Abstract
The COVID-19 pandemic is a public health emergency. Individuals with substance use disorder have a higher risk of infection and may suffer from more severe forms of the disease. Our goal is to investigate the prevalence of risk factors for COVID-19 severity in individuals with different substance use and explore whether specific types of substance are potentially associated with more clinical risk factors which could increase morbimortality in this population. The sample included 821 men hospitalized at an inpatient Addiction unit (305 alcohol users, 233 cocaine/crack users, and 283 multiusers). Data were collected using the Addiction Severity Index version 6. The most prevalent risk factors for COVID-19 severity observed in our sample were: smoking (82.5%), arterial hypertension (26.6%), respiratory problems (23.4%), and history of homelessness (25.1%). Arterial hypertension and cirrhosis occurred more frequently among alcohol users. Multiusers lived in the streets longer and had a higher prevalence of HIV than alcohol users. Overall, 28% of the sample had three or more risk factors. The frequency of risk factors was high and this scenario suggests that these individuals could be more susceptible to worse COVID-19 prognosis. Therefore, prevention strategies directed at specific characteristics of substance users merit attention during the pandemic.
Keywords: Crack cocaine, Substance use disorders, Addiction, Pandemic
1. Introduction
The identification of vulnerable individuals and those who are more susceptible to the infection for COVID-19 – with more severe clinical conditions and higher mortality rates – is essential to implement specific and efficient strategies (CDC, 2020). Individuals with substance use disorder (SUD) have a complex clinical profile, presenting many psychiatric and clinical comorbidities, besides social vulnerabilities (Lagisetty et al., 2017; Peacock et al., 2018). This population often has an unhealthy lifestyle, represented by poor nutritional status (Jeynes and Gibson, 2017) and body mass index, lack of exercise (Blackstone and Herrmann, 2016; Sayon-Orea et al., 2011; Traversy and Chaput, 2015), with compromised employment and academic performance (WHO, 2020). Moreover, vulnerable populations are less likely to adopt protective measures (for example, wearing masks, hand sanitizers, and social distancing), hampering the implementation of public health policies (Mesa Vieira et al., 2020). In this population, the countless difficulties related to accessing the health system and the monitoring of treatment end up aggravating this challenging scenario.
In addition, immunological alterations have been observed in individuals with SUD (Cohen et al., 1993; Schuch-Goi et al., 2017; Sureshchandra et al., 2019; Zaparte et al., 2019). Studies showed that alcohol and cocaine/crack abuse increase the risk for infectious diseases (Butler et al., 2017; GBD 2016 Alcohol and Drug Use Collaborators., 2018; Halpern et al., 2017; Peacock et al., 2018; WHO, 2018). For instance, the use of substances facilitates influenza infection and leads to a worse prognosis (Godoy et al., 2018; Meyerholz et al., 2008).
In this sense, individuals diagnosed with SUD might have an increased risk of COVID-19 and a worse prognosis. Indeed, higher rates of hospitalizations and deaths were observed in individuals with SUD and COVID-19 compared to individuals with COVID-19 but without SUD (Wang et al., 2021). Nonetheless, these individuals still have received little attention during the COVID-19 pandemic (Harris, 2020; Ornell et al., 2020), mainly in developing countries.
All of these aspects represent major challenges for the health system. Public policies for individuals who use substances should be developed based on the particularities of this population, including prevention and treatment strategies that address both medical and psychosocial care. Since few data is available, the first step to implement these policies is to identify epidemiological characteristics and vulnerabilities previously associated with COVID-19 severity in this group of individuals. In this sense, our goal is to investigate the prevalence of risk factors for COVID-19 severity in a sample of individuals who use illicit and licit substances and explore whether specific types of substance are potentially associated with more clinical risk factors which could increase morbimortality in this population.
