Abstract
The global pandemic caused by the 2019 coronavirus (COVID-19) has led to a dramatic increase in medical waste worldwide. This tremendous increase in medical waste is an important transmission medium for the virus and thus poses new and serious challenges to urban medical waste management. This study investigates the response of medical waste management to the COVID-19 pandemic and subsequent changes in Wuhan City based on the most detailed data available, including waste generation, storage, transportation, and disposal. The results show that despite a 5-fold increase in the demand for daily medical waste disposal in the peak period, the quick responses in the storage, transportation, and disposal sectors during the pandemic ensured that all medical waste was disposed of within 24 hours of generation. Furthermore, this paper discusses medical waste management during future emergencies in Wuhan. The ability of the medical waste management system in Wuhan to successfully cope with the rapid increase in medical waste caused by major public health emergencies has important implications for other cities suffering from the pandemic and demonstrates the need to establish resilient medical emergency systems in urban areas.
Keywords: COVID-19, Medical waste, Public health, Emergency management, Health risk
1. Introduction
The incidence of Coronavirus 2019 (COVID-19) increased to the level of a global pandemic in early 2020, with more than 103 million confirmed cases worldwide by February 1st, 2021 (World Health Organization, 2021). The COVID-19 pandemic has changed the social activities, production, consumption, and travel patterns of most people and thus had a significant influence on pollution discharge and environmental quality (Klemeš et al., 2020). The medical waste management experience of Wuhan, in the context of the COVID-19 pandemic, can be featured as a valuable example of an emergency response that can inform cities worldwide regarding environmental policy-making occurring simultaneously with pandemic control and other urgent environmental stressors. Hence, it is particularly significant to study the impact of the COVID-19 pandemic on medical waste and countermeasures.
Researchers have found that the COVID-19 pandemic has had a significant and immediate impact on the environment. The majority of studies mainly explored atmospheric environmental changes during the pandemic. The pandemic has led to production shutdowns and significant decreases in travel, thus significantly influencing pollution emissions and air quality (Le et al., 2020; Han et al., 2020; Wang et al., 2020; He et al., 2021; Shen et al., 2021; Wang et al., 2021). For example, Liu et al. estimated that global CO2 emissions (1,551 metric tons) sharply decreased by 9% in the first half of 2020 compared with those in the same period of 2019 (Liu et al., 2020). Lv et al. found that the increase in secondary aerosols in China offset the benefit of the reduction in NOx and VOC emissions on air quality (Lv et al., 2020). Other studies explored the health benefits of the improvement in air quality during the COVID-19 pandemic (Alsayedahmed, 2020; Anderson et al., 2020; Markandeya et al., 2020; Giani et al., 2020).
As the COVID-19 pandemic continues, solid waste is attracting the attention of researchers. The pandemic has profoundly changed travel and hygiene behaviors (Tripathi et al., 2020), and more people are choosing to use single-use plastic cutlery (Vanapalli et al., 2021). The inability of existing waste management systems to effectively deal with plastics has made them a serious threat to natural ecosystems and human health, prompting much discussion about medical waste disposal systems (Patrício Silva et al., 2020). For example, Ikiz et al. revealed that the pandemic has led to an increase in personal protective equipment garbage and a decrease in waste diversion and recycling activities. Silva et al. believe that the incineration and landfilling of plastic waste were prioritized over recycling during the pandemic, which will result in the emission of toxic and harmful gases in the medium to long term (Patrício Silva et al., 2021). Increasing solid waste may pose a public health problem. Specifically, medical waste may become a new source of infection, as the global demand for personal protective equipment led to a drastic increase in global medical waste. It is estimated that 129 billion masks and 65 billion gloves are used globally each month (Prata et al., 2020). According to the Ministry of Industry and Information Technology, China produced 116 million disposable masks every day in February, which represents a 12-fold increase compared to production levels before the COVID-19 pandemic (Ministry of Industry and Information Technology of the People s Republic of China, 2020). There is no doubt that most of the personal protection equipment will eventually become medical waste. Some studies have shown that the COVID-19 virus can survive on various surfaces for as long as nine days (Kampf et al., 2020; van Doremalen et al., 2020). In some developing countries, such as India and South Africa, waste is left in commonly used open dumps, making it a potential source of infection for individuals who pick through the waste without proper medical protection (People's Archive of Rural India, 2020; Thomson Reuters Foundation News, 2020; Tripathi et al., 2020). Therefore, contaminated medical waste can be a highly risky virus reservoir that threatens public health if it is not properly disposed of and sustainably managed (Adyel, 2020; Borrelle et al., 2020). To the best of our knowledge, existing studies have focused only on the challenges of medical waste disposal during the COVID-19 pandemic and solutions. For example, Jackson et al. investigated waste management compliance in health care facilities at the hospital level and found that the level of waste management compliance among health workers was 43% (Powell-Jackson et al., 2020). Singh et al. suggested that medical waste would increase dramatically due to the COVID-19 pandemic. Safe and sustainable waste management is critical for controlling transmission of the virus (Singh et al., 2020a; Singh et al., 2020b). Yang et al. discussed the medical waste disposal measures employed in Wuhan and analyzed the benefits and drawbacks of different measures, suggesting that stationary facilities and municipal incinerators were preferred for medical waste disposal (Yang et al., 2021). Sharma et al. argued that the crisis caused by the COVID-19 pandemic has altered the dynamics of global waste production, and unexpected fluctuations in waste composition and quantities require a dynamic response from policymakers to address gaps in the system (Mohammad et al., 2021; Neumeyer et al., 2020; Sharma et al., 2020). Previous research has primarily targeted the technologies and strategies employed for medical waste disposal during pandemics, but there has been little research on medical waste disposal during major public health emergencies and the impact of pandemics on medical waste management systems due to the lack of data. Nevertheless, unexpected increases in medical waste during emergencies will make it challenging to contain the spread of the virus and increase the challenges faced by waste management systems. Therefore, the safe and efficient disposal of medical waste during public health emergencies and continuous attention to the improvement of medical waste management are extremely important for safeguarding people's health and life (Asari et al., 2013; Brown et al., 2011).
In China, medical waste disposal is a regional environmental issue that should be addressed by local authorities (usually city administrations). The COVID-19 pandemic has created serious challenges for local authorities in terms of waste management (Prem et al., 2020; Zhang et al., 2020). Fortunately, Wuhan seems to have successfully addressed this problem (Lau et al., 2020). During the COVID-19 pandemic, medical waste treatment capacity has increased over time to ensure that medical waste was disposed of within 24 hours of generation. Hence, analyzing the response of medical waste disposal to COVID-19 in Wuhan has important management implications for reducing the risk of cross-infection during future health emergencies and for other cities worldwide that are suffering from COVID-19. Therefore, we collected detailed data on the generation, transportation, and disposal of medical waste at the hospital level in Wuhan during the COVID-19 pandemic. Then, the performance of each waste management process was analyzed. To the best of our knowledge, this is the most detailed and most recent study of medical waste management during the pandemic to date.
