Abstract
Aim:
Sensory processing impairments are well characterized in children with neurodevelopmental disorders, particularly autism, and have been associated with maladaptive behaviors. However, little is known regarding sensory processing difficulties within Down syndrome, or how these difficulties may influence maladaptive behavior. This study aims to characterize sensory processing difficulties within the Down syndrome phenotype and determine the influence of processing difficulties on maladaptive behavior.
Methods:
To explore this issue, we administered the Short Sensory Profile and the Developmental Behavior Checklist to parents or primary caregivers of young children with DS (N = 49; M nonverbal mental age (NVMA) = 30.92 months (SD = 12.30); M chronological age (CA) = 67.04 (SD = 25.13).
Results:
Results indicated that Low Energy/Weak, Under-responsive/Seeks Sensation, and Auditory Filtering were the areas of greatest sensory regulation difficulty, and that Self-Absorbed behavior and Disruptive/Antisocial behavior were elevated areas of maladaptive behavior. Multivariate regression analyses indicated that Under-responsive/Seeks Sensation was the only sensory regulation domain significantly associated with Self-Absorbed and Disruptive/Antisocial behavior.
Conclusion:
Findings indicate a consistent pattern of sensory processing impairments and associations with maladaptive behavior in children with DS. Implications for interventions are discussed.
Keywords: Autism, behavior, Down syndrome, sensory processing, social-emotional development
Sensory processing is the continuous integration of information from the senses, movement, and muscle/joint position by the nervous system that facilitates an individual’s adaptive response to the demands of everyday life (Ayres, 1972; Miller, Anzalone, Lane, Cermak, & Osten, 2007). Impairments in sensory processing may include over- or under-responsiveness, difficulties with stimuli discrimination, and challenges with proprioception and motor planning (Miller et al., 2005). These impairments are common across various neurodevelopmental disorders and linked to a range of maladaptive outcomes for these individuals (Baranek et al., 2018). However, sensory processing profiles have been more thoroughly characterized in some neurodevelopmental disorders, such as autism spectrum disorders ([ASD; Baranek et al., 2002; Ben-Sasson et al., 2007; Lane et al., 2010; Lane, Reynolds, & Dumenci, 2012), and less so in other disorders such as Down syndrome (DS). There is evidence for phenotypic variation in sensory processing profiles both across neurodevelopmental disorders (Ben-Sasson et al., 2009; Reynolds, Kreider, & Bendixen, 2012) as well as within neurodevelopmental disorders (Miller et al., 2005). As such, a more thorough characterization of sensory processing profiles within the broader DS phenotype, and in particular in the context of concurrent ASD (DS + ASD), is necessary and may improve targeted intervention efforts.
DS, the most prevalent genetic cause of intellectual disability, occurs in 1 in approximately 691 live births (Parker et al., 2010) and has a comorbidity rate of approximately 20% with concurrent ASD (DiGuiseppi et al., 2010). Several features of the broader DS behavioral-cognitive phenotype predispose individuals to a greater propensity for sensory processing impairment (Bruni, Cameron, Dua, & Noy, 2010). From infancy, individuals with DS demonstrate greater ability (relative to their mental age) with aspects of visual-spatial processing, yet significant challenges in aspects of auditory processing and motor functioning (for a review, see Daunhauer & Fidler, 2011). This differential processing ability within the DS behavioral phenotype may contribute to specific challenges with sensory processing; yet our understanding of this aspect of the DS behavioral phenotype is limited. While sensory processing difficulties are well documented in ASD (Baranek et al., 2002; Ben-Sasson et al., 2007; Lane et al., 2010; Lane et al., 2012), this has not been explored in populations with DS + ASD. This subgroup within DS may experience unique challenges related to sensory processing difficulties and related outcomes than those with DS-only.
There is a considerable lack of empirical focus on sensory abnormalities in DS and the nature and impact of these impairments other areas of functioning for individuals with DS remains unclear. A study conducted by Wuang and Su (2011) used the Sensory Profile (Dunn, 1999) in 200 school-aged children with DS. The Sensory Profile classifies children as having “typical performance,” a “probable difference” (i.e., one standard deviation below the mean) or “definite difference” (i.e., two standard deviations below the mean; Dunn, 1999). Approximately 41% of their sample was reported to have a definite difference with “low registration,” 40% were reported to have a definite difference with low endurance/muscle tone, and 39% were reported to have a definite difference in sensory sensitivity (Wuang & Su, 2011). They also found small to moderate correlations between sensory processing domains and adaptive behavior (r = .41–.48) as well as between sensory processing and participation in school (r = .30–.38).
In another study, Bruni et al. (2010) examined sensory processing in school-aged children between 3 and 10 years old with DS using the parent-reported, abbreviated version of the Sensory Profile, the Short Sensory Profile (SSP; Dunn, 1999), which also stratifies sensory processing across categories of “typical performance,” a “probable difference,” and “definite difference.” In this study, almost half of children with DS were reported to experience a “definite difference” on the Total SSP scores, with the majority of parents (69 – 74%) reporting a probable to definite difference on the Low Energy/Weak (i.e., passive responses to stimuli), Under-responsive/Seeks sensation (i.e., less responsive or sought input), and the Auditory Filtering domains.
Although this limited evidence indicates that sensory processing is disrupted in individuals with DS, our knowledge is restricted to only these few studies, and the potential impact on other areas of functioning, such as maladaptive behavior has not been well explored. Maladaptive behavior, or challenging behavior, broadly encompasses consistent patterns of negative behavior, such as tantrums, aggression, and disobedience, that interfere with optimal functioning and engagement with one’s environment (Powell et al., 2006). An association between sensory processing impairments and maladaptive behavior has been reported in children with ASD (Baker et al., 2008; Lane et al., 2010; McIntosh et al., 1999; Miller et al., 2005; O’Donnell, Deitz, Kartin, Nalty, & Dawson, 2012). In a sample of children with a diagnosis of Autistic Disorder based on DSM-IV diagnostic categories, sensory processing domains of Under-responsive/Seeks Sensation, Auditory Filtering, and Low Energy/Weak were significantly correlated (r = .36–.59) with the Vineland Adaptive Behavior Scales Maladaptive Behavior domain (Lane et al., 2010). In preschoolers with ASD and no comorbid diagnoses, sensory processing impairments were moderately correlated with maladaptive behavior in irritability/agitation, lethargy/social withdrawal, hyperactivity, and inappropriate speech (O’Donnell et al., 2012). Given features associated with DS, such as hypotonia, challenges with verbal/auditory processing, and co-occurring DS + ASD for a subgroup (Daunhauer & Fidler, 2011), individuals with DS may experience similar sensory processing difficulties, which may influence maladaptive behavior.
