Abstract
Objectives
To examine the impact of workplace injury on opioid dependence, abuse and overdose (opioid-related morbidity) and if severity of injury increases the hazard of these health effects.
Methods
We used MarketScan databases to follow injured and propensity score matched non-injured workers, both without prior opioid-related diagnoses. Using a Cox proportional hazard model, we examined the impact of workplace injury on opioid-related morbidity.
Results
The hazard of opioid-related morbidity for injured workers was 1.79 times than that of matched non-injured workers (95% CI 1.89 to 3.60). For medical-only and lost-time injured workers, it was respectively 1.54 (95% CI 1.02 to 2.32) and 2.91 (95% CI 1.75 to 4.84) times that of non-injured workers.
Conclusions
Reducing workplace injury or severity of workplace injury, as well as efforts to ensure appropriate opioid prescribing for injured workers, may help to reduce the societal costs of opioid use.
INTRODUCTION
Opioid overdoses have been rising rapidly since 2000 and are major public health concerns. Age-adjusted mortality rates from opioid overdose in 2015 were about 2.5 times higher than rates in 2000,1 and they increased by 13% between 2015 and 2016.2 In 2017, among more than 70 200 drug overdose deaths, nearly 68% involved an opioid.3
Studies have shown that workplace injuries are associated with acute and chronic pain,4 and injured workers may receive prescription opioids. In one prospective study, 42% of workers with back injuries were prescribed opioids within a year after injury; in addition, approximately 16% of those prescribed opioids continued taking them for four quarters, with doses increasing substantially over time.5 In another study, 28.6% of injured workers filled an opioid prescription more than 90 days after injury.6
In recent years, there has been a decline in overall opioid prescriptions, and this may be reflected in prescribing for work-related injuries. Still, levels remain high, and there is a wide degree of state-level variability.7–9 In 2016, 44% of all workers’ compensation claims with prescriptions had at least one prescription for opioids based on data from 40 states. While still high, this number has declined from 55% since 2012.10 Despite their widespread use, evidence is insufficient to determine the effectiveness of long-term opioid therapy for improving chronic pain, while suggesting risks for serious harms.11
Evidence about the relationship between opioid use and work-r elated injuries is sparse. A recent study in Washington State concluded that opioid use in the 90 days before injury was associated with higher probability of losing more than 3 days from work.12 A related study used local prescribing patterns as an instrument to estimate the causal impact of longer term opioid prescribing on disability duration. The authors concluded that longer term opioid prescribing tripled the duration of temporary disability.13
Recent research has shown a relationship between workplace injuries and opioid-involved overdose mortality. A Massachusetts study found that opioid mortality rates were highest in construction and extraction and farming, fishing and forestry occupations, all of which have high injury rates.14 A study conducted in West Virginia showed that morality due to drug overdoses involving opioids was elevated among workers’ with lost-time claims compared with those not receiving lost-time benefits.15 Also, a study of New Mexico workers’ compensation cases determined that drug-related mortality was elevated among people with work-related injuries involving more than 7 days of lost work compared with injuries resulting in 0–7 days of lost work.16 However, no studies to date have explicitly addressed the extent to which injuries have led to opioid dependence, abuse, illicit use and overdose, as distinguished from opioid use leading to greater workplace injury and thereby excess mortality risks. Because this study examines postinjury opioid morbidity in a population with no known preinjury opioid morbidity, it directly addresses the causal link from injury to opioid dependence, abuse, illicit use and overdose.
The major objective of this study was to examine the impact of workplace injury on opioid-related morbidity following a cohort of injured and non-injured workers for 36 months after the index date of injury. The study also examined if severity of injury would increase the hazard of these health effects.
STUDY DATA AND METHODS
In this study, we used the deidentified, person-level data obtained from the MarketScan Commercial Claims and Encounters (CCAE) (MarketScan) databases. The MarketScan databases are constructed and maintained by Truven Health (formerly known as Thomson Reuters) from over 250 medium and large employers and health plans throughout the USA.17 The data are fully compliant with the Health Insurance Portability and Accountability Act, and no Institutional Review Board approval was necessary because individual patients were not identifiable with the data.18 In this study, we used the CCAE and the Health and Productivity Management (HPM) databases. The CCAE database has several subsections including enrolment in group health insurance and outpatient, inpatient and outpatient prescription drug claims. The HPM database includes information on workers’ compensation (eg, date injured, causes of injury, body part injured and medical and indemnity payments) and eligibility (eligibility to be included in this data set) files. In this study, we used the 2013–2017 enrolment, outpatient and inpatient prescription drug claims, workers’ compensation and eligibility files.
