Defining Comorbidity and Multimorbidity
Comorbidity and multimorbidity are important health factors that require complex medical management and are associated with worse health outcomes and increased health care costs. Comorbidity is defined as the occurrence of more than one disease or age-related health condition in an individual. Multimorbidity is broadly defined as the co-occurrence of two or more diseases or conditions in the same individual.1,2 However, simply counting the number of illnesses does not fully capture the extent of their impact on a patient’s health and number alone cannot be used alone to examine the impact of multimorbidity on healthcare barriers, utilization and costs. Currently, there exists no consensus on how to the term “multimorbidity” should be operationalized and its definition has varied based on the context in which it is used, i.e. for clinical care, epidemiological research or health service planning.
The three major operational definitions of multimorbidity that exist in literature are3:
≥2 concurrent diseases in the same individual, without considering effect of disease on function
Cumulative indices such as the Charlson Comorbidity Index4 that incorporate both number and severity of concurrent diseases
The presence of not only concurrent diseases, but also symptoms and impairments in physical and cognitive function
Multimorbidity is thought to differ from comorbidity in that it examines overall health issues whereas comorbidity is considered in the relation to an index disease.
Measuring Multimorbidity
Measuring multimorbidity is important for determining its impact on individuals and outcomes. However, the absence of a clear definition for multimorbidity contributes to the lack of standardized methods to measure it. Measurements are complex as they are dependent on the population studied, outcome of interest (i.e. mortality vs disability) and the context in which it is used (i.e. clinical practice vs outcomes research). For the time being, these measures are largely used in research studies and have not been applied in clinical practice.
The most extensively studied method is the Charlson Comorbidity Index (CCI) which calculates disease severity by mortality risk. CCI, developed in 1987, includes 19 conditions with each condition weighted based on estimated 1-year mortality hazard ratio from a Cox proportional hazards model and generates a total comorbidity score by summing the weighted conditions (Table 1).4 It has been reliably shown to predict mortality across a variety of populations, including but not limited to older adults, patients with cancer, heart disease, end-stage renal disease as well as in patients undergoing surgical procedures.5 It has also been shown to be associated with disability, hospital length of stay and hospital readmissions.
Table 1.
Comorbidities and Assigned Scores for the Comorbidity Charlson Index. Based on Table 2 from Quah H et al. American Journal of Epidemiology, 2011;173(6):676–682.
| Comorbidity | Score |
|---|---|
| Prior myocardial infarction | 1 |
| Congestive heart failure | 1 |
| Peripheral vascular disease | 1 |
| Cerebrovascular disease | 1 |
| Dementia | 1 |
| Chronic pulmonary disease | 1 |
| Rheumatologic disease | 1 |
| Peptic ulcer disease | 1 |
| Mild liver disease | 1 |
| Diabetes | 1 |
| Cerebrovascular (hemiplegia) event | 2 |
| Moderate-to-severe renal disease | 2 |
| Diabetes with chronic complications | 2 |
| Cancer without metastases | 2 |
| Leukemia | 2 |
| Lymphoma | 2 |
| Moderate to severe liver disease | 3 |
| Metastatic solid tumor | 6 |
| Acquired immune-deficiency syndrome (AIDS) | 6 |
The Cumulative Illness Rating Scale (CIRS) is another commonly used scale.6 It was developed in 1968 to assess physical impairment and differs from the CCI in that it assesses severity of impairment in 13 areas grouped by body systems rather than the presence of specific illnesses and it is heavily dependent on clinical judgement (Table 2). Similar to the CCI, it has been shown to be reliable in a variety of different clinical contexts and it has been shown to predict a variety of outcomes such as morbidity, health outcomes and health care utilization.7,8
Table 2.
Diseases and Scoring System for Cumulative Illness Rating Scale for Geriatrics. Based on Figure 1 from Miller M et al. Psychiatry Research, 1992; 41:237-248.
| Organ-System Categories | Rating Strategy |
|---|---|
| 1. Heart 2. Vascular 3. Hematopoietic 4. Respiratory 5. Eyes, ears, nose, throat and larynx 6. Upper gastrointestinal tract 7. Lower gastrointestinal tract 8. Liver 9. Renal 10. Genito-urinary 11. Musculoskeletal/integument 12. Neurological 13. Endocrine/metabolic and breast 14. Psychiatric illness |
0 – No problem 1 – Current mild problem or past significant problem 2 – Moderate disability or morbidity/requires “first line” therapy 3 – Severe/constant significant difficulty/”uncontrollable” chronic problems 4 – Extremely severe/immediate treatment required/end organ failure/severe impairment of function |
Wei et al recently developed and validated a multimorbidity weighted index (MWI) for community-dwelling adults aged 54-89 years that combines both presence of chronic conditions but also their impact.9,10 Their index weighs chronic conditions to their impact on the Short Form-36 (SF-36) physical functioning scale, a validated instrument used to assess health-related quality of life. It was found to accurately predict mortality and outperformed the CCI even though the MWI weighted to physical functioning and the CCI is weighted to mortality. This patient-centered, quantitative measure of multimorbidity is proposed as a readily feasible tool for research and ambulatory practice, requiring only self-reported information on past medical history and impact on function. An online calculator for MWI has been developed and is publicly available through the Division of Geriatrics at the University of California San Francisco (See Box 1, 2 and Case example).11
Box 1: Conditions included in the MWI calculator.
Dementia/Alzheimer disease
Stroke
Chronic lung disease (COPD)
Hypertension
Angina or Myocardial infarction
Congestive heart failure (CHF) or other heart condition
Arrhythmia
Diabetes
Cancer excluding skin
Arthritis (Osteoarthritis or Rheumatoid)
Knee/Hip replacement
Connective tissue disease (Systemic Lupus Erythematosus, Sjogren's Disease, Dermatomyositis, Polymyositis)
Glaucoma
Chronic kidney disease
Herniated disc
Cirrhosis
PE/DVT
AIDS
Multiple sclerosis
Parkinson's disease
Box 2: Weighting scheme for MWI.
For women:
1 point on MWI = 1 point on SF-36 = +3.5 years over 8 years in the same person.