Although individuals with DS demonstrate less maladaptive behavior than individuals with other developmental disorders on average (Dykens & Kasari, 1997), it is estimated that approximately one-third of individuals with DS have significant levels of maladaptive behavior (Coe et al., 1999; Dykens, 2007). Children with DS demonstrate low-level aggressive behaviors, such as argumentativeness, disobedience, and stubbornness, as well as inattention (Coe et al., 1999; Dykens, Shah, Sagun, Beck, & King, 2002; Will et al., 2016), whereas adolescents demonstrate elevated levels of internalizing behavior such as withdrawal (Dykens et al., 2002; Jacola et al., 2014). Temperament (Fidler, Hepburn, & Rogers, 2006) and health comorbidities such as anxiety (Esbensen, 2016), have been linked to elevated levels of some maladaptive behaviors in children and adolescents, respectively. Despite some evidence of areas of maladaptive behavior and associated mechanisms in DS, a comprehensive understanding of the nature of these behaviors remains unclear. Similar to other neurodevelopmental disorders, it is likely that certain areas of maladaptive behaviors are particularly elevated relative to others in DS, and sensory processing impairments are also likely to have a differential impact on maladaptive behavior profile in children with DS.
This study has three primary aims: (1) to identify areas of sensory processing impairment in children with DS, with and without comorbid ASD; (2) to identify areas of elevated maladaptive behavior in children with DS, with and without comorbid ASD; and (3) to identify the extent to which difficulties in sensory processing are associated with maladaptive behavior outcomes.
Method
Participants
The participants in this study were enrolled in a larger project examining social and communicative behaviors in children with DS in Colorado. For the larger study, participants born between January 1, 1996 and December 31, 2003 were recruited through a mailing from the state’s Department of Public Health and the Environment to all families of children with DS in a 10-county area and a local parent-run advocacy group for DS. Inclusion for the present study required completing sensory processing, problem behaviors, and developmental status assessments (see below). Of the 123 participants in the larger study, 49 participants between the ages of 2 years, 7 months old and 10 years 6 months old (M NVMA = 30.92 months; M CA = 67.04 months) had completed sensory and maladaptive behavior measures and were therefore included in this study (see Table 1 for participant characteristics). Participants with a diagnosis of blindness, deafness, or other severe impairments were excluded.
Table 1.
Participant characteristics.
| M | SD | |
|---|---|---|
| Chronological age | 67.04 | 25.13 |
| Mental age | 30.92 | 12.30 |
| DBC disruptive/antisocial | 10.53 | 6.49 |
| DBC self-absorbed | 15.16 | 10.10 |
| n | % | |
| Gender (male) | 33 | 67% |
| Race | ||
| Caucasian | 39 | 80% |
| Black | 2 | 4% |
| Biracial | 4 | 8% |
| Hispanic | 3 | 6% |
| Unreported | 1 | 2% |
Procedures
The University of Denver, Colorado institutional review board approved the larger project as well as the present study. During an initial clinic visit, a psychologist or Master’s-level clinician administered developmental testing to obtain mental age. Parent assessments of sensory processing and problem behaviors were obtained during follow-up visits related to the larger study. Participants were also screened for comorbid ASD through the larger project. The lead psychologist reviewed all diagnostic information (including the Autism Diagnostic Observation Schedule- Generic; Lord et al., 1999; and the Autism Diagnostic Interview-Revised; Lord et al., 1994; Rutter et al., 2003) and medical information, with a second clinician who reviewed every third case. If a disagreement occurred regarding a classification of co-morbid ASD, a discussion was held to reach consensus. Of the 49 participants included, 12 had co-morbid DS and ASD.
Measures
Developmental Status
The Mullen Scales of Early Learning (MSEL; Mullen, 1995) is a standardized developmental test that yields five subscale scores representing developmental ages: gross motor, fine motor, visual reception, expressive language, and receptive language. The MSEL demonstrates strong concurrent validity with other well-known developmental tests of motor, language, and cognitive development. The MSEL was administered to all subjects by advanced trained research staff and according to standard instructions.
Sensory Processing
The Short Sensory Profile (SSP; Dunn, 1999) was used to measure functional behaviors associated with responses to sensory input. The SSP is a parent- or caregiver-reported instrument for children ages 3 to 10 years-old with or without disabilities. It is a factor-derived, abbreviated version of the Sensory Profile (Dunn, 1999), which has been well-utilized and accepted for research purposes (Dunn, 1999; McIntosh et al., 1999). Parents rate their children’s sensory responses on a 5-point Likert scale. The 38-item measure yields both a total sensory dysfunction score, as well as seven domain scores including: tactile sensitivity (e.g., “avoids going barefoot”), taste/smell sensitivity (e.g., “will only eat certain tastes”), under-responsive/seeks sensation (e.g., “touches people and objects”), movement sensitivity (e.g. “fears falling or heights”), auditory filtering (e.g., “can’t work with background noise”), low energy/weak (e.g., “seems to have weak muscles”), and visual/auditory sensitivity (e.g., “hold hands over ears to protect ears from sound”). It was standardized on over 1,000 children with and without disabilities. The SSP is reported to have both adequate test-retest reliability (r = .90; Dunn, 1999) and construct validity (Dunn, 1999; McIntosh et al., 1999; Miller et al. 2005). Lower scores on this assessment indicate greater problems and scores are classified within a range of “Typical Development,” a “Probable Difference,” or a “Definite Difference.” Scale classification was used to identify the greatest proportion of participants across categories of sensory processing classifications. Total raw scores for each subdomain of greatest difficulty were used in multivariate regression analyses.