We considered workers who were included in the workers’ compensation file and enrolled in group health insurance for the period of 2013–2017. We excluded workers who were injured and filed for workers’ compensation in 2013. This helped us reduce the effects of earlier injuries on opioid use. In 2014, 29 370 injured workers filed one or more workers’ compensation claims. We considered 28 861 workers (98.3%) who were injured in 2014 and did not have missing information on industry, health plan type and region. For all estimates, we used the MarketScan national weights that are designed to reflect the national distribution of people with employer-sponsored private health insurance, using data from the Medical Expenditure Panel Survey.
In a non-randomised retrospective study like this, there could be significant sociodemographic differences between the control and treated groups at baseline. To minimise the impact of possible resulting selection bias, we used propensity score matching. Propensity score matching helps balance the distribution of all baseline observed sociodemographic characteristics between injured and non-injured workers, and consequently reduce the impact of selection bias.19 In this study, we used a one-to-one nearest-neighbour propensity score matching method without replacement. Despite the large sample of non-injured or control workers in our sample (n = 9 78 389), we used a one-to-one matching method because it gives a better estimate of the treatment (injury) effect than many-to-one or other forms of matching.20 We also used nearest-neighbour propensity score matching without replacement for its simplicity and best performance.21 The HPM and CCAE data sets have a limited number of sociodemographic variables. We used the following variables available in the data to match injured and non-injured workers: age group (four categories), sex, industry (four broad categories), health insurance plan type (six types) and region (four categories). The health plan categories we used included comprehensive, health maintenance organisation (HMO), point-of-service (POS), preferred provider organisation (PPO), consumer-driven health plan (CDHP) and other. For details on the characteristics of the health plan types, see Online supplementary appendix 1. We tested the balance of the variables before and after the matching process using a variance ratio22 and standardised differences tests.23 A variance ratio close to one is considered balanced and a variance ratio greater than 2.0 and less than 0.5 is considered unbalanced. A standardised difference greater than 0.10 is also considered unbalanced.
The exposure variable was workplace injury in 2014. We classified workers into two cohorts as not injured between 2013 and 2017 and injured only in 2014 (model 1). To further explore if severity of injury was associated with increasing hazard of opioid-related morbidity, we divided the second cohort into two: medical only (workers received workers’ compensation medical benefits only) and lost-time (workers received workers’ compensation medical and wage replacement benefits) injured workers (model 2). Lost-time injured workers missed a minimum of four to eight working days (depending on the state) due to the injury. In both cases, the control group consisted of workers not injured during 2013–2017. In addition to injury, we included the following covariates: sex, age, health insurance plan type, industry and region.
Our dependent variable was diagnosed opioid abuse, dependence, adverse effects or poisoning (hereafter opioid-related morbidity) after the index date of injury. Because dates of injury are not available for non-injured workers, each non-injured worker was assigned the date of injury of his or her matched injured worker. This means that every worker in our sample would have an index date of injury: a true date of injury for injured workers and a pseudodate of injury for non-injured workers. In line with the literature in this area, we used the International Classification of Diseases (ICD) codes to identify opioid-related morbidity.24 The ICD-9 and ICD-10 codes we used to identify these conditions are presented in Online supplementary appendix 2. We used ICD-9 and ICD-10 codes because most diagnoses in year 2014, 2015 and part of 2016 used ICD-9 codes. We considered both outpatient and inpatient cases. The follow-up period was from the index date of injury to the first report of an opioid-related morbidity or to the end of the follow-up period, whichever came first. The end of the follow-up period varies from 1 January 2017 to 31 December 2017 depending on the index date of injury. Workers were right censored if not diagnosed up to the end of the follow-up period. Within the 36-month-long follow-up period, the study outcome was assessed in 3-month intervals. Workers who were treated for diagnosed opioid-related conditions within a year before the index date of injury were excluded from the analysis (131 injured and 66 non-injured) because past opioid-related morbidity is a risk factor for both injury and future opioid-related morbidity.25
The Nelson-Aalen method, a non-parametric method for estimating the Kaplan-Meier cumulative hazard, was used for estimating the cumulative curves for the injured and non-injured workers, and we used a log-rank test to test whether the survival curves were identical.26 For the multivariable analysis, we used a Cox proportional hazard (PH) model to adjust for the effects of baseline variables. We tested all variables for the PH assumption of the Cox PH model using the Schoenfeld and scaled Schoenfeld residuals tests.
RESULTS
Characteristics at baseline
We balanced the baseline covariates between injured and non-injured workers using a one-to-one nearest-neighbour propensity score matching method without replacement. The method matched 28 861 injured workers to 28 861 non-injured workers. Online supplementary appendix 3 presents the variance ratio of the covariates before and after matching. Before matching, there were significant imbalances between injured and non-injured workers in health insurance type and region. The matching process created similar distributions of all covariates between the two groups of workers at the baseline. We found similar results when we used standardised differences of the covariates (not presented).
