Abstract
Purpose of Review:
To review the epidemiological characteristics and clinical features associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections among children in the United States (US).
Recent Findings:
In the US, the majority of SARS-CoV-2 infections in children have been mild illnesses, with those 5–17 years of age having the highest frequency. Specifically, the incidence of SARS-CoV-2 in children is two times higher in adolescents (12–17 years) than younger school-aged children (5–11 years). Despite the higher case counts in older children, 10% of pediatric hospitalizations have been in infants less than one year. In addition, severe respiratory and renal complications, hospitalization, and even death have been documented in children.
Summary:
Clinical manifestations of SARS-CoV-2 infection in children range from asymptomatic to severe respiratory distress, with mild non-specific symptoms being the most commonly reported. The broad clinical presentation and the frequency of asymptomatic or mimimally symptomatic infections in children pose challenges for controlling and detecting SARS-CoV-2. However, severe disease has been noted in children with associated medical complications and death. Thus, additional active surveillance and research is needed to understand the burden children contribute to the SARS-CoV-2 pandemic in the US.
Keywords: COVID-19, SARS-CoV-2, COVID-19 epidemiology, children
Introduction
The coronavirus disease 2019 (COVID-19) pandemic—caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)—has inflicted significant global morbidity and mortality. On January 7, 2020, SARS-CoV-2 was confirmed as the pathogen causing an outbreak of “pneumonia of unknown etiology” that was initially reported in early December in Wuhan city, Hubei province, China [1,2]. As of October 26, 2020, more than 8.6 million SARS-CoV-2 cases have been identified in the United States (US), of which approximately 580,000 cases have occurred in children under the age of 18 [3]. The majority of reported pediatric cases have been mild; however, severe illness and even death have been documented. In May 2020, an emerging syndrome now known as multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19 was reported to cause systemic inflammation and multisystem organ dysfunction in children and young adults in the weeks following SARS-CoV-2 exposure. In this review, we summarize the epidemiological and clinical characteristics of SARS-CoV-2 infections, exclusive of MIS-C, among children in the US (Table 1).
Table 1.
Studies Assessing Pediatric SARS-CoV-2 Cases in the United States, Excluding MIS-C Published from March-October, 2020
| Authors | Study period | Study location | N | Setting(s) (%) | Ages included | Most common clinical features (%) | No. hospitalized (%) | No. admitted to ICU (%) | No. asymptomatic (%) |
|---|---|---|---|---|---|---|---|---|---|
| Leeb et al. [7] | 03/01/2020–09/19/2020 | US | 277,285 | N/A | 5–17 years | Not reported | 3,240 (1.2) | 404 (0.1) | 12,806 (4.6) |
| CDC COVID-19 Response Team [5] | 02/12/2020–04/02/2020 | US | 2,572 | N/A | <18 years | Fever (56)a Cough (54)a Headache (28)a |
147b (20) | 15b (2) | Unknown |
| Kim et al. [6] | 03/01/2020–07/25/2020 | 14 US states¥ | 576 | Inpatient | <18 years | Fever/chills (54)d Nausea/vomiting (31)d Cough (30)d |
576 (100) | 69e (33) | 0 (0) |
| Howard et al. [38] | 03/12/2020–07/17/2020 | TN | 459 | Inpatient ED Ambulatory |
≤18 years | Cough (51) Fever >100.4°F (42) Headache (41) |
18 (4) | 0 (0) | 46c (1) |
| Otto et al. [4] | 03/09/2020–06/01/2020 | PA and NJ | 424 | Inpatient ED Ambulatory |
≤21 years | Cough (52) Fever (51) Congestion or rhinorrhea (31) |
77 (18) | 25 (5) | 52 (13) |
