Supplemental Digital Content is available in the text.
Keywords: Hip fracture, Incidence, Recurrence, Survival, Education, Comorbidities, Trends
Background:
Hip fractures are common and severe conditions among older individuals, associated with high mortality, and the Nordic countries have the highest incidence rates globally. With this study, we aim to present a comprehensive picture of trends in hip fracture incidence and survival in the older Swedish population stratified by education, birth country, and comorbidity level.
Methods:
This study is based on a linkage of several population registers and included the entire population over the age of 60 living in Sweden. We calculated age-standardized incidence rates for first and recurrent hip fractures as well as age-standardized proportions of patients surviving 30 and 365 days through the time period 1998 to 2017. We calculated all outcomes for men and women in the total population and in each population stratum.
Results:
Altogether, we observed 289,603 first hip fractures during the study period. Age-standardized incidence rates of first and recurrent fractures declined among men and women in the total population and in each educational-, birth country-, and comorbidity group. Declines in incidence were more pronounced for recurrent than for first fractures. Approximately 20% of women and 30% of men died within 1 year of their first hip fracture. Overall, survival proportions remained constant throughout the study period but improved when taking into account comorbidity level.
Conclusions:
Hip fracture incidence has declined across the Swedish population, but mortality after hip fracture remained high, especially among men. Hip fracture patients constitute a vulnerable population group with increasing comorbidity burden and high mortality risk.
The Nordic countries have the highest incidence rates of hip fractures worldwide.1 In Sweden, one out of five women and one out of nine of men are expected to sustain a hip fracture during their life.2 Being most common among the oldest old, hip fractures are debilitating conditions, which often have severe consequences including immobilization, loss of muscle mass, physical impairment, care-dependency, and a high risk of complications such as infections.3,4 As a result, more than 20% of female patients, and more than 30% of male patients die within one year of sustaining a hip fracture.5,6 Despite declining incidence rates observed in many countries since the 1990s, population aging is projected to cause increasing numbers of hip fractures in the future.2,7–11
Although hip fracture incidence has declined in Sweden and in many other countries, mortality among hip fracture patients remains high.1,6–8,11–19 A growing body of research suggests that rising comorbidity levels among hip fracture patients may have contributed to the persistently high mortality.12,15,19,20 These studies further suggest that mortality after hip fracture declined when taking into account the rising comorbidity levels among patients.12,15,19,20 This illustrates that a changing population composition, in this case increasing shares of individuals with comorbidities, may influence trends observed in the total population and, as a result, conclusions drawn from epidemiologic research. It is likely that increasing comorbidity levels in the population have not only affected mortality but also impacted trends in hip fracture incidence and recurrence rates. Hip fractures have been postponed to higher ages2 at which patients may be frailer and more frequently affected by comorbidities. It is thus possible that survivors are at higher risk of sustaining a second fracture; however, few studies have examined trends in hip fracture recurrence or the impact of changing comorbidity levels on the incidence of first and recurrent fractures in the population.
Population aging has not only been accompanied by a trend toward higher prevalence of many chronic conditions and multimorbidity among the old21,22 but also by an educational expansion and increase in international migration. Previous research has shown that both incidence of and mortality after hip fracture vary between men and women2,7–12,23 as well as between socioeconomic24–35 and ethnic10,36–39 groups. Hip fractures are considerably more common among women than among men,2,7–10 but men are at higher risk of death after experiencing a hip fracture.2,10,12,23 Furthermore, while research on socioeconomic disparities in hip fracture incidence yielded inconsistent results,24–28,35 many studies found that low socioeconomic position is associated with higher mortality after hip fracture.4,29–34 Data from Sweden indicate that higher education may be associated with a lower fracture risk among women but not men24 and with lower mortality after hip fracture among both genders.33 Ethnic differences in fracture incidence are well-known with Caucasian men and women being at higher risk in both Europe and North America,10,36–39 but research on ethnic differences in mortality after hip fracture is not available for the Nordic countries.
Despite these established differences in hip fracture incidence and mortality between population strata, evidence on secular trends is rare. However, it is important to monitor disease incidence and mortality in population groups to improve the understanding of trends observed in the total population and to allow the identification of vulnerable individuals. Such knowledge will, moreover, support decision-makers and healthcare professionals to allocate resources in accordance with the needs of the population, for instance by prioritizing interventions for those with the greatest need. With this study, we present secular trends in hip fracture incidence and mortality in the Swedish population over the age of 60 between 1998 and 2017 and explore whether trends have developed in a similar pattern among individuals with different educational and comorbidity levels, as well as among individuals with migration background.
METHODS
Data and Variables
The entire population over the age of 60 living in Sweden at any point between 1998 and 2017 was identified in national registers. Several administrative registers were linked using the personal identity number assigned to all residents of Sweden; a description of all data sources is provided in eFigure 1; http://links.lww.com/EDE/B772. Hip fracture diagnoses were retrieved from the National Patient Register (NPR), which contains all hospital admissions within Sweden since 1987 including International Classification of Diseases (ICD)-diagnoses assigned by physicians. Previous studies demonstrated high levels of validity and completeness for hip fracture diagnoses in administrative inpatient registers including the Swedish NPR.40–43
We defined incident hip fractures through ICD-codes 820 (ICD-9) and S720-722 (ICD-10) occurring as primary causes for hospitalization in the NPR. These codes have been commonly used in previous studies on hip fracture incidence and mortality as well as in validation studies of hip fracture diagnoses in administrative data.40–42,44 Due to their different etiology and survival chances, we did not include pathologic hip fractures. First hip fractures were defined as a person’s first hospitalization due to hip fracture in the NPR. Since the NPR has nationwide coverage since 1987, the prevalence of prior hip fractures could be traced back for at least 11 years for each person. A hospitalization for hip fracture at least 14 days after a previous hospital admission for hip fracture was considered a recurrent event. Thus, for the estimation of recurrent (i.e., second) hip fracture incidence, individuals were at risk from 14 days after their first hip fracture. These definitions of first and recurrent fractures were chosen in accordance with a previous study comparing diagnoses in the Swedish NPR to clinically confirmed hip fracture records in the Swedish Hip Fracture Register (RIKSHÖFT).44
Educational level was defined as a person’s highest achieved level of education distinguishing between compulsory education (up to 8–9 years, depending on birth cohort) and more than basic education. We chose to examine educational level rather than other socioeconomic indicators owing to its stability over the life course, its association with health-related behaviors and other indicators of socioeconomic position, and high level of coverage in population registers among individuals born from 1911 onwards. Birth country was divided into three groups: Sweden, the other Nordic countries (Denmark, Finland, Iceland, Norway), and other countries. Charlson comorbidity index (CCI) scores45,46 were calculated based on diagnoses made during previous hospital admissions. In each year of the study period, all primary and secondary diagnoses within the past 10 years were taken into account to estimate CCI scores. Individuals who emigrated from Sweden were censored at the time of their emigration. Data linkage were conducted by Statistics Sweden, and the researchers received a pseudonymized dataset. All data were available up to 31 December 2017.
