Introduction
The Department of Veteran’s Affairs (VA) Home Based Primary Care (HBPC) Program delivers in-home care to chronically ill geriatric veterans.1 During the COVID-19 pandemic, older adults adults were required to minimize in-person contact, and the home-based care delivery model became untenable.2,3 National VA leadership encouraged replacing in-person visits with videoconferencing. This posed challenges for HBPC, where video visits represented only 0.3% of over 1 million total national HBPC visits from January 2019-February 2020 despite efforts to promote adoption. Prior to the pandemic, national VA and HBPC leadership had developed structural changes, defined as changes related to resources, management systems and policy guidelines,4 which laid the groundwork for video visit adoption. This included development of the VA Video Connect (VVC) videoconferencing software, investment in support lines to troubleshoot software issues, creation of a health record provider note template, and provision of government-issued laptops and cell phones to providers. Providers could enroll patients in a program distributing video-capable tablets to veterans with need.5 National leadership developed VVC training modules and incentivized replacing in-person visits with video visits. Nevertheless, it was not until additional key local and national changes occurred around the time of the pandemic declaration that adoption rapidly increased in the San Francisco VA Health Care System’s (SFVAHCS) HBPC from February to June 2020. We highlight key changes facilitating this increase.
Methods
We developed a timeline of changes and categorized changes guided by the COM-B model of behavior change, a framework used to demonstrate how behavior (B) change occurs when individuals have the physical and mental capability (C) to seize available opportunities (O) if there is sufficient motivation (M) for change.6 Utilizing VA national (Corporate Data Warehouse) data, we trended video visits as a percentage of total visits between January 2020 through June 2020 in relation to aforementioned timeline. We trended percentages of providers becoming video visit capable.
Results
Changes involved augmenting provider capability (leadership encouraging providers to upgrade computing hardware and complete training modules, temporary expansion of allowable videoconferencing platforms besides VVC), opportunity (large group didactics as well as individual tutorials and biweekly virtual office hours for VVC training, encouragement of peer education, triage changes to favor VVC visits), and motivation (local mandate for all clinicians to become VVC capable, heightened desire to keep patients healthy during the pandemic) (Figure 1). Behavior change occurred rapidly, as video-visit-capability among clinicians increased from 12% to 94% from March 1 to 27 and video visits increased from 0% to 2% of total visits from February to March, to 8% in April onward. This surpassed the regional Sierra Pacific Network to which SFVAHCS HBPC belongs, where video visits similarly increased from 0% to 2% in from February to March but increased only to 6–7% in April onward.
Figure 1.
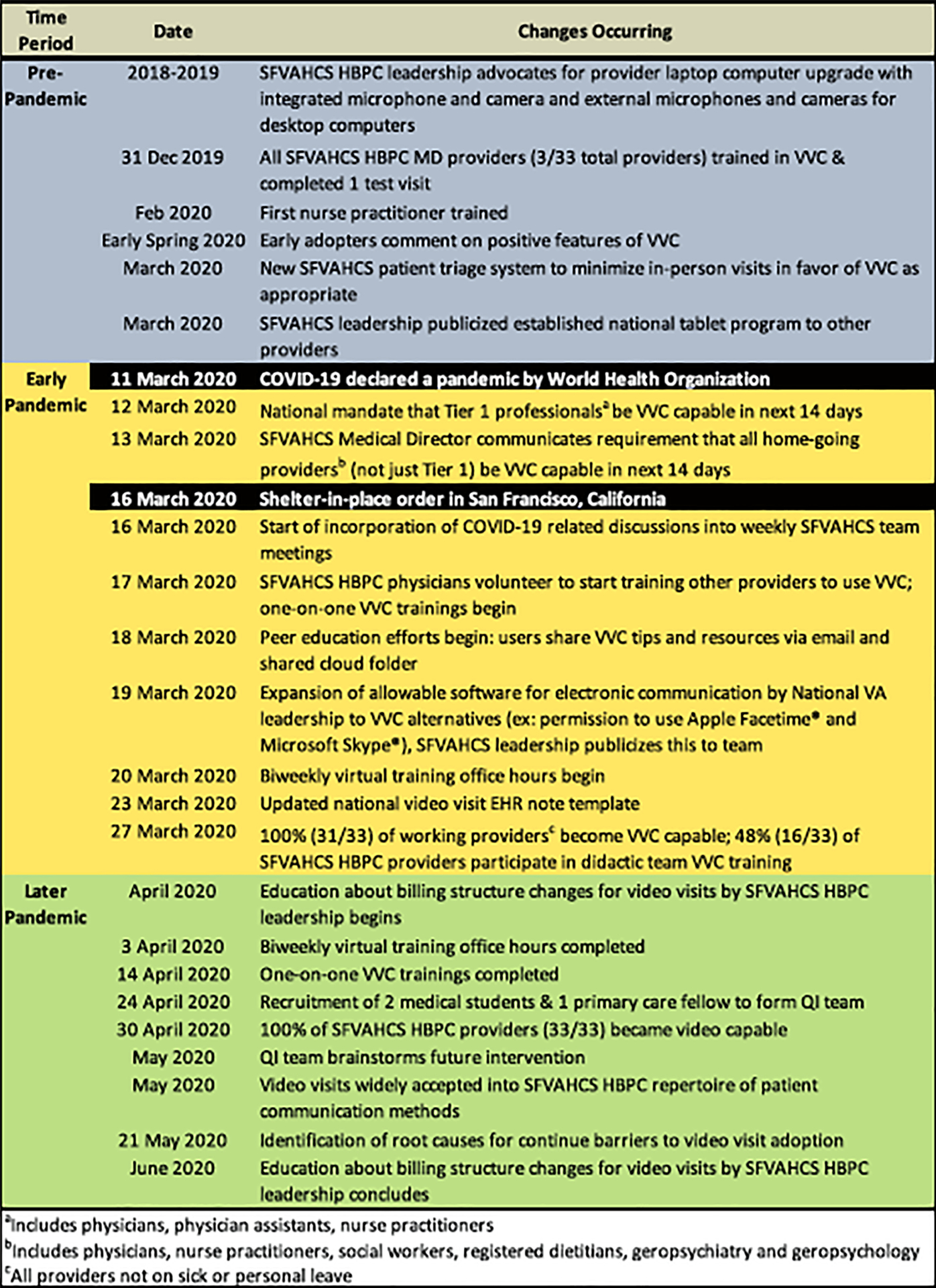
Timeline of national and local changes/interventions affecting video visit adoption within the San Francisco Department of Veterans Affairs Healthcare System (SFVAHCS) Home Based Primary Care (HBPC) Program. Pre-pandemic period=before March 11th, 2020; early pandemic period=March 11th, 2020 to March 27th, 2020; and later pandemic period=after March 27th, 2020. VVC=Veterans Affair Video Connect video visit software platform, VA=Department of Veterans Affairs, EHR=electronic health record, QI=quality improvement.