Maladaptive Behavior
The Developmental Behavior Checklist (DBC, Einfeld & Tonge, 1995; Dekker, Nunn, Einfeld, Tonge, & Koot, 2002) was used as a measure of maladaptive behavior. The DBC is a 96-item checklist completed by parents, primary caregivers, or teachers to assess behavioral and emotional problems in children with developmental disabilities. Each item is scored on a 3-point Likert scale. Based on the revised factor structure of the DBC (Dekker et al., 2002), a Total Behavior Problem Score is derived, in addition to five subscale factor derived scores: Disruptive/Antisocial behavior (“deliberately runs away” or “has temper tantrums”), Self-Absorbed behavior (“Aloof” or “has poor attention span”), Communications Disturbance (“gets obsessed with an idea” or arranged objects in a strict order”), Anxiety (“cries easily for no reason”), and Social Relating (“avoids eye contact” or “doesn’t show affection”). The DBC has an adequately established parent to parent reliability (ICC = .80) and adequate concurrent validity with similar measures (.70–.80). Higher scores on this assessment indicate greater problems. DBC norms based on developmental level were used, providing an appropriate fit for the sample given the developmental delay. Mean scale scores were used in profile analyses, and raw scale scores for the most elevated domains were included in multivariate regression analyses.
Analytic Approach
Descriptive statistics and participant characteristics were computed for each subgroup (DS-Only and DS + ASD), as well as the overall sample (see Table 1). Calculated frequencies of normed classifications of the SSP (Dunn, 1999) were used to examine the profile of sensory processing across DS subgroups (DS-Only and DS + ASD), as well as the overall sample. Specifically, the proportion of participants within each normed classification category of performance: “Typical Performance,” “Probable Difference,” and “Definite Difference” was calculated. Proportions were used to account for incomplete responses across domains. Proportions of participants within each performance category across the DS-Only and the DS + ASD subgroups, as well as the combined groups are presented in Table 2. Given the small sample size in the DS + ASD group and the consistency in profiles of sensory processing impairments between the DS-Only and DS + ASD group, a maladaptive behavior profile was examined using descriptive distributions of maladaptive behavior raw scores on the DBC across DS subgroups, as well as the combined groups. Similarly, due to power constraints given the combined group (n = 49) and consistency in patterns of sensory processing and maladaptive behavior across DS subgroups, the areas of greatest impairment in both sensory processing and maladaptive behavior were retained for subsequent analyses (Will et al., 2016). A multivariate regression model was used to test the association between sensory processing impairments and maladaptive behavior across the overall sample. Preliminarily correlations between nonverbal mental age, sensory processing, and maladaptive behavior variables were examined to determine whether to covary for cognitive functioning but found no significant associations.
Table 2.
Sensory processing distributions.
| All Participants | DS Only | DS + ASD | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Typical performance | Probable difference | Definite difference | Typical performance | Probable difference | Definite difference | Typical performance | Probable difference | Definite difference | ||||||||||
| All participants | N | % | N | % | N | % | n | % | n | % | n | % | n | % | n | % | n | % |
| Tactile sensitivity | 18 | 37 | 10 | 20 | 9 | 18 | 18 | 49 | 10 | 27 | 9 | 24 | – | – | – | – | – | – |
| Taste/smell sensitivity | 25 | 51 | 7 | 14 | 8 | 16 | 24 | 65 | 6 | 16 | 7 | 19 | 1 | 8 | 1 | 8 | 1 | 8 |
| Under-responsivity/seeks Sensation | 25 | 51 | 7 | 14 | 17 | 35 | 22 | 56 | 5 | 14 | 10 | 27 | 3 | 25 | 2 | 17 | 7 | 58 |
| Auditory filtering | 14 | 29 | 19 | 39 | 16 | 33 | 12 | 32 | 14 | 38 | 11 | 30 | 2 | 17 | 5 | 42 | 5 | 42 |
| Visual/auditory sensitivity | 31 | 63 | 6 | 12 | 12 | 25 | 23 | 62 | 5 | 14 | 9 | 24 | 8 | 67 | 1 | 8 | 3 | 25 |
| Low energy/weak | 14 | 29 | 3 | 6 | 32 | 65 | 12 | 32 | 3 | 8 | 22 | 60 | 2 | 17 | 0 | 0 | 10 | 83 |
| Movement sensitivity | 32 | 65 | 9 | 18 | 7 | 14 | 25 | 68 | 6 | 16 | 6 | 16 | 7 | 58 | 3 | 25 | 1 | 8 |
Results
Sensory Profile Classifications
Results from computing frequency distributions across areas of sensory processing indicated the greatest proportion of participants experienced difficulties in the areas of Low Energy/Weak (65% reporting a Definite Difference), Auditory Filtering (33% reporting a Definite Difference), and Under-responsivity/Seeks Sensation (35% reporting a Definite Difference; see Table 2 for full results). Distributions of sensory processing challenges were similar across the DS-Only and DS + ASD subgroups (see Table 2). Low Energy/Weak, Auditory Filtering, and Under-responsive/seeks sensation were retained as predictors in subsequent multivariate regression analyses.
Maladaptive Behavior Profile
Results from descriptive maladaptive profile analyses indicated that the Disruptive/Antisocial scale and the Self-Absorbed scale were the most problematic areas of maladaptive behavior (see Figure 1) across both the DS-Only and DS + ASD groups. Due to limited statistical power, these two domains were retained for multivariate regression analyses.
Figure 1.
