OBJECTIVE:
The Affordable Care Act was signed in March 2010, aiming to improve health outcomes, primarily through coverage expansions and protections.1 Most policies were implemented universally, but Medicaid expansion was delayed by litigation and ultimately made an optional program for states.2 We sought to capitalize on variable policy uptake using quasi-experimental, difference-indifference methods to assess the association of Medicaid expansion with gynecologic cancer mortality.
STUDY DESIGN:
We accessed mortality data from the National Center for Health Statistics from 1999 to 2018.3 Age-adjusted annual gynecologic cancer (International Classification of Diseases, 10th Revision, C51–C58) mortality rates per 100,000 women ages 15 to 64 were assessed. We compared mortality by cancer (ovary, C56, C57.0, C57.4; uterus, C54, C55; cervix, C53; vulva and vagina, C51, C52), race, ethnicity, metro or nonmetro residence, and January 2014 Medicaid expansion (AZ, AR, CO, DE, HI, IL, IA, KY, MD, MA, NV, NM, NY, ND, OH, OR, RI, VT, WV) vs nonexpansion states (AL, FL, GA, ID, KA, ME, MS, MO, NE, NC, OK, SC, SD, TE, TX, UT, VA, WI, WY). We assessed for policy impact with difference in differences (DID), by comparing means and changes in mortality in the preexpansion vs postexpansion period (2010–2013 vs 2015–2018, with 2014 as an a priori assigned washout year owing to expectation of some delay in mortality impact of insurance change).
RESULTS:
From 1999 to 2018, age-adjusted annual gynecologic cancer mortality among women ages 15 to 64 fell from 9.9 to 8.6 per 100,000, although uterine cancer mortality increased slightly (1.8/100,000 to 2.5/100,000). Across races, mortality was consistently highest for black women (10.6/100,000 for black women vs 8.5/100,000 for white women in 2018), but trends over time were similar. Although comparable in early years, mortality was significantly higher among nonmetro vs metro women in 2018 (Δ=1.0/100,000; P<.001). The nonexpansion states represented a larger population of women ages 15 to 64 compared with the expansion states (41.6 vs 31.6 million). Nonexpansion states had relatively more black women (18.8% vs 13.7%) and fewer Asian women (4.4% vs 7.4%), but growth in minority, Hispanic, and metro populations over time was similar. Expansion and nonexpansion states exhibited overall parallel trends in gynecologic cancer mortality across 1999–2009 and the preexpansion period (2010–2013; ΔExp=−0.10/100,000; ΔNon-exp=−0.05/100,000) but diverged in the postexpansion period (2015–2018; ΔExp=−0.48/100,000; ΔNon-exp=0.16/100,000), with significantly lower mortality in 2018 in expansion states (Δ=0.64/100,000; P=.001). By DID (Figure), Medicaid expansion was associated with significant reduction in mean annual age-adjusted gynecologic cancer mortality among women ages 15 to 64 (ΔΔμ=−0.56/100,000; 95% confidence interval, −0.85 to −0.27; P=.002). Change in mortality in the postexpansion vs preexpansion period in expansion states trended more negatively (ΔΔΔ=−0.59/ 100,00; P=.16). Within subgroups, we estimated treatment effect reductions in mean mortality within uterine cancer (ΔΔμ=−0.18/100,000; P=.01), cervical cancer (ΔΔμ=−0.25/100,000; P=.002), and nonmetro women (ΔΔμ=1.03/100,000). Overall, we estimated that 246 deaths from gynecologic cancers in nonexpansion states might have been prevented with Medicaid expansion in 2018 alone.
FIGURE.
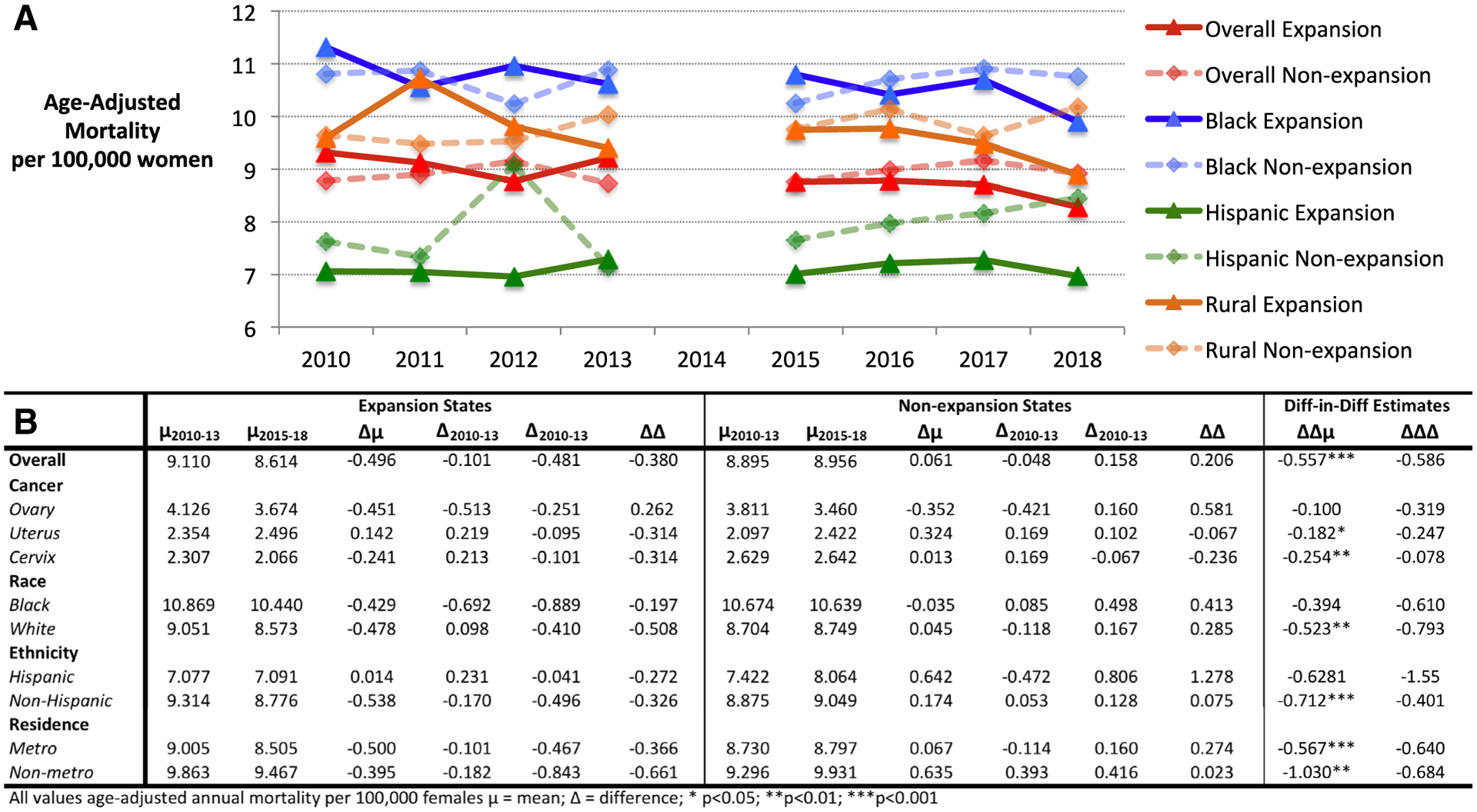