2. Methods
2.1. Sample
The total sample included 821 males with diagnosis of SUD (following DSM-5 criteria) hospitalized at an inpatient unit specialized in drug addiction at a public hospital in Porto Alegre, Brazil. Only individuals with 18 years of age or older who reported alcohol and/or cocaine/crack as the preferred substances were included in the study. Individuals with presence of psychotic disorders, and/or severe cognitive deficits that could impaire the reliability of the answers were excluded
2.2. Procedures
The research protocol was applied by trained junior researchers under the supervision of a senior with broad experience in SUD. This assessment was performed after stabilization of initial withdrawal symptoms (usually between the 5th and the 15th day of hospitalization). Sociodemographic and clinical data, as well as data concerning the patient's substance use profile, were collected using the Addiction Severity Index version 6 (ASI-6) (Kessler et al., 2012). Clinical comorbidities were assessed through self-report. This data was also extracted from ASI-6, and individuals were asked to only report health complications diagnosed by medical or other health professionals, ensuring greater reliability. Additionally, data on the presence of HIV infection was obtained from hospital records, through laboratory tests.
2.3. Ethics
The study was approved by the Ethics committee of Hospital de Clínicas de Porto Alegre (protocol number 2014-0249). All participants provided written informed consent prior to the inclusion.
2.4. Statistical analysis
Data were entered into the online platform REDCap and exported to the IBM SPSS statistics for analysis. Based on recent studies, the following risk factors for COVID-19 severity were evaluated: age, smoking history, positive diagnosis for HIV, clinical comorbidities (hypertension, diabetes, and heart, respiratory, kidney, or liver disease), and recent history of homelessness (living on the streets or in shelters)(Cook et al., 2020; Grasselli et al., 2020; Onder et al., 2020; Shi et al., 2020; Williamson et al., 2020). The age of de patients was described by the mean and standard deviation. Prevalence of factors are presented using percentages and 95% confidence intervals. Association analyses between each risk factor and substance type were performed using Pearson chi-square. All p-values reported were adjusted by Bonferroni correction. In all analyses, a significance level of 5% was adopted.
3. Results
Our sample included 305 alcohol users, 233 cocaine/crack users, and 283 men who used multiple substances (including alcohol and cocaine/crack). Mean age was 41 years; SD:12 years. Regarding the risk factors listed above, we found a high prevalence of smoking history (82.5%), with similar estimates across groups. Other risk factors were frequently detected among individuals with SUD, including arterial hypertension, respiratory problems, and recent history of homelessness (Table 1 ).
Table 1.
Prevalence (95% CI) of risk factors for COVID-19 in individuals with substance use disorder.
| Total n=821 |
Alcohol n=305 |
Cocaine/Crack n=233 |
Multiusers1 n=283 |
|||||
|---|---|---|---|---|---|---|---|---|
| Nicotine dependence | 82.5 | (79.7-85.0) | 80.7 | (75.8-84.9) | 83.7 | (78.3-88.2) | 83.4 | (78.5-87.5) |
| High blood pressure | 26.6 | (23.6-29.7) | 38.0 | (32.6-43.7)a | 12.9 | (8.9-17.9)b | 25.4 | (20.5-30.9)c |
| Homelessness* | 25.1 | (22.1-28.2) | 15.4 | (11.5-20.0)a | 28.4 | (22.6-34.7)b | 32.9 | (27.4-38.7)b |
| Respiratory* | 23.4 | (20.5-26.4) | 23.3 | (18.7-28.4) | 21.2 | (16.1-27.1) | 25.2 | (20.2-30.7) |
| HIV | 7.3 | (5.6-9.3) | 3.7 | (1.9-6.5)a | 7.1 | (4.1-11.3)a,b | 11.4 | (7.9-15.7)b |
| Cardiac disease* | 6.7 | (5.1-8.6) | 11.5 | (8.1-15.6)a | 3.9 | (1.8-7.2)b | 3.9 | (2.0-6.9)b |
| Age > 60 years | 6.3 | (4.8-8.2) | 15.7 | (11.8-20.3)a | 0 | (0-1.6)b | 1.4 | (0.4-3.6)b |
| Diabetes | 5.7 | (4.2-7.6) | 7.9 | (5.1-11.5) | 3.9 | (1.8-7.2) | 4.9 | (2.7-8.1) |
| Cirrhosis | 4.4 | (3.1-6.1) | 7.9 | (5.1-11.6)a | 0.9 | (0.1-3.1)b | 3.5 | (1.7-6.4)a,b |
| Chronic kidney disease* | 3.6 | (2.4-5.1) | 3.6 | (1.8-6.4) | 2.1 | (0.7-4.9) | 4.6 | (2.5-7.7) |
Data shown as % (95% confidence interval). 1Includes individuals with disorders related to the use of multiple substances – cocaine/crack and alcohol. *Respiratory: respiratory problems or tuberculosis; Homelessness: having spent nights on the streets or in shelters within the last 5 months; Cardiac and chronic kidney disease: presence of any cardiac or kidney problem. a,b,cdistinct letters indicate statistically significant differences.
