Abstract
Background
To investigate intention rates to get vaccinated against COVID-19 among healthcare personnel (HCP) in Greece.
Methods
Cross-sectional survey.
Results
The response rate was 14.5%. Of 1521 HCP with a known profession, 607 (39.9%) were nursing personnel, 480 (31.6%) physicians, 171 (11.2%) paramedical personnel, 72 (4.7%) supportive personnel, and 191 (12.6%) administrative personnel. Overall, 803 of 1571 HCP (51.1%) stated their intention to get vaccinated while 768 (48.9%) stated their intention to decline vaccination. Most HCP (71.3%) who reported intent to get vaccinated noted contributing to the control of the pandemic and protecting their families and themselves as their reasons, while the most common reason for reporting intent to decline vaccination was inadequate information about the vaccines (74.9%), followed by concerns about vaccine safety (36.2%). Logistic regression analysis revealed that the probability of intending to get vaccinated increased with male gender, being a physician, history of complete vaccination against hepatitis B, history of vaccination against pandemic A (H1N1) in 2009–2010, belief that COVID-19 vaccination should be mandatory for HCP, and increased confidence in vaccines in general during the COVID-19 pandemic. The following factors were associated with a lower intention to get vaccinated: no vaccination against influenza the past season, no intention to get vaccinated against influenza in 2020–2021, and no intention to recommend COVID-19 vaccination to high-risk patients.
Conclusion
There is an urgent need to built safety perception towards COVID-19 vaccines and raise vaccine uptake rates by HCP, and thus to protect the healthcare workforce and the healthcare services.
Keywords: COVID-19, SARS-CoV-2, Vaccine, Healthcare personnel, Knowledge, Attitudes
Introduction
Shortly following the emergence in late 2019 and global spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the etiologic agent of coronavirus disease 2019 (COVID-19), the consequences on healthcare systems became evident [1]. HCP have been recognized as a high-risk group for occupational exposure to SARS-CoV-2 and onset of clinical illness, while fatalities occurred [[2], [3], [4], [5], [6]]. Moreover, high rates of absenteeism were noted among HCP, either because of infection or for post-exposure isolation purposes [7].
Starting this autumn, healthcare facilities around the world are experiencing an unprecedented surge of healthcare demands in association with a considerable influx of patients [1,8]. HCP constitute a high-priority group for COVID-19 vaccination [9,10]. Aside from protection of HCP, the rationale for vaccination relies also on the need to preserve the essential healthcare services from outbreaks and HCP absenteeism [9]. The underlying arguments for HCP prioritization for vaccination also include the principle of reciprocity, given their work under intense conditions, putting themselves but also potentially their households at higher risk for the sake of patients [9]. Nonetheless, there are scarce published data about the attitudes and practices of HCP towards COVID-19 vaccines [[11], [12], [13]]. Beyond the expected benefits for themselves and the healthcare systems, their attitudes may influence the acceptance of COVID-19 vaccines by the general population, given their role as trusted sources of information about vaccines [14,15], and about COVID-19 in particular [16]. This could be crucial since high vaccine uptake rates are needed to achieve herd immunity [17]. Herein we present the results of a cross-sectional survey that was conducted in order to estimate the level of intention to get vaccinated against COVID-19 and to explore factors that drive vaccine decision-making in HCP in Greece.
Methods
We contacted the Infection Control Committees of eight tertiary-care hospitals (five public hospitals including one pediatric, two private hospitals and one military hospital) across Greece and invited them to participate in the survey. All hospitals agreed to participate. There were 10,930 HCP employed in these hospitals.