2. Data and methods
2.1. Study area
The study area is Wuhan, which is the capital of Hubei Province and an industrial, scientific and educational base and transportation center in central China. By 2019, the resident population was 11.21 million, with a land area of 8,569 km2 (The government of Wuhan, 2019a). Wuhan has 6,497 medical institutions with 99,400 beds, with 7.56 hospital beds, 117,100 health workers, and 3.83 doctors per 1,000 people (The government of Wuhan, 2019b). Before the COVID-19 pandemic, Wuhan had only one large stationary medical waste disposal facility, with a designed capacity of 50 tonnes/day for medical waste incineration. The definition of medical waste has been expanded during the COVID-19 pandemic based on careful consideration that all waste might carry the live virus (Nzediegwu and Chang, 2020). All waste that had contact with healthcare personnel, patients, and related workers during the pandemic, including but not limited to disposable tableware, toiletries, and food leftovers, was also classified as medical waste (You et al., 2020). As a result, medical waste dramatically increased because of both the expansion of the definition and the increasing number of hospitalized patients and isolated close contacts.
2.2. Methods
-
(1)
Assessing the performance of medical waste storage
The dramatic increase in medical waste production during the COVID-19 pandemic has made the timely disposal of medical waste very difficult, and some medical waste has had to be stored in temporary sites designated by medical institutions. Due to the limited space of these institutions and fluctuations in medical waste production, some institutions may have insufficient storage space, and thus, medical waste has to be placed in nondesignated locations, which may pose a risk in terms of the spread of the virus. There is considered to be a storage space shortage when the required storage space exceeds the actual storage area provided by a medical institution. The formula for calculating the floor space used for the storage of medical waste is as follows:
where represents the required storage space for medical waste at date in medical institution (m2); represents the storage space of a single medical waste bin (measured in m2); represents the number of medical waste bins in use at date j in medical institution ; denotes the storage performance (storage space shortage) at date for medical institution (SR > 1: the storage area required for medical waste exceeds the institution's capacity and medical waste storage is insufficient; SR < 1: the institution has sufficient storage space); represents the percentage of storage space shortage days to the studied days in region (%); represents the sum of the number of days that all medical institutions in region with storage space shortage (day); stands for the total number of days in the study period (day); and represents the number of medical institutions in region .
-
(1)
Assessing the performance of medical waste transportation
The performance of waste transportation was estimated based on the measured shortest route for medical waste vehicles and the accident rate for Chinese freight vehicles, as shown by the following formulas:
where is medical waste turnover (the total volume of freight transported within a period) at date (kmt); represents the total medical waste at date (tonnes); stands for the average transportation distance (average round trip distance of a single medical waste transport) of medical waste on date (km); represents the total medical waste transportation distance on date (km); and is the frequency of medical waste transportation (number of round trips for transporting medical waste) on date (time).
2.3. Data sources
The dataset was derived from public statistics and survey data. Public statistics were collected from reports published by the National Health Commission of the People's Republic of China, Health Commission of Hubei Province, and Wuhan Municipal Health Commission, including the number of current confirmed cases and medical beds. Data on the capacity and quantity of medical waste disposal in Wuhan were collected from reports published by the Ministry of Ecology and Environment of the People's Republic of China, Department of Ecology and Environmental of Hubei Province, and Wuhan Ecological Environment Bureau. The plan to upgrade the medical management system in Wuhan due to the COVID-19 pandemic (May 2020 to today) was obtained from reports published by the Hubei Provincial Government and Wuhan Government. The survey data mainly include information obtained from daily reports on medical waste disposal in Wuhan (production mass, disposal capacity, disposal mass, etc.), detailed medical dispatch plans (storage space, transportation distance, etc.), and statistics on medical waste disposal in Wuhan in 2019; all these data were obtained from the Hubei Solid Waste and Chemical Pollution Prevention Center and Hubei Academy of Ecology and Environmental Sciences.
The data span from January 22nd (Wuhan lockdown) to April 26th (zero current confirmed cases in Wuhan). However, some data were missing due to the lockdown of the city during the pandemic.
3. Results and discussion
3.1. Overview of medical waste during the pandemic
To prevent COVID-19 transmission, Wuhan was locked down for 76 days from January 23rd, 2020, until April 8th, 2020. To mitigate the shortage of medical beds during the COVID-19 pandemic, in addition to the 24,378 beds (by February 25th) that were available at designated medical institutions, Wuhan also received patients from February 3rd to February 22nd at newly constructed mobile cabin hospitals (and expropriated gymnasiums). Furthermore, some schools were expropriated as isolation areas for potential patients. The increase in hospitalizations led to an increase in medical waste. The total mass of disposed medical waste in Wuhan reached 10,475 tonnes during these 76 days, with a daily maximum of 263 tonnes. In contrast, in 2019, the medical waste generated in Wuhan was approximately 19,531 tonnes, with an average daily disposal demand of approximately 55 tonnes. The rapid increase in medical waste in such a short time far exceeded the original disposal capacity that in the most difficult time, led to a shortage in the medical waste disposal capacity of more than 60 tonnes.
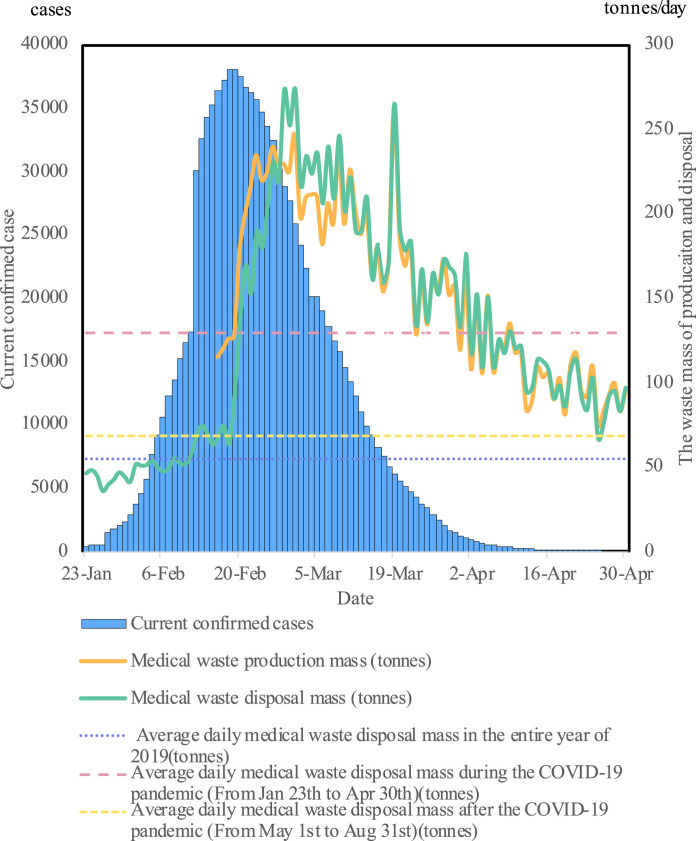
As shown in Fig. 1 , the number of current confirmed COVID-19 cases peaked from the middle to the end of February and then gradually tapered off. However, the data analysis indicated that the peak of medical waste production showed a lag and occurred between late February and early March. This information is presented in the supplemental materials. Before late February, the disposal capacity was unable to meet the demand for timely medical waste disposal, resulting in a serious backlog of medical waste. After late February, the medical waste disposal capacity was increased to 224 tonnes per day to ensure the disposal of daily produced medical waste in a timely manner, and the previous medical waste backlog was addressed. However, after the end of the Wuhan lockdown on April 8th, medical waste production remained at a high level until May. The level at this time was 30% higher than the average daily production (55 tonnes) before the COVID-19 pandemic due to cautious preventative measures (Xiao and Torok, 2020), such as additional testing in medical institutions and communities. Since May 2020, Wuhan has gradually loosened its emergency restrictions, and people have fully resumed their production activities and normal lives. The daily average medical waste generation from May to August 2020 was approximately 69.1 tonnes/day, which is approximately one-half the mass during the pandemic but still 26% higher than that in 2019 due to increased COVID-19 testing and precautions that took place after the pandemic began.
