Abstract
Background
Kawasaki disease (KD) is a form of systemic febrile vasculitis that is complicated with coronary artery lesions (CAL). The tight junctions that maintain the intestinal barrier also play a role in systemic inflammatory diseases. Serum zonula occludens-1 (ZO-1) expression was found to be significantly lower in asthmatic patients, and another study reported that elevated systemic ZO-1 was positively correlated with inflammation in cirrhotic patients. A murine model of KD vasculitis demonstrated that vasculitis depended on intestinal barrier dysfunction, which is maintained by tight junctions. In this study, we aimed to investigate the role of the tight junction zonula occludens-1 (ZO-1) in the treatment response of intravenous immunoglobulin (IVIG) and the occurrence of CAL formation in KD patients.
Methods
We enrolled 40 KD patients, 12 healthy controls, and 12 febrile controls in this study. The serum levels of tight junction ZO-1 were determined by enzyme-linked immunosorbent assay.
Results
The serum ZO-1 level was higher in the fever control group but did not reach a statistical significance. KD patients who received a second dose of IVIG treatment due to initial IVIG unresponsiveness had a higher serum levels of tight junction ZO-1, but without statistical significance (2.15 ± 0.18 vs. 2.69 ± 0.31 ng/mL, p = 0.058). KD patients who developed a CAL demonstrated a significant lower serum tight junction ZO-1 levels than KD without CAL formation (1.89 ± 0.16 vs. 2.39 ± 0.15 ng/mL, p = 0.027). After multiple logistic regression analysis, ZO-1 levels [(95% confidence interval (CI): 0.058 ~ 0.941, odds ratio (OR) = 0.235, p = 0.041)] showed as the risk factor for CAL formation.
Conclusion
Serum levels of tight junction ZO-1 levels were lower in KD patients than fever controls and associated with CAL formation.
Keywords: Kawasaki disease, Tight junction protein, Coronary artery lesions
Background
Kawasaki disease (KD) is an acute febrile coronary vasculitis disease that primarily occurs in children under the age of 5 years old. First described by Dr. Tomisaku Kawasaki in 1967, the first report of Kawasaki disease in English was published in 1974 [1]. The clinical presentation of complete Kawasaki disease patients includes prolonged fever (more than 5 days) and at least four of the following five major symptoms: cervical lymphadenopathy, bilateral non-purulent conjunctivitis, indurative angioedema of the hands and feet, diffuse mucosal inflammation, and polymorphous skin rashes [2]. Cardiovascular involvement such as fistula formation [3], coronary artery lesions (CAL), coronary artery dilatation and coronary artery aneurysm (CAA), are major complications of KD [4, 5].
KD also affects the mucosal intestinal immune responses, and KD patients have an increased number of activated T cells and macrophages in the small intestine [6]. A recent multicenter study of more than 300 patients revealed that abdominal and gastrointestinal symptoms at KD onset can complicate KD diagnosis, cause therapeutic delay, and increase the risk for IVIG resistance and coronary aneurysms [7, 8]. Furthermore, Rivas et al. demonstrated that a murine model of KD vasculitis depended on intestinal barrier dysfunction, which led to secretory IgA leakage and IgA-C3 immune complex deposition in cardiovascular lesions [8]. Zonula occludens (ZO)-1 is a multi-domain polypeptide required for the assembly of tight junctions [9] and thus essential for the intestinal barrier.
Recent studies showed that ZO-1 was also associated with inflammation. ZO-1 expression levels were significantly lower in asthmatic patients and may have played a role in inflammation [10]. Another study reported that elevated systemic ZO-1 was positively correlated with inflammation in cirrhotic patients [11]. Kawasaki disease is also a systemic febrile inflammatory disease. However, no studies have investigated the role of the tight junction ZO-1 protein in the development of KD vasculitis. The purpose of this study was to observe the serum ZO-1 levels in KD patients and evaluate the possible association between ZO-1 expression and the disease outcome of KD.