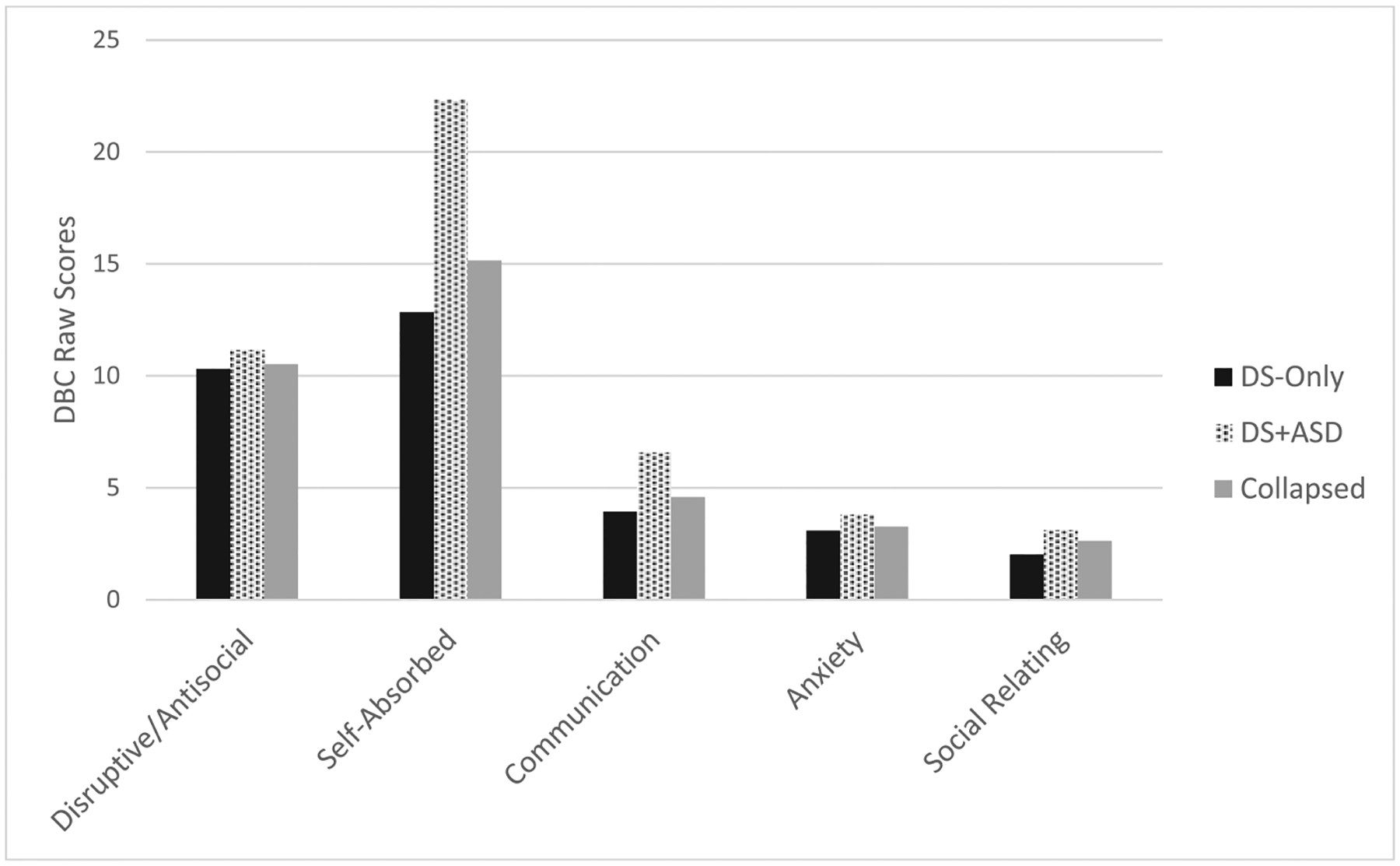
Challenging behavior profile.
Sensory Predictors of Maladaptive Behavior
Due to the consistency in patterns of sensory processing and maladaptive behavior in the DS-Only and DS + ASD subgroups, as well as statistical power considerations, these groups were collapsed for multivariate regression analyses. The Disruptive/Antisocial and Self-Absorbed scales were regressed on Low Energy/Weak, Under-responsive/Seeks Sensation, and Auditory Filtering in a multivariate multiple regression (see Table 3). Collectively, sensory processing accounted for 51% of the variance in maladaptive behavior domains. Under-responsive/Seeks sensation was the only sensory processing predictor that significantly predicted collective outcomes in maladaptive behavior (F(2,44) = 9.32; p < .001; η2 = .30). In addition, sensory processing collectively and significantly predicted Disruptive/Antisocial behavior (F(3,48) = 4.60; p = 0.007), and accounted for approximately 24% of the variance (R2 = 0.24). Sensory processing also collectively and significantly predicted Self-Absorbed behavior (F(3,48) = 14.62; p < 0.001), and accounted for approximately 49% of the variance (R2 = 0.49). Univariate results indicated that Under-responsive/Seeks sensation was the primary sensory processing variable associated with these outcomes, such that more competence in this domain was associated with decreased maladaptive behavior (see Table 3). Under-responsive/Seeks sensation significantly predicted Disruptive/Antisocial behavior (b = −0.44; p = 0.011) such that more competent performances, that is better responsivity and less sensation seeking, was associated with a decrease in Disruptive/Antisocial behavior (of approximately .44 units). Low energy/Weak and Auditory Filtering did not significantly predict Disruptive/Antisocial outcomes. Under-responsive/Seeks sensation also significantly predicted Self-Absorbed behavior (b = −0.90; p < 0.001), such that better responsivity and less sensation seeking was associated with an approximate 1-point decrease in Self-Absorbed behavior. Low Energy/Weak and Auditory Filtering did not significantly predict Self-Absorbed behavior.
Table 3.
Sensory processing predictors of challenging behavior.
| Disruptive/antisocial | Self-absorbed | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | 95% CI | |||||||||
| b | SE(b) | p | Lower | Upper | b | SE(b) | p | Lower | Upper | |
| Intercept | 24.54 | 5.12 | 14.23 | 34.84 | 52.92 | 6.48 | 39.87 | 65.97 | ||
| Auditory filtering | −0.23 | 0.25 | 0.372 | −0.74 | 0.28 | −0.63 | 0.32 | 0.06 | −1.28 | 0.02 |
| Low energy/weak | 0.10 | 0.14 | 0.463 | −0.17 | 0.38 | −0.07 | 0.17 | 0.704 | −0.41 | 0.28 |
| Under-responsive/seeks | −0.44 | 0.17 | 0.011 | −0.77 | −0.11 | −0.90 | 0.21 | 0.000 | −1.32 | −0.48 |
| R2 = 0.24 | R2 = 0.49 | |||||||||
Overall multivariate R2 = 0.51.
