Abstract
PURPOSE:
There is a gap in knowledge regarding the use of emergency services by pediatric spina bifida patients. The goal of this study was to describe Emergency Department utilization patterns in this population.
METHODS:
Through a retrospective observational study, patients with spina bifida who visited the emergency department during a four-year period were identified; medical and demographic information was obtained though the Centers for Disease Control National Spina Bifida Patient Registry. Chief complaints and final diagnoses of visits were classified and related to medical needs of spina bifida to determine the appropriate care level.
RESULTS:
Among 303 children within the registry, 161 patients (53%) accounted for 579 visits. 70% of visits were for spina bifida-related complaints. Approximately half (51.7%) had a shunt-related chief complaint, although final diagnosis was largely unrelated to the shunt. Admission rate was 39%, higher than institutional baseline, and largely represented by genitourinary (GU) complaints.
CONCLUSION:
Pediatric patients with spina bifida presenting to a single center emergency department were most likely to present with shunt and urinary concerns; these patients were most likely to be admitted. This potentially suggests that improving outpatient care for bladder management may decrease emergency department use among this population.
Keywords: Pediatrics, spina bifida, emergency care, resource utilization, special health care needs
1. Introduction
Spina bifida, a neurodevelopmental condition that results from failure of embryonic neural tube closure, occurs in approximately 3.7/10,000 births in the United States [1] and occurs across ethnicities [2]. The term spina bifida is inclusive of multiple lesions involving protrusion of neural elements through a defect in the vertebral arches. Myelomeningocele is the most common lesion, involving herniation of the spinal cord, neural elements, and meninges. Myelomeningocele results in variable amounts of damage to the spinal cord due to exposure to amniotic fluid, as well as from incomplete development and maturation of neural pathways. The associated co-morbidities common in children with spina bifida include Chiari II malformation, hydrocephalus, neurogenic bladder and bowel, extremity paralysis and associated limitations in mobility, pressure ulcers, and lower extremity malformation[3–8]. Children and adults with spina bifida require comprehensive multi-disciplinary care to address the many associated sequelae.
Patients with spina bifida may receive prenatal interventions, uniformly need tertiary care as newborns, and often require multiple surgical interventions during childhood. Previous work has documented that children with chronic conditions and developmental disabilities diagnosed in infancy or childhood utilize the healthcare system more than children without these conditions [9–13]. Recognizing the medical complexity and sub-specialty care needs among children with spina bifida, there is also likely a high need for healthcare utilization including acute care services. Studies of adult spina bifida populations have shown higher than baseline admission rates, predominantly due to urinary diagnoses [14,15]. There may be differences in complications and practices within the pediatric population which could impact utilization of acute care services. There is little data available regarding emergency department (ED) usage or admission rates in pediatric patients with spina bifida.
The primary objective of this study is to describe ED utilization patterns among a pediatric population with spina bifida, and to define co-morbidities that may increase this usage. This could inform efforts to provide multidisciplinary coordination of care in the outpatient setting aimed at preventing unnecessary ED visits.
2. Methods
2.1. Study design, population, and setting
This single center study is a retrospective, observational study of ED use in children and adolescents with a diagnosis of spina bifida between the ages of 2 weeks and 25 years. It involves the EDs and urgent care clinics at an urban Level I trauma center and tertiary care teaching hospital with approximately 150,000 visits annually. This study was reviewed and approved by our center’s Institutional Review Board.
The Centers for Disease Control and Prevention (CDC) National Spina Bifida Patient Registry (NS-BPR) is a national electronic registry tool developed to provide a framework for a systematic approach to improving the quality of care received at spina bifida clinics across the United States [16]. The NSBPR collects comparative data on patient demographics, treatment, and outcomes for children, adolescents, and adults who attend spina bifida clinics. All patients seen in the multidisciplinary Center for Spina Bifida clinic were eligible for inclusion in the Registry. Informed consent was obtained at clinic visits.
2.2. Data collection and analysis
A cohort of patients attending the multidisciplinary Center for Spina Bifida were identified by their participation in the NSBPR. Patient co-morbidities, medical and surgical history, and demographic information were extracted from the NSBPR database. The electronic medical record was then queried for ED and urgent care clinic visits by these patients between January 1, 2009 and December 31, 2013. An automated query of medical records yielded visit dates, method of arrival, chief complaint(s) as stated by patient or family, final encounter diagnoses, and disposition. When an automated query did not yield adequate information, the visit record was reviewed by the primary author. Electronic medical records were assessed for relevant data. The linked medical record numbers were then referenced to each patient’s NSBPR information. Data retrieved from the registry included demographics, functional level, ambulation status, shunt status, bladder management strategy and continence, previous surgical history, and the patient’s visit history in the multidisciplinary spina bifida clinic.
