Abstract
The COVID-19 health crisis has reached pandemic scale spreading globally. The present study examines the COVID-19 pandemic’s impact on psychological and physical health-related quality of life (HRQOL) among university students in Turkey. A cross-sectional survey design was used for data collection. From May 11th to May 15th 2020, the study utilized snowball sampling techniques to gather data through an online survey. The pandemic’s psychological effects on participants were measured by the Impact of Event Scale-Revised. Depression, Anxiety and Stress Scale-21 and the 12-Item Short Form Health Survey assess related HRQOL were used to make mental health assessments. 1120 university students were contacted to complete the survey. Of these, a total of 1095 completed the survey, translating to a participation rate of 97.7%. Overall, 64.6%, 48.6% and 45.2%, and 34.5% of all participants self-reported symptomatic signs of depression, anxiety, stress and post-traumatic stress disorder (PTSD), respectively. Female gender and poor family relationships were identified as risk factors for probably PTSD, and symptoms of depression, anxiety, and stress as well. The mean scores of Physical Component Summary (PCS-12) and Mental Component Summary (MCS-12) were 66.99 ± 2.14 and 40.76 ± 2.31, respectively. Students suspected of a history with PTSD had considerably lower total scores for PCS-12 and MCS-12, when cross checked for similarity to those without such a history. The findings of this research suggest that evidence of PTSD, depression, anxiety, and stress is commonly apparent among university students during the period of the COVID-19 crisis. Prevention and intervention approaches to attenuate the psychosocial impact should be an integral component of crisis response during pandemic conditions.
Keywords: Coronavirus, Universities, Students, Mental health, Quality of life
Introduction
Known to cause illness in both humans and animals, coronaviruses constitute a large body of related viruses. Prior to the 2019 outbreak, several coronaviruses were known to be the causes for respiratory infections in humans ranging in severity from the common cold to the more acute diseases Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS). COVID-19, then, is an infectious disease that results from a novel coronavirus. Before winter 2019, there was no public knowledge of this new virus and disease; that all changed when the spread began to gather pace from the viral epicenter in Wuhan, China, in December 2019. COVID-19 is now a pandemic affecting many countries globally (WHO, 2020). In spring 2020, the COVID-19 crisis was confirmed to be present in Turkey; with the first Turkish case of the pandemic being formally confirmed on 11 March 2020 (Republic of Turkey Ministry of Health, 2020).
The pandemic has caused considerable public panic and resulting mental health challenges for individuals (Xiong et al., 2020), as was similarly experienced during the onset of the MERS coronavirus outbreak. In addition, the overwhelming levels of myths and misinformation relating to COVID-19, alongside unprecedented modern bans on travel and executive orders to quarantine travelers, are factors that are likely to affect the public’s mental health. This in turn could have an impact on health-related quality of life (HRQOL) (Huang & Zhao, 2020). HRQOL is an individual’s or a group’s perceived physical and mental health over time. Examining HRQOL has increasingly become a key element of public health surveillance and such research is generally considered a valid measure of identifying unmet needs and potential intervention outcomes. Allowing an individual to self-assess their health status is also a more effective tool in the prediction of mortality and morbidity than many unbiased health assessment systems. Analyses of HRQOL can help provide the framework for interventions that can improve situations for subgroups with contextually poor perceived help. This, in turn, can help to avoid more large scale consequences (Centers for Disease Control and Prevention, 2020). A study in Vietnam using a questionnaire to measure Health-Related Quality of Life (HRQOL) of the Vietnamese citizen has illustrated that COVID-19 disease generated negative effects on health-related quality of life (Tran, Nguyen, et al., 2020).
At present, the impact of the peak of the COVID-19 pandemic on the general public’s psychological and mental well being has not been made clear (Tran, Ha, et al., 2020). This is particularly necessary to address, given the confusion and insecurity brought by a modern virus spread of seemingly unprecedented magnitude. From what can be gathered from the literature, most COVID-19 related research focuses on identifying the epidemiological and genomic makeup of the virus, the clinical attributes of infected individuals, and the challenges posed for global health governance (Wang, Pan, Wan, Tan, Xu, Ho, & Ho, 2020). Although as of yet the effects of COVID-19 on mental health have not been studied systematically, it is expected to have significant effects based on recent public reaction (Shuja et al., 2020).
The ongoing outbreak, strict isolation measures and the suspension of attendance at schools, colleges, and universities across the country is believed to have an impact on the mental health of students. There have been reports on the psychological impact of the epidemic on the general public, patients, medical staff, children, and older adults (Chen et al., 2020; Golberstein et al., 2020; Hao et al., 2020; Tee, Salido, et al., 2020; Wang, Pan, Wan, Tan, Xu, Ho, & Ho, 2020; Yao et al., 2020). However, no evidence of in-depth research on the specific mental health challenge to university students as a result of the global health crisis has been published to date (Cao et al., 2020).
Thus, the present study will represent the first psychological impact and mental health evaluation survey conducted on university student population in Turkey within the first eight weeks of the country’s first COVID-19 case. The study aims to examine if there was an immediate impact of the pandemic on mental health, and on its health-related quality of life among university students in Turkey. This study also investigated the effect of potentially affecting factors such as gender, age, types of family, living areas, household size, father’s education, mother’s education, relationship with family, and self-reported family income on these variables.
Methods
Study Design and Population
This is a cross-sectional descriptive study ran across the period between May 11th and May 15th, 2020. The flowchart methodology of this research is available in the Fig. 1. The participants were 1120 undergraduate students from a university in the Turkey. A snowball sampling strategy was utilized and placed its focus on recruiting a pool of under graduate student residents living in Turkey during the outbreak of COVID-19. As the Turkish Government advised the public to minimize all face-to-face social interaction and to self-isolate at home for indefinite periods of time, many survey respondents were digitally invited to take part in the study by their fellow respondents. The online survey was first disseminated to university students and they were encouraged to disperse it further to their peers.