Table 1 provides descriptive statistics for the study variables. Of worker injuries, 21% were lost-time injuries. The share of male workers was 53.3%, which is similar to the 53.1% reported by the Bureau of Labor Statistics for the whole working population.27 The share of workers in the age group 35–44 years was the highest (29.4%), followed by the age group 45–54 years (28.1%). More than half of the workers had a PPO health insurance plan, followed by a CDHP plan (17.4%). The share of workers in the durable goods manufacturing sector was the highest (37.4%), followed by services (27.2%). Most of the workers were from the south (35.7%), followed by the west (22.9%) and the north (22.4%).
Table 1.
Descriptive statistics of variables used from MarketScan data: 2014
| Total | Non-injured | Injured | |
|---|---|---|---|
| Number of workers | 57 525 | 28 795* | 28 730† |
| Mean follow-up months | 35.95 | 35.95 | 35.90 |
| Number of workers treated for opioid-related morbidity during the follow-up period | 253 | 93 | 160 |
| Male (%) | 53.3 | 53.34 | 52.94 |
| Age categories in years (column sum %) | |||
| 18–29 | 23.6 | 23.57 | 23.76 |
| 30–44 | 29.35 | 29.37 | 29.13 |
| 45–54 | 28.11 | 28.11 | 28.01 |
| 55–65 | 18.94 | 18.94 | 19.11 |
| Health insurance type (column sum %) | |||
| Preferred provider organisation plan | 54.68 | 54.70 | 54.21 |
| Consumer directed health plans | 17.44 | 17.42 | 18.01 |
| Comprehensive | 3.67 | 3.66 | 3.65 |
| High-deductible health and exclusive provider organisation plan | 2.65 | 2.65 | 2.77 |
| Health maintenance organisation | 11.55 | 11.56 | 11.34 |
| Point-of-service plan | 10.01 | 10.01 | 9.99 |
| Industry (%) | |||
| Manufacturing – durable goods | 37.36 | 37.36 | 37.27 |
| Manufacturing – non-durable goods | 15.81 | 15.42 | 15.42 |
| Transportation, communications and utilities | 19.11 | 19.1 | 19.46 |
| Services | 27.18 | 27.17 | 27.29 |
| Other† | 0.55 | 0.55 | 0.56 |
| Region | |||
| Northeast | 22.35 | 22.35 | 22.26 |
| Northcentral | 19.16 | 19.18 | 18.63 |
| South | 35.54 | 35.53 | 36.49 |
| West | 22.95 | 22.94 | 22.62 |
From 28 861 matched non-injured workers in the sample, 66 had diagnosed opioid-related morbidity diagnosed within a year before the index date of injury were excluded.
From 28 861 injured workers in the sample, 131 had opioid-related morbidity diagnosed within a year before the date of injury were excluded.
Univariate analysis
Mean follow-up was 35.95 months (min 3 months, max 36 months, SD 1.38) and median follow-up was 36 months. There were no statistically significant differences in the follow-up period between injured and non-injured workers. The mean age at the index date of injury was 45 (min 19, max 65). Of 57 525 workers who we followed for up to 36 months, 253 workers were diagnosed with opioid-related morbidity during the follow-up period, 1 January 2014 to 31 December 2017. The overall weighted incidence rate of opioid-related morbidity during the study period was 323 workers per 100 000 workers. We observed a significant difference between injured and non-injured workers. The incidence rate for non-injured workers during the study period was 316 workers per 100 000 workers compared with 534 workers per 100 000 injured workers, and the difference was statistically significant (Pearson χ2=17.9, Pr <0.001). The incidence rate was much higher for lost-time injured workers: 748 workers per 100 000 lost-time injured workers.
Figure 1 shows the estimated Nelson-Aalen cumulative hazard of opioid-related morbidity for injured and non-injured workers after the index date of injury. The cumulative hazard of these conditions was higher for injured workers compared with their matched non-injured workers, and the difference was statistically significant at the less than one percent level (log-rank test, χ2 =3518, P <0.001). Figure 2 presents separately the cumulative hazard for non-injured, medical-only injured and lost-time injured workers. Among non-injured workers, the cumulative hazard was considerably lower than that of medical-only and lost-time injured workers, and the differences were statistically significant (log-rank test, χ2=4383, Pr <0.001).
Figure 1.