For men:
1 point on MWI = 1 point on SF-36 = 3 years of additional aging over 8 years in the same person.
Case Examples Calculating Functional Decline and Mortality Using MWI:
Example 1:
Community-dwelling woman aged 54-89 years with prior history of tobacco use, stroke, chronic lung disease, hypertension, osteoarthritis and knee replacement.
Her total MWI score is 22.41. She is in the 95-100th MWI percentile. Her 10-year all-cause mortality risk is 48.9%.
Example 2:
Community-dwelling man aged 54-89 years with hypertension and chronic kidney disease.
His total MWI score is 5.43-6.99. He is in the 70-80th MWI percentile. His 10 year all-cause mortality risk is 15.1%.
Information for Box 1, 2 and case example from https://eprognosis.ucsf.edu/mwi.php, accessed 12/15/2019
Demographics of Adults with Comorbidity/Multimorbidity
Overall life expectancy is improving worldwide, with the World Health Organization (WHO) estimating the mean age of 72 years in more than 60 countries. As the prevalence of chronic medical conditions increases with age, the prevalence of multimorbidity is also expected to increase (Figure 1).12,13
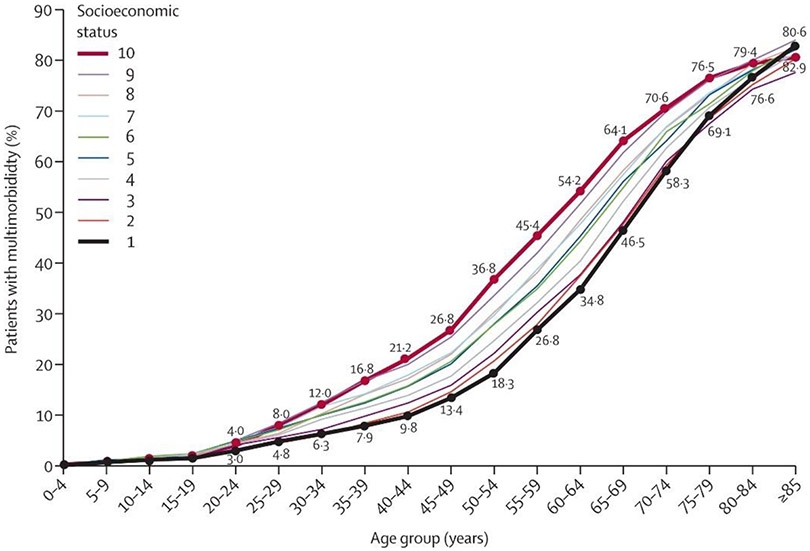
Figure 1.
Prevalence of multimorbidity by age and socioeconomic status. From Barnett K et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. The Lancet, 2012; 380(9836):37-43. Permission Pending
Estimating prevalence of multimorbidity is important in determining population disease burden, resources for interventions and health care costs but estimates can vary based on definition and measure of multimorbidity use. In a systemic review and meta-analysis, Nguyen et al. found that although there were regional variations, the global prevalence of multimorbidity was 33.1% (95% confidence interval: 30-36.3%).14 Prevalence of multimorbidity is increasing over time in part due to improved survival, an aging population, earlier and improved detection of diseases as well as changing lifestyle factors.15 In the US, a 2010 National Health Interview Survey, found that 26% of adults had 2+ chronic conditions, increased from 21.8% in 2001.16 Studies have also shown the following patterns of prevalence of multimorbidity17,18:
Prevalence of multimorbidity increases with age. More than 50% of individuals 65+ have multimorbidity. The highest prevalence in the “oldest old” 85+ group.
Women have greater prevalence of multimorbidity than men.
Prevalence varies by race/ethnicity. In the US population, prevalence was highest among American Indian/Alaska native, followed by non-Hispanic white and non-Hispanic black adults and lowest in Hispanic and Asian adults.
Multimorbidity is more prevalent in people with mental health disorders.
Socioeconomic Status on Prevalence
There are differences in the prevalence of multimorbidity based on socioeconomic status and education (Figure 1). In a cross-sectional study of self-reported multimorbidity of 5010 adults ≥18 years in Canada, the prevalence of multimorbidity was lower in individuals with higher income (11.6% in those earing >100K vs 32.5% in those earing <30K CI 95% 1.72-3.33, p=0.041) and in those with higher education (15.2% in those with University level education vs 20.8% in those with high school education; OR 1.11 CI 95% 0.86-1.42, p=0.007).17 In a cross-sectional study in Scotland, compared to age-matched controls, multimorbidity occurred 10-15 years earlier in adults living in deprived areas and socioeconomic deprivation was associated with more physical and mental health disorders (11%, 95% CI 10.9-11.2% in most deprived areas vs 5.9%, 95% CI 5.8%-6% in least deprived).8 Certain illnesses including chronic obstructive pulmonary disease, coronary heart disease, diabetes, cancer, depression and pain disorders were more common in lower income areas whereas others such as dementia and atrial fibrillation were more common in higher income areas.
Mechanism of Disease and Disability
There are complex interactions between biological, psychological, behavioral, socioeconomic and environmental factors that result in multimorbidity, accelerate aging and cause decline.