Fig. 1.
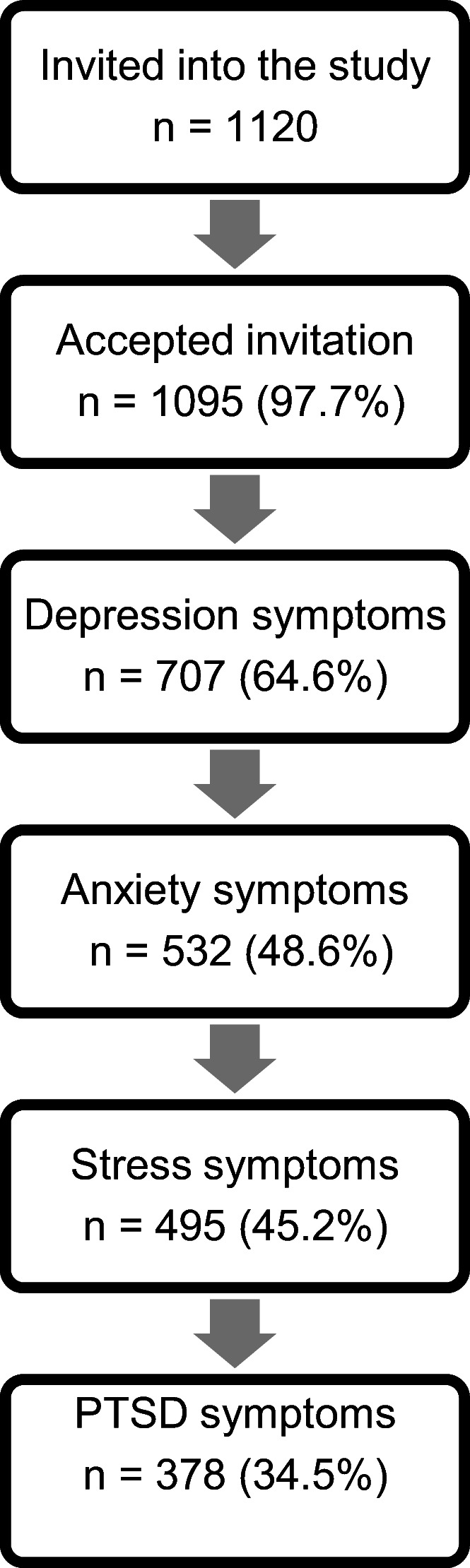
Flow chart of research methodology
Data Collection Tools
Socio-Demographic Information Form
This form consisted of questions that aimed to obtain an overview of respondents’ socio-demographic status and characteristics. Socio-demographic data were collected on gender, age, types of family, living areas, household size, father’s education, mother’s education, relationship with family, and self-reported family income.
Impact of Event Scale - Revised (IES-R)
The IES-R is a 22-item self-assessment measurement tool (for DSM-IV) that reports subjective distress catalyzed by traumatic events. Respondents to an IES-R are asked to outline a specific stressful life event and then evaluate the levels of distress during the previous week by rating each “difficulty” listed. Items are measured on a 5-point scale rating system ranging from 0 (“not at all”) to 4 (“extremely”). The IES-R calculates an overall total score (ranging between 0 and 88), and subscale scores can also be determined for the Intrusion, Avoidance, and Hyperarousal subscales. Generally, the IES-R (and IES) is not used to diagnosis (PTSD). Despite this, cutoff scores for initial diagnoses of PTSD have been present in much of the literature (Weiss & Marmar, 1997). Adaptation of IES-R to the Turkish language, achieved by Corapcioglu et al. (2006) on 104 individuals with and 65 individuals without PTSD diagnosis, had an internal consistency coefficient of 0.94. Furthermore the span for scale specificity was 70.7–81.0% and the sensitivity varied as 74.0%–92.2% in respect of cut off points of 24–33. In this study, the Turkish language version of the IES-R was used. Scoring above 33 was interpreted as a cut off for a “probable PTSD case” (Corapcioglu et al., 2006).
Depression, Anxiety and Stress Scale-21 (DASS-21)
The 21-item DASS is a set of three self-assessment measurement scales which aim to statistically calculate the emotional states of depression, anxiety and stress. A 4-point severity scale measures the levels each “state” the participant has reported experiencing over the last 7 days. The research categorized depression, anxiety, and stress scores into a dichotomous response (“yes/no”) before submitting the results to a univariate analysis. Participants with a cut-off score of ≥10 in depression, ≥8 in anxiety, and ≥ 15 in stress dimension were interpreted as likely experiencing these disorders (as referenced by the DASS manual) (Lovibond & Lovibond, 1995). There is abundant evidence confirming the preliminary reliability and construct soundness of the Turkish translation of Depression, Anxiety, and Stress Scale-21 (DASS-21). Cronbach’s alpha was 0.87 for the depression, 0.85 for the stress, and 0.81 for the anxiety, indicating a good internal consistency for each subscale (Sarıçam, 2018).
The IES-R and DASS-21 were used in the following COVID-19 studies in various countries: Vietnam, Philippines, China and Poland (Le, Dang, et al., 2020; Le, Lai, et al., 2020; Tee, Tee, et al., 2020; Wang, Chudzicka-Czupała, Grabowski, Pan, Adamus, Wan, et al., 2020; Wang, Pan, Wan, Tan, Xu, McIntyre, et al., 2020).
