et al., 2015). In the first, Mama et al. (2015) examined the effectiveness of a lifestyle intervention (physical activity vs. dietary habits) to reduce BE symptoms in a sample of predominately Black women (N=310; 84.8% Black). Participants in both groups completed six intervention sessions over a 24-week period. In addition to receiving intervention content on personal goal setting, reducing barriers, and increasing self-efficacy and support, participants in the physical activity group walked for 15-minutes as a group together. Those in the fruit and vegetable group sampled two new vegetables or fruits prepared by the research team (Lee et al., 2011). BE was not explicitly discussed during the intervention. At baseline, 27.8% of participants reported BE, and at the post-intervention assessment (24 months), those randomized to the physical activity group reported greater decreases in BE than those in the dietary habits group.
In the second study, Goode, Kalarchian, Craighead, Conroy, Wallace, et al. (2018) examined the feasibility and acceptability of an 8-week Appetite Awareness Treatment (AAT), a cognitive-behavioral intervention to treat BE, in a sample (n=31) of Black women with overweight and obesity (BMI=25–40 kg/m²) and with moderately severe BE behavior. Participants were randomized to AAT or a wait-list control group. Overall, retention was high (88%), and women randomized to AAT showed significantly reduced BE and improved self-efficacy for weight loss at 8 weeks compared to controls (Goode, Kalarchian, Craighead, Conroy, Wallace, et al. (2018).
Access and Participation in Treatment for BE, BED, and disordered eating behaviors
Five studies examined rates of access and treatment participation for BE and disordered eating among Black women (Cachelin et al., 2001; Marques et al., 2011; Pike et al., 2001; Striegel-Moore et al., 2003; Thompson-Brenner et al., 2013). In one of the five studies (20%), no significant differences were observed in treatment seeking among racial/ethnic groups (Black, White, Hispanic, Asian) (Cachelin et al., 2001). In contrast, in three of the five studies (60%), Black women were less likely to seek treatment for eating disorders than Non-Hispanic, White women (Marques et al., 2011; Pike et al., 2001; Striegel-Moore et al., 2003). For example, Marques et al. (2011), reported that mental health service utilization was significantly lower among Black women than Non-Hispanic, White women with a lifetime history of any eating disorder. Additionally, less than 8% of Black women with BED sought treatment, compared to approximately 22% of White women with BED (Pike et al., 2001; Scott et al., 2018). Moreover, White women were nearly five times more likely than Black women to receive treatment for an eating disorder (Striegel-Moore et al., 2003). Furthermore, when engaged in psychosocial treatment trials for BED, data aggregated across 11 clinical trials indicated that Black participants were more than twice as likely as White participants to drop out of treatment (Thompson-Brenner et al., 2013).
Methodological Limitations of the Current Literature
Several methodological limitations are present in the existing literature examining BE in Black women. First, the considerable variability in assessment tools used to measure BE challenged our ability to compare the prevalence of this behavior across studies. Within our review, eleven measures were used to examine BE outcomes. Because these measures were validated in samples primarily consisting of White women, there is a risk of not characterizing eating disorder symptoms and risk factors as accurately in Black women (Kelly, Mitchell, et al., 2012). For example, several studies have reported that, compared with White women, Black women may experience less subjective distress and shame related to engagement in BE behaviors (Franko, Becker, Thomas, & Herzog, 2007; Napolitano & Himes, 2011). This racial difference might be due to the presence of cultural norms that may permit eating larger portions of food and/or using food for emotional coping (Beauboeuf-Lafontant, 2003; Goode, Kalarchian, Craighead, Conroy, Gary-Webb, et al., 2018). The experience of marked distress is a key diagnostic criterion for BED (American Psychiatric Association, 2000, 2013); if Black women indicate binge-eating behavior, yet also indicate the absence of marked distress, which may be influenced by cultural factors and norms, their eating pathology might be mischaracterized or underestimated. Further investigation of these eating patterns and cultural considerations in the diagnosis of BED among Black women is warranted (Napolitano & Himes, 2011).