Methods
Patients
According to the American Heart Association [12], the diagnosis of Kawasaki disease can be established using the clinical criteria of fever for ≥5 days (body temperature ≥ 38 °C) and the presence of ≥4 of the 5 following principal clinical features: cervical lymphadenopathy, bilateral non-purulent conjunctivitis, indurative angioedema of the hands and feet, diffuse mucosal inflammation, and polymorphous skin rashes [2]. In this case control study, we enrolled 40 patients who fulfilled the complete criteria of KD (blood samples were collected 24 h before IVIG treatment), 12 healthy controls, and 12 febrile controls. KD patients who were treated pursuant to the American Heart Association’s recommendations [5] of one dose of intravenous immunoglobulin (dosage: 2 g/kg) in a 12-h period. The Institutional Review Board of Chang Gung Memorial Hospital approved the study with registry number 102-5947C. We obtained written informed consent from the parents or guardians of all patients. Patients whose symptoms did not meet the diagnostic criteria of Kawasaki disease were excluded. Coronary artery lesion (CAL) was defined as a coronary artery internal diameter greater than 3 mm (or 4 mm if the patient was more than 5 years old) or of a segment greater than 1.5 times the inner diameter of an adjacent segment exanimated in echocardiography [13, 14]. The definition of patient responsiveness to IVIG treatment was patients’ body temperature within a normal range for 48 h, without recurrence of fever for more than 7 days after completing IVIG treatment, as well as the clinical improvement of inflammatory signs [15, 16]. Febrile control patients were admitted because of upper and/or lower respiratory tract infections, such as acute pharyngitis/tonsillitis, croup, and acute bronchiolitis/bronchitis. Blood samples from the febrile controls were used for comparison. The blood samples were immediately placed in tubes containing heparin, and the remaining serum aliquots were stored at − 80 °C until assay.
Measurement of ZO-1 by enzyme-linked immunoassay (ELISA)
We followed the manufacturer’s instructions to measure ZO-1 (Aviva Systems Biology, OKDD00562) using enzyme-linked immunoassays (ELISA).
Statistical analysis
The data are presented as mean ± standard deviation. We adopted student’s t-test (for comparison of 2 variances) or one-way analysis of variance (ANOVA, for comparison of KD, fever control and health control) to analyze the quantitative data. Multivariate analysis with logistic regression were used to assess the parameters of CAL risk in KD. Statistical significance was considered as two-sided p-values less than 0.05. We used SPSS version 13.0 for Windows XP (SPSS, Inc., Chicago, USA) to perform all the statistical tests.
Results
We enrolled 12 non-fever healthy control (HC) subjects, 12 fever control (FC) patients (patients with fever but without a history of KD or diagnosed as having KD), and 40 KD patients in this study. No significant difference was observed in age or sex between the non-fever healthy control, fever control, and KD groups. All the KD patients met the AHA 2004 diagnostic criteria (complete KD) [5].
The demographic data of HC, FC and KD were showed in Table 1. (age, sex, fever duration, CAL and IVIG resistance) There were no significant difference in regarding age and sex in HC, FC and KD. (p > 0.05) KD patients had higher fever during than FC group (p = 0.03). There were 8 cases with IVIG resistance and 21 cases with CAL formation in KD in this case control study. The average serum tight junction ZO-1 level of each group was 2.15 ± 0.19 ng/mL in the HC group, 2.63 ± 0.18 ng/mL in the FC group, and 2.26 ± 0.12 ng/mL in the KD group. The fever control group had a higher serum ZO-1 level, but did not reach statistical significance (HC vs. FC, P = 0.08; HC vs. KD, p = 0.65; FC vs. KD, p = 0.11) (Fig. 1).
Table 1.
