Abstract
Although much of the extant research on low-income families has targeted parental depression as the predominant psychological response to economic hardship, the current study examined a range of maternal psychological symptoms that may mediate the relations between early economic pressure and later parenting behaviors. A family stress model was examined using data from 1,142 mothers living in 2 areas of high rural poverty, focusing on the infancy through toddlerhood period. Maternal questionnaires and observations of mother–child interactions were collected across 4 time points (6, 15, 24, and 36 months). Results from structural equation analyses indicated that early economic pressure was significantly related to a variety of symptoms (depression, hostility, anxiety, and somatization), but only depression and somatization were significantly related to decreased levels of sensitive, supportive parenting behaviors. In contrast, anxiety was positively associated with sensitive parenting. Depression and anxiety were both found to mediate the relations between economic pressure and sensitive parenting behaviors. Results further suggest that mothers did not experience change in objective economic hardship over time but did experience a small decrease in economic pressure. Discussion centers on the apparent indirect influence of early economic hardship on later psychological symptoms and parenting behaviors, as well as detailing the need for broader and more complex perspectives on maternal psychological responses that arise as a result of economic disadvantage.
Keywords: parenting, maternal psychological symptoms, economic hardship
Research continues to substantiate the damaging effects of economic hardship for parents and children. With approximately 20% of all families with a child under 18 years of age living below the poverty level in 2009 (U.S. Census Bureau, 2009), understanding the negative consequences of economic problems among families is of crucial importance. Children living in poverty experience significant disadvantages in terms of cognitive development, socioemotional functioning, behavior problems, and physical health (Conger & Donnellan, 2007; McLoyd, 1998). Furthermore, economic hardship affecting parents is associated with psychological distress, marital conflict, and harsh parenting behavior, and these factors are proposed to mediate the relation between poverty and childhood disadvantage (Barnett, 2008; McLoyd, 1998). The extant literature exploring economic disadvantage and parenting has focused largely on parental depression as the distress mediator connecting income and economic pressure with poor child outcomes. The current study aimed to disentangle depression from other psychological symptoms and determine whether particular symptoms are differentially predicted by economic hardship and economic pressure, as well as associated with specific dimensions of parenting behaviors.
The detrimental associations between economic disadvantage and poor outcomes for parents and children are usually not direct, but are instead typically mediated by a number of intervening factors. The family stress model (e.g., Conger et al., 1992; Conger & Elder, 1994) presents a conceptual framework from which to understand the effects of economic hardship, proposing a multitude of family process factors that link economic hardship and child maladjustment. First, objective economic hardship, which may include factors such as low income, debt-to-asset ratio, income loss, and unstable work, influences economic pressure, which is conceptualized as the psychological implication or meaning of economic hardship. High economic pressure leads to increased depressed mood in parents, under the assumption that parents will become “depressed, demoralized, pessimistic about the future, and generally less stable emotionally” (Conger et al., 1992, p. 528). Parental depressed mood is expected to cause marital conflict and withdrawal, which, in turn, leads to hostile or ineffective parenting. Finally, disruptions in parenting behavior affect child well-being and adjustment.
Although some interpretations of the family stress model posit that parents living in poverty may be susceptible to a range of mental health issues beyond depression, including anxiety, anger, antisocial behavior, and substance use (Conger & Donnellan, 2007), the majority of the existing theoretical and empirical work focuses solely on depression or, if not specifically depression, general psychological distress. In actuality, economic hardship is associated with a plethora of chronic and acute stressors, diminishing the ability to cope (McLoyd & Wilson, 1994). The abundance of stressors outside of one’s own control could feasibly bring feelings of hopelessness and, consequently, depressive symptoms. Indeed, there is evidence of depression-specific effects of economic strain (Wadsworth, Raviv, Compas, & Connor-Smith, 2005), and the associations between economic hardship and parental depression are well established.
However, economic hardship could similarly lead to other psychological symptoms in addition to, or in place of, depression as evidenced by findings that those living in poverty are more likely to experience numerous psychological disorders (Bruce, Takeuchi, & Leaf, 1991). For example, the stressors that accompany economic problems may impede anticipated or desired goals and, as proposed by Berkowitz’s (1989) reformulated frustration–aggression hypothesis, may lead a parent to respond with heightened aggression and parental hostility. Furthermore, low-income individuals may experience increased anxiety and somatization, as it is conceivable that parents will react to economic deprivation with worry about finances, job insecurity, and the future (Ladwig, Marten-Mittag, Erazo, & Gündel, 2001). Given the increased medical care visits and medical costs for somaticizing individuals (Barsky, Orav, & Bates, 2005), somatization may be particularly important to understand for those living in poverty, who likely have fewer resources to expend on medical care. In differentiating mental health outcomes associated with economic hardship, Leinonen, Solantaus, and Punamäki (2002) found that both depression and anxiety act as mediators linking economic pressure and marital and parenting processes. In reality, many low-income individuals who experience psychological symptoms may be facing comorbid symptoms or disorders, consistent with the general population (Kessler, Chiu, Demler, Walters, & Merikangas, 2005). Although depression has been indexed as the primary mental health outcome of poverty, there is strong reason to believe that additional psychological symptoms are also predicted by economic hardship.
Given that distinct psychological disorders may follow different courses and have dissimilar outcomes, distinguishing the particular symptoms that arise due to economic disadvantage could have important theoretical and applied implications. For instance, depression can be construed as a chronic and intermittent disorder that has wide-ranging effects on interpersonal relations (Downey & Coyne, 1990), whereas other disorders, such as anxiety or aggression, may have different consequences for the individual and the family. Of particular importance, the value of differentiating parental depression from other psychological symptoms is reflected in the potentially distinct effects that different parental disorders have on children and the family. Maternal depression has vast consequences for children, including greater risk for internalizing and externalizing problems, low social and academic competence, insecure attachment relationships, and general adjustment difficulties (Cummings & Davies, 1994; Downey & Coyne, 1990; Herring & Kaslow, 2002). With respect to specific parenting behaviors, depressed parents exhibit more hostility, coerciveness, and disengagement and less warmth and monitoring (Elgar, Mills, McGrath, Waschbusch, & Brownridge, 2007; Goodman & Gotlib, 1999; Lovejoy, Graczyk, O’Hare, & Neuman, 2000). Furthermore, maternal depression is significantly associated with paternal depression, and the additive effects of depression in both parents may be particularly detrimental for children (Brennan, Hammen, Katz, & Le Brocque, 2002; Burke, 2003).
In addition to parental depression, other parental psychological disorders show important relations to child maladjustment. Children whose mothers have an anxiety disorder have a greater probability of developing an anxiety disorder themselves (Schreier, Wittchen, Höfler, & Lieb, 2008), and children of alcoholics are at risk for developing substance abuse disorders, depression, anxiety, antisocial behaviors, and a number of other difficulties (Harter, 2000). In general, a range of maternal psychiatric symptoms have been linked to negative parenting behaviors (Johnson, Cohen, Kasen, & Brook, 2006). Comorbidity among symptoms may, in fact, provide the greatest risk for children, as mothers who experience depression plus other types of psychopathology are more likely to exhibit adverse play interactions and have an insecure attachment with their infants than are mothers with depression only (Carter, Garrity-Rokous, Chazan-Cohen, Little, & Briggs-Gowan, 2001). Particular maternal psychopathology symptoms may set in motion distinct trajectories for children; thus, disentangling the specific symptoms that are most common among parents with low resources represents an important step in understanding the diverse ways in which children are affected by economic hardship.