Summary
Results suggested a similar profile of both sensory processing difficulties and maladaptive behavior across the DS-Only and DS + ASD subgroups. Specifically, Under-responsive/Seeks sensation, Auditory Filtering, and Low Energy/Weak emerged as the most problematic areas of sensory processing in both groups, and Disruptive/Antisocial and Self-Absorbed behavior emerged as the most elevated areas of maladaptive behavior in both the DS-Only and DS + ASD subgroups. Regression model results examining sensory predictors of maladaptive behavior domains across the overall DS sample indicated that under-responsive/seeks sensation was the only aspect of sensory processing associated with maladaptive behavior outcomes.
Discussion
This study is among the first to evaluate sensory processing predictors of maladaptive behavior in children with DS. Findings indicate that children with DS demonstrate a complex pattern of sensory processing challenges, with greatest challenges in Low Energy/Weak, Under-responsive/Seeks sensation, and Auditory Filtering. Results from the current study also replicate previous findings across all three areas of sensory processing challenges (Bruni et al., 2010), suggesting these areas are of particular challenge for individuals with DS. The present study also extends previous findings by providing new information regarding elevated areas of maladaptive behavior. Specifically, Disruptive/Antisocial behavior, and Self-Absorbed behavior were identified as the most problematic areas of maladaptive behavior for children with DS-Only and DS + ASD. Under-responsive/Seeks sensation was the only significant predictor of each area of maladaptive behavior.
Sensory Processing Profile
The current study replicates previous findings which identified Low Energy/Weak, (demonstrating low strength and initiation); Under-responsive/Seeks Sensation (demonstrating low sensory responsivity and sensory seeking behaviors); and Auditory Filtering (demonstrating difficulty attending when multiple auditory stimuli are present) as the most problematic for individuals with DS (Bruni et al., 2010). Percentages reported here differ slightly from previous reports because they were within sample proportions rather than relative to normed cutoffs. Collective results suggest a high consistency between characteristics of the DS phenotype and challenges in certain aspects of sensory processing. Hypotonia (i.e., low muscle tone; for a review see Lott, 2012), for example, is characteristic to DS and speculated to affect attainment of motor milestones and other areas of development (Fidler et al., 2011). Many items on these scales are related to decreased sensory perception (e.g., under-responsive/Seeks sensation), or are directly related to having a weakened grasp or core support (e.g., Low Energy/Weak), which may also result from low muscle tone. This aspect of the DS phenotype may increase the propensity for children with DS to experience greater impairment in the areas of Low Energy/Weak and Under-responsive/Seeks Sensation (Bruni et al., 2010). In turn, this may also impact overall goal-orientation, which is also associated with problem behaviors in typically developing children (Graziano et al., 2015; Riggs, Blair, & Greenberg, 2004).
In addition to hypotonia, other aspects of the DS behavioral phenotype, such as difficulties with verbal/auditory processing (Daunhauer, 2011), may contribute to sensory processing impairments. For example, many items in the Auditory Filtering area involve being hyper-sensitive to sounds, not seeming to notice loud sounds, and having the ability to complete tasks with background noise. Thus, individuals who have difficulties with filtering irrelevant sounds in the environment or who are overly sensitive to sounds may have difficulty attending to speech sounds that are crucial to the completion of verbal tasks. These difficulties may in turn affect how attuned a child with DS is with aspects of their daily environment.
Relying on informant report to assess for sensory processing challenges in a population with co-occurring intellectual disability is not without challenges. Parents may misinterpret the ability to complete tasks with background noise as relating to sensory processing difficulties when it actually relates to a primary verbal impairment. For example, attention and attentional control are noted areas of difficulty in children with DS (Coe et al., 1999; Ekstein et al. 2011; Will et al., 2016), which may have implications for informant reported sensory processing challenges. Specifically, these difficulties may be interpreted as auditory processing impairment (Baker et al., 2008) rather than attentional difficulty, resulting in elevated scores on this index of the SSP. However, it may be unproductive to interpret the underlying causes of observed sensory processing difficulties – i.e., is the sensory problem primary or an attentional problem primary. Likewise, Under-responsive/Seeks sensation is a continuum of sensory processing in which the individual can only demonstrate under-responsivity to input from their environment, or engage in sensory seeking behaviors to increase input, or both (Ben-Sasson et al., 2009). Without careful item-level analysis of sensory processing measures or utilizing direct observation measures, it may be difficult to further specify which end of the continuum (i.e., under-responsive or seeks sensation) may be characteristic to children with DS. These interpretative challenges also highlight the need for objective psychophysiological studies that investigate the presence (or absence) of sensory processing difficulties in DS (e.g., Miller et al., 2005).
Maladaptive Behavior
In addition to areas of sensory processing challenges, we identified Disruptive/Antisocial and Self-Absorbed domains as the most elevated areas of maladaptive behavior. The Disruptive/Antisocial domain includes several items related to impulsivity and low-level aggressive behaviors, such as property destruction, disobedience, and elopement, which are consistently found as areas of elevated maladaptive behavior in children with DS (Coe et al., 1999; Daunhauer, Fidler, & Will, 2014; Dykens et al., 2002). In addition, individuals with DS also demonstrate relatively high rates of repetitive and stereotypic behavior such as rocking or arm flapping (Evans, Kleinpeter, Slane, & Boomer, 2014), which are measured by several items on the Self-Absorbed scale of the DBC (Einfeld & Tonge, 1995). These two broader categories of maladaptive behavior (i.e., Disruptive/Antisocial and Self-Absorbed) and their associated behaviors, such as aggression and stereotypy, have a demonstrated impact and association with adaptive outcomes in children with DS (Evans et al., 2014; Will et al., 2016). However, further consideration regarding targeted intervention towards maladaptive behavior in DS and those with DS + ASD is warranted.
Sensory Processing Predictors Of Maladaptive Behavior
Sensory processing difficulties have been linked to maladaptive behavior in other populations, such as ASD (Baranek et al., 2002; Ben-Sasson et al., 2009; Lane et al., 2012); however, this study is one of the first to evaluate sensory processing impairments in DS (see also Bruni et al., 2010), and more specifically, to characterize sensory processing difficulties in children with DS + ASD. Further, it is also one of the first to determine how these difficulties relate to maladaptive behavior in DS. Findings suggest atypical sensory processing abilities (i.e., Auditory Filtering, Under-responsive/Seeks Sensation, and Low Energy/Weak) indeed contribute to areas of maladaptive behavior (i.e., Self-Absorbed and Disruptive/Antisocial) in DS. However, Under-responsive/Seeks Sensation was found to solely account for this effect beyond that of other areas of sensory processing impairments. Collectively, this suggests that decreased sensory sensation and perception is associated with increased engagement in low-level aggressive behaviors and repetitive and stereotypic behaviors in children with DS.