Data collection
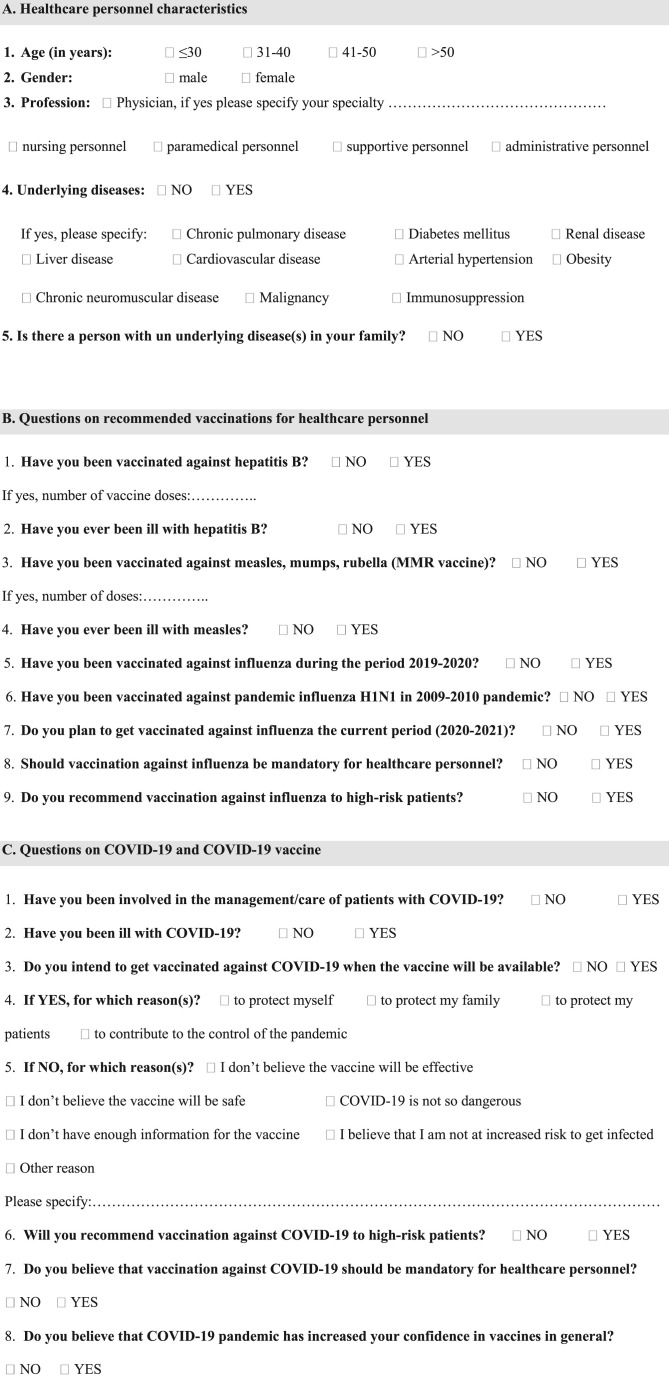
A structured questionnaire was developed based on our past experience with studies on seasonal and pandemic influenza vaccination of HCP (Fig. 1 ) [18,19]. The printed questionnaire (in Greek language) was distributed to HCP, regardless of their characteristics, during their work shift by the Infection Control nurses Committee of each hospital. The Infection Control Committees are established by low in each hospital in order to promote measures for the prevention and control of healthcare-associated infections, including vaccinations of HCP. The following data were collected per HCP: demographic and professional characteristics, vaccination history against hepatitis B and measles, history of hepatitis B and measles, attitudes and practices toward seasonal influenza vaccination, history of vaccination against H1N1 during the 2009–2010 pandemic, and attitudes toward mandatory COVID-19 vaccination. The HCP’ intention to get vaccinated against COVID-19 was recorded, as well as their reasons for intention to accept to decline vaccination. Data were self-reported and anonymous. The survey was conducted from September 1 through October 31, 2020.
Figure 1.
Questionnaire on the intention of healthcare personnel to get vaccinated against COVID-19.
Definitions
HCP were defined as persons employed in healthcare facilities with or without direct contact with patients or infectious materials and regardless of their employment status (permanent, casual, or contract HCP). HCP were grouped as follows: physicians, nursing personnel (nurses, midwifes, and nurse assistants), paramedical personnel (pharmacists, biologists, laboratory technicians, physiotherapists, ambulance personnel, social workers, health visitors), supportive personnel (information systems personnel, engineers, waiters, cleaners, laundry personnel, security personnel), and administrative personnel. Physicians were further grouped according to their specialty/subspecialty as follows: internal medicine specialists (e.g. internists, pediatricians, infectious diseases specialists, intensive care physicians, gastroenterologists, neurologists), surgical specialists (e.g. surgeons, obstetricians, urologists, ophthalmologists, orthopedics, neurosurgeons), laboratory physicians (e.g. microbiologists, immunologists, cytologists, anatomists), and imaging specialists (radiologists, nuclear medicine specialists). Complete vaccination was defined as three hepatitis B vaccine shots for hepatitis B and two measles vaccine shots for measles (all shots within the appropriate dose scheme for each disease).
Ethical issues
Participation of HCP was voluntary following oral informed consent obtained by the Infection Control Committees. Approval was obtained from the Ethics Committees of the participating hospitals. The data were managed in accordance with the national and European laws.
Statistical analysis
Frequencies and percentages were used for categorical variables. Comparisons between groups were performed by using the two-tailed t-test for continuous variables with normal distribution, and the chi-square test for categorical variables. In order to explore the factors that predict HCP's intention to get vaccinated against SARS-CoV-2, a logistic regression analysis has been conducted by integrating in the model only variables with a p-value of ≤0.10 in the univariate analyses. Odds ratio (OR) and confidence intervals (CIs) were estimated. P-values of ≤0.05 were considered statistically significant. The statistical analysis was conducted using the IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp.