Baseline characteristics of patients with KD and controls
| Characteristic | Healthy controls (n = 12) |
Febrile controls (n = 12) |
KD (n = 40) |
p value |
|---|---|---|---|---|
| Male sex | 4/12 (33.3%) | 5/12 (41.7%) | 20/40 (50%) | 0.573 |
| Age (year, range) | 2.04 ± 0.12 | 2.87 ± 0.41 | 1.87 ± 0.25 | 0.108 |
| (1.4–2.7) | (1.0–4.6) | (0.3–8.5) | ||
| Fever days | 5.75 ± 0.90 | 8.48 ± 0.61 | 0.269 | |
| WBC (1000/uL) | 8.4 ± 0.8 | 8.0 ± 0.7 | 13.2 ± 1.0 | 0.001* |
| RBC (million/Ul) | 4.7 ± 0.1 | 4.4 ± 0.1 | 4.4 ± 0.1 | 0.182 |
| Hemoglobin (g/dL) | 12.5 ± 0.3 | 11.7 ± 0.3 | 11.3 ± 0.1 | 0.001* |
| CRP (mg/L) | 61.0 ± 15.7 | 73.9 ± 12.7 | 0.074 | |
| CAL formation | 21/40 (52.5%) | |||
| IVIG resistance | 8/40 (20%) |
CAL coronary artery lesion, IVIG intravenous immunoglobulin, KD Kawasaki disease, CRP C-Reactive protein, WBC white blood cell, RBC red blood cell
Data expressed as mean ± SD
* indicate p value < 0.05
Fig. 1.
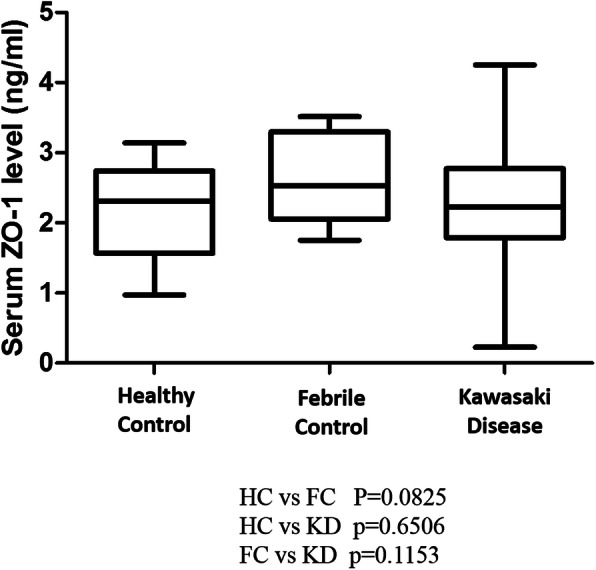
ZO-1 protein expression is determined by ELISA. We enrolled 40 patients with KD, 12 healthy controls, and 12 febrile controls in this study
We classified Kawasaki disease patients into two groups: IVIG responsive (N = 32) and IVIG resistant (N = 8). As shown in Fig. 2, the IVIG-resistant group had a higher serum ZO-1 level, but did not reach statistical significance (2.15 ± 0.12 vs. 2.69 ± 0.31 ng/mL, p = 0.058). In the KD group, which consisted of a total of 40 patients, after removed 8 cases with IVIG resistance, there were 16/32 (50%) patients had CAL for further analysis. The average Z-score of CAL patients was 3.04 ± 0.92. The finding indicates that the CAL group had a significant lower serum levels of tight junction ZO-1 level than without CAL group (1.89 ± 0.16 vs. 2.40 ± 0.15 ng/mL, p = 0.027) (Fig. 3). After multiple logistic regression analysis, ZO-1 levels [(95% confidence interval (CI): 0.058 ~ 0.941, odds ratio (OR) = 0.235, p = 0.041)] showed as the risk factor for CAL formation, but not found in regarding fever duration (95% CI: 0.909 ~ 1.291, OR = 1.08, p = 0.37), IVIG resistance (95% CI: 0.340 ~ 8.175, OR = 1.67, p = 0.53), and age (95% CI: 0.74 ~ 1.67, OR = 1.11, p = 0.61).
Fig. 2.