The prevalence of arterial hypertension differed between the three groups of substance users. This risk factor was more frequent among alcohol users, followed by users of multiple substances and cocaine/crack users (p-value ranging between .003 and <.001). History of heart disease was also more prevalent in the alcohol group than in the other two groups (χ²=11.0; p = .003 for cocaine/crack and χ²=12.3; p = .001 for users of multiple substances), as well as the number of individuals over 60 years of age (χ²=58.1; p < .001 for cocaine/crack group and χ²=44.0; p < .001 for users of multiple substances). Moreover, alcohol users present more cirrhosis than cocaine/crack users (χ²=17.2; p < .001). On the other hand, users of multiple substances and cocaine/crack users showed a higher prevalence of recent history of homelessness compared to alcohol users (χ²=24.5; p < .001 and χ²=13.1; p = .001). Users of multiple substances showed a higher frequency of HIV than alcohol users (χ²=12.7; p = .001).
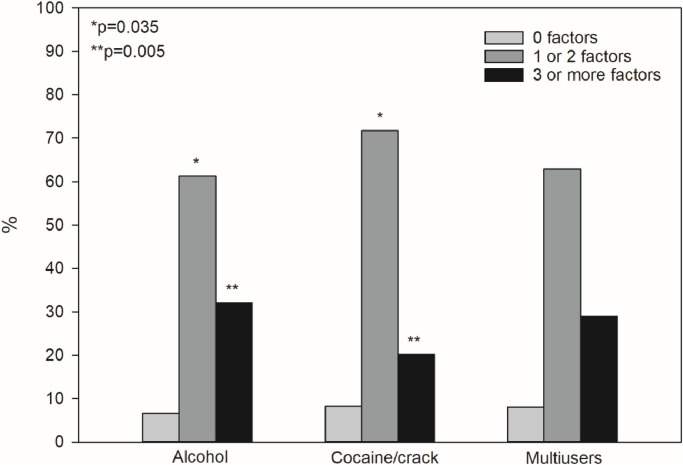
The frequencies of number of risk factors associated with higher COVID-19 severity (from the 10 listed above) in our sample are showed in Fig. 1 . Three or more clinical risk factors were more frequent among alcohol users compared to cocaine/crack users (χ²=9.8; p = 0.005), whom, on the other hand, had a higher frequency of only 1 or 2 factors (χ²=6.4; p = 0.035). Considering our data, approximately 8% of the sample had no risk factors for COVID-19, around 65% had 1 or 2 risk factors, and approximately 28% had 3 or more risk factors.
Fig. 1.
Frequency and comparison of number of risk factors for COVID-19 according to substance use. *Frequency of 1 or 2 factors differs between alcohol and cocaine/crack users (p = 0.035) ⁎⁎Three or more risk factors differs between alcohol and cocaine/crack users (p = 0.005)
4. Discussion
This study shows a high prevalence of risk factors related to the severity and mortality by COVID-19 among users of alcohol and other substances. Alcohol users exhibit a larger number of risk factors for more severe forms of COVID-19 compared to cocaine/crack and multiusers groups. In fact, chronic alcohol use was previously related to metabolic, and hepatic diseases (Li et al., 2019; Stubbs and Morgan, 2011), and cardiac hypertrophy, which may increase the severity of heart disease (Varga et al., 2015). This is alarming since COVID-19 infection could affect multiple organs, such as heart, liver, and hematopoietic tissue, resulting in the worsening of the disease.
Among the risk factors analyzed, the prevalence of tobacco consumption stands out since it is very common in our sample (82%), compared to the estimates for the Brazilian population (15%; Malta et al., 2015b). The use of alcohol and tobacco are risk factors not only for COVID-19, but for other respiratory infections, such as influenza, worsening the prognosis (Godoy et al., 2018; Meyerholz et al., 2008). The effects of tobacco on lung health and on the immune system make this population especially vulnerable to COVID-19 (Vardavas and Nikitara, 2020). Accordingly, a recent Chinese study found that patients with smoking history are 14 times more likely to progress from COVID-19 to pneumonia (Liu et al., 2020).