| Chao et al. [36] | 03/15/2020–04/13/2020 | NY | 67 | Inpatient ED |
1 month-≤21 years | Cough (63) Fever (61) SOB (48) |
46 (69) | 13 (28) | 0 (0) |
| Zachariah et al. [39] | 03/01/2020–04/15/2020 | NY | 50 | Inpatient | ≤21 years | Fever (80) Cough (46) SOB (34) |
50 (100) | Unknown | 0 (0) |
| Lin et al. [42] | 03/26/2020–04/22/2020 | PA, TX, and WA | 12 | Surgical unit | <19 years | Fever (25) Rhinorrhea (17) Cough (8) |
3/12 (25) | Unknown | 6 (50) |
Footnote:
n=291
n=745
n=5752
n=224
n=208
California, Colorado, Connecticut, Georgia, Iowa, Maryland, Michigan, Minnesota, New Mexico, New York, Ohio, Oregon, Tennessee, and Utah; ambulatory includes urgent cares, testing sites, an outpatient settings
Abbreviations: ED, emergency department; N/A, not applicable; NJ, New Jersey; NY, New York; PA, Pennsylvania; SOB, shortness of breath; TX, Texas, US, United States, WA, Washington
Epidemiological Trends of SARS-CoV-2 in Children
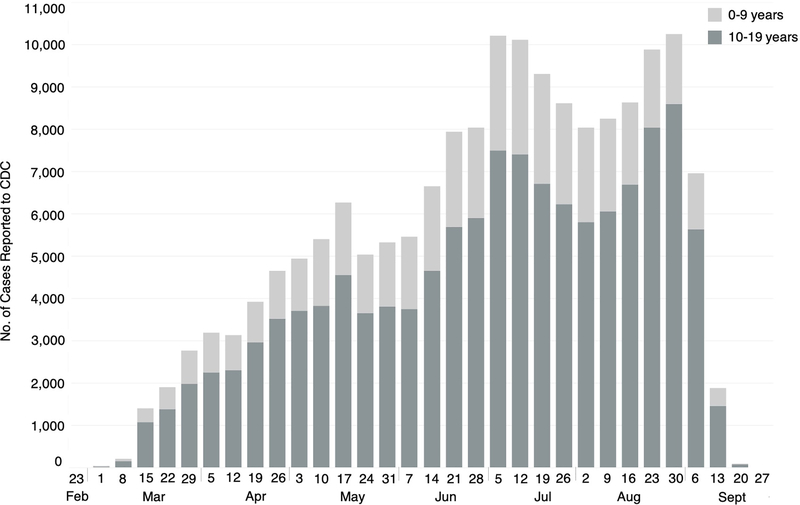
The current epidemiology and trends of SARS-CoV-2 in children remains under-described on a national scale [4], especially in non-hospitalized children. The first pediatric COVID-19 case in the US was reported to the Centers for Disease Control and Prevention (CDC) on March 2, 2020 (Figure 1) [5]. Since then, pediatric cases continue to increase, with children <18 years of age comprising approximately 9% of the number of cases passively reported to the CDC by October 2020 [3]. Among these cases, more than three-quarters have occurred in those aged 5–17 years and 37% among children and adolescents of Hispanic or Latino ethnicity [3]. Children of Hispanic or Latino ethnicity and of black race have higher cumulative rates of hospitalization attributed to SARS-CoV-2 (16.4 and 10.5 per 100,000, respectively) than non-Hispanic white children (Table 1) [6]. The average weekly incidence rate is twice that among adolescents (12–17 years: 37.4 cases per 100,000) as compared to younger children (5–11 years: 19.0 cases per 100,000) [7]. A recent case series evaluating pediatric encounters for SARS-CoV-2 reported that the majority of testing was performed at drive-thru testing sites (2846/7256, 39%) or the emergency department (2311/7256, 32%); and the remaining 29% tests were conducted in three settings: outpatient (15%), inpatient (11%), or urgent care (3%) [4].
Figure 1.
Epidemic Curve of Pediatric Cases Reported to the Centers for Disease Control and Prevention from March-September, 2020, by Age Group
Footnote: Data was retrieved from CDC’s COVID-19 surveillance public use data, last updated September 30, 2020 [41].
Abbreviations CDC, the Centers for Disease Control and Prevention; No. number
Mortality in pediatric cases in the US is less than 1%, supporting prior reports from China, noting milder illness in children compared to adults [3,8]. As of July 31, 2020, public health officials reported 121 SARS-CoV-2 associated deaths in individuals <21 years of age, with 10% occurring in children <1 year, 20% in children 1–9 years, and 70% in children and adolescents aged 10–20 years. Almost two-thirds of deaths (63%) occurred in males, and 45% were Hispanic [9]. Notably, a quarter of these children had no known underlying medical condition [9].
These findings provide a framework for the current trends of SARS-CoV-2 infections in children in the US. However, national case counts likely underestimate the true prevalence of disease due to lack of or limited testing capacity in many locations, limited sensitivity of several SARS-CoV-2 diagnostic tests, and the lack of aggregate case reports from states. Comprehensive active surveillance is needed to understand the complexity of SARS-CoV-2 in children.