Each ED visit was reviewed by 3 authors. Based on the chief complaints, discharge diagnoses, and patient disposition, each visit was classified as whether it was related to spina bifida and if the visit was an appropriate use of emergency services. Classification was performed via independent review by 3 authors (SR, SW, JMD), with consensus reached for each visit. A priori, several categories encompassing common spina bifida-related complaints were determined: shunt, fever, bladder, bowel, injury/fall, and skin. Upon review of each visit record, the chief complaint was classified into one of these categories or placed into an “other” category. For example, a chief complaint of “blood in urine” was placed in the bladder category, whereas “sore throat” was placed in the other category. If one of multiple chief complaints was classified as spina bifida-related, the entire visit was classified as spina-bifida related. Final diagnoses were classified using categorization by ICD-9 codes.
Descriptive statistics were used to characterize the study group. Differences in patient characteristics by emergency department use were tested using a chi square or Fisher’s exact test. SAS version 9.3 (SAS Institute, Cary, NC, USA) was used for data analysis; p values < 0.05 were considered significant.
3. Results
3.1. Patient characteristics
Patient characteristics for the entire cohort stratified by emergency department use are described in Table 1. The most common diagnosis was myelomeningocele (85%); there was a predominance of lumbar lesions with approximately 69% of patients having lumbar functional levels. The majority of patients had postnatal spina bifida repair (95%), with the remaining having fetal repair (5%).
Table 1.
Demographic and clinical characteristics of study population and emergency department (ED) utilization
| Characteristics | Total N = 303 (%) | ED use N = 161 (%) | No ED use N = 142 (%) | p-value |
|---|---|---|---|---|
| Gender | ||||
| Female gender | 170 (56.1) | 85 (52.8) | 85 (59.9) | 0.22 |
| Race | 0.33 | |||
| African American | 19 (6.3) | 13 (8.1) | 6 (4.2) | |
| White | 256 (84.5) | 132 (82) | 124 (87.3) | |
| Other/refused | 28 (9.2) | 16 (9.9) | 12 (8.4) | |
| Diagnosis | 0.10** | |||
| Myelomeningocele/meningocele | 257 (84.8) | 141 (87.6) | 116 (81.7) | |
| Lipoma/fibrolipoma | 44 (14.5) | 18 (11.2) | 26 (18.3) | |
| Cervical myelomeningocele | 1 (0.3) | 1 (0.6) | 0 | |
| Myelocystocele | 1 (0.3) | 1 (0.6) | 0 | |
| Functional level of lesion | 0.02 | |||
| Thoracic | 20 (6.6) | 13 (8.1) | 7 (4.9) | |
| High-lumbar | 34 (11.2) | 23 (14.3) | 11 (7.8) | |
| Mid-lumbar | 82 (27.1) | 50 (31.1) | 32 (22.5) | |
| Low-lumbar | 94 (31.0) | 45 (28.0) | 49 (34.5) | |
| Sacral | 73 (24.1) | 30 (18.6) | 43 (30.3) | |
| Ambulation status (at first annual visit) | 0.64 | |||
| Community ambulators | 128 (42.2) | 64 (39.8) | 64 (45.1) | |
| Household ambulators | 11 (3.6) | 5 (3.1) | 6 (4.2) | |
| Non-/non-functional-ambulators | 131 (43.2) | 75 (46.6) | 56 (39.4) | |
| Not applicable due to age | 33 (10.9) | 17 (10.6) | 16 (11.3) | |
| Prenatal closures | 14 (4.6) | 6 (3.7) | 8 (5.6) | 0.43 |
| Presence of shunted hydrocephalus | 205 (67.7) | 120 (74.5) | 85 (59.9) | 0.006 |
| Continence* | ||||
| Bladder | 70/280 (25.0) | 35/152 (23.0) | 35/128 (27.3) | 0.41 |
| Bowel | 71/280 (25.4) | 36/152 (23.7) | 35/128 (27.3) | 0.48 |
Missing data
Fisher’s exact test.
