Abstract
[Purpose] To promote community involvement in children, the factors that influence and limit their participation must be well understood. The purpose of this study was to clarify the factors that limit the community participation of children with disabilities. [Participants and Methods] In total, 235 questionnaires were distributed to parents at special support schools, pediatric hospitals, home-visit nursing stations, and after-school daycare services in Tokyo, Gunma, Hiroshima, and Saga prefectures in Japan. Data related to the Participation and Environment Measure for Children and Youth, age, height, weight, gross motor function, presence of medical care, diagnosis, and parental age were recorded for school-aged children. [Results] Multiple regression analysis using the 100 valid questionnaire responses revealed that the number of community activities that the children participated in depended on the children’s need for medical care (standardized partial regression coefficient: −0.20). The frequency was affected by gross motor function (standardized partial regression coefficient: −0.24). When respiratory, feeding, and excretion-related medical care were required, the children tended to participate in fewer community activities. [Conclusion] Community participation is influenced by the different factors in each aspect analyzed (number of activities, frequency, and degree of involvement). The factors that should be considered when promoting children’s participation in rehabilitation must be identified.
Key words: Children with disabilities, Participation in community, Need for medical care
INTRODUCTION
Although the mortality rate of premature and very-low-birth weight infants is low in Japan owing to the advancement in perinatal care1), children can still have a wide range of disabilities. Furthermore, the numbers of children with severe motor limitations and those who require medical care at home are increasing in Japan. This is a similar trend not only in Japan but also in other countries2). In Japan, the Ministry of Health, Labour and Welfare is trying to expand support for children with disabilities to enable living at home3).
Home health care for children with disabilities allow patients to live safely with their family, maintain a good quality of life, promote development, and prevent secondary disabilities. Since the introduction of these concepts by The International Classification of Functioning, Disability and Health by the World Health Organization 20 years ago, participation or involvement in a life situation (activities of daily living) has become one of the key components4, 5). For a child with a disability to be able to live safely with the family, physical therapists need to focus not only on the child’s physical function but also on their participation. In particular, it is important to promote participation in the community after leaving the hospital.
However, there are currently no established interventions aimed at improving participation6). To promote participation in the community, it is necessary to know what factors influence and limit their participation. Previous studies have reported that disabilities and younger age limit participation7, 8). However, given the increasing number of children in need of medical care, it is necessary to clarify the relationship between medical care and participation. Certain medical devices may limit or prohibit participation in some community activities because of physical, spatial and time factors. A children’s participation in the community is likely to be influenced by a variety of factors, so there is a need to identify these factors that influence participation or, in particular, those factors that necessitate medical care.
The purpose of this study was to clarify the limiting factors of participation of children with disabilities in the community. We used The Participation and Environment Measure for Children and Youth (PEM-CY), which is a method of assessing a child’s participation in terms of the number of items of participation, frequency, and level of involvement9). In this study, we investigated the factors affecting the PEM-CY findings through a questionnaire.
PARTICIPANTS AND METHODS
This was a cross-sectional study. A questionnaire was conducted by mail.
Patients were recruited from July 2019 to February 2020. Data related to PEM-CY (community setting), age, height, weight, gross motor function, use of medical care, diagnosis, and parental age, were collected through a questionnaire survey administered from October 2019 to March 2020. Parents were deemed eligible for the study if they provided consent by signing the beginning of the questionnaire, if their child had a physical disability, and if the child was school-aged (between 6 and 18 years of age; from elementary school to high school graduation) at the time of enrollment. In the case of hospitalization, the child was excluded. Two hundred and thirty-five questionnaires were distributed to parents by the teachers at special support schools, and by the staff (therapists and nurses) at childcare hospitals, home-visit nursing stations, and after-school daycare services in Tokyo, Gunma, Hiroshima, and Saga prefectures in Japan. The completed questionnaires were returned to Tokyo Metropolitan University with the enclosed return envelope. This study was approved by the institutional research ethics committee of the Tokyo Metropolitan University Arakawa Campus (approval number 19040) and Mejiro University (approval number 19-40).