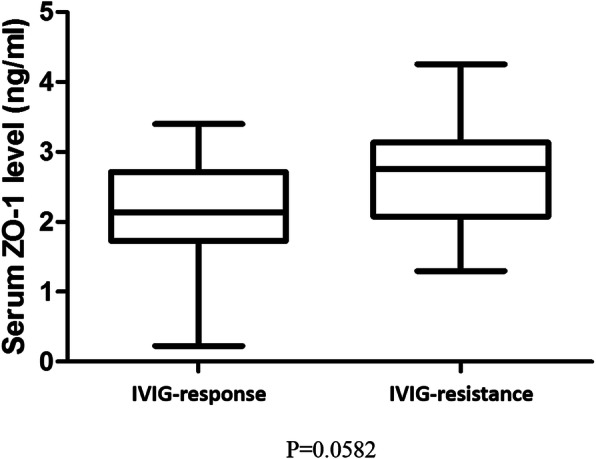
There is no significant difference in ZO-1 protein between intravenous immunoglobulin responsiveness or resistance in Kawasaki disease patients
Fig. 3.
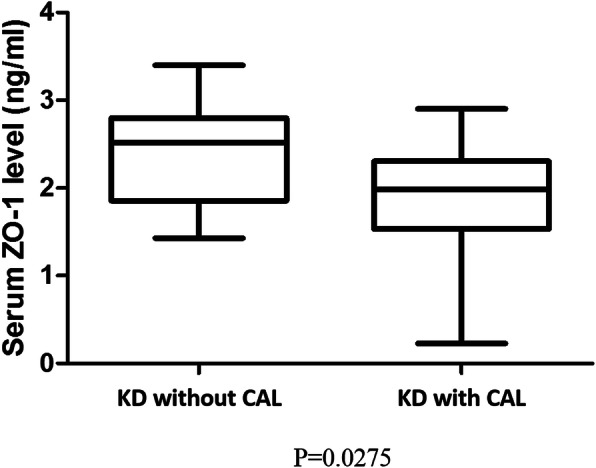
The ZO-1 protein is higher in Kawasaki disease patients with coronary arterial lesion. *p < 0.05. Data are presented as mean ± standard deviation
Discussion
Dr. Tomisaku Kawasaki of Japan first prescribed a case series of Kawasaki disease patients in 1967 [1]. The first case of KD in Taiwan was described in 1976 [17]. The prevalence of KD is highest in Japan [18] and lowest among children of European descent [19]. Although the incidence of Kawasaki disease has been steadily increasing worldwide [20], a definitive disease pathogenesis remains uncertain. A practical biomarker may help physicians to stratify therapy for KD according to the likelihood of developing CAL. Some studies have reported that the tight junction ZO-1 protein was related to some inflammatory diseases and was correlated with the inflammatory marker. Ram et al. reported that hepatocellular carcinoma patients have significantly increased serum ZO-1 levels, which has a positive correlation with inflammatory markers [21]. To the best of our knowledge, our study is the first to survey the correlation of tight junction ZO-1 protein expression in KD patients.
In one KD mice model, TNF-α levels rapidly increased during Lactobacillus-cell wall extract (LCWE)-induced coronary arteritis, as well as were essential to inducing coronary artery inflammation and aneurysm formation [22]. Rochfort reported TNF-αdose-dependent reduced ZO-1 expression in brain endothelium [23]. In our study, lower serum ZO-1 levels were noted in the CAL group among KD patients. Therefore, we may interpret that the serum ZO-1 level has a negative correlation with the development of coronary arterial lesions in humans.
In one mice KD study [24], Lactobacillus-cell wall extract (LCWE)-injected mice developed KD vasculitis and exhibited a significant increase in intestinal leakage. The intestinal barrier dysfunction was associated with decreased Zo-1 expression [25]. Kawasaki disease also affects mucosal intestinal immune responses, and KD patients demonstrated an increased amount of activated macrophages and T cells in the small intestine [6, 8]. New evidence has suggested that strong development of immune responses may lead to endothelial dysfunction, which is also essential for CAL development in Kawasaki disease patients [16, 26, 27].