Fig. 1.
Overview of medical waste production and disposal during the COVID-19 pandemic.
3.2. Medical waste production
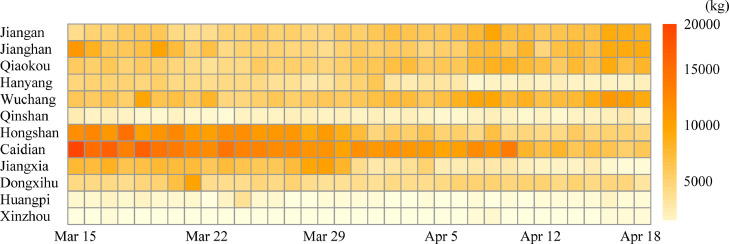
Medical waste production can indicate the pressure of medical waste disposal and changing trends of the pandemic (Windfeld and Brooks, 2015). Fig. 2 presents the production of medical waste from March 15th to April 18th in selected administrative districts of Wuhan City. The trends of medical waste production on other days could not be presented at the district or hospital level due to the lack of data. Generally, the waste production in each district declined with the mitigation of the pandemic. Caidian and Jiangxia generated more medical waste than other districts in March because their two primary mobile cabin hospitals, namely, Huoshenshan Hospital and Leishenshan Hospital, were quickly established and received 5050 patients (more than 10% of the total number of confirmed cases in Wuhan during the COVID-19 pandemic) in response to the rapid increase in the number of patients in the city (Zhu et al., 2020). Remote districts with a low population density and fewer medical institutions, such as Xinzhou and Huangpi, produced a smaller proportion of medical waste.
Fig. 2.
Medical waste production in the districts of Wuhan.
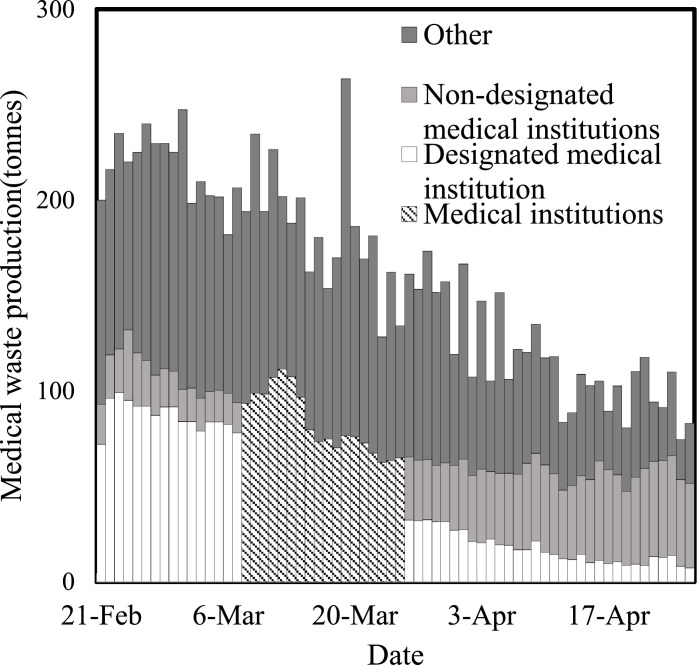
Fig. 3 presents the sources of medical waste. The source of waste was not distinguished between designated and non-designated medical institutions from March 8th to March 25th due to the lack of data; ‘Other’ refers to medical waste from nonmedical sources, such as domestic waste produced by medical personnel. As the number of COVID-19 cases decreased, the medical waste produced by designated medical institutions (mostly hospitals with well-developed and extensive medical facilities) gradually decreased, and that produced by other sources also decreased. During the later stages of the pandemic, the medical waste produced by designated medical institutions declined, while that produced by non-designated institutions quickly increased because the latter began to provide more medical services to non-COVID-19 patients, resulting in a larger proportion of the medical waste generated by non-designated medical institutions (Nagano et al., 2020).
Fig. 3.
Daily total medical waste mass generated from different sources. Designated medical institutions: Medical institutions that focused on the treatment of COVID-19 patients during the pandemic. Non-designated medical institutions: Medical institutions that had limited resources and were not able to receive and treat COVID-19 patients during the pandemic.
3.3. Performance of medical waste storage
Medical waste storage management in Wuhan went through two phases during the COVID-19 pandemic: the first phase (from Jan 22nd to Mar 1st), in which daily waste disposal was less than daily production and medical waste had to be stored in temporary storage sites and the second phase (from March 2nd to April 19th), in which Wuhan eliminated its medical waste backlog and stopped the use of local temporary storage, during which medical waste was stored in designated areas of the medical institutions and disposed of within 24 hours of production. In the first phase, 16 large regional storage sites were established in Wuhan, with a total storage capacity of 1,066.6 tonnes and an area of 13,610 m2. According to the data from February 21st to March 1st, the regional temporary medical waste storage sites had ample space, and the utilization rate was only 34% at the maximum and lower than 20% most of the time.