The PEM-CY is a parent-report instrument that examines participation and environment across three settings: home, school, and community9). There are 10 items in the participation section for the community setting, including neighborhood outings, community events, organized physical activities, unstructured physical activities, classes and lessons (not school sponsored), groups/clubs/volunteer activities, religious or spiritual gatherings and activities, getting together with other children in the community, working for pay, and overnight visits or trips.
The PEM-CY consists of queries regarding the number of items of participation, frequency, involvement, or interest and change in desire for each item. In this study, the number of items, frequency, and involvement in the community setting for the participation section were analyzed. The frequency over the past 4 months ranged from daily to never (7 to 0 points). The frequency of participation was asked for each of the 10 items of community setting participation, and we counted other than those that answered “never” with respect to frequency. These were used as the “number of items”. For example, if a respondent answered “never” for 3 of the 10 items in frequency, the “number of items” would be 7. Involvement scores were counted, except in cases where the frequency response was never, and they ranged from very involved to minimally involved (5 to 1 points). Involvement refers to how engaged or interested a child is in an activity using whatever supports, assistance, adaptations, or methods routinely used or has available9). The frequency and involvement scores were computed as the average (average values were calculated by excluding the items that answered “never” in terms of frequency). The reliability and validity of the Japanese version of PEM-CY have been examined previously in a pilot study involving 100 disabled children and 34 healthy children, and a high reliability with an intraclass correlation coefficient of 3.1 (0.73–0.96) and small to moderate validity (effect size between 0.05 and 0.32) were noted.
In Japan, “medical care” is not a legally defined concept, but it generally refers to medical practices, such as the aspiration of phlegm, tube feeding, and sanitary management of a tracheotomy, which is performed daily in schools and at home. In this study, ventilator management was defined as medical care with a ventilator. Tracheostomy, oxygen inhalation or SpO2 less than 90% in more than 10% of the day, suction (1 time/hour or more), and nebulizer use (more than 6 times/day or continuous use) were defined as respiratory-related care; treatment with tube feeding (including gastrostomy and enterostomy) was defined as feeding-related care; and catheterization (3 or more times/day) and stoma were defined as excretion-related care. If any of the above conditions were met, we considered the participants to use medical care.
The Gross Motor Function Classification System (GMFCS) is a classification scale to measure the severity of motor performance for children with cerebral palsy10). The GMFCS is used for compartmentalization of gross motor functions and predictive purposes. Prognosis varies by disease; therefore, the GMFCS cannot be used as a predictive evaluation method in diseases other than cerebral palsy. However, the GMFCS can be used to compartmentalize motor function in other diseases11). In this study, the GMFCS was used for the compartmentalization of gross motor function and not for predictive purposes. Severity was classified into five functional levels based on the child’s gross motor skills, which included mainly sitting and mobility skills. Level I was defined as the ability to leap and run without restriction. Level II was the ability to walk in most environments. Level III was defined as the ability to walk using a hand-held mobility device in an indoor environment. Level IV required physical assistance in most living environments, and Level V was the requirement of full physical assistance in all environments. In this study, the number that best described the child’s motor function was recorded on the questionnaire. Levels I–II, those who can go around without the help of others or the use of tools, were defined as high functioning, and levels III–V, those who need to use the help or tools of others to get around, were defined as low functioning.
We included children’s ages in the survey because it has been reported that community participation increases with age9). Parental age and the weight and height of children were included in the survey because they were thought to be related to the sense of caregiving burden.