Calculation of Incidence Rates and Survival
Incidence rates of first and recurrent hip fractures were calculated as number of hip fractures divided by person–years at risk in each population group. To reduce random fluctuations in yearly rates owing to small numbers of fractures, we estimated all rates as an average of 4-year intervals, that is, for 1998–2001, 2002–2005, 2006–2009, 2010–2013, and 2014–2017. We calculated survival during the first 30 days and the first year after hip fracture as the proportion of hip fracture patients alive at 30 days or 1 year after their fracture, respectively. We age-standardized incidence rates and survival proportions using direct standardization. Since established standard populations have different age structures than the population of older hip fracture patients, we used our own data as a standard. We used the total Swedish population in the middle of the study period (2008) as the standard population for the incidence of first fractures. For the calculation of recurrent fracture rates and survival proportions, the population of patients with first hip fracture in 2008 was used as standard population. We estimated 95% confidence intervals using the normal approximation method. Educational level was not recorded for most men and women born before 1911 in the Swedish registers; hence, we restricted the analyses of educational groups to individuals up to age 90.
To examine how changes in health status of hip fracture patients over time influenced trends in survival after hip fracture in the general population, we estimated time trends in mortality risk after first hip fracture using Cox proportional hazard regression with age as the underlying time scale. In these analyses, we defined health status as the CCI score at the time of the fracture. The proportionality of hazards-assumption was tested through Schoenfeld residuals and log-log plots. All analyses were stratified by sex and conducted in Stata version 14.2 and R version 3.6.1.
Sensitivity Analyses
Data available in the NPR do not allow to distinguish between hospitalizations for an incident hip fracture and hospitalizations owing to complications and readmissions for a previous fracture. Therefore, researchers need to define recurrent fractures carefully. In this study, recurrent fractures are defined through hospitalizations with hip fracture as primary cause occurring at least 14 days after admission for a previous fracture. We have shown that this definition is reasonable in a recent validation study, although it may result in some overestimation of the incidence of recurrent fractures.44 To reduce the risk of misclassifying hospitalizations owing to complications of a previous fracture as incident recurrent fractures, we conducted sensitivity analyses increasing the time from which a person begins to be at risk for a recurrent fracture from 14 to 90 days. However, it should be noted that this strategy may instead lead to an underestimation of recurrent fracture incidence since many recurrent fractures occur within the first 3 months after the first. We conducted analyses using the Swedish Hip Fracture Register, which includes clinically confirmed fractures only, finding than 10% of second hip fractures occurred within 90 days after the first fracture and roughly 1% occurred within the first 14 days.
Ethical Approval and Consent to Participate
This study was approved by the regional ethics committee in Stockholm (permit numbers Dnr 2011/136-31/5 and Dnr 2015/1917-32). The board waived the need for patient consent.
RESULTS
During the study period, we observed 289,603 first hip fractures, 69% of which occurred among women. Despite a growing and aging population, the total number of annual first hip fractures decreased by 16% from 15,393 fractures in 1998 to 13,148 fractures in 2017. However, the number of fractures increased among men. Table 1 shows the characteristics of patients at the time of their first hip fracture. In 1998–2001, 6.0% of patients were born outside Sweden, but the proportion of foreign-born men and women increased during the study period to 9.5% in 2014–2017. The group of individuals born outside the Nordic countries was heterogeneous with a majority (69.4%) born in other European countries, 16.3% born in Asian, 5.0%, in South American, and 3.7% in African countries. We found trends toward patients being older, having higher education, and having a higher comorbidity level over time. While the median age at first hip fracture increased by 1.2 years among both sexes, the proportion of hip fracture patients with a CCI of two or more increased by 14 percentage points among women and 19 percentage points among men during the study period. In 1998–2001, approximately 7% of patients experienced a recurrent fracture within 1 year of their first fracture and this proportion was reduced to 4% in 2014–2017. The proportion of patients alive 30 days after their first fracture decreased among men and women, while the proportion alive after 365 days declined among women but remained stable among men. Approximately 20% of women and 30% of men died during the first year after experiencing their first hip fracture.
TABLE 1.