Results
A total of 1591 HCP participated in the study (14.5% of HCP working in the participating hospitals). Table 1 shows their characteristics. Nursing personnel accounted for most participants followed by physicians [607 (38.2%) and 480 (30.2%), respectively]. Twenty HCP did not answer the question about their intention to get vaccinated against COVID-19. Of the remaining 1571 HCP, 803 HCP (51.1%) stated their intention to get vaccinated against COVID-19 while 768 (48.9%) stated that they did not intent to get vaccinated. Table 2 shows the results of the univariate analyses in relation to intention to get vaccinated against COVID-19. Men, physicians, HCP with comorbidities, and HCP already involved in the healthcare of patients with COVID-19 had higher rates of intention to get vaccinated compared to women, professions other than physicians, HCP with no comorbidities, and HCP with no history of involvement in the healthcare of COVID-19 patients (p-values <0.001, <0.001, <0.001, and 0.006, respectively). Table 3 shows the rates of intention of HCP to get vaccinated against COVID-19 according to their attitudes and practices towards occupational vaccinations. Significantly higher rates of intention to get vaccinated were noted among HCP who have completed their vaccination against hepatitis B, had received the pandemic A (H1N1) vaccine in 2009–2010 and the seasonal influenza vaccine the past season, intend to receive influenza vaccination the current season, agree with mandatory vaccination policies for HCP against influenza and COVID-19, recommend vaccination against influenza and COVID-19 to high-risk patients, and whose confidence to vaccines in general increased during the COVID-19 pandemic (p-values <0.001 for all comparisons). In particular, 776 (49.8%) of participating HCP favored mandatory vaccinations policies, and 83.9% of those who intend to get a COVID-19 vaccine. Overall, 78.7% of responding HCP reported that they intend to recommend COVID-19 vaccination to high-risk patients, regardless of their intention to get vaccinated. The total number of HCP who intended to get a COVID-19 vaccine and intended to recommend it to high-risk patients was 785. Of them, 589 (75%) received influenza vaccine the past season, 679 (86.5%) intended to get influenza vaccine the 2020–2021 season, 775 (99.4%) recommended influenza vaccination to high-risk patients, 665 (85.4%) believe that influenza vaccination should be mandatory for HCP and 637 (81.7%) believe that COVID-19 vaccination should be mandatory for HCP (p-values <0.001 for all comparisons).
Table 1.
Characteristics of 1591 HCP.
| Characteristic | HCP N (%) |
|---|---|
| Gender (n = 1544) | |
| Male | 540 (35) |
| Female | 1004 (65) |
| Age group, years (n = 1591) | |
| ≤30 | 282 (17.7) |
| 31-40 | 363 (22.8) |
| 41-50 | 450 (28.3) |
| >50 | 496 (31.2) |
| Profession (n = 1521) | |
| Physiciana | 480 (31.6) |
| Nursing personnel | 607 (39.9) |
| Paramedical personnel | 171 (11.2) |
| Supportive personnel | 72 (4.7) |
| Administrative personnel | 191 (12.6) |
| Comorbiditiesb (n = 1591) | 361 (22.7) |
| Family member with a comorbidity (n = 1591) | 702 (44.1) |
| Complete vaccination against hepatitis B (n = 639) | 480 (75.1) |
| Complete vaccination against measles (n = 294) | 253 (86.1) |
| Vaccination against pandemic A (H1N1)c (n = 1591) | 445 (28) |
| Influenza vaccination in 2019–2020 (n = 1591) | 945 (59.4) |
| Intention to get influenza vaccination in 2020–2021 (n = 1583) | 1084 (68.5) |
| Involvement in care of a COVID-19 case (n = 1591) | 431 (27.1) |
| History of COVID-19 (n = 1591) | 115 (7.2) |
COVID-19: coronavirus disease 2019; n: the number of HCP who answered the specific question.
Of 424 physicians for whom their specialty was known: internal medicine specialists: 257; surgical specialists: 107; laboratory specialists: 35; imaging specialists: 11; no specialty: 14.
361 HCP had a total of 442 comorbidities: hypertension (129); obesity (71); diabetes mellitus (59); chronic pulmonary disease (50); immunosuppression (44); chronic cardiovascular disease (37); malignancy (28); chronic neurological disease (12); chronic renal disease (7); chronic hepatic disease (5).
In 2009–2010.
Table 2.
Intention to get vaccinated against COVID-19 by characteristics of HCP (univariate analyses).
| Characteristic | Intention to get vaccinated (%) | P-value |
|---|---|---|
| Gender (n = 1525) | ||
| Male | 66.4 | <0.001 |
| Female | 43.0 | |
| Age group, years (n = 1571) | ||
| ≤30 | 50.2 | 0.744∗ |
| 31-40 | 52.8 | |
| 41-50 | 49.3 | |
| >50 | 52.0 | |
| Profession (n = 1504) | ||
| Physician | 71.5 | <0.001∗∗ |
| Nursing personnel | 43.0 | |
| Paramedical personnel | 46.1 | |
| Supportive personnel | 48.6 | |
| Administrative personnel | 42.6 | |
| Comorbidities (n = 1571) | ||
| Yes | 61.1 | <0.001 |
| No | 48.1 | |
| Family member with a comorbidity (n = 1571) | ||
| Yes | 51.7 | 0.664 |
| No | 50.6 | |
| Involvement in the care of patients with COVID-19 (n = 1571) | ||
| Yes | 56.8 | 0.006 |
| No | 49.0 | |
COVID-19: coronavirus disease 2019; HCP: healthcare personnel; n: the number of HCP who answered.