12-Item Short Form Health Survey (SF-12)
The SF-12 is a non-specific dimension which does not zone in on any one particular age group or disease category. It was initially created as a justifiable shorter counterpart of the SF-36, which has been found to be too lengthy a process of administration in large sample studies. The SF-12 is easily interpreted, as it is weighted and summed, therefore providing transparent physical and mental health scales. The Physical Component Summary (PCS-12) and Mental Component Summary (MCS-12) scores are calculated using 12 questions with a range of 0–100 (zero indicating the poorest level of health measured and 100 indicating the highest) (Ware et al., 1995). The PCS-12 and MCS-12 were individually analyzed as two different six-item physical and mental health scales, respectively. The Turkish validity study was prepared by Kocyigit et al. The Cronbach’s alpha reliability of the scale was 0.73–0.76 (Kocyigit et al., 1999).
Ethics Approval
The research has been ratified by the Ethics Committee of the Zonguldak Bülent Ecevit University. All questionnaires were anonymized, and participation was actively stated as non- mandatory. Informed consent was provided by all survey respondents.
Statistical Analysis
Statistical analyses were performed using the statistical software package SPSS version 20 for Windows. P values <0.05 were considered to be statistically significant. Descriptive statistics (means, standard deviations, percentages and frequencies) were calculated to assess the percentages and levels of depression, anxiety, stress and post-traumatic stress disorder among the study participants. Categorical variables were expressed as numbers (n) and percentages (%), and were compared using the chi-square (χ2) test. The independent t-test was used to compare the mean values of continuous variables. Multivariable Logistic Regression Analysis was performed to identify the predictors for the depression, anxiety, stress and post-traumatic stress disorder symptoms.
Results
Table 1 illustrates socio-demographic attributes. The 1095 students included in the analyses were made up of 279 (25.5%) males and 816 (74.5%) females. The mean age of participants was 21.72 ± 3.47, and 65.9% are aged 21–35 years. The majority of survey respondents (73.5%) are in nuclear family. It was clear from respondents’ addresses that 877 (80.1%) were from urban areas and 218 (19.9%) were from rural areas. Over 50% of respondents lived in a household of 1–4 family members (53.9%). Almost half (49.5%) of students’ fathers and 30.9% of mothers had completed high school education or above. Poor family relationships were reported by 104 (9.5%) of the students. The majority of students (84.2%) reported being part of middle-income families.
Table 1.
Socio-demographic characteristics of participants (n = 1095)
| Characteristics | n | % |
|---|---|---|
| Gender | ||
| Male | 279 | 25.5 |
| Female | 816 | 74.5 |
| Age (years) (Mean ± SD = 21.72 ± 3.47) | ||
| 18–20 years old | 373 | 34.1 |
| 21–35 years old | 722 | 65.9 |
| Types of family | ||
| Extended family | 215 | 19.6 |
| Nuclear family | 805 | 73.5 |
| Single parent family | 75 | 6.8 |
| Living areas | ||
| Rural | 218 | 19.9 |
| Urban | 877 | 80.1 |
| Household size | ||
| One to four people | 590 | 53.9 |
| Five people or more | 505 | 46.1 |
| Father’s education | ||
| ≤Secondary school | 553 | 50.5 |
| ≥High school | 542 | 49.5 |
| Mother’s education | ||
| ≤Secondary school | 757 | 69.1 |
| ≥High school | 338 | 30.9 |
| Relationship with family | ||
| Good | 489 | 44.7 |
| Average | 502 | 45.8 |
| Poor | 104 | 9.5 |
| Self-reported family income | ||
| Lower | 96 | 8.8 |
| Middle | 922 | 84.2 |
| Higher | 77 | 7.0 |
| Total | 1095 | 100.0 |
The psychological impact on Turkish university students, as a result of the COVID-19 pandemic, was measured using the IES-R scale, revealed a sample mean score of 28.29 (SD = 14.78). The mean total scores for the respondents were 13.80 (SD = 9.75) for depression, 8.34 (SD = 7.50) for anxiety and 14.98 (SD = ± 9.26) for stress. For the depression subscale, 388 (35.4%) were interpreted as having normal score; 175 (16.0%) were considered to suffer from mild depression; 294 (26.8%) were considered to suffer from moderate depression; 117 (10.7%) were considered to suffer from severe depression; and 121 (11.1%) were considered to suffer from extremely severe depression. For the anxiety subscale, 563 (51.4%) were interpreted as having a normal score; 121 (11.1%) were seen as suffering from mild anxiety; 222 (20.3%) from moderate anxiety; 75 (6.8%) from severe anxiety; and 114 (10.4%) were interpreted as suffering from extremely severe/intense anxiety. For the stress subscale, 600 (54.8%) were interpreted as having a normal score; 162 (14.8%) were considered to suffer from mild stress; 163 (14.9%) were considered to suffer from moderate stress; 122 (11.1%) were considered to suffer from severe stress; and 48 (4.4%) were considered to suffer from extremely severe stress (Table 2).
Table 2.