Individuals who demonstrate sensory under-responsivity appear to have a low drive for sensory input and are characterized as quiet, impassive, and difficult to engage (Bundy, Lane, & Murray, 2002), while those who are sensory seeking are captivated by stimuli (Ben-Sasson et al., 2009; Miller et al., 2007). Accordingly, on one hand children with DS may be difficult to engage in tasks or even social interaction given decreased sensory perception and under-responsivity, which may result in their behavior being interpreted as anti-social or self-absorbed. For example, if a child is more under-responsive to stimuli and therefore participating less in the environment, an adult may perceive this as engaging in withdrawn and self-absorbed behavior. Conversely, sensation seeking behavior is hypothesized to be driven by a need for intense sensory input and sometimes looks like excessive running, jumping, swinging, and other active pursuits (Bundy et al., 2002) which in some contexts (e.g., the classroom,) can be viewed as disruptive. Therefore, if a child is engaging in sensory seeking behaviors such as noise making or hand flapping, an adult may perceive this as disruptive behavior. Future work incorporating direct observation measures of maladaptive behavior and psychophysiological measures of sensory processing is necessary to gain a better understanding of how difficulties on the continuum of sensory under-responsivity and sensory seeking behaviors contribute to maladaptive behavior outcomes and impede overall engagement.
DS + ASD Subgroup
Although children with DS-Only and DS + ASD demonstrated similar profiles of sensory processing difficulties and maladaptive behavior, there may be differences in both of these areas that were not identified in the present study. To our knowledge, this is the first study to examine sensory processing profiles in children with DS + ASD and prior work on sensory processing in DS does not appear to have considered co-occurring ASD (Bruni et al., 2010). Thus, future and more extensive work is needed to adequately determine whether there is complete overlap in a sensory processing profile between children with DS-Only and DS + ASD. In fact, given that the Under-responsive/Seeks sensation domain captures a spectrum of processing difficulties, it is a possibility that children with DS-Only are endorsed on one end and children with DS + ASD are endorsed on the other, yet this subgroup variation is masked given that this construct or constructs are measured on a single domain. Such effects require item-level analysis, which are beyond the scope of the present study. However, such an analysis would provide important information on the specific nature of not only sensory processing impairments within each subgroup of DS, but also determine whether there are also differential effects on maladaptive behavior outcomes.
Limitations
This study is not without limitations. Most notably, no comparison group was assessed, and therefore it is unclear whether the relation found between sensory processing and maladaptive behavior is specific to DS. This information is critical for characterizing a sensory processing profile specific to DS relative to other populations of neurodevelopmental disorders. In addition, the present study was lacking in direct observation measures, which afford the opportunity to more precisely determine possible underlying mechanisms of maladaptive behavior. For example, there are potential alternative functions to observed maladaptive behavior (e.g., access to attention, or escape from demands) that may or may not relate to sensory processing difficulties. Finally, the broad age range of the sample and cross-sectional design limit the generalizability of study findings. Profiles of sensory processing and maladaptive behavior, as well as their association with one another, likely shift across development. As such, examining these profiles within certain developmental periods and their developmental changes over time can provide a more comprehensive picture of areas of need for targeted intervention.
Implications and Conclusions
While there is a great deal of individual variability in children with DS, findings here indicate that sensory processing issues in areas such as Low Energy/Weak, Under-Responsive/Seeks sensation, and Auditory Filtering are likely a component of the DS phenotypic behavioral profile and that these issues, particularly Under responsive/Seeks sensation, appear to relate to maladaptive behaviors. The Under-responsive/Seeks sensation domain presents as a continuum of responsivity to stimuli, but a challenge with either direction of this continuum indicates difficulties in regulating sensory responsiveness or activity level. A deeper understanding regarding sensory processing impairments in this area could prevent problem behaviors that likely impact outcomes related to school achievement and social interactions. For example, if a child with DS demonstrates a lack of engagement in his/her environment or in social contexts due to low sensory responsivity, targeted intervention related to facilitating greater levels of participation can potentially circumvent maladaptive behavior. In addition, if a child with DS is engaging in sensory seeking behavior in a disruptive way, intervention promoting self-regulation and monitoring skills could also potentially circumvent maladaptive behavior and in turn promote engagement and participation. As suggested by Boyd et al. (2010) the associations between the continuum of under-responsive and seeking behaviors may suggest shared neurobiological underpinnings with disruptive and antisocial behaviors. Consequently, under-responsive or sensory seeking behavior and these associated maladaptive behavioral manifestations may be addressed via occupational or physical therapy approaches, as well as behavioral interventions.
Current findings also have implications for individuals with co-occurring DS + ASD, a vastly understudied population. We identified similar profiles of difficulties in both sensory processing and maladaptive behavior between children with DS-Only and DS + ASD. Given that this study is the first to examine sensory processing profiles in subgroups of children with DS, it is difficult to draw conclusions regarding specific needs of children with co-occurring DS + ASD. Research on high-risk infant siblings of children with ASD indicate that sensory seeking behaviors serve as an early indicator of ASD comorbidity (Baranek et al., 2018). Thus, sensory seeking behaviors do not appear to be an indicator of ASD for children with DS, given that this was a heightened area of sensory processing difficulty across children with DS with and without ASD. Intervention approaches commonly used for children with ASD are likely to also benefit children with DS + ASD but may also provide benefits to those with DS-Only as well. Profile consistencies between the DS-Only and DS + ASD subgroups also suggest that children with DS-Only may have levels of maladaptive behavior more similar to ASD populations than previously thought. However, direct comparisons between children with DS-Only, DS + ASD, and ASD only are required to fully determine similarities in maladaptive behavior profiles. Finally, similarities between the DS subgroups also suggest that all children with DS may benefit from interventions commonly used for children with ASD to address sensory processing and maladaptive behavior difficulties.