Additionally, Kelly et al. examined the construct validity of several eating disorder measures (e.g., Binge Eating Scale (BES) (Gormally et al., 1982), Eating Disorder Diagnostic Scale (Stice, Telch, & Rizvi, 2000), Eating Attitudes Test-26 (Garner, Olmsted, Bohr, & Garfinkel, 1982), and discovered that although most yielded internally consistent scores across Black and White women, there was a subset of measures (including the BES) which factor analyses suggested were assessing different underlying constructs. Moreover, some specific items on these measures were endorsed by Black women at lower rates than White women (Kelly, Mitchell, et al., 2012). Similarly, an investigation of racial differences in EDE-Q norms indicated that, although Black and White women obtained similar scores, Black women endorsed significantly less BE and compensatory behavior (Kelly, Cotter, et al., 2012). Recent evidence, however, suggests similarities between the EDE and the EDE-Q scores in Black women with BED and White women with BED (Lydecker et al., 2016). In total, these studies indicate further research is warranted to enhance our understanding of the optimal approach to the assessment of disordered eating in Black women.
Many of the studies included in this review used cross-sectional survey methodology, and although the EDE was used frequently to assess BE, self-report measures were often used to assess BE (e.g., BES, EDE-Q). Using the BES as a self-report measurement for BE has limitations. Evidence suggests that the BES might provide an accurate screening for BED, but appears to have less accuracy than the EDE-Q in identifying the severity of binge eating episodes (Celio et al., 2004; Mama et al., 2015). Also, it does not address binge eating frequency. Finally, to the best of our knowledge, and as included within this review, very few published studies report intervention outcomes specific to BE in Black women (Goode, Kalarchian, Craighead, Conroy, Wallace, et al., 2018; Mama et al., 2015).
Discussion
We systematically reviewed the literature on the prevalence of BE and BED among Black women, the nature and course of binge-eating pathology, factors that may influence BE in this population, possible evidence-based treatments, and access and participation in treatment for BE and BED. Most research on BE and BED has focused on White women, with Black individuals underrepresented in clinical trials (Cachelin et al., 2001). Many disparities exist in access to treatment and retention; moreover, little intervention research has examined best practices for treating BE in the Black patient population (Grilo et al., 2005; Marques et al., 2011; Pike et al., 2001; Thompson-Brenner et al., 2013).
Prevalence of BE and BED in Black Women
Our results indicate that the prevalence of BE and BED among Black women is similar and/or higher than that has been observed in White women (Grilo et al., 2005; Jarosz et al., 2007; Mazzeo et al., 2005). Although some have suggested that Black women might be protected from disordered eating due to cultural norms permitting larger body sizes (Williamson, 1998), ample evidence now suggests that BE in particular, occurs across racial and ethnic lines (Alegria et al., 2007; Marques et al., 2011). Because BED is associated with numerous comorbid health conditions, including severe obesity (Hales, Carroll, Fryar, & Ogden, 2017), its prevention and treatment is of paramount importance.
Nature and Course of Eating Disorder Pathology
Results of this review also highlight that few studies have identified racial differences in eating disorder psychopathology and concerns about shape, weight, and eating (Grilo et al., 2005; Lydecker & Grilo, 2016; Striegel-Moore et al., 2000; Udo et al., 2016). Indeed, while Black women were more likely to have higher BMIs, and less likely to engage in self-induced vomiting, and/or laxative/diuretic misuse (correlates of BE) (Grilo et al., 2005; Kelly, Mitchell, et al., 2012; Lydecker & Grilo, 2016), eating disorder psychopathology levels overall were similar to those observed in White women. These similarities, along with the results of prior research (Franko et al., 2012; Lydecker & Grilo, 2016; Lydecker et al., 2019; Thompson-Brenner et al., 2013), might provide additional support for the use of established treatments for BED to be examined in samples of Black participants. However, due to the documented challenges with the recruitment, engagement, and retention of Black participants in BED treatment studies, (Cachelin et al., 2001; Marques et al., 2011; Thompson-Brenner et al., 2013) adjustments in the setting, recruitment strategy, and the incorporation of relevant sociocultural factors might be necessary to facilitate Black women’s access to appropriate care (Scott et al., 2018).
Factors Affecting Development of BE
Although a nascent literature has identified factors affecting the development of BE in Black women, many questions remain. For example, although we have some evidence to suggest that trauma exposure and distress might be significant predictors of BE severity (Harrington et al., 2006; Harrington et al., 2010), limited information exists on the conditions, risk factors, and pathways that might moderate this relation (Harrington et al., 2010). Furthermore, evidence also suggests the presence of alternative mechanisms affecting the disordered eating behaviors of Black women; for example, compared with White women with BED, Black women with BED report lower levels of dietary restraint, weight bias, and concern about their shape and weight (Barnes, Ivezaj, & Grilo, 2014; Pike et al., 2001; Scott et al., 2018). In sum, there remains a need for research investigating the experiences of Black women with BE, to enhance our ability to design culturally sensitive interventions.