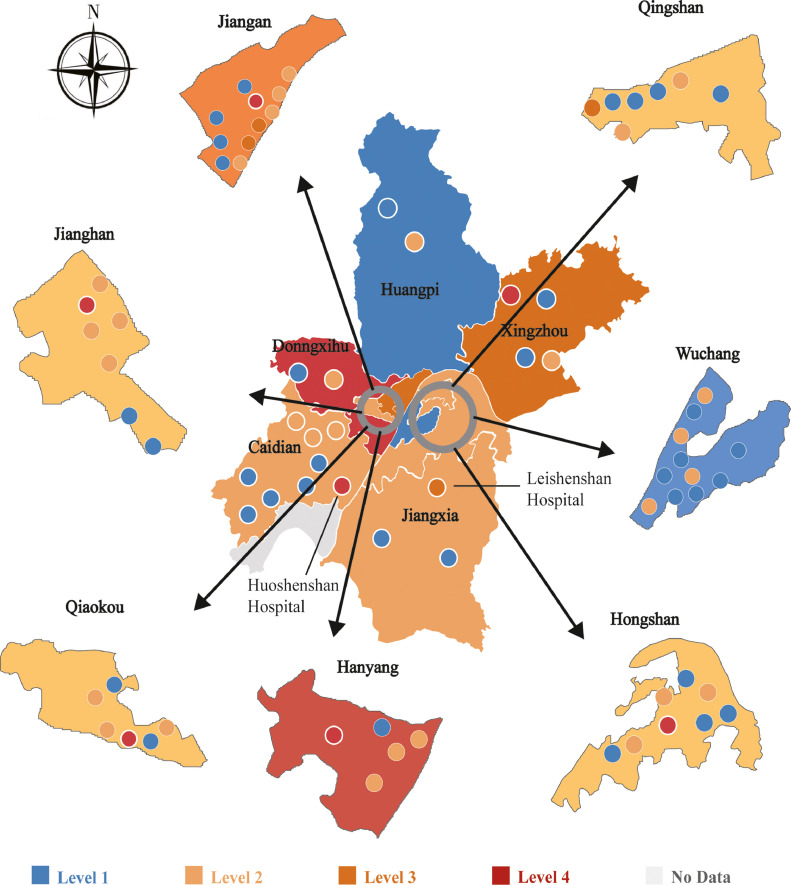
However, the storage capacity of some medical institutions is not adequate during the pandemic. We analyzed the storage space shortage of 78 major medical institutions in Wuhan in the late period of the second phase to evaluate the performance of Wuhan's medical waste management. Fig. 4 presents the performance of medical waste storage for major medical institutions from March 16th to April 19th. District levels were assigned based on the number of days that a storage space shortage existed in the medical institutions. Overall, the performance of medical waste storage varied in each district. Dongxihu was the district with the most serious storage space shortage. Its storage space demand exceeded the actual storage space on 33% of the studied days. This storage space shortage could be primarily attributed to the fact that the largest infectious disease hospital and medical treatment center in Wuhan, which is located in this district, had a high medical load during the pandemic and provided most of its space to patients as wards. The Hanyang district has a shortage of medical waste storage space on 30% of the studied days, which was primarily due to insufficient storage space for medical waste in some small non-designated hospitals in this district. Usually, small non-designated hospitals are designed to divert patients with minor illnesses, such as colds and minor trauma, from larger hospitals. Therefore, the infrastructure of these hospitals is obviously weaker than that of large designated general hospitals (Chen et al., 2020). During the pandemic, these small non-designated hospitals provided far more medical care than usual. Other districts generally had a relatively lower degree of storage space shortage, with insufficient storage space on 2% to 26% of the studied days, respectively.
Fig. 4.
Medical waste storage space shortage of different districts and hospitals. Levels 1, 2, 3, and 4 indicate the proportion of days with a medical waste storage space shortage compared to the studied days. Dots denote hospitals.
We further conducted a hospital-level analysis to investigate the performance of medical waste storage. Generally, the hospitals carried different levels of storage space shortage, and their waste storage capacity was lower than the mass of waste produced. The hospitals with the highest storage space shortage needed more than four times the available storage space. The total storage space of the hospitals was 3,755 m2, which far exceeded the daily storage demand (2,124 m2). In summary, the percentage of days with storage space shortage was lower than 17% on average in all hospitals. Due to the uneven distribution of medical waste storage facilities, some hospitals did not have sufficient space and others had excess space. In Wuhan, the hospitals with a storage space shortage on more days were mostly mobile cabin hospitals, specialty hospitals, and small non-designated hospitals.
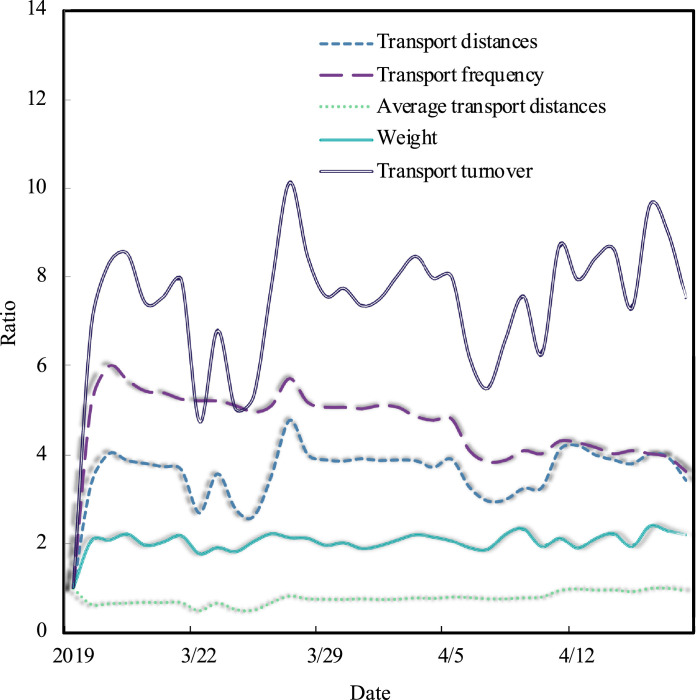
3.4. Performance of medical waste transportation
The COVID-19 pandemic led to extremely sharp increases in medical waste production in Wuhan, leading to a substantial increase in the demand for medical waste transportation. Before March 16th, the transportation of medical waste in Wuhan was in an emergency mode. After March 16th, Wuhan employed a comprehensive scheduling process for medical waste transportation that clarified the destination of medical waste for each hospital and arranged dedicated vehicles for transporting medical waste. Due to data availability, we focused only on the period of scheduled transportation, which may better indicate how well the transport turnover of medical waste can be controlled.
The average daily data in 2019 was used as a benchmark for comparison (i.e., the value of 1 for 2019). The transportation turnover in this period was approximately 5-10 times that on regular days in 2019. Fig. 5 shows that the average transportation distance was even shorter than that of 2019. However, the transportation frequency increased 4-6-fold. The primary reason for the decrease in distance and increase in frequency was that four disposal sites were newly established during the pandemic. The increase in the number of sites (or options) allowed Wuhan to better plan the transportation routes, which greatly shortened the one-way transportation distance and increased the frequency. In contrast, the average weight remained relatively stable and high and was approximately twice that in 2019. These temporary disposal sites were shut down around the first week of April due to the decrease in medical waste production; thus, the average transportation distance per trip gradually increased to levels in 2019.
Fig. 5.