Lifestyle Factors
Lifestyle factors that predispose individuals to multimorbidity include obesity, lack of physical activity, tobacco and excess alcohol use and diet low in fruit and vegetables.19-22 Overall risk of developing multimorbidity from these factors may be dependent on specific combinations and additive effects of individual factors.19,22 In a large study of older adults, although physical activity was the only variable independently associated with increased risk of multimorbidity, a combination of 2, 3 and 4 or more unhealthy lifestyle factors (inactivity, obesity, smoking, alcohol consumption, fruit and vegetable consumption, and BMI) significantly increased multimorbidity compared with none from 42%-116%.19
Physical Inactivity
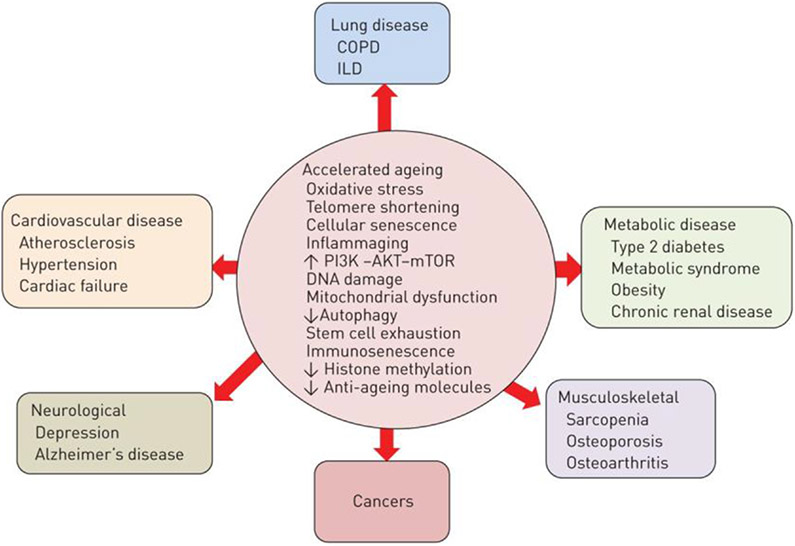
Physical activity has been shown to have important effects on physical and mental well-being (Figure 2).23 It can modify the effects of chronic conditions and improve outcomes in a variety of conditions, as well as reduce disability, morbidity and mortality. In addition to its benefits on cardiovascular and metabolic conditions, physical activity has been shown to prevent cognitive decline and reduces the risk of developing dementia.24,25 Effects of physical activity on health outcomes are thought to be due to its effects on regulating body weight and its effects on reducing insulin resistance, hypertension, dyslipidemia and inflammation.26 It appears to have a protective effect on neurodegeneration and psychological health by causing structural and functional changes such as increasing cerebral vascular blood flow and increasing neuroplasticity.25-27
Figure 2.
Changes induced by physical inactivity. From Booth FW and Laye MJ. Lack of adequate appreciation of physical exercise's complexities can preempt appropriate design and interpretation in scientific discovery. The Journal of Physiology, 2009; 587(23): 5527-39; with permission. (Figure 2 in original)
Studies on the effects of physical activity on multimorbidity as a whole, however, have been mixed. Studies of older adults have generally found that active older adults benefit from increased activity, and have fewer comorbid conditions and lower odds ratio for multimorbidity than non-active older adults.28,29 This benefit was found to be true especially in regards to the cardiovascular and metabolic disease cluster.29 However, a study of younger patients, which did not include older adults over the age of 69, did not show this benefit.30 While it is difficult to compare these studies as they used different physical activity assessments, the studies overall seem to suggest there may be age and gender differences in the effects of physical activity on multimorbidity which need to be further elucidated.
Nutrition
High calorie diets, rich in carbohydrates, saturated fats and cholesterol have been shown to be associated with metabolic dysregulation, increased oxidative stress and increased inflammation which are all risk factors for obesity, cardiovascular disease, metabolic disorders, arthritis and various cancers.31 There are limited studies however on the effects of nutrition on multimorbidity. A cross-sectional study found that that individuals with high consumption of a “meat and potatoes” diet had greater likelihood of cardiometabolic morbidity, with obesity as a likely intermediate step.32 Similarly, sugar sweetened beverages have also been associated obesity, cardiovascular disease and metabolic syndromes. An Australian study found that drinking >0.5L of soft drink per day vs not drinking any soft drink increased risk of multimorbidity, and the risk was higher for women than for men.33 A cohort study of Chinese adults, based on a 3-day weighted food record, found that fruit, vegetable, whole grain, and fiber consumption was greater in healthier individuals.21
Obesity
Obesity, closely linked to poor nutrition and physical inactivity, is strongly associated with increased inflammation, metabolic derangements, and decrease in physical function, all of which are shared risk factors for cardiovascular and non-cardiovascular disease.34 In a large pooled analysis of 120,813 adults in the US and Europe, Kivimäki et al. found that cardiometabolic multimorbidity, which is defined as the coexistence of more than one of type 2 diabetes, coronary artery disease, and stroke, increases with obesity.35 Compared to individuals with a healthy BMI (20-24.9 kg/m2), overweight people (BMI 25-29.9 kg/m2) had twice the risk, and severely obese people (BMI ≥35 kg/m2) had ten times the risk of cardiometabolic multimorbidity. This pattern was similar across age, gender, and ethnicities.
Tobacco and Alcohol Use
Tobacco and alcohol use, which frequently occur in conjunction with psychiatric comorbidities are similarly associated with multimorbidity.36,37 Cigarette smoking is a major risk factor for diseases in all organ systems including but not limited to cardiovascular and pulmonary disease and cancer.38 Both longer duration and higher intensity of smoking (amount of tobacco smoked per day) are associated with an increased risk of tobacco-related diseases.
Although low levels of alcohol use may have protective effects on heart disease and diabetes, average volume alcohol consumption is associated with increased risk of multiple diseases, including liver cirrhosis, eight different cancers, and cardiovascular outcomes such as hypertension and stroke.39 A recent study showed that alcohol use by men may result in three times higher health loss than by women.40
Inflammation and Multimorbidity
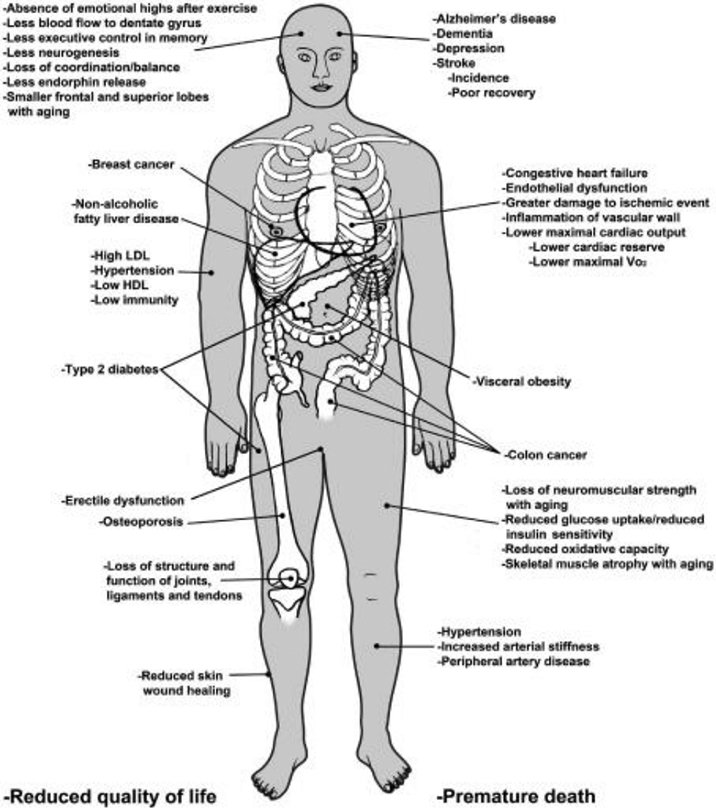
Many of the factors involved in multimorbidity appear to share similar biology pathways (Figure 3).41 Studies suggest that certain mechanisms related to oxidative stress and chronic inflammation that result in cellular senescence, impaired cell signaling, and cell death are involved.