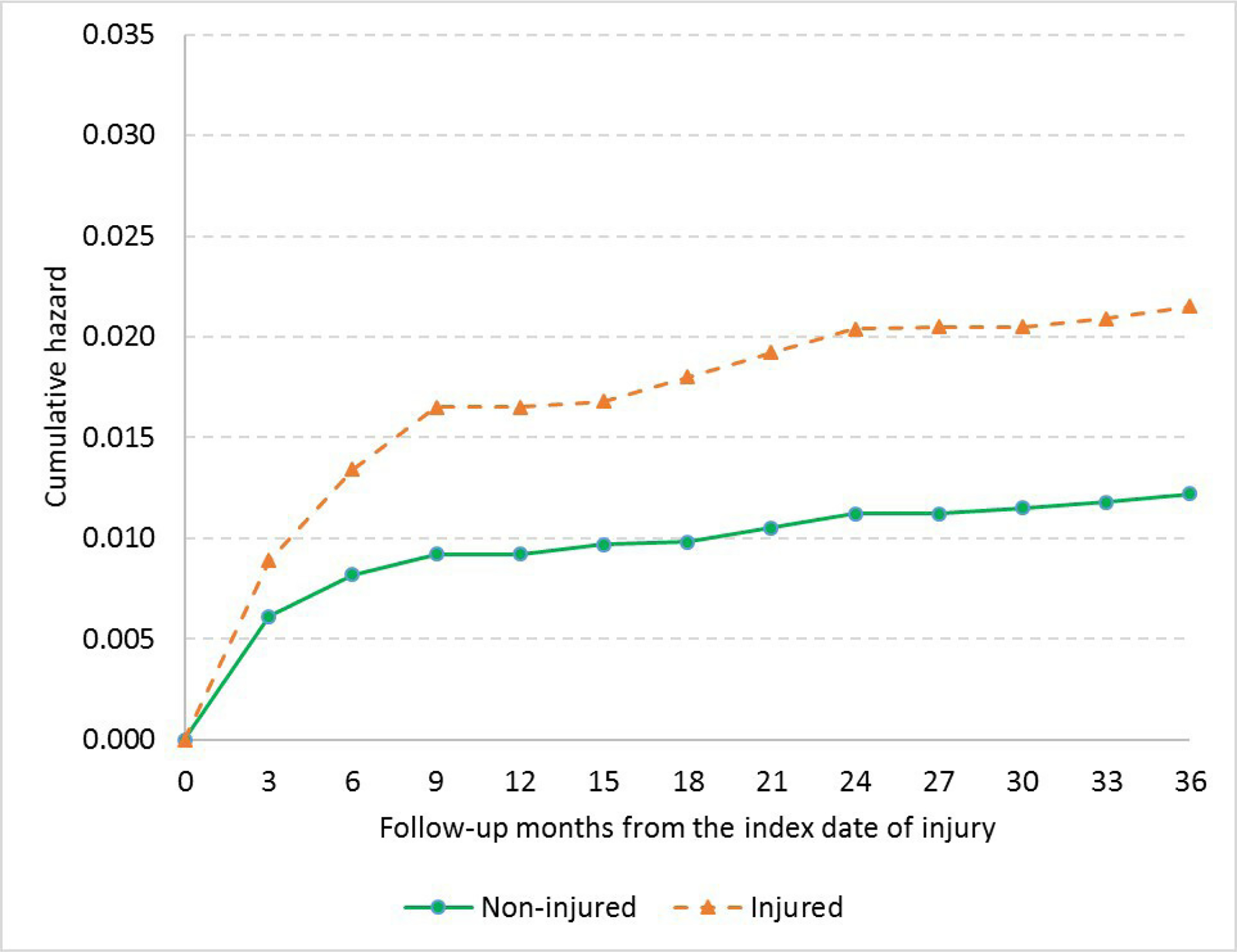
Nelson-Aalen cumulative hazard of opioid-related morbidity for non-injured and injured workers.
Figure 2.
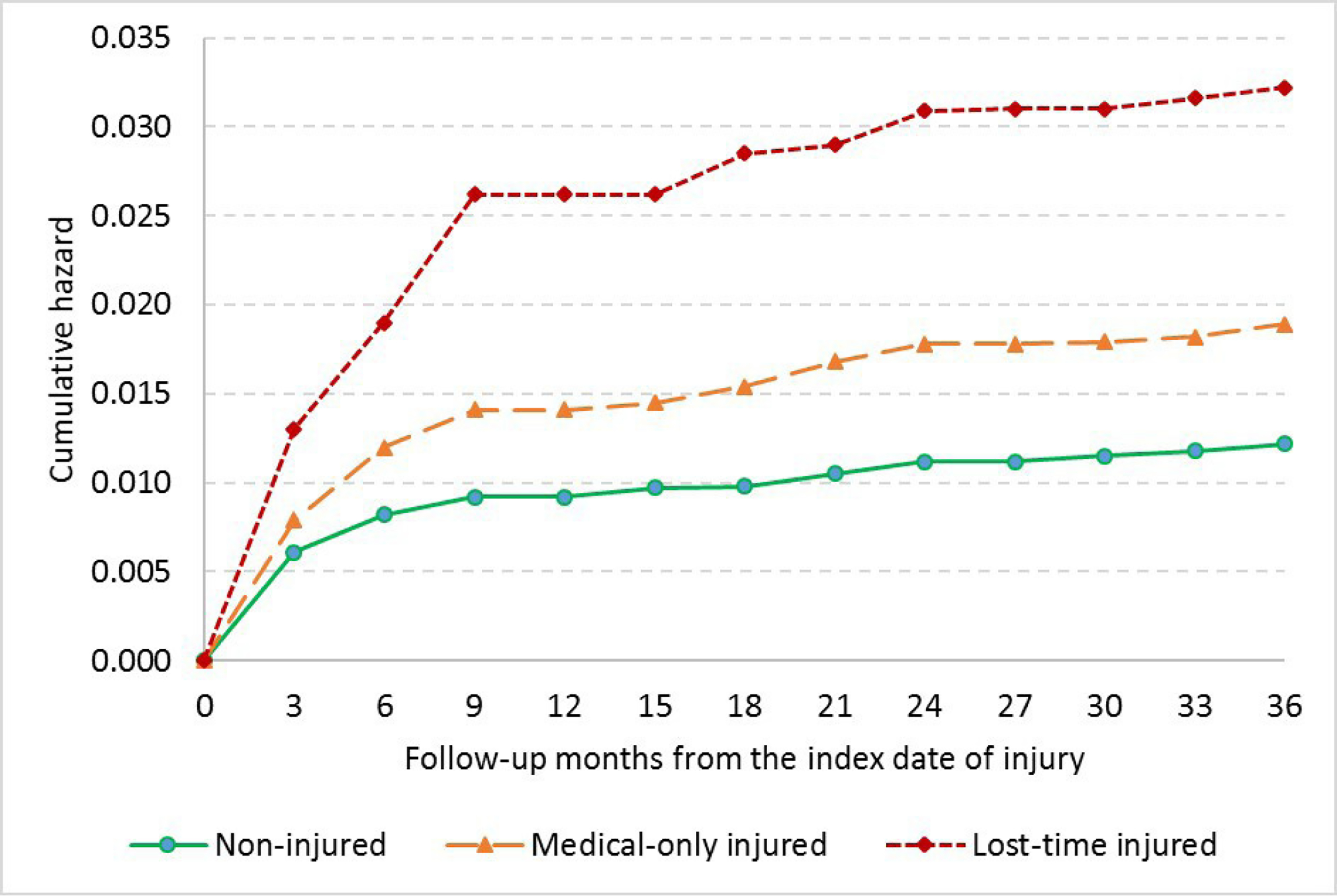
Nelson-Aalen cumulative hazard of opioid-related morbidity for non-injured, medical-only injured and lost-time injured workers.
Multivariable analysis: Cox PH regression
In the multivariable analysis, we estimated a Cox PH model. All variables, except age group and region, satisfied the PH assumption. Therefore, we stratified the results by age group and region. Table 2 presents the estimated HRs for opioid-related morbidity, adjusted for sex, health insurance plan type, industry and region and stratified by age group and region.
Table 2.
Hazard of opioid-related morbidity: Cox PH regression results stratified by age groups and region
| Model 1* |
Model 2† |
|||
|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | |
| Non-injured (ref.) | ||||
| Injured | 1.79 | 1.24 to 2.60 | ||
| Medical-only injured | 1.54 | 1.02 to 2.32 | ||
| Lost-time injured | 2.91 | 1.75 to 4.84 | ||
| Male | 1.14 | 0.65 to 2.01 | 1.14 | 0.65 to 2.01 |