Ratio of medical waste transportation statistics during the pandemic to the average value of 2019. Transport distance: total distance of medical waste transported for the day (km); Average transport distance: average round trip distance for one-way medical waste transportation (km); Transport frequency: frequency of medical waste transportation for the day (times); Weight: total weight of medical waste transportation for the day (tonnes).
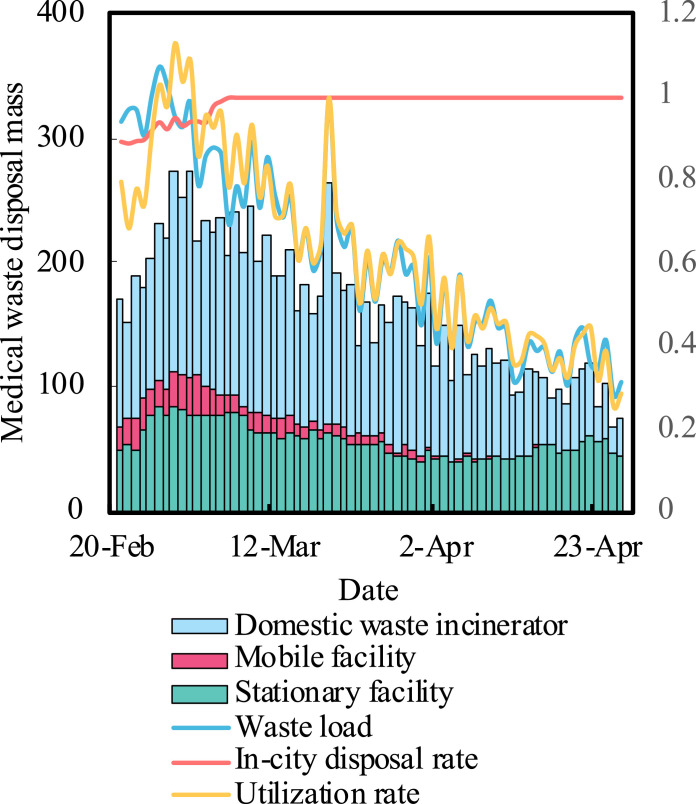
3.5. Performance of medical waste disposal
Despite the lack of medical waste disposal capacity at the initial stage of the COVID-19 pandemic, Wuhan employed three emergency measures in response to the rapid spread of COVID-19: the use of mobile disposal facilities, the expropriation of municipal waste incinerators, and the implementation of off-site disposal. Fig. 6 presents the methods used for various medical waste disposal from February 21st to April 19th, 2020. Stationary facilities were the main method used for the traditional disposal of medical waste, mobile facilities supported traditional medical waste disposal, and municipal waste incinerators were temporarily used for pandemic-related waste. The use of mobile facilities for disposal gradually decreased and was terminated at the end of March. The curve of the waste load, as shown in Fig. 6, indicates that the daily disposal demand of medical waste could generally be met by the stationary facilities and expropriated municipal waste incinerators. After an exceptional increase (the daily medical waste production increased from 127 tonnes on February 19th to 178 tonnes on February 20th and then increased steadily to 240 tonnes on February 26th due to the increase in current confirmed cases from 17,361 to 30,043 on February 12th; this number remained higher than 30,000 until February 27th) in medical waste production, the increase in medical waste disposal capacity did not keep pace with the increase in demand (the weekly increase in the medical waste disposal capacity during this period was approximately 20 tonnes), which may have increased the risk of transmission.
Fig. 6.
Treatment proportion of the different methods. Waste load: the ratio of medical waste production to the disposal capacity; in-city disposal rate: the ratio of medical waste disposed in Wuhan City to the total disposed medical waste; utilization rate: the ratio of the actual mass of medical waste disposed of to the total disposal capacity.
Because the situation and disposal capacity improved, Wuhan halted the off-site disposal of medical waste, and the in-city disposal rate of medical waste (the proportion of medical waste treated in Wuhan) increased to 100% after March 5th and remained at this level. Overall, Wuhan's medical waste disposal system was overloaded (utilization rate higher than 100%) only at the end of February, and with the help of acquisitions, donations, and support, the medical waste disposal capacity of Wuhan increased from the initial 50 tonnes/day to 265.6 tonnes/day on March 11th, 2020. However, during the period from February 21st to April 1st, the expropriated municipal waste incinerators were overloaded for approximately 75% of the period, with the highest overload rate reaching 94%.
3.6. Current changes in medical waste management
The unexpected pandemic made administrators aware of the shortcomings of medical waste management. Therefore, after the overall situation returned to normal, Wuhan improved its medical waste management system in three ways: increasing disposal capacity, employing smart management, and instituting policy regulations. The details are shown in Table 1 .
Table 1.
Current changes made in medical waste management.
| Before pandemic | After the cancellation of Wuhan's emergency |
|---|---|
| Disposal capacity: 50 tonnes/day | Disposal capacity up to 110 tonnes/day Hazardous waste treatment facilities project an annual treatment capacity of 50,000 tonnes at the design stage (cnhubei.com, 2020). |
| Fixed medical waste bins in hospital with manual operation and no monitoring | Smart portable waste treatment devices automatic operation and dynamic monitoring |
| No local regulations for medical waste | Waste discharge regulation for local medical waste was implemented, and a new regulation on comprehensive medical waste management is being considered. |
The pandemic has led to a significant increase in Wuhan's medical waste disposal and emergency response capabilities. After the pandemic, the increase in the medical waste disposal capacity was 60 tonnes/day, but the emergency disposal capacity was 30 tonnes/day. Furthermore, Wuhan had 180 tonnes/day of back-up emergency disposal capacity (including 80 tonnes/day of hazardous waste incineration disposal capacity and 100 tonnes/day of municipal waste incineration disposal capacity). In addition, Wuhan is planning a large project to meet possible future waste disposal demands, with a maximum treatment capacity of 50,000 tonnes per year (HubeiDaily, 2020b). At the hospital level, for more effective medical waste management, smart medical waste transfer vehicles are being used to automatically collect and transfer medical waste from hospitals, which could reduce the operator's contact with medical waste, thereby reducing the related risks (People.cn, 2020). A smart software system has been established to promote dynamic medical waste monitoring and transfer scheduling. A warning will be sent by the system to the waste management department that a transfer is required, thus reducing the risk. Furthermore, the legislative process has been largely accelerated to facilitate the implementation of medical waste treatment projects due to the implementation of simplified procedures and provide tax incentives and other policies to support waste disposal enterprises (HubeiDaily, 2020a). Specifically, regulation involving a waste charge was recently implemented using this new rapid process to delineate the responsibilities of stakeholders for medical waste treatment (The government of Wuhan, 2020).