About 20% of KD patients presented with various gastrointestinal manifestations, such as abdominal distension or pain, vomiting, diarrhea, jaundice, paralytic ileus, hepatomegaly, gallbladder hydrops, and related echographic findings [5, 28, 29]. A recent multicenter study that enrolled more than 300 patients revealed that Kawasaki disease patients with gastrointestinal presentations at the onset of the disease had a complicated KD diagnosis, therapeutic delay, or risk for IVIG-unresponsiveness and coronary aneurysms [7]. Our results showed no significant difference between groups of IVIG responsiveness and resistance in KD patients; however, a similar difference in a slightly larger sample size would have likely resulted in a statistical significance, and further studies are needed. Future research may survey the association between serum ZO-1 levels and IVIG responsiveness in additional large-size studies.
To the best of our understanding, this study was the first to investigate the association between Kawasaki disease and tight junction Zo-1 level. However, the limitation of this study is that the direct correlation between Zo-1 concentration in serum and coronary or intestinal tissue has not been studied in KD patients. This required larger scale of study or further investigation.
Conclusions
In conclusion, tight junction ZO-1 levels decrease in KD patients with coronary artery lesions. Tight junction ZO-1 may participate in the intestinal barrier dysfunction of KD and may be a potential serum marker for predicting CAL in KD patients. The pathophysiological basis of these findings in KD warrants further investigation.
Acknowledgments
The authors wish to acknowledge their patients and the families who agreed to participate in the study.
Abbreviations
- KD
Kawasaki disease
- CAL
Coronary artery lesion
- CAA
Coronary artery aneurysm
- ZO
Zonula occludens
- IVIG
Intravenous immunoglobulin
- TJs
Tight junctions
- HC
Healthy control
- LCWE
Lactobacillus-cell wall extract
Authors’ contributions
WTL, HCL, YHH, and HCK conceptualized and designed the study, drafted the initial manuscript, critically reviewed the manuscript, and approved the final manuscript as submitted. MHL designed the data collection instruments, coordinated and supervised data collection, and approved the final manuscript as submitted.
Funding
This study received funding from the following grants: MOST 108–2314-B-182 -037 -MY3 from the Ministry of Science and Technology of Taiwan, CPRPG8F0793, CMRPG8L0021 and CMRPG8E1611 from Chang Gung Memorial Hospital in Taiwan. Although these institutes provided financial support, they had no influence on the way in which we collected, analyzed, or interpreted the data or wrote this manuscript.
Availability of data and materials
The datasets used and/or analyzed during the current study are not publicly available for ethical and privacy reasons, but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Chang Gung Memorial Hospital (registry number 102-5947C). Informed consent will be obtained in writing from all participants or, in the case of children, their parent or legal guardian, prior to participation.
Consent for publication
Not applicable.