SPSS Statistics version 24 (IBM Corp.) was used for statistical analysis. The χ2 test and Kruskal-Wallis test were used to examine differences in the degree of gross motor function, proportion of medical care use, and differences in PEM-CY scores in the community and institutions. To analyze factors influencing a child’s participation in the community, 1) the correlation between each PEM-CY score and the child’s age, height, weight, and parents’ ages were examined by calculating the Spearman’s rank correlation coefficients; and 2) the Mann-Whitney U-test was used to perform comparisons between groups with high and low gross motor function and between groups with and without medical care. Next, multiple regression analysis (forced entry method) was conducted. The independent variables were those items that were significantly different or significantly correlated in the previous statistics (1 and 2). The PEM-CY score (number of items, frequency, and level of involvement) was the dependent variable. High and low gross motor function and the use of medical care were transformed into dummy variables (GMFCS, high: 0, low: 1; use of medical care, no: 0, yes: 1).
If medical care was found to be a significant item in the multiple regression analysis, it was examined in more detail. If it was significant in the number of items, the χ2 test for the PEM-CY sub-items and medical care details was performed. If it was significant in the frequency and involvement, we conducted a Mann-Whitney U test with the scores of the PEM-CY sub-items as the dependent variable and the use of the medical care sub-items as the independent variable.
RESULTS
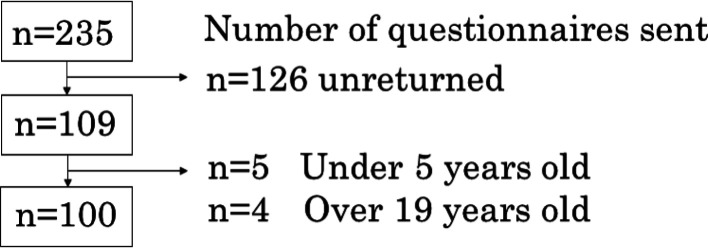
A total of 235 questionnaires were distributed, and 100 valid responses were obtained (Fig. 1). The results for gender, age, height, weight, diagnosis, gross motor function, and medical care are shown in Table 1.
Fig. 1.
Participant enrolment flow chart.
Table 1. Demographic characteristics of the participants.
| Total (n) | 100 |
| Parents | |
| Gender (n) | Male: 4, Female: 96 |
| Age (years), mean ± SD | 44.1 ± 5.2 |
| Children | |
| Gender (n) | Male: 48, Female: 52 |
| Age (years), mean ± SD | 11.9 ± 3.6 |
| Height (cm), mean ± SD | 130.2 ± 18.6 |
| Weight (kg), mean ± SD | 27.1 ± 10.9 |
| Diagnoses (n) | |
| Cerebral palsy | 51 |
| Chromosomal abnormalities | 18 |
| Neuromuscular diseases | 14 |
| Malignant tumors | 3 |
| Osteoarthritic diseases | 3 |
| Metabolic disorder | 2 |
| Endocrine diseases | 1 |
| Unknown | 8 |
| Medical care (n) | |
| Ventilator | 15 |
| Respiratory-related | 19 |
| Feeding-related | 30 |
| Excretion-related | 7 |
| Gross motor function (n) | |
| High function grade | 32 (I: 2, II: 14, III: 15) |
| Low function grade | 69 (IV: 20, V: 49) |
Differences in the degree of gross motor function, percentage of medical care use, and differences in PEM-CY scores in the community and institutions were examined, with a significant difference in all items except for the frequency of PEM-CY (Table 2).
Table 2. Response rate, degree of gross motor capacity, medical care use, and PEM-CY results for each region and facility.