Discussion
This project showed that improved VVC adoption required multiple domains of change. The combination of national structural changes and local changes addressing provider capability, opportunity, and motivation led to increased adoption. Given the diverse organizational, technological, and social barriers impacting the adoption of telemedicine,7 a multi-dimensional approach to change is important for effectiveness. Our findings support those of another study, which found that changes in multiple domains, including modified workflow processes and improved technology infrastructure, correlated with increased telehealth adoption.8 However, our study is unique as it examines the correlation of these changes with telehealth adoption in the distinct HBPC older adult population that typically receives high-touch in-home care.
This study also highlights the skillful use of different modes of education to efficiently train providers to host video visits. This aligns with a recent educational review supporting the use of diverse educational methods within a single intervention as a key feature of effective faculty development education.9 These various training options accommodated the varying levels of provider expertise and knowledge gaps. For example, didactic trainings benefitted providers needing to learn the basics of VVC software utilization and virtual patient interaction, while one-on-one demonstrations and office hours catered to seasoned learners seeking advanced expertise.
The San Francisco VA HBPC program, which cares for a particularly vulnerable geriatric population, increased video visit adoption exponentially and rapidly through a combination of national structural interventions and local changes addressing provider capability, opportunities, and motivation. This paper shows how these changes operationalized on a local level, shedding light on national trends. Similar clinics may benefit from changes enacted in various domains and levels like this to decrease the digital divide for these patients.10 Future steps for our project will focus on addressing behavior change from the patient perspective.
ACKNOWLEDGEMENTS
We thank the SFVAHCS HBPC Program team for their dedication to patient care and quick adaptation to unprecedented challenges. We thank Darlene M. Davis for her manuscript feedback and her efforts procuring data from the VA Corporate Data Warehouse on our behalf. We thank Dayna Cooper for her manuscript feedback.
Financial disclosure: The authors do not have any financial disclosures to report.
Sponsor Role: Unfunded quality improvement project. Dr. Allison’s time was supported in part by the National Institute on Aging (K23AG062613-01). No sponsors had any role in the design, methods, subject recruitment, data collection, analysis and preparation of the paper.
Footnotes
Conflict of interest: The authors do not have any financial or personal conflicts of interest to report.
Prior academic meeting submissions: This paper was not previously submitted or presented at an academic meeting.
References
- 1.Haverhals LM, Manheim C, Gilman C, et al. Dedicated to the Mission: Strategies US Department of Veterans Affairs Home-Based Primary Care Teams Apply to Keep Veterans at Home. Journal of the American Geriatrics Society 2019;67(12):2511–2518. doi: 10.1111/jgs.16171 [DOI] [PubMed] [Google Scholar]
- 2.CDC. Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention Published February 11, 2020. Accessed August 13, 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html [Google Scholar]
- 3.Figliozzi S, Masci P-G, Ahmadi N, et al. Predictors of Adverse Prognosis in Covid-19: A Systematic Review and Meta-analysis. European Journal of Clinical Investigation n/a(n/a):e13362. doi: 10.1111/eci.13362 [DOI] [PubMed] [Google Scholar]
- 4.Varkey P, Reller MK, Resar RK. Basics of Quality Improvement in Health Care. Mayo Clinic Proceedings 2007;82(6):735–739. doi: 10.4065/82.6.735 [DOI] [PubMed] [Google Scholar]
- 5.Slightam C, Gregory AJ, Hu J, et al. Patient Perceptions of Video Visits Using Veterans Affairs Telehealth Tablets: Survey Study. J Med Internet Res 2020;22(4). doi: 10.2196/15682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Michie S, van Stralen MM, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42. doi: 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare 2018;24(1):4–12. doi: 10.1177/1357633X16674087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ranganathan C, Balaji S. Key Factors Affecting the Adoption of Telemedicine by Ambulatory Clinics: Insights from a Statewide Survey. Telemedicine and e-Health 2019;26(2):218–225. doi: 10.1089/tmj.2018.0114 [DOI] [PubMed] [Google Scholar]
- 9.Steinert Y, Mann K, Centeno A, et al. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Medical Teacher 2006;28(6):497–526. doi: 10.1080/01421590600902976 [DOI] [PubMed] [Google Scholar]
- 10.Chesser A, Burke A, Reyes J, Rohrberg T. Navigating the digital divide: A systematic review of eHealth literacy in underserved populations in the United States. Informatics for Health and Social Care 2016;41(1):1–19. doi: 10.3109/17538157.2014.948171 [DOI] [PubMed] [Google Scholar]