Competing interests
Dr. Ho-Chang Kuo is an associate editor of BMC Pediatrics.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kawasaki T, Kosaki F, Okawa S, Shigematsu I, Yanagawa H. A new infantile acute febrile mucocutaneous lymph node syndrome (MLNS) prevailing in Japan. Pediatrics. 1974;54(3):271–276. [PubMed] [Google Scholar]
- 2.Kuo H-C, Hsu Y-W, Wu M-S, Chien S-C, Liu S-F, Chang W-C. Intravenous immunoglobulin, pharmacogenomics, and Kawasaki disease. J Microbiol Immunol Infect. 2016;49(1):1–7. doi: 10.1016/j.jmii.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 3.Liang CD, Kuo HC, Yang KD, Wang CL, Ko SF. Coronary artery fistula associated with Kawasaki disease. Am Heart J. 2009;157(3):584–588. doi: 10.1016/j.ahj.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 4.Burns JC, Glode MP. Kawasaki syndrome. Lancet. 2004;364(9433):533–544. doi: 10.1016/S0140-6736(04)16814-1. [DOI] [PubMed] [Google Scholar]
- 5.Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the committee on rheumatic fever, endocarditis and Kawasaki disease, council on cardiovascular disease in the young, American Heart Association. Circulation. 2004;110(17):2747–2771. doi: 10.1161/01.CIR.0000145143.19711.78. [DOI] [PubMed] [Google Scholar]
- 6.Nagata S, Yamashiro Y, Maeda M, Ohtsuka Y, Yabuta K. Immunohistochemical studies on small intestinal mucosa in Kawasaki disease. Pediatr Res. 1993;33(6):557–563. doi: 10.1203/00006450-199306000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Fabi M, Corinaldesi E, Pierantoni L, Mazzoni E, Landini C, Bigucci B, et al. Gastrointestinal presentation of Kawasaki disease: a red flag for severe disease? PLoS One. 2018;13(9):e0202658. 10.1371/journal.pone.0202658. [DOI] [PMC free article] [PubMed]
- 8.Rivas MN, Wakita D, Franklin MK, Carvalho TT, Abolhesn A, Gomez AC, et al. Intestinal permeability and IgA provoke immune vasculitis linked to cardiovascular inflammation. Immunity. 2019;51(3):508–21. e6. doi: 10.1016/j.immuni.2019.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rodgers LS, Beam MT, Anderson JM, Fanning AS. Epithelial barrier assembly requires coordinated activity of multiple domains of the tight junction protein ZO-1. J Cell Sci. 2013;126(7):1565–1575. doi: 10.1242/jcs.113399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Boer W, Sharma HS, Baelemans S, Hoogsteden H, Lambrecht B, Braunstahl G-J. Altered expression of epithelial junctional proteins in atopic asthma: possible role in inflammation. Can J Physiol Pharmacol. 2008;86(3):105–112. doi: 10.1139/Y08-004. [DOI] [PubMed] [Google Scholar]
- 11.Karthikeyan A, Mohan P, Chinnakali P, Vairappan B. Elevated systemic zonula occludens 1 is positively correlated with inflammation in cirrhosis. Clin Chim Acta. 2018;480:193–198. doi: 10.1016/j.cca.2018.02.017. [DOI] [PubMed] [Google Scholar]
- 12.McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, et al. Diagnosis, treatment, and long-term Management of Kawasaki Disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135(17):e927–ee99. doi: 10.1161/CIR.0000000000000484. [DOI] [PubMed] [Google Scholar]
- 13.Shulman ST, De Inocencio J, Hirsch R. Kawasaki disease. Pediatr Clin N Am. 1995;42(5):1205–1222. doi: 10.1016/S0031-3955(16)40059-3. [DOI] [PubMed] [Google Scholar]
- 14.Kuo HC, Yu HR, Juo SH, Yang KD, Wang YS, Liang CD, et al. CASP3 gene single-nucleotide polymorphism (rs72689236) and Kawasaki disease in Taiwanese children. J Hum Genet. 2011;56(2):161–165. doi: 10.1038/jhg.2010.154. [DOI] [PubMed] [Google Scholar]
- 15.Kuo HC, Yang KD, Liang CD, Bong CN, Yu HR, Wang L, et al. The relationship of eosinophilia to intravenous immunoglobulin treatment failure in Kawasaki disease. Pediatr Allergy Immunol. 2007;18(4):354–9. 10.1111/j.1399-3038.2007.00516.x. [DOI] [PubMed]