| Area | Institution | ||||||||||
| ALL | Tokyo | Hiroshima | Gunma | Hospital | Home-visit nursing stations | Special support schools | After-school daycare services | ||||
| Response rate (Number of responses/distributed) | 42.5% (100/235) | 40% (44/110) | 47.1% (49/104) | 43.7% (7/16) | 80% (12/15) | 47.1% (49/104) | 30.9% (26/84) | 48.1% (13/27) | |||
| GMFCS rate | |||||||||||
| high | 21% | 10% | 0% | ** | 7% | 10% | 13% | 1% | ** | ||
| low | 23% | 39% | 7% | 5% | 39% | 13% | 12% | ||||
| Medical care rate | |||||||||||
| No | 33% | 28% | 0% | ** | 11% | 28% | 21% | 1% | ** | ||
| Yes | 11% | 21% | 7% | 1% | 21% | 5% | 12% | ||||
| PEM-CY | |||||||||||
| Number of items | 4.0 ± 2.1 | 4.7 ± 2.2 | 3.6 ± 1.9 | 2.6 ± 1.3 | * | 4.5 ± 2.4 | 3.6 ± 1.9 | 5.1 ± 2.1 | 2.8 ± 1.8 | ** | |
| Frequency | 2.8 ± 1.1 | 2.8 ± 0.8 | 2.8 ± 1.1 | 2.2 ± 1.1 | 2.9 ± 0.7 | 2.8 ± 1.1 | 2.9 ± 0.7 | 2.3 ± 1.2 | |||
| Involvement | 3.6 ± 1.2 | 4.1 ± 0.8 | 3.4 ± 1.3 | 3.0 ± 1.7 | ** | 4.3 ± 1.0 | 3.4 ± 1.3 | 3.9 ± 0.7 | 3.6 ± 1.5 | * | |
No valid responses were obtained from Saga prefectures, to which five questionnaires were sent.
The χ2 test was used to examine differences in the degree of gross motor capacity and proportion of medical care use.
The Kruskal-Wallis test was used to examine differences in PEM-CY scores.
*p<0.05, **p<0.01.
GMFCS: Gross Motor Function Classification System; PEM-CY: Participation and Environment Measure for Children and Youth.
Spearman rank correlation coefficients were calculated, and significant positive correlations of a child’s height and weight with the number of items and the involvement ware observed. Significant negative correlations of child’s and parent’s age with the frequency were observed. Results of the Mann-Whitney U-test showed significant differences in the number of items and frequency between high and low gross motor function groups and the use and absence of medical care groups (Table 3).
Table 3. Correlation analysis and intergroup comparisons.
| Gross Motor Function mean ± SD | Presence of medical care mean ± SD | Children | Parent | ||||||||||||||
| Low | High | Yes | No | Age | Height | Weight | Age | ||||||||||
| Number of items | 2.1 | 5.1 ± 1.6 | * | 3.3 ± 1.9 | 4.4 ± 2.1 | ** | −0.01 | 0.29 | ** | 0.36 | ** | 0.09 | |||||
| Frequency | 2.6 ± 1.0 | 3.5 ± 1.0 | ** | 2.5 ± 1.2 | 2.9 ± 0.8 | ** | −0.21 | * | −0.10 | 0.01 | −0.21 | * | |||||
| Involvement | 3.6 ± 1.2 | 3.5 ± 0.9 | 3.3 ± 1.4 | 3.8 ± 0.9 | 0.05 | 0.18 | * | 0.23 | * | 0.08 | |||||||
The Mann-Whitney U-test was used to perform comparisons between groups with high and low gross motor function and between groups with and without medical care.
Spearman rank correlation coefficients with PEM-CY are listed under age, height, and weight of the child and parental age.
*p<0.05, **p<0.01.
PEM-CY: Participation and Environment Measure for Children and Youth.
Multiple regression analysis revealed that the number of items was affected by the use of medical care. Frequency was affected by gross motor function (Table 4). The variance inflation factor (VIF) was 1.06–2.94.
Table 4. Results of multiple regression analysis.
| Number of items | Frequency | Involvement | ||||||||||||
| B | β | VIF | B | β | VIF | B | β | VIF | ||||||
| (Intercept) | 16.86 | 4.07 | ** | 2.38 | ||||||||||
| Gross motor function | −10.67 | −0.18 | 1.06 | −0.67 | −0.24 | * | 1.15 | |||||||
| Use of medical care | −8.64 | −0.20 | * | 1.12 | −0.31 | −0.15 | 1.12 | |||||||
| Children age | −0.03 | −0.12 | 1.48 | |||||||||||
| Children height | 0.21 | 0.19 | 2.85 | 0.01 | 0.10 | 2.73 | ||||||||
| Children weight | 0.28 | 0.14 | 2.94 | 0.02 | 0.16 | 2.73 | ||||||||
| Parent age | −0.01 | −0.03 | 1.44 | |||||||||||
| R2 | 0.20 | 0.10 | 0.06 | |||||||||||
β, standardized partial regression coefficient; B: partial regression coefficient; VIF: variance inflation factor.