Characteristics of Patients With First Hip Fracture During the Study Period 1998–2017
| Women (N = 200,172) | |||||
|---|---|---|---|---|---|
| 1998–2001 | 2002–2005 | 2006–2009 | 2010–2013 | 2014–2017 | |
| Number of patients | 43,248 | 41,355 | 40,206 | 38,759 | 36,604 |
| Age, n (%) | |||||
| 60–69 | 2,980 (6.9) | 2,832 (6.9) | 3,144 (7.8) | 3,337 (8.6) | 3,003 (8.2) |
| 70–79 | 11,415 (26.4) | 9,923 (24.0) | 8,787 (21.9) | 8,253 (21.3) | 8,338 (22.8) |
| 80–89 | 21,644 (50.1) | 21,001 (50.8) | 20,238 (50.3) | 18,401 (47.5) | 16,434 (44.9) |
| 90+ | 7,209 (16.7) | 7,599 (18.4) | 8,037 (20.0) | 8,768 (22.6) | 8,829 (24.1) |
| Educational level, n (%) | |||||
| Basic | 23,533 (54.4) | 24,865 (60.1) | 24,188 (60.2) | 21,861 (56.4) | 18,255 (49.9) |
| Higher education | 9,446 (21.8) | 11,965 (28.9) | 14,270 (35.5) | 16,041 (41.4) | 17,819 (48.7) |
| Educational level missingd | 10,269 (23.7) | 4,525 (10.9) | 1,748 (4.4) | 857 (2.2) | 530 (1.5) |
| Birth country, n (%) | |||||
| Sweden | 40,549 (93.8) | 38,435 (92.9) | 37,047 (92.1) | 35,175 (90.8) | 33,007 (90.2) |
| Other Nordic countries | 1,505 (3.5) | 1,648 (4.0) | 1,814 (4.5) | 2,022 (5.2) | 1,937 (5.3) |
| Other birth country | 1,194 (2.8) | 1,272 (3.1) | 1,345 (3.4) | 1,562 (4.0) | 1,660 (4.5) |
| CCI at fracture, n (%) | |||||
| 0 | 20,157 (46.6) | 18,066 (43.7) | 15,957 (39.7) | 12,884 (33.2) | 11,626 (31.8) |
| 1 | 13,820 (32.0) | 13,291 (32.1) | 13,151 (32.7) | 12,886 (33.3) | 12,019 (32.8) |
| 2+ | 9,271 (21.4) | 9,998 (24.2) | 11,098 (27.6) | 12,989 (33.5) | 12,959 (35.4) |
| Surviving 30 daysa (%) | 95.5 | 94.7 | 94.1 | 93.6 | 93.9 |
| Surviving 365 daysb (%) | 79.5 | 78.9 | 78.2 | 77.5 | 78.1 |
| Recurrent fracture within 365 daysc (%) | 7.1 | 5.5 | 5.4 | 4.6 | 4.1 |
| Men (N = 89,431) | |||||
| 1998–2001 | 2002–2005 | 2006–2009 | 2010–2013 | 2014–2017 | |
| Number of patients | 17,155 | 17,438 | 18,130 | 18,569 | 18,139 |
| Age, n (%) | |||||
| 60–69 | 1,857 (10.8) | 1,959 (11.2) | 2,350 (13.0) | 2,493 (13.4) | 2,275 (12.5) |
| 70–79 | 5,491 (32.0) | 4,854 (27.8) | 4,588 (25.3) | 4,589 (24.7) | 4,904 (27.0) |
| 80–89 | 7,742 (45.1) | 8,340 (47.8) | 8,584 (47.4) | 8,476 (45.7) | 7,710 (42.5) |
| 90+ | 2,065 (12.0) | 2,285 (13.1) | 2,608 (14.4) | 3,011 (16.2) | 3,250 (17.9) |
| Educational level, n (%) | |||||
| Basic | 8,907 (51.9) | 9,667 (55.4) | 9,825 (54.2) | 9,279 (50.0) | 8,329 (45.9) |
| Higher education | 5,130 (29.9) | 6,452 (37.0) | 7,758 (42.8) | 8,991 (48.4) | 9,578 (52.8) |
| Educational level missingd | 3,118 (18.2) | 1,319 (7.6) | 547 (3.0) | 299 (1.6) | 232 (1.3) |
| Birth country, n (%) | |||||
| Sweden | 16,260 (94.8) | 16,368 (93.9) | 16,877 (93.1) | 17,118 (92.2) | 16,616 (91.6) |
| Other Nordic countries | 490 (2.9) | 548 (3.1) | 659 (3.6) | 727 (3.9) | 746 (4.1) |
| Other birth country | 405 (2.4) | 522 (3.0) | 594 (3.3) | 724 (3.9) | 777 (4.3) |
| CCI at fracture, n (%) | |||||
| 0 | 6,219 (36.3) | 5,763 (33.1) | 5,484 (30.3) | 4,369 (23.5) | 4,052 (22.3) |
| 1 | 5,678 (33.1) | 5,595 (32.1) | 5,474 (30.2) | 5,312 (28.6) | 5,048 (27.8) |
| 2+ | 5,258 (30.7) | 5,258 (30.7) | 7,172 (39.6) | 8,888 (47.9) | 9,039 (49.8) |
| Surviving 30 daysa (%) | 90.5 | 88.9 | 88.5 | 88.2 | 88.8 |
| Surviving 365 daysb (%) | 67.4 | 66.9 | 67.0 | 67.1 | 67.9 |
| Recurrent fracture within 365 daysc (%) | 6.4 | 5.0 | 4.6 | 4.1 | 3.7 |
aPatients with hip fracture in December 2017 excluded.
bPatients with hip fracture in 2017 excluded.
cAmong patients alive after 365 days.
dPrimarily due to missing registration of educational level for individuals born before 1911 in Swedish population registers.
CCI, Charlson Comorbidity Index score.
Incidence Rates of First and Recurrent Hip Fractures
Incidence rates of first hip fracture were higher among women than among men and rose with increasing age (Figure 1, eFigure 2; http://links.lww.com/EDE/B772). We observed the highest incidence rates of approximately 50 hip fractures per 1000 person–years among women aged 95 and older. Fracture risk was higher among individuals with low educational level than among individuals with higher education. At the end of the study period, the age-standardized incidence of first fractures was 4.3 and 6.2 fractures per 1,000 person–years among men and women with basic education compared with 3.7 and 5.6 fractures per 1,000 person–years among men and women with higher education. Swedish-born individuals were at considerably higher risk of sustaining a hip fracture than those born outside the Nordic countries. Compared with individuals born in the other Nordic countries, however, there were no differences in incidence rates. Aside from age, comorbidity level was the strongest predictor for fracture risk; age-standardized incidence rates were more than twice as high among men and women with a CCI score of two or more than among those with a CCI score of zero.
FIGURE 1.
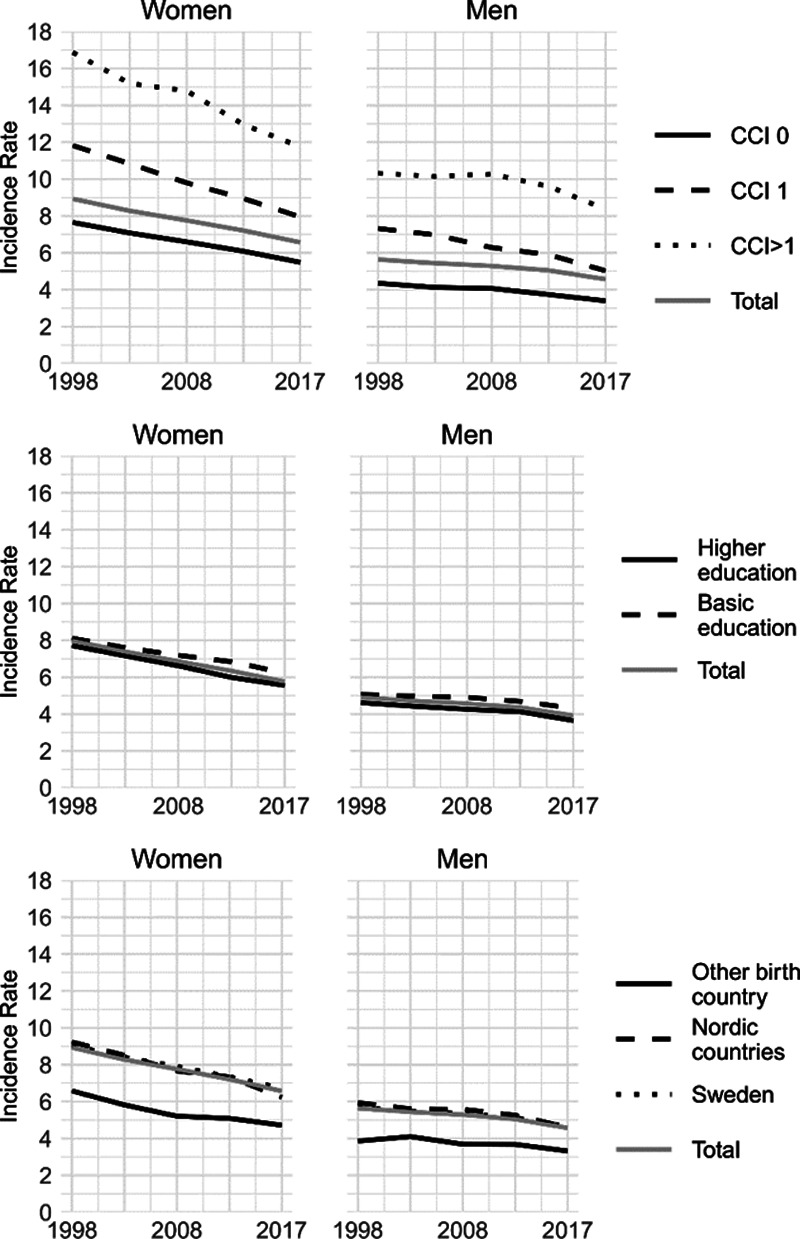
Age-standardized incidence rates of first hip fractures (rates per 1000 person–years) by comorbidity level, educational level, and birth country among men and women 1998–2017. Incidence by educational level includes individuals up to age 90 only. CCI, Charlson Comorbidity Index score.