Difference-in-difference analysis of mortality from gynecologic cancers in relation to medicaid expansion
Difference-in-difference analysis for change in age-adjusted annual mortality rate from gynecologic cancers per 100,000 women comparing January 2014 Medicaid expansion with nonexpansion states in preexpansion (2010–2013) and postexpansion (2015–2018) periods. A, Time plots. B, Difference-in-difference calculation table.
Albright. Impact of Medicaid expansion on mortality from gynecologic cancers. Am J Obstet Gynecol 2021.
CONCLUSION:
Building on previous evidence of improved access for gynecologic cancer patients,4 we used DID methods to demonstrate evidence of small relative reductions in gynecologic cancer mortality, particularly from uterine and cervical diseases, in states that expanded Medicaid relative to those that did not, possibly owing to improved access to screening and treatment. This analysis is limited in model precision and statistical testing by availability of data only at the group level and not patient level. Although more states have adopted expansion recently, 13 states continue to decline the policy.5 Patients with gynecologic cancer in these states may benefit from expansion.
Acknowledgments
H.A.M. is supported by a Building Interdisciplinary Research Careers in Women’s Health career development award from the National Institutes of Health (NIH). Outside of this work, F.C. is supported by the Chanel Foundation and the Radiation Oncology Institute. F.C. and E.M.A are supported in part by the NIH and National Cancer Institute Cancer Center Support Grant P30 CA008748. Other authors have no funding to report. This work is not a clinical trial.
Footnotes
The authors report no conflict of interest.
A related but unique abstract, “Changes in cancer mortality rates after the adoption of the Affordable Care Act,” was presented at the 2020 meeting of the American Society of Clinical Oncology, held virtually on May 29–31, 2020.
No authors are employed by the Federal Government or Armed Forces.
Contributor Information
Benjamin B. Albright, Department of Obstetrics and Gynecology, Duke University Medical Center, 20 Duke Medicine Circle, Durham, NC 27710.
Fumiko Chino, Memorial Sloan Kettering Cancer Center, New York, NY.
Junzo P. Chino, Department of Radiation Oncology, Duke University Medical Center, Durham, NC.
Laura J. Havrilesky, Department of Obstetrics and Gynecology, Duke University Medical Center, Durham, NC.
Emeline M. Aviki, Memorial Sloan Kettering Cancer Center, New York, NY.
Haley A. Moss, Department of Obstetrics and Gynecology, Duke University Medical Center, Durham, NC.
REFERENCES
- 1.Office of the Legislative Counsel. Patient Protection and Affordable Care Act. Available at: https://www.hhs.gov/sites/default/files/ppacacon.pdf 2010. Accessed February 19, 2021.
- 2.Blumenthal D, Collins SR, Fowler EJ. The Affordable Care Act at 10 years - its coverage and access provisions. N Engl J Med 2020;382:963–9. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Multiple cause of death data. Available at: https://wonder.cdc.gov/mcd.html. Accessed July 12, 2020.
- 4.Albright BB, Nasioudis D, Craig S, et al. Impact of Medicaid expansion on women with gynecologic cancer: a difference-in-difference analysis. Am J Obstet Gynecol 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaiser Family Foundation. Status of state Medicaid expansion decisions: interactive map. Available at: https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/. Accessed February 2, 2020.