4. Conclusion and additional policy implications
COVID-19 has posed a great challenge for Wuhan's medical waste disposal system. During peak periods, the demand for daily disposal was more than five times the normal daily demand. Large designated medical institutions had relatively more sufficient storage space for medical waste and thus a lower storage space shortage. Mobile cabin hospitals, small non-designated hospitals, and non-general hospitals need to simultaneously expand their storage space to reduce the storage space shortage. An increase in the production of medical waste and the need for more time-sensitive disposal will increase the transport turnover. Even with a dramatic decrease in patients, the transport turnover is still 5-10 times higher than that on regular days. Fortunately, Wuhan's quick response helped it address the lack of medical waste disposal capacity during the COVID-19 pandemic, which greatly reduced the possibility of virus transmission by medical waste through the use of mobile facilities and the expropriation of municipal waste incinerators (Tabish et al., 2020). The pandemic has been a powerful warning to Wuhan, which improved its medical waste treatment capacity and management after the city returned to normalcy.
The successful experiences of Wuhan suggest that improving the emergency management system for medical waste from multiple aspects is vital for minimizing human health risks. Our findings outline the experiences of medical waste management in Wuhan as it responded to the public health emergency, which provides guidance for new policy implications and decision-making for future waste management processes and other cities around the world that are suffering from the pandemic in terms of medical waste disposal and seek to address the public health risk (Tabish et al., 2020).
-
(1)
A sophisticated medical data system should be implemented. At the beginning of the pandemic, medical waste storage, transportation, and disposal processes were hastily implemented due to the unexpected increase in medical waste. Due to the gradual improvement in medical waste data, Wuhan started to develop a medical waste management plan and began to effectively allocate resources to improve the medical waste management system. The availability of medical data can support the visualization of different scenarios and prediction of waste generation trends, thus guiding medical waste management and promptly increasing the capacity and resilience of urban medical treatment in response to major public emergencies.
-
(2)
The medical waste storage capacity of hospitals needs to be improved to deal with dramatic increases in medical waste during emergencies (Alshraideh and Abu Qdais, 2017). Based on the average data before the COVID-19 pandemic and daily production, five times the available space is needed. Some upgrading activities should be implemented that involve mobile cabin hospitals, specialist hospitals, and urban nonpublic hospitals, which have relatively little space, to at a minimum, establish temporary storage areas for medical waste. In addition, temporary bins should be used during emergencies. Based on Wuhan's experiences during the COVID-19 pandemic, 0.58 bins (for detailed information, please refer to the supplementary materials) and 0.25 m2 of storage space are recommended for each hospital bed.
-
(3)
Emergency plans should be developed to coordinate resources for disposal capacity throughout the broader region. Upon the outbreak of a medical emergency, medical waste can be transferred to disposal sites in neighboring cities as soon as possible to achieve joint prevention and control. Therefore, coordinating the infrastructure at the regional level should be emphasized during major public emergencies. The administration needs to estimate the spatial distribution pattern of medical waste production, identify storage needs, establish a regional dispatching center, address the shortage of storage space in small hospitals and increase this space in large hospitals, and establish a plan so that storage space can be shared within the region. Moreover, to prepare for future emergencies, the capacity for medical waste disposal should be increased. In addition to using expropriated incinerators, other possible solutions, including reusing medical personal protective equipment after proper disinfection, can be implemented to address dramatic increases in waste. However, every solution must reduce the risk of infection.
-
(4)
Finally, in the context of the global pandemic, medical waste is increasing in almost every city around the world. Wuhan's emergency response capacity has been increased through nationwide collaboration and support (Lin et al., 2020). It is recommended that other cities pay attention to the safe storage and the transportation and disposal of solid waste and strengthen cooperation to mitigate the pressure of medical waste disposal to reduce the risk of infection (Mo et al., 2020; Seppänen et al., 2013). Of course, there is also a need for stricter control measures to reduce the incidence of COVID-19 and medical waste production at the source.
Credit Author Statement
Chang Chen: Conceptualization, Methodology, Formal analysis, Writing - Original Draft Jiaao Chen: Visualization Investigation. Ran Fang: Data curation, Investigation Zhenglun Yang : Visualization Zhen Wang: Conceptualization, Methodology, Writing - Review & Editing Feng Shi: Conceptualization, Writing - Review & Editing Wenfeng Tan: Conceptualization, Supervision
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This study is financially supported by the Startup Fund of Huazhong Agricultural University for High-Level Talent to Zhen Wang.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.resconrec.2021.105600.
Appendix. Supplementary materials
References
- Adyel T.M. Accumulation of plastic waste during COVID-19. Science. 2020;369(6509):1314–1315. doi: 10.1126/science.abd9925. [DOI] [PubMed] [Google Scholar]
- Alsayedahmed H.H. COVID-19 Pandemic's precautionary measures had hit the reset button of the quality of life at different aspects. J. Infect. Dev. Countries. 2020;14(8):812–816. doi: 10.3855/jidc.12943. [DOI] [PubMed] [Google Scholar]
- Alshraideh H., Abu Qdais H. Stochastic modeling and optimization of medical waste collection in Northern Jordan. J. Mater. Cycles Waste Manag. 2017;19(2):743–753. doi: 10.1007/s10163-016-0474-3. [DOI] [Google Scholar]
- Anderson D.C., Grey T., Kennelly S., O'Neill D. Nursing home design and COVID-19: balancing infection control, quality of life, and resilience. J. Am. Med. Direct. Assoc. 2020;21(11):1519–1524. doi: 10.1016/j.jamda.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asari M., Sakai S., Yoshioka T., Tojo Y., Tasaki T., Takigami H., Watanabe K. Strategy for separation and treatment of disaster waste: a manual for earthquake and tsunami disaster waste management in Japan. J. Material Cycles And Waste Management. 2013;15(3):290–299. doi: 10.1007/s10163-013-0154-5. [DOI] [Google Scholar]
- Borrelle S.B., Ringma J., Law K.L., Monnahan C.C., Lebreton L., McGivern A., Murphy E., Jambeck J., Leonard G.H., Hilleary M.A., Eriksen M., Possingham H.P., De Frond H., Gerber L.R., Polidoro B., Tahir A., Bernard M., Mallos N., Barnes M., Rochman C.M. Predicted growth in plastic waste exceeds efforts to mitigate plastic pollution. Science. 2020;369(6510):1515–1518. doi: 10.1126/science.aba3656. [DOI] [PubMed] [Google Scholar]
- Brown C., Milke M., Seville E. Disaster waste management: a review article. Waste Manag. 2011;31(6):1085–1098. doi: 10.1016/j.wasman.2011.01.027. [DOI] [PubMed] [Google Scholar]
- cnhubei.com, 2020. Wuhan qianzishan circular economy industrial park hazardous waste disposal project handed over to CCBC. http://news.cnhubei.com/content/2020-09/23/content_13354029.html. (Accessed 16 December 2020).