Throughout the study period, incidence rates declined both among men and women in all age groups (eFigure 2; http://links.lww.com/EDE/B772). In the total population, the age-standardized incidence of first hip fractures declined by approximately 20% from 8.9 to 6.6 fractures per 1,000 person years among women and from 5.6 to 4.6 fractures per 1,000 person–years among men (Figure 1, eTable 1; http://links.lww.com/EDE/B772). Declines in age-standardized incidence rates were observed in all population strata. Relative declines were overall smaller among men than among women and ranged from 14% among men born outside of the Nordic countries to 33% among women born in the Nordic countries outside of Sweden.
The age-standardized incidence of recurrent fractures was higher than the incidence of first fractures. However, the incidence of recurrent fractures showed a stronger decline over time than the incidence of first fractures (Figure 2, eTable 1; http://links.lww.com/EDE/B772). In contrast to the incidence rates for first fractures, the incidence of recurrent fractures was similar for men and women as well as between population groups defined by educational level and birth country. Among men, the age-standardized incidence of recurrent hip fractures decreased from 66.0 fractures per 1,000 person–years in 1998–2001 to 34.3 fractures in 2014–2017. Among women, it decreased from 69.7 to 37.3 fractures per 1,000 person–years. Patients with higher comorbidity level at the time of their first hip fracture were at elevated risk of sustaining a recurrent fracture. In 2014–2017 men and women with a CCI score of two or more had an age-standardized incidence of 40.8 and 39.7 recurrent fractures per 1,000 person–years although the incidence was 33.8 and 31.4 recurrent fractures per 1,000 person–years among men and women with a CCI score of zero, respectively. Increasing the time from which a person is at risk for a recurrent fracture from 14 to 90 days yielded similar results (eFigure 3; http://links.lww.com/EDE/B772).
FIGURE 2.
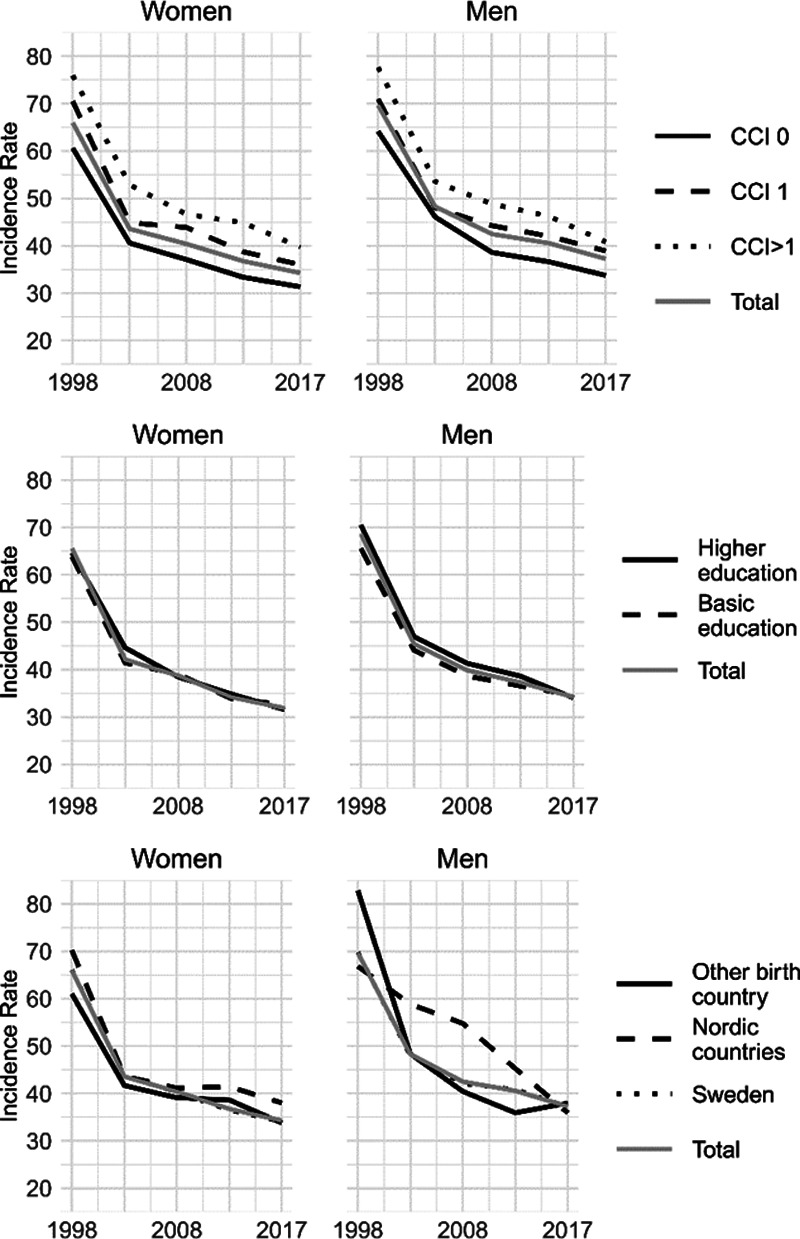
Age-standardized incidence rates of recurrent hip fractures (rates per 1,000 person–years) by comorbidity level, educational level, and birth country among men and women 1998–2017. Incidence by educational level includes individuals up to age 90 only. CCI, Charlson Comorbidity Index score.
Survival After Hip Fracture
Figures 3 and 4 show the age-standardized proportion of patients with first hip fracture that survived at least 30 and 365 days throughout the study period. Mortality was generally higher among men than among women. During the study period, age-standardized survival proportions remained overall unchanged in the general population, within educational groups, and within population groups defined by birth country. Nevertheless, 1-year survival improved substantially within groups defined by CCI score among both men and women (Figure 4, eTable 1; http://links.lww.com/EDE/B772). For example, the age-standardized proportion of patients with a CCI score of two or more surviving at least 365 days increased from 49% to 57% among men and 72% to 78% among women throughout the study period.
FIGURE 3.