Future research is required to better disentangle associations between sensory processing difficulties and maladaptive behavior outcomes. Specifically, longitudinal work can inform the direction of influence and determine whether challenges in sensory processing precede problem behaviors. More work is also necessary to gain a better understanding of phenotypic similarities and differences between children with DS-Only and DS + ASD. Despite similarities across profiles identified in the present study, children with DS + ASD are vastly understudied as a subgroup of DS and additional work in this area is necessary to enhance our understanding of the broader DS behavioral phenotype. Addressing these specific gaps in current knowledge on areas of challenge in DS and their impact on behavioral outcomes has cross-disciplinary implications for understanding the nature and treatment of behavioral profiles in children with DS.
Footnotes
Disclosure statement
The authors report no conflicts of interest.
References
- Ayres AJ (1972). Sensory integration and learning disorders. Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Baker AE, Lane A, Angley MT, & Young RL (2008). The relationship between sensory processing patterns and behavioral responsiveness in autistic disorder: A pilot study. Journal of Autism and Developmental Disorders, 38(5), 867–875. doi: 10.1007/s10803-007-0459-0 [DOI] [PubMed] [Google Scholar]
- Baranek GT, Chin YH, Hess LMG, Yankee JG, Hatton DD, & Hooper SR (2002). Sensory processing correlates of occupational performance in children with fragile X syndrome: Preliminary findings. The American Journal of Occupational Therapy, 56(5), 538. doi: 10.5014/ajot.56.5.538 [DOI] [PubMed] [Google Scholar]
- Baranek GT, Woynaroski TG, Nowell S, Turner-Brown L, DuBay M, Crais ER, & Watson LR (2018). Cascading effects of attention disengagement and sensory seeking on social symptoms in a community sample of infants at-risk for a future diagnosis of autism spectrum disorder. Developmental Cognitive Neuroscience, 29, 30–40. doi: 10.1016/j.dcn.2017.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Sasson A, Hen L, Fluss R, Cermak SA, Engel-Yeger B, & Gal E (2009). A meta-analysis of sensory modulation symptoms in individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders, 39(1), 1–11. doi: 10.1007/s10803-008-0593-3 [DOI] [PubMed] [Google Scholar]
- Ben-Sasson A, Cermak SA, Orsmond GI, Tager-Flusberg H, Carter AS, Kadlec MB,& Dunn W (2007). Extreme sensory modulation behaviors in toddlers with autism spectrum disorders. The American Journal of Occupational Therapy, 61(5), 584–592. doi: 10.5014/ajot.61.5.584 [DOI] [PubMed] [Google Scholar]
- Boyd BA, Baranek GT, Sideris J, Poe MD, Watson LR, Patten E, & Miller H (2010). Sensory features and repetitive behaviors in children with autism and developmental delays. Autism Research, 3(2), 78–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruni M, Cameron D, Dua S, & Noy S (2010). Reported sensory processing of children with Down syndrome. Physical & Occupational Therapy in Pediatrics, 30(4), 280–293. doi: 10.3109/01942638.2010.486962 [DOI] [PubMed] [Google Scholar]
- Bundy AC, Lane SJ, & Murray EA (2002). Sensory integration: Theory and practice. FA Davis. [Google Scholar]
- Coe DA, Matson JL, Russell DW, Slifer KJ, Capone GT, Baglio C, & Stallings S (1999). Behavior problems of children with Down syndrome and life events. Journal of Autism and Developmental Disorders, 29(2), 149–156. [DOI] [PubMed] [Google Scholar]
- Daunhauer LA (2011). The early development of adaptive behavior and functional abilities in young children with Down syndrome: Current knowledge and future directions. International Review of Research in Developmental Disabilities, 40, 109–137. [Google Scholar]
- Daunhauer LA, & Fidler DJ (2011). The Down syndrome behavioral phenotype: Implications for practice and research. Occupational Therapy in Health Care, 25(1), 7–25. doi: 10.3109/07380577 [DOI] [PubMed] [Google Scholar]
- Daunhauer LA, Fidler DJ, & Will E (2014). School function in students with Down syndrome. American Journal of Occupational Therapy, 68(2), 167–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dekker MC, Nunn RJ, Einfeld SE, Tonge BJ, & Koot HM (2002). Assessing emotional and behavioral problems in children with intellectual disability: Revisiting the factor structure of the developmental behavior checklist. Journal of Autism and Developmental Disorders, 32(6), 601–610. doi: 10.1023/A:1021263216093 [DOI] [PubMed] [Google Scholar]
- DiGuiseppi C, Hepburn S, Davis JM, Fidler DJ, Hartway S, Lee NR, … Robinson C (2010). Screening for autism spectrum disorders in children with Down syndrome: Population prevalence and screening test characteristics. Journal of Developmental & Behavioral Pediatrics, 31(3), 181. doi: 10.1097/DBP.0b013e3181d5aa6d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn W (1999). The sensory profile manual. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Dykens EM, & Kasari C (1997). Maladaptive behavior in children with Prader-Willi syndrome, Down syndrome, and nonspecific mental retardation. American Journal on Mental Retardation, 102(3), 228–237. doi: [DOI] [PubMed] [Google Scholar]
- Dykens EM, Shah B, Sagun J, Beck T, & King B (2002). Maladaptive behavior in children and adolescents with Down’s syndrome. Journal of Intellectual Disability Research, 46(6), 484–492. doi: 10.1046/j.1365-2788.2002.00431.x [DOI] [PubMed] [Google Scholar]
- Dykens EM (2007). Psychiatric and behavioral disorders in persons with Down syndrome. Mental Retardation and Developmental Disabilities Research Reviews, 13(3), 272–278. doi: 10.1002/mrdd.20159 [DOI] [PubMed] [Google Scholar]
- Einfeld SL, & Tonge BJ (1995). The developmental behavior checklist: The development and validation of an instrument to assess behavioral and emotional disturbance in children and adolescents with mental retardation. Journal of Autism and Developmental Disorders, 25(2), 81–104. [DOI] [PubMed] [Google Scholar]