Most studies exploring the family stress model use a measure of income or economic hardship from a single time point or averaged across the span of the investigation. But, in reality, family income across childhood may fluctuate (Duncan, Yeung, Brooks-Gunn, & Smith, 1998). Analyses of a nationally representative sample found that families follow different trajectories of poverty (Wagmiller, Lennon, & Kuang, 2008), and changes in income may be most influential in the early childhood period, when increases or decreases in income are most likely to shape the trajectory of childhood (Duncan et al., 1998). Furthermore, changes in the ratio of income to needs are especially influential for children from poor families, wherein decreases in the ratio of income to needs are associated with poorer overall outcomes (Dearing, McCartney, & Taylor, 2001). At the same time, the poorest families have typically been the least likely to experience economic mobility in recent decades (Bradbury & Katz, 2009), suggesting that change in economic conditions might be rare among families living in rural poverty.
Little is known about the ways in which variations in income affect changes in economic pressure, a factor typically thought to bridge income and family outcomes. Nonetheless, changes in levels of both objective economic hardship and subjective economic pressure could alter some of the consequences of poverty. Changes in economic pressure may reflect actual changes in economic hardship, but families may likewise alter the ways in which they deal with poverty across time, leading to changes in economic pressure in the absence of substantial changes in income. Social comparison processes (Parke et al., 2004), as well as the utilization of different strategies to cope with economic difficulties (e.g., creating a budget, getting support from friends; Mistry, Lowe, Benner, & Chien, 2008), could affect levels of economic pressure. Thus, it seems sensible that economic pressure could vary over time, and whether families experience increases, decreases, or stability of either economic hardship or economic pressure could influence the processes delineated by the family stress model.
The present study aimed first to consider the stability or change of economic hardship and economic pressure and second to understand the particular maternal psychological symptoms that are related to earlier levels of economic hardship and later parenting behaviors. To this end, the current study explored families living in poor rural counties of North Carolina and Pennsylvania across a 30-month period. The stability of economic hardship and pressure was examined in an exploratory fashion so as to better understand the nature of poverty in the current sample. It was expected that mothers would experience not only depression but also a range of symptoms in the context of living in poverty, and that each of the psychological symptoms would affect later parenting, perhaps differentially.
Method
Participants
Data for the current study were drawn from the Family Life Project, a longitudinal investigation of families living in areas of high rural poverty. Three counties in central Pennsylvania and three counties in eastern North Carolina were chosen as representative of Appalachia and of African Americans living in the South, respectively (see Vernon-Feagans et al., 2008, for a full description of sampling and recruitment procedures). In the counties chosen, approximately 32% to 48% of children were eligible for free and reduced price lunch (as determined by income adjusted for family size at <180% of the national poverty line), and these children were likely to be spending time in and out of poverty. A stratified random sampling procedure was used to recruit 1,292 families in which the mothers had lived in one of the six counties at the time of the child’s birth. Poverty and, in North Carolina, African American families were oversampled. The family was considered low income if the household income was less than 200% of the national poverty line in 2002, if the mother received any economic social service (e.g., food stamps, WIC, Medicaid), or if she or the head of the household had less than a high school education. Families were recruited in person from hospitals or by phone using birth records every calendar date from September 15, 2003, to September 14, 2004, using a standardized script and screening protocol. Families were told that recruitment targeted mothers giving birth in the hospital, were given information about the study, and were informed of monetary incentives provided for each home visit. Families were excluded if English was not the primary language spoken in the home, if they intended to move out of state in the next 3 years, or if the state had terminated parental rights. Of mothers who were contacted, approximately 70% agreed to participate and approximately 80% of those mothers were formally enrolled in the study. Participating mothers gave written informed consent.
The current study included 1,142 mothers for whom data on the 6-month covariates, plus any of the other key study variables, were available (see Table 1 for demographic characteristics and descriptive statistics for the overall sample, by state). Approximately 38% of families at child age 6 months, 38% of families at child age 15 months, and 34% of families at child age 24 months had a family income at or below the poverty line ($19,806 for a two-parent family with two children under the age of 18, according to the poverty thresholds in 2005). An additional 31% of families at 6 months, 32% of families at 15 months, and 33% of families at 24 months had incomes up to twice the poverty indicator, although it is noteworthy that these low-income families have been found to experience similar levels of economic hardship and difficulties meeting needs as those who fall below the poverty line (Boushey, Brocht, Gundersen, & Bernstein, 2001). At 6 months, data were collected from biological mothers in all cases except 11 (two foster parents, five maternal grandmothers, three paternal grandmothers, and one other adult relative), but primary caregivers are referred to as mothers for the purposes of the current study. Forty percent of mothers were African American, and 49% were married at child age 6 months. Rates of marriage did not change substantially across the course of the present investigation (e.g., 52% of mothers were married at child age 15 months and 53% were married at child age 24 months). Participants with missing data for both of the outcome measurements (i.e., missing at both 24 and 36 months; n = 34) did not differ from participants with complete data on any demographic characteristics or key study variables.
Table 1.
Demographic Characteristics and Descriptive Statistics of Key Variables by State
| Variable | Overall | PA | NC | χ2 or T score | Range |
|---|---|---|---|---|---|
| Demographic characteristics at 6 months | |||||
| Mother married | 42% | 60% | 41% | 38.85* | |
| Mother African American | 41% | 3% | 67% | 443.38* | |
| Mother employed | 53% | 54% | 52% | 0.74 | |
| Maternal age (years) | 26.33 (5.90) | 27.27 (6.00) | 25.66 (5.75) | −4.57* | 14.70–26.33 |
| Maternal education (years) | 14.49 (2.82) | 15.04 (2.88) | 14.10 (2.71) | −5.58* | 6–22 |
| Children in home | 2.20 (1.10) | 2.11 (1.04) | 2.26 (1.14) | 2.29* | 1–8 |
| Key study variables | |||||
| Income-to-needs ratio, 6 months | 1.77 (1.64) | 2.24 (1.93) | 1.43 (1.30) | −7.98* | 0–15.95 |
| Economic pressure, 6 months | 13.74 (4.22) | 12.87 (4.08) | 14.37 (4.22) | 6.01* | 6–26 |
| Income-to-needs ratio, 15 months | 1.78 (1.68) | 2.24 (1.91) | 1.45 (1.40) | −7.60* | 0–16.76 |
| Economic pressure, 15 months | 13.44 (4.17) | 12.61 (3.94) | 14.03 (4.23) | 5.70* | 6–26 |
| Income-to-needs ratio, 24 months | 1.87 (1.72) | 2.34 (2.00) | 1.53 (1.40) | −7.38* | 0–16.76 |
| Economic pressure, 24 months | 13.04 (4.18) | 12.49 (4.17) | 13.45 (4.15) | 3.71* | 6–26 |
| Depression T score, 24 months | 47.30 (8.93) | 47.38 (9.04) | 47.24 (8.86) | −0.26 | 40–81 |
| Somatization T score, 24 months | 48.55 (8.95) | 48.27 (8.77) | 48.75 (9.08) | 0.87 | 41–79 |
| Anxiety T score, 24 months | 46.09 (8.93) | 47.11 (9.15) | 45.32 (8.69) | −3.23* | 38–81 |
| Hostility T score, 24 months | 50.29 (10.63) | 51.66 (9.82) | 49.26 (11.10) | −3.70* | 34–80 |
| Sensitive parenting, 36 months | 3.82 (1.09) | 4.19 (0.96) | 3.54 (1.09) | −10.10* | 1.00–6.4 |
| Harsh parenting, 36 months | 2.88 (1.24) | 2.49 (1.07) | 3.17 (1.28) | 9.29* | 1.00–7.0 |
Note. ns ranged from 1,021 to 1,142 (ns for PA ranged from 432 to 475; ns for NC ranged from 589 to 667). All participants endorsed primary race as African American or White, with the exception of four (0.4%) individuals.