Modes of Transmission
SARS-CoV-2 is highly contagious, yet data providing evidence on whether children contribute to transmission as effectively as adults are limited [10]. Although the viral reproductive rate (R0), the average number of secondary transmisisons from a single infected individual, is still being estimated; studies from Wuhan, China have reported a range of R0 to be 2.2–5.7 (95% CI; 1.4–8.9) [1,11]. The R0 vary regionally and may be dependent on a combination of social mitigation strategies and early detection [1]. Nevertheless, compared to other epidemic coronavirus strains (i.e., severe acute respiratory syndrome coronavirus [SARS-CoV] and Middle East respiratory syndrome coronavirus [MERS-CoV]), the estimated R0 is higher in SARS-CoV-2, posing a challenge for controlling spread.
Droplet & Airborne Transmission
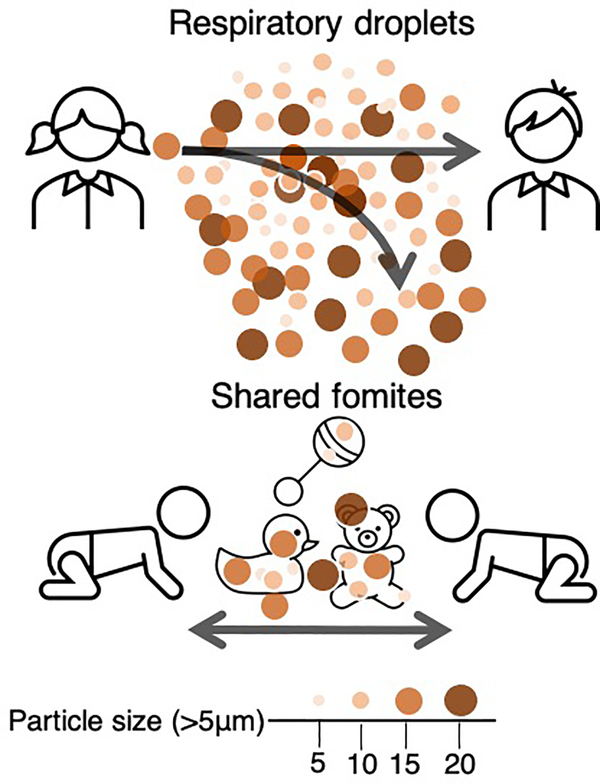
SARS-CoV-2 is transmitted predominantly person-to-person through direct or close contact with an infectious person [12–14]. Infectious respiratory droplets (>5 μm) expelled through coughing, sneezing, or talking may drop to the surrounding environment within 3-to-5 feet of the source person [12,13], leading in turn to transmission to a susceptible person if the droplets reach their eyes, nose, and/or mouth (Figure 2) [12–14]. The role of airborne transmission of SARS-CoV-2 in community transmission is less certain, although this potential is thought to be greater during aerosolizing generating medical procedures (e.g., bronchoscopy, endotracheal intubation and extubation, sputum induction, etc.) [10,14,15]. Aerosols are smaller droplet particles (<5 μm) and may be suspended into the air for hours [13,14,16]. Although at least a few cases of community airborne transmission of SARS-CoV-2 have been suspected [17], public health researchers are still determining whether airborne transmission of SARS-CoV-2 is plausible as a major contributor to community transmission, such as in indoor settings with poor ventilation [12,14,16,18]. Current recommendations to prevent children from contracting SARS-CoV-2 through infectious respiratory droplets include restriction of in-person playtime outside of childcare or school, limitation of contact with persons at an increased risk for severe COVID-19 infections, wearing a mask (children ≥2 years) when in public or around others who they do not reside with, and washing hands often with soap and water for at least 20 seconds [19].
Figure 2.
Primary Routes of Transmission of SARS-CoV-2 in Children.
Infectious respiratory particles (>5 μm) are spread person-to-person primarily through respiratory droplets; however, particles may survive on surfaces and serve as an indirect mode of transmission. Limiting contact with children outside of childcare, wearing of masks (children >2 years), disinfection of toys after use, restricting the use of toys that cannot be disinfected, and assiting children with performing hand hygiene are measures for preventing acquisition of SARS-CoV-2 [20].