Evidence-Based Treatment
Although intervention research conducted with Black women is scarce, two studies have offered promising results from different treatments: (1) behavioral interventions to increase physical activity and (2) Appetite Awareness Training, a cognitive-behavioral treatment to improve maladaptive eating behaviors (Goode, Kalarchian, Craighead, Conroy, Wallace, et al., 2018; Mama et al., 2015). Pilot evaluations of these interventions suggest that they have the potential to reduce BE and improve eating self-efficacy in this population. These studies were conducted using traditional, face-to-face, group-based interventions, and included samples in which at least 85% of the participants were Black. Both studies, however, examined the change in BE in a sample with mild to moderate BE severity based on BES scores, and did not explicitly include participants diagnosed with BED. Future research should examine the long-term potential of these and other interventions to reduce BE and to prevent and treat BED in Black women.
Access to and Participation in Treatment for BE and BED
Results from this systematic review highlight evidence suggesting that Black women are less likely than White women to seek eating disorder treatment, and even when engaged, are more likely to drop out (Becker, Franko, Speck, & Herzog, 2003; Cachelin et al., 2001; Marques et al., 2011; Thompson-Brenner et al., 2013). Though the reasons for these disparities are likely complex, further investigation of the factors associated with retention in treatment for BE/BED in this population might be helpful. In a recent feasibility trial that included Black women with BE behaviors, retention was nearly 90%; the authors report that scheduling intervention sessions in a familiar community location and in the evening might have contributed to study retention (Goode et al., 2018). Additionally, in focus groups following the feasibility trial, participants acknowledged the benefit of feeling support from the facilitator and other group members (Goode, Kalarchian, Craighead, Conroy, Gary-Webb, et al., 2018). Experiencing support while engaging in treatment for mental health or BE concerns might be particularly important for Black individuals; in previous research exploring the relation between ethnicity and mental health utilization, experiencing a positive alliance (e.g, feeling understood or heard by the therapist) was significantly associated with increased session completion in Black participants (Bender et al., 2007). Additional research on the factors influencing BE/BED treatment retention and drop-out among Black women is needed.
Racial stereotyping might also contribute to disparities in treatment seeking for BE; several studies have demonstrated that Black women are considered far less likely to be affected by eating disorders, and are less likely than Whites to receive a recommendation or referral for further evaluation or care, and/or to have been asked by their doctor about eating disorder symptoms (Becker et al., 2003; Gordon, Perez, & Joiner, 2002; Kelly, Mitchell, et al., 2012). Moreover, Black women might not be aware of BE and BED as clinical concerns. For example, in a recent focus group investigation in a sample of Black women with BED, participants were surprised that BE is considered disordered eating, and were unaware that their eating concerns met diagnostic criteria for BED (Scott et al., 2018). Indeed, Black women have reported experiencing cultural norms that encourage them to eat larger portions and not to waste food (Beauboeuf-Lafontant, 2003; Goode, Kalarchian, Craighead, Conroy, Gary-Webb, et al., 2018). In addition, Black women have acknowledged that within their cultural group, it is considered acceptable to use food to cope with negative emotions (Beauboeuf-Lafontant, 2003; Goode, Kalarchian, Craighead, Conroy, Gary-Webb, et al., 2018). Further research is needed to identify and evaluate strategies for increasing BED awareness, and mitigating racial biases in the identification of eating disorder symptoms in Black women.
Methodological Limitations of the Current Literature
Results of this review highlight the great variability in assessment tools for the measurement of BE and BED, and raise some concern about their construct validity for Black women. Moreover, the presentation of disordered eating might differ across cultural boundaries. For example, marked distress (a current DSM-5 diagnostic criteria for BED) does not appear to co-occur with BE in Black women as frequently as it does in White women (Napolitano & Himes, 2011). Furthermore, evidence suggests that emotional overeating and/or obesity, which have been associated with BE frequency and severity, might warrant consideration as early symptoms of BED in Black women (Masheb & Grilo, 2006; Taylor et al., 2013). Indeed, Black women have the highest rates of obesity of any racial and ethnic group in the U.S. (Hales et al., 2017), and experience cultural norms that may permit the use of food as a coping technique for negative emotions (Beauboeuf-Lafontant, 2003; Taylor et al., 2013; Willig, Richardson, Agne, & Cherrington, 2014). Additionally, because obesity onset generally precedes the development of BED (Lydecker & Grilo, 2016), increasing providers’ awareness of emotional eating and obesity as potential BED correlates might enhance treatment access for this population.