Number and percentage of students in each category of the two questionnaires: IES-R and DASS-21 with mean (SD) scores (n = 1095)
| n | % | |
|---|---|---|
| Impact of Event Scale-Revised (IES-R) | ||
| IES-R Score (Mean ± SD = 28.29 ± 14.78) | ||
| No PTSD (IES-R score < 33) | 717 | 65.5 |
| PTSD (IES-R ≥ 33) | 378 | 34.5 |
| Depression Anxiety Stress Scale–21 (DASS-21) | ||
| DASS 21 Depression Score (Mean ± SD = 13.80 ± 9.75) | ||
| DASS-21 (Depression) | ||
| Normal (0–9) | 388 | 35.4 |
| Mild (10–13) | 175 | 16.0 |
| Moderate (14–20) | 294 | 26.8 |
| Severe (21–27) | 117 | 10.7 |
| Extremely Severe (28+) | 121 | 11.1 |
| DASS 21 Anxiety Score (Mean ± SD = 8.34 ± 7.50) | ||
| DASS-21 (Anxiety) | ||
| Normal (0–7) | 563 | 51.4 |
| Mild (8–9) | 121 | 11.1 |
| Moderate (10–14) | 222 | 20.3 |
| Severe (15–19) | 75 | 6.8 |
| Extremely Severe (20+) | 114 | 10.4 |
| DASS 21 Stress Score (Mean ± SD = 14.98 ± 9.26) | ||
| DASS-21 (Stress) | ||
| Normal (0–14) | 600 | 54.8 |
| Mild (15–18) | 162 | 14.8 |
| Moderate (19–25) | 163 | 14.9 |
| Severe (26–33) | 122 | 11.1 |
| Extremely Severe (34+) | 48 | 4.4 |
Of those that took part in this survey, 378 reported a high level of PTSD symptoms, with an IES-R score of 33 or higher, suggesting that the prevalence of PTSD symptoms in this cohort is 34.5%. In total, the widespread presence of mild to extremely intense symptoms of ill-mental health (depression, anxiety and stress) within this group distributed at 64.6%, 48.6% and 45.2%, respectively. PTSD was found to have a significant association with the female gender, single parent families, higher maternal education, poor family relationships, and lower family incomes (p < 0.05). Depression was also found to be significantly associated with some of these factors, namely with female gender, poor family relationships, and low family income (p < 0.05). In addition, it was clearly evident that anxiety was significantly associated with the female gender and poor family relationships (p < 0.05). It was further noted that stress had a significant presence in women, as well as clear links to single parent families, higher maternal education, poor family relationships, and low family income (p < 0.05) (Table 3).
Table 3.
Associations between socio-demographic characteristics and depression, anxiety, stress and post-traumatic stress disorder symptoms during the COVID-19 outbreak
| Characteristics | PTSD (Yes) | Depression (Yes) | Anxiety (Yes) | Stress (Yes) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | p a | n | % | p a | n | % | p a | n | % | p a | |
| Total | 378 | 34.5 | 707 | 64.6 | 532 | 48.6 | 495 | 45.2 | ||||
| Gender | ||||||||||||
| Male | 80 | 28.7 | 0.01 | 159 | 57.0 | 0.00 | 106 | 38.0 | 0.00 | 97 | 34.8 | 0.00 |
| Female | 298 | 36.5 | 548 | 67.2 | 426 | 52.2 | 398 | 48.8 | ||||
| Age (years) | ||||||||||||
| 18–20 years old | 131 | 35.1 | 0.76 | 247 | 66.2 | 0.41 | 178 | 47.7 | 0.68 | 177 | 47.5 | 0.28 |
| 21–35 years old | 247 | 34.2 | 460 | 63.7 | 354 | 49.0 | 318 | 44.0 | ||||
| Types of family | ||||||||||||
| Extended family | 73 | 34.0 | 0.03 | 140 | 65.1 | 0.35 | 110 | 51.2 | 0.43 | 90 | 41.9 | 0.03 |
| Nuclear family | 269 | 33.4 | 513 | 63.7 | 382 | 47.5 | 361 | 44.8 | ||||
| Single parent family | 36 | 48.0 | 54 | 72.0 | 40 | 53.3 | 44 | 58.7 | ||||
| Living areas | ||||||||||||
| Rural | 74 | 33.9 | 0.84 | 145 | 66.5 | 0.50 | 111 | 50.9 | 0.44 | 102 | 46.8 | 0.60 |
| Urban | 304 | 34.7 | 562 | 64.1 | 421 | 48.0 | 393 | 44.8 | ||||
| Household size | ||||||||||||
| One to four people | 206 | 34.9 | 0.76 | 376 | 63.7 | 0.53 | 273 | 46.3 | 0.09 | 262 | 44.4 | 0.56 |
| Five people or more | 172 | 34.1 | 331 | 65.5 | 259 | 51.3 | 233 | 46.1 | ||||
| Father’s education | ||||||||||||
| ≤Secondary school | 182 | 32.9 | 0.25 | 354 | 64.0 | 0.70 | 266 | 48.1 | 0.74 | 247 | 44.7 | 0.71 |
| ≥High school | 196 | 36.2 | 353 | 65.1 | 266 | 49.1 | 248 | 45.8 | ||||
| Mother’s education | ||||||||||||
| ≤Secondary school | 247 | 32.6 | 0.04 | 481 | 63.5 | 0.28 | 364 | 48.1 | 0.62 | 332 | 43.9 | 0.18 |
| ≥High school | 131 | 38.8 | 226 | 66.9 | 168 | 49.7 | 163 | 48.2 | ||||
| Relationship with family | ||||||||||||
| Good | 156 | 31.9 | 0.00 | 268 | 54.8 | 0.00 | 201 | 41.1 | 0.00 | 173 | 35.4 | 0.00 |
| Average | 166 | 33.1 | 355 | 70.7 | 262 | 52.2 | 249 | 49.6 | ||||
| Poor | 56 | 53.8 | 84 | 80.8 | 69 | 66.3 | 73 | 70.2 | ||||
| Self-reported family income | ||||||||||||
| Lower | 47 | 49.0 | 0.00 | 66 | 68.8 | 0.04 | 49 | 51.0 | 0.20 | 61 | 63.5 | 0.00 |
| Middle | 308 | 33.4 | 601 | 65.2 | 453 | 49.1 | 407 | 44.1 | ||||
| Higher | 23 | 29.9 | 40 | 51.9 | 30 | 39.0 | 27 | 35.1 | ||||
aPearson Chi-Square Test
Table 4 displays the results of the logistic regression analysis for the independent factors and PTSD, depression, anxiety, and stress. Female gender and poor family relationships were found to be significantly associated with typical signs of PTSD, depression, anxiety, and stress. Lower family incomes were noticeably linked with PTSD, depression, and stress symptoms. Interestingly, symptoms of PTSD and stress were significantly correlated with a higher level of maternal education.