Significant at p < .05.
Procedure
All procedures were approved by the Academic Affairs Institutional Review Board at the University of North Carolina at Chapel Hill. For the current investigation, all procedures were completed when the target child was approximately 6, 15, 24, and 36 months old. Mothers and children participated in 2- to 3-hr home visits at each age, consisting of interviews, questionnaires, child assessments, and observations of mother–child interactions. At 6, 24, and 36 months, two separate visits were conducted within 2 weeks of each other, but only one home visit was conducted at 15 months. All interviews and questionnaires were computerized, with interviewers and respondents entering information into laptop computers. Mothers completed the Kaufman Functional Academic Skills Test literacy screener (Kaufman & Kaufman, 1994) to determine whether they could complete the questionnaires independently. Mothers who read at an eighth-grade reading level or beyond were given the opportunity to complete questionnaires on their own, whereas those who read below an eighth-grade reading level had questionnaires read to them.
At the 6- and 15-month home visits, mothers and children were videotaped for 10 min, during which they were given a set of toys and instructed to play with the child as they normally would if they had free time during the day. At the 24- and 36-month assessment periods, mothers and children were videotaped while engaging in a 10-min puzzle task. Mothers were told that the puzzles were for the child, but they could provide any assistance they thought was necessary. Mothers and children were first given an easy puzzle, and, if they completed the first puzzle, a medium-difficulty puzzle was provided, followed by a difficult puzzle.
Measures
Economic hardship.
Economic hardship was measured by the income-to-needs ratio. At the 6-, 15-, and 24-month assessments, mothers reported income from all sources and any income from other household members. This information was used as an estimate of total household income and was divided by the federal poverty threshold for 2005, which is adjusted for the number of persons in the household, to compute the income-to-needs ratio. An income-to-needs ratio of 1.00 or below indicates that the family income is at or below the poverty line, adjusted for family size. Given nonnormality of the variable, we transformed the income-to-needs ratio using a log10 transformation. The untransformed measure is presented in the descriptive statistics.
Economic pressure.
The Economic Strain Questionnaire (Conger & Elder, 1994) was completed by mothers at 6, 15, and 24 months to capture economic pressure. This measure is a six-item index; two items assess the degree to which families are able to make ends meet (“can’t make ends meet” index) and four items assess the degree to which there is enough money in the household for a home, clothing, food, and medical care (“not enough money” index). The questionnaire was modified from Conger and Elder’s (1994) larger construct of economic pressure. Reliability for the measure was acceptable at 6 (Cronbach’s alpha = .81), 15 (α = .83), and 24 months (α = .84). Exploratory factor analyses indicated that the full six items can be combined to create a global measure of economic pressure, and for the current study, the total score for economic strain was used.
Maternal psychological symptoms.
Maternal symptoms were assessed at child age 24 months using the Brief Symptom Inventory 18 (BSI-18; Derogatis, 2000). The BSI-18 is an 18-item self-report screening index for psychological distress. Items on the BSI-18 are divided equally across three dimensions: depression, anxiety, and somatization. In addition to these 18 items, five items were adopted from the original Brief Symptom Inventory (Derogatis, 1993) to form a Hostility subscale. The measure has been found to be reliable and valid using a large community sample (Derogatis, 2000). In the current sample, reliability was acceptable for each subscale (Depression α = .86, Anxiety α = .82, Somatization α = .79, Hostility α = .81).
Maternal parenting.
Mother–child interactions during the puzzle task at 36 months were videotaped and later coded to assess levels of mothers’ sensitivity, detachment, intrusiveness, positive regard, negative regard, animation, and stimulation of development (Cox, Paley, Burchinal, & Payne, 1999; National Institute of Child Health and Human Development Early Child Care Research Network, 1999). Two trained coders coded each of the ratings on a scale ranging from 1 (not at all characteristic) to 7 (highly characteristic). Based on results of factor analyses conducted with oblique rotation (i.e., Promax), composites were formed based on the two parenting factors that emerged: sensitive, supportive parenting and harsh, controlling parenting. Sensitive, supportive parenting included global sensitivity (level of responsiveness to child’s needs), detachment (reversed; degree to which mother is emotionally uninvolved or disengaged), positive regard (positive feelings toward child), animation (level of energy), and stimulation of development (degree to which mother tries to foster child’s development, achievement, and learning). Harsh, controlling parenting included intrusiveness (degree to which mother imposes own agenda despite child’s cues) and negative regard (harsh, negative feelings expressed toward child). Coding teams had four to five coders, including one or two master coders. Each coder was trained to be reliable with the master coder(s), as well as all other coders. Reliability was determined by calculating the intraclass correlation for ratings made by two coders on approximately 30% of the tapes distributed equally across all coding assignments; reliability across pairs of coders at each time point was maintained at r = .80 or greater for all subscales and composites. Reliability for each subscale was calculated and revised each week to monitor and prevent drift. Coders of the mother–child interactions identified as White, African American, and Asian American, and videos were randomly assigned such that each coder watched and discussed approximately equal numbers of White and African American caregivers.
Data Analytic Plan
The primary research questions were addressed using structural equation modeling (SEM) in Mplus 6.12 (Muthén & Muthén, 2010), which allowed for the complex sampling design (including stratification on income and race and individual probability weights associated with oversampling of low-income and African American families). To address the first aim exploring stability or change in the income-to-needs ratio and economic pressure over time in the current sample, we used latent growth curve modeling (LGCM; McArdle & Epstein, 1987). LGCM uses an SEM framework to create two latent variables to represent the growth curve for each individual: the intercept (mean level) and the slope (rate of change). To address the second aim examining specificity in maternal psychological symptoms, we explored mediated pathways among economic pressure, maternal psychological symptoms, and parenting behaviors, while controlling for the income-to-needs ratio, in a full SEM model. Results from the growth curve analyses were used to determine whether to include the growth curves as a part of the path model or, alternatively, to include the economic variables as observed variables. The models were tested using a robust maximum likelihood estimator. Given the bias associated with likelihood ratio tests with large sample sizes (MacCallum, 1990), we tested overall fit using root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR), and comparative fit index (CFI). Good fit was defined as CFI values ≥ 0.95, RMSEA values ≤ .06, and SRMR values ≤ .08 (Hu & Bentler, 1999). To handle missing data across time points, we used full information maximum likelihood estimation in all analyses (Enders & Bandalos, 2001).