∗The p-value refers to the comparison of HCP ≤30 years old with other age categories.
∗∗The p-value refers to the comparison of physicians with all other professional categories separately.
Table 3.
Intention to get vaccinated against COVID-19 by attitudes and practices about occupational vaccinations of HCP (univariate analyses).
| Finding | Intention to get vaccinated (%) | P-value |
|---|---|---|
| Complete vaccination against hepatitis B (n = 631) | ||
| Yes | 64.3 | 0.001 |
| No | 49.0 | |
| Complete vaccination against measles (n = 287) | ||
| Yes | 61.5 | 0.676 |
| No | 65.0 | |
| Vaccination against pandemic A (H1N1)a (n = 1571) | ||
| Yes | 72.0 | <0.001 |
| No | 43.0 | |
| Influenza vaccination in 2019–2020 (n = 1571) | ||
| Yes | 64.0 | <0.001 |
| No | 32.0 | |
| Intention to get influenza vaccination in 2020–2021 (n = 1571) | ||
| Yes | 64.5 | <0.001 |
| No | 22.2 | |
| Influenza vaccination should be mandatory for HCP (n = 1554) | ||
| Yes | 66.4 | <0.001 |
| No | 22.2 | |
| Recommend influenza vaccination to high-risk patients (n = 1560) | ||
| Yes | 53.3 | <0.001 |
| No | 7.7 | |
| COVID-19 vaccination should be mandatory for HCP (n = 1548) | ||
| Yes | 83.9 | <0.001 |
| No | 19.0 | |
| Intend to recommend SARS-CoV-2 vaccination to high-risk patients (n = 1547) | ||
| Yes | 64.6 | <0.001 |
| No | 3.9 | |
| Increased confidence to vaccines because of COVID-19 pandemic (n = 1548) | ||
| Yes | 75.9 | <0.001 |
| No | 40.7 | |
COVID-19: coronavirus disease 2019; HCP: healthcare personnel; n: the number of HCP who answered.
In 2009–2010.
Table 4, Table 5 summarize the reasons for reporting intention to get vaccinated against COVID-19 or for reporting intention to decline COVID-19 vaccination, respectively. The mean, median, and mode of cited reasons for intention to get vaccinated were 2.7, 3, and 4, respectively. The mean, median and mode of cited reasons for intention to decline vaccination were 1.34, 1, and 1, respectively. Most HCP (71.3%) who reported intention to get vaccinated noted contributing to the control of the pandemic and protecting their families and themselves as their most commonly selected reasons, while the most common reason for reporting intention to decline vaccination was, at least in part, inadequate information about the vaccines (74.9%) followed by concerns about vaccine safety (36.2%). The logistic regression analysis found that the following variables were significantly associated with an increased rate of intention to get vaccinated against COVID-19: male gender, being a physician, being completely vaccinated against hepatitis B, have been vaccinated against pandemic A (H1N1) in 2009–2010, belief that COVID-19 vaccination should be mandatory for HCP, and increased confidence in vaccines in general during the ongoing COVID-19 pandemic (Table 6 ). In addition, the following factors were significantly associated with a lower intention to get vaccinated against COVID-19: no vaccination against influenza the past season, no intention to get vaccinated against influenza in 2020–2021, and no intention to recommend COVID-19 vaccination to high-risk patients (Table 6). The logistic regression model was statistically significant explaining 67.4% of the variance in the intention of HCP to get vaccinated against COVID-19; this was based on an adjusted R2. Eighty-five percent of the cases were correctly classified. The area under the curve was 0.922 (95% CIs: 0.907 to 0.935; p-value = 0.006).
Table 4.
Reasons for reporting intention to get vaccinated against COVID-19 among HCP in Greece.
| Reason | Reporting rate∗ (%) N = 803 |
|---|---|
|
544 (67.6) |
|
560 (69.7) |
|
464 (57.8) |
|
573 (71.3) |
∗Percentages do not round up to 100 since more than one answers were acceptable.
∗∗The differences between answer 1 and answers 2 and 4 were not statistically significant (p-values 0.179 and 0.555, respectively).
∗∗∗The differences between answer 3 and answers 1, 2 and 4 were statistically significant (p-values <0.05).
Table 5.