*p<0.05, **p<0.01.
As medical care increased as a significant item in the “number of items” in the multiple regression analysis, the chi-square test was performed, and the results showed that “community events” was when feeding-related care is needed, “getting together with other children in the community” was when respiratory-related care and feeding-related care was needed, “unstructured physical activities” was when feeding-related care was needed, “classes and lessons” was when excretion-related care was needed, and “overnight visits or trips” was when feeding-related care was required, with a high percentage of participants unable to participate (Table 5).
Table 5. χ2 test results for the PEM-CY sub-items and medical care details.
| Ventilator | Respiratory-related | Feeding-related | Excretion-related | ||||||||||||
| Yes | No | Yes | No | Yes | No | Yes | No | ||||||||
| Neighborhood outings | Yes | 14 | 85 | 18 | 81 | 29 | 70 | 7 | 92 | ||||||
| No | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | |||||||
| Community events | Yes | 10 | 58 | 11 | 57 | 15 | 53 | * | 3 | 62 | |||||
| No | 5 | 27 | 8 | 24 | 15 | 17 | 1 | 31 | |||||||
| Getting together with other children in the community | Yes | 2 | 35 | 2 | 35 | * | 6 | 31 | * | 4 | 33 | ||||
| No | 13 | 50 | 17 | 46 | 24 | 39 | 3 | 60 | |||||||
| Organized physical activities | Yes | 3 | 25 | 4 | 24 | 6 | 22 | 2 | 26 | ||||||
| No | 12 | 60 | 15 | 57 | 24 | 48 | 5 | 67 | |||||||
| Unstructured physical activities | Yes | 3 | 28 | 3 | 28 | 4 | 27 | * | 3 | 28 | |||||
| No | 12 | 57 | 16 | 53 | 26 | 43 | 4 | 65 | |||||||
| Classes and lessons | Yes | 5 | 34 | 6 | 33 | 8 | 31 | 6 | 33 | * | |||||
| No | 10 | 51 | 13 | 48 | 22 | 39 | 1 | 60 | |||||||
| Organizations, groups, clubs, and volunteer or leadership activities | Yes | 1 | 17 | 1 | 17 | 3 | 15 | 2 | 16 | ||||||
| No | 14 | 68 | 18 | 64 | 27 | 55 | 5 | 77 | |||||||
| Religious or spiritual gatherings and activities | Yes | 1 | 4 | 2 | 3 | 2 | 3 | 0 | 5 | ||||||
| No | 14 | 81 | 17 | 78 | 28 | 67 | 7 | 88 | |||||||
| Working for pay | Yes | 1 | 6 | 1 | 6 | 1 | 6 | 0 | 7 | ||||||
| No | 14 | 79 | 18 | 75 | 29 | 64 | 7 | 86 | |||||||
| Overnight visits or trips | Yes | 9 | 65 | 12 | 62 | 17 | 57 | * | 6 | 68 | |||||
| No | 6 | 20 | 7 | 19 | 13 | 13 | 1 | 25 | |||||||
*p<0.05.
PEM-CY: Participation and Environment Measure for Children and Youth.
DISCUSSION
Multiple regression analysis between extracted items and the PEM-CY score revealed that the factors that affected the number of items, frequency, and involvement in the community were different, and number of items in the community setting was affected by the use of medical care. When the VIF was >10, multicollinearity was suspected, but our VIF in this study was low. The low VIF value indicates that gross motor function and medical care should be considered as independent factors. The results of the χ2 test of the community setting sub-items of the PEM-CY and the type of medical care revealed that the medical care affected by the type of participation item differed.