Results
Growth Curve Model Testing
Descriptive statistics (see Table 1) show a slight increase in the income-to-needs ratio and a slight decline in economic pressure from 6 months to 15 months to 24 months. Individual LCGMs were used to evaluate initial levels and rates of change for the income-to-needs ratio and economic pressure, separately. For the income-to-needs ratio growth model, 1,142 mothers were included in the model. The intercept was centered at 6 months, and residual variances for income to needs were constrained across time points. Table 2 shows the parameter estimates and fit statistics for the growth model, which indicate a significant intercept but a nonsignificant slope. For the economic pressure growth model, 1,140 mothers were included in the analyses. The intercept was centered at 15 months, as the full predictive model includes 6-month predictors and 24-month outcomes. Residual variances for economic pressure were constrained across time points. Table 2 shows parameter estimates for the growth model, which indicate a significant intercept and slope. Despite the significant slope estimate, the mean value was small (unstandardized estimate = −.29), and the variance of the slope was not significant, suggesting that there was little variation among individuals in growth of economic pressure over time.
Table 2.
Parameter Estimates for Latent Growth Curve Models of Income-to-Needs Ratio and Economic Pressure
| Model/parameter | Estimate (SE) |
|---|---|
| Income-to-needs ratio: χ2(3) = 1.91, p = .59; CFI = 1.00; RMSEA = .00; SRMR = .01 | |
| Mean intercept | 0.43 (0.01)** |
| Mean slope | 0.00 (0.00) |
| Intercept variance | 0.04 (0.00)** |
| Slope variance | 0.00 (0.00)* |
| Intercept-slope covariance | 0.00 (0.00) |
| Residual variances | 0.01 (0.00)** |
| Economic pressure: χ2(3) = 4.14, p = .25; CFI = 1.00; RMSEA = .02; SRMR = .03 | |
| Mean intercept | 12.96 (0.11)** |
| Mean slope | −0.29 (0.06)** |
| Intercept variance | 10.53 (0.59)** |
| Slope variance | 0.29 (0.28) |
| Intercept-slope covariance | −0.05 (0.22) |
| Residual variances | 6.77 (0.45)** |
Note. Unstandardized parameter estimates shown for individual growth models. Income-to-needs ratio transformed with a log transformation. Income-to-needs ratio centered at 6 months, and economic strain centered at 15 months. Residual variances of income-to-needs ratio at 6, 15, and 24 months constrained to be equal, as were residual variances of economic pressure at 6, 15, and 24 months (separately). CFI = comparative fit index; RMSEA = root mean square error of approximation; SRMR = standardized root mean residual.
p < .05.
p < .001.
Given that there was no significant growth in the income-to-needs ratio and little growth, with no significant variance in economic pressure, both the income-to-needs ratio and the economic pressure growth curves were trimmed from the subsequent path analyses and replaced with observed variables to create a simpler model.
Initial Analyses of the Full Model
The second aim of the study was to examine aspects of the family stress model, including a range of maternal psychological symptoms, to determine whether depression is the key psychological outcome associated with economic hardship. Descriptive statistics for all variables are shown in Table 1, and correlations among the variables are presented in Table 3. Geographic region (Pennsylvania coded as 1, North Carolina coded as 0), race (African American coded as 1, others coded as 0), age, education, and marital status (married coded as 1) were covaried in the analyses, given the significant correlations among the variables of interest.
Table 3.
Correlation Table of Key Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | State (PA = 1) | — | −.64* | .14* | .17* | .19* | .24* | −.18* | .23* | −.17* | .23* | −.11* | .01 | −.03 | .10* | .11* | .30* | −.27* |
| 2. | Mother African American | — | −.19* | −.22* | −.36* | −.37* | .17* | −.34* | .18* | −.32* | .13* | .08* | .13* | −.05 | −.06 | −.40* | .36* | |
| 3. | Mother age | — | .49* | .46* | .37* | −.04 | .35* | .01 | .36* | .04 | −.08* | −.14* | .02 | .00 | .35* | −.20* | ||
| 4. | Maternal education | — | .46* | .52* | −.22* | .50* | −.20* | .53* | −.21* | −.18* | −.23* | −.11* | −.06 | .43* | −.33* | |||
| 5. | Mother married | — | .48* | −.19* | .43* | −.16* | .44* | −.14* | −.13* | −.16* | −.04 | .01 | .39* | −.31* | ||||
| 6. | Income-to-needs ratio, 6 months | — | −.32* | .79* | −.32* | .80* | −.30* | −.16* | −.17* | −.05 | −.04 | .37* | −.27* | |||||
| 7. | Economic pressure, 6 months | — | −.30* | .56* | −.32* | .56* | .29* | .23* | .23* | .18* | −.18* | .08* | ||||||
| 8. | Income-to-needs ratio, 15 months | — | −.33* | .80* | −.31* | −.14* | −.16* | −.04 | −.02 | .36* | −.24* | |||||||
| 9. | Economic pressure, 15 months | — | −.33* | .62* | .30* | .22* | .23* | .19* | −.18* | .12* | ||||||||
| 10. | Income-to-needs ratio, 24 months | — | −.34* | −.15* | −.16* | −.04 | .02 | .36* | −.25* | |||||||||
| 11. | Economic pressure, 24 months | — | .34* | .28* | .30* | .25* | −.17* | .11* | ||||||||||
| 12. | Depression T score, 24 months | — | .57* | .70* | .60* | −.13* | .12* | |||||||||||
| 13. | Somatization T score, 24 months | — | .59* | .48* | −.18* | .14* | ||||||||||||
| 14. | Anxiety T score, 24 months | — | .67* | −.01 | .01 | |||||||||||||
| 15. | Hostility T score, 24 months | — | .02 | .00 | ||||||||||||||
| 16. | Sensitive parenting, 36 months | — | −.50* | |||||||||||||||
| 17. | Harsh parenting, 36 months | — |
Note. Pairwise deletion was used; ns ranged from 965 to 1,142.
Significant at p < .05.
Before examining the full model, we explored the data to ensure that we had created appropriate models. It is possible that nonlinear relations exist between the variables in the model, such that stronger associations may exist between the income-to-needs ratio and parenting behaviors at lower levels of income to needs. We examined scatterplots between both the economic hardship and economic pressure variables and the family process variables to assess fit with linear, quadratic, and lowess lines. The nature of the relations between the variables appeared linear for all of the scatterplots; moreover, quadratic fit lines did not account for substantially more of the variability than did linear fit lines. Consequently, all further analyses consider only the linear relations between the variables.
The comorbidity of depression with other symptoms also presented a challenge. If, in fact, most mothers experience comorbidities of other symptoms with depression, it may be unnecessary to disentangle depression from the other potential psychological consequences of economic hardship. Thus, we created cutoff scores at a T score of 60 (slightly below the clinical cutoff of 65 to include more mothers with somewhat elevated scores) to examine rates of psychological distress in this population. Although most (73.7%) mothers experienced no elevated symptoms, 15.9% (n = 168) experienced elevated psychological symptoms (anxiety, somatization, and/or hostility) without elevated depression scores, most of whom (75%) reported elevated symptoms on only one type of distress. Only 1.3% (n = 14) of mothers reported only elevated symptoms of depression, and 9% (n = 95) experienced depressive symptoms plus other psychological symptom(s). Thus, given that the highest proportion of those experiencing elevated psychological symptoms did not report symptoms of depression, it appeared possible to disentangle depression from other psychological symptoms. Psychological symptoms were used as continuous variables in the later analyses.