Table 4.
Risk factors for mental health outcomes identified by multivariable logistic regression analysis
| Variables | Categories | B | p | AOR | 95.0% C.I. | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| PTSD | ||||||
| Gender | Male + | – | – | 1.00 | – | – |
| Female | 0.35 | 0.02 | 1.43 | 1.05 | 1.93 | |
| Types of family | Extended family + | – | – | 1.00 | – | – |
| Nuclear family | −0.03 | 0.83 | 0.96 | 0.69 | 1.33 | |
| Single parent family | 0.25 | 0.37 | 1.28 | 0.73 | 2.25 | |
| Mother’s education | ≤ Secondary school + | – | – | 1.00 | – | – |
| ≥ High school | 0.32 | 0.02 | 1.38 | 1.04 | 1.83 | |
| Relationship with family | Good + | – | – | 1.00 | – | – |
| Average | 0.02 | 0.88 | 1.02 | 0.77 | 1.33 | |
| Poor | 0.73 | 0.00 | 2.08 | 1.33 | 3.26 | |
| Self-reported family income | Lower | 0.93 | 0.00 | 2.55 | 1.31 | 4.96 |
| Middle | 0.33 | 0.21 | 1.39 | 0.82 | 2.35 | |
| Higher + | – | – | 1.00 | – | – | |
| Constant | −0.64 | 0.00 | 0.52 | |||
| Depression | ||||||
| Gender | Male + | – | – | 1.00 | – | – |
| Female | 0.40 | 0.00 | 1.49 | 1.12 | 1.98 | |
| Relationship with family | Good + | – | – | 1.00 | – | – |
| Average | 0.65 | 0.00 | 1.92 | 1.47 | 2.50 | |
| Poor | 1.20 | 0.00 | 3.34 | 1.97 | 5.67 | |
| Self-reported family income | Lower | 0.54 | 0.03 | 1.72 | 0.90 | 3.27 |
| Middle | 0.51 | 0.09 | 1.67 | 1.03 | 2.71 | |
| Higher + | – | – | 1.00 | – | – | |
| Constant | 0.60 | 0.00 | 1.82 | |||
| Anxiety | ||||||
| Gender | Male + | – | – | 1.00 | – | – |
| Female | 0.53 | 0.00 | 1.71 | 1.29 | 2.27 | |
| Relationship with family | Good + | – | – | 1.00 | – | – |
| Average | 0.44 | 0.00 | 1.55 | 1.20 | 2.00 | |
| Poor | 0.98 | 0.00 | 2.67 | 1.70 | 4.18 | |
| Constant | −0.05 | 0.00 | 0.94 | |||
| Stress | ||||||
| Gender | Male + | – | – | 1.00 | – | – |
| Female | 0.57 | 0.00 | 1.71 | 1.32 | 2.37 | |
| Types of family | Extended family + | – | – | 1.00 | – | – |
| Nuclear family | 0.14 | 0.38 | 1.15 | 0.83 | 1.58 | |
| Single parent family | 0.27 | 0.34 | 1.31 | 0.74 | 2.32 | |
| Mother’s education | ≤ Secondary school + | – | – | 1.00 | – | – |
| ≥ High school | 0.29 | 0.03 | 1.34 | 1.02 | 1.77 | |
| Relationship with family | Good + | – | – | 1.00 | – | – |
| Average | 0.56 | 0.00 | 1.75 | 1.34 | 2.27 | |
| Poor | 1.29 | 0.00 | 3.65 | 2.26 | 5.88 | |
| Self-reported family income | Lower | 1.22 | 0.00 | 3.39 | 1.73 | 6.61 |
| Middle | 0.47 | 0.68 | 1.61 | 0.96 | 2.69 | |
| Higher + | – | – | 1.00 | – | – | |
| Constant | −0.19 | 0.00 | 0.82 | |||
+Reference group, AOR Adjusted odds ratios
The mean scores of PCS-12 and MCS-12 were 66.99 ± 2.14 and 40.76 ± 2.31, respectively. Students who had an associative history with probable PTSD had demonstrably lower summary scores for both PCS-12 and MCS-12 when contrasted to those without such a history (Table 5).
Table 5.
Mean SF-12 Physical Component Summary (PCS-12) scores and mean Mental Component Summary (MCS-12) scores by PTSD history during the COVID-19 outbreak
| Variables | Impact of Event | |||
|---|---|---|---|---|
| SF-12 Composite Scores | Overall (n = 1095) |
PTSD (n = 378, 34.5%) |
No PTSD (n = 717, 65.5%) |
p b |
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| Physical Component Summary (PCS-12) | 66.99 ± 21.48 | 60.10 ± 21.67 | 70.61 ± 20.48 | 0.00 |
| Mental Component Summary (MCS-12) | 40.76 ± 23.19 | 30.20 ± 19.53 | 46.33 ± 19.53 | 0.00 |
bIndependent-Samples T Test
Discussion
In total, 64.6%, 48.6% and 45.2%, and 34.5% of all survey respondents self-diagnosed with symptoms of depression, anxiety, stress and PTSD, respectively. The female gender and lacking a strong familial relationship were identified as two main risk factors indicating signs of PTSD, depression, anxiety, and stress. Low socioeconomic status was notably linked with symptoms of PTSD, depression, and stress. The findings of the present study also confirm that PTSD was significantly associated with poor HRQOL.