Figure 3.
Biological mechanisms of multimorbidity. From Barnes PJ. Mechanisms of development of multimorbidity in the elderly. European Respiratory Journal, 2015; 45:790-806. Permission pending
Role of Oxidative Stress
Oxidative stress occurs when there is an imbalance in the formation of reactive oxygen species (ROS) which are toxic metabolic byproducts and molecules (anti-oxidants) that are protective against injury by these free radicals. ROS include superoxide anion (•O2 −), hydroxyl radical (•OH), singlet oxygen (1O2), hydrogen peroxide (H2O2) and hypochlorous acid (HOCl). They are unstable molecules because of unpaired electrons and have the capacity to produce damaging free radical chain reactions.42 ROS are endogenously produced as by-products of oxygen metabolism. They can be increased in various inflammatory processes including infections and ischemic injuries. They are also produced by environmental exposures such as ultraviolet (UV) radiation, cigarette smoking, and alcohol consumption. ROS are removed by enzymatic antioxidants such as such as superoxide dismutase, catalase and peroxidase as well as non-enzymatic antioxidants such as vitamin E, β-carotene and coenzyme Q.42 At normal levels, ROS have important roles in cellular function and tissue homeostasis. Overproduction of ROS results in alteration of cellular processes and tissue damage. Oxidative stress has been linked to pathogenesis of aging and disease in every organ including but not limited to cancer, cardiovascular disease, diabetes mellitus, respiratory disease, gastrointestinal disorders and neurodegenerative diseases.43
Role of Inflammation
There are numerous studies that suggest that dysregulated inflammation plays a key role in aging and in many chronic illness including cancers, heart disease, diabetes, dementia and mental health disorders.44,45 The Midlife in the United States (MIDUS) study showed using cross-sectional data from 1229 participants with mean age 54.5 years, that multimorbidity was associated with inflammation using the markers interleukin-6, C-reactive protein, and fibrinogen and that inflammation.46 Not only is inflammation implicated in the incidence of disease, studies suggest that inflammation may also be a link between multimorbidity and disability. Levels of inflammatory markers were found to be higher with accumulation of chronic diseases and higher levels of inflammation are associated with greater disability.47,48 The mechanism by which inflammatory cytokines exert their effects are yet to be fully elucidated but may be related to their direct effects on muscle catabolism and their effects on age-related changes in body composition. Inflammation may also play a role in health disparities. Studies have shown that socioeconomic factors such as income and education are associated with inflammatory cytokines.49,50
Disease Clustering and Synergistic Effects
As a result of the shared risk factors discussed above, certain diseases cluster together beyond chance. In a systematic study of the prevalence of disease clusters studied in older adults with multimorbidity, 20 disease pairs comprising of 12 different diseases were found to occur frequently.51 Hypertension, coronary artery disease and diabetes was the most highly prevalent combination. Depression was the most frequently clustered and occurred in conjunction with 8 different diseases. In fact, mental health disorders are frequently found clustered together. Compared to the general population, psychiatric patients have higher age-standardized relative risk for chronic illness, with obesity, hypertension, hyperlipidemia, and diabetes being significantly more prevalent in this population.52 In addition to lifestyle factors such as substance use as well as treatment-related effects, psychiatric illness in itself appears to be an important risk factor for developing other comorbid conditions such as coronary heart disease.53
The complex interactions between individual conditions appears to have synergistic effects that accelerate aging and cause functional decline (Figure 4). Using self-reported data from 13,232 adults ≥50 years, Koroukian et al. demonstrated that the co-occurrence of chronic conditions, functional limitations and/or geriatric syndromes had additive effects on mortality. Adults with co-occurrence of all three were 12 times as likely to die within 2 years.54 Wei et al. also demonstrated in their development of the MWI that individual diseases do not have equal weighted effects on physical performance and mortality and that determination of both these outcomes is dependent on cumulative effects of chronic disease.55
Figure 4.