Full Model Tests
The full SEM included interrelations among income-to-needs ratio at 6 months, economic pressure at 15 months, maternal psychological symptoms at 24 months, and parenting behaviors at 36 months, as well as direct paths from the income-to-needs ratio to psychological symptoms and to parenting behaviors so as to control for levels of objective economic hardship. Covariances between each of the symptoms were estimated (data not shown). In addition, direct paths were included between each of the covariates and the exogenous variables in the model (data not shown); the significant coefficients for the covariates are shown in Table 4. All other parameter estimates are also shown in Table 4. The model, shown in Figure 1, provided a good fit to the data: χ2(2) = 3.92, p = .14; CFI = 1.00; RMSEA = .03; SRMR = .01. Nonsignificant paths are not shown in the figure for readability. Path coefficients indicate a significant negative relation between the income-to-needs ratio and economic pressure at 15 months. Furthermore, higher levels of economic pressure were significantly related to higher levels of all maternal psychological symptoms. Although all symptoms were associated with previous levels of economic pressure, only depression, somatization, and anxiety showed links to parenting behaviors, after controlling for the set of covariates and including the covariances among each of the other symptoms. Greater levels of both depression and somatization were significantly associated with lower levels of sensitive, supportive parenting, whereas, contrary to expectation, more anxiety was significantly related to higher levels of sensitive, supportive parenting. Furthermore, after controlling for the demographic covariates, none of the symptom presentations was related to harsh, controlling parenting.
Table 4.
Parameter Estimates for the Full Structural Equation Model
| Parameter | β | B (SE) |
|---|---|---|
| INR, 6 months → economic pressure, 15 months | −.32** | −5.77 (0.78) |
| INR, 6 months → depression, 24 months | .00 | 0.12(1.67) |
| INR, 6 months → somatization, 24 months | −.00 | −0.16 (1.67) |
| INR, 6 months → anxiety, 24 months | .05 | 1.92 (1.79) |
| INR, 6 months → hostility, 24 months | .00 | 0.07 (2.09) |
| INR, 6 months → sensitive parenting, 36 months | .04 | 0.17 (0.18) |
| INR, 6 months → harsh parenting, 36 months | .00 | −0.00 (0.19) |
| Economic pressure, 15 months → depression, 24 months | .27** | 0.58 (0.08) |
| Economic pressure, 15 months → somatization, 24 months | .18** | 0.39 (0.07) |
| Economic pressure, 15 months → anxiety, 24 months | .25** | 0.53 (0.09) |
| Economic pressure, 15 months → hostility, 24 months | .21** | 0.51 (0.09) |
| Depression, 24 months → sensitive parenting, 36 months | −.10* | −0.01 (0.01) |
| Depression, 24 months → harsh parenting, 36 months | .07 | 0.01 (0.01) |
| Somatization, 24 months → sensitive parenting, 36 months | −.08* | −0.01 (0.01) |
| Somatization, 24 months → harsh parenting, 36 months | .03 | 0.00 (0.01) |
| Anxiety, 24 months → sensitive parenting, 36 months | .11* | 0.01 (0.01) |
| Anxiety, 24 months → harsh parenting, 36 months | −.05 | −0.01 (0.01) |
| Hostility, 24 months → sensitive parenting, 36 months | .03 | 0.00 (0.00) |
| Hostility, 24 months → harsh parenting, 36 months | −.03 | 0.00 (0.01) |
| State → economic pressure, 15 months | −.11* | −0.92 (0.32) |
| State → depression, 24 months | .13* | 2.28 (0.68) |
| State → somatization, 24 months | .10* | 1.70 (0.64) |
| State → anxiety, 24 months | .14** | 2.56 (0.67) |
| State → hostility, 24 months | .15** | 3.15 (0.86) |
| Mother AA → depression, 24 months | .08* | 1.78 (0.83) |
| Mother AA → somatization, 24 months | .09* | 1.87 (0.79) |
| Mother AA → sensitive parenting, 36 months | −.17** | −0.44 (0.11) |
| Mother AA → harsh parenting, 36 months | .20** | 0.56 (0.11) |
| Mother age → economic pressure, 15 months | .16** | 0.11 (0.03) |
| Mother age → sensitive parenting, 36 months | .10* | 0.02 (0.01) |
| Maternal education → economic pressure, 15 months | −.12* | −0.17 (0.07) |
| Maternal education → depression, 24 months | −.12* | −0.36 (0.14) |
| Maternal education → somatization, 24 months | −.13* | −0.40 (0.13) |
| Maternal education → anxiety, 24 months | −.09* | −0.28 (0.15) |
| Maternal education → sensitive parenting, 36 months | .25** | 0.09 (0.01) |
| Maternal education → harsh parenting, 36 months | −.22** | −0.09 (0.02) |
| Mother married → sensitive parenting, 36 months | .11* | 0.24 (0.08) |
| Mother married → harsh parenting, 36 months | −.12* | −0.27 (0.09) |
| Covariances | ||
| Depression with somatization | .51** | 35.09 (3.47) |
| Depression with anxiety | .68** | 48.36 (3.78) |
| Depression with hostility | .58** | 48.16 (3.53) |
| Somatization with anxiety | .58** | 40.97 (3.47) |
| Somatization with hostility | .44** | 36.54 (3.34) |
| Anxiety with hostility | .64** | 54.15 (3.47) |
| Sensitive parenting with harsh parenting | −.36** | −0.33 (0.03) |
Note. INR = income-to-needs ratio; AA = African American. Only significant path coefficients for covariates (state, race, age, education, and marital status) are shown.
p < .05.
p < .001.
Figure 1.
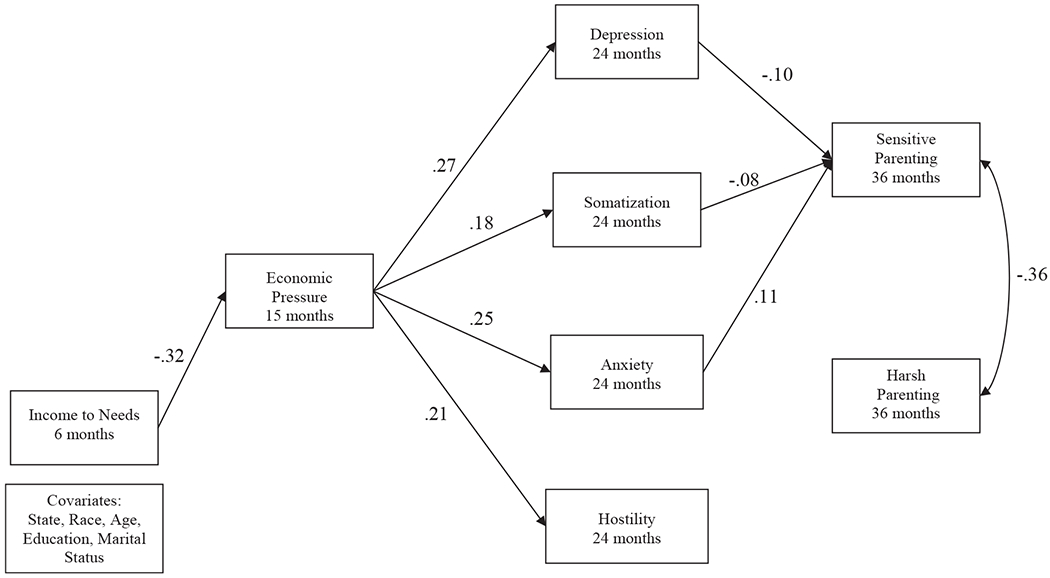
Path model of relations between economic hardship, economic pressure, symptoms, and parenting. Numbers indicate standardized path coefficients. Only significant paths are shown for ease of readability. Direct paths were included from all covariates to all exogenous variables in the model, but are not shown. Covariances among psychological symptoms are not shown. Model provides an acceptable fit to the data: χ2(2) = 3.92, p = .14; comparative fit index = 1.00; root mean square error of approximation = .03; standardized root mean residual = .01.