In addition, the prevalence of chronic diseases in our sample is higher than in the general Brazilian population (Sousa et al., 2012), especially in alcohol users. These individuals are typically older when seeking treatment for addiction, which contributes to their vulnerability and presence of more chronic conditions. Overall, our sample presents a higher prevalence of hypertension (26.6%, up to 38% in alcohol users) (Malta et al., 2015a), heart disease (6.7%, up to 11.5% in alcohol users), respiratory disease (23.4%) (Leal et al., 2018), kidney disease (3.6%, up to 4.6% in multiusers) (Moura et al., 2015), and cirrhosis (4.4%, up to 7.9% in alcohol users) (de Carvalho et al., 2020) compared to the Brazilian general population (21.4%, 3.9%, 3% 1.4%, and <1% respectively). On the other hand, the rate of diabetes was slightly lower (5.7%) if compared to the data from the National Study on Health (6.2%) (Malta et al., 2015a).
The high prevalence of HIV, of about 7% (in multiusers, this estimate reached 11.4%) found in our study is another important point to be discussed. In Brazil, the estimated prevalence of HIV is 0.4% (Pereira et al., 2019; Szwarcwald et al., 2016). The occurrence of HIV is associated with a substantial imbalance in the immune system, especially regarding CD4+ T cells. Furthermore, the interruption of retroviral treatment was previously described among individuals with SUD (McNeil et al., 2017). Altogether, this scenario illustrates important clinical vulnerabilities and higher susceptibility to infections among individuals with addiction.
Individuals with SUD, especially cocaine/crack users, show higher rates of mental and physical health problems (Santos Cruz et al., 2013). Emotional symptoms, such as fear, loneliness, anxiety, stress, and sadness, might be intensified during the quarantine (Brooks et al., 2020), leading to negative impacts in the lifestyle routine. Especially in individuals with SUD, the management of negative emotions and feelings may be impaired, followed by substance use and relapse (Kelly et al., 2010; Serafini et al., 2016; Sinha et al., 2009). In the United States, for example, there has been an increase in marijuana sales after the onset of the quarantine (Levin, 2020). Individuals can also break through the isolation and go in search of substances, increasing the risk of contamination or even becoming potential vectors of transmission. Despite their numerous vulnerabilities (Halpern et al., 2017), this population faces barriers to access the health system, even in primary care (McNeil et al., 2017). Moreover, around 25% of our sample was homeless recently, being exposed to greater risk situations for infectious diseases, and having less support and access to preventive health measures (Arcadepani et al., 2020). Along with the stigma related to the characteristics of this population, this scenario may result in greater obstacles to treatment of COVID-19 symptoms (Volkow, 2020).
Despite the contributions, this study has some limitations. As our sample was recruited from an inpatient addiction unit, characterized by individuals with severe addiction, the data presented here may not be representative of all individuals who use alcohol or other substances in Brazil. These data may not be generalizable to substances’ users in the community. These findings were analysed from a convenience sample of inpatients, and the frequencies of the factors may be overestimated. Users who require hospitalization may have a greater deleterious effect on health by prolonged use of the substances.
Another limitation involves self-reported data. Although this is a quite common approach in cross-sectional studies, it can be unreliable and influenced by memory bias. However, researchers involved in data collection were instructed to always confirm the data collected with patients, ensuring understanding of the question and the answer obtained. Finally, the presence of psychiatric comorbidities could be a possible confounder, in the sense that other psychiatric disorders, in addition to the substance use disorder itself, may be related to the risk factors analyzed in this study.
In summary, there are three main points in this study: a) people who use substances have more risk factors for COVID-19 than the general population; b) they are more prone to complex clinical conditions, associated with worse prognoses and possibly higher morbimortality by the virus; c) since the literature shows that the emotional effects of the pandemic and the quarantine (or lockdown) may intensify the use of alcohol or other substances, as well as relapse, this study suggests that the surrounding environment, and possibly substance use and substance seeking might increase the risk for infection by physical contact. To this, we add the increased risk due to sharing drug paraphernalia between users of substances such as crack. Neglecting specific characteristics and risks of this population may contribute to the collapse of the health system and impact other areas such as public safety. Therefore, prevention strategies directed at specific characteristics of substance users merit particular attention during the pandemic.