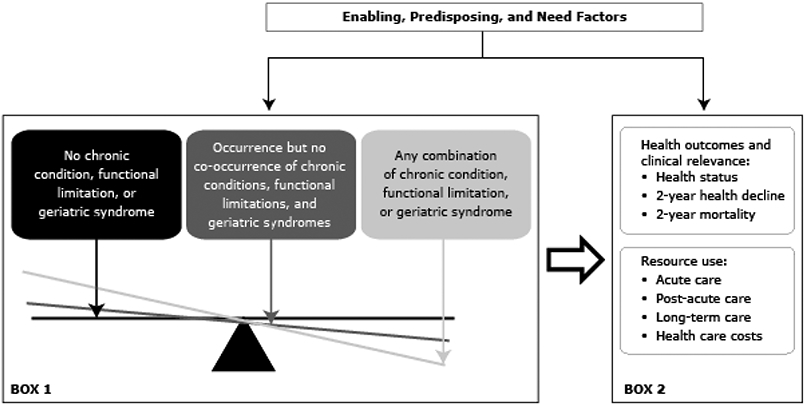
Cumulative effects of chronic disease, functional limitations and geriatric syndromes. Reproduced from Koroukian S et al. Multimorbidity Redefined: Prospective Health Outcomes and the Cumulative Effect of Co-Occurring Conditions. Preventing Chronic Disease, 2015;12:140478. Open Access (Figure 1 in original)
Effects of Multimorbidity on Outcomes
Effects of Multimorbidity on Survival
Multimorbidity is associated with many adverse health outcomes in the general older adult population as well as in specific populations (e.g., cancer, health failure, diabetes).56-58 These health outcomes include reduced physical functioning, cognitive functioning, and quality of life, as well as increased healthcare utilization and mortality.59-61 In a population-based cohort study of adults age 78 years and over in Sweden, multimorbidity (2 or more chronic conditions, out of 38 conditions) affected 70.4% of the population and accounted for most deaths (69.3% of total deaths), followed by cardiovascular (28.0%) and neuropsychiatric diseases (17.0%).62 It also leads to 7.5 years of life lost, compared to 5.0 and 4.3, respectively, for cardiovascular disease and cancer.62 Similarly, among community dwelling adults age 65 years and over enrolled on the National Health and Aging Trends Study in the United States, multimorbidity (or high multisystem morbidity as defined in the study, determined based on Bayesian information criterion) was associated with a greater risk of death.63
Effects of Multimorbidity on Physical Functioning
While survival is important, understanding how multimorbidity affects other patient-centered outcomes such as physical functioning, cognitive functioning, mental health, quality of life, disability, and healthcare utilization is also meaningful. Older adults prioritize these outcomes just as much, if not more, than survival.64,65 They may choose to have a shorter life span (length of life) for a longer health span (length of healthy life). To this end, several population-based cohort studies have evaluated the relationships of multimorbidity with these patient-centered outcomes.59,66,67 In a longitudinal analysis of adults age 51 and older enrolled on the Health Retirement Study (HRS) in the United States, those with higher MWI experienced more decline in physical functioning (measured using the modified Short-Form 36).66 For example, in a 68 year-old male with stroke and myocardial infarction, his MWI is 5.5 which translates to approximately 5.5 points decrease on the Short-Form 36 physical functioning scale, or 16.5 years of additional aging over the course of 8 years. In another cross-sectional analysis of adults age 65 and older enrolled on the National Health and Nutrition Examination Survey in the United States, multimorbidity (2 or more chronic conditions, out of 9 conditions ) was associated with an increase in functional limitations.67 The association was stronger in those age 75 years and older, emphasizing particular vulnerability as one ages.67
Effects of Multimorbidity on Cognitive Functioning, Mental Health, and Quality of Life
Like physical functioning, multimorbidity is associated with decline in cognitive functioning. In the HRS study, patients with higher MWI were more likely to experience declines in cognition, specifically global cognition, immediate and delayed recall, and working memory after 14 years of follow-up.68 In the Longitudinal Baltimore Study of Aging in the United States, multimorbidity (faster accumulation of 12 chronic diseases i.e., ≥0.25 diseases/year) was associated with decline in performance on verbal fluency tests, measured using standardized neuropsychological batteries.69 In the Mayo Clinic Study of Aging that included older adults age 70 to 89 years at enrollment, multimorbidity (2 or more chronic conditions, out of 17 conditions and not including dementia) is also linked to mild cognitive impairment and dementia over a median follow-up of 4 years.70 In terms of mental health and quality of life, patients with higher MWI had worse mental health-related quality of life.71 In addition, risk of suicide mortality was increased (2-3 fold higher risk in adults in the highest vs. lowest quartile MWI). 71 Two systematic reviews and meta-analyses that included 40 and 74 studies, respectively, also demonstrated that patients with multimorbidity (variable definitions) were more likely to develop depression and reported decreased overall quality of life.72,73
Effects of Multimorbidity on Healthcare Utilization and Costs
Hospitalization leads to decline in physical and cognitive functioning, increased disability, and poor quality of life.74,75 Therefore, there are efforts to optimize outpatient management and prevent hospitalization among older adults. Patients with multimorbidity visit their primary care providers and specialists more often, and are more likely to be admitted to the hospital and experience a longer hospital length of stay.76,77 They are also more likely to require long-term care services.78 Multimorbidity thereby contributes to higher healthcare costs and a significant economic burden.79
Effects of Multimorbidity On Outcomes in Older Adults With Various Diseases
The negative impact of multimorbidity is consistent across various diseases. For example, among long-term breast cancer survivors, multimorbidity (assessed on a continuous scale) is associated with reduced physical functioning.80 Older adults with cancer and multimorbidity also experience higher cancer-specific and overall mortality.81,82 Among older patients with heart failure, those with multimorbidity (assessed on a continuous scale) reported lower quality of life.83 Among middle-aged and older adults with diabetes, its combination with multimorbidity (specifically high depressive symptoms and stroke) also increases the risk of disability.84 These findings reinforce the impact of multimorbidity on health outcomes in all older adults across all settings.
Effects of Multimorbidity On Outcomes in Middle- and Lower- Income Countries
Multimorbidity is not limited to high-income countries. In middle- and lower- income countries, multimorbidity is similarly associated with functional limitation, depression, poor self-rated health, and lower quality of life, although data is more limited in these settings.85 They are also more susceptible to developing disability.86 In addition, each unit increase in multimorbidity count increases the cumulative risk of care dependence (needing help from caregivers) by 20%.87 Mental- (e.g., depression and anxiety) and cognitive-related multimorbidity (e.g., dementia) were found to increase the risk of care dependence more than physical multimorbidity.
Together, the aforementioned studies suggest that multimorbidity is a global health challenge and highlight the need for healthcare systems to better care for this growing population as well as to better incentivize healthcare providers to provide the necessary complex care. Interventions are needed to address risk factors for disease, including obesity, physical inactivity and poor nutrition. Interventions are also required to address the effects of multimorbidity on disability once it occurs.