- 16.Kuo HC, Liang CD, Wang CL, Yu HR, Hwang KP, Yang KD. Serum albumin level predicts initial intravenous immunoglobulin treatment failure in Kawasaki disease. Acta Paediatr. 2010;99(10):1578–1583. doi: 10.1111/j.1651-2227.2010.01875.x. [DOI] [PubMed] [Google Scholar]
- 17.Yang H-Y, Lin G-J, Lee C-Y, Lue H-C. Clinical observation of mucocutaneous lymph node syndrome. Acta Paediatr Sin. 1985;26(3):213–222. [Google Scholar]
- 18.Huang W-C, Huang L-M, Chang I-S, Chang L-Y, Chiang B-L, Chen P-J, et al. Epidemiologic features of Kawasaki disease in Taiwan, 2003–2006. Pediatrics. 2009;123(3):e401–e5. 10.1542/peds.2008-2187. [DOI] [PubMed]
- 19.Huang Y-H, Lin K-M, Ho S-C, Yan J-H, Lo M-H, Kuo H-C. Increased incidence of Kawasaki disease in Taiwan in recent years: a 15 years nationwide population-based cohort study. Front Pediatr. 2019;7:121. doi: 10.3389/fped.2019.00121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hall GC, Tulloh LE, Tulloh RMR. Kawasaki disease incidence in children and adolescents: an observational study in primary care. Br J Gen Pract. 2016;66(645):e271–e2e6. doi: 10.3399/bjgp16X684325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ram AK, Pottakat B, Vairappan B. Increased systemic zonula occludens 1 associated with inflammation and independent biomarker in patients with hepatocellular carcinoma. BMC Cancer. 2018;18(1):572. doi: 10.1186/s12885-018-4484-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hui-Yuen JS, Duong TT, Yeung RS. TNF-α is necessary for induction of coronary artery inflammation and aneurysm formation in an animal model of Kawasaki disease. J Immunol. 2006;176(10):6294–6301. doi: 10.4049/jimmunol.176.10.6294. [DOI] [PubMed] [Google Scholar]
- 23.Rochfort KD, Cummins PM. Cytokine-mediated dysregulation of zonula occludens-1 properties in human brain microvascular endothelium. Microvasc Res. 2015;100:48–53. doi: 10.1016/j.mvr.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 24.Noval Rivas M, Wakita D, Abe M, Franklin MK, Chen S, Shimada K, et al. Role of intestinal permeability and secretory iga in the development of cardiovascular pathology in a murine model of kawasaki disease. Circulation. 2017;136(suppl_1):A20825. [Google Scholar]
- 25.Tian S, Guo R, Wei S, Kong Y, Wei X, Wang W, et al. Curcumin protects against the intestinal ischemia-reperfusion injury: involvement of the tight junction protein ZO-1 and TNF-α related mechanism. Korean J Physiol Pharmacol. 2016;20(2):147–52. 10.4196/kjpp.2016.20.2.147. [DOI] [PMC free article] [PubMed]
- 26.Furukawa S, Matsubara T, Motohashi T, Tsuda M, Sugimoto H, Yabuta K. Immunological abnormalities in Kawasaki disease with coronary artery lesions. Pediatr Int. 1991;33(6):745–751. doi: 10.1111/j.1442-200X.1991.tb02603.x. [DOI] [PubMed] [Google Scholar]
- 27.Yamakawa R, Ishii M, Sugimura T, Akagi T, Eto G, Iemura M, et al. Coronary endothelial dysfunction after Kawasaki disease: evaluation by intracoronary injection of acetylcholine. J Am Coll Cardiol. 1998;31(5):1074–80. 10.1016/s0735-1097(98)00033-3. [DOI] [PubMed]
- 28.Yaniv L, Jaffe M, Shaoul R. The surgical manifestations of the intestinal tract in Kawasaki disease. J Pediatr Surg. 2005;40(9):e1–e4. doi: 10.1016/j.jpedsurg.2005.05.063. [DOI] [PubMed] [Google Scholar]
- 29.Chen CJ, Huang FC, Tiao MM, Huang YH, Lin LY, Yu HR, et al. Sonographic gallbladder abnormality is associated with intravenous immunoglobulin resistance in Kawasaki disease. Sci World J. 2012;2012:485758. doi: 10.1100/2012/485758. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are not publicly available for ethical and privacy reasons, but are available from the corresponding author on reasonable request.