Funding
This study was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) [grant number 478492/2013-8], Secretaria Nacional de Políticas sobre Drogas (SENAD) / Ministério da Justiça e Segurança Pública [grant number 08129.015636/2017-78], Research Support Fund at Hospital de Clínicas de Porto Alegre (FIPE-HCPA) [grant number 2014-0249] and, Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brazil (CAPES) – [finance code 001]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
CRediT authorship contribution statement
Daniela Benzano: Conceptualization, Writing – original draft, Methodology, Formal analysis. Felipe Ornell: Conceptualization, Writing – original draft. Jaqueline Bohrer Schuch: Conceptualization, Data curtion, Writing – review & editing. Flavio Pechansky: Writing – review & editing, Resources. Anne Orgler Sordi: Writing – review & editing. Lisia von Diemen: Writing – review & editing, Resources. Felix Henrique Paim Kessler: Conceptualization, Writing – review & editing, Resources, Supervision.
Declaration of Competing Interest
None
References
- Arcadepani F.B., Tardelli V.S., Fidalgo T.M. The SARS-Cov-2 threat in Cracolândia, an open-air drug use scene in Brazil. Int. J. Drug Policy. 2020 doi: 10.1016/j.drugpo.2020.102835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackstone S.R., Herrmann L.K. Relationships between illicit drug use and body mass index among adolescents. Health Educ. Behav. 2016;43(1):21–24. doi: 10.1177/1090198115579414. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227) doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler A.J., Rehm J., Fischer B. Health outcomes associated with crack-cocaine use: systematic review and meta-analyses. Drug Alcohol Depend. 2017;180:401–416. doi: 10.1016/j.drugalcdep.2017.08.036. [DOI] [PubMed] [Google Scholar]
- CDC . MMWR. Morb. Mortal. Wkly. Rep; United States: 2020. Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions Among Patients with Coronavirus Disease 2019. February 12–March 28, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Tyrrell D.A., Russell M.A., Jarvis M.J., Smith A.P. Smoking, alcohol consumption, and susceptibility to the common cold. Am. J. Public Health. 1993;83(9):1277–1283. doi: 10.2105/ajph.83.9.1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook D.J., Marshall J.C., Fowler R.A. Critical illness in patients with COVID-19: mounting an effective clinical and research response. JAMA. 2020 doi: 10.1001/jama.2020.5775. [DOI] [PubMed] [Google Scholar]
- de Carvalho J.R., Portugal F.B., Flor S.L., Campos R.M., Schramm J.M.A. Method for estimating the prevalence of chronic hepatitis B and C and cirrhosis of the liver in Brazil, 2008. Epidemiol. e Serviços Saúde. 2020;23:9. doi: 10.5123/S1679-49742014000400011. [DOI] [Google Scholar]
- GBD 2016 Alcohol and Drug Use Collaborators. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5(12):987–1012. doi: 10.1016/S2215-0366(18)30337-77-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godoy P., Castilla J., Soldevila N., Mayoral J.M., Toledo D., Martin V., Astray J., Egurrola M., Morales-Suarez-Varela M., Dominguez A. Smoking may increase the risk of influenza hospitalization and reduce influenza vaccine effectiveness in the elderly. Eur. J. Public Health. 2018;28(1):150–155. doi: 10.1093/eurpub/ckx130. [DOI] [PubMed] [Google Scholar]
- Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A., Cereda D., Coluccello A., Foti G., Fumagalli R., Iotti G., Latronico N., Lorini L., Merler S., Natalini G., Piatti A., Ranieri M.V., Scandroglio A.M., Storti E., Cecconi M., Pesenti A., Nailescu A., Corona A., Zangrillo A., Protti A., Albertin A., Forastieri M.A., Lombardo A., Pezzi A., Benini A., Scandroglio A.M., Malara A., Castelli A., Coluccello A., Micucci A., Pesenti A., Sala A., Alborghetti A., Antonini B., Capra C., Troiano C., Roscitano C., Radrizzani D., Chiumello D., Coppini D., Guzzon D., Costantini E., Malpetti E., Zoia E., Catena E., Agosteo E., Barbara E., Beretta E., Boselli E., Storti E., Harizay F., Della M.F., Lorini F.L., Donato S.F., Marino F., Mojoli F., Rasulo F., Grasselli G., Casella G., De-Filippi G., Castelli G., Aldegheri G., Gallioli G., Lotti G., Albano G., Landoni G., Marino G., Vitale G., Battista P.G., Evasi G., Citerio G., Foti G., Natalini G., Merli G., Sforzini I., Bianciardi L., Carnevale L., Grazioli L., Cabrini L., Guatteri L., Salvi L., Dei P.M., Galletti M., Gemma M., Ranucci M., Riccio M., Borelli M., Zambon M., Subert M., Cecconi M., Mazzoni M.G., Raimondi M., Panigada M., Belliato M., Bronzini N., Latronico N., Petrucci N., Belgiorno N., Tagliabue P., Cortellazzi P., Gnesin P., Grosso P., Gritti P., Perazzo P., Severgnini P., Ruggeri P., Sebastiano P., Covello R.D., Fernandez-Olmos R., Fumagalli R., Keim R., Rona R., Valsecchi R., Cattaneo S., Colombo S., Cirri S., Bonazzi S., Greco S., Muttini S., Langer T., Alaimo V., Viola U. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16) doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern S.C., Scherer J.N., Roglio V., Faller S., Sordi A., Ornell F., Dalbosco C., Pechansky F., Kessler F., Diemen L.V. Clinical and social vulnerabilities in crack users according to housing status: a multicenter study in six Brazilian state capitals. Cad. Saude Publica. 2017;33(6) doi: 10.1590/0102-311X00037517. [DOI] [PubMed] [Google Scholar]
- Harris M. An urgent impetus for action: safe inhalation interventions to reduce COVID-19 transmission and fatality risk among people who smoke crack cocaine in the United Kingdom. Int. J. Drug Policy. 2020 doi: 10.1016/j.drugpo.2020.102829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeynes K.D., Gibson E.L. The importance of nutrition in aiding recovery from substance use disorders: a review. Drug Alcohol Depend. 2017;179:229–239. doi: 10.1016/j.drugalcdep.2017.07.006. [DOI] [PubMed] [Google Scholar]
- Kelly J.F., Stout R.L., Tonigan J.S., Magill M., Pagano M.E. Negative affect, relapse, and alcoholics anonymous (AA): does AA work by reducing anger? J. Stud. Alcohol Drugs. 2010;71(3):434–444. doi: 10.15288/jsad.2010.71.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler F., Cacciola J., Alterman A., Faller S., Souza-Formigoni M.L., Cruz M.S., Brasiliano S., Pechansky F. Psychometric properties of the sixth version of the Addiction Severity Index (ASI-6) in Brazil. Rev. Bras. Psiquiatr. 2012;34(1):24–33. doi: 10.1590/s1516-44462012000100006. [DOI] [PubMed] [Google Scholar]
- Lagisetty P.A., Maust D., Heisler M., Bohnert A. Physical and mental health comorbidities associated with primary care visits for substance use disorders. J. Addict. Med. 2017;11(2):161–162. doi: 10.1097/ADM.0000000000000280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leal L.F., Bertoldi A.D., Menezes A.M.B., Borges R.B., Mengue S.S., Gazzana M.B., Pizzol T.D.S.0.D. Indication, access, and use of medicines for chronic respiratory diseases in Brazil: results from the National Survey on Access, Utilization, and Promotion of Rational Use of Medicines in Brazil (PNAUM), 2014. Cad. Saude Publica. 2018;34(10) doi: 10.1590/0102-311X00208217. [DOI] [PubMed] [Google Scholar]
- Levin D. Is Marijuana an ‘Essential’ Like Milk or Bread? Some States Say Yes. https://www.nytimes.com/article/coronavirus-weed-marijuana.html. The New York Times. 2020 [Google Scholar]