References
- 1.van den Akker M, Buntinx F, Knottnerus JA. Comorbidity or multimorbidity. European Journal of General Practice. 1996;2(2):65–70. [Google Scholar]
- 2.Yancik R, Ershler W, Satariano W, Hazzard W, Cohen HJ, Ferrucci L. Report of the national institute on aging task force on comorbidity. J Gerontol A Biol Sci Med Sci. 2007;62(3):275–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: A systematic review of the literature. Ageing Research Reviews. 2011;10(4):430–439. [DOI] [PubMed] [Google Scholar]
- 4.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of chronic diseases. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 5.de Groot V, Beckerman H, Lankhorst GJ, Bouter LM. How to measure comorbidity: a critical review of available methods. Journal of clinical epidemiology. 2003;56(3):221–229. [DOI] [PubMed] [Google Scholar]
- 6.LINN BS, LINN MW, GUREL L. CUMULATIVE ILLNESS RATING SCALE. Journal of the American Geriatrics Society. 1968;16(5):622–626. [DOI] [PubMed] [Google Scholar]
- 7.Huntley AL, Johnson R, Purdy S, Valderas JM, Salisbury C. Measures of Multimorbidity and Morbidity Burden for Use in Primary Care and Community Settings: A Systematic Review and Guide. The Annals of Family Medicine. 2012;10(2):134–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller MD, Paradis CF, Houck PR, et al. Rating chronic medical illness burden in geropsychiatric practice and research: Application of the Cumulative Illness Rating Scale. Psychiatry Research. 1992;41(3):237–248. [DOI] [PubMed] [Google Scholar]
- 9.Wei MY, Kabeto MU, Langa KM, Mukamal KJ. Multimorbidity and Physical and Cognitive Function: Performance of a New Multimorbidity-Weighted Index. The Journals of Gerontology: Series A. 2017;73(2):225–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wei MY, Mukamal KJ. Multimorbidity, Mortality, and Long-Term Physical Functioning in 3 Prospective Cohorts of Community-Dwelling Adults. American journal of epidemiology. 2018;187(1):103–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sei Lee AS, Eric Widera. Multimorbidity-Weighted Index. https://eprognosis.ucsf.edu/mwi.php. Accessed. [Google Scholar]
- 12.Violan C, Foguet-Boreu Q, Flores-Mateo G, et al. Prevalence, Determinants and Patterns of Multimorbidity in Primary Care: A Systematic Review of Observational Studies. PLOS ONE. 2014;9(7):e102149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Organization WH. World health statistics 2018: monitoring health for the SDGs, sustainable develoment goals. 2018.
- 14.Nguyen H, Manolova G, Daskalopoulou C, Vitoratou S, Prince M, Prina AM. Prevalence of multimorbidity in community settings: A systematic review and meta-analysis of observational studies. J Comorb. 2019;9:2235042X19870934–12235042X19870934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Oostrom SH, Gijsen R, Stirbu I, et al. Time Trends in Prevalence of Chronic Diseases and Multimorbidity Not Only due to Aging: Data from General Practices and Health Surveys. PloS one. 2016;11(8):e0160264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ward BW, Schiller JS. Prevalence of multiple chronic conditions among US adults: estimates from the National Health Interview Survey, 2010. Prev Chronic Dis. 2013;10:E65–E65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agborsangaya CB, Lau D, Lahtinen M, Cooke T, Johnson JA. Multimorbidity prevalence and patterns across socioeconomic determinants: a cross-sectional survey. BMC public health. 2012;12(1):201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. [DOI] [PubMed] [Google Scholar]
- 19.Dhalwani NN, Zaccardi F, O’Donovan G, et al. Association Between Lifestyle Factors and the Incidence of Multimorbidity in an Older English Population. The Journals of Gerontology: Series A. 2016;72(4):528–534. [DOI] [PubMed] [Google Scholar]
- 20.Wikström K, Lindström J, Harald K, Peltonen M, Laatikainen T. Clinical and lifestyle-related risk factors for incident multimorbidity: 10-year follow-up of Finnish population-based cohorts 1982–2012. European Journal of Internal Medicine. 2015;26(3):211–216. [DOI] [PubMed] [Google Scholar]
- 21.Ruel G, Shi Z, Zhen S, et al. Association between nutrition and the evolution of multimorbidity: The importance of fruits and vegetables and whole grain products. Clinical Nutrition. 2014;33(3):513–520. [DOI] [PubMed] [Google Scholar]
- 22.Fortin M, Haggerty J, Almirall J, Bouhali T, Sasseville M, Lemieux M. Lifestyle factors and multimorbidity: a cross sectional study. BMC public health. 2014;14(1):686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Booth FW, Laye MJ. Lack of adequate appreciation of physical exercise's complexities can pre-empt appropriate design and interpretation in scientific discovery. J Physiol. 2009;587(Pt 23):5527–5539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Laurin D, Verreault R, Lindsay J, MacPherson K, Rockwood K. Physical Activity and Risk of Cognitive Impairment and Dementia in Elderly Persons. Archives of Neurology. 2001;58(3):498–504. [DOI] [PubMed] [Google Scholar]
- 25.Podewils LJ, Guallar E, Kuller LH, et al. Physical Activity, APOE Genotype, and Dementia Risk: Findings from the Cardiovascular Health Cognition Study. American journal of epidemiology. 2005;161(7):639–651. [DOI] [PubMed] [Google Scholar]
- 26.Bassuk SS, Manson JE. Epidemiological evidence for the role of physical activity in reducing risk of type 2 diabetes and cardiovascular disease. Journal of applied physiology (Bethesda, Md : 1985). 2005;99(3):1193–1204. [DOI] [PubMed] [Google Scholar]
- 27.Hotting K, Roder B. Beneficial effects of physical exercise on neuroplasticity and cognition. Neuroscience and biobehavioral reviews. 2013;37(9 Pt B):2243–2257. [DOI] [PubMed] [Google Scholar]
- 28.Hudon C, Soubhi H, Fortin M. Relationship between multimorbidity and physical activity: Secondary analysis from the Quebec health survey. BMC public health. 2008;8(1):304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Autenrieth CS, Kirchberger I, Heier M, et al. Physical activity is inversely associated with multimorbidity in elderly men: results from the KORA-Age Augsburg Study. Preventive medicine. 2013;57(1):17–19. [DOI] [PubMed] [Google Scholar]
- 30.Kaplan MS, Newsom JT, McFarland BH, Lu L. Demographic and psychosocial correlates of physical activity in late life. American journal of preventive medicine. 2001;21(4):306–312. [DOI] [PubMed] [Google Scholar]