Mediated pathways from economic pressure to parenting behaviors through psychological symptoms were tested using the delta method for estimating indirect effects in Mplus. Results indicate that the relation between economic pressure and maternal sensitive parenting was significantly mediated by depression, with a standardized estimate of the indirect effect of −.03, p < .05, as well as by anxiety, with a standardized estimate of the indirect effect of .03, p < .05. In contrast, somatization did not significantly mediate the relation between economic pressure and sensitive parenting (standardized estimate = −.01, p = .07).
Discussion
Process models of economic disadvantage imply a depression-specific response to economic hardship, with parental depression proposed to mediate the relations between economic hardship and poor child functioning. The current study, in contrast, highlights the range of maternal psychological symptoms that are associated with economic hardship and its resultant pressure. Nonetheless, and despite the measurable variation in psychological distress, maternal depression and somatization may be the most influential predictors of later sensitive parenting behaviors. The results support a portion of the family stress model, while also suggesting the need for broader conceptualizations of maternal psychological well-being that result from low-resource contexts.
Although income was stable, on average, across the 18-month time period, families experienced a slight decrease in economic pressure. Individuals living in rural areas, exemplified by mothers in the current sample, may experience higher rates of long-term or persistent poverty than those living in urban areas (Adams & Duncan, 1992; Weber, Jensen, Miller, Mosley, & Fisher, 2005). In addition, there are a greater proportion of low-skill jobs in rural areas, such that individuals may experience particular difficulty gaining jobs that would provide economic security (Gibbs, Kusmin, & Cromartie, 2005). The dynamics of rurality may create especially risky conditions for families facing economic hardship. Despite increased prevalence of mental health concerns, those living in rural poverty hold a greater stigma toward seeking mental health services (Hoyt, Conger, Valde, & Weihs, 1997). As children living in persistent poverty experience the most adverse outcomes (Brooks-Gunn & Duncan, 1997), understanding the effects of economic disadvantage on parental symptomatology and child development among those living in more rural areas of America becomes even more critical.
Economic hardship and pressure largely produce an indirect influence on parents and children through the effects on parental symptomatology. Consistent with previous research on the family stress model (Conger et al., 1992; Mistry et al., 2008), we found associations among economic hardship, economic pressure, psychological symptoms, and parenting behavior. Notably, mothers experience not only depressive symptoms as a response to economic hardship, but also increased anxiety, somatization, and hostility, expanding support for diffusion among psychological symptoms beyond depression that may be associated with income level (Leinonen et al., 2002; Wadsworth et al., 2005). Mothers may feel worried about finances and angry about a perceived lack of ability to achieve goals, in addition to feeling hopeless or sad. The economic costs of somatization (Barsky et al., 2005), in particular, might be neglected in a depression-specific model of hardship. Moreover, rates of psychological symptoms may be even higher than the self-report measures would suggest given the possibility for underreporting of symptoms in less educated populations (Enns, Larsen, & Cox, 2000). Regardless, symptom diffusion encourages the expansion of current models and broadens working assumptions to reflect the breadth of psychological impact resulting from economic hardship.
Economic hardship appears to create a context in which mothers are less sensitive with their children. Indeed, our findings indicate that economic factors affect parenting through a complex pathway of influence whereby objective economic hardship produces higher levels of economic pressure, which is associated with greater maternal feelings of depression, somatization, and anxiety, which in turn affect parenting behaviors. These pathways not only reflect important process determinants of parenting (Belsky & Jaffee, 2006), but may also produce even broader influences on the family as maternal mood and decreased quality of the mother–child relationship may spillover to the marital and father–child relationship (Erel & Burman, 1995). Specific, albeit differential, relations emerged for depressive, somaticizing, and anxious symptoms with sensitive, supportive parenting, indicating that these particular aspects of maternal well-being may be most influential for families under conditions of economic hardship.
Maternal depression is a well-established risk factor for adverse developmental outcomes, and poor parenting behaviors and parent–child interactions are the key mechanisms through which depression affects children (Cummings & Davies, 1994; Goodman & Gotlib, 1999). Evidence continues to accrue that mothers living in poor economic conditions exhibit fewer positive parenting behaviors than nondepressed mothers or mothers who are not economically disadvantaged (Lovejoy et al., 2000). Similar results were found in a study of family stress and mental health symptoms among parents experiencing economic hardship, wherein maternal depression was related to less authoritative parenting but was not related to harsh, negative parenting behaviors (Leinonen et al., 2002). Still, maternal depression typically shows links to negative parenting behaviors, but it may be that the negative interaction style between mothers and young children is due to comorbidities among psychological symptoms rather than depression alone (Carter et al., 2001). Thus, considering the effect of each symptom individually suggests that the specific symptoms of depression, including withdrawal, decreased energy, and helplessness, are more likely to decrease sensitive, involved, and supportive parenting, whereas comorbidities may account for the link between depression and harsh, intrusive, negative parenting. Whereas maternal depression has captured strong research interest, somewhat less is known about the effects of maternal somatization on parenting and child functioning. A recent observational study found that somaticizing mothers were less responsive, expressed less praise toward their children, and exhibited fewer instances of joint attention than healthy mothers or mothers with a known medical condition (Craig, Bialas, Hodson, & Cox, 2004). These results provide further evidence that sensitive maternal behavior is multiply determined, and psychological implications extend beyond the putative effects of depression.
Conceptual and empirical evidence suggests that maternal anxiety creates risk for poor parenting, with anxious mothers exhibiting less warmth and more control, although some of these negative parenting behaviors may be displayed more in response to child anxiety (Wood, McLeod, Sigman, Hwang, & Chu, 2003). In contrast, our results suggest that higher levels of maternal anxiety are associated with more sensitive, supportive parenting. Although counterintuitive, most mothers in our sample had relatively low levels of anxiety, and the effects of other psychological symptoms were included separately in the analyses. In the absence of comorbid depressive symptoms, low levels of maternal anxiety may actually lead to increased vigilance and responsivity in parenting and not the hostility and negativity typical of more diffuse distress. In addition, as most evidence for the family stress model examines general psychological distress rather than extracting different symptoms, it may mask important specificity of effect between types of psychological distress and key parenting attributes. Still, given the counterintuitive nature of this finding, such interpretations merit further scrutiny in research.
Several limitations should be noted when interpreting the results. First, the relations in the current investigation assume a particular direction of effect. However, it is possible that the links are spurious, and psychological distress could lead to poverty or mothers with more distress could view their economic conditions more negatively (Duncan et al., 1998). Although we controlled for important demographic characteristics that could influence symptomatology and parenting behaviors, the possibility for alternative directionality should be considered. Second, although the present study provides extensive information on family processes among mothers living in poverty, fathers were not included in the analyses. The role of fathers is understudied, particularly among families in poverty (Coley, 2001), and it is likely that the mental health symptoms and parenting behaviors associated with economic hardship are different for fathers than for mothers (Leinonen et al., 2002). Third, the current sample includes a large, representative sample of families in rural communities in the South and Appalachia, but the results may not be generalizable to all families exposed to economic hardship. However, the family stress model has been substantiated in families living in urban and rural poverty in a variety of geographical regions, providing reason to believe that the current results are representative of many families. Finally, psychological symptoms were considered along a continuum rather than including only levels of clinical significance. This approach does not allow us to fully disentangle particular disorders or comorbidities experienced by mothers in the sample or determine whether clinical thresholds may operate differently in relation to economic hardship and parenting.