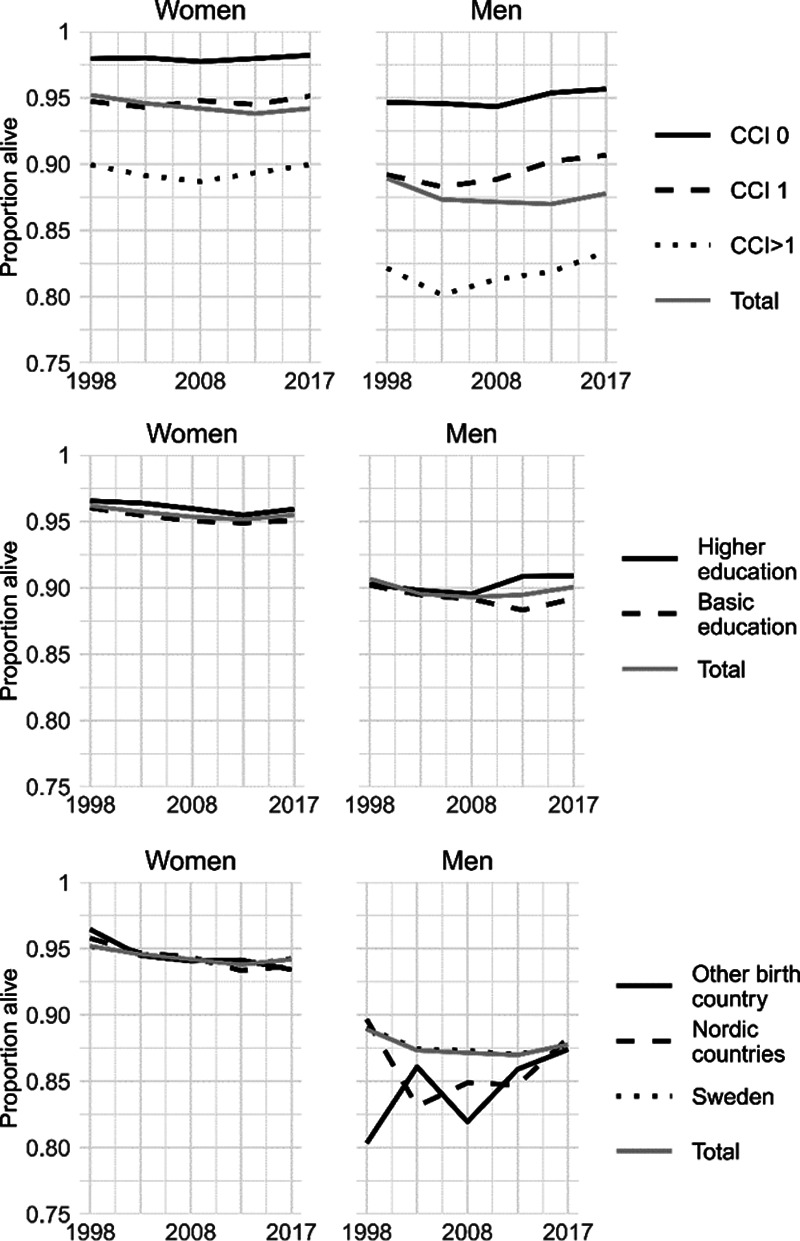
Age-standardized proportion of patients with first hip fracture surviving 30 days by comorbidity level, educational level, and birth country among men and women 1998–2017. Survival by educational level and birth country includes individuals up to age 90 only. CCI, Charlson Comorbidity Index score.
FIGURE 4.
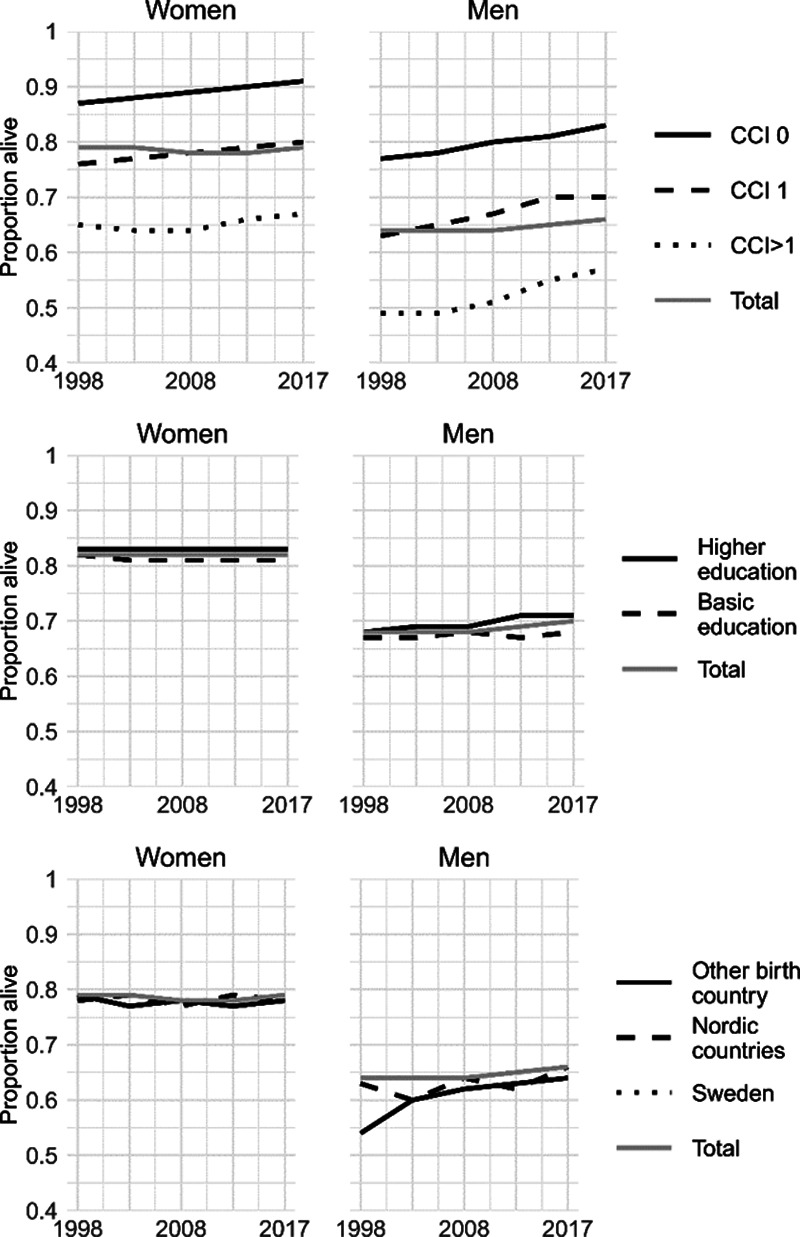
Age-standardized proportion of patients with first hip fracture surviving 365 days by comorbidity level, educational level, and birth country among men and women 1998–2017. Survival by educational level and birth country includes individuals up to age 90 only. CCI, Charlson Comorbidity Index score.