Limitations
Due to the lack of a consistent measure of BE and associated factors across studies, we were unable to conduct a meta-analysis. Moreover, due to the reliance on self-report measures to assess BE in most studies, social desirability might have influenced the accuracy of reported BE and other disordered eating behaviors. Additional limitations include the exclusion of grey literature, and the exclusion of studies not published in English.
Conclusion
This systematic review supports the finding that Black women experience BE and BED at rates similar to those observed in White women. Moreover, few differences in eating disorder psychopathology and concerns about shape, weight, eating, were noted between racial groups. Limited evidence-based treatment for BE and BED has been evaluated in Black women, and future research is needed to examine additional factors associated with disordered eating behaviors. Additionally, due to continued disparities in the referral and access to treatment for BE and BED, psychoeducation on the symptoms of BE and BED, and adjustments in recruitment, engagement, intervention methods, and treatment settings are likely needed to provide Black women with access to adequate levels of care. Furthermore, due to the well-documented disparities in obesity [e.g., 82% of Black women are affected by overweight or obesity (Hales et al., 2017; Ogden, Carroll, Fryar, & Flegal, 2015)], more than adequate justification exists for additional research to develop, implement, and evaluate interventions targeting the prevention and treatment of BED in this population.
Supplementary Material
ACKNOWLEDGMENTS:
RWG would like to acknowledge financial support from the Feeding Hope Fund for Clinical Research, National Eating Disorders Association and from the Nutrition and Obesity Research Center, University of North Carolina at Chapel Hill (DK056350). RWG and CMB also acknowledge support from H79 SM081924. CMB also acknowledges R34MH113681.
References
- Adamus-Leach HJ, Wilson PL, O’Connor DP, Rhode PC, Mama SK, & Lee RE (2013). Depression, stress and body fat are associated with binge eating in a community sample of African American and Hispanic women. Eating and Weight Disorders, 18(2), 221–227. doi: 10.1007/s40519-013-0021-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Woo M, Cao Z, Torres M, Meng XL, & Striegel-Moore R (2007). Prevalence and correlates of eating disorders in Latinos in the United States. International Journal of Eating Disorders, 40 Suppl, S15–21. doi: 10.1002/eat.20406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., Text Revision). Washington, DC. [Google Scholar]
- American Psychiatric Association. (2013). Feeding and Eating Disorders. In Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC. [Google Scholar]
- Assari S (2018). Perceived Discrimination and Binge Eating Disorder; Gender Difference in African Americans. Journal of Clinical Medicine, 7(5). doi: 10.3390/jcm7050089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azarbad L, Corsica J, Hall B, & Hood M (2010). Psychosocial correlates of binge eating in Hispanic, African American, and Caucasian women presenting for bariatric surgery. Eating Behaviors, 11(2), 79–84. doi: 10.1016/j.eatbeh.2009.10.001 [DOI] [PubMed] [Google Scholar]
- Barnes RD, Ivezaj V, & Grilo CM (2014). An examination of weight bias among treatment-seeking obese patients with and without binge eating disorder. General Hospital Psychiatry, 36(2), 177–180. doi: 10.1016/j.genhosppsych.2013.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauboeuf-Lafontant T (2003). Strong and large black women? Exploring relationships between deviant womanhood and weight. Gender & Society, 17(1), 111–121. [Google Scholar]
- Becker AE, Franko DL, Speck A, & Herzog DB (2003). Ethnicity and differential access to care for eating disorder symptoms. International Journal of Eating Disorders, 33(2), 205–212. doi: 10.1002/eat.10129 [DOI] [PubMed] [Google Scholar]
- Bender DS, Skodol AE, Dyck IR, Markowitz JC, Shea MT, Yen S, … Grilo CM (2007). Ethnicity and mental health treatment utilization by patients with personality disorders. Journal of Consulting and Clinical Psychology, 75(6), 992–999. doi: 10.1037/0022-006X.75.6.992 [DOI] [PubMed] [Google Scholar]