- Ekstein S, Glick B, Weill M, Kay B, & Berger I (2011). Down syndrome and attention-deficit/hyperactivity disorder (ADHD). Journal of Child Neurology, 26(10), 1290–1295. doi: 10.1177/0883073811405201 [DOI] [PubMed] [Google Scholar]
- Esbensen AJ (2016). Sleep problems and associated comorbidities among adults with Down syndrome. Journal of Intellectual Disability Research, 60(1), 68–79. doi: 10.1111/jir.12236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans DW, Kleinpeter FL, Slane MM, & Boomer KB (2014). Adaptive and maladaptive correlates of repetitive behavior and restricted interests in persons with Down syndrome and developmentally-matched typical children: A two-year longitudinal sequential design. PLoS One, 9(4), e93951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fidler D, Hepburn SL, Osaki D, Rondal J, & Perera J (2011). Goal-directedness as a target for early intervention in Down syndrome. Neurocognitive Rehabilitation of down Syndrome: Early Years, 191–204. [Google Scholar]
- Fidler D, Hepburn S, & Rogers S (2006). Early learning and adaptive behavior in toddlers with Down syndrome: Evidence for an emerging behavioral phenotype? Down Syndrome Research and Practice, 9(3), 37–44. doi: 10.3104/reports.297 [DOI] [PubMed] [Google Scholar]
- Graziano PA, Slavec J, Ros R, Garb L, Hart K, & Garcia A (2015). Self-regulation assessment among preschoolers with externalizing behavior problems. Psychological Assessment, 27(4), 1337–1348. doi: 10.1037/pas0000113 [DOI] [PubMed] [Google Scholar]
- Jacola LM, Hickey F, Howe SR, Esbensen A, & Shear PK (2014). Behavior and adaptive functioning in adolescents with Down syndrome: Specifying targets for intervention. Journal of Mental Health Research in Intellectual Disabilities, 7(4), 287–305. doi: 10.1080/19315864.2014.920941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane SJ, Reynolds S, & Dumenci L (2012). Sensory overresponsivity and anxiety in typically developing children and children with autism and attention deficit hyperactivity disorder: cause or coexistence? American Journal of Occupational Therapy, 66(5), 595–603. [DOI] [PubMed] [Google Scholar]
- Lane A, Young R, Baker A, & Angley M (2010). Sensory processing subtypes in autism: Association with adaptive behavior. Journal of Autism and Developmental Disorders, 40(1), 112–122. doi: 10.1007/s10803-009-0840-2 [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, & Risi S (1999). Autism diagnostic observation schedule-WPS (ADOS-WPS). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Lord C, Rutter M, & Le Couteur A (1994). Autism diagnostic interview revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24(5), 659–685. doi: 10.1007/BF02172145 [DOI] [PubMed] [Google Scholar]
- Lott IT (2012). Neurological phenotypes for Down syndrome across the life span. Progress in Brain Research, 197, 101–121. (Vol. Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntosh DN, Miller LJ, Shyu V, & Hagerman RJ (1999). Sensory-modulation disruption, electrodermal responses, and functional behaviors. Developmental Medicine & Child Neurology, 41(9), 608–615. doi: 10.1017/S0012162299001267 [DOI] [PubMed] [Google Scholar]
- Miller LJ, Anzalone ME, Lane SJ, Cermak SA, & Osten ET (2007). Concept evolution in sensory integration: A proposed nosology for diagnosis. The American Journal of Occupational Therapy, 61(2), 135–140. doi: 10.5014/ajot.61.2.135 [DOI] [PubMed] [Google Scholar]
- Miller LJ, Schoen S, Coll J, Brett-Green B, & Reale M (2005). Final report: Quantitative psychophysiologic examination of sensory processing in children with autism spectrum disorders. Los Angeles, CA: Cure Autism Now. [Google Scholar]
- Mullen EM (1995). Mullen scales of early learning. San Antonio, TX: Pearson. [Google Scholar]
- O’Donnell S, Deitz J, Kartin D, Nalty T, & Dawson G (2012). Sensory processing, problem behavior, adaptive behavior, and cognition in preschool children with autism spectrum disorders. The American Journal of Occupational Therapy, 66(5), 586–594. doi: 10.5014/ajot.2012.004168 [DOI] [PubMed] [Google Scholar]
- Parker SE, Mai CT, Canfield MA, Rickard R, Wang Y, Meyer RE, … Correa A(2010). Updated national birth prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Research Part A: Clinical and Molecular Teratology, 88(12), 1008–1016. doi: 10.1002/bdra.20735 [DOI] [PubMed] [Google Scholar]
- Powell D, Dunlap G, & Fox L (2006). Prevention and intervention for the challenging behaviors of toddlers and preschoolers. Infants & Young Children, 19(1), 25–35. doi: 10.1097/00001163-200601000-00004 [DOI] [Google Scholar]
- Reynolds S, Kreider CM, & Bendixen R (2012). A mixed-methods investigation of sensory response patterns in Barth syndrome: A clinical phenotype? American Journal of Medical Genetics Part A, 158A(7), 1647–1653. doi: 10.1002/ajmg.a.35413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggs NR, Blair CB, & Greenberg MT (2004). Concurrent and 2-year longitudinal relations between executive function and the behavior of 1st and 2nd grade children. Child Neuropsychology, 9(4), 267–276. doi: 10.1076/chin.9.4.267.23513 [DOI] [PubMed] [Google Scholar]
- Rutter M, LeCouteur A, & Lord C (2003). Autism diagnostic interview––revised. Los Angeles,CA: Western Psychological Services. [Google Scholar]
- Will EA, Gerlach-McDonald B, Fidler DJ, & Daunhauer LA (2016). Impact of maladaptive behavior on school function in Down syndrome. Research in Developmental Disabilities, 59, 328–337. doi: 10.1016/j.ridd.2016.08.018 [DOI] [PubMed] [Google Scholar]
- Wuang Y, & Su C (2011). Correlations of sensory processing and visual organization ability with participation in school-aged children with Down syndrome. Research in Developmental Disabilities, 32(6), 2398–2407. doi: 10.1016/j.ridd.2011.07.020 [DOI] [PubMed] [Google Scholar]