In accordance with these findings, our Cox regression models adjusted for age only indicated stable mortality rates throughout the study period among men and slightly increasing mortality among women (Table 2). However, mortality rates declined when additionally adjusting for comorbidity level. When we adjusted for CCI score, the hazards of dying within the first year of sustaining a hip fracture were 13% among women and 21% lower among men in 2013–2017 compared with 1998–2011. Although we detected slight deviations from proportional hazards, hazard functions did not cross and restrictions of follow-up to time periods under which the proportional hazards assumption was met did not change the results notably.
TABLE 2.
Hazard Ratios for Mortality During the First 365 Days After First Hip Fracture
| Women (N = 199,831) | Men (N = 89,145) | |||
|---|---|---|---|---|
| M1 HR (95% CI) |
M2 HR (95% CI) |
M1 HR (95% CI) |
M2 HR (95% CI) |
|
| Year | ||||
| 1998–2001 | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.00) |
| 2002–2005 | 1.01 (0.98, 1.04) | 0.98 (0.92, 1.03) | 1.01 (0.97, 1.04) | 0.98 (0.91, 1.05) |
| 2006–2009 | 1.03 (1.00, 1.06) | 0.93 (0.88, 0.98) | 0.99 (0.95, 1.02) | 0.91 (0.85, 0.97) |
| 2010–2013 | 1.05 (1.02, 1.08) | 0.90 (0.86, 0.95) | 0.97 (0.94, 1.01) | 0.84 (0.79, 0.90) |
| 2014–2017 | 1.06 (1.02, 1.09) | 0.87 (0.82, 0.92) | 0.98 (0.94, 1.02) | 0.83 (0.77, 0.88) |
M1 adjusted for age; M2 adjusted for age and CCI score.
CCI, Charlson Comorbidity Index score; CI, confidence interval; HR, hazard ratio.
DISCUSSION
During the past 20 years, incidence rates of hip fracture have declined across the Swedish population. Our study demonstrates that declines in hip fracture incidence are not limited to certain population strata. In fact, improvements were observed among men and women of all age groups regardless of educational level, comorbidity level, and birth country—both for first and recurrent hip fractures.
Despite declining incidence rates, however, survival chances among affected individuals did not improve in the total population. Especially among men, mortality remained substantial throughout the study period with almost one-third of men dying within 1 year. These findings are in line with several previous studies from the Nordic and other countries.2,5–9,11,12,16,19,20,47,48 We further show that the lack of mortality improvements is at least partly attributable to an increasing comorbidity burden among patients and that mortality declined when accounting for patients’ comorbidity level.
Several explanations for the substantial declines in hip fracture incidence have been put forward. Improved diagnosis and treatment of osteoporosis may have contributed to reductions in fracture risk, but a few studies suggest that osteoporosis treatment cannot completely explain the observed improvements in incidence.7,48 In addition, fall prevention may have improved, for instance through increased uptake of walking aids and home adjustments.13,17,49 The rising prevalence of overweight among the old is another suggested mechanism, since a higher body mass index is associated with lower hip fracture risk that is largely explained by increased bone mineral density.7,50 On the other hand, overweight increases the risk of many comorbidities which in turn may elevate fracture risk. Furthermore, several authors hypothesized that general trends toward a better functional status among older men and women from later-born cohorts contributed to their declining hip fracture risk.7,8,18 Such cohort effects could be attributable to lifestyle factors including nutrition and vitamin D supplementation, smoking, exercise, or working conditions throughout the life course.7,8,18 Nevertheless, this hypothesis is challenged by the increasing comorbidity levels among hip fracture patients. This rising comorbidity burden is likely driven by population aging and a longer survival with chronic conditions such as cardiovascular diseases and diabetes. However, it may also reflect improved diagnostic procedures or changes in comorbidity documentation in the registers rather than a worsening health status per se.
The longer survival after a first hip fracture could potentially increase the risk of recurrent fractures. Despite this, trends in the incidence of recurrent hip fractures have rarely been studied. In this study, we found steep declines in recurrent fracture rates in all population strata. In contrast, Omsland and colleagues examined the incidence of second hip fractures between 1999 and 2008 in Norway and found a stable incidence of second fractures.18 A possible explanation for the difference to our findings might lie in the fact that Omsland et al. considered recurrent fractures within one year after index fracture only.18 It is possible that improvements in recurrent fracture rates were less pronounced within the first year after a hip fracture. The mechanisms behind the declining incidence of recurrent fractures are likely similar to those affecting the incidence of first fractures. In addition, more aggressive treatments of osteoporosis, often not detected until an osteoporotic fracture has occurred,51 may have enhanced the prevention of subsequent fractures.14
The risk of overestimating the incidence of recurrent fractures when using data from administrative inpatient registers should be considered. Repeated hospital admissions for hip fracture may partly consist of readmissions due to a previous fracture rather than incident recurrent fractures. We investigated the potential overestimation in the Swedish inpatient register in a previous study44 and found that the number recurrent fractures may be overestimated by approximately 10% when applying the definition used in this study. We see little reason to believe that this proportion varied substantially over time. Thus, this may have affected the level of recurrence rates but it unlikely to have caused the pronounced declines observed in this study. Furthermore, our sensitivity analyses extending the time between two fractures from 14 to 90 days produced trends similar to our main findings.
In line with our findings, various studies have reported stagnating or only slowly declining mortality rates among hip fracture patients12,15,16,19 although life expectancy rose markedly in the general population.8,15,17,18 Even though the lack of mortality improvements is at least partly explained by rising comorbidity levels among patients, it is still possible that changes in treatment and care, such as a trend towards shorter hospitalizations, have negatively affected survival chances. Indeed, one Swedish study showed that hospitalizations of hip fracture patients have become shorter during the past decades and that shorter stays in hospital were associated with higher mortality after discharge.52
Although some studies indicated elevated postfracture mortality among individuals with low socioeconomic status,29–32,34 educational disparities in survival were nonsignificant in this study. Moreover, educational disparities in hip fracture incidence were small. It is possible that this finding is limited to the Nordic countries where hip fracture incidence is high and social inequality – at least comparatively—low. Nevertheless, two register-based studies from other Nordic countries reported approximately 20% reduced 30-day and 1-year mortality risks after hip fracture among individuals with completed university education compared with those with basic education.29,32 In this study, we merely distinguished between two educational categories which are only a crude proxy for socioeconomic position attained later in life, especially among the old. It is thus possible that larger socioeconomic disparities in hip fracture risk come to light when considering a more fine-grained categorization of education or other indicators of socioeconomic position, such as income or former occupation.