- Blostein F, Assari S, & Caldwell CH (2017). Gender and Ethnic Differences in the Association Between Body Image Dissatisfaction and Binge Eating Disorder among Blacks. Journal of Racial and Ethnic Health Disparities, 4(4), 529–538. doi: 10.1007/s40615-016-0255-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cachelin FM, Rebeck R, Veisel C, & Striegel-Moore RH (2001). Barriers to treatment for eating disorders among ethnically diverse women. International Journal of Eating Disorders, 30(3), 269–278. [DOI] [PubMed] [Google Scholar]
- Celio AA, Wilfley DE, Crow SJ, Mitchell J, & Walsh BT (2004). A comparison of the binge eating scale, questionnaire for eating and weight patterns-revised, and eating disorder examination questionnaire with instructions with the eating disorder examination in the assessment of binge eating disorder and its symptoms. International Journal of Eating Disorders, 36(4), 434–444. doi: 10.1002/eat.20057 [DOI] [PubMed] [Google Scholar]
- Fairburn CG, & Cooper Z (1993). The Eating Disorder Examination (12th ed). In Fairburn CG & Wilson GT (Eds.), Binge eating: Nautre, assessment, and treatment (pp. 333–360). New York: Guilford Press. [Google Scholar]
- First M, Spitzer R, Gibbon M, & Williams J (2002). Structured Clinical Interview for the DSM-IV TR Axis I Disorders, Research Version, Patient Edition. In N. Y. S. P. Institute (Ed.), Biometrics Research. New York. [Google Scholar]
- Fitzgibbon ML, Spring B, Avellone ME, Blackman LR, Pingitore R, & Stolley MR (1998). Correlates of binge eating in Hispanic, black, and white women. International Journal of Eating Disorders, 24(1), 43–52. [DOI] [PubMed] [Google Scholar]
- Franko DL, Becker AE, Thomas JJ, & Herzog DB (2007). Cross-ethnic differences in eating disorder symptoms and related distress. International Journal of Eating Disorders, 40(2), 156–164. doi: 10.1002/eat.20341 [DOI] [PubMed] [Google Scholar]
- Franko DL, Thompson-Brenner H, Thompson DR, Boisseau CL, Davis A, Forbush KT, … Wilson GT (2012). Racial/ethnic differences in adults in randomized clinical trials of binge eating disorder. Journal of Consulting and Clinical Psychology, 80(2), 186–195. doi: 10.1037/a0026700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner DM, Olmsted MP, Bohr Y, & Garfinkel PE (1982). The eating attitudes test: psychometric features and clinical correlates. Psychological Medicine, 12(4), 871–878. [DOI] [PubMed] [Google Scholar]
- Gayle JL, Fitzgibbon ML, & Martinovich Z (2004). A preliminary analysis of binge episodes: comparison of a treatment-seeking sample of Black and White women. Eating Behaivors, 5(4), 303–313. doi: 10.1016/j.eatbeh.2004.04.010 [DOI] [PubMed] [Google Scholar]
- Goode RW, Kalarchian MA, Craighead L, Conroy MB, Gary-Webb T, Bennett E, … Burke LE (2018). Perceptions and experiences of appetite awareness training among African-American women who binge eat. Eating and Weight Disorders. doi: 10.1007/s40519-018-0577-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goode RW, Kalarchian MA, Craighead L, Conroy MB, Wallace J Jr., Eack SM, & Burke LE (2018). The feasibility of a binge eating intervention in Black women with obesity. Eating Behaviors, 29, 83–90. doi: 10.1016/j.eatbeh.2018.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon KH, Perez M, & Joiner TE Jr. (2002). The impact of racial stereotypes on eating disorder recognition. International Journal of Eating Disorders, 32(2), 219–224. doi: 10.1002/eat.10070 [DOI] [PubMed] [Google Scholar]
- Gormally J, Black S, Daston S, & Rardin D (1982). The assessment of binge eating severity among obese persons. Addictive Behaviors, 7(1), 47–55. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Lozano C, & Masheb RM (2005). Ethnicity and sampling bias in binge eating disorder: Black women who seek treatment have different characteristics than those who do not. International Journal of Eating Disorders, 38(3), 257–262. doi: 10.1002/eat.20183 [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, White MA, Gueorguieva R, Barnes RD, Walsh BT, … Garcia R (2014). Treatment of binge eating disorder in racially and ethnically diverse obese patients in primary care: randomized placebo-controlled clinical trial of self-help and medication. Behavior Research Therapy, 58, 1–9. doi: 10.1016/j.brat.2014.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Wilson GT, Gueorguieva R, & White MA (2011). Cognitive-behavioral therapy, behavioral weight loss, and sequential treatment for obese patients with binge-eating disorder: a randomized controlled trial. Journal of Consulting and Clinical Psychology, 79(5), 675–685. doi: 10.1037/a0025049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales CM, Carroll MD, Fryar CD, & Ogden CL (2017). Prevalence of Obesity among Adults and Youth: United States, 2015–2016. (288). Retrieved from https://www.cdc.gov/nchs/data/databriefs/db288.pdf. [PubMed] [Google Scholar]