- Giani P., Castruccio S., Anav A., Howard D., Hu W., Crippa P. Short-term and long-term health impacts of air pollution reductions from COVID-19 lockdowns in China and Europe: a modelling study. Lancet Planetary Health. 2020;4(10):E474–E482. doi: 10.1016/s2542-5196(20)30224-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han P., Cai Q., Oda T., Zeng N., Shan Y., Lin X., Liu D. Assessing the recent impact of COVID-19 on carbon emissions from China using domestic economic data. Sci. Total Environ. 2020;750 doi: 10.1016/j.scitotenv.2020.141688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He C., Yang L., Cai B.F., Ruan Q.Y., Hong S., Wang Z. Impacts of the COVID-19 event on the NOx emissions of key polluting enterprises in China. Appl. Energy. 2021;281 doi: 10.1016/j.apenergy.2020.116042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HubeiDaily, 2020a. Wuhan chemical industry district tax service helps renewable energy enterprises to get 1.38 million yuan policy dividend. http://news.hubeidaily.net/web/1512/202012/01/791164.html. (Accessed 16 December 2020).
- HubeiDaily, 2020b. Wuhan qianzishan medical waste disposal plant and other 13 projects have started. http://news.cnhubei.com/content/2020-09/23/content_13354029.html. (Accessed 16 December 2020).
- Ikiz E., Maclaren V.W., Alfred E., Sivanesan S. Impact of COVID-19 on household waste flows, diversion and reuse: The case of multi-residential buildings in Toronto, Canada. Resour. Conserv. Recycl. 2021;164 doi: 10.1016/j.resconrec.2020.105111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hospital Infect. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klemeš J.J., Fan Y.V., Tan R.R., Jiang P. Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew. Sustain. Energy Rev. 2020;127 doi: 10.1016/j.rser.2020.109883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau H., Khosrawipour V., Kocbach P., Mikolajczyk A., Schubert J., Bania J., Khosrawipour T. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J. Travel Med. 2020;27(3):taaa037. doi: 10.1093/jtm/taaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le T., Wang Y., Liu L., Yang J., Yung Y.L., Li G., Seinfeld J.H. Unexpected air pollution with marked emission reductions during the COVID-19 outbreak in China. Science. 2020;369(6504):702–706. doi: 10.1126/SCIENCE.ABB7431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Q.Y., Zhao S., Gao D.Z., Lou Y.J., Yang S., Musa S.S., Wang M.G.H., Cai Y.L., Wang W.M., Yang L., He D.H. A conceptual model for the coronavirus disease 2019 (COVID-19) outbreak in Wuhan, China with individual reaction and governmental action. International J. Infectious Diseases. 2020;93:211–216. doi: 10.1016/j.ijid.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z., Ciais P., Deng Z., Lei R., Davis S.J., Feng S., Zheng B., Cui D., Dou X., Zhu B., Guo R., Ke P., Sun T., Lu C., He P., Wang Y., Yue X., Wang Y., Lei Y., Zhou H., Cai Z., Wu Y., Guo R., Han T., Xue J., Boucher O., Boucher E., Chevallier F., Tanaka K., Wei Y., Zhong H., Kang C., Zhang N., Chen B., Xi F., Liu M., Breon F.-M., Lu Y., Zhang Q., Guan D., Gong P., Kammen D.M., He K., Schellnhuber H.J. Near-real-time monitoring of global CO2 emissions reveals the effects of the COVID-19 pandemic. Nat. Commun. 2020;11(1):5172. doi: 10.1038/s41467-020-18922-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lv Z., Wang X., Deng F., Ying Q., Archibald A.T., Jones R.L., Ding Y., Cheng Y., Fu M., Liu Y., Man H., Xue Z., He K., Hao J., Liu H. Source-receptor relationship revealed by the halted traffic and aggravated haze in Beijing during the COVID-19 lockdown. Environ. Sci. Technol. 2020;54(24):15660–15670. doi: 10.1021/acs.est.0c04941. [DOI] [PubMed] [Google Scholar]
- Markandeya, Verma, P.K., Mishra, V., Singh, N.K., Shukla, S.P., Mohan, D., 2020. Spatio-temporal assessment of ambient air quality, their health effects and improvement during COVID-19 lockdown in one of the most polluted cities of India. Environ. Sci. Pollut. Res.. 10.1007/s11356-020-11248-3. [DOI] [PMC free article] [PubMed]
- Ministry of Industry and Information Technology of the People s Republic of China, 2020. COVID-19 pandemic prevention and control report. https://www.miit.gov.cn/ztzl/rdzt/xxgzbdgrdfyyqfkgz/gzdt/art/2020/art_cea12b5000b8474da3bd8e85918723f1.html. (Accessed 4 December 2020).
- Mo Y.Y., Deng L., Zhang L.Y., Lang Q.Y., Liao C.Y., Wang N.N., Qin M.Q., Huang H.Q. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J. Nurs. Manag. 2020;28(5):1002–1009. doi: 10.1111/jonm.13014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammad A., Goli V.S.N.S., Singh D.N. Discussion on 'Challenges, opportunities, and innovations for effective solid waste management during and post COVID-19 pandemic, by Sharma etal. (2020)'. Resour. Conserv. Recycl. 2021;164 doi: 10.1016/j.resconrec.2020.105175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagano T., Arii J., Nishimura M., Yoshida N., Iida K., Nishimura Y., Mori Y. Diligent medical activities of a publicly designated medical institution for infectious diseases pave the way for overcoming COVID-19: A positive message to people working at the cutting edge. Clin. Infect. Dis. 2020;ciaa694 doi: 10.1093/cid/ciaa694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumeyer X., Ashton W.S., Dentchev N. Addressing resource and waste management challenges imposed by COVID-19: An entrepreneurship perspective. Resour. Conserv. Recycl. 2020;162 doi: 10.1016/j.resconrec.2020.105058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nzediegwu C., Chang S.X. Improper solid waste management increases potential for COVID-19 spread in developing countries. Resour. Conserv. Recycl. 2020;161 doi: 10.1016/j.resconrec.2020.104947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrício Silva A.L., Prata J.C., Walker T.R., Campos D., Duarte A.C., Soares A.M.V.M., Barcelò D., Rocha-Santos T. Rethinking and optimising plastic waste management under COVID-19 pandemic: Policy solutions based on redesign and reduction of single-use plastics and personal protective equipment. Sci. Total Environ. 2020;742 doi: 10.1016/j.scitotenv.2020.140565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrício Silva A.L., Prata J.C., Walker T.R., Duarte A.C., Ouyang W., Barcelò D., Rocha-Santos T. Increased plastic pollution due to COVID-19 pandemic: Challenges and recommendations. Chem. Eng. J. 2021;405 doi: 10.1016/j.cej.2020.126683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- People's Archive of Rural India, 2020. Essential services, expendable lives. https://ruralindiaonline.org/en/articles/essential-services-expendable-lives/. (Accessed 28 Jan 2021).