Hip fracture incidence in the Nordic countries exceeds those in most other countries globally.1 This pattern is also evident within the Swedish population; foreign-born men and women had a lower risk of sustaining a hip fracture than those born within the Nordic countries. A similar result has been found in a previous Swedish study,38 but mechanisms behind this finding remain to be studied further. Individuals born outside the Nordic countries constitute a diverse population group and birth country may be associated with fracture risk through different pathways including genetic predisposition, health-related behaviors, exposure to environmental factors, or selection processes such as the “healthy-migrant effect.”1,38
One limitation of our work is that we merely used the CCI score to measure comorbidity and did not examine the impact of specific comorbidities or other risk- and lifestyle factors on observed trends. Future epidemiologic research should investigate how specific comorbid conditions or factors such as obesity, smoking, and diet have affected trends in hip fracture incidence, recurrence, and survival. This will further facilitate prevention efforts aimed at reducing fracture risk and mortality. Examining the role of other established risk factors such as bone mineral density, length of hospital stay, treatment, or rehabilitation may further improve the understanding of trends in hip fracture epidemiology.
Mortality during the first year after hip fracture is at least 50% higher among men than women.2,10,12,23 In our study men carried a higher comorbidity burden than women despite being younger when affected by hip fracture, which is in line with another study that associated male sex with a higher comorbidity level and a higher risk of severe adverse outcomes such as pneumonia or cardiac complications.23 In accordance with previous findings,6–9,11,12 declines in the incidence of first hip fracture were also less pronounced among men than women. Although studies suggest that osteoporosis is undertreated among both sexes, men may face an even higher risk to receive insufficient treatment than women.51,53 Older men are therefore an important target for hip fracture prevention measures and their higher mortality after hip fracture deserves scientific and medical attention.
CONCLUSION
The incidence of both first and recurrent hip fractures has declined throughout the Swedish population during the past 20 years. Improvements have occurred among men and women in all educational groups, comorbidity levels, and among Swedish-born and those with migration background. As a result of increasing numbers of comorbidities, however, survival chances among hip fracture patients remained essentially unchanged. Especially male hip fracture patients constitute a vulnerable population group characterized by increasing comorbidity levels and high mortality.
Supplementary Material
Footnotes
The results reported herein correspond to specific aims of grant M18-005 to investigator Karin Modig from the Åke Wiberg Foundation. This work was also supported by grant 2019135 from the Kamprad Family Foundation for Entrepreneurship, Research, and Charity.
Availability of Data and Code: Data were provided by the Swedish National Board of Health and Welfare and Statistics Sweden. Restrictions apply to the availability of these data, which are thus not publicly accessible. Data are, however, available from the authors upon reasonable request and with permission of the regional ethics board in Stockholm. Statistical code is available upon request from the corresponding author at anna.meyer@ki.se.
The authors report no conflicts of interest.
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.epidem.com).
REFERENCES
- 1.Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C; IOF Working Group on Epidemiology and Quality of Life. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int. 2012;23:2239–2256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karampampa K, Ahlbom A, Michaëlsson K, Andersson T, Drefahl S, Modig K. Declining incidence trends for hip fractures have not been accompanied by improvements in lifetime risk or post-fracture survival—a nationwide study of the Swedish population 60 years and older. Bone. 2015;78:55–61. [DOI] [PubMed] [Google Scholar]
- 3.Dyer SM, Crotty M, Fairhall N, et al. ; Fragility Fracture Network (FFN) Rehabilitation Research Special Interest Group. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr. 2016;16:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bentler SE, Liu L, Obrizan M, et al. The aftermath of hip fracture: discharge placement, functional status change, and mortality. Am J Epidemiol. 2009;170:1290–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2009;20:1633–1650. [DOI] [PubMed] [Google Scholar]
- 6.Pedersen AB, Ehrenstein V, Szépligeti SK, et al. Thirty-five-year trends in first-time hospitalization for hip fracture, 1-year mortality, and the prognostic impact of comorbidity: a Danish Nationwide Cohort Study, 1980-2014. Epidemiology. 2017;28:898–905. [DOI] [PubMed] [Google Scholar]
- 7.Kannus P, Niemi S, Parkkari J, Sievänen H. Continuously declining incidence of hip fracture in Finland: analysis of nationwide database in 1970-2016. Arch Gerontol Geriatr. 2018;77:64–67. [DOI] [PubMed] [Google Scholar]
- 8.Rosengren BE, Björk J, Cooper C, Abrahamsen B. Recent hip fracture trends in Sweden and Denmark with age-period-cohort effects. Osteoporos Int. 2017;28:139–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lucas R, Martins A, Severo M, et al. Quantitative modelling of hip fracture trends in 14 European countries: testing variations of a shared reversal over time. Sci Rep. 2017;7:3754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sullivan KJ, Husak LE, Altebarmakian M, Brox WT. Demographic factors in hip fracture incidence and mortality rates in California, 2000-2011. J Orthop Surg Res. 2016;11:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Søgaard AJ, Holvik K, Meyer HE, et al. Continued decline in hip fracture incidence in Norway: a NOREPOS study. Osteoporos Int. 2016;27:2217–2222. [DOI] [PubMed] [Google Scholar]
- 12.Jantzen C, Madsen CM, Lauritzen JB, Jørgensen HL. Temporal trends in hip fracture incidence, mortality, and morbidity in Denmark from 1999 to 2012. Acta Orthop. 2018;89:170–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Löfgren S, Ljunggren G, Brommels M. No ticking time bomb: hospital utilisation of 28,528 hip fracture patients in Stockholm during 1998-2007. Scand J Public Health. 2010;38:418–425. [DOI] [PubMed] [Google Scholar]
- 14.Melton LJ, 3rd, Kearns AE, Atkinson EJ, et al. Secular trends in hip fracture incidence and recurrence. Osteoporos Int. 2009;20:687–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meyer AC, Drefahl S, Ahlbom A, Lambe M, Modig K. Trends in life expectancy: did the gap between the healthy and the ill widen or close? BMC Med. 2020;18:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mundi S, Pindiprolu B, Simunovic N, Bhandari M. Similar mortality rates in hip fracture patients over the past 31 years. Acta Orthop. 2014;85:54–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nilson F, Moniruzzaman S, Gustavsson J, Andersson R. Trends in hip fracture incidence rates among the elderly in Sweden 1987–2009. J Public Health (Oxf). 2012;35:125–131. [DOI] [PubMed] [Google Scholar]