Economic hardship is associated with adverse outcomes in both parents and children, and the family stress model has provided the foundation for much of our current understanding. By identifying mediating factors that help explain the associations between economic hardship and parenting, we expand this model to further represent the complexity of the mechanisms in play. The range of maternal psychological symptoms that arise in response to economic hardship brings question to the utility of a depression-specific process model of poverty, although maternal depression has powerful implications for parenting and subsequent child and family functioning. Expanded developmental perspectives must extend the study of families into later developmental periods with a focus on the mechanisms through which low-income conditions affect families as they age.
Acknowledgments
Support for this research was provided by National Institute of Child Health and Human Development Grant P01-HD-039667, with cofunding from the National Institute on Drug Abuse.
Contributor Information
Rebecca P. Newland, Department of Psychology, Arizona State University
Keith A. Crnic, Department of Psychology, Arizona State University
Martha J. Cox, Department of Psychology, University of North Carolina at Chapel Hill
W. Roger Mills-Koonce, Department of Psychology, University of North Carolina at Chapel Hill.
References
- Adams TK, & Duncan GJ (1992). Long-term poverty in rural areas. In Duncan CM (Ed.), Rural poverty in America (pp. 63–96). New York, NY: Auburn House. [Google Scholar]
- Barnett MA (2008). Economic disadvantage in complex family systems: Expansion of family stress models. Clinical Child and Family Psychology Review, 11, 145–161. doi: 10.1007/s10567-008-0034-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barsky AJ, Orav EJ, & Bates DW (2005). Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Archives of General Psychiatry, 62, 903–910. doi: 10.1001/archpsyc.62.8.903 [DOI] [PubMed] [Google Scholar]
- Belsky J, & Jaffee S (2006). The multiple determinants of parenting. In Cicchetti D & Cohen DJ (Eds.), Developmental psychopathology: Vol. 3. Risk, disorder, and adaptation (2nd ed., pp. 38–85). New York, NY: Wiley. [Google Scholar]
- Berkowitz L (1989). Frustration-aggression hypothesis: Examination and reformulation. Psychological Bulletin, 106, 59–73. doi: 10.1037/0033-2909.106.1.59 [DOI] [PubMed] [Google Scholar]
- Boushey H, Brocht C, Gundersen B, & Bernstein J (2001). Hardships in America: The real story of working families. Washington, DC: Economic Policy Institute. [Google Scholar]
- Bradbury K, & Katz J (2009). Trends in U.S. family income mobility, 1967–2004 (Working Paper No. 09–7). Boston, MA: Federal Reserve Bank of Boston. [Google Scholar]
- Brennan PA, Hammen C, Katz AR, & Le Brocque RM (2002). Maternal depression, paternal psychopathology, and adolescent diagnostic outcomes. Journal of Consulting and Clinical Psychology, 70, 1075–1085. doi: 10.1037/0022-006X.70.5.1075 [DOI] [PubMed] [Google Scholar]
- Brooks-Gunn J, & Duncan GT (1997). The effects of poverty on children. The Future of Children, 7, 55–71. doi: 10.2307/1602387 [DOI] [PubMed] [Google Scholar]
- Bruce ML, Takeuchi DT, & Leaf PJ (1991). Poverty and psychiatric status: Longitudinal evidence from the New Haven Epidemiologic Catchment Area Study. Archives of General Psychiatry, 48, 470–474. doi: 10.1001/archpsyc.1991.01810290082015 [DOI] [PubMed] [Google Scholar]
- Burke L (2003). The impact of maternal depression on familial relationships. International Review of Psychiatry, 15, 243–255. doi: 10.1080/0954026031000136866 [DOI] [PubMed] [Google Scholar]
- Carter AS, Garrity-Rokous FE, Chazan-Cohen R, Little C, & Briggs-Gowan MJ (2001). Maternal depression and comorbidity: Predicting early parenting, attachment security, and toddler social–emotional problems and competencies. Journal of the American Academy of Child & Adolescent Psychiatry, 40, 18–26. doi: 10.1097/00004583-200101000-00012 [DOI] [PubMed] [Google Scholar]
- Coley RL (2001). (In)visible men: Emerging research on low-income, unmarried, and minority fathers. American Psychologist, 56, 743–753. doi: 10.1037/0003-066X.56.9.743 [DOI] [PubMed] [Google Scholar]
- Conger RD, Conger KJ, Elder GH Jr., Lorenz FO, Simons RL, & Whitbeck LB (1992). A family process model of economic hardship and adjustment of early adolescent boys. Child Development, 63, 526–541. doi: 10.2307/1131344 [DOI] [PubMed] [Google Scholar]
- Conger RD, & Donnellan MB (2007). An interactionist perspective on the socioeconomic context of human development. Annual Review of Psychology, 58, 175–199. doi: 10.1146/annurev.psych.58.110405.085551 [DOI] [PubMed] [Google Scholar]
- Conger RD, & Elder GH Jr. (1994). Families in troubled times: Adapting to change in rural America. New York, NY: De Gruyter Aldine. [Google Scholar]
- Cox MJ, Paley B, Burchinal M, & Payne CC (1999). Marital perceptions and interactions across the transition to parenthood. Journal of Marriage and the Family, 61, 611–625. doi: 10.2307/353564 [DOI] [Google Scholar]
- Craig TKJ, Bialas I, Hodson S, & Cox AD (2004). Intergenerational transmission of somatization behaviour: 2. Observations of joint attention and bids for attention. Psychological Medicine, 34, 199–209. doi: 10.1017/S0033291703001120 [DOI] [PubMed] [Google Scholar]
- Cummings EM, & Davies PT (1994). Maternal depression and child development. Journal of Child Psychology and Psychiatry, 35, 73–112. doi: 10.1111/j.1469-7610.1994.tb01133.x [DOI] [PubMed] [Google Scholar]
- Dearing E, McCartney K, & Taylor BA (2001). Change in family income-to-needs matters more for children with less. Child Development, 72, 1779–1793. doi: 10.1111/1467-8624.00378 [DOI] [PubMed] [Google Scholar]
- Derogatis LR (1993). Brief Symptom Inventory: Administration, scoring, and procedures manual. Minneapolis, MN: National Computer Systems. [Google Scholar]
- Derogatis LR (2000). Brief Symptom Inventory 18: Administration, scoring, and procedures manual. Minneapolis, MN: National Computer Systems. [Google Scholar]
- Downey G, & Coyne JC (1990). Children of depressed parents: An integrative review. Psychological Bulletin, 108, 50–76. doi: 10.1037/0033-2909.108.1.50 [DOI] [PubMed] [Google Scholar]
- Duncan GJ, Yeung WJ, Brooks-Gunn J, & Smith JR (1998). How much does childhood poverty affect the life chances of children? American Sociological Review, 63, 406–423. doi: 10.2307/2657556 [DOI] [Google Scholar]
- Elgar FJ, Mills RS, McGrath PJ, Waschbusch DA, & Brownridge DA (2007). Maternal and paternal depressive symptoms and child maladjustment: The mediating role of parental behavior. Journal of Abnormal Child Psychology, 35, 943–955. doi: 10.1007/s10802-007-9145-0 [DOI] [PubMed] [Google Scholar]