- Harrington EF, Crowther JH, Henrickson HC, & Mickelson KD (2006). The relationships among trauma, stress, ethnicity, and binge eating. Cultural Diversity and Ethnic Minority Psychology, 12(2), 212–229. doi: 10.1037/1099-9809.12.2.212 [DOI] [PubMed] [Google Scholar]
- Harrington EF, Crowther JH, & Shipherd JC (2010). Trauma, binge eating, and the “strong Black woman”. Journal of Consulting and Clinical Psychology, 78(4), 469–479. doi: 10.1037/a0019174 [DOI] [PubMed] [Google Scholar]
- Higgins MK, Lin SL, Alvarez A, & Bardone-Cone AM (2015). Examining impulsivity as a moderator of the relationship between body shame and bulimic symptoms in Black and White young women. Body Image, 14, 39–46. doi: 10.1016/j.bodyim.2015.03.007 [DOI] [PubMed] [Google Scholar]
- Hrabosky JI, & Grilo CM (2007). Body image and eating disordered behavior in a community sample of Black and Hispanic women. Eating Behaviors, 8(1), 106–114. doi: 10.1016/j.eatbeh.2006.02.005 [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG Jr., & Kessler RC (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry, 61(3), 348–358. doi: 10.1016/j.biopsych.2006.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson JI, Lalonde JK, Coit CE, Tsuang MT, McElroy SL, Crow SJ, … Pope HG Jr. (2010). Longitudinal study of the diagnosis of components of the metabolic syndrome in individuals with binge-eating disorder. American Journal of Clinical Nutrition, 91(6), 1568–1573. doi: 10.3945/ajcn.2010.29203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivezaj V, Kalebjian R, Grilo CM, & Barnes RD (2014). Comparing weight gain in the year prior to treatment for overweight and obese patients with and without binge eating disorder in primary care. Journal of Psychosometric Research, 77(2), 151–154. doi: 10.1016/j.jpsychores.2014.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarosz PA, Dobal MT, Wilson FL, & Schram CA (2007). Disordered eating and food cravings among urban obese African American women. Eating Behaviors, 8(3), 374–381. doi: 10.1016/j.eatbeh.2006.11.014 [DOI] [PubMed] [Google Scholar]
- Kelly NR, Cotter EW, & Mazzeo SE (2012). Eating Disorder Examination Questionnaire (EDE-Q): norms for Black women. Eating Behaviors, 13(4), 429–432. doi: 10.1016/j.eatbeh.2012.09.001 [DOI] [PubMed] [Google Scholar]
- Kelly NR, Mitchell KS, Gow RW, Trace SE, Lydecker JA, Bair CE, & Mazzeo S (2012). An evaluation of the reliability and construct validity of eating disorder measures in white and black women. Psychological Assessment, 24(3), 608–617. doi: 10.1037/a0026457 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, … Xavier M (2013). The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biological Psychiatry, 73(9), 904–914. doi: 10.1016/j.biopsych.2012.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, & Ustun TB (2004). The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal of Methods in Psychiatric Research, 13(2), 93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kmet LM, Lee RC, & Cook LS (2004). Standard quality assessment criteria for evaluating research papers from a variety of fields. Edmonton: Alberta Heritage Foundation for Medical Research. [Google Scholar]
- Lee RE, Medina AV, Mama SK, Reese-Smith JY, O’Connor DP, Brosnan M, … Estabrooks PA (2011). Health is Power: an ecological, theory-based health intervention for women of color. Contemporary Clinical Trials, 32(6), 916–923. doi: 10.1016/j.cct.2011.