The results of this study revealed that gross motor function had a small effect on participation items in the community setting, but it had a significant effect on frequency. It has been reported that a child’s gross motor function is negatively correlated with physical independence and mobility12) and that children with disabilities have a limited participation frequency compared to normal children7, 13). It was suggested that the frequency in the community setting was lower when they were less independent and required assistance. However, the use of medical care was found to increase the number of items that prevented participation but had a low effect on frequency. On the other hand, multiple regression analysis revealed that the height, weight, and age of children and parental age did not affect the number, frequency, or level of community involvement of children.
The results of the number of items in the community setting and the chi-square test results of medical care use showed that respiratory-related care, feeding-related care, and elimination-related care had an effect. Feeding-related medical care is an important means of nutrition for children who are unable to take their food orally because of aspiration or reflux14). It has been also reported that the introduction of feeding-related medical care improves the quality of life of parents15). However, if feeding-related medical care is used, it is necessary to prepare for tube feeding, clean up, and rest after eating to avoid reflux. These factors may limit participation in community events, such as festivals and trips that involve meals. The use of tube feeding was also found to limit the use of “getting together with other children in the community” and “unstructured physical activities” that involve physical movement and mobility, and because tube feeding does not limit movement, it is thought that rest and other confounding factors of tube feeding may have affected participation. Respiratory-related medical care includes tracheostomy and inhalation to secure the airway and O2 to secure SpO216). This care may be difficult to provide when patients are outdoors and their destination is not stable, such as “going out with other children”, which may limit their participation. The use of excretion-related care, such as urinary induction and colostomy, requires a space for care and understanding of others. In particular, when a colostomy is used, a special toilet and a space to deal with leakage are required. In this study, participation in “classes and lessons”, in which the participation rate decreases when medical care related to toileting is needed, is considered to be limited because of the lack of such an environment.
This study has a few limitations. First, we were unable to examine regional differences and environmental effects on participation. This is because the number of participants differed greatly between regions and facilities, resulting in differences in scores between these regions and facilities. Second, this study involved a survey conducted by mail; therefore, the author could not observe the children in the real-world setting. Therefore, there may be dissociation between the results returned in the questionnaire and the actual GMFCS levels. Third, there was variation in the illnesses of the children who were included in the study, and we were unable to examine the effect of the characteristics of the illnesses on their participation. This is considered to be a limitation of this study. Lastly, the economic situation, jobs of the parents, and educational background, which are supposed to affect family participation, were not examined in this study because of ethical considerations17). It has been also reported that there was a correlation between gross motor function and intellectual function18), which may have been a confounding factor. Therefore, the results of this study need to be validated further before they can be generalized.
Gross motor function and use of medical care were found to be factors that affected the participation of children with disabilities in the community. In particular, the number of items of community activities that the children could not participate in tended to increase when respiratory-related medical care, feeding-related medical care and excretion-related medical car were included in the study. Thus, it is necessary to determine which factors should be considered when promoting participation in rehabilitation. The effect of the rehabilitation approach on participation has not been clarified and needs to be clarified in the future.
Funding
This study was funded by the Japan Academy of Health Sciences.
Conflict of interest
There are no conflicts of interest to declare.
Acknowledgments
This study was funded by the Japan Academy of Health Sciences. I would like to express our gratitude to Ms. Tamaru of Kirigaoka Special Support School, University of Tsukuba, Ms. Kogure of After School Day Service Hibiki, Mr. Koyanagi of Visiting Nurse Station Asuka, and Mr. Mori of Orthopaedic Surgery Ryu for their cooperation in data collection.