- Li X., Jiao Y., Xing Y., Gao P. Diabetes mellitus and risk of hepatic fibrosis/cirrhosis. BioMed Res. Int. 2019 doi: 10.1155/2019/5308308. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W., Tao Z.W., Wang L., Yuan M.L., Liu K., Zhou L., Wei S., Deng Y., Liu J., Liu H.G., Ming Y., Yi H. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin. Med. J. 2020 doi: 10.1097/cm9.0000000000000775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malta D.C., Stopa S.R., Andrade S.S., Szwarcwald C.L., Silva-Júnior J.B., Dos Reis A.A. Health care in adults with self-reported hypertension in Brazil according to the National Health Survey, 2013. Rev. Bras. Epidemiol. 2015;18(Suppl 2) doi: 10.1590/1980-5497201500060010. [DOI] [PubMed] [Google Scholar]
- Malta D.C., Vieira M.L., Szwarcwald C.L., Caixeta R., Brito S.M., Dos-Reis A.A. Smoking trends among Brazilian population - National Household Survey, 2008 and the National Health Survey, 2013. Rev. Bras. Epidemiol. 2015;18(Suppl 2) doi: 10.1590/1980-5497201500060005. [DOI] [PubMed] [Google Scholar]
- McNeil R., Kerr T., Coleman B., Maher L., Milloy M.J., Small W. Antiretroviral therapy interruption among HIV positive people who use drugs in a setting with a community-wide HIV treatment-as-prevention initiative. AIDS Behav. 2017;21(2):402–409. doi: 10.1007/s10461-016-1470-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesa Vieira C., Franco O.H., Gómez Restrepo C., Abel T. COVID-19: the forgotten priorities of the pandemic. Maturitas. 2020;136:38–41. doi: 10.1016/j.maturitas.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyerholz D.K., Edsen-Moore M., McGill J., Coleman R.A., Cook R.T., Legge K.L. Chronic alcohol consumption increases the severity of murine influenza virus infections. J. Immunol. 2008;181(1):641–648. doi: 10.4049/jimmunol.181.1.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moura L., Andrade S.S., Malta D.C., Pereira C.A., Passos J.E. Prevalence of self-reported chronic kidney disease in Brazil: National Health Survey of 2013. Rev. Bras. Epidemiol. 2015;18(Suppl 2) doi: 10.1590/1980-5497201500060016. [DOI] [PubMed] [Google Scholar]
- Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- Ornell F., Moura H.F., Scherer J.N., Pechansky F., Kessler F.H.P., von Diemen L. The COVID-19 pandemic and its impact on substance use: implications for prevention and treatment. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peacock A., Leung J., Larney S., Colledge S., Hickman M., Rehm J., Giovino G.A., West R., Hall W., Griffiths P., Ali R., Gowing L., Marsden J., Ferrari A.J., Grebely J., Farrell M., Degenhardt L. Global statistics on alcohol, tobacco and illicit drug use: 2017 status report. Addiction. 2018;113(10):1905–1926. doi: 10.1111/add.14234. [DOI] [PubMed] [Google Scholar]
- Pereira G.F.M., Pimenta M.C., Giozza S.P., Caruso A.R., Bastos F.I., Guimarães M.D.C. HIV/AIDS, STIs and viral hepatitis in Brazil: epidemiological trends. Rev. Bras. Epidemiol. 2019;22(Suppl 1) doi: 10.1590/1980-549720190001.supl.1. Suppl 1. [DOI] [PubMed] [Google Scholar]
- Santos Cruz M., Andrade T., Bastos F.I., Leal E., Bertoni N., Lipman L., Burnett C., Fischer B. Patterns, determinants and barriers of health and social service utilization among young urban crack users in Brazil. BMC Health Serv. Res. 2013;13:536. doi: 10.1186/1472-6963-13-536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayon-Orea C., Martinez-Gonzalez M.A., Bes-Rastrollo M. Alcohol consumption and body weight: a systematic review. Nutr. Rev. 2011;69(8):419–431. doi: 10.1111/j.1753-4887.2011.00403.x. [DOI] [PubMed] [Google Scholar]
- Schuch-Goi S.B., Scherer J.N., Kessler F.H.P., Sordi A.O., Pechansky F., von Diemen L. Hepatitis C: clinical and biological features related to different forms of cocaine use. Trends Psychiatry Psychother. 2017;39(4):285–292. doi: 10.1590/2237-6089-2016-0076. [DOI] [PubMed] [Google Scholar]