- People.cn, 2020. Greate a safe barrier for medical waste - Wuhan union hospital establish a new model of medical waste management. http://health.people.com.cn/n1/2020/1118/c14739-31935592.html. (Accessed 16 December 2020).
- Powell-Jackson T., King J.J.C., Makungu C., Spieker N., Woodd S., Risha P., Goodman C. Infection prevention and control compliance in Tanzanian outpatient facilities: a cross-sectional study with implications for the control of COVID-19. Lancet Global Health. 2020;8(6):E780–E789. doi: 10.1016/s2214-109x(20)30222-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata J.C., Silva A.L.P., Walker T.R., Duarte A.C., Rocha-Santos T. COVID-19 pandemic repercussions on the use and management of plastics. Environ. Sci. Technol. 2020;54(13):7760–7765. doi: 10.1021/acs.est.0c02178. [DOI] [PubMed] [Google Scholar]
- Prem K., Liu Y., Russell T.W., Kucharski A.J., Eggo R.M., Davies N., Jit M., Klepac P., Ctr Math Modelling Infect Dis C. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5(5):E261–E270. doi: 10.1016/s2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seppänen H., Mäkelä J., Luokkala P., Virrantaus K. Developing shared situational awareness for emergency management. Safety Science. 2013;55:1–9. doi: 10.1016/j.ssci.2012.12.009. [DOI] [Google Scholar]
- Sharma H.B., Vanapalli K.R., Cheela V.R.S., Ranjan V.P., Jaglan A.K., Dubey B., Goel S., Bhattacharya J. Challenges, opportunities, and innovations for effective solid waste management during and post COVID-19 pandemic. Resour. Conserv. Recycl. 2020;162 doi: 10.1016/j.resconrec.2020.105052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen, H.Z., Shen, G.F., Chen, Y.L., Russell, A.G., Hu, Y.T., Duan, X.L., Meng, W.J., Xu, Y., Yun, X., Lyu, B.L., Zhao, S.L., Hakami, A., Guo, J.P., Tao, S., Smith, K.R., 2021. Increased air pollution exposure among the Chinese population during the national quarantine in 2020. Nat. Hum. Behav.. 10.1038/s41562-020-01018-z. [DOI] [PubMed]
- Singh N., Tang Y., Ogunseitan O.A. Environmentally sustainable management of used personal protective equipment. Environ. Sci. Technol. 2020;54(14):8500–8502. doi: 10.1021/acs.est.0c03022. [DOI] [PubMed] [Google Scholar]
- Singh N., Tang Y., Zhang Z., Zheng C. COVID-19 waste management: Effective and successful measures in Wuhan, China. Resour. Conserv. Recycl. 2020;163 doi: 10.1016/j.resconrec.2020.105071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabish, M., Khatoon, A., Alkahtani, S., Alkahtane, A., Alghamdi, J., Ahmed, S.A., Mir, S.S., Albasher, G., Almeer, R., Al-Sultan, N.K., Aljarba, N.H., Al-Qahtani, W.S., Al-Zharani, M., Nayak, A.K., Hasnain, M.S., 2020. Approaches for prevention and environmental management of novel COVID-19. Environ. Sci. Pollut. Res.. 10.1007/s11356-020-10640-3. [DOI] [PMC free article] [PubMed]
- The government of Wuhan, 2019a. Wuhan overview. http://www.wuhan.gov.cn/zjwh/. (Accessed 4 December 2020).
- The government of Wuhan, 2019b. Wuhan Social Services - Health. http://www.wuhan.gov.cn/zjwh/shsy/202003/t20200316_976491.shtml. (Accessed 4 December 2020).
- The government of Wuhan, 2020. Wuhan domestic waste classification management regulations.
- Thomson reuters foundation news, 2020. 'How are we meant to eat?': A South African waste picker on life under lockdown. https://news.trust.org/item/20200407102057-bcmya/?fbclid=IwAR1zi_Lj-KoMrgbhGt3FgKKenVUqJ2sWkl6GtjsxxD6Q3k_qr4LTtjA4OGk. (Accessed 28 Jan 2021).
- Tripathi A., Tyagi V.K., Vivekanand V., Bose P., Suthar S. Challenges, opportunities and progress in solid waste management during COVID-19 pandemic. Case Stud. Chem. Environ. Eng. 2020;2 doi: 10.1016/j.cscee.2020.100060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., Lloyd-Smith J.O., de Wit E., Munster V.J. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. New Engl. J. Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanapalli K.R., Sharma H.B., Ranjan V.P., Samal B., Bhattacharya J., Dubey B.K., Goel S. Challenges and strategies for effective plastic waste management during and post COVID-19 pandemic. Sci. Total Environ. 2021;750 doi: 10.1016/j.scitotenv.2020.141514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J.F., Xu X.Y., Wang S.M., He S.T., He P. Heterogeneous effects of COVID-19 lockdown measures on air quality in Northern China. Appl. Energy. 2021;282 doi: 10.1016/j.apenergy.2020.116179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Lu M., Bai Z., Wang K. Coronavirus pandemic reduced China's CO2 emissions in short-term, while stimulus packages may lead to emissions growth in medium- and long-term. Appl. Energy. 2020;278 doi: 10.1016/j.apenergy.2020.115735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windfeld E.S., Brooks M.S.-L. Medical waste management–a review. J. Environ. Manag. 2015;163:98–108. doi: 10.1016/j.jenvman.2015.08.013. [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2021. WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/. (Accessed 1 February 2020).
- Xiao Y., Torok M.E. Taking the right measures to control COVID-19. Lancet Infect. Dis. 2020;20(5):523–524. doi: 10.1016/S1473-3099(20)30152-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L., Yu X., Wu X., Wang J., Yan X., Jiang S., Chen Z. Emergency response to the explosive growth of health care wastes during COVID-19 pandemic in Wuhan, China. Resour. Conserv. Recycl. 2021;164 doi: 10.1016/j.resconrec.2020.105074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- You S.M., Sonne C., Ok Y.S. COVID-19′s unsustainable waste management. Science. 2020;368(6498):1438. doi: 10.1126/science.abc7778. [DOI] [PubMed] [Google Scholar]
- Zhang J., Wang X., Jia X., Li J., Hu K., Chen G., Wei J., Gong Z., Zhou C., Yu H., Yu M., Lei H., Cheng F., Zhang B., Xu Y., Wang G., Dong W. Risk factors for disease severity, unimprovement, and mortality in COVID-19 patients in Wuhan, China. Clin. Microbiol. Infect. 2020;26(6):767–772. doi: 10.1016/j.cmi.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu W., Wang Y., Xiao K., Zhang H., Tian Y., Clifford S.P., Xu J., Huang J. Establishing and managing a temporary coronavirus disease 2019 specialty hospital in Wuhan, China. Anesthesiol. J. Am. Soc. Anesthesiol. 2020;132(6):1339–1345. doi: 10.1097/ALN.0000000000003299. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.