Indirect Transmission
Indirect transmission occurs when an individual has contact with an inanimate object or surface (i.e., fomite) that has been contaminated with viable droplet particles containing SARS-CoV-2 [14]. The role of indirect transmission in children is important to understand, specifically in environments such as schools and daycares—where contact with toys and other items or surfaces (i.e., diapering stations, floors, etc.) is often shared. Similar to direct contact, susceptible individuals who touch the fomite and then touch their eyes, nose, or mouth may acquire the virus (Figure 2) [14]. SARS-CoV-2 may be viable on surfaces for prolonged periods (i.e., hours to days), depending on the surface type and temperature of the environment [14]. Outbreak investigations have suggested fomites as a possible source of transmission; however, evidence of transmission solely occurring from a fomite has yet to be documented [13,14]. While these uncertainties remain, recommended prevention efforts to minimize indirect contact transmission among young children include careful disinfection of toys after use, prohibiting the use of toys that cannot be disinfected, disinfection of diapering areas after each child, and assist children with performing hand hygiene regularly [20].
Other Potential Modes of Transmission
In addition to respiratory specimens, SARS-CoV-2 RNA has been detected from other specimen sources, including urine, blood, and feces [14], suggesting potential for non-respiratory modes of transmission. Recently, a brief report from Italy found SARS-CoV-2 from a rectal swab of two infants, suggesting evidence of viral RNA shedding in the feces [21]. However, viral isolation via culture has not always occurred in stool specimens that are positive via molecular diagnostics; thus, it is not clear that these molecular detects reflect infectious viral particles [22]. Additional studies are needed to determine whether fecal-oral transmission in children is possible [21].
In addition, a hospital in Texas has reported a case of SARS-CoV-2 infection in a 24-hour old infant born via vaginal delivery to a mother with COVID-19 [23], thus supporting the potential of intrauterine transmission, although this is likely uncommon, with very few cases of SARS-CoV-2 infection reported in infants in the immediate perinatal period [23]. Despite the other potential modes of transmission, there is no evidence that SARS-CoV-2 is transmitted to an infant from their mother during breastfeeding [14,24]. Breastfeeding should still be encouraged among mothers with suspected and confirmed SARS-CoV-2 infection [14,24].
Pre-symptomatic & Asymptomatic Transmission in the Community
A key component of transmissibility of SARS-CoV-2 is the ability to shed in the upper respiratory tract of infected persons at high viral loads, including those who are in the pre-symptomatic phase of illness [22,25]. In addition, asymptomatic transmission has been postulated to contribute to community propagation [14]. However, the prevalence of asymptomatic transmission is unknown, especially in children, as studies have reported asymptomatic individuals at the time of testing, but after follow-up interviews, many of these persons reported they developed symptoms [14,26]. Nevertheless, children are suggested to be one of the primary age-groups contributing to asymptomatic transmission [27].
Illustratively, two community outbreak investigations have reported asymptomatic transmission among children [28,29]. The first study by Szablewski et al. investigated an SARS-CoV-2 outbreak among attendees and staff members from an overnight camp in Georgia in June 2020 [29]. A total of 597 Georgia residents attended the camp, of which 344 (58%; ≤19 years) were tested for SARS-CoV-2 after a confirmed case was identified two days following the start of the camp. Among the 344 tested camp attendees, 260 were positive, with a median age of 12 years (range=6–19 years), and 36/136 (26%) cases reported no symptoms [29]. A second SARS-CoV-2 investigation from three separate childcare facilities noted that 12/110 (11%) children (age range: 0.2–16 years) tested positive for SARS-CoV-2, of which three (25%) were asymptomatic [28]. Secondary transmission was identified among seven household contacts of these 12 children. Notably, two of the secondary cases were contacts of two asymptomatic children [28]. Overall, both outbreak investigations provide evidence that children play a role in asymptomatic transmission. Additional research is needed to determine the transmission rate among asymptomatic children.
Incubation Period
The time between contracting SARS-CoV-2 and developing symptoms (incubation period) in children is similar to that in adults with an average of 5–6 days (range: 2–14 days) [10,30]. Studies have shown that approximately 98% of persons who develop symptoms will show signs within 11.5 days after being infected [31]. The infectious period still remains unclear; but evidence suggests that persons are contagious around two days prior to symptom onset and remain infectious for a minimum of 10 days after symptoms started [30]. For those who are asymptomatic, it is hypothesized that the infectious period may extend for at least 10 days following the first positive test result [30]. Additionally, children with an immunodeficiency can shed the virus for weeks [32].