- Serafini K., Toohey M.J., Kiluk B.D., Carroll K.M. Anger and its association with substance use treatment outcomes in a sample of adolescents. J. Child Adolesc. Subst. Abuse. 2016;25(5):391–398. doi: 10.1080/1067828X.2015.1049394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F., Gong W., Liu X., Liang J., Zhao Q., Huang H., Yang B., Huang C. Association of cardiac injury with mortality in hospitalized patients With COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5(7) doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R., Fox H.C., Hong K.A., Bergquist K., Bhagwagar Z., Siedlarz K.M. Enhanced negative emotion and alcohol craving, and altered physiological responses following stress and cue exposure in alcohol dependent individuals. Neuropsychopharmacology. 2009;34(5):1198–1208. doi: 10.1038/npp.2008.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sousa S.P.O., Mascarenhas M.D.M., Silva M.C.B., Almeida R.A.M. Knowledge about mandatory notifiable diseases among professionals of Family Health Strategy in the municipality of Teresina, state of Piauí, Brazil - 2010. Epidemiol. Serv. Saúde. 2012;21:9. doi: 10.5123/S1679-49742012000300012. [DOI] [Google Scholar]
- Stubbs M.A., Morgan M.Y. Managing alcohol dependence and alcohol-related liver disease: a problem for the hepatologist, psychiatrist or economist? Clin. Med. 2011;11(2) doi: 10.7861/clinmedicine.11-2-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sureshchandra S., Raus A., Jankeel A., Ligh B.J.K., Walter N.A.R., Newman N., Grant K.A., Messaoudi I. Dose-dependent effects of chronic alcohol drinking on peripheral immune responses. Sci. Rep. 2019;9(1) doi: 10.1038/s41598-019-44302-3. 7847-7847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szwarcwald C.L., Ferreira Junior O.C., Brito A.M., Luhm K.R., Ribeiro C.E., Silva A.M., Cavalcanti A.M., Ito T.S., Raboni S.M., Souza P.R., Pereira G.F. Estimation of HIV incidence in two Brazilian municipalities, 2013. Rev. Saude Publica. 2016;50 doi: 10.1590/S1518-8787.2016050006310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traversy G., Chaput J.P. Alcohol consumption and obesity: an update. Curr. Obes. Rep. 2015;4(1):122–130. doi: 10.1007/s13679-014-0129-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vardavas C.I., Nikitara K. COVID-19 and smoking: a systematic review of the evidence. Tobacco Induc. Dis. 2020;18 doi: 10.18332/tid/119324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varga Z.V., Ferdinandy P., Liaudet L., Pacher P. Drug-induced mitochondrial dysfunction and cardiotoxicity. American journal of physiology. Heart and circulatory physiology. 2015;309(9) doi: 10.1152/ajpheart.00554.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N. COVID-19: Potential Implications for Individuals with Substance Use Disorders. NIDA. 2020 [Google Scholar]
- Wang Q.Q., Kaelber D.C., Xu R., Volkow N.D. Correction: COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol. Psychiatry. 2021;26(1):40. doi: 10.1038/s41380-020-00895-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; Geneva: 2018. Global Status report on Alcohol and Health 2018. [Google Scholar]
- WHO . W. H. Organization; 2020. World Drug Report 2020. //wdr.unodc.org/wdr2020/en/press.html. [Google Scholar]
- Williamson E.J., Walker A.J., Bhaskaran K., Bacon S., Bates C., Morton C.E., Curtis H.J., Mehrkar A., Evans D., Inglesby P., Cockburn J., McDonald H.I., MacKenna B., Tomlinson L., Douglas I.J., Rentsch C.T., Mathur R., Wong A.Y.S., Grieve R., Harrison D., Forbes H., Schultze A., Croker R., Parry J., Hester F., Harper S., Perera R., Evans S.J.W., Smeeth L., Goldacre B. OpenSAFELY: factors associated with COVID-19 death in 17 million patients. Nature. 2020 doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaparte A., Schuch J.B., Viola T.W., Baptista T.A.S., Beidacki A.S., do Prado C.H., Sanvicente-Vieira B., Bauer M.E., Grassi-Oliveira R. Cocaine use disorder is associated with changes in Th1/Th2/Th17 cytokines and lymphocytes subsets. Front. Immunol. 2019;10 doi: 10.3389/fimmu.2019.02435. [DOI] [PMC free article] [PubMed] [Google Scholar]