A total prevalence rate of 34.5% of likely PTSD during the outbreak (established as an IES-R score of 33 or more) was clear in the results. In a 2020 study conducted in China, 11.1% of university students described experiences of PTSD during the 2020 pandemic outbreak (Li et al., 2020). A 2020 Spanish national survey similarly found that the prevalence of PTSD was 15.8%, this time among the general population, during the onset of virus spread (González-Sanguino et al., 2020). In a study of the Chinese general population, Wang, Pan, Wan, Tan, Xu, Ho, and Ho (2020), identified the prevalence of PTSD was 53.8% during outbreak period (Wang, Pan, Wan, Tan, Xu, Ho, & Ho, 2020). The comparison between rates of prevalence in studies is restricted by the necessity of using varied instruments, symptom time periods, and samples.
Our findings suggest that more acute PTSD, depression, anxiety, and stress symptoms were self-reported by women. This is consistent with the findings of earlier studies, many of which regularly have shown a connection between the female gender and high levers of mental ill-health (González-Sanguino et al., 2020; Liu et al., 2020; Ozdin & Bayrak Özdin, 2020; Wang, Pan, Wan, Tan, Xu, Ho, & Ho, 2020). It may be further linked to the thesis from international research which puts forward the theory that women are perhaps are susceptible to experiencing stress and symptoms of PTSD (Mazza et al., 2020). For example, much of epidemiological scholarship has identified gender-specific risk for the development of PTSD. Indeed, it has been found that the likeliness of developing PTSD following exposure to a traumatic event is twice that for women as to men (Breslau et al., 1998; Kessler et al., 1995). It has been theorized that a number of different characteristics (both individual and trauma-related) may contribute to this PTSD-related gender difference, including psychophysiological sex differences, contrasting threat appraisals, dissociation, coping styles, and availability of social supports (Irish et al., 2011). It is known that women and men experience pandemics in different ways and those circumstances, in addition to strengthening situations of women’s vulnerability, tend to aggravate family tensions, especially in families with a history of recurrent domestic violence (Augusto de Lima et al., 2020).
Our study found that positive family relationships were linked with lowered risks of possible PTSD. Comparably, Li et al.’s (2020) study indicated that poor family functioning was associated with higher prevalence of PTSD in Chinese university students. It has been thoroughly noted that familial or social support after trauma may have an alleviating impaction PTSD symptoms. The data from this study add to the pool of knowledge that emotional support from loved ones before a trauma may improve the likelihood of each person’s individual resilience to stress, independently of baseline level of symptomatic stress (Li et al., 2020).
The findings of this research are in congruence with, but actually go beyond, general population studies that have indicate having both a low income and living in a low-income area can independently heighten PTSD risk (Golin et al., 2016). For example, it has been shown that lower socioeconomic status is linked to increased levels of PTSD and depression among people who have been exposed to trauma. However, it is important to note that most of this research was carried out in countries that largely have high-income populations. The few studies in low-income countries do, however, also corroborated the links between socioeconomic disadvantages and increase of emotional distress or poorer health—both psychological and physical (Ayazi et al., 2012). There is considerable evidence, for example, that common mental illnesses (depression and anxiety) may be causally distributed across a gradient of societal economic disadvantage, meaning that there is disproportionate ill-health and suffering for poor and marginalized, as well as from additional challenging consequences that ill-health can result in (WHO and Calouste Gulbenkian Foundation, 2014).
The present study found that PTSD was also the leading factor associated with deterioration, in both physical and mental health performance, in participants who displayed a historical symptomatic relationship with probable PTSD. Past literature has identified an association between PTSD and decline in functioning across a wide array of areas and challenges to overall quality of life (Lunney & Schnurr, 2007; Schnurr et al., 2006). Schnurr et al. (2006) found that the higher the severity in occurrences of PTSD symptom, the higher the alignment with increased functional impairment of both psychosocial and physical health. In 2007, Lunney and Schnurr reported that clinically significant alleviation of PTSD symptoms were associated with beneficial advances in various aspects relating to quality of life. These findings suggest a two-way dynamic between PTSD and functional impairments and quality of life (Holowka & Marx, 2012).
The most evidence-based treatment is cognitive behavioral therapy (CBT), especially Internet CBT that can prevent the spread of infection during the pandemic. Recent systematic reviews and meta-analysis conducted have highlighted the efficacy and effectiveness of cognitive behavioral therapies which are delivered via the Internet (Ho, Chee, & Ho, 2020). Internet based cognitive behavioral therapy has been demonstrated to be effective in the treatment of comorbid depressive symptoms amongst individuals who have post-traumatic stress disorder as a primary condition (Ho, Chee, & Ho, 2020).
There are several limitations associated with this study. First, the major limitation is certainly the cross-sectional design, which does not allow now drawing any conclusions about the causality of the results. Second, given the limited resources available and time-sensitivity of the COVID-19 outbreak, we adopted the snowball sampling strategy. The snowball sampling strategy was not based on a random selection of the sample, and the study population did not reflect the actual pattern of the general population. Another limitation is that this study mainly used self-reported questionnaires to measure psychiatric symptoms and did not make clinical diagnosis. The gold standard for establishing psychiatric diagnosis involved structured clinical interview and functional neuroimaging (Ho, Lim, et al., 2020; Husain et al., 2020).
Conclusions
The findings of this research suggest that evidence of PTSD, depression, anxiety, and stress is commonly apparent among university students during the period of the COVID-19 pandemic. Our study found that more than one-third of respondents presented symptoms of PTSD during the Turkish outbreak of the COVID-19 pandemic. The global health crisis of 2020 has clearly caused collateral health damage in as much as it has also had adverse effects on mental health and on physical health in more indirect ways. These are consequences that may, in turn, have a negative influence on the general health of university students. Female gender and poor family relationships were associated with increased risk of psychological effects from the outbreak, as well as with high prevalence levels of stress, anxiety, and depression. These findings can be used to form the foundations of psychological interventions that may improve mental health and psychological resilience during the ongoing health crisis. For example, adequate and effective counseling services should be made available to support students’ mental health and wellbeing.