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, … Moher D (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ, 339, b2700. doi: 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lydecker JA, & Grilo CM (2016). Different yet similar: Examining race and ethnicity in treatment-seeking adults with binge eating disorder. Journal of Consulting and Clinical Psychology, 84(1), 88–94. doi: 10.1037/ccp0000048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lydecker JA, Gueorguieva R, Masheb R, White MA, & Grilo CM (2019). Examining race as a predictor and moderator of treatment outcomes for binge-eating disorder: Analysis of aggregated randomized controlled trials. Journal of Consulting and Clinical Psychology, 87(6), 530–540. doi: 10.1037/ccp0000404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lydecker JA, White MA, & Grilo CM (2016). Black patients with binge-eating disorder: Comparison of different assessment methods. Psychological Assessment, 28(10), 1319–1324. doi: 10.1037/pas0000246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mama SK, Schembre SM, O’Connor DP, Kaplan CD, Bode S, & Lee RE (2015). Effectiveness of lifestyle interventions to reduce binge eating symptoms in African American and Hispanic women. Appetite, 95, 269–274. doi: 10.1016/j.appet.2015.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus MD, Bromberger JT, Wei HL, Brown C, & Kravitz HM (2007). Prevalence and selected correlates of eating disorder symptoms among a multiethnic community sample of midlife women. Annals of Behavioral Medicine, 33(3), 269–277. doi: 10.1007/bf02879909 [DOI] [PubMed] [Google Scholar]
- Marques L, Alegria M, Becker AE, Chen CN, Fang A, Chosak A, & Diniz JB (2011). Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: Implications for reducing ethnic disparities in health care access for eating disorders. International Journal of Eating Disorders, 44(5), 412–420. doi: 10.1002/eat.20787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masheb RM, & Grilo CM (2006). Emotional overeating and its associations with eating disorder psychopathology among overweight patients with binge eating disorder. International Journal of Eating Disorders, 39(2), 141–146. doi: 10.1002/eat.20221 [DOI] [PubMed] [Google Scholar]
- Mazzeo SE, Saunders R, & Mitchell KS (2005). Binge eating among African American and Caucasian bariatric surgery candidates. Eating Behaviors, 6(3), 189–196. doi: 10.1016/j.eatbeh.2004.12.001 [DOI] [PubMed] [Google Scholar]
- Mitchell KS, & Mazzeo SE (2004). Binge eating and psychological distress in ethnically diverse undergraduate men and women. Eating Behaviors, 5(2), 157–169. doi: 10.1016/j.eatbeh.2003.07.004 [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & Group P (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med, 6(7), e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munn-Chernoff MA, Grant JD, Agrawal A, Koren R, Glowinski AL, Bucholz KK, … Duncan AE (2015). Are there common familial influences for major depressive disorder and an overeating-binge eating dimension in both European American and African American female twins? International Journal of Eating Disorders, 48(4), 375–382. doi: 10.1002/eat.22280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napolitano MA, & Himes S (2011). Race, weight, and correlates of binge eating in female college students. Eating Behaviors, 12(1), 29–36. doi: 10.1016/j.eatbeh.2010.09.003 [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Fryar CD, & Flegal KM (2015). Prevalence of Obesity Among Adults and Youth: United States, 2011–2014. NCHS Data Brief(219), 1–8. [PubMed] [Google Scholar]
- Pike KM, Dohm FA, Striegel-Moore RH, Wilfley DE, & Fairburn CG (2001). A comparison of black and white women with binge eating disorder. American Journal of Psychiatry, 158(9), 1455–1460. [DOI] [PubMed] [Google Scholar]
- Scott TN, Gil-Rivas V, & Cachelin FM (2018). The need for cultural adaptations to health interventions for African American women: A qualitative analysis. Cultural Diversity and Ethnic Minority Psychology. doi: 10.1037/cdp0000228 [DOI] [PubMed] [Google Scholar]
- Shuttlesworth ME, & Zotter D (2011). Disordered eating in African American and Caucasian women: the role of ethnic identity. Journal of Black Studies, 42(6), 906–922. [DOI] [PubMed] [Google Scholar]
- Smith DE, Marcus MD, Lewis CE, Fitzgibbon M, & Schreiner P (1998). Prevalence of binge eating disorder, obesity, and depression in a biracial cohort of young adults. Annals of Behavioral Medicine, 20(3), 227–232. doi: 10.1007/BF02884965 [DOI] [PubMed] [Google Scholar]
- Spitzer R, Yanovski S, & Marcus M (1994). Questionnaire on Eating and Weight Patterns, Revised. Retrieved from Pittsburgh, PA: [Google Scholar]