- 31.Farooqui AA. Effects of the High Calorie Diet on the Development of Chronic Visceral Disease. In: Farooqui AA, ed. High Calorie Diet and the Human Brain: Metabolic Consequences of Long-Term Consumption. Cham: Springer International Publishing; 2015:219–244. [Google Scholar]
- 32.Dekker LH, de Borst MH, Meems LMG, de Boer RA, Bakker SJL, Navis GJ. The association of multimorbidity within cardio-metabolic disease domains with dietary patterns: A cross-sectional study in 129 369 men and women from the Lifelines cohort. PLOS ONE. 2019;14(8):e0220368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shi Z, Ruel G, Dal Grande E, Pilkington R, Taylor AW. Soft drink consumption and multimorbidity among adults. Clinical Nutrition ESPEN. 2015;10(2):e71–e76. [DOI] [PubMed] [Google Scholar]
- 34.Fontana L, Hu FB. Optimal body weight for health and longevity: bridging basic, clinical, and population research. Aging cell. 2014;13(3):391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kivimäki M, Kuosma E, Ferrie JE, et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. The Lancet Public Health. 2017;2(6):e277–e285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rachel Lipari SVH. Smoking and Mental Illness Among Adults in the United States. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; March 30, 2017 2017. [PubMed] [Google Scholar]
- 37.Castillo-Carniglia A, Keyes KM, Hasin DS, Cerda M. Psychiatric comorbidities in alcohol use disorder. The lancet Psychiatry. 2019;6(12):1068–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease C, Prevention, National Center for Chronic Disease P, Health P, Office on S, Health. Publications and Reports of the Surgeon General. In: How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2010. [PubMed] [Google Scholar]
- 39.Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction (Abingdon, England). 2003;98(9):1209–1228. [DOI] [PubMed] [Google Scholar]
- 40.Griswold MG, Fullman N, Hawley C, et al. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2018;392(10152):1015–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barnes PJ. Mechanisms of development of multimorbidity in the elderly. European Respiratory Journal. 2015;45(3):790. [DOI] [PubMed] [Google Scholar]
- 42.Betteridge DJ. What is oxidative stress? Metabolism: clinical and experimental. 2000;49(2 Suppl 1):3–8. [DOI] [PubMed] [Google Scholar]
- 43.Pizzino G, Irrera N, Cucinotta M, et al. Oxidative Stress: Harms and Benefits for Human Health. Oxid Med Cell Longev. 2017;2017:8416763–8416763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Netea MG, Balkwill F, Chonchol M, et al. A guiding map for inflammation. Nature immunology. 2017;18(8):826–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Friedman E, Shorey C. Inflammation in multimorbidity and disability: An integrative review. Health Psychol. 2019;38(9):791–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Friedman EM, Christ SL, Mroczek DK. Inflammation Partially Mediates the Association of Multimorbidity and Functional Limitations in a National Sample of Middle-Aged and Older Adults: The MIDUS Study. J Aging Health. 2015;27(5):843–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fabbri E, An Y, Zoli M, et al. Aging and the burden of multimorbidity: associations with inflammatory and anabolic hormonal biomarkers. The journals of gerontology Series A, Biological sciences and medical sciences. 2015;70(1):63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brinkley TE, Leng X, Miller ME, et al. Chronic inflammation is associated with low physical function in older adults across multiple comorbidities. The journals of gerontology Series A, Biological sciences and medical sciences. 2009;64(4):455–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Friedman EM, Herd P. Income, education, and inflammation: differential associations in a national probability sample (The MIDUS study). Psychosomatic medicine. 2010;72(3):290–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gruenewald TL, Cohen S, Matthews KA, Tracy R, Seeman TE. Association of socioeconomic status with inflammation markers in black and white men and women in the Coronary Artery Risk Development in Young Adults (CARDIA) study. Social science & medicine (1982). 2009;69(3):451–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sinnige J, Braspenning J, Schellevis F, Stirbu-Wagner I, Westert G, Korevaar J. The prevalence of disease clusters in older adults with multiple chronic diseases--a systematic literature review. PloS one. 2013;8(11):e79641–e79641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Filipčić I, Šimunović Filipčić I, Grošić V, et al. Patterns of chronic physical multimorbidity in psychiatric and general population. Journal of psychosomatic research. 2018;114:72–80. [DOI] [PubMed] [Google Scholar]
- 53.Dhar AK, Barton DA. Depression and the Link with Cardiovascular Disease. Front Psychiatry. 2016;7:33–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Koroukian SM, Warner DF, Owusu C, Given CW. Multimorbidity redefined: prospective health outcomes and the cumulative effect of co-occurring conditions. Prev Chronic Dis. 2015;12:E55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wei MY, Kawachi I, Okereke OI, Mukamal KJ. Diverse Cumulative Impact of Chronic Diseases on Physical Health–Related Quality of Life: Implications for a Measure of Multimorbidity. American journal of epidemiology. 2016;184(5):357–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hall M, Dondo TB, Yan AT, et al. Multimorbidity and survival for patients with acute myocardial infarction in England and Wales: Latent class analysis of a nationwide population-based cohort. PLoS medicine. 2018;15(3):e1002501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Seigneurin A, Delafosse P, Tretarre B, et al. Are comorbidities associated with long-term survival of lung cancer? A population-based cohort study from French cancer registries. BMC cancer. 2018;18(1):1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chiang JI, Jani BD, Mair FS, et al. Associations between multimorbidity, all-cause mortality and glycaemia in people with type 2 diabetes: A systematic review. PLoS One. 2018;13(12):e0209585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kadam UT, Croft PR. Clinical multimorbidity and physical function in older adults: a record and health status linkage study in general practice. Family practice. 2007;24(5):412–419. [DOI] [PubMed] [Google Scholar]