REFERENCES
- 1.United Nations Children’s Fund: New York: Levels and trends in child mortality 2019. https://www.unicef.org/sites/default/files/2019–10/UN-IGME-child-mortality-report-2019 (Accessed Nov. 3, 2020)
- 2.Chau SK, Yung AW, Lee SL: Long-term management for ventilator-assisted children in Hong Kong: 2 decades’ experience. Respir Care, 2017, 62: 54–64. [DOI] [PubMed] [Google Scholar]
- 3.Ministry of Health, Labor and Welfare: Tokyo: Iryotekikea ga hituyouna syougaiji eno siennjujitu ni mukete [To improve support for children with disabilities with medical care needs]. https://www.mhlw.go.jp/file/06-Seisakujouhou-12200000-Shakaiengokyokushougaihokenfukushibu/0000180993.pdf (Accessed Nov. 3, 2020)
- 4.World Health Organization: Geneva: International classification of functioning, disability and health: ICF. https://apps.who.int/iris/bitstream/handle/10665/42407/9241545429.pdf (Accessed Nov. 3, 2020)
- 5.World Health Organization: Geneva: International classification of functioning, disability, and health: children & youth version: ICF-CY. https://apps.who.int/iris/bitstream/handle/10665/43737/9789241547321_eng.pdf?sequence=1&isAllowed (Accessed Nov. 3, 2020)
- 6.Novak I, Honan I: Effectiveness of paediatric occupational therapy for children with disabilities: a systematic review. Aust Occup Ther J, 2019, 66: 258–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coster W, Law M, Bedell G, et al. : School participation, supports and barriers of students with and without disabilities. Child Care Health Dev, 2013, 39: 535–543. [DOI] [PubMed] [Google Scholar]
- 8.Palisano RJ, Kang LJ, Chiarello LA, et al. : Social and community participation of children and youth with cerebral palsy is associated with age and gross motor function classification. Phys Ther, 2009, 89: 1304–1314. [DOI] [PubMed] [Google Scholar]
- 9.Coster W, Bedell G, Law M, et al. : Psychometric evaluation of the participation and environment measure for children and youth. Dev Med Child Neurol, 2011, 53: 1030–1037. [DOI] [PubMed] [Google Scholar]
- 10.Palisano RJ, Rosenbaum P, Bartlett D, et al. : Content validity of the expanded and revised Gross Motor Function Classification System. Dev Med Child Neurol, 2008, 50: 744–750. [DOI] [PubMed] [Google Scholar]
- 11.Baque E, Barber L, Sakzewski L, et al. : Test-re-test reproducibility of activity capacity measures for children with an acquired brain injury. Brain Inj, 2016, 30: 1143–1149. [DOI] [PubMed] [Google Scholar]
- 12.Kerr C, McDowell B, McDonough S: The relationship between gross motor function and participation restriction in children with cerebral palsy: an exploratory analysis. Child Care Health Dev, 2007, 33: 22–27. [DOI] [PubMed] [Google Scholar]
- 13.Jeong Y, Law M, Stratford P, et al. : Measuring participation of children and environmental factors at home, school, and in community: construct validation of the Korean PEM-CY. Phys Occup Ther Pediatr, 2017, 37: 541–554. [DOI] [PubMed] [Google Scholar]
- 14.Gottrand F, Sullivan PB: Gastrostomy tube feeding: when to start, what to feed and how to stop. Eur J Clin Nutr, 2010, 64: S17–S21. [DOI] [PubMed] [Google Scholar]
- 15.Sullivan PB, Juszczak E, Bachlet AM, et al. : Impact of gastrostomy tube feeding on the quality of life of carers of children with cerebral palsy. Dev Med Child Neurol, 2004, 46: 796–800. [DOI] [PubMed] [Google Scholar]
- 16.Seddon PC, Khan Y: Respiratory problems in children with neurological impairment. Arch Dis Child, 2003, 88: 75–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khetani M, Marley J, Baker M, et al. : Validity of the participation and environment measure for children and youth (PEM-CY) for health impact assessment (HIA) in sustainable development projects. Disabil Health J, 2014, 7: 226–235. [DOI] [PubMed] [Google Scholar]
- 18.Dalvand H, Dehghan L, Hadian MR, et al. : Relationship between gross motor and intellectual function in children with cerebral palsy: a cross-sectional study. Arch Phys Med Rehabil, 2012, 93: 480–484. [DOI] [PubMed] [Google Scholar]