- Stice E, Telch CF, & Rizvi SL (2000). Development and validation of the Eating Disorder Diagnostic Scale: a brief self-report measure of anorexia, bulimia, and binge-eating disorder. Psychological Assessment, 12(2), 123–131. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Dohm FA, Kraemer HC, Taylor CB, Daniels S, Crawford PB, & Schreiber GB (2003). Eating disorders in white and black women. American Journal of Psychiatry, 160(7), 1326–1331. doi: 10.1176/appi.ajp.160.7.1326 [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Dohm FA, Pike KM, Wilfley DE, & Fairburn CG (2002). Abuse, bullying, and discrimination as risk factors for binge eating disorder. American Journal of Psychiatry, 159(11), 1902–1907. doi: 10.1176/appi.ajp.159.11.1902 [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Fairburn CG, Wilfley DE, Pike KM, Dohm FA, & Kraemer HC (2005). Toward an understanding of risk factors for binge-eating disorder in black and white women: a community-based case-control study. Psychological Medicine, 35(6), 907–917. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Wilfley DE, Pike KM, Dohm FA, & Fairburn CG (2000). Recurrent binge eating in black American women. Archives of Family Medicine, 9(1), 83–87. [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Bulik CM, Marcus MD, Striegel RH, Wilfley DE, Wonderlich SA, & Hudson JI (2013). Binge eating disorder: the next generation of research. International Journal of Eating Disorders, 46(3), 193–207. doi: 10.1002/eat.22089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JY, Caldwell CH, Baser RE, Faison N, & Jackson JS (2007). Prevalence of eating disorders among Blacks in the National Survey of American Life. International Journal of Eating Disorders, 40 Suppl, S10–14. doi: 10.1002/eat.20451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JY, Caldwell CH, Baser RE, Matusko N, Faison N, & Jackson JS (2013). Classification and correlates of eating disorders among Blacks: findings from the National Survey of American Life. Journal of Health Care for the Poor and Underserved, 24(1), 289–310. doi: 10.1353/hpu.2013.0027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson-Brenner H, Franko DL, Thompson DR, Grilo CM, Boisseau CL, Roehrig JP, … Wilson GT (2013). Race/ethnicity, education, and treatment parameters as moderators and predictors of outcome in binge eating disorder. Journal of Consulting and Clinical Psychology, 81(4), 710–721. doi: 10.1037/a0032946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornton LM, Watson HJ, Jangmo A, Welch E, Wiklund C, von Hausswolff-Juhlin Y, … Bulik CM (2017). Binge-eating disorder in the Swedish national registers: Somatic comorbidity. International Journal of Eating Disorders, 50(1), 58–65. doi: 10.1002/eat.22624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Udo T, & Grilo CM (2018). Prevalence and Correlates of DSM-5-Defined Eating Disorders in a Nationally Representative Sample of U.S. Adults. Biological Psychiatry, 84(5), 345–354. doi: 10.1016/j.biopsych.2018.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Udo T, White MA, Lydecker JL, Barnes RD, Genao I, Garcia R, … Grilo CM (2016). Biopsychosocial Correlates of Binge Eating Disorder in Caucasian and African American Women with Obesity in Primary Care Settings. European Eating Disorders Review, 24(3), 181–186. doi: 10.1002/erv.2417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch E, Jangmo A, Thornton LM, Norring C, von Hausswolff-Juhlin Y, Herman BK, … Bulik CM (2016). Treatment-seeking patients with binge-eating disorder in the Swedish national registers: clinical course and psychiatric comorbidity. BMC Psychiatry, 16, 163. doi: 10.1186/s12888-016-0840-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson L (1998). Eating disorders and the cultural forces behind the drive for thinness: are African American women really protected? Social Work in Health Care, 28(1), 61–73. doi: 10.1300/J010v28n01_04 [DOI] [PubMed] [Google Scholar]
- Willig AL, Richardson BS, Agne A, & Cherrington A (2014). Intuitive eating practices among African-American women living with type 2 diabetes: a qualitative study. Journal of Academic Nutrition and Dietetics, 114(6), 889–896. doi: 10.1016/j.jand.2014.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson PL, O’Connor DP, Kaplan CD, Bode S, Mama SK, & Lee RE (2012). Relationship of Fruit, Vegetable, and Fat Consumption to Binge Eating Symptoms and African-American and Hispanic or Latina Women. Eating Behaviors, 13(2), 179–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