Clinical Features
In general, children and adults share many of the same clinical manifestations of SARS-CoV-2, ranging from asymptomatic to severe respiratory distress [10,33]. For both age groups, severe disease is more frequent in persons with underlying medical conditions, including obesity and asthma [34,35]. Children with SARS-CoV-2 present with a wide array of non-specific symptoms, such as fever, fatigue, headache, myalgia, cough, rhinorrhea, shortness of breath, abdominal pain, diarrhea, nausea, vomiting, and/or poor appetite [10]. Reports from the US have shown most children who develop mild symptoms primarily present with fever and/or cough, (56% and 54%, respectively) (Table 1). These same symptoms have been documented at a higher frequency in hospitalized children (80% and 63%, respectively) (Table 1) [5,6,36]. In addition to fever and cough, 42% hospitalized children have reported experiencing at least one gastrointestinal symptom (nausea, vomiting, diarrhea, or abdominal pain) (Table 1) [6]. The clinical symptoms in children with SARS-CoV-2 are similar to the 2009 influenza H1N1 pandemic where nearly a quarter of children presented with gastrointestinal symptoms; with higher frequencies in children with severe disease, including hospitalizations [37]. Despite these similarities, two unique clinical features, anomia and ageusia, have been reported in cases with SARS-CoV-2; less frequently being reported in children than adults [38].
While children are less likely to develop severe SARS-CoV-2 illness compared to adults, severe complications have been reported [10]. Complications that have been described include pneumonia, acute respiratory failure, acute kidney injury, diabetic ketoacidosis, and acute distress syndrome (Table 1) [6]. Reports of abnormal radiographic findings have also been reported in children. For example, Kim et al. demonstrated 208 hospitalized children with SARS-CoV-2 infections, 67 children had a chest radiograph performed and of those, 44 (66%) had an infiltrate or consolidation [6]. Further, 71% (10/14) children had ground-glass opacities—a nonspecific sign indicating infection or alveolar disease—depicted from a chest computed tomography scan [6]. Whether these complications and/or abnormal radiographic findings will be short-term and/or have long-term lasting effects remains unclear and needs further investigation.
Clinical Outcomes
The vast majority of children with SARS-CoV-2 require no and/or little medical attention and are managed in the ambulatory setting. Hospitalization has been associated with an estimated 1–20% of pediatric SARS-CoV-2 infections, although this may be an overestimate, given that many asymptomatic or minimally symptomatic pediatric SARS-CoV-2 infections may go undiagnosed (Table 1) [4,5,7,38]. Underlying medical conditions, including asthma and obesity, have been identified as important risk factors for more severe disease requiring hospitalization [4,39,40]. In one report assessing hospitalization rates and characteristics of 576 children with SARS-CoV-2 infections from 14 states, the frequency of hospitalization was highest in children younger than two years compared to other pediatric age groups [6]. Nearly a quarter of hospitalizations were in infants younger than three months (Table 1) [6]. This study also noted that 42% (94/222) of children had an underlying medical condition (obesity: 42/111, 38% and asthma: 30/222, 14%) [6]. The median hospital duration was 2.5 days (IQR: 1–5 days), 33% (69/424) children were admitted to the intensive care unit (ICU), and 6% (12/207) required mechanical ventilation (Table 1) [6]. Despite the fact that one-third of children were admitted to the ICU, mortality attributed to SARS-CoV-2 was less than one percent [6]. In another study, similar demographic characteristics were reported; however, 16% of children required mechanical ventilation and 3% died (Table 1) [4]. Additional reports of clinical characteristics are needed to better understand the potential risk factors and severe outcomes of SARS-CoV-2 infections in children. Understanding why children have milder disease compared to adults remains an important question and additional research is required.
Conclusion
Currently, SARS-CoV-2 cases in children account for 9% of all reported cases in the US [3]. Specifically, COVID-19 incidence among adolescents aged 12–17 years was approximately twice that in children aged 5–11 years. Although most children have predominantly developed mild disease, severe illness has been reported, mainly in children with comorbidities. The broad clinical presentation and the frequency of asymptomatic infections in children pose challenges for controlling and detecting SARS-CoV-2. Additional research is vital to understand the mechanisms of why the majority of children appear to be less susceptible than adults to severe SARS-CoV-2 associated disease.