| Health insurance type | ||||
| Preferred provider organisation plan (ref.) | ||||
| Consumer directed health plans | 0.94 | 0.49 to 1.82 | 0.94 | 0.49 to 1.82 |
| Comprehensive | 0.49 | 0.13 to 1.83 | 0.49 | 0.13 to 1.84 |
| High-deductible health and exclusive provider organisation plan | 0.04 | 0.01 to 0.15 | 0.04 | 0.01 to 0.15 |
| Health maintenance organisation | 2.47 | 0.91 to 6.71 | 2.47 | 0.91 to 6.72 |
| Point-of-service plan | 2.54 | 1.14 to 5.67 | 2.54 | 1.14 to 5.66 |
| Industry | ||||
| Services (ref.) | ||||
| Manufacturing – durable goods | 2.65 | 1.08 to 6.49 | 2.64 | 1.08 to 6.47 |
| Manufacturing – non-durable goods | 1.76 | 0.61 to 5.11 | 1.75 | 0.60 to 5.09 |
| Transportation, communications and utilities | 1.40 | 0.60 to 3.24 | 1.38 | 0.59 to 3.21 |
| Other‡ | ||||
| Number of obs. | 57 525 | |||
| Wald χ2 (14) | 114.34 | |||
| Prob>χ2 | 0.0001 | |||
All injured workers together.
Injured workers were divided into two: medical-only and lost-time injured workers.
Coefficients could not be estimated due to small number of observations for this category.
PH, proportional hazard.