3.2. Emergency department utilization
Among 303 patients with spina bifida identified in the CDC registry, 161 (53%) accounted for 579 ED visits during the study period (Table 1). Of the 161 patients using the ED, forty nine (30%) had only one visit, while 112 (70%) had multiple visits (Table 2). ED utilization was highest in the first few years of life (Fig. 1), with a median age of 6.7 years (range 2 weeks to 25 years). There was no difference in ED utilization by age based on birth year. The functional level of the lesion was significantly associated with ED visits (p = 0.02); those with higher lesion levels were most likely to utilize the ED (Table 1). The presence of shunted hydrocephalus was also associated with an increased risk for ED utilization (p < 0.01). Ambulation status and the presence of bowel or bladder incontinence were not associated with ED utilization.
Table 2.
Characteristics of multi-visit patients
| Multiple ED visits N = 112 (%) | Single ED visit N = 49 (%) | p-value | |
|---|---|---|---|
| Median number of ED visits [IQR] | 3 [2,7] | ||
| Gender | |||
| Female | 57 (50.9) | 28 (57.1) | 0.46 |
| Race | |||
| African American | 8 (7.1) | 5 (10.2) | 0.62 |
| White | 94 (83.9) | 38 (77.6) | |
| Other/refused | 10 (8.9) | 6 (12.2) | |
| Highest functional level | |||
| Thoracic | 12 (10.7) | 1 (2.0) | 0.02 |
| High-lumbar | 18 (16.1) | 5 (10.2) | |
| Mid-lumbar | 37 (33.0) | 13 (26.5) | |
| Low-lumbar | 31 (27.7) | 14 (28.6) | |
| Sacral | 14 (12.5) | 16 (32.6) | |
| Presence of shunted hydrocephalus | 88 (78.6) | 32 (65.3) | 0.07 |
| Continence* | |||
| Bladder | 25/104 (24.0) | 10/48 (20.8) | 0.66 |
| Bowel | 25/104 (24.0) | 11/48 (22.9) | 0.88 |
= missing data.
Fig. 1.
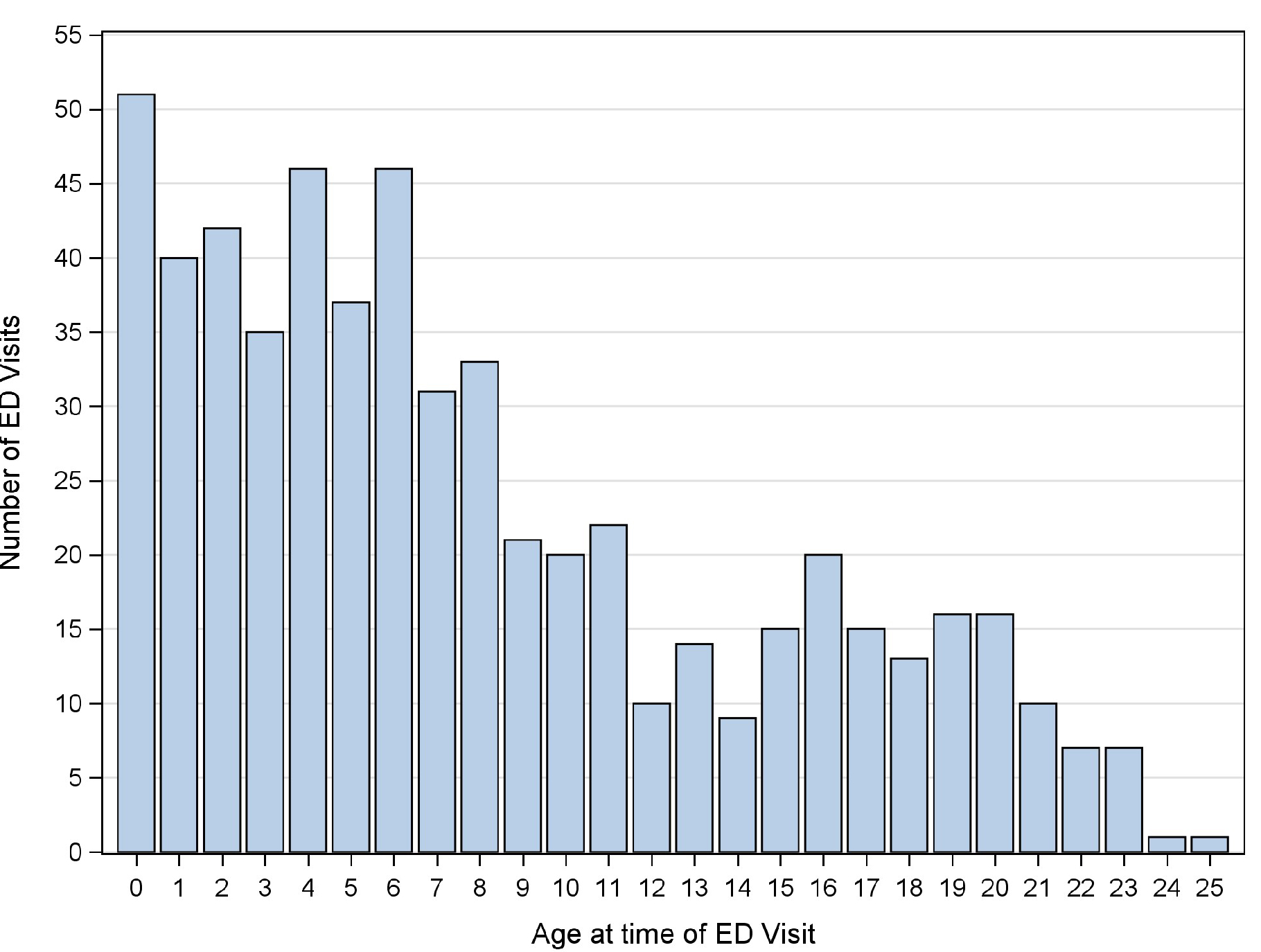
Age at time of ED visit.
Seventy percent of the ED visits were for spina bifida-related complaints, including concerns related to shunts (51.6%), fever (24.4%), bladder (8.1%), bowel (3.9%), injury/fall (11.8%), and skin (1.3%) (Table 3). While fifty-two percent (n = 197) of visits had a chief complaint that was shunt-related, only 20 (10%) of these