Key points:
Detected prevalence of SARS-CoV-2 infections in children is lower than adults and elderly.
Children predominantly present with mild illness; however, severe complications, hospitalizations, and death have been reported.
Due to the broad clinical presentation and frequency of asymptomatic or minimally symptomatic infections, children pose unique challenges to controlling and detecting SARS-CoV-2.
SARS-CoV-2 is transmitted person-to-person through direct or close contact with an infectious individual, mainly through respiratory droplets.
Acknowledgments
Financial Support and Sponsorship
Danielle A. Rankin is supported by the National Institutes of Health under award number TL1TR002244 and Dr. Howard is supported by the National Institutes of Health under award number 1K23AI141621.
Conflicts of Interest
Dr. Halasa receives grant support from Sanofi, Quidel, and speaker compensation from an education grant supported by Genentech. Sanofi also donated vaccines and influenza antibody testing for influenza vaccine trial.
Abbreviations:
- COVID-19
coronavirus disease, 2019
- CDC
Centers for Disease Control and Prevention
- children
less than 18 years
- ICU
intensive care unit
- MERS-CoV
Middle East respiratory syndrome coronavirus
- SARS-CoV
severe acute respiratory syndrome coronavirus
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2
- (US)
United States
References
* denotes special interest
** denotes outstanding interest
- 1.Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R: High Contagiousness and Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2. Emerg Infect Dis 2020, 26:1470–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO: Novel Coronavirus (2019-nCoV) Situation Report-1 Edited by; 2020. vol 2020.] [Google Scholar]
- 3.CDC: CDC COVID Data Tracker. Edited by; 2020. vol 2020.] [Google Scholar]
- 4.Otto WR, Geoghegan S, Posch LC, Bell LM, Coffin SE, Sammons JS, Harris RM, Odom John AR, Luan X, Gerber JS: The Epidemiology of Severe Acute Respiratory Syndrome Coronavirus 2 in a Pediatric Healthcare Network in the United States. Journal of the Pediatric Infectious Diseases Society 2020.** This is one of the largest studies assessing the epidemology of pediatric cases in the United States across healthcare settings (i.e., ambulatory care, testing facilities, emergency department, and inpatient). These findings will help public health officials with implementing and developing guidance for preventing children from acquiring SARS-CoV-2.
- 5.CDC COVID-19 Response Team: Coronavirus Disease 2019 in Children - United States, February 12-April 2, 2020. MMWR Morb Mortal Wkly Rep 2020, 69:422–426.** This is the first surveillance study reported from the Centers for Disease Control and Prevention. These findings provide vital information on the first clinical manifestations and epidemiology of SARS-CoV-2 in children.
- 6.Kim L, Whitaker M, O’Halloran A, Kambhampati A, Chai SJ, Reingold A, Armistead I, Kawasaki B, Meek J, Yousey-Hindes K, et al. : Hospitalization Rates and Characteristics of Children Aged <18 Years Hospitalized with Laboratory-Confirmed COVID-19 - COVID-NET, 14 States, March 1-July 25, 2020. MMWR Morb Mortal Wkly Rep 2020, 69:1081–1088.** This study is one of the largest population-based surveillance study describing pediatric hospitalizations attributed to COVID-19 in the United States. The authors findings provide context about hospitalizations across 14 states, which likely provides generalizeable epidemiologic data on pediatric COVID-19 infections.
- 7.Leeb RT, Price S, Sliwa S, Kimball A, Szucs L, Caruso E, Godfred-Cato S, Lozier M: COVID-19 Trends Among School-Aged Children - United States, March 1-September 19, 2020. MMWR Morb Mortal Wkly Rep 2020, 69:1410–1415.* This study assessed the incidence rates of COVID-19 infections among school-aged children dating back to the first reported pediatric case in the United States.
- 8.Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, Tong S: Epidemiology of COVID-19 Among Children in China. Pediatrics 2020, 145. [DOI] [PubMed] [Google Scholar]
- 9.Bixler D, Miller AD, Mattison CP, Taylor B, Komatsu K, Peterson Pompa X, Moon S, Karmarkar E, Liu CY, Openshaw JJ, et al. : SARS-CoV-2-Associated Deaths Among Persons Aged <21 Years - United States, February 12-July 31, 2020. MMWR Morb Mortal Wkly Rep 2020, 69:1324–1329.* This study provides insightful characteristics of pediatric deaths associated with SARS-CoV-2 infections in the United States.