Reasons for reporting intention to decline COVID-19 vaccination among HCP in Greece.
| Reason | Reporting ratea (%) N = 768 |
|---|---|
| Concerns about vaccine efficacy | 77 (10.0) |
| Concerns about vaccine safety | 278 (36.2) |
| Perception that COVID-19 is not a dangerous disease | 24 (3.1) |
| Not enough information about the vaccine | 575 (74.9) |
| Perception of not being at risk for infection | 30 (3.9) |
| Other reasonb | 35 (4.5) |
Percentages do not round up to 100 since more than one answers were acceptable.
In 19 cases, the HCP raised concerns about the rapid development and entry of COVID-19 vaccines in the market.
Table 6.
Factors associated with intention to get vaccinated against COVID-19 among HCP (logistic regression analysis).
| Significant factors | OR | 95% CIs | p-value |
|---|---|---|---|
| Male gender | 2.20 | 1.57–3.08 | <0.001 |
| Physician | 1.95 | 1.33–2.87 | <0.001 |
| Complete vaccination against hepatitis B | 1.50 | 1.06–2.14 | 0.02 |
| Vaccination against pandemic A (H1N1)a | 1.90 | 1.31–2.75 | <0.001 |
| No influenza vaccination the past year | 0.47 | 0.32–0.69 | <0.001 |
| No intention to get influenza vaccination this season | 0.34 | 0.23–0.52 | <0.001 |
| No recommendation of COVID-19 vaccination to high-risk patients | 0.06 | 0.03–0.12 | <0.001 |
| Belief that COVID-19 vaccination should be mandatory for HCP | 11.6 | 7.98–17.07 | <0.001 |
| Belief that the COVID-19 pandemic increased their confidence to vaccines in general | 1.50 | 1.06–2.12 | 0.02 |
COVID-19: coronavirus disease 2019; HCP: healthcare personnel; OR: odds ratio.
CIs: confidence intervals.
In 2009–2010.
Discussion
This is a cross-sectional survey conducted to estimate the level of intention to get vaccinated against COVID-19 and to understand characteristics and perceptions that may drive vaccine decision-making among HCP in Greece. To the best of our knowledge, there are few similar studies published so far [[11], [12], [13],20].
We found that only half of surveyed HCP intended to get the COVID-19 vaccine, which is of concern. Our finding could be partially attributed to the fact that our study was conducted at the beginning of the second pandemic wave in Greece, before the high demand on healthcare that far exceeded that of influenza season and the numerous fatalities that were recorded the next weeks. The lack of information about COVID-19 vaccines at that time also was critical for our surveyed HCP. Surveys of intention are only rough proxies for the actual behavior. A similar (55%) rate of intention to get vaccinated against COVID-19 was found in December 2020 in a survey conducted among 16,158 employees in a large Pennsylvania health system [21]. In this latter study, a substantial increase (79% among 1155 participating employees) in intention to receive a COVID-19 vaccine was recorded after the United States Food and Drug Administration voted to recommend an Emergency Use Authorization of a COVID-19 vaccine [21]. Notably, in a study that was conducted in the Democratic Republic of Congo, as low as 27.7% of 613 hospital-based HCP would accept COVID-19 vaccination [12]. In contrast, in a survey at a university hospital in France, 81.5% of 1421 HCP stated that they will certainly or probably agree to get vaccinated against COVID-19 [13]. The latter study was conducted during the first pandemic wave in a severely affected area, which most likely had an impact of HCP positive attitude towards vaccination [13]. Risk perception is crucial for vaccine decision-making. Evidence from a recently published survey that presented seven vaccine-preventable diseases in the United States revealed a significant increase in the proportion of people who intended to get vaccinated as risk of infection increased, and that increase was more pronounced when mortality was considered than mere morbidity [22]. Additional factors that may influence vaccine acceptance among HCP include knowledge, training but also the consolidation of a culture of occupation safety within healthcare facilities.
We also found significant differences across HCP professions. As also shown in studies from France, Congo, and Israel [12,20,23], physicians were more likely to report intention to get vaccinated against COVID-19 compared to other professions. In particular in our survey 71.5% of physicians and 43% of nursing personnel favored COVID-19 vaccination, which is similar to the 40% acceptance rate reported among nurses in Hong-Kong and the significant intention rate to delay COVID-19 vaccination among nurses compared to physicians in a Los Angeles study [11,24]. As of March 17 2021, the nationwide COVID-19 vaccine uptake rates were 77% among physicians and 51% among nursing personnel, which are increased compared to the recorded rates of intention to get vaccinated in our survey. Furthermore, in our study HCP involved in the management of patients with COVID-19 had higher rates of intention to get vaccinated compared to HCP with no involvement however, this was not the case in the Pennsylvania survey among 16,158 employees [21].