In model 1, we divided workers into two groups: injured and non-injured; in model 2, we divided them into three: non-injured, medical-only injured and lost-time injured. Compared with their matched non-injured workers, the hazard of opioid-related morbidity was statistically significantly higher among injured workers (HR=1.79; 95% CI 1.24 to 2.60), controlling for covariates. In model 2, the hazard of opioid-related morbidity for medical-only and lost-time injured workers was 1.54 (95% CI 1.02 to 2.32) and 2.91 (95% CI 1.75 to 4.84), respectively.
Table 2 also presents the HR associated with other covariates. We did not find a statistically significant difference in HRs by sex. We identified an increased hazard in workers insured through HMO and POS health insurance plans compared with workers insured through PPOs, the reference health insurance type. The hazard was also higher for workers in manufacturing compared with workers in services, the reference industry sector.
DISCUSSION
Opioid overdose and related harms have become a leading public health problem in the USA, with 70 000 drug overdose deaths in 2017 alone, of which about 68% involved opioids.3 Degenhardt et al,28 reviewed the literature on mortality among people who were opioid dependent and concluded that their crude mortality rates were significantly elevated, and the most common cause of death was opioid overdose. In a longitudinal study, Joe and Simpson29 showed that the death rate for people with opioid addiction was 6.9 times that of the general population.
In this study, we examined the impact of workplace injury on opioid-related morbidity, following a cohort of injured and noninjured workers for 36 months after the index date of injury. Previous studies have suggested a link between workplace injuries and opioid-related morbidity.16,25,30 However, because preinjury opioid misuse, overdose and use disorders are potential confounders, estimates of the causal effect of workplace injuries may have suffered from confounding bias. This study reduces this confounding by limiting subjects to people who had not been diagnosed prior to injury.
Both univariate and multivariable analyses showed that workplace injury increased the hazard of opioid- related morbidity within 36 months after the index date of injury. The univariate analysis showed that the overall incidence rate for injured workers during the 3-year study period was 0.0053. Extrapolating to the US population of workers with private health insurance suggests that about 13 000 workers injured in 2014 were newly diagnosed with opioid-related morbidity between 2014 and 2017 due to workplace injury.
The Cox regression results showed that workplace injury increased the hazard of opioid-related morbidity by 79% within 36 months after the index date of injury, controlling for covariates and baseline differences in observed characteristics. There was a dose-response relationship between severity of injury and the hazard of opioid-r elated morbidity. Compared with non-injured workers, the hazard was 54% higher for medical-only injured workers and 191% higher for lost-time injured workers (table 2). Our results are consistent with the results of recent studies that showed elevated risk of mortality from drug overdose for lost-time injured workers compared with medical-only injured workers, controlling for covariates.15,16
There could be several reasons why workplace injuries, particularly, severe workplace injuries are associated with an increased hazard of opioid-related morbidity. First, there is evidence that injured workers are frequently prescribed opioids. Using workers’ compensation data, Stover et at31 showed that 1 out of 3 workers with a low back injury received an opioid prescription. Franklin et al also showed that half of workers with workplace injury received opioids at their first medical visit.32 Second, workers might not be able to afford to stay out of work and want to return to work quickly, despite lingering pain.5,14 In addition, work-related injury increases the risk of depression,33 and depression can lead to opioid-related morbidity.25
Workers insured through HMO and POS health insurance plans had increased risk of being diagnosed with opioid-related morbidity compared with workers insured through a PPO plan, the reference category. We are not aware of evidence that might explain this finding. Health plan types might differ in prescribing patterns, diagnostic practices, coverage for treatment of opioid related conditions, deductibles, network services and referral from primary physicians. Future studies could further explore the impact of health plan type on opioid-related diagnoses.
We note that pharmaceutical opioid use in the USA is much higher than in other countries.34 Still, opioid prescribing has been increasing, for example, in Canada and several Western European countries.34 If these trends continue, these countries may consider addressing the possible increased risk to injured workers of oversubscribing of opioids.
The study has some limitations. First, MarketScan data do not have detailed sociodemographic information such as race, education, marital status and wages. Consequently, we could not control for the effect of these variables or for imbalances between injured and non-injured workers in these variables. As a result, unlike randomised controlled studies where the two groups are expected to be similar in both observed and unobserved characteristics, our study guaranteed a balanced distribution only of the limited covariates available. Second, MarketScan has very crude industry classification, and this might limit our ability to control for the substantial variation in injury risk and substance use across different industries. In addition to this, although the MarketScan weights are designed to reflect the national distribution of people with employer-sponsored private health insurance, they do not reflect the industry composition of the US workforce. Third, the data source for opioid-related morbidity in this study is the group health insurance system. It could be that opioids are initially prescribed through the workers’ compensation system, and then opioid-related morbidity is diagnosed and treated through the regular health insurance system. We do not know if some workers received treatment for opioid- related morbidity through the workers’ compensation system. This would bias our estimates towards the null. Fourth, some workers may have developed opioid morbidity but not been diagnosed. If this undiagnosed opioid morbidity was differential with respect to injury status, it could bias the estimated results. Moreover, we did not consider the injury status of workers before 2013, so we may have included some previously injured workers in our analysis. We might have thus underestimated the effect of injury on opioid-related morbidity. Fifth, we considered workers who were employed and enrolled in the group health insurance continuously between 2013 and 2017. This might underestimate the effect of injury on opioid- related morbidity if injured workers are more likely to leave their jobs than non-injured workers. Six, the MarketScan data represent workers at medium to large employers offering health insurance, who enrol in that health insurance and who are not generally enrolled in Medicaid or Medicare. Finally, we considered only diagnosed opioid-related morbidity, and this might have underestimated the true proportion of workers with opioid-related morbidity but who did not get treatment.