- 60.Fried LP, Bandeen-Roche K, Kasper JD, Guralnik JM. Association of comorbidity with disability in older women: the Women's Health and Aging Study. Journal of clinical epidemiology. 1999;52(1):27–37. [DOI] [PubMed] [Google Scholar]
- 61.Fortin M, Lapointe L, Hudon C, Vanasse A, Ntetu AL, Maltais D. Multimorbidity and quality of life in primary care: a systematic review. Health and quality of life outcomes. 2004;2:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rizzuto D, Melis RJF, Angleman S, Qiu C, Marengoni A. Effect of Chronic Diseases and Multimorbidity on Survival and Functioning in Elderly Adults. Journal of the American Geriatrics Society. 2017;65(5):1056–1060. [DOI] [PubMed] [Google Scholar]
- 63.Nguyen QD, Wu C, Odden MC, Kim DH. Multimorbidity Patterns, Frailty, and Survival in Community-Dwelling Older Adults. J Gerontol A Biol Sci Med Sci. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. The New England journal of medicine. 2002;346(14):1061–1066. [DOI] [PubMed] [Google Scholar]
- 65.Loh KP, Mohile SG, Epstein RM, et al. Willingness to bear adversity and beliefs about the curability of advanced cancer in older adults. Cancer. 2019;125(14):2506–2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wei MY, Kabeto MU, Galecki AT, Langa KM. Physical Functioning Decline and Mortality in Older Adults With Multimorbidity: Joint Modeling of Longitudinal and Survival Data. J Gerontol A Biol Sci Med Sci. 2019;74(2):226–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jindai K, Nielson CM, Vorderstrasse BA, Quinones AR. Multimorbidity and Functional Limitations Among Adults 65 or Older, NHANES 2005-2012. Preventing chronic disease. 2016;13:E151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wei MY, Levine DA, Zahodne LB, Kabeto MU, Langa KM. Multimorbidity and cognitive decline over 14 years in older Americans. J Gerontol A Biol Sci Med Sci. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fabbri E, An Y, Zoli M, et al. Association Between Accelerated Multimorbidity and Age-Related Cognitive Decline in Older Baltimore Longitudinal Study of Aging Participants without Dementia. Journal of the American Geriatrics Society. 2016;64(5):965–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Vassilaki M, Aakre JA, Cha RH, et al. Multimorbidity and Risk of Mild Cognitive Impairment. Journal of the American Geriatrics Society. 2015;63(9):1783–1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wei MY, Mukamal KJ. Multimorbidity and Mental Health-Related Quality of Life and Risk of Completed Suicide. Journal of the American Geriatrics Society. 2019;67(3):511–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Makovski TT, Schmitz S, Zeegers MP, Stranges S, van den Akker M. Multimorbidity and quality of life: Systematic literature review and meta-analysis. Ageing Res Rev. 2019;53:100903. [DOI] [PubMed] [Google Scholar]
- 73.Read JR, Sharpe L, Modini M, Dear BF. Multimorbidity and depression: A systematic review and meta-analysis. Journal of affective disorders. 2017;221:36–46. [DOI] [PubMed] [Google Scholar]
- 74.Patrick L, Gaskovski P, Rexroth D. Cumulative illness and neuropsychological decline in hospitalized geriatric patients. The Clinical neuropsychologist. 2002;16(2):145–156. [DOI] [PubMed] [Google Scholar]
- 75.Moen K, Ormstad H, Wang-Hansen MS, Brovold T. Physical function of elderly patients with multimorbidity upon acute hospital admission versus 3 weeks post-discharge. Disability and rehabilitation. 2018;40(11):1280–1287. [DOI] [PubMed] [Google Scholar]
- 76.Bahler C, Huber CA, Brungger B, Reich O. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: a claims data based observational study. BMC health services research. 2015;15:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Frolich A, Ghith N, Schiotz M, Jacobsen R, Stockmarr A. Multimorbidity, healthcare utilization and socioeconomic status: A register-based study in Denmark. PLoS One. 2019;14(8):e0214183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Koller D, Schon G, Schafer I, Glaeske G, van den Bussche H, Hansen H. Multimorbidity and long-term care dependency--a five-year follow-up. BMC Geriatr. 2014;14:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wang L, Si L, Cocker F, Palmer AJ, Sanderson K. A Systematic Review of Cost-of-Illness Studies of Multimorbidity. Applied health economics and health policy. 2018;16(1):15–29. [DOI] [PubMed] [Google Scholar]
- 80.Cohen HJ, Lan L, Archer L, Kornblith AB. Impact of age, comorbidity and symptoms on physical function in long-term breast cancer survivors (CALGB 70803). Journal of geriatric oncology. 2012;3(2):82–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kimmick GG, Li X, Fleming ST, et al. Risk of cancer death by comorbidity severity and use of adjuvant chemotherapy among women with locoregional breast cancer. Journal of geriatric oncology. 2018;9(3):214–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jorgensen TL, Hallas J, Friis S, Herrstedt J. Comorbidity in elderly cancer patients in relation to overall and cancer-specific mortality. British journal of cancer. 2012;106(7):1353–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Buck HG, Dickson VV, Fida R, et al. Predictors of hospitalization and quality of life in heart failure: A model of comorbidity, self-efficacy and self-care. International journal of nursing studies. 2015;52(11):1714–1722. [DOI] [PubMed] [Google Scholar]
- 84.Quinones AR, Markwardt S, Botoseneanu A. Diabetes-Multimorbidity Combinations and Disability Among Middle-aged and Older Adults. Journal of general internal medicine. 2019;34(6):944–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Arokiasamy P, Uttamacharya U, Jain K, et al. The impact of multimorbidity on adult physical and mental health in low- and middle-income countries: what does the study on global ageing and adult health (SAGE) reveal? BMC medicine. 2015;13:178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Su P, Ding H, Zhang W, et al. The association of multimorbidity and disability in a community-based sample of elderly aged 80 or older in Shanghai, China. BMC Geriatr. 2016;16(1):178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bao J, Chua KC, Prina M, Prince M. Multimorbidity and care dependence in older adults: a longitudinal analysis of findings from the 10/66 study. BMC public health. 2019;19(1):585. [DOI] [PMC free article] [PubMed] [Google Scholar]