To address the needs of the student population during this pandemic, it is worthwhile to contemplate the introduction of online or smart phone based psycho education on the outbreak to promote mental wellness and psychological interventions such as cognitive behavioral therapy (CBT) and mindfulness based cognitive therapy (MBCT) (Ho, Chee, & Ho, 2020).
The announcement of an increase in the number of patients with the disease and the death toll also adds to the emotional excitement. Therefore, to prevent mental and psychological diseases as well as other social harms, people can make it easier and more tolerable of quarantine conditions and issues on the margins of illness, by studying and reading books. Research has shown that studying, especially reading books plays an important role in preventing diseases such as depression and stress (Arab-Rahmatipour et al., 2020).
Acknowledgments
The authors would like to thank all the students who participated in the study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics
Ethics Committee consent (2020–801) received to perform the study.
Conflict of Interest
The authors declare that there is no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Hasan Huseyin Cam, Email: cam_hasanhuseyin@hotmail.com.
Fadime Ustuner Top, Email: fadime.ustuner@giresun.edu.tr.
Tülay Kuzlu Ayyildiz, Email: tayyildiz67@hotmail.com.
References
- Arab-Rahmatipour M, Ebadollahi-Natanzi A, Arab-Rahmatipour G. Prevention of depression and psychological stress by studying book in quarantine conditions of COVID-19. SciMedicine Journal. 2020;2(3):182–183. doi: 10.28991/SciMedJ-2020-0203-7. [DOI] [Google Scholar]
- Augusto de Lima C, Alves P, Barauna de Oliverira C, Nascimento de Oliverira T, Barbosa K, Marcene H, Vilges de Oliveira S. COVID-19: Isolations, quarantines and domestic violence in rural areas. SciMedicine Journal. 2020;2(1):44–45. doi: 10.28991/SciMedJ-2020-0201-7. [DOI] [Google Scholar]
- Ayazi T, Lien L, Eide AH, Ruom MM, Hauff E. What are the risk factors for the comorbidity of posttraumatic stress disorder and depression in a war-affected population? A cross-sectional community study in South Sudan. BMC Psychiatry. 2012;12:175. doi: 10.1186/1471-244X-12-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: The 1996 Detroit area survey of trauma. Archives of General Psychiatry. 1998;55(7):626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2020). Health-Related Quality of Life (HRQOL). https://www.cdc.gov/hrqol/concept.htm
- Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, He L, Sheng C, Cai Y, Li X, Wang J, Zhang Z. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corapcioglu A, Yargiç İ, Geyran P, Kocabaşoğlu N. Validity and reliability of Turkish version of "impact of event scale-revised" (IES-R) New Symposium: A Journal of Psychiatry, Neurology and Behavioral Sciences. 2006;44(1):14–22. [Google Scholar]
- Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatrics. 2020;174:819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- Golin CE, Haley DF, Wang J, Hughes JP, Kuo I, Justman J, Adimora AA, Soto-Torres L, O’Leary A, Hodder S. Post-traumatic stress disorder symptoms and mental health over time among low-income women at increased risk of HIV in the U.S. Journal of Health Care for the Poor and Underserved. 2016;27(2):891–910. doi: 10.1353/hpu.2016.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Sanguino, C., Ausín, B., Ángel Castellanos, M., Saiz, J., López-Gómez, A., Ugidos, C., & Muñoz, M. (2020). Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain, Behavior, and Immunity. Advance online publication. 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed]
- Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, Hu Y, Luo X, Jiang X, McIntyre RS, Tran B, Sun J, Zhang Z, Ho R, Ho C, Tam W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain, Behavior, and Immunity. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho C, Lim L, Lim AQ, Chan N, Tan RS, Lee SH, Ho R. Diagnostic and predictive applications of functional near-infrared spectroscopy for major depressive disorder: A systematic review. Frontiers in Psychiatry. 2020;11:378. doi: 10.3389/fpsyt.2020.00378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Annals of the Academy of Medicine, Singapore. 2020;49(3):155–160. doi: 10.47102/annals-acadmedsg.202043. [DOI] [PubMed] [Google Scholar]
- Holowka, D. W., & Marx, B. P. (2012). Assessing PTSD-related functional impairment and quality of life. In G. J. Beck & D. M. Sloan (Eds.), Oxford handbook of traumatic stress disorders (pp. 315–332). Oxford University Press. 10.1093/oxfordhb/9780195399066.013.0021.