- 18.Omsland TK, Holvik K, Meyer HE, et al. Hip fractures in Norway 1999-2008: time trends in total incidence and second hip fracture rates: a NOREPOS study. Eur J Epidemiol. 2012;27:807–814. [DOI] [PubMed] [Google Scholar]
- 19.Trevisan C, Gallinari G, Klumpp R, Menon A, Compagnoni R. Year to year comparison of 2000–2015 in hip fracture management: same survival rate despite older and more fragile patients. Aging Clin Exp Res. 2019;31:1097–1103. [DOI] [PubMed] [Google Scholar]
- 20.Gjertsen JE, Dybvik E, Furnes O, et al. Improved outcome after hip fracture surgery in Norway. Acta Orthop. 2017;88:505–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meinow B, Kåreholt I, Thorslund M, Parker MG. Complex health problems among the oldest old in Sweden: increased prevalence rates between 1992 and 2002 and stable rates thereafter. Eur J Ageing. 2015;12:285–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosén M, Haglund B. From healthy survivors to sick survivors–implications for the twenty-first century. Scand J Public Health. 2005;33:151–155. [DOI] [PubMed] [Google Scholar]
- 23.Ekström W, Samuelsson B, Ponzer S, Cederholm T, Thorngren KG, Hedström M. Sex effects on short-term complications after hip fracture: a prospective cohort study. Clin Interv Aging. 2015;10:1259–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Benetou V, Orfanos P, Feskanich D, et al. Education, marital status, and risk of hip fractures in older men and women: the CHANCES project. Osteoporos Int. 2015;26:1733–1746. [DOI] [PubMed] [Google Scholar]
- 25.Hansen L, Judge A, Javaid MK, et al. Social inequality and fractures—secular trends in the Danish population: a case-control study. Osteoporos Int. 2018;29:2243–2250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bacon WE, Hadden WC. Occurrence of hip fractures and socioeconomic position. J Aging Health. 2000;12:193–203. [DOI] [PubMed] [Google Scholar]
- 27.Reyes C, García-Gil M, Elorza JM, et al. Socioeconomic status and its association with the risk of developing hip fractures: a region-wide ecological study. Bone. 2015;73:127–131. [DOI] [PubMed] [Google Scholar]
- 28.Icks A, Haastert B, Wildner M, et al. Hip fractures and area level socioeconomic conditions: a population-based study. BMC Public Health. 2009;9:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kristensen PK, Thillemann TM, Pedersen AB, Søballe K, Johnsen SP. Socioeconomic inequality in clinical outcome among hip fracture patients: a nationwide cohort study. Osteoporos Int. 2017;28:1233–1243. [DOI] [PubMed] [Google Scholar]
- 30.Barone AP, Fusco D, Colais P, et al. Effects of socioeconomic position on 30-day mortality and wait for surgery after hip fracture. Int J Qual Health Care. 2009;21:379–386. [DOI] [PubMed] [Google Scholar]
- 31.Thorne K, Johansen A, Akbari A, Williams JG, Roberts SE. The impact of social deprivation on mortality following hip fracture in England and Wales: a record linkage study. Osteoporos Int. 2016;27:2727–2737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Omsland TK, Eisman JA, Næss Ø, et al. Educational inequalities in post-hip fracture mortality: a NOREPOS Studys. J Bone Miner Res. 2015;30:2221–2228. [DOI] [PubMed] [Google Scholar]
- 33.Hailer NP, Garland A, Rogmark C, Garellick G, Kärrholm J. Early mortality and morbidity after total hip arthroplasty in patients with femoral neck fracture. Acta Orthop. 2016;87:560–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Valentin G, Pedersen SE, Christensen R, et al. Socio-economic inequalities in fragility fracture outcomes: a systematic review and meta-analysis of prognostic observational studies. Osteoporos Int. 2020;31:31–42. [DOI] [PubMed] [Google Scholar]
- 35.Petit M, Bryère J, Maravic M, Pallaro F, Marcelli C. Hip fracture incidence and social deprivation: results from a French ecological study. Osteoporos Int. 2017;28:2045–2051. [DOI] [PubMed] [Google Scholar]
- 36.Curtis EM, van der Velde R, Moon RJ, et al. Epidemiology of fractures in the United Kingdom 1988-2012: variation with age, sex, geography, ethnicity and socioeconomic status. Bone. 2016;87:19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wright NC, Saag KG, Curtis JR, et al. Recent trends in hip fracture rates by race/ethnicity among older US adults. J Bone Miner Res. 2012;27:2325–2332. [DOI] [PubMed] [Google Scholar]
- 38.Albin B, Hjelm K, Elmståhl S. Lower prevalence of hip fractures in foreign-born individuals than in Swedish-born individuals during the period 1987-1999. BMC Musculoskelet Disord. 2010;11:203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sterling RS. Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clin Orthop Relat Res. 2011;469:1913–1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hudson M, Avina-Zubieta A, Lacaille D, Bernatsky S, Lix L, Jean S. The validity of administrative data to identify hip fractures is high–a systematic review. J Clin Epidemiol. 2013;66:278–285. [DOI] [PubMed] [Google Scholar]
- 41.Huttunen TT, Kannus P, Pihlajamäki H, Mattila VM. Pertrochanteric fracture of the femur in the Finnish National Hospital Discharge Register: validity of procedural coding, external cause for injury and diagnosis. BMC Musculoskelet Disord. 2014;15:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lofthus CM, Cappelen I, Osnes EK, et al. Local and national electronic databases in Norway demonstrate a varying degree of validity. J Clin Epidemiol. 2005;58:280–285. [DOI] [PubMed] [Google Scholar]
- 43.Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Meyer AC, Hedström M, Modig K. The Swedish Hip Fracture Register and National Patient Register were valuable for research on hip fractures: comparison of two registers. J Clin Epidemiol. 2020;125:91–99. [DOI] [PubMed] [Google Scholar]
- 45.Brusselaers N, Lagergren J. The charlson comorbidity index in registry-based research. Methods Inf Med. 2017;56:401–406. [DOI] [PubMed] [Google Scholar]
- 46.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–1251. [DOI] [PubMed] [Google Scholar]
- 47.Gundel O, Thygesen LC, Gögenur I, Ekeloef S. Postoperative mortality after a hip fracture over a 15-year period in Denmark: a national register study. Acta Orthop. 2020;91:58–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Abrahamsen B, Vestergaard P. Declining incidence of hip fractures and the extent of use of anti-osteoporotic therapy in Denmark 1997–2006. Osteoporos Int. 2010;21:373–380. [DOI] [PubMed] [Google Scholar]
- 49.Nilson F, Moniruzzaman S, Andersson R. Fall-related fracture trends among elderly in Sweden–exoring transitions among hospitalized cases. J Safety Res. 2013;45:141–145. [DOI] [PubMed] [Google Scholar]
- 50.De Laet C, Kanis JA, Odén A, et al. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int. 2005;16:1330–1338. [DOI] [PubMed] [Google Scholar]
- 51.Lorentzon M, Nilsson AG, Johansson H, Kanis JA, Mellström D, Sundh D. Extensive undertreatment of osteoporosis in older Swedish women. Osteoporos Int. 2019;30:1297–1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nordström P, Gustafson Y, Michaëlsson K, Nordström A. Length of hospital stay after hip fracture and short term risk of death after discharge: a total cohort study in Sweden. BMJ. 2015;350:h696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cadarette SM, Katz JN, Brookhart MA, et al. Trends in drug prescribing for osteoporosis after hip fracture, 1995-2004. J Rheumatol. 2008;35:319–326. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