- Enders CK, & Bandalos DL (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling, 8, 430–457. doi: 10.1207/S15328007SEM0803_5 [DOI] [Google Scholar]
- Enns MW, Larsen D, & Cox BJ (2000). Discrepancies between self and observer ratings of depression: The relationship to demographic, clinical and personality variables. Journal of Affective Disorders, 60, 33–41. doi: 10.1016/S0165-0327(99)00156-1 [DOI] [PubMed] [Google Scholar]
- Erel O, & Burman B (1995). Interrelatedness of marital relations and parent–child relations: A meta-analytic review. Psychological Bulletin, 118, 108–132. doi: 10.1037/0033-2909.118.1.108 [DOI] [PubMed] [Google Scholar]
- Gibbs R, Kusmin L, & Cromartie J (2005). Low-skill employment and the changing economy of rural America (Economic Research Report No. 10). Washington, DC: U. S. Department of Agriculture. [Google Scholar]
- Goodman SH, & Gotlib IH (1999). Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review, 106, 458–490. doi: 10.1037/0033-295X.106.3.458 [DOI] [PubMed] [Google Scholar]
- Harter SL (2000). Psychosocial adjustment of adult children of alcoholics: A review of the recent empirical literature. Clinical Psychology Review, 20, 311–337. doi: 10.1016/S0272-7358(98)00084-1 [DOI] [PubMed] [Google Scholar]
- Herring M, & Kaslow NJ (2002). Depression and attachment in families: A child-focused perspective. Family Process, 41, 494–518. doi: 10.1111/j.1545-5300.2002.41313.x [DOI] [PubMed] [Google Scholar]
- Hoyt DR, Conger RD, Valde JG, & Weihs K (1997). Psychological distress and help seeking in rural America. American Journal of Community Psychology, 25, 449–470. doi: 10.1023/A:1024655521619 [DOI] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional versus new alternatives. Structural Equation Modeling, 6, 1–55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, & Brook JS (2006). Maternal psychiatric disorders, parenting, and maternal behavior in the home during the child rearing years. Journal of Child and Family Studies, 15, 96–113. doi: 10.1007/s10826-005-9003-z [DOI] [Google Scholar]
- Kaufman AS, & Kaufman NL (1994). K-FAST: Kaufman functional academic skills test. Toronto, ON, Canada: PSYCAN. [Google Scholar]
- Kessler RC, Chiu W-T, Demler O, Walters EE, & Merikangas KR (2005). Prevalence, severity, and comorbidity of 12-month DSM–IV disorders in the National Comorbidity Replication. Archives of General Psychiatry, 62, 617–627. doi: 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladwig K-H, Marten-Mittag B, Erazo N, & Gündel H (2001). Identifying somatization disorder in a population-based health examination survey: Psychosocial burden and gender differences. Psychosomatics, 42, 511–518. doi: 10.1176/appi.psy.42.6.511 [DOI] [PubMed] [Google Scholar]
- Leinonen JA, Solantaus TS, & Punamäki RL (2002). The specific mediating paths between economic hardship and the quality of parenting. International Journal of Behavioral Development, 26, 423–435. doi: 10.1080/01650250143000364 [DOI] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, & Neuman G (2000). Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review, 20, 561–592. doi: 10.1016/S0272-7358(98)00100-7 [DOI] [PubMed] [Google Scholar]
- MacCallum RC (1990). The need for alternative measures of fit in covariance structure modeling. Multivariate Behavioral Research, 25, 157–162. doi: 10.1207/s15327906mbr2502_2 [DOI] [PubMed] [Google Scholar]
- McArdle JJ, & Epstein D (1987). Latent growth curves within developmental structural equation models. Child Development, 58, 110–133. doi: 10.2307/1130295 [DOI] [PubMed] [Google Scholar]
- McLoyd VC (1998). Socioeconomic disadvantage and child development. American Psychologist, 53, 185–204. doi: 10.1037/0003-066X.53.2.185 [DOI] [PubMed] [Google Scholar]
- McLoyd VC, & Wilson L (1994). The strain of living poor: Parenting, social support, and child mental health. In Huston AC (Ed.), Children in poverty: Child development and public policy (pp. 105–135). Cambridge, UK: Cambridge University Press. [Google Scholar]
- Mistry RS, Lowe ED, Benner AD, & Chien N (2008). Expanding the family economic stress model: Insights from a mixed-methods approach. Journal of Marriage and Family, 70, 196–209. doi: 10.1111/j.1741-3737.2007.00471.x [DOI] [Google Scholar]
- Muthén LK, & Muthén BO (2010). Mplus user’s guide (6th ed.). Los Angeles, CA: Author. [Google Scholar]
- National Institute of Child Health and Human Development Early Child Care Research Network. (1999). Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning at 36 months. Developmental Psychology, 35, 1297–1310. doi: 10.1037/0012-1649.35.5.1297 [DOI] [PubMed] [Google Scholar]
- Parke RD, Coltrane S, Duffy S, Buriel R, Dennis J, Powers J, … Widaman KF (2004). Economic stress, parenting, and child adjustment in Mexican American and European American families. Child Development, 75, 1632–1656. doi: 10.1111/j.1467-8624.2004.00807.x [DOI] [PubMed] [Google Scholar]
- Schreier A, Wittchen HU, Höfler M, & Lieb R (2008). Anxiety disorders in mothers and children: Prospective longitudinal community study. British Journal of Psychiatry, 192, 308–309. doi: 10.1192/bjp.bp.106.033589 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2009). People and families in poverty by selected characteristics: 2008 and 2009. Retrieved from http://www.census.gov/hhes/www/poverty/data/incpovhlth/2009/table4.pdf
- Vernon-Feagans L, Pancsofar N, Willoughby M, Odom E, Quade A, Cox M, & Family Life Key Investigators. (2008). Predictors of maternal language to infants during a picture book task in the home: Family SES, child characteristics, and the parenting environment. Journal of Applied Developmental Psychology, 29, 213–226. doi: 10.1016/j.appdev.2008.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadsworth ME, Raviv T, Compas BE, & Connor-Smith JK (2005). Parent and adolescent responses to poverty-related stress: Tests of mediated and moderated coping models. Journal of Child and Family Studies, 14, 283–298. doi: 10.1007/s10826-005-5056-2 [DOI] [Google Scholar]
- Wagmiller RL Jr., Lennon MC, & Kuang L (2008). Parental health and children’s economic well-being. Journal of Health and Social Behavior, 49, 37–55. doi: 10.1177/002214650804900104 [DOI] [PubMed] [Google Scholar]
- Weber B, Jensen L, Miller K, Mosley J, & Fisher M (2005). A critical review of the rural poverty literature: Is there truly a rural effect? International Regional Science Review, 28, 381–414. doi: 10.1177/0160017605278996 [DOI] [Google Scholar]
- Wood JJ, McLeod BD, Sigman M, Hwang W, & Chu BC (2003). Parenting and childhood anxiety: Theory, empirical findings, and future directions. Journal of Child Psychology and Psychiatry, 44, 134–151. doi: 10.1111/1469-7610.00106 [DOI] [PubMed] [Google Scholar]