Differences of vaccine acceptance among HCP groups have been observed in seasonal influenza and pandemic H1N1 vaccines as well as in other vaccines and are attributed to different levels of knowledge or motivation for vaccination [19,25,26]. In our study men were also more likely to report intention to get vaccinated against COVID-19, as reported in other studies [12,20,23], but also in studies of pandemic H1N1 vaccine uptake [26], and it may be related to the perception of level of risk [22]. These findings can be used to guide interventions and focus on specific HCP groups. In accordance with the Israeli study [20], age was not a determinant of intention to get vaccinated in our study, which could be partially explained by the fact that the oldest HCP were 67 years old, as this is the retirement threshold.
Another finding of our study was that a positive attitude towards occupational vaccinations, as indicated by a history of complete hepatitis B vaccination, consecutive seasonal influenza vaccinations and pandemic H1N1 vaccination in 2009–2010, was significantly associated with increased rates of intention to get vaccinated against COVID-19. Higher rates of intention to get vaccinated against COVID-19 were also recorded among nurses who had received influenza vaccine in Hong Kong, and among HCP in France and Israel [11,23,25]. Higher vaccine uptake rates against pandemic H1N1, seasonal influenza, and hepatitis B have been recorded among HCP with a history of previous vaccination against seasonal influenza in Greece [18,19,26,27]. These findings underline the importance of increasing seasonal influenza vaccine uptake among HCP [28]. We should kept in mind however the limitation of generalizing from non-COVID-19 to COVID-19 vaccines. We also found that approximately half of HCP in our study favor a mandatory vaccination policy for COVID-19, while most HCP reported increased confidence in vaccines in general during the COVID-19 pandemic; these characteristics were significantly higher among those HCP who intent to get the COVID-19 vaccine. A recent Italian study found that HCP were more favorable to occupational vaccinations in general in September–December 2020 compared to January–December 2019, which indicates a potential role of the COVID-19 pandemic on their attitudes towards vaccines [29]. A recent United States study also found that persons who intended to get a COVID-19 vaccine significantly more often accepted COVID-19 vaccine mandates for adults, children and employees [30].
Our study also revealed that gaps in information and safety concerns were the main barriers for reporting intent to decline COVID-19 vaccination in surveyed HCP. In a similar line, the overwhelming majority (90.3%) of hesitant responders in the Pennsylvania survey reported concerns about unknown risks and insufficient data as main reasons for intending to decline vaccination [21]. In an Israeli study, a higher proportion (70%) of 829 HCP questioned the safety of COVID-19 vaccines [20]. Similarly, the main reasons for vaccine refusal among nurses in Hong-Kong were suspicion on its efficacy and safety [11]. Safety issues towards pandemic H1N1 vaccines were also raised by 43% of HCP who refused vaccination in a study of ours in 2009–2010, while gaps in information were reported by 27.8% [26]. Gaps in knowledge and misconceptions about their own risk for infection, vaccine effectiveness, and vaccine safety have been consistently identified as barriers to raise influenza vaccine uptake among HCP [28]. On the other hand, behavioral characteristics and education have been well recognized as core determinants of HCP attitudes and practices toward vaccinations [28]. Our findings point out to the need to early identify HCP hesitant to COVID-19 vaccine and efficiently address their concerns or gap of information. This is even more imperative since we found that vaccine hesitant HCP were less likely to recommend the COVID-19 vaccine to high-risk patients. Studies have shown that HCP serve as trusted sources of information about vaccines in general and COVID-19 vaccines in particular, and therefore may influence vaccine uptake by their patients [[14], [15], [16]]. In addition the current survey studied reasons for intending to receive a COVID-19 vaccine. To contribute to the control of the pandemic and protect their families and themselves were the most frequently cited reasons for intending to get vaccinated against COVID-19 in our surveyed HCP, along with the need to protect their families and themselves. The need to protect their patients was cited by slightly more than half of HCP who intended to get vaccinated, which also indicates gaps in knowledge and potentially gaps in the establishment and promotion of a safety culture in healthcare facilities. Nevertheless, although reasons for vaccine hesitancy are critical to understand in order to design more effective vaccine communications campaigns, those campaigns can also helpfully build on reasons why HCP do intend to get vaccinated.
Our study has several strengths. First, the survey was conducted in eight tertiary-care hospitals in Greece, which gave us the opportunity to study a large number of HCP of various professions and backgrounds. Second, reasons not only for intending to decline a COVID-19 vaccine but also for intending to receive one were studied. The fact that we did not follow the HCP in order to record their practices about COVID-19 vaccine in real-life is a potential weakness. However, their past attitudes towards occupational vaccinations were studied and were in the same line with their intentions for COVID-19 vaccination. It should be noted that the numbers of HCP who answered the questions about their hepatitis B and measles vaccine history were much lower than the number of HCP who answered the basic question about their intention to get a COVID-19 vaccine. The relatively low participation rate of HCP is an additional limitation. Another potential limitation is that the study was conducted in September and October before the peak of the second epidemic wave in Greece. It is possible and the high COVID-19-associated morbidity and mortality faced in our healthcare system during the second epidemic wave will have an additional impact on acceptance of vaccines. Lastly, at that time information about specific vaccines was rather preliminary, which may account for the gap in information reported by several HCP.