resulted in a diagnosis of shunt malfunction based on ICD-9 coding. Table 3 displays the chief presenting complaints and final diagnoses for these visits. There was a seasonal pattern with peak use during the winter season (Fig. 2). This suggests that common pediatric problems such as viral illnesses were also occurring in this group of children.
Table 3.
Summary of chief complaints and most common final diagnoses by ICD-9 code; multiple diagnostic codes could be used in a single visit therefore will not equal number of visits
| Chief complaint category | ICD-9 diagnosis | N |
|---|---|---|
| Shunt (N = 197) | Neurogenic bladder | 47 |
| UTI/pyelonephritis | 37 | |
| Headache | 36 | |
| Shunt malfunction | 20 | |
| Hydrocephalus | 19 | |
| Seizure | 11 | |
| Viral illness | 9 | |
| Fever (N = 93) | UTI/pyelonephritis | 47 |
| Neurogenic bladder | 28 | |
| Upper and lower respiratory tract | 13 | |
| Infections (URI/LRTI) | 7 | |
| Neurogenic bowel Viral illness | 6 | |
| Injury (N = 45) | Osteomyelitis | 5 |
| Leg pain | 5 | |
| Fracture | 4 | |
| Fall | 4 | |
| Pressure ulcer | 4 | |
| Cellulitis | 3 | |
| Bladder (N = 31) | UTI/pyelonephritis | 14 |
| Neurogenic bladder | 7 | |
| Hematuria | 4 | |
| Neurogenic bowel/constipation | 4 | |
| Bowel (N = 15) | Neurogenic bowel | 11 |
| Constipation/impaction | 5 | |
| Neurogenic bladder | 5 | |
| Bloody stool | 2 | |
| Skin (N = 5) | Osteomyelitis | 5 |
| Decubitus ulcer | 5 | |
| Neurogenic bladder | 3 | |
| Post-op (N = 15) | Wound dehiscence | 4 |
| Neurogenic bladder | 4 | |
| UTI | 3 | |
| Neurogenic bowel/constipation | 3 | |
| Vomiting | 2 |
N = number of visits.
Table 4 demonstrates that a child’s functional level has an impact on the types of problems leading to emergency department use. Those with thoracic and lumbar lesions will most frequently require cerebrospinal fluid (CSF) diversion, generally by VP shunt. Thus, it is expected that this represents the most common acute care concern in these populations. However, children with sacral lesions require CSF diversion less frequently, and are more commonly ambulatory.
Table 4.