- 10.CDC: Information for Pediatric Healthcare Providers. Edited by; 2020. vol 2020.]* This guidance provides valuable and up-to-date information for pediatric healthcare providers caring for children with SARS-CoV-2.
- 11.Petersen E, Koopmans M, Go U, Hamer DH, Petrosillo N, Castelli F, Storgaard M, Al Khalili S, Simonsen L: Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect Dis 2020, 20:e238–e244.* This study assesses the reproductive rate of SARS-CoV-2 and compares to other viruses (i.e., SARS-CoV, MERS-CoV, and influenza) that have historically contributed to large outbreaks, epidemics, and pandemics.
- 12.Meselson M: Droplets and Aerosols in the Transmission of SARS-CoV-2. N Engl J Med 2020, 382:2063.* This is a correspondence that provides a concise overview of the modes of SARS-CoV-2 transmission.
- 13.Meyerowitz EA, Richterman A, Gandhi RT, Sax PE: Transmission of SARS-CoV-2: A Review of Viral, Host, and Environmental Factors. Ann Intern Med 2020.** This study provides a comprehensive review of the factors that affect transmisison of SARS-CoV-2. These findings may provide knowledge to assist in educating the public and further slowing the spread of SARS-CoV-2.
- 14.WHO: Transmission of SARS-CoV-2: implications for infection prevention precautions. Edited by; 2020. vol 2020.]* This scientific brief by the World Health Organization provides an overview of the modes of transmission and the infection control strategies and recommendations for halting transmission of SARS-CoV-2.
- 15.CDC: Clinical Questions about COVID-19: Questions and Answers. Edited by; 2020. vol 2020.] [Google Scholar]
- 16.Klompas M, Baker MA, Rhee C: Airborne Transmission of SARS-CoV-2: Theoretical Considerations and Available Evidence. Jama 2020, 324:441–442. [DOI] [PubMed] [Google Scholar]
- 17.CDC: Scientific Brief: SARS-CoV-2 and Potential Airborne Transmission. Edited by; 2020. vol 2020.]* This scientific brief from the Centers for Disease Control and Prevention provides the concept for the potential for SARS-CoV-2 to be transmitted though aerosols.
- 18.Prather KA, Wang CC, Schooley RT: Reducing transmission of SARS-CoV-2. Science 2020, 368:1422–1424. [DOI] [PubMed] [Google Scholar]
- 19.CDC: Help Stop the Spread of COVID-19 in Children. Edited by; 2020. vol 2020.] [Google Scholar]
- 20.CDC: Guidance for Child Care Programs that Remain Open. Edited by; 2020. vol 2020.] [Google Scholar]
- 21.Donà D, Minotti C, Costenaro P, Da Dalt L, Giaquinto C: Fecal-Oral Transmission of SARS-CoV-2 In Children: is it Time to Change Our Approach? Pediatr Infect Dis J 2020, 39:e133–e134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, Niemeyer D, Jones TC, Vollmar P, Rothe C, et al. : Virological assessment of hospitalized patients with COVID-2019. Nature 2020, 581:465–469.* This study gives an overview of the specimen sources that render replication of SARS-CoV-2.
- 23.Sisman J, Jaleel MA, Moreno W, Rajaram V, Collins RRJ, Savani RC, Rakheja D, Evans AS: Intrauterine Transmission of SARS-COV-2 Infection in a Preterm Infant. Pediatr Infect Dis J 2020, 39:e265–e267. [DOI] [PubMed] [Google Scholar]
- 24.Lubbe W, Botha E, Niela-Vilen H, Reimers P: Breastfeeding during the COVID-19 pandemic - a literature review for clinical practice. Int Breastfeed J 2020, 15:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gandhi M, Yokoe DS, Havlir DV: Asymptomatic Transmission, the Achilles’ Heel of Current Strategies to Control Covid-19. N Engl J Med 2020, 382:2158–2160.* This editorial provides insight to asymptomatic transmission of SARS-CoV-2 and the current public health measures in place to control spread.