In conclusion, only half of HCP in our study intended to get vaccinated against COVID-19. Main barriers for reporting intention to decline vaccination were gaps in information and concerns about vaccine safety. Evidence-based educational interventions should be implemented to built safety perception towards COVID-19 vaccines among HCP, in order to raise vaccine uptake rates and thus to protect them and the essential healthcare services during the pandemic.
Ethics
The study was approved from the Ethics Committees of the participating hospitals (approval numbers: Φ076/ΑΔ.2159/Σ.767, 28405/1-9-20, EΣ12/Θ2/17-9-20, 2098/15-9-20, 100/16/13/19-8-20).
Authorship statement
HCM and MT conceived the study. HCM, XD, CL and NVS designed the study. HCM and NVS supervised the study. ID, EB, GA, AS, EL, MNG, DK, NM and VP acquired the data, critically reviewed and approved the submitted manuscript. VR analyzed the data. HCM wrote the original draft. All authors interpreted the data, provided critical review and approved the final manuscript.
Conflict of interest
All authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Provenance and peer review
Not commissioned; externally peer reviewed.
Acknowledgements
We are thankful to Infection Control Committees of participating hospitals. We also thank Anastasia Tedoma and Panagiota Isari for technical assistance. The opinions presented in this article are those of the authors, and do not necessarily represent those of their institutions.
References
- 1.Verelst F., Kuylen E., Beutels P. Indications for healthcare surge capacity in European countries facing an exponential increase in coronavirus disease (COVID-19) cases, March 2020. Euro Surveill. 2020;25:2000323. doi: 10.2807/1560-7917.ES.2020.25.13.2000323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maltezou H.C., Dedoukou X., Tsonou P., Tseroni M., Raftopoulos V., Pavli A. Hospital factors associated with SARS-CoV-2 infection among healthcare personnel in Greece. J Hosp Infect. 2021;109:40–43. doi: 10.1016/j.jhin.2020.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heinzerling A., Stuckey M.J., Scheuer T., Xu K., Perkins K.M., Resseger H. Transmission of COVID-19 to health care personnel during exposures to a hospitalized patient – Solano County, California, February 2020. MMWR Morb Mortal Wkly Rep. 2020;69:472–476. doi: 10.15585/mmwr.mm6915e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.CDC COVID-19 response team Characteristics of health care personnel with COVID-19—United States, February 12-April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:477–481. doi: 10.15585/mmwr.mm6915e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilson N.M., Norton A., Young F.P., Collins D.W. Airborne transmission of severe acute respiratory syndrome coronavirus-2 to healthcare workers: a narrative review. Anaesthesia. 2020;75:1086–1095. doi: 10.1111/anae.15093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gostin L.O., Salmon D.A. The dual epidemics of COVID-19 and influenza: vaccine acceptance, coverage, and mandates. J Am Med Assoc. 2020;324:335–336. doi: 10.1001/jama.2020.10802. [DOI] [PubMed] [Google Scholar]
- 7.Maltezou H.C., Dedoukou X., Tseroni M., Tsonou P., Raftopoulos V., Papadima K. SARS-CoV-2 infection in healthcare personnel with high-risk occupational exposure: evaluation of 7-day exclusion from work policy. Clin Infect Dis. 2020;71:3182–3187. doi: 10.1093/cid/ciaa888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization Maintaining essential health services during the COVID-19 outbreak. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/related-health-issues [DOI] [PMC free article] [PubMed]
- 9.World Health Organization . November 2020. World Health Organization Strategic Advisory Group of Experts on Immunization roadmap for prioritizing uses of COVID-19 vaccines in the context of limited supply.https://www.who.int/docs/default-source/immunization/sage/covid/sage-prioritization-roadmap-covid19-vaccines.pdf?Status=Temp&sfvrsn=bf227443_2 Version 1.1 13. [Google Scholar]
- 10.Centers for Disease Control and Prevention COVID-19 vaccine prioritization: work Group considerations. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-08/COVID-08-Dooling.pdf