- Huang Y, Zhao N. Mental health burden for the public affected by the COVID-19 outbreak in China: Who will be the high-risk group? Psychology, Health & Medicine. 2020;26:23–34. doi: 10.1080/13548506.2020.1754438. [DOI] [PubMed] [Google Scholar]
- Husain SF, Yu R, Tang TB, Tam WW, Tran B, Quek TT, Hwang SH, Chang CW, Ho CS, Ho RC. Validating a functional near-infrared spectroscopy diagnostic paradigm for major depressive disorder. Scientific Reports. 2020;10(1):9740. doi: 10.1038/s41598-020-66784-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irish LA, Fischer B, Fallon W, Spoonster E, Sledjeski EM, Delahanty DL. Gender differences in PTSD symptoms: An exploration of peritraumatic mechanisms. Journal of Anxiety Disorders. 2011;25(2):209–216. doi: 10.1016/j.janxdis.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kocyigit H, Aydemir O, Olmez N, Memis A. Reliability and validity of the Turkish version of short Form-36 (SF-36) Turkish Journal of Drugs Therapeutics. 1999;12(2):102–106. [Google Scholar]
- Le HT, Lai A, Sun J, Hoang MT, Vu LG, Pham HQ, et al. Anxiety and depression among people under the Nationwide partial lockdown in Vietnam. Frontiers in Public Health. 2020;8:589359. doi: 10.3389/fpubh.2020.589359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le X, Dang AK, Toweh J, Nguyen QN, Le HT, Do T, et al. Evaluating the psychological impacts related to COVID-19 of Vietnamese people under the first Nationwide partial lockdown in Vietnam. Frontiers in Psychiatry. 2020;11:824. doi: 10.3389/fpsyt.2020.00824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Y., Wang, Y., Jiang, J., Valdimarsdóttir, U. A., Fall, K., Fang, F., … Zhang, W. (2020). Psychological distress among health professional students during the COVID-19 outbreak. Psychological Medicine. Advance online publication. 10.1017/S0033291720001555. [DOI] [PMC free article] [PubMed]
- Liu N, Zhang F, Wei C, Jia Y, Shang Z, Sun L, Wu L, Sun Z, Zhou Y, Wang Y, Liu W. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Research. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond, S. H., & Lovibond, P. F. (1995). Manual for the depression anxiety stress scales (2nd ed.). Psychology Foundation.
- Lunney CA, Schnurr PP. Domains of quality of life and symptoms in male veterans treated for posttraumatic stress disorder. Journal of Traumatic Stress. 2007;20(6):955–964. doi: 10.1002/jts.20269. [DOI] [PubMed] [Google Scholar]
- Mazza C, Ricci E, Biondi S, Colasanti M, Ferracuti S, Napoli C, Roma P. A Nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors. International Journal of Environmental Research and Public Health. 2020;17(9):E3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozdin S, Bayrak Özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. The International Journal of Social Psychiatry. 2020;66:504–511. doi: 10.1177/0020764020927051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Republic of Turkey Ministry of Health. (2020). COVID-19 (SARS-CoV2 Infection) Guide.https://covid19bilgi.saglik.gov.tr/depo/rehberler/COVID-19_Rehberi.pdf
- Sarıçam H. The psychometric properties of Turkish version of depression anxiety stress Scale-21 (DASS-21) in health control and clinical samples. Journal of Cognitive-Behavioral Psychotherapy and Research. 2018;7(1):19–30. doi: 10.5455/JCBPR.274847. [DOI] [Google Scholar]
- Schnurr PP, Hayes AF, Lunney CA, McFall M, Uddo M. Longitudinal analysis of the relationship between symptoms and quality of life in veterans treated for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2006;74(4):707–713. doi: 10.1037/0022-006X.74.4.707. [DOI] [PubMed] [Google Scholar]
- Shuja KH, Aqeel M, Jaffar A, Ahmed A. COVID-19 pandemic and impending global mental health implications. Psychiatria Danubina. 2020;32(1):32–35. doi: 10.24869/psyd.2020.32. [DOI] [PubMed] [Google Scholar]
- Tee CA, Salido EO, Reyes P, Ho RC, Tee ML. Psychological state and associated factors during the 2019 coronavirus disease (COVID-19) pandemic among Filipinos with rheumatoid arthritis or systemic lupus Erythematosus. Open Access Rheumatology: Research and Reviews. 2020;12:215–222. doi: 10.2147/OARRR.S269889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tee ML, Tee CA, Anlacan JP, Aligam K, Reyes P, Kuruchittham V, Ho RC. Psychological impact of COVID-19 pandemic in the Philippines. Journal of Affective Disorders. 2020;277:379–391. doi: 10.1016/j.jad.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran BX, Ha GH, Nguyen LH, Vu GT, Hoang MT, Le HT, et al. Studies of novel coronavirus disease 19 (COVID-19) pandemic: A global analysis of literature. International Journal of Environmental Research and Public Health. 2020;17(11):4095. doi: 10.3390/ijerph17114095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran, B. X., Nguyen, H. T., Le, H. T., Latkin, C. A., Pham, H. Q., Vu, L. G., et al. (2020). Impact of COVID-19 on economic well-being and quality of life of the Vietnamese during the National Social Distancing. Frontiers in Psychology. Advance online publication, 11. 10.3389/fpsyg.2020.565153. [DOI] [PMC free article] [PubMed]
- Wang C, Chudzicka-Czupała A, Grabowski D, Pan R, Adamus K, Wan X, Hetnał M, Tan Y, Olszewska-Guizzo A, Xu L, McIntyre RS, Quek J, Ho R, Ho C. The association between physical and mental health and face mask use during the COVID-19 pandemic: A comparison of two countries with different views and practices. Frontiers in Psychiatry. 2020;11:569981. doi: 10.3389/fpsyt.2020.569981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5):E1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, Choo FN, Tran B, Ho R, Sharma VK, Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware, J. E., Kosinski, M., & Keller, S. D. (1995). SF-12: How to score the SF-12 physical and mental health summary scales (2nd ed.). The Health İnstitute, New England Medical Center.
- Weiss, D. S., & Marmar, C. R. (1997). The impact of event scale-revised. In J. P. Wilson & T. M. Keane (Eds.), Assessing psychological trauma and PTSD: A Practitioner’s handbook (pp. 399–411). Guilford Press.
- World Health Organization (WHO). (2020). Questions and Answers (Q&A) on coronaviruses (COVID-19). https://www.who.int/news-room/q-a-detail/q-a-coronaviruses
- World Health Organization and Calouste Gulbenkian Foundation. (2014). Social determinants of mental health. World Health Organization https://www.who.int/mental_health/publications/gulbenkian_paper_social_determinants_of_mental_health/en/.
- Xiong J, Lipsitz O, Nasri F, Lui L, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.