CONCLUSION
We found a statistically significant impact of workplace injury on opioid-related morbidity. Workplace injury increased the hazard of opioid-r elated morbidity by 54% for medical-only injured workers and by 191% for lost-time injured workers compared with individually matched non-injured workers and controlling for covariates. We conclude that medical providers may want to pay special attention to the elevated risk of opioid-related morbidity among injured workers. A recent study of injured workers has concluded that initial prescribing patterns and the part of body injured can affect long-term opioid use.35 Also, prior studies have shown that both insurer and state-level policies sensitive to this risk have reduced the number of postinjury opioid prescriptions.36 Reducing workplace injury or severity of workplace injury, as well as efforts to ensure opioid prescriptions for injured workers are limited to situations where benefits are likely to outweigh risks may help to reduce opioid dependence, opioid abuse, illicit opioid use, overdose and subsequent mortality.
Supplementary Material
Key messages.
What is already known about this subject?
► Recent papers have shown the association of work-related injuries and opioid use. However, the direction of causation could not be determined, because preinjury opioid use could increase the risk of injury.
What are the new findings?
► This paper addresses this concern by estimating the postinjury increase in opioid-related diagnoses in a population without prior diagnoses. This is the first paper to isolate the impact of work-related injuries on opioid-related morbidity.
How might this impact on policy or clinical practice in the foreseeable future?
► The opioid epidemic has been a major public health concern for several decades. This paper makes it clear that treatment of injured workers has contributed to this epidemic and presents the case for focusing on that treatment. Measures that reduce workplace injury or severity as well as efforts to ensure appropriate opioid prescribing for injured workers can help to reduce the societal costs of opioid use.
Acknowledgements
We would like to thank Regina Pana-Cryan, Erin Parker, Brian Quay, Suzanne Marsh, Steven Wurzelbacher, Brian Chin and Edward Krieg for their valuable comments and suggestions.
Footnotes
Competing interests None declared.
Patient consent for publication Not required.
Ethics approval MarketScan Research Databases are fully compliant with the Health Insurance Portability and Accountability Act, and no Institutional Review Board approval was necessary because individual patients were not identifiable with the data.
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement Data are available on reasonable request. Data may be obtained from a third party and are not publicly available. The data we used for the analyses, the IBM MarketScan Research Databases, are available only for subscribers (https://www.ibm.com/products/marketscan-research-databases).
REFERENCES
- 1.Dowell D, Arias E, Kochanek K, et al. Contribution of Opioid-Involved poisoning to the change in life expectancy in the United States, 2000–2015. JAMA 2017;318:1065–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seth P, Scholl L, Rudd RA, et al. Overdose Deaths Involving Opioids, Cocaine, and Psychostimulants - United States, 2015–2016. MMWR Morb Mortal Wkly Rep 2018;67:349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scholl L, Seth P, Kariisa M, et al. Drug and opioid-involved overdose deaths—United states, 2013–2017. MMWR 2019;67:1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strunin L, Boden LI. Family consequences of chronic back pain. Soc Sci Med 2004;58:1385–93. [DOI] [PubMed] [Google Scholar]
- 5.Franklin GM, Rahman EA, Turner JA, et al. Opioid use for chronic low back pain: a prospective, population-based study among injured workers in Washington state, 2002–2005. Clin J Pain 2009;25:743–51. [DOI] [PubMed] [Google Scholar]
- 6.O’Hara NN, Pollak AN, Welsh CJ, et al. Factors associated with persistent opioid use among injured workers’ compensation claimants. JAMA Netw Open 2018;1:e184050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernacki EJ, Yuspeh L, Lavin R, et al. Increases in the use and cost of opioids to treat acute and chronic pain in injured workers, 1999 to 2009. J Occup Environ Med 2012;54:216–23. [DOI] [PubMed] [Google Scholar]
- 8.Schieber LZ, Guy GP, Seth P, et al. Trends and patterns of geographic variation in opioid prescribing practices by state, United States, 2006–2017. JAMA Netw Open 2019;2:e190665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thumula V, Wang D, Liu T. Interstate variations in use of opioids. Workers Compensation Research Institute; 2017:1–129. [Google Scholar]
- 10.NCCI. Medical data report opioid utilization supplement for the state of new Mexico, 2017.