- 26.Kimball A, Hatfield KM, Arons M, James A, Taylor J, Spicer K, Bardossy AC, Oakley LP, Tanwar S, Chisty Z, et al. : Asymptomatic and Presymptomatic SARS-CoV-2 Infections in Residents of a Long-Term Care Skilled Nursing Facility - King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep 2020, 69:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DeBiasi RL, Delaney M: Symptomatic and Asymptomatic Viral Shedding in Pediatric Patients Infected With Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): Under the Surface. JAMA Pediatr 2020. [DOI] [PubMed] [Google Scholar]
- 28.Lopez AS, Hill M, Antezano J, Vilven D, Rutner T, Bogdanow L, Claflin C, Kracalik IT, Fields VL, Dunn A, et al. : Transmission Dynamics of COVID-19 Outbreaks Associated with Child Care Facilities - Salt Lake City, Utah, April-July 2020. MMWR Morb Mortal Wkly Rep 2020, 69:1319–1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Szablewski CM, Chang KT, Brown MM, Chu VT, Yousaf AR, Anyalechi N, Aryee PA, Kirking HL, Lumsden M, Mayweather E, et al. : SARS-CoV-2 Transmission and Infection Among Attendees of an Overnight Camp - Georgia, June 2020. MMWR Morb Mortal Wkly Rep 2020, 69:1023–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.CDC: Similarities and Differences between Flu and COVID-19. Edited by; 2020. vol 2020.] [Google Scholar]
- 31.Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC: Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. Jama 2020, 324:782–793.* This study provides an in-depth review of the pathophysiology, clnical presenation, and transmission of SARS-CoV-2.
- 32.Widders A, Broom A, Broom J: SARS-CoV-2: The viral shedding vs infectivity dilemma. Infect Dis Health 2020, 25:210–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tenforde MW, Billig Rose E, Lindsell CJ, Shapiro NI, Files DC, Gibbs KW, Prekker ME, Steingrub JS, Smithline HA, Gong MN, et al. : Characteristics of Adult Outpatients and Inpatients with COVID-19 – 11 Academic Medical Centers, United States, March-May 2020. MMWR Morb Mortal Wkly Rep 2020, 69:841–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cunningham JW, Vaduganathan M, Claggett BL, Jering KS, Bhatt AS, Rosenthal N, Solomon SD: Clinical Outcomes in Young US Adults Hospitalized With COVID-19. JAMA Intern Med 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Götzinger F, Santiago-García B, Noguera-Julián A, Lanaspa M, Lancella L, Calò Carducci FI, Gabrovska N, Velizarova S, Prunk P, Osterman V, et al. : COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health 2020, 4:653–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chao JY, Derespina KR, Herold BC, Goldman DL, Aldrich M, Weingarten J, Ushay HM, Cabana MD, Medar SS: Clinical Characteristics and Outcomes of Hospitalized and Critically Ill Children and Adolescents with Coronavirus Disease 2019 at a Tertiary Care Medical Center in New York City. J Pediatr 2020, 223:14–19.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Halasa NB: Update on the 2009 pandemic influenza A H1N1 in children. Curr Opin Pediatr 2010, 22:83–87. [DOI] [PubMed] [Google Scholar]
- 38.Howard LM, Garguilo K, Gillon J, Seegmiller AC, Schmitz JE, Webber SA, Halasa NB, Banerjee R: Characteristics and clinical features of SARS-CoV-2 infections among ambulatory and hospitalized children and adolescents in an integrated health care system in Tennessee. medRxiv 2020. [Google Scholar]
- 39.DeBiasi RL, Song X, Delaney M, Bell M, Smith K, Pershad J, Ansusinha E, Hahn A, Hamdy R, Harik N, et al. : Severe Coronavirus Disease-2019 in Children and Young Adults in the Washington, DC, Metropolitan Region. J Pediatr 2020, 223:199–203.e191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zachariah P, Johnson CL, Halabi KC, Ahn D, Sen AI, Fischer A, Banker SL, Giordano M, Manice CS, Diamond R, et al. : Epidemiology, Clinical Features, and Disease Severity in Patients With Coronavirus Disease 2019 (COVID-19) in a Children’s Hospital in New York City, New York. JAMA Pediatr 2020:e202430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.CDC: COVID-19 Case Surveillance Public Use Data. Edited by; 2020. [Google Scholar]
- 42.Lin EE, Blumberg TJ, Adler AC, Fazal FZ, Talwar D, Ellingsen K, Shah AS: Incidence of COVID-19 in Pediatric Surgical Patients Among 3 US Children’s Hospitals. JAMA Surg 2020, 155:775–777. [DOI] [PMC free article] [PubMed] [Google Scholar]