Visit chief complaint by functional level
| Functional level of lesion |
|||||
|---|---|---|---|---|---|
| Thoracic N = 28 (%) | High-lumbar N = 83 (%) | Mid-lumbar N = 130 (%) | Low-lumbar N = 97 (%) | Sacral N = 44 (%) | |
| Shunt | 17 (60.7) | 47 (56.6) | 59 (45.4) | 61 (62.9) | 13 (29.6) |
| Fever | 6 (21.4) | 20 (24.1) | 33 (25.4) | 20 (20.6) | 14 (31.8) |
| Injury/falls | 4 (14.3) | 11 (13.2) | 14 (10.8) | 8 (8.2) | 8 (18.2) |
| Bladder | 2 (7.1) | 8 (9.6) | 15 (11.5) | 3 (3.1) | 3 (6.8) |
| Bowel | 3 (10.7) | 0 | 7 (5.4) | 2 (2.1) | 3 (6.8) |
| Skin | 0 | 2 (2.4) | 3 (2.3) | 0 | 0 |
| Post-op | 0 | 2 (2.4) | 6 (4.6) | 4 (4.1) | 3 (6.8) |
N = number of ED visits.
Multi-visit users represented a large portion of the population utilizing the ED, which were associated with the functional level of the lesion (Table 2). Those with a higher level lesion were most likely to have multiple ED visits (p < 0.02). However, the presence of shunted hydrocephalus was not associated with multiple ED visits.
Of 579 ED visits in the study population, 225 (39%) resulted in hospital admission compared to an institutional baseline rate of 25%. Thirteen patients had a repeat ED visit in less than 48 hours. Children with genitourinary diagnoses, representing the largest organ-specific diagnostic category, were admitted most frequently (49%, n = 44), although digestive (45%), general (49%), and injury categories (47%) resulted in admissions in nearly half of visits (Table 5). Children with shunts were admitted more frequently than children without shunts (85% of visits compared to 28%, p < 0.001), regardless of visit diagnoses.
Table 5.
Disposition by ICD-9 diagnostic category
| Diagnosis category | N | Admit | Discharge home |
|---|---|---|---|
| Genitourinary | 90 | 44 (48.9) | 46(51.1) |
| General | 49 | 24 (49.0) | 25 (51.0) |
| Head/neck | 35 | 8 (22.9) | 27 (77.1) |
| Digestive | 22 | 10 (45.4) | 12 (54.6) |
| Injury | 51 | 24 (47.1) | 27 (52.9) |
4. Discussion
This is the first published study looking at emergency services utilization in a large pediatric population with spina bifida. Based on the described classification, use of acute care services at our center was most often secondary to concerns related to spina bifida and its sequelae. This is consistent with previous studies of adults with spina bifida [17]. Shunt and urinary concerns were common, and children with these symptoms were the most likely to be admitted. Shunt concerns were the most common presenting complaints and carried a high rate of hospital admission regardless of final diagnosis, despite a low occurrence of a diagnosis of shunt malfunction. Urinary diagnoses were the most common, regardless of the presenting complaint and importantly, in those patients with concerns for shunt malfunction.
The admission rate in this pediatric population over the five-year period was 39%, higher than our institutional baseline, which suggests an appropriate utilization of emergency services. Previous work by Caterino et al. [15] demonstrated a 43% admission rate in a group primarily composed of adults with spina bifida, and a predominance of urinary diagnoses. Similarly, in a national sample of hospitalized adults with spina bifida, Dicianno and Wilson [18] found the most common primary diagnosis was urinary tract infection. Our study found similar admission rates (39%) in a pediatric spina bifida population and identified urinary diagnoses as the most common diagnoses in children admitted from the ED. In addition, our study discovered that a large percentage of those patients utilizing the ED presented for multiple visits. Those with the highest risk for ED utilization (i.e., multiple ED visits) were more likely to have higher lesion levels. Furthermore, there was a trend toward being more likely to be shunted (p = 0.07). This is expected, as those with higher lesions are most likely to have the most severe complications of hydrocephalus and paralysis. Patients less than 7 years old represented a small majority in the group; this association with lower age and higher ED use has been documented in pediatric emergency department use generally, and especially in those with chronic conditions [19,20].
These findings may be helpful in identifying patients for which targeted care management or other interventions may have the most impact on utilization and health outcomes. The high rate of urinary concerns provide opportunities to direct efforts towards aggressive bladder management and early assessment of urinary tract infection (UTI) symptoms, which may decrease ED use among this population. This highlights the need for standard care practices, and the importance of studying their impact on acute care utilization. Underscoring this importance, the CDC has recently announced a Quality Initiative aimed at studying and standardizing optimal bladder management practices across the country [21]. Future directions may include quality improvement interventions utilizing nurse coordinators specifically knowledgeable in spina bifida care who can triage patient complaints towards either acute care or outpatient services as appropriate.