- 11.Krebs EE, Gravely A, Nugent S, et al. Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: the space randomized clinical trial. JAMA 2018;319:872–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nkyekyer EW, Fulton-Kehoe D, Spector J, et al. Opioid and benzodiazepine use before injury among workers in Washington state, 2012 to 2015. J Occup Environ Med 2018;60:820–6. [DOI] [PubMed] [Google Scholar]
- 13.Savych B, Neumark D, Lea R. Do opioids help injured workers recover and get back to work? the impact of opioid prescriptions on duration of temporary disability. Ind Relat 2019;58:549–90. [Google Scholar]
- 14.Hawkins D, Roelofs C, Laing J, et al. Opioid-related overdose deaths by industry and occupation-Massachusetts, 201 1–2015. Am J Ind Med 2019;62:815–25. [DOI] [PubMed] [Google Scholar]
- 15.Martin CJ, Jin C, Bertke SJ, et al. Increased overall and cause-specific mortality associated with disability among workers’ compensation claimants with low back injuries. Am J Ind Med 2020;63:209–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Applebaum KM, Asfaw A, O’Leary PK, et al. Suicide and drug-related mortality following occupational injury. Am J Ind Med 2019;62:733–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leslie DL, Kobre RA, Richmand BJ, et al. Temporal association of certain neuropsychiatric disorders following vaccination of children and adolescents: a pilot case-control study. Front Psychiatry 2017;8:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hansen L The Truven health MarketScan databases for life sciences researchers: Truven health analytics. IBM Watson Health, 2017. [Google Scholar]
- 19.D’gostino RB. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 1998;17:2265–81. [DOI] [PubMed] [Google Scholar]
- 20.Austin PC. Statistical criteria for selecting the optimal number of untreated subjects matched to each treated subject when using many-to-one matching on the propensity score. Am J Epidemiol 2010;172:1092–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci 2010;25:1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rubin DB. Using propensity scores to help design observational studies: application to the tobacco litigation. Ann Intern Med 2001;2:169–88. [Google Scholar]
- 23.Cohen J Statistical power analysis for the behavioral sciences. Routledge, 2013. [Google Scholar]
- 24.Maeda A, Bateman BT, Clancy CR, et al. Opioid abuse and dependence during pregnancy: temporal trends and obstetrical outcomes. Anesthesiology 2014;121:1 158–65. [DOI] [PubMed] [Google Scholar]
- 25.Boscarino JA, Rukstalis M, Hoffman SN, et al. Risk factors for drug dependence among out-patients on opioid therapy in a large US health-care system. Addiction 2010;105:1776–82. [DOI] [PubMed] [Google Scholar]
- 26.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958;53:457–81. [Google Scholar]
- 27.Bureau of Labor Statistics (BLS). Employed persons by occupation, sex, and age Labor Force Statistics from the Current Population Survey.
- 28.Degenhardt L, Bucello C, Mathers B, et al. Mortality among regular or dependent users of heroin and other opioids: a systematic review and meta-analysis of cohort studies. Addiction 2011;106:32–51. [DOI] [PubMed] [Google Scholar]
- 29.Joe GW, Simpson DD. Mortality rates among opioid addicts in a longitudinal study. Am J Public Health 1987;77:347–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shei A, Rice JB, Kirson NY, et al. Sources of prescription opioids among diagnosed opioid abusers. Curr Med Res Opin 2015;31:779–84. [DOI] [PubMed] [Google Scholar]
- 31.Stover BD, Turner JA, Franklin G, et al. Factors associated with early opioid prescription among workers with low back injuries. J Pain 2006;7:718–25. [DOI] [PubMed] [Google Scholar]
- 32.Franklin GM, Stover BD, Turner JA, et al. Early opioid prescription and subsequent disability among workers with back injuries: the disability risk identification study cohort. Spine 2008;33:199–204. [DOI] [PubMed] [Google Scholar]
- 33.Asfaw A, Souza K. Incidence and cost of depression after occupational injury. J Occup Environ Med 2012;54:1086–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Degenhardt L, Grebely J, Stone J, et al. Global patterns of opioid use and dependence: harms to populations, interventions, and future action. The Lancet 2019;394:1560–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Durand Z, Nechuta S, Krishnaswami S, et al. Prevalence and risk factors associated with long-term opioid use after injury among previously Opioid-Free workers. JAMA Netw Open 2019;2:e197222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Franklin G, Sabel J, Jones CM, et al. A comprehensive approach to address the prescription opioid epidemic in Washington state: milestones and lessons learned. Am J Public Health 2015;105:463–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