- 11.Wang K., Wong E.L.Y., Ho K.F., Cheung A.W.L., Chan E.Y.Y., Yeoh E.K. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: a cross-sectional survey. Vaccine. 2020;38:7049–7056. doi: 10.1016/j.vaccine.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kabamba Nzaji M., Kabamba Ngombe L., Ngoie Mwamba G., Banza Ndala D.B., Mbidi Miema J., Luhata Lungoyo C. Acceptability of vaccination against COVID-19 among healthcare workers in the Democratic Republic of the Congo. Pragmatic Observational Res. 2020;11:103–109. doi: 10.2147/POR.S271096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Detoc M., Bruel S., Frappe P., Tardy B., Botelho-Nevers E., Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38:7002–7006. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maltezou H.C., Theodora M., Lytras T., Fotiou A., Nino E., Rodolakis A. Knowledge, attitudes and practices about vaccine-preventable diseases and vaccinations of children among pregnant women in Greece. Vaccine. 2020;38:7654–7658. doi: 10.1016/j.vaccine.2020.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Danchin M., Biezen R., Manski-Nankervis J.A., Kaufman J., Leask J. Preparing the public for COVID-19 vaccines: how can general practitioners build vaccine confidence and optimise uptake for themselves and their patients? Aust J Gen Pract. 2020;49:625–629. doi: 10.31128/AJGP-08-20-5559. [DOI] [PubMed] [Google Scholar]
- 16.Earnshaw V.A., Eaton L.A., Kalichman S.C., Brousseau N.M., Carly Hill E., Fox A.B. COVID-19 conspiracy beliefs, health behaviors, and policy support. Transl Behav Med. 2020;10:850–856. doi: 10.1093/tbm/ibaa090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schaffer DeRoo S., Pudalov N.J., Fu L.Y. Planning for a COVID-19 vaccination program. J Am Med Assoc. 2020;323:2458–2459. doi: 10.1001/jama.2020.8711. [DOI] [PubMed] [Google Scholar]
- 18.Dedoukou X., Nikolopoulos G., Maragos A., Giannoulidou S., Maltezou H.C. Attitudes towards vaccination against seasonal influenza of healthcare workers in primary healthcare settings in Greece. Vaccine. 2010;28:5931–5933. doi: 10.1016/j.vaccine.2010.06.108. [DOI] [PubMed] [Google Scholar]
- 19.Maltezou H.C., Dedoukou X., Patrinos S., Maragos A., Poufta S., Gargalianos P. Determinants of intention to get vaccinated against novel (pandemic) influenza A H1N1 among healthcare workers in a nationwide survey. J Infect. 2010;61:252–258. doi: 10.1016/j.jinf.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 20.Dror A.A., Eisenbach N., Taiber S., Morozov N.G., Mizrachi M., Zigron A. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35:775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meyer M.N., Gjorgjieva T., Rosica D. Trends in health care worker intentions to receive a COVID-19 vaccine and reasons for hesitancy. JAMA Netw Open. 2021;4:e215344. doi: 10.1001/jamanetworkopen.2021.5344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baumgaertner B., Ridenhour B.J., Justwan F., Carlisle J.E., Miller C.R. Risk of disease and willingness to vaccinated in the United States: a population-based survey. PLoS Med. 2020;17 doi: 10.1371/journal.pmed.1003354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gagneux-Brunon A., Detoc M., Bruel S., Tardy B., Rozaire O., Frappe P. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross sectional survey. J Hosp Infect. 2021;108:168–173. doi: 10.1016/j.jhin.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gadoth A., Halbrook M., Martin-Blais R., Gray A., Tobin N.H., Ferbas K.G. Assement of COVID-19 vaccine acceptance among healthcare workers in Los Angeles. Medrxiv. 2020 doi: 10.7326/M20-7580. https://www.medrxiv.org/content/10.1101/2020.11.18.20234468v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maltezou H.C. Nosocomial influenza: new concepts and practice. Curr Opin Infect Dis. 2008;21:337–343. doi: 10.1097/QCO.0b013e3283013945. [DOI] [PubMed] [Google Scholar]
- 26.Maltezou H.C., Gargalianos P., Nikolaidis P., Katerelos P., Tedoma N., Maltezos E. Attitudes towards mandatory vaccination and vaccination coverage against vaccine preventable diseases among health-care workers in tertiary-care hospitals. J Infect. 2012;64:319–324. doi: 10.1016/j.jinf.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 27.Maltezou H.C., Lourida A., Katragkou A., Grivea I.N., Katerelos P., Wicker S. Attitudes regarding occupational vaccines and vaccination coverage against vaccine-preventable diseases among healthcare workers working in pediatric departments in Greece. Pediatr Infect Dis J. 2012;31:623–625. doi: 10.1097/INF.0b013e31824ddc1e. [DOI] [PubMed] [Google Scholar]
- 28.Maltezou H.C., Poland G.A. Immunization of health-care providers: necessity and public health policies. Healthcare. 2016;4:47. doi: 10.3390/healthcare4030047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ledda C., Costantino C., Cuccia M., Maltezou H.C., Rapisarda V. Attitudes of healthcare personnel towards vaccinations before and during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18:2703. doi: 10.3390/ijerph18052703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Largent E.A., Persad G., Sangenito S., Glickman A., Boyle C., Emanuel E.J. US public attitudes toward COVID-19 vaccine mandtes. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.33324. [DOI] [PMC free article] [PubMed] [Google Scholar]