Abstract
Human papilloma virus (HPV)-16 is associated with cervical cancers and induces expression of the E6 and E7 oncogenes. Using a murine cell line that expresses these, the genes were sequenced and 6 predicted major histocompatibility complex (MHC) class I (MHC-I) epitopes were identified. A liposomal vaccine adjuvant based on cobalt-porphyrin-phospholipid (CoPoP) was admixed with synthetic 9-mer epitopes appended with 3 histidine residues, resulting in rapid formation of stable peptide-liposome particles. Synthetic monophosphoryl lipid A and QS-21 were also included in the liposome bilayer. Immunization with multivalent peptides led to protection from tumor challenge. Of the peptides screened, only the previously identified E749–57 epitope was functional. The peptide-liposome particles that formed upon mixing E7HHH49–57 with CoPoP liposomes were stable in serum and avidly taken up by immune cells in vitro. Immunization with E7HHH49–57 admixed with CoPoP liposomes resulted in robust protection from tumor challenge and re-challenge. Immunization with the synthetic short peptide at a dose of 100 ng protected mice in a therapeutic tumor challenge when admixed with CoPoP liposomes, whereas 200-fold higher peptide doses were ineffective with the Poly(I:C) adjuvant. CoPoP induced strong infiltrating CD8+ T response within the tumor microenvironment with improved functional profile. Vaccine monotherapy using nanogram dosing of the E7HHH49–57 peptide admixed with CoPoP reversed the growth of large established tumors, permanently eradicating subcutaneous tumors upwards of 100 mm3. Immunization also eradicated lung tumors in a metastasis model.
Keywords: HPV, Peptide, CD8+ T cell, Liposome, Vaccine, Cancer, Immunotherapy
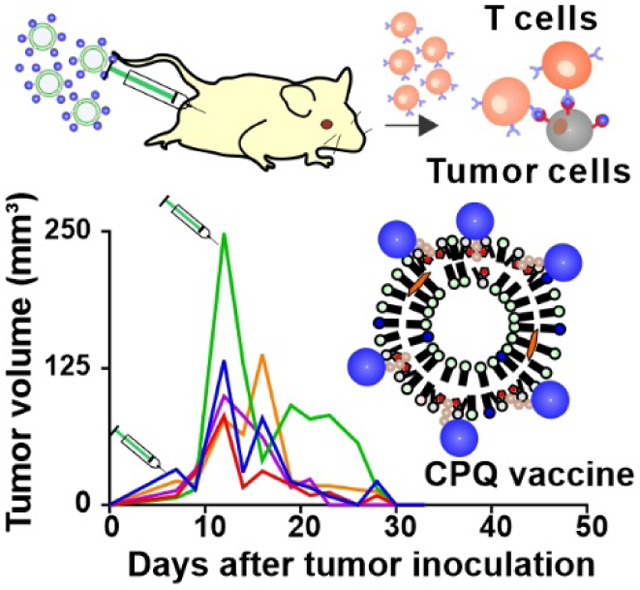
Graphical Abstract
A liposomal vaccine based that induces spontaneous conversion of peptides into serum-stable particles was developed with a synthetic short peptide derived from the human papillomavirus. Vaccination resulted in robust protection from tumor challenge and re-challenge, a strong infiltrating CD8+ T cell response within the tumor microenvironment as well as reversal of established tumors; including eradication of tumors upwards of 100 mm3 and lung metastases.
Introduction
High-risk human papillomavirus (HPV, such as type 16 (HPV-16) is often associated with cervical cancer, which remains the second most prevalent female cancer.[1, 2] HPVs are also related with penile, vulvar and anal carcinomas and more than 40% of oropharyngeal cancers.[3, 4] Prophylactic HPV vaccines (i.e., Gardasil and Cervarix) generate neutralizing capsid antibodies against the virus and represent the most successful cancer vaccines, having been adopted into national immunization programs in most industrial nations, preventing significant numbers of cancer deaths.[5] However, there are currently no HPV therapeutic vaccines approved for use in humans against established malignancies, which require strong cellular immune responses rather than humoral ones. The HPV-16 cellular oncoproteins E6 and E7 (E6/E7) transform infected cells, are expressed constitutively at high levels, and represent potential rejection antigens for therapeutic HPV vaccines.[6–8] Clinical cervical cancer trials have been carried out using epitopes derived from the E6/E7 oncogenes.[9–11] For preclinical HPV-expressing tumor research, the TC-1 murine cell-line, which expresses E6/E7, has been widely used.[12]
Many approaches have been examined for enhancing the cellular immune responses against E6/E7, including the use of live-vector vaccines that spread antigen inside host cells,[9, 13, 14] proteins,[15, 16] nucleic acids,[17] cells,[18] peptide vaccines,[19] and combinatorial approaches.[20] Amongst these strategies, short peptide vaccines (i.e. ~8–12 amino acids in length) corresponding to CD8+ T cell epitopes are likely the simplest to produce. However, they are often suffer from poor immunogenicity. To bypass this, peptide sequences can be elongated to generate synthetic long peptides (SLPs) that cover both CD4+ T cell and CD8+ T cell epitopes.[21–26] In clinical trials, SLPs induced the regression of premalignant lesions in early stage but not late-stage HPV16+ cervical cancer patients.[19, 27]
Another way to enhance the immunogenicity of short peptide is to include strong adjuvants or peptide delivery systems to induce tumor antigen (Ag)-specific CD8+ T cells.[28, 29] This has been done in clinical trials using short peptides derived from E7 with incomplete Freund’s adjuvant, for example.[11] In pre-clinical studies, numerous experimental approaches have been explored, frequently using the short E749–57 epitope (sequence: RAHYNIVTF) along with: Virus like particles,[30] very small size proteoliposomes (VSSP),[31] granulocyte-macrophage colony stimulating factor (GM-CSF) genes,[32] lipopeptides,[33] glycolipid-peptides, carrageenan,[34] toll-like receptor (TLR) agoinsts TLR3 ligand polyinosinic-polycytidylic (poly(I:C)),[35, 36] the TLR9 agonist CpG[37, 38] and the TLR1/2 agonist Pam3CSK4[39].
Among adjuvants in licensed human vaccines, AS01, a liposome formulation incorporating monophosphoryl lipid A (MPLA) and the saponin QS-21 is one of the most potent.[40, 41] Our laboratory has previously shown that liposomes that incorporate MPLA, as well as cobalt-porphyrin-phospholipid (CoPoP), can induce strong antibody (Ab) generation for peptides and proteins.[42–46] The mechanism of CoPoP is to induce spontaneous particle formation of Ags bearing a polyhistidine segment. In this study, we use so-called CPQ liposomes formed with CoPoP, PHAD-3D6A (a synthetic derivative of MPLA) and QS-21. We also test control liposomes in which the cobalt of CoPoP is replaced with 2 hydrogens, to generate 2HPQ, which contain the identical amount of MPLA and QS-21. This enables us to assess the effect of particle formation by comparing CPQ to 2HPQ, which both contain active components similar to AS01, but only CPQ forms stable antigenic particles. CPQ is admixed with short peptides targeted against E6/E7 epitopes in the TC-1 mouse model that expresses them to screen for functional epitopes following gene sequencing, and also demonstrate potent immune responses against primary and metastatic disease responses.
Results
In vivo Screening of HPV-16 E6/E7 CD8+ T cell epitopes
The E6 and E7 genes of TC-1 cells were sequenced from extracted DNA using Sanger sequencing (Table S1). Six predicted H-2Kb- and H-2Db-restricted epitopes within the top percentile of MHC-I binders were identified using a neural network simulation algorithm.[47, 48] These short 9-mer peptides were then chemically synthesized as shown in Table 1, along with a 3-residue polyhistidine sequence to induce particle formation upon admixing with CPQ liposomes. These 6 peptides were combined with CPQ to form a single multivalent vaccine for mice and the immunogenicity of each peptide were assessed by interferon-gamma (IFN-γ) production after individual peptide stimulation of collected peripheral blood mononuclear cells (PBMCs). Mice were then challenged with TC-1 cells subcutaneously to assess the tumor protection of the vaccine (Figure 1A).
Table 1.
Predicted MHC-I epitopes in E6/E7 oncogenes sequenced from TC-1 cells.
| Position | Sequence* | MHC allele | NetMHC percentile |
HPLC purity (%) | Theoretical M.W. | Observed M.W. |
|---|---|---|---|---|---|---|
| E749–57 | H3-RAHYNIVTF | H-2Db | 0.0101 | 98 | 1531.7 | 1531.6 |
| E771–79 | H3-STHVDIRTL | H-2Db | 0.3098 | 97.7 | 1452.6 | 1452.4 |
| E76–14 | H3-TLHEYMLDL | H-2Db | 0.9233 | 92.9 | 1545.7 | 1545.9 |
| E661–69 | H3-YRDGNPYAV | H-2Db | 0.6144 | 98.4 | 1465.5 | 1465.2 |
| E662–70 | H3-FAFRDLCIV | H-2Db | 0.7017 | 91.0 | 1494.7 | 1494.6 |
| E682–90 | H3-KCLKFYSKI | H-2Kb | 0.4193 | 95.3 | 1540.8 | 1540.8 |
H3 represents three histidine residues on the N terminus. M.W. represents molecular weight.
Figure 1. E6/E7 MHC-I epitope candidates form immunogenic particles that inhibit TC-1 tumor growth.

A) Approach for screening for functional MHC-I restricted epitopes by DNA sequencing the E6/E7 oncogenes; predicting MHC-I epitopes; using CPQ to form a multivalent vaccine; and immunizing mice to assess functional immunogenicity. B) Binding of the 6 synthetized peptides identified to CPQ or 2HPQ liposomes. C57BL/6 mice were vaccinated with the multivalent vaccine on days 0 and 7; then on day 14, blood was collected and central memory (C) and effector memory phenotypes (D) within the gated CD8+ T cell population was assessed. E) Epitope-specific, IFN-γ producing CD8+ T cells from PBMCs of mice vaccinated with the multiplexed vaccine. F) Tumor growth in mice challenged with TC-1 cells following immunization with the multiplexed vaccine. Error bars show mean +/−std. dev. for n=3 per group for binding and size studies and n=5 per group for mice studies. * p < 0.05, *** p < 0.001 and **** p < 0.0001, analyzed by (E, F) two-way ANOVA with Bonferroni multiple comparisons post-test or (B, C, D) two-tailed unpaired Student’s t test.
The multivalent peptide vaccine was prepared by simple admixing of the 6 peptides with CPQ liposomes at a total peptide to CoPoP mass ratio of 1:4. The dose of each peptide was 100 ng. QS-21 and MPLA were also present in the liposomes at a peptide to each adjuvant mass ratio of 1:1.6. After mixing the 6 pooled E6/E7 epitope candidates with CPQ liposomes for 1 hr at room temperature, ~100% of the peptides were converted into particle form, as assessed by a microcentrifugal filtration assay (Figure 1B). Identical 2HPQ liposomes lacking cobalt, displayed minimal binding with peptides. Following particle formation with the peptides, the size of liposomes (CPQ and 2HPQ) remained ~100 nm (Figure S1A). The polydispersity index (PDI) of these liposomes was less than 0.15 (Figure S1B) with narrow size distribution (Figure S1C). We did not assess the size stability of the liposomes in this study but previously found that CoPoP liposomes are stable in refrigerated storage for at least 9 months.[42]
To determine immunogenicity, C57BL/6 mice were then vaccinated intramuscularly with the multivalent vaccine on days 0 & 7, and peripheral blood mononuclear cells (PBMCs) were collected and mice challenged with TC-1 tumor cells on day 14. By then, there was a significant increase in the percentage of both central memory T cells (TCM) of CD8+ T cells, defined as CD44+CD62L+ (Figure 1C), and effector memory T cells (TEM) of CD8+ T cells, defined as CD44+CD62L− (Figure 1D) in mice immunized with the peptides mixed with CPQ, but not 2HPQ. Thus, the presentation of the peptides in the form of a particle, even with identical amounts of QS-21 and MPLA, appeared to be important for inducing memory CD8+ T cells.
Collected PBMCs were re-stimulated with the epitope candidates that comprised the multivalent vaccine after which CD8+ T cells were assessed for intracellular IFN-γ production, indicating the induction of Ag-specific CD8+ T cells. Three peptides induced higher percentage of IFN-γ producing cells of CD8 + T cells over background in the post-immune PBMCs; E749–57, E771–79 and E76–14. When PBMCs from mice injected with the non-particle forming 2HPQ/peptides were re-stimulated with the peptides, none induced IFN-γ producing CD8+ T cells (Figure 1E). When immunized mice were challenged with TC-1 cells injected subcutaneously, the multivalent CPQ/peptides vaccine group completely rejected tumor growth. In contrast, mice vaccinated with the 2HPQ/peptides formulation developed rapidly growing tumors (Figure 1F).
Next, to determine which of the peptide epitopes provided anti-tumor activity, peptides were admixed individually with CPQ or 2HPQ liposomes (Figure 2A). Individually, all of the peptides effectively bound to CPQ liposomes, but not to 2HPQ liposomes lacking cobalt (Figure 2B). Liposome size remained ~100 nm after binding with E6 and E7 peptides (Figure 2C). Next, mice were vaccinated with the peptides admixed with CPQ on days 0 & 7 at a peptide dose of 500 ng. Each mouse was then challenged with TC-1 cells on day 14. Of all the synthetic short peptide epitopes assessed, only the E7HHH49–57 peptide (sequence: HHH-RAHYNIVTF) inhibited tumor growth (Figure 2D). Prolonged tumor-free survival was maintained to at least 60 days (Figure 2E) reflecting the observational period, while no other predicted peptide epitopes had any measurable anti-tumor efficacy.
Figure 2. All E6/E7 synthetic epitopes formed particles with CPQ, but only E749–57 inhibited TC-1 tumor growth.

A) Schematic of single peptide vaccines assessed to identify functional epitopes. Binding (B) and size (C) of predicted HPV-16 E6/E7 epitopes to CPQ and 2HPQ liposomes. Peptides were incubated for 1 hr at room temperatures with liposomes prior to measurement. Error bars show mean +/− std. dev. for n=3. Mice were immunized with 500 ng of each peptide mixed with CPQ on days 0 and 7 and subjected to TC-1 tumor challenge on day 14. Mean tumor volume (D) and percentage of mice with tumors size less than 1 cm (E) for n=5 mice per group. All mice in the CPQ/E749–57 group were tumor free at the end of the study.
CPQ forms particles with E7HHH49–57 and enhances antigen delivery.
Given that only the E7HHH49–57 peptide produced significant anti-tumor responses, we investigated in more detail the mechanisms accounting for its efficacy. Cryo-electron microscopy revealed that both CPQ liposomes with or without peptide bound were spherical and unilamellar, with size close to 100 nm (Figure 3A). Incubation with the peptide did not impact CPQ and 2HPQ liposome polydispersity (Figure 3B) or surface charge (Figure 3C), which have negative zeta potential. Using a C-terminus fluorescently labeled analog of the peptide, binding to the liposomes was monitored in real-time, owing to fluorescence energy transfer from the fluorophore to the porphyrin chromophore in CPQ or 2HPQ liposomes. Within an hour of incubation, the labeled E7HHH49–57 peptide fluorescence became more than 80% quenched, reflecting rapid binding to the liposomes (Figure 3D). Incubation with 2HPQ liposomes did not result in quenching of the fluorescence of the peptide, consistent with the microcentrifugal filtration assay using the unlabeled peptide (Figure 1B and 2B). These data are also consistent with the biological notion that if the peptide is a hapten, then only if it can form particles (i.e. with CPQ in this work) does it have the potential to be immunogenic. In the presence of fetal bovine serum (FBS), > 70 % of the E7HHH49–57 peptide remained fluorescently quenched and bound to CPQ liposomes for at least two weeks of incubation, reflecting peptide-particle formation is relatively stable in biological fluids (Figure 3E).
Figure 3. CPQ/E7HHH49–57 particles form rapidly, are serum stable and deliver the synthetic short peptide to macrophages in vitro.

A) Cryo-electron micrographs of CPQ liposomes with or without E7HHH49–57 peptide bound. Polydispersity (B) and zeta potential (C) of CPQ and 2HPQ liposome with or without E7HHH49–57 peptide bound. D) Binding kinetic of a HiLyte488-fluorescently labeled E7HHH49–57 synthetic short peptide to CPQ or 2HPQ liposomes. E) Stability of the fluorescent E7HHH49–57 peptide with CPQ or 2HPQ in PBS or 10% fetal bovine serum (FBS). F) Labeled peptide uptake in RAW264.7 macrophages after admixing the peptide with indicated liposomes. 2HPQ (but not CPQ) liposomes themselves are fluorescent and were imaged. G) Fluorescence microscopy images of murine macrophages incubated with labeled peptide admixed with indicated liposomes. H) In vitro peptide binding to CPQ, and stability in serum and commercial lysosome extract. Error bars show mean +/−std. dev. for n=3 per group. **** p < 0.0001, analyzed by (F) one-way ANOVA with Bonferroni multiple comparisons post-test. Figure D to H made use of a fluorescently labeled E7HHH49–57 peptide.
To gain insights into the mechanism of peptide uptake, the labeled E7HHH49–57 peptide was assessed by incubation with murine macrophages. When admixed with CPQ, 5% of the total peptide in the incubation mixture was taken up by macrophages (Figure 3F). However, there was no Ag uptake when E7HHH49–57 alone or following admixture with 2HPQ. This result was confirmed by fluorescence microscopy, as the labeled peptide was only effectively taken up when mixed with CPQ liposomes (Figure 3G). As the cobalt in CPQ quenches the fluorescence of the labeled peptide upon binding (Figure 3D), the fluorescence shown in the macrophages suggests that the peptide is released from the liposomes after cellular uptake. It should be noted that cobalt also quenches the fluorescence of the porphyrin moiety, and for that reason no fluorescence was detected in the 2HPQ channel.
The enhanced uptake of the peptide antigen was not unexpected, as we previously have shown that CoPoP liposomes enhance antigen delivery to a range of antigen-presenting cells (APCs) including macrophages, dendritic cells, and B cells in draining lymph nodes in vivo.[42] The particle-based presentation of the antigen results in improved delivery to the APCs while the adjuvant components can support dendritic cell maturation.[42] In the case of small peptides presented on CoPoP liposomes, we speculate that they may be released into endosomes and transferred directly onto MHC-I, based on the vacuolar model of MHC-I epitope presentation.[49] To determine if this was possible, we assessed the binding and release of the fluorescently labeled E7HHH49–57 peptide to CPQ under different conditions (Figure 3H). Rapid binding was observed after the addition of CoPoP liposomes in PBS, and this binding remained stable following serum addition. However, when incubated with commercial lysosome extract in vitro, release of the peptide was observed. While further investigation is required to enhance our understanding of this mechanism, and how it relates to the biochemical conditions in the lysosome, these observations support a putative basis for at least part of the effective immunization mechanism.
Potent CD8+ T cell responses induced by CPQ/ E7HHH49–57
To determine immunogenicity, naïve C57BL/6 mice were either untreated or vaccinated with E7HHH49–57 on days 0 and day 7; then spleens were collected for Ag-specific T cell analyses. When the peptide was admixed with CPQ, ~30% of the CD8+ T cells in the blood and 20% of the CD8+ T cells in the spleen were determined to be Ag-specific, based on tetramer staining (Figure 4A and Figure 4B). In contrast, when the peptide was admixed with 2HPQ for immunization, virtually no Ag-specific CD8+ T cell was induced, similar to the untreated mice. After vaccination with CPQ/E7HHH49–57, there was a significant increase of both central memory CD8+ T cells (Figure 4C) and effector memory CD8+ T cells (Figure 4D). After re-stimulation with the peptide, splenocytes from CPQ/E7HHH49–57 vaccinated mice showed ~10% of all CD8+ T cells were capable of producing IFN-γ, but not CD4+ T cells (Figure 4E and Figure 4F). This reflects that E7HHH49–57 is an MHC-I-binding epitope capable only of inducing Ag-specific CD8+ T cells. After CPQ/E7HHH49–57 vaccination, the induced CD8+ T also produced Tumor necrosis factor alpha (TNF-α) (Figure 4G) and interleukin-2 (IL-2) (Figure 4H).
Figure 4. Immunization with CPQ/E7HHH49–57 induces a robust Ag-specific, cytokine-producing CD8+ T response.

Naive C57BL/6 mice were vaccinated on days 0&7, then spleen and blood were collected on day 14. A) Flow cytometry gating of the E7 peptide-specific T cells in the blood. B) Percentage of CD8+ tet+ cells in the blood and spleen. C) Percentage of central memory T cell phenotypes in the CD8+ T cell population in the blood. D) Percentage of effector memory T cell phenotypes in the CD8+ T cell population in the blood. E) Flow cytometric gating of the IFN-γ producing CD8+ T cells. Percentage of IFN-γ (F), TNF-α (G) or IL-2 (H) producing cells within the CD8+ T cell population in the spleen. Error bars show mean +/−std. dev. for n=5 per group. * p < 0.05, ** p < 0.01, *** p < 0.001 and **** p < 0.0001, analyzed by one-way ANOVA with Bonferroni multiple comparisons post-test.
CPQ/E7HHH49–57 as a prophylactic and therapeutic cancer vaccine
Next, we compared immunization with 500 ng E7HHH49–57 admixed with CPQ and 2HPQ (lacking cobalt). Mice immunized with CPQ admixed with 500 ng E7HHH49–57 completely rejected subsequent TC-1 tumor challenge (Figure 5A), and survived without tumor growth under an observational period of more than 60 days (Figure 5B), whereas mice immunized with 500 ng E7HHH49–57 admixed with 2HPQ showed no significant delay of tumor growth compared to a non-immunized group. Thus, CPQ strongly improved the anti-tumor efficacy of immunization with the E7HHH49–57 peptide, while 2HPQ was completely ineffective.
Figure 5. Prophylactic protection from TC-1 tumor challenge induced by immunization with E7HHH49–57 admixed with CPQ liposomes.

C57BL/6 mice were vaccinated with 500 ng peptide admixed with CPQ or 2HPQ on day 0 and 7; then TC-1 tumor cells were inoculated on day 14 subcutaneously. (A) Tumor growth and percentage of mice with tumors smaller than 1 cm (B) of untreated mice or mice vaccinated E7HHH49–57 peptide with CPQ or 2HPQ. Error bars show mean +/−std. dev. for n=5 per group.
Since CPQ/E7HHH49–57 was effective in a prophylactic setting, we next assessed the vaccine on established TC-1 tumors, which is also the setting in which most cancer vaccines would be initially tested clinically. Poly(I:C) was used as an adjuvant comparator. For poly(I:C), the synthetic short peptide dose ranged from 20 μg to 2 μg per mouse while the poly(I:C) dose remained fixed at 20 μg/mouse. For the CPQ liposome adjuvant, the peptide dosing varied from 1 to 0.1 μg per mouse. Given that the ratio of liposomes to peptide was fixed, this corresponds to a 3D6A-PHAD dose and QS-21 dose ranging from 1.6 to 0.16 μg, along with a CoPoP dose ranging from 4 to 0.4 μg. The identical E7HHH49–57 peptide was admixed with either of the adjuvants just prior to intramuscularly immunization. Mice were first inoculated with TC-1 cells on day 0 and then vaccinated on days 2 and 9. Under these conditions, only the CPQ adjuvant, but not the poly(I:C) adjuvant resulted in effective tumor growth inhibition (Figure 6A). On day 19, CPQ vaccinated mice had no detectable tumor growth, but nearly all the of the poly(I:C) vaccinated mice did, even at the highest dose of peptide (20 μg) (Figure 6B). The tumors of all the poly(I:C)-vaccinated mice reached the 1 cm endpoint within 60 days, whereas all CPQ-vaccinated mice remained tumor-free even at just a 0.1 μg E7 peptide dose, which reflects a 200-fold lower dose compared to the upper peptide dose with poly(I:C) (Figure 6C). As anti-tumor efficacy would be expected to relate to the frequency of Ag-specific CD8+ T cells, we examined this 19 days post-tumor inoculation. In the CPQ vaccinated mice, there were higher percent of CD8+ T cells that were Ag-specific in the blood, with increasing peptide dose. A peptide dose of 1 μg resulted in ~30% tetramer-positive (tet+) CD8+ T cells, whereas, a peptide dose of 0.1 μg resulted in tet+ conversion of ~20% CD8+ T cells. In strong contrast, poly(I:C) vaccinated mice had almost no Ag-specific CD8+ T cells in the blood (Figure 6D). The percentage of TEM of CD8+ T cells (Figure S2A), but not TCM of CD8+ T cells (Figure S2B) increased drastically in the CPQ vaccinated group compared to the poly(I:C) vaccinated mice.
Figure 6. Immunization with E7HHH49–57-admixed with CPQ inhibits tumor growth in a therapeutic setting more potently than poly(I:C).

C57BL/6 mice were inoculated with TC-1 cells subcutaneously on day 0; then different vaccines were given 2 days post-tumor inoculation. Blood was collected 18 days post-tumor inoculation for CD8+ T cell analyses. A) Tumor growth of mice that vaccinated with indicated vaccine. B) Tumor sizes of mice on day 19. C) Survival of mice. D) Percentage of CD8+E749–57 tet+ cells in the blood. Error bars show mean +/−std. dev. for n=5 per group. * p < 0.05, ** p < 0.01 and **** p < 0.0001, analyzed by (C) long rank test or (D) one-way ANOVA with Bonferroni multiple comparisons post-test.
Systemic dysfunction of antigen-specific CD8+ T cells in the tumor
Next, we investigated the impact of vaccination on the T cell response in the tumor microenvironment (TME). Given the efficacy of the vaccine to eradicate smaller tumors inoculated two days before immunization (Figure 6), we assessed vaccine efficacy on days 8 and 16 following tumor inoculation. As in the prior study, mice were immunized with 500 ng of E7HHH49–57 peptide admixed with CPQ or 20 μg of E7HHH49–57 peptide poly(I:C). On day 18, tumor and spleen were collected for analyses. Within the TME, a significantly higher frequency of CD8+ T cells infiltrated in response to CPQ vaccination compared to poly(I:C) vaccination or the untreated groups (Figure 7A and Figure 7B), as judged by immunohistochemistry (IHC) and flow cytometry. For CPQ/E7HHH49–57 immunized mice, ~80% of the CD8+ T cells in the TME were Ag-specific, whereas, ~30% of CD8+ T cells were Ag-specific in the spleen (Figure 7C and Figure S3). In response to immunization with poly(I:C)/E7HHH49–57 ~70% of the CD8+ T cells in the tumor were Ag-specific; however, the overall frequency of CD8+ T cells in the tumor was very low. The phenotype of these CD8+ T cells was different in both E749–57 tet+ and tet− CD8+ T cells. We observed a significantly greater effector memory CD8+ T cell phenotype in the tet+ cells compared to the tet− fraction (Figure S4), which trended in both the spleen and TME of mice vaccinated with either CPQ or poly(I:C). For CPQ vaccinated mice, less Ag-specific T cells were effector T cell phenotype or central memory T cells comparing the tumor to the spleen.
Figure 7. Intratumoral CD8+ T cell infiltration following immunization with the E7HHH49–57 peptide.

C57BL/6 mice were inoculated with TC-1 cells subcutaneously on day 0 and vaccinated 8 and 15 days post-tumor inoculation. Spleen and tumor tissue were collected 18 days post-tumor inoculation for CD8+ T cell analysis. A) Immunohistochemistry of CD8 staining. B) Percentage of CD8+ T cells within the live cells. C) Percentage of E749–57 tet+ cells within the CD8+ T cell population. Percentage of PD-1+ (D), TIM-3+ (E), LAG-3+ (F) or IFN-γ+ (G) cells within the E749–57 tet+ CD8+ T cells. Error bars show mean +/−std. dev. for n=3 per group. * p < 0.05, ** p < 0.01, *** p < 0.001 and **** p < 0.0001, analyzed by two-way ANOVA with Bonferroni multiple comparisons post-test.
To understand the potential exhaustion and anergy of T cells, we examined the expression of the inhibitory receptors, programmed cell death protein 1 (PD-1), lymphocyte-activation gene 3 (LAG-3) and T-cell immunoglobulin mucin-3 (TIM-3) in both the spleen and the TME. Based on flow cytometry gating (Figure S5), a significantly higher frequency of intratumoral CD8+ tet+ T cells expressed the inhibitory receptors, PD-1 (Figure 7D), TIM-3 (Figure 7E) or LAG-3 (Figure 7F) compared with splenic CD8+ tet+ T cells. Compared to poly(I:C)/E7HHH49–57 vaccinated mice, CPQ/E7HHH49–57 vaccinated mice had a significantly lower proportion of CD8+ tet+ T cells that expressed PD-1, TIM-3 or LAG-3 within the TME. Compared to poly(I:C)/E7HHH49–57, CPQ/E7HHH49–57 vaccinated mice had a much higher proportion of CD8+ tet+ T cells that produced IFN-γ following ex vivo re-stimulation of splenic cells with the E7 synthetic short peptide (Figure 7G). However, in the TME that proportion was only slightly higher. Considering there was a much higher number of CD8+ tet+ T cells in the TME of CPQ-vaccinated mice (Figure 7B), the unexpectedly low frequency of cytokine-secreting CD8+ tet+ T cells in the TME may contribute to a lack of efficacy in using the vaccine to permanently eradicate large established tumors, as will be discussed below.
To determine whether immunization with CPQ could eradicate established tumors, mice were inoculated with TC-1 cells subcutaneously, then vaccinated 2, 4, 6, or 8 days later. Mice were primed with 500 ng E7HHH49–57 at the indicated days, and boosted with the same dose 7 days after the first vaccination. When the vaccine was administered 2, 4 or 6 days after tumor inoculation, tumors were completely eradicated after the boosting vaccination and did not regrow (Figure 8A and Figure 8B). The vaccine extended tumor-free survival to more than 60 days under this observational period (Figure 8C). However, when the first immunization was carried out 8 days after tumor inoculation, the tumor reached a volume as large as 500 mm3 before boosting. After boosting, tumors began drastically shrinking and regressed to a volume of ~100 mm3, detectable 2 weeks after the second vaccination. However, the tumors then started to regrow on day 30 even though ~40% E749–57 specific CD8+ T cells still remained in the blood (Figure 8D), and there were still significantly more TEM cells (Figure 8E) and TCM cells (Figure 8F) in the blood compared to the untreated mice. Also, there was no significant difference of either percent of tet+ or TEM or TCM cells of CD8+ T cells in the blood of mice vaccinated on day 8 compared to mice vaccinated on day 2, 4 or day 6. To understand the poor-function Ag-specific T cells, we compared mice vaccinated with CPQ/E749–57 18- or 40-days post tumor inoculation. There were fewer CD8+ T cells in the tumor on day 40 compared to day 18 (Figure S6A and Figure S6B), and among these CD8+ T cells, a lower percent of CD8+ T cells were Ag-specific on day 40 (Figure S6C). In the spleen, there were less Ag-specific CD8+ cells that were IFN-γ producing in the tumor there were less Ag-specific TEM cells (Figure S6E).
Figure 8. CPQ/E7HHH49–57 immunization eradicates or reverses growth of established TC-1 tumors.

C57BL/6 mice were inoculated with TC-1 cells subcutaneously on day 0 and vaccinated 2, 4, 6, or 8 days later, and boosted 7 days after the prime vaccination. Blood was collected 18 days post tumor inoculation for CD8+ T cell analysis. A) Tumor growth of mice that were vaccinated on different days post-tumor inoculation. B) Tumor growth of individual mice. C) Percentage of mice with tumors smaller than 1 cm following tumor challenge. D) Percentage of E749–57 tet+ cells of CD8+ T cells in the blood. Percentage of TEM cells (E) and TCM cells (F) of CD8+ T cells in the blood. Error bars show mean +/−std. dev. for n=5 per group. * p < 0.05, ** p < 0.01, *** p < 0.001 and **** p < 0.0001, analyzed by (C) long rank test or (D, E) one-way ANOVA with Bonferroni multiple comparisons post-test.
To determine whether vaccinated mice experienced long-lasting protection, two months after the initial tumor challenge, mice with no evidence of tumor growth were re-challenged in the same way as the initial tumor challenge (Figure 9). All mice showed complete resistance to the tumor re-challenge, whereas all mice in the naive group rapidly developed tumors. These results demonstrate that strong memory responses are induced after therapeutic vaccination with CPQ/E7HHH49–57 and tumor challenge. Full protection is achieved from a repeat tumor challenge.
Figure 9. Vaccinated mice are protected from TC-1 tumor re-challenge.

Mice surviving from the tumor challenge studies described in both Figures 6 and 8 were re-challenged with TC-1 cells 2 months after initial challenge. Tumor growth were monitored. Error bars show mean +/−std. dev. for n=5 per group. * p < 0.05 and ** p < 0.01, analyzed by two-way ANOVA with Bonferroni multiple comparisons post-test.
To test the efficacy of CPQ immunization in a metastatic setting, an experimental TC-1 lung metastasis model was established by intravenous injection of tumors cells. Three and 10 days later, mice were immunized with 500 ng E7HHH49–57. Lung nodules were quantified 23 days after the tumor cell injection. In untreated mice or mice receiving the 2HPQ/E7HHH49–57 vaccine, dozens of nodules were observed (Figure 10A). In contrast, nodules were not detectable in mice that were immunized with CPQ/ E7HHH49–57. Control mice or mice injected with 2HPQ/E7HHH49–57 had ~40 lung nodules per mouse but mice immunized with CPQ/E7HHH49–57 did not have any visible evidence of disease (Figure 10B). Lung tumor burden was confirmed by increased lung weight; mice without any treatment or injected with 2HPQ/E7HHH49–57 had heavier lung weights compared to mice immunized with CPQ/E7HHH49–57 (Figure 10C).
Figure 10. CPQ/E7HHH49–57 immunization eradicates lung metastases.

C57BL/6 mice (n=5 per group) were inoculated with TC-1 cells intravenously on day 0 and immunized on day 3 and 10 with 500 ng E7HHH49–57 admixed with CPQ or 2HPQ liposomes. A) Photographs of lungs excised on day 23. B) Count of lung metastasis nodules in indicated treatment groups. C) Lung weights. * p < 0.05, ** p < 0.01 and *** p < 0.001, analyzed by one-way ANOVA with Bonferroni multiple comparisons post-test.
Discussion
In this study, we demonstrated that CPQ liposomes in combination with short peptides represent a convenient platform to screen and identify immunogenic CD8+ T cell epitopes with strong potency. In this study, of 6 epitopes screened, only the previously identified E749–57 epitope was effective. Such a strategy could be adapted for neo-antigen screening or screening of MHC-I epitopes from other tumor-associated Ags.
Liposomal adjuvants can enhance antigen dendritic cell uptake and maturation.[50, 51] The CPQ liposome were effective with the synthetic short peptide E7HHH49–57 instead of SLPs to induce activation signals, such as IL-2[52] and elicit strong IFN-γ and TNF-α associated T cell responses,[53–55] all of which were exclusively CD8+, and not CD4+ T cell-driven. While vaccines containing CD4+ epitopes have advantages and is the basis of vaccine approaches with SLPs, synthetic short peptides may represent a simpler paradigm than SLPs, which make use of activation of multiple epitopes and thereby represent an intermediate-length antigen in between the short CD8+ epitopes and the whole protein target itself from which the peptides are derived.[56]
Poly(I:C), a synthetic agonist of TLR3,[57] was used as a comparator adjuvant. Poly(I:C) has been used with the naked E749–57 epitope in the TC-1 model using short peptides[58] or using long peptides together with a liposomal delivery platform.[54] In our experiments, we used a poly(I:C) dose of 20 μg, whereas prior studies that have used naked peptides used a higher dose of 50 μg.[58] Long peptides have also been used with CpG emulsions.[59] In our study a dose-response comparison of E7HHH49–57 admixed with CPQ or poly(I:C) was assessed with intramuscular vaccination and clearly showed the advantage of CPQ. The route of immunization influences the cell types that can be targets, which is an important determinant for the nature of T cell response.[60] Subcutaneous immunization at the tail base in mice is common in preclinical vaccine studies, whereas we used intramuscular vaccination exclusively. Based on the strong potency of the system, it would be worthwhile to assess various routes of vaccine adminsitration and determine the draining local lymph node response to the vaccine.
Despite the efficacy of the immunization strategy to shrink rapidly growing tumors, regrowth did occur eventually in mice treated with the vaccine 8 days post-tumor implantation. The reasons for this remain clear, but may relate to poor penetration or proximity of T cells in certain portions of the heterogeneous solid tumor; an insufficient number of CD8+ T cells to sustain tumor regression; tumor-induced mechanisms of immunosuppression; or other tumor-intrinsic alterations enabling tumors to evade the immune system. In support of some of these possibilities, it is important to note that the tumors that regrew had lower percentages of CD8+ T cells and antigen-specific CD8+ T cells, indicating that further boosting may be required (Figure S6). Moreover, analysis of tumor-infiltrating CD8+ T cells showed increases in markers of immune exhaustion, PD-1, TIM-3 and LAG-3 expression in the tumor tissue. Finally, the frequency of cytokine producing Ag-specific T cells was lower than expected in the tumor microenvironment (Figure 7G). Overall, together with these observations, this mouse tumor model and vaccine system affords a framework to test the efficacy of combination strategies, such an immune checkpoint inhibitors. In addition to testing the immunization in combination with other treatments, additional toxicity testing and chemical and physical stability studies are warranted for the vaccine.
Conclusion
A liposomal vaccine platform was used to screen potential cancer vaccine epitopes by admixing CPQ with multiple predicted 9-mer MHC-I binding peptides found by sequencing the HPV16 E6/E7 oncogenes. CPQ liposomes effectively induced Ag-specific CD8+ T cell responses and anti-tumor efficacy using the HPV E7HHH49–57 epitope, the only functional one identified from the E6/E7 screen. Immunization with CPQ resulted in rejection of TC-1 tumor challenge in a prophylactic setting, and also eradicated established tumors in multiple local and metastatic therapeutic settings. When mixed with control liposomes (2HPQ) that lacked cobalt, but contained the same QS-21 and MPLA components, the peptide was completely ineffective. A head-to-head comparison revealed the superiority of CPQ compared to the poly(I:C) vaccine adjuvant with respect to CD8+ T cell numbers, activation, and exhaustion states (systemically and within the TME) as well as anti-tumor activities, even at orders of magnitude lower peptide doses, suggesting the CPQ platform is an efficient and powerful tool for in vivo epitope screening of peptide immunogenicity and anti-tumor CD8+ T cell responses across other tumor models and antigen targets. In future work, such a strategy may also be combined with immune checkpoint inhibitors or current HPV vaccine formulations to potentially elicit even greater therapeutic benefits in HPV-derived malignancies or other cancer types.
Materials
E6 and E7 peptides were synthesized by GenScript. E7HHH49–57-HiLyte488 was synthesized by Anaspec. CoPoP was produced as previously described.[43] The following lipids were used: DOPC (Corden; catalog number: LP-R4-070), cholesterol (PhytoChol; Wilshire Technologies), synthetic PHAD-3D6A (Avanti; catalog number: 699855), and QS-21 (Desert King; catalog number: NC0949192). Poly (I:C) was obtained from Sigma (catalog number: P1530). Lysosomes and 10x catabolic buffer were obtained from Xeno tech (catalog numbers: H0610.L and K5200, respectively). The following antibodies were obtained from BioLegend, APC-CD8a antibody (0.2 mg mL−1, catalog number: 100712), FITC-CD4 antibody (0.5 mg mL−1, catalog number: 100405), APC-Cy7-CD44 (0.2 mg mL−1, catalog number: 103027), PE/Cy7-CD62L antibody (0.2 mg mL−1, catalog number: 104417), PerCP-Cy5.5-PD-1 (0.2 mg mL−1, catalog number: 109119), BV605-TIM-3 (0.2 mg mL−1, catalog number: 119721), PE-Cy7-LAG3 (0.2 mg mL−1, catalog number: 125225), pacific blue-IFN-γ (0.5 mg mL−1, catalog number: 505818), BV605-TNF-α (catalog number: 506329), PE-Cy7-IL-2 (0.2 mg mL−1, catalog number: 503821). Other reagents included: Brefeldin A/Golgiplug (BD; catalog number: 555029), Live/Dead dye (Invitrogen; catalog number: L34857), Fc-block (BD; catalog number: 553142). Fixation/permeabilization kit (BD; catalog number: 554714), Cell lysis buffer (BioVision; catalog number: 5830), Collagenase Type I (Gibco; catalog number: 17018-029), and DNase I (Roche Diagnostics; catalog number: 04536282001)
Methods
Vaccine preparation and characterization
Liposomes were prepared by ethanol injection and lipid extrusion as reported previously.[42] Ethanol was removed from prepared liposome by dialyzing in PBS at 4°C, then liposome were passed through a 0.2 μm sterile filter. For CPQ and 2HPQ preparation, QS-21 (1 mg mL−1) was added to liposomes overnight at 4 °C for a [DOPC: Cholesterol: CoPoP/PoP: PHAD: QS-21] mass ratio of [20:5:1:0.4:0.4]. The final liposome concentration was adjusted to 320 μg/mL CoPoP or 2HPoP by dilution in PBS. To prepare CPQ and 2HPQ vaccine, liposome and peptides were incubated at mass ratio of 4:1 for 1 hr at room temperature. For desired Ag dosing, liposomes were first incubated with Ag as described and then diluted in PBS. To prepare the poly(I:C) vaccine, the indicated dose of peptide was mixed with poly (I:C) for 1 hr and diluted in PBS. The dose of poly (I:C) was 20 μg per mouse.
To characterize the binding of peptides to liposomes, peptides were incubated with liposomes or PBS for an hour at room temperature and then subjected to micro-centrifugal filtration tube with a 100 kDa cutoff (PALL; catalog number: 29300) to separate free peptide from liposomes. To determine the concentration of free peptide in the filtrate, micro BCA (Thermo; catalog number: 23235) assays were used. Dynamic light scattering with a NanoBrook 90 plus PALS instrument was used to measure sizes and polydispersity index (PDI) of dilute samples in PBS and zeta potential in water.
To measure fluorescent peptide binding, the fluorescence of the E7HHH49–57-HiLyte488 peptide was monitored was with 491 nm excitation and 527 nm emission in a microplate reader (TECAN Safire). Upon binding to the liposomes, the fluorescence becomes quenched due to energy transfer from HiLyte488 to porphyrin of CPQ or 2HPQ. The percentage binding of peptide was calculated based on the percentage of fluorescence quenching of peptide in the test conditions compared to the free peptide. Binding kinetics were ascertained by monitoring the changes in fluorescence after incubating the same volume of peptide (80 μg mL−1) with liposomes in PBS (320 μg mL−1 CoPoP or 2HPoP) or PBS. Samples were diluted 50 fold prior to measurement in the plate reader. To characterize the serum stability of vaccine, pre-assembled peptide-liposome particles were incubated in 0 or 10 % FBS in PBS at 37 °C (0.8 μg mL−1 peptide concentration) and sample fluorescence was measured directly at different time points. For the in vitro release of peptide in lysosome study, lysosome solutions were prepared as described in the manufacturer instruction. Briefly, in a 96-wells plate, 10 μL 10 × catabolic buffer was mixed with 50 μL of 1 × lysosome mixture and 40 μL water. CPQ/E7HHH49–57-HiLyte488, 2HPQ/E7HHH49–57-HiLyte488 or PBS/E7HHH49–57-HiLyte488 were added to lysosome solution and incubated at 37 °C at a final concentration of 0.8 μg mL−1 peptide. The fluorescence of the mixture was measured at indicated time points.
For cryo-electron microscopy, to analyze the morphology of CPQ liposomes before and after binding of E7HHH49–57 peptide, approximately 3.6 μL of each sample was applied to the holey carbon grids and manually blotted using the Vitrobot blotting paper (Standard Vitrobot Filter Paper, Ø55/20mm, Grade 595). Right after blotting, a new drop of the sample was applied to the EM grid and blotted again using the standard routine with the two blotting pads in the Vitrobot Mark IV (Thermo Fisher Scientific) for 3 sec and a blot force +1. The grid was then immediately plunged into liquid ethane. The Vitrobot was set at 25 °C and 100 % relative humidity. For all samples, we used c-flat grids (C-Flat 2/2-3Cu-T), which were washed with chloroform for 2 hr negative glow discharge in air at 5mA for 15 seconds right before the sample was applied for vitrification. Samples were imaged in a Tecnai F20 electron microscope operated at 200 kV using a side-entry Gatan 626 single tilt cryo-holder. Images were collected in a TVIPS XF416 CMOS camera at a magnification of 50,000x, which produced images with a calibrated pixel size of 2.145Å. Images were collected with a total dose of ~ 10 e−/Å2 using a defocus ranging from −1.75 to − 2.50 μm.
Cell studies
TC-1 cells were kindly provided by Dr. Jorge Gomez-Gutierrez, (University of Louisville, Kentucky, USA) and cultured in Dulbecco’s modified Eagle’s medium (DMEM) with 10% FBS and 1% penicillin/streptomycin (pen/strep). RAW264.7 murine macrophage cells were obtained from the ATCC and cultured in DMEM with 10% fetal bovine serum (FBS) and 1% pen/strep. For splenocyte studies, freshly isolated spleens were dissociated and filtered through a 70 μm cell strainer. The plunger from a sterile 3 mL syringe was used to dissociate tissue through the strainer, and 5 mL of cold PBS was used to wash cells into a 50 mL tube. Cells were centrifuged at 500 × g for 5 min, the supernatants were discarded. Red blood cells were lysed with a 5 mL red blood cell lysis buffer for 5 min, then 35 mL PBS was added to the tube. Cells were centrifuged again and the cell pellets were collected for further use. For tumor infiltrating lymphocyte (TIL) studies, tumor was isolated and cut to 1–2 mm pieces then digested with collagenase Type I (2 mg mL−1) and DNase I (100 μg mL−1) for an hour in the cell culture incubator. Then the plunger from a sterile 3 mL syringe was used to dissociate tumor tissue through the 70 μm strainer, cells were collected and washed for further experiment. PBMCs were prepared by lysing 100 μL of whole blood with 2mL of RBC lysis buffer and washed twice for further use. Splenocytes, TILs and PBMCs were cultured in Roswell Park Memorial Institute (RPMI) 1640 supplemented with 10% FBS, 1% pen/strep, glutamine (2 mM), sodium pyruvate (1 mM), 1x diluted non-essential amino acids solution and β-Mercapethanol (50 μM). Cells were cultured in 5% CO2 / 95% air at 37 °C in a humidified chamber.
For in vitro macrophage cell uptake studies, RAW264.7 cells (2.5 × 105 per well) were cultured in a 24-well plates overnight, then treated with CPQ/E7HHH49–57-HiLyte488, 2HPQ/E7HHH49–57- HiLyte488 and PBS/E7HHH49–57- HiLyte488 (peptide concentration of 1 μg mL−1) for an hour. Cells were washed and lysed with 0.1 % Triton X-100 and dithiothreitol (DTT) (10 mM). The fluorescence signals were measured, and cellular E7HHH49–57- HiLyte488 uptakes were calculated by preparing an E7HHH49–57- HiLyte488 standard curve.
Murine studies
Murine studies were performed according to protocols approved by the University at Buffalo IACUC. 5–6 week-old female C57BL/6 mice (Jackson Laboratory) were intramuscularly immunized with 50 μL vaccine on the right quadriceps. For the prophylactic vaccine tumor model, mice were vaccinated on days 0 and 7, and challenged with 1 × 105 TC-1 cells subcutaneously near the right groin on day 14. For the therapeutic vaccine tumor model, mice were inoculated with 1 × 105 TC-1 tumor subcutaneously near the right groin on day 0, and then vaccinated with indicated vaccine on day 2, 4, 6 or day 8 and then boosted 7 days after the prime vaccination. For the tumor re-challenge study, surviving mice from therapeutic vaccine studies were re-challenged with 1×105 TC-1 cells subcutaneously 60 days after the first tumor challenge. Tumor growth was monitored three times a week and tumor sizes were calculated by equation: Tumor volume = length × width2/2. Animals were euthanized when the tumor size reached 1 cm in diameter or when tumors developed an ulceration. For the experimental lung metastasis tumor model, animals were injected 1×105 TC-1 cells intravenously via tail vein on day 0, then untreated or intramuscular injected with the indicated vaccines on days 3 and 10. Lungs were excised and stained with Bouin’s solution (Sigma; catalog number: HT10132) on day 23. Tumor nodules were counted and lungs were weighed.
Antibody staining
For tetramer staining, immunized mice were analyzed for the percentages of tet+ cells of CD8+ T cells by a tetramer staining assay. H-2Db-restricted E7 (RAHYNIVTF) peptide was complexed with MHC-I (H-2Db) and conjugated with PE (the NIH Tetramer core facility). PBMC from 100 μL of blood or 1 × 106 splenocytes or 5 × 106 tumor infiltrating cells were incubated with the tetramer (500x diluted) for 30 minutes at 4 °C. For T cell phenotyping, antibody mixture of Fc-block (100 × diluted), CD45 (200 × diluted), CD8a (200 × diluted), CD4 (200 × diluted), CD44 (200 × diluted) and CD62L (200 × diluted) were added to cells. For T cell exhaustion study, antibody mixture of Fc-block (100 × diluted), CD45 (200 × diluted), CD8a (200 × diluted), CD4 (200 × diluted), PD-1 (200 × diluted), TIM-3 (200 × diluted) and Lag-3(200 × diluted) were added to cells. Cells were incubated with these antibodies for 30 min at 4 °C, then, washed twice for flow cytometry analysis. Flow cytometry studies were carried out using a BD LSRFortessa™ X-20 cytometer. Flowjo (version 10) software was used for data analysis.
For intracellular staining: PBMCs from 100 μL blood, or 1 × 106 splenocytes, or 5 × 106 tumor infiltrating cells in 100 μL cell culture medium were seeded in a flat bottom 96-wells plate and stimulated with antigen (10 μg mL−1) for 15–18 hours in the cell culture incubator. Then GolgiPlug (Brefeldin A) was added to the wells at the recommended final dilution of 1000 × the stock concentration for another 5 hours. Cells were transferred to a 96-wells round bottom plate and centrifuged at 1350 rpm. Cell pellets were washed twice and stained with E7-tetramer for 30 mins at 4 °C then stained with live/dead fixable dye (500 × diluted), Fc-block (100 × diluted) and the following antibodies against CD45 (200 × diluted), CD8 (200 × diluted) and CD4 (200 × diluted) for 25 mins at 4°C. Cells were fixed, permeabilized according to the manufacture’s instruction. Cells were further stained with antibodies against IFN-γ (200 × diluted), TNF-α (200 × diluted) and IL-2 (200 × diluted) for 30 mins at 4 °C, then washed for flow cytometry.
For immunohistochemistry: Formalin fixed paraffin sections of tumors were cut at 4 μm, placed on charged slides, and dried at 60°C for one hour. Slides were cooled to room temperature and added to the Leica Bond Rx, where they were deparaffinized with Bond Dewax Solution (Leica; catalog: AR9222) and rinsed in water. Bond Epitope Retrieval 2 (Leica; catalog: AR9640) was used for target retrieval for 30 minutes. Slides were blocked using peroxide block from Bond Polymer Refine Detection kit (Leica; catalog: DS9800) for 5 minutes. Slides were incubated with a CD8 antibody (Abcam; catalog: ab209775) for 20 minutes followed by Rabbit Envision (Agilent; catalog: K4003) for 30 minutes. Diaminobenzidine (DAB) from the Bond Polymer Refine Detection kit (Leica; catalog: DS9800) was applied for 10 minutes for visualization. Slides were counterstained with Hematoxylin from the Bond Polymer Refine Detection kit (Leica; catalog: DS9800) for 8 minutes then placed into water. After removing slides from the Bond, they were dehydrated, cleared and cover slipped prior to scanning.
Statistical analysis
Data were analyzed by one- or two-way analysis of variance (ANOVA), followed by Bonferroni post hoc test for comparison of multiple groups or analyzed by Student’s t test for comparison of two groups or analyzed by log-rank test for comparison of percent of mice have tumor sizes smaller than 1 cm with Prism 8 (GraphPad Software). P values less than 0.05 were considered statistically significant. All values are reported as means ± S.D. with the indicated sample size.
Supplementary Material
Acknowledgements
The authors acknowledge assistance from Dr. Prashant Singh from Roswell park with DNA sequencing. This study was supported by the National Institutes of Health grant # R01CA247771 (to both J.F.L. and S.I.A.). Cryo-EM images were collected at the Facility for Electron Microscopy Research (FEMR) at McGill University. FEMR is supported by the Canadian Foundation for Innovation, the Quebec government and McGill University. The NIH Tetramer Core Facility provided MHC-I tetramers.
Footnotes
Competing Interests
J.F.L and W.-C.H. hold interest in POP Biotechnologies. Other authors declare no competing interests.
References
- [1].Zur Hausen H, Virology 1991, 184, 9. [DOI] [PubMed] [Google Scholar]
- [2].Brinton LA, IARC Sci. Publ 1992, 119, 3. [PubMed] [Google Scholar]
- [3].Moody CA, Laimins LA, Nat. Rev. Cancer 2010, 10, 550. [DOI] [PubMed] [Google Scholar]
- [4].Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJ, Peto J, Meijer CJ, Muñoz N, J. Pathol 1999, 189, 12. [DOI] [PubMed] [Google Scholar]
- [5].Kane MA, Cancer Prev. Res 2012, 5, 24. [DOI] [PubMed] [Google Scholar]
- [6].Petrone L, Ammendolia MG, Cesolini A, Caimi S, Superti F, Giorgi C, Di Bonito P, J. Transl. Med 2011, 9, 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Chen L, Thomas EK, Hu S-L, Hellström I, Hellström KE, PNAS 1991, 88, 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Scheffner M, Huibregtse JM, Vierstra RD, Howley PM, Cell 1993, 75, 495. [DOI] [PubMed] [Google Scholar]
- [9].Borysiewicz L, Fiander A, Nimako M, Man S, Wilkinson GWG, Westmoreland D, Evans A, Adams M, Stacey SN, Boursnell M, Lancet 1996, 347, 1523. [DOI] [PubMed] [Google Scholar]
- [10].Kaufmann AM, Stern PL, Rankin EM, Sommer H, Nuessler V, Schneider A, Adams M, Onon TS, Bauknecht T, Wagner U, Clin. Cancer Res 2002, 8, 3676. [PubMed] [Google Scholar]
- [11].Muderspach L, Wilczynski S, Roman L, Bade L, Felix J, Small L, Kast WM, Fascio G, Marty V, Weber J, Clin. Cancer Res 2000, 6, 3406. [PubMed] [Google Scholar]
- [12].Ji H, Chang EY, Lin K-Y, Kurman RJ, Pardoll DM, Wu T-C, Int. J. Cancer 1998, 78, 41. [DOI] [PubMed] [Google Scholar]
- [13].Maciag PC, Radulovic S, Rothman JJV, Vaccine 2009, 27, 3975. [DOI] [PubMed] [Google Scholar]
- [14].Kawana K, Adachi K, Kojima S, Taguchi A, Tomio K, Yamashita A, Nishida H, Nagasaka K, Arimoto T, Yokoyama TJV, Vaccine 2014, 32, 6233. [DOI] [PubMed] [Google Scholar]
- [15].De Jong A, O’Neill T, Khan A, Kwappenberg K, Chisholm S, Whittle N, Dobson J, Jack L, Roberts JSC, Offringa R, Vaccine 2002, 20, 3456. [DOI] [PubMed] [Google Scholar]
- [16].Granadillo M, Vallespi MG, Batte A, Mendoza O, Soria Y, Lugo VM, Torrens I, Vaccine 2011, 29, 920. [DOI] [PubMed] [Google Scholar]
- [17].Kim TJ, Jin H-T, Hur S-Y, Yang HG, Seo YB, Hong SR, Lee C-W, Kim S, Woo J-W, Park KS, Nat. Commun 2014, 5, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Santin AD, Bellone S, Palmieri M, Zanolini A, Ravaggi A, Siegel ER, Roman JJ, Pecorelli S, Cannon MJ, J. Virol 2008, 82, 1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Kenter GG, Welters MJ, Valentijn ARP, Lowik MJ, Berends-van der Meer DM, Vloon AP, Essahsah F, Fathers LM, Offringa R, Drijfhout JW, N. Engl. J. Med 2009, 361, 1838. [DOI] [PubMed] [Google Scholar]
- [20].Ma W, Melief CJ, van der Burg SH, Curr. Opin. Virol 2017, 23, 16. [DOI] [PubMed] [Google Scholar]
- [21].Zwaveling S, Mota SCF, Nouta J, Johnson M, Lipford GB, Offringa R, van der Burg SH, Melief CJ, J. Immunol. Res 2002, 169, 350. [DOI] [PubMed] [Google Scholar]
- [22].Vambutas A, DeVoti J, Nouri M, Drijfhout J, Lipford G, Bonagura V, Van der Burg S, Melief CJV, Vaccine 2005, 23, 5271. [DOI] [PubMed] [Google Scholar]
- [23].Luo M, Wang H, Wang Z, Cai H, Lu Z, Li Y, Du M, Huang G, Wang C, Chen X, Nat. Nanotechnol 2017, 12, 648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Luo M, Liu Z, Zhang X, Han C, Samandi LZ, Dong C, Sumer BD, Lea J, Fu Y-X, Gao J, J. Control Release 2019, 300, 154. [DOI] [PubMed] [Google Scholar]
- [25].Galliverti G, Tichet M, Domingos-Pereira S, Hauert S, Nardelli-Haefliger D, Swartz MA, Hanahan D, Wullschleger S, Cancer Immunol. Res 2018, 6, 1301. [DOI] [PubMed] [Google Scholar]
- [26].Rahimian S, Fransen MF, Kleinovink JW, Christensen JR, Amidi M, Hennink WE, Ossendorp F, J. Control Release 2015, 203, 16. [DOI] [PubMed] [Google Scholar]
- [27].Kenter GG, Welters MJ, Valentijn ARP, Löwik MJ, Berends-van der Meer DM, Vloon AP, Drijfhout JW, Wafelman AR, Oostendorp J, Fleuren GJ, Clin. Cancer Res 2008, 14, 169. [DOI] [PubMed] [Google Scholar]
- [28].He X, Abrams SI, Lovell JF, Adv. Ther 2018, 1, 1800060. [Google Scholar]
- [29].Khong H, Overwijk WW, J. immunother. Cancer 2016, 4, 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Chu X, Li Y, Long Q, Xia Y, Yao Y, Sun W, Huang W, Yang X, Liu C, Ma Y, Int. J. Nanomedicine 2016, 11, 2417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Torréns I, Mendoza O, Batte A, Reyes O, Fernández LE, Mesa C, Guillén G, Vaccine 2005, 23, 5768. [DOI] [PubMed] [Google Scholar]
- [32].Tang J, Yin R, Tian Y, Huang Z, Shi J, Fu X, Wang L, Wu Y, Hao F, Ni B, Vaccine 2012, 30, 1071. [DOI] [PubMed] [Google Scholar]
- [33].Chen W, Huang L, Mol. Pharm 2008, 5, 464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Zhang Y-Q, Tsai Y-C, Monie A, Hung C-F, Wu T-C, Vaccine 2010, 28, 5212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Barrios K, Celis E, Cancer Immunol. Immunother 2012, 61, 1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Wu C-Y, Monie A, Pang X, Hung C-F, Wu T, J. Biomed. Sci 2010, 17, 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Kochenderfer JN, Simpson JL, Chien CD, Gress RE, Blood 2007, 110, 450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Gendron KB, Rodriguez A, Sewell DA, Arch. Otolaryngol. Head Neck Surg 2006, 132, 327. [DOI] [PubMed] [Google Scholar]
- [39].Cho H-I, Barrios K, Lee Y-R, Linowski AK, Celis E, Cancer Immunol. Immunother 2013, 62, 787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Didierlaurent AM, Laupèze B, Di Pasquale A, Hergli N, Collignon C, Garçon N, Expert Rev. Vaccines 2017, 16, 55. [DOI] [PubMed] [Google Scholar]
- [41].Del Giudice G, Rappuoli R, Didierlaurent AM, Semin. Immunol 2018, 39, 14. [DOI] [PubMed] [Google Scholar]
- [42].Huang W-C, Deng B, Lin C, Carter KA, Geng J, Razi A, He X, Chitgupi U, Federizon J, Sun B, Long CA, Ortega J, Dutta S, King CR, Miura K, Lee S-M, Lovell JF, Nat. Nanotechnol 2018, 13, 1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Shao S, Geng J, Ah Yi H, Gogia S, Neelamegham S, Jacobs A, Lovell JF, Nat. Chem 2015, 7, 438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Huang W-C, Deng B, Seffouh A, Ortega J, Long CA, Suresh RV, He X, Miura K, Lee S-M, Wu Y, NPJ vaccines 2020, 5, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Federizon J, Frye A, Huang W-C, Hart TM, He X, Beltran C, Marcinkiewicz AL, Mainprize IL, Wills MK, Lin Y-P, Vaccine 2020, 38, 942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Shao S, Huang W-C, Lin C, Hicar MD, LaBranche CC, Montefiori DC, Lovell JF, Ann. Biomed. Eng 2019, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Andreatta M, Nielsen M, Bioinformatics 2016, 32, 511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Nielsen M, Lundegaard C, Worning P, Lauemøller SL, Lamberth K, Buus S, Brunak S, Lund O, Protein Sci. 2003, 12, 1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Mantegazza AR, Magalhaes JG, Amigorena S, Marks MS, Traffic 2013, 14, 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Joshi MD, Unger WJ, Storm G, Van Kooyk Y, Mastrobattista E, J. Control Release 2012, 161, 25. [DOI] [PubMed] [Google Scholar]
- [51].Fehres CM, Unger WW, Garcia-Vallejo JJ, van Kooyk Y, Front. Immunol 2014, 5, 149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Yang B, Yang A, Peng S, Pang X, Roden RB, Wu T-C, Hung C-F, bioscience, Cell 2015, 5, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Welters MJ, Kenter GG, Van Steenwijk PJDV, Löwik MJ, Berends-van Der Meer DM, Essahsah F, Stynenbosch LF, Vloon AP, Ramwadhdoebe TH, Piersma SJ, PNAS 2010, 107, 11895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Varypataki EM, Benne N, Bouwstra J, Jiskoot W, Ossendorp F, Cancer Immunol. Res 2017, 5, 222. [DOI] [PubMed] [Google Scholar]
- [55].Yang Y, Che Y, Zhao Y, Wang X, Int. Immunopharmacol 2019, 69, 279. [DOI] [PubMed] [Google Scholar]
- [56].van der Burg SH, Arens R, Ossendorp F, van Hall T, Melief CJ, Nat. Rev. Cancer 2016, 16, 219. [DOI] [PubMed] [Google Scholar]
- [57].Alexopoulou L, Holt AC, Medzhitov R, Flavell RA, Nature 2001, 413, 732. [DOI] [PubMed] [Google Scholar]
- [58].Cui Z, Qiu FJCI, Immunotherapy, Cancer Immunol. Immunother 2006, 55, 1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Maynard SK, Marshall JD, MacGill RS, Yu L, Cann JA, Cheng LI, McCarthy MP, Cayatte C, Robbins S. H. J. B. c., BMC cancer 2019, 19, 540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Lesterhuis WJ, de Vries IJM, Schreibelt G, Lambeck AJ, Aarntzen EH, Jacobs JF, Scharenborg NM, van de Rakt MW, de Boer AJ, Croockewit S, Clin. Cancer Res 2011, 17, 5725. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