Interestingly, injury and falls were not affected by ambulation status but were more common in children with sacral lesions (representing nearly 20% of visits by this group versus 8–14% in other levels; full data not shown). This may imply that patients with sacral lesions are generally ambulatory but have less awareness of potential limitations in mobility, even subtle limitations. While non-ambulators were not more likely to present for fall or injuries than community ambulators, they exclusively represented visits for skin concerns (data not shown). Skin issues were also most common in older patients (median age 16 years; data not shown). This is consistent with a recent study utilizing CDC NSBPR data that identified high rates of skin complaints in patients that had high lesion levels and were associated with wheelchair use [22]. Our findings confirm that skin breakdown prevention is an important potential area for intervention.
This study has several limitations. Its retrospective, single center design may limit generalizability to other institutions or patient populations. We utilized ICD-9 codes to identify diagnoses; in the case of multiple diagnoses, prioritization could not be determined except when based on the order the diagnoses were given by the clinical provider. Reliance on ICD-9 coding may vary across providers and diagnoses not pertinent to the visit could have been missing. Adjudication of visit diagnoses did not allow for accounting of clinical decision-making, such as in the determination of symptomatic UTI versus colonization. However, our center’s practice is for the ED provider to involve Urology consultants experienced with this patient population and condition. Our classification was not based on a validated system, although multiple reviewers were able to achieve consensus. Bias may also be introduced as most patients utilizing the ED may be representative of the local population rather than the multidisciplinary clinic as a whole. Information from recent surgical procedures as well as visits to primary care providers and other institution’s EDs was not available. Data regarding the compliance of patients with spina bifida clinic or pediatrician visits was unavailable. We preliminarily analyzed time and day of patient presentation, to ensure that off hours referral was not confounding ED use in this population (data not shown). The time of day of patient presentation, while an interesting question, does not necessarily correlate with access to outpatient care. Care that may prevent admissions also has to do with access to knowledgeable providers and coordination of care – regardless of time or day. The study is not designed to describe how an intervention, such as a spina bifida clinic, impacted ED utilization – and is a logical next step in this work. Further next steps include reviewing hospital admissions across institutions such as those participating in the NSBPR, and using these methods to identify differences in utilization by institution and associated clinical characteristics.
5. Conclusion
Pediatric spina bifida patients have high ED utilization and hospital admission rates which appear to be largely due to spina bifida-related complaints and sequelae. With high rates of urinary complaints, improving outpatient care for bladder management may represent a targeted area to decrease ED utilization among this population.
Fig. 2.
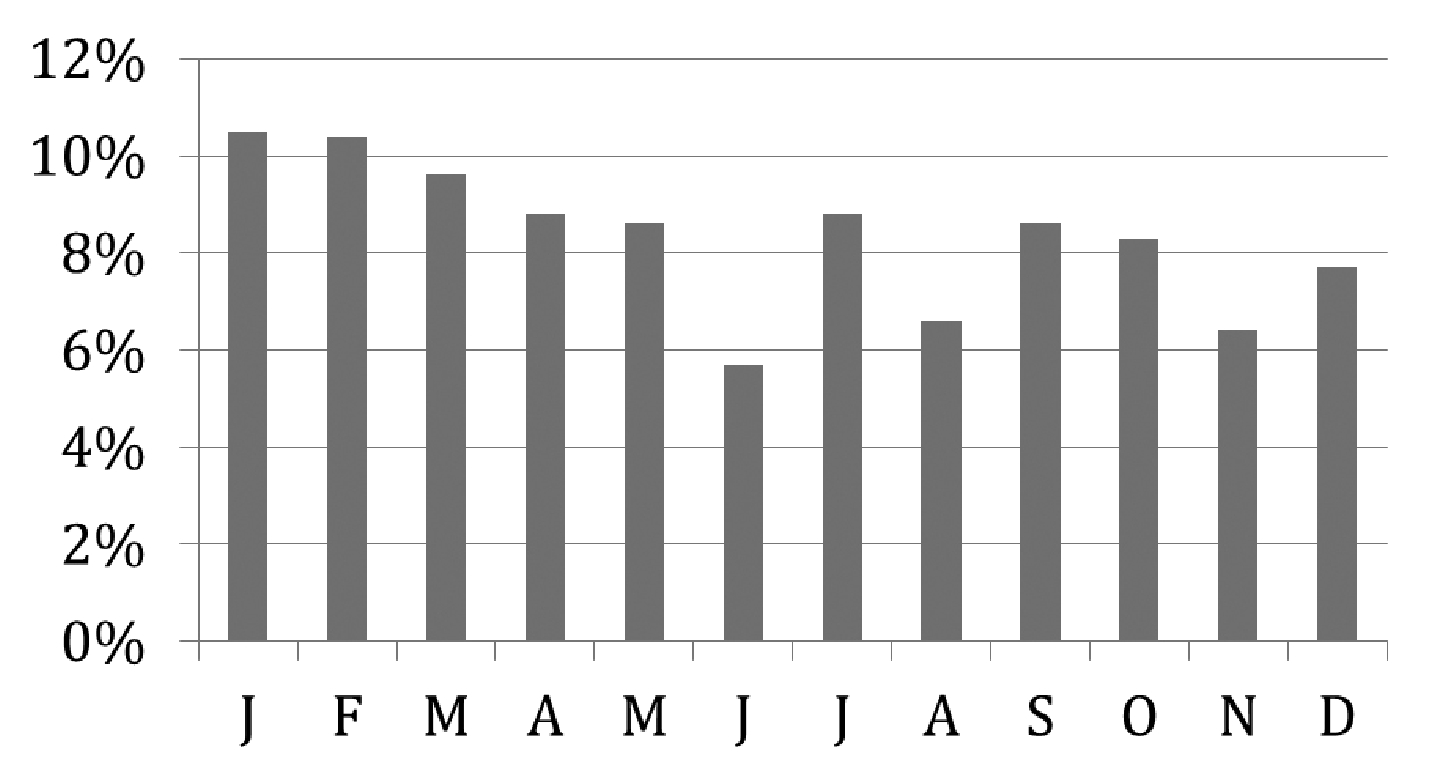
Emergency department visits by month.
Acknowledgments
We acknowledge the Centers for Disease Control and Prevention National Spina Bifida Registry (Centers for Disease Control and Prevention: National Spina Bifida Registry Longitudinal Data Collection and Evaluation, U01 DD) for providing support for the maintenance of our center’s registry.
Footnotes
Conflict of interest
The authors have no conflict of interest to report.
References
- [1].Canfield MA, Honein MA, Yuskiv N, Xing J, Mai CT, Collins JS, et al. National estimates and race/ethnic-specific variation of selected birth defects in the united states, 1999–2001. Birth Defects Res A Clin Mol Teratol. 2006; 76(11): 747–56. doi: 10.1002/bdra.20294. [DOI] [PubMed] [Google Scholar]
- [2].Canfield MA, Mai CT, Wang Y, O’Halloran A, Marengo LK, Olney RS, et al. The association between race/ethnicity and major birth defects in the united states, 1999–2007. Am J Public Health. 2014; 104(9): e14–23. doi: 10.2105/AJPH.2014.302098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Amarante MA, Shrensel JA, Tomei KL, Carmel PW, Gandhi CD. Management of urological dysfunction in pediatric patients with spinal dysraphism: Review of the literature. Neurosurg Focus 2012; 33(4): E4. doi: 10.3171/2012.7.FOCUS12232. [DOI] [PubMed] [Google Scholar]
- [4].Tarcan T, Bauer S, Olmedo E, Khoshbin S, Kelly M, Darbey M. Long-term followup of newborns with myelodysplasia and normal urodynamic findings: Is followup necessary? J Urol. 2001; 165(2): 564–7. doi: 10.1097/00005392-200102000-00070. [DOI] [PubMed] [Google Scholar]
- [5].Dik P, Klijn AJ, van Gool JD, de Jong-de Vos van Steenwijk CC, de Jong TP. Early start to therapy preserves kidney function in spina bifida patients. Eur Urol. 2006; 49(5): 908–13. doi: 10.1016/j.eururo.2005.12.056. [DOI] [PubMed] [Google Scholar]
- [6].Kochakarn W, Ratana-Olarn K, Lertsithichai P, Roongreungsilp U. Follow-up of long-term treatment with clean intermittent catheterization for neurogenic bladder in children. Asian J Surg. 2004; 27(2): 134–6. doi: 10.1016/S1015-9584(09)60327-4. [DOI] [PubMed] [Google Scholar]
- [7].Williams EN, Broughton NS, Menelaus MB. Age-related walking in children with spina bifida. Dev Med Child Neurol. 1999; 41(7): 446–9. [PubMed] [Google Scholar]
- [8].Bartonek A, Saraste H. Factors influencing ambulation in myelomeningocele: A cross-sectional study. Dev Med Child Neurol. 2001; 43(4): 253–60. [DOI] [PubMed] [Google Scholar]
- [9].O’Mahony L, O’Mahony DS, Simon TD, Neff J, Klein EJ, Quan L. Medical complexity and pediatric emergency department and inpatient utilization. Pediatrics. 2013; 131(2): e559–65. doi: 10.1542/peds.2012-1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Boulet SL, Boyle CA, Schieve LA. Health care use and health and functional impact of developmental disabilities among US children, 1997–2005. Arch Pediatr Adolesc Med. 2009; 163(1): 19–26. doi: 10.1001/archpediatrics.2008.506. [DOI] [PubMed] [Google Scholar]
- [11].Boyle CA, Decoufle P, Yeargin-Allsopp M. Prevalence and health impact of developmental disabilities in US children. Pediatrics. 1994; 93(3): 399–403. [PubMed] [Google Scholar]
- [12].Newacheck PW, Kim SE. A national profile of health care utilization and expenditures for children with special health care needs. Arch Pediatr Adolesc Med. 2005; 159(1): 10–7. doi: 10.1001/archpedi.159.1.10. [DOI] [PubMed] [Google Scholar]
- [13].Newacheck PW, Inkelas M, Kim SE. Health services use and health care expenditures for children with disabilities. Pediatrics. 2004; 114(1): 79–85. [DOI] [PubMed] [Google Scholar]
- [14].Wang HH, Wiener JS, Ross SS, Routh JC. Emergent care patterns in patients with spina bifida: A case-control study. J Urol. 2015; 193(1): 268–73. doi: 10.1016/j.juro.2014.06.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Caterino JM, Scheatzle MD, D’Antonio JA. Descriptive analysis of 258 emergency department visits by spina bifida patients. J Emerg Med 2006; 31(1): 17–22. doi: 10.1016/j.jemermed.2005.09.005. [DOI] [PubMed] [Google Scholar]
- [16].Thibadeau JK, Ward EA, Soe MM, Liu T, Swanson M, Sawin KJ, et al. Testing the feasibility of a national spina bifida patient registry. Birth Defects Res A Clin Mol Teratol. 2013; 97(1): 36–41. doi: 10.1002/bdra.23094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Young NL, Steele C, Fehlings D, Jutai J, Olmsted N, Williams JI. Use of health care among adults with chronic and complex physical disabilities of childhood. Disabil Rehabil. 2005; 27(23): 1455–60. [DOI] [PubMed] [Google Scholar]
- [18].Dicianno BE, Wilson R. Hospitalizations of adults with spina bifida and congenital spinal cord anomalies. Arch Phys Med Rehabil. 2010; 91(4): 529–35. doi: 10.1016/j.apmr.2009.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Alpern ER, Clark AE, Alessandrini EA, Gorelick MH, Kittick M, Stanley RM, et al. Recurrent and high-frequency use of the emergency department by pediatric patients. Acad Emerg Med. 2014; 21(4): 365–73. doi: 10.1111/acem.12347. [DOI] [PubMed] [Google Scholar]
- [20].Alpern ER, Stanley RM, Gorelick MH, Donaldson A, Knight S, Teach SJ, et al. Epidemiology of a pediatric emergency medicine research network: The PECARN core data project. Pediatr Emerg Care. 2006; 22(10): 689–99. doi: 10.1097/01.pec.0000236830.39194.c0. [DOI] [PubMed] [Google Scholar]
- [21].Routh JC, Cheng EY, Austin JC, Baum MA, Gargollo PC, Grady RW, et al. Design and methodological considerations of the centers for disease control and prevention urologic and renal protocol for the newborn and young child with spina bifida. J Urol. 2016; 196(6): 1728–34. doi: 10.1016/j.juro.2016.07.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Kim S, Ward E, Dicianno BE, Clayton GH, Sawin KJ, Beier-waltes P, et al. Factors associated with pressure ulcers in individuals with spina bifida. Arch Phys Med Rehabil. 2015; 96(8): 1435–41. doi: e110.1016/j.apmr